Abstract
Following baseline assessment, 166 patients in medication maintenance at a community mental health center who were experiencing both persistent positive symptoms of schizophrenia and impairments in functioning were randomized to 1 of 4 treatments for 9 months: (1) Cognitive Behavior Therapy for psychosis (CBTp)—a therapy designed to identify and alter reasoning and appraisal biases that contribute to the formation and maintenance of positive symptoms, (2) Cognitive Adaptation Training (CAT)—a treatment using environmental supports including signs, alarms, checklists and the organization of belongings established at weekly home visits to compensate for impairments in cognitive functioning and improve everyday functional outcomes, (3) Multi-modal Cognitive treatment—a combination of CBTp and CAT, and (4) Treatment as Usual. Data on symptoms and functional outcomes were obtained every 3 months. A mixed effects regression model with repeated measures using a 2 (CAT/no CAT) × 2 (CBT/no CBT) design indicated that functioning as measured by the Multnomah Community Ability Scale improved more in groups receiving CAT than other treatment groups. Auditory hallucinations and associated distress improved slightly more in groups receiving CAT. In this study, CBTp did not improve outcomes. Combining CAT with CBTp did not improve outcomes more than CAT alone.
Introduction
Schizophrenia is a complex illness characterized by multiple signs and symptoms. Many treatments developed for schizophrenia target specific behaviors rather than the constellation of problems associated with the illness. Cognitive Behavior Therapy for psychosis (CBTp) is a collaborative talk-therapy designed to help the individual to identify appraisal biases, cognitive distortions, and alternative explanations for events, and to find ways to cope with the distress caused by persistent psychotic symptoms. Cognitive Adaptation Training (CAT) is home-based therapy using environmental supports, such as signs, checklists, alarm reminders, and the organization of belongings to bypass cognitive and motivational impairments and improve every-day functioning. We were interested in determining whether a multimodal intervention combining these therapies would improve a broader range of outcomes for individuals with schizophrenia than either single modality treatment.
Both CBTp and CAT attempt to deal with cognitive problems in different ways. CAT uses supports in the environment to bypass formal neurocognitive deficits and cue and sequence functional behaviors.1 CBTp seeks to identify and alter emotional processes and behaviors associated with reasoning and appraisal biases that contribute to the formation and maintenance of positive symptoms and functional problems.2 The integration of treatment primarily aimed at reducing positive symptoms with another designed to cue behavior in the home is a novel multimodal approach we have called Mcog.3
Both CBTp and CAT are designed to customize treatments to the needs of the individual. CBTp accomplishes this by developing an individual problem list collaboratively with the consumer, developing an individual case formulation regarding how symptoms are formed and maintained, and by customizing homework to deal with specific aspects of the problems identified.2 CAT accomplishes this by assessing cognition, functional skills, overt behavior, and environmental triggers, and customizing the environment and supports based upon these dimensions.1 We reasoned that because these treatments address different aspects of cognitive processing, CAT and CBTp should be complementary. Post hoc analysis from previous CAT studies supported this notion.3 We examined hallucinations and delusions as rated by the Brief Psychiatric Rating Scale (BPRS) and found that patients improved to a greater extent on these symptoms when CAT was conducted by individuals trained in CBT techniques than when CAT was delivered by individuals not familiar with CBT techniques for managing positive symptoms.3
This study assessed the impact of treatments that included CAT (CAT and Mcog) vs treatments that included CBTp (CBTp and Mcog) on persistent symptoms and functional outcome. We hypothesized that treatments that included CBTp would improve symptoms and associated distress to a greater degree than treatments without CBTp and that treatments with CAT would improve community functioning to a greater extent than treatments without CAT. We hypothesized that the combined Mcog treatment would address both symptom and functional domains and thus be superior to single modality treatments.
Methods
Study Design
Participants had a diagnosis of schizophrenia or schizoaffective disorder and were seen at a community mental health center for medication follow-up. They received a baseline assessment and were randomized in a 2×2 factorial design into 1 of 4 treatment conditions for 9 months. Treatment conditions were Treatment as Usual (TAU) only, CBTp, CAT, and CAT + CBTp (Mcog). Randomization was stratified by gender and age using a computer generated algorithm created by the study statistician who had no patient contact. Assessments of symptomatology and functioning were conducted at baseline and every 3 months during treatment. There were 2 post-treatment follow-up assessments at months 12 and 15.
Participants
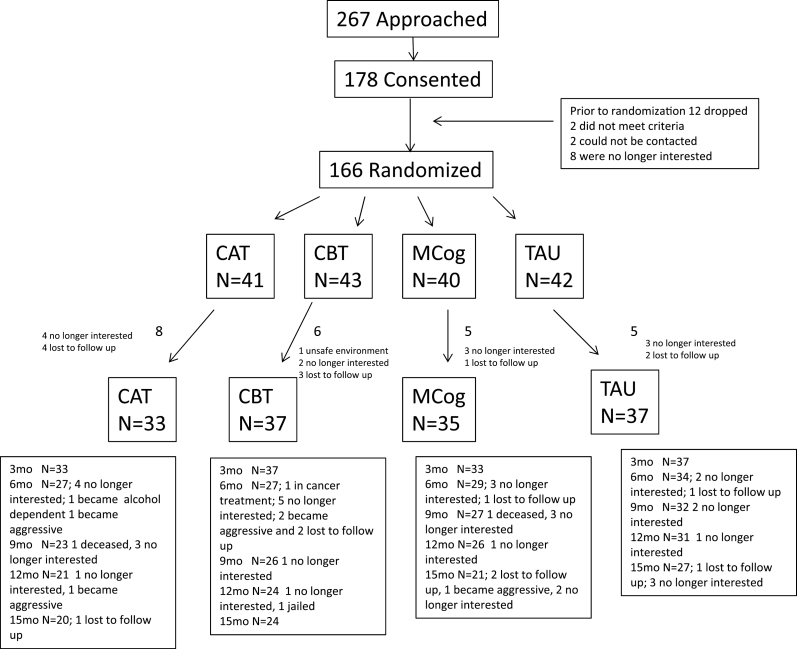
Participants were recruited from public mental health clinics in 2 counties in Texas, identified through chart reviews by research staff credentialed at participating sites in accordance with HIPAA requirements. All participants signed a written consent form approved by an Institutional Review Board. Procedures were consistent with internationally recognized standards for ethical conduct of human research. The study was registered with ClinicalTrials.gov (identifier #NCT01915017). As shown in figure 1, of the 178 patients signing consent, 166 were randomized. Of these 166, there were 142 subjects with baseline and follow-up data for data analyses. Reasons for drops are listed in the consort diagram in figure 1.
Fig. 1.
Consort diagram.
Diagnoses were confirmed utilizing the Structured Clinical Interview for DSM-IV based on chart documentation and patient interview by a trained rater.4 Participants were fluent English speakers between the ages of 18 and 60 years; receiving ongoing treatment with an oral antipsychotic; had persisting positive symptoms as evidenced by a score of ≥4 on BPRS expanded version ratings of delusions, hallucinations, and/or suspiciousness; had functional impairment as evidenced by a score of <70 on the social and occupational functioning scale; had a stable residence; and were able to understand and complete assessments. Individuals were excluded if they had a documented history of significant head trauma, seizure disorder, or mental retardation; a history of substance abuse or dependence in the past month; or a history of violence in the past 6 months (as a safety measure for staff making home visits).
Of the 142 participants with baseline assessments, 74 were male and 68 were female. Sixty-five participants were Hispanic, 40 were non-Hispanic white, 35 were African American, and 2 were from other or mixed ethnic groups. Mean age was 40.6 (S D = 11.8). The average participant did not complete high school (11.6; S D = 2.2). All patients were prescribed antipsychotic medication in clinics following the Texas Implementation of Medication Algorithms Guidelines. There were no significant differences in demographics for participants not making it to randomization vs those randomized to treatment (all P’s > .20).
Treatment Groups
All active treatments were designed to be delivered weekly for 9 months for up to 38 visits during the treatment period. Sessions lasted for ~1 hour. Missed sessions were rescheduled for later in the same week whenever possible. Different teams provided CAT and CBT/Mcog. Of the 6 therapists providing CAT, 3 had 2 years of experience with the treatment modality and 3 had no experience prior to training at the beginning of the study. Of the 6 therapists conducting CBT/Mcog, one had 1 year of experience in CBTp, 5 years of experience in standard CBT, and 20 years of experience in CAT; one had 7 years of experience with CBTp, 7 years of experience in standard CBT, and no experience in CAT prior to the study; one had no experience with CBTp, 5 years of experience in standard CBT, and no experience with CAT, 2 had no experience with CBTp, at least 2 years of experience in standard CBT, and no experience in CAT; one neither had experience in CBTp nor in standard CBT and 2 years of experience in CAT. All therapists had a minimum of 2 years of experience working with individuals with serious mental illness. All sessions for all therapies were audio recorded, and 20% of them selected randomly for each therapy were rated for fidelity and as a check that there were not CAT techniques being applied during CBTp sessions or the reverse. Supervision was conducted weekly to biweekly for all treatments to ensure fidelity to the treatment manuals, and audio tapes were reviewed in supervision on an as-needed basis.
CBTp.
CBTp is a talk therapy designed to treat persistent symptoms of psychosis and the accompanying distress. A 9-month treatment manual was developed based upon Kingdon and Turkington5 and included simple handouts and homework assignments based on the work of Granhom et al.6 The focus of the sessions was on patient identified problems, particularly those that interfered with daily functioning or were distressing, normalizing symptoms, and using CBT techniques to develop alternative explanatory models of events. Therapists were master’s and doctoral level professionals with >2 years experience in assessment and treatment of serious mental illness. All therapists participated in a 2-week formal training program delivered by Drs Turkington and Tai. Additional formal on-site training was provided annually for 4 years following the initial training. Supervision of CBTp was provided throughout the trial by Drs Turkington and Tai, through teleconference for 5 years spanned by the study. Fidelity to the CBTp model was rated by Dr Tai and her colleagues in the UK.
CAT.
CAT is a series of manual-driven compensatory strategies and environmental supports (signs, checklists, electronic cueing devices) established and maintained on weekly home visits by a CAT therapist/trainer. According to the CAT model, individuals with poor executive functioning need high levels of structure and more obviously placed environmental cues, whereas those with somewhat better executive functioning need less structure and more subtle cues.7–9 Individuals with apathetic behavior benefit from environmental supports that cue and sequence behavior. Those with disinhibition benefit most from the removal of distracting stimuli and organization of belongings, and those with mixed behavior benefit from a combination of these strategies. Cognitive Adaptation Training interventions are based on a comprehensive assessment of cognition, behavior, and the person’s environment. Assessment results yield 1 of 6 CAT classifications for which interventions can be targeted.7–9 Environmental supports in CAT target a variety of functional areas and independent living skills. Each support is linked to specific recovery goals articulated by the consumer. Supports are established and maintained on weekly home visits. All therapists were bachelor’s and master’s level psychology staff trained in the CAT model by Dr Velligan and certified CAT trainers using a combination of didactic sessions and observation of CAT treatment conducted in the homes of patients. Fidelity was rated by certified CAT trainers including Dr Velligan.
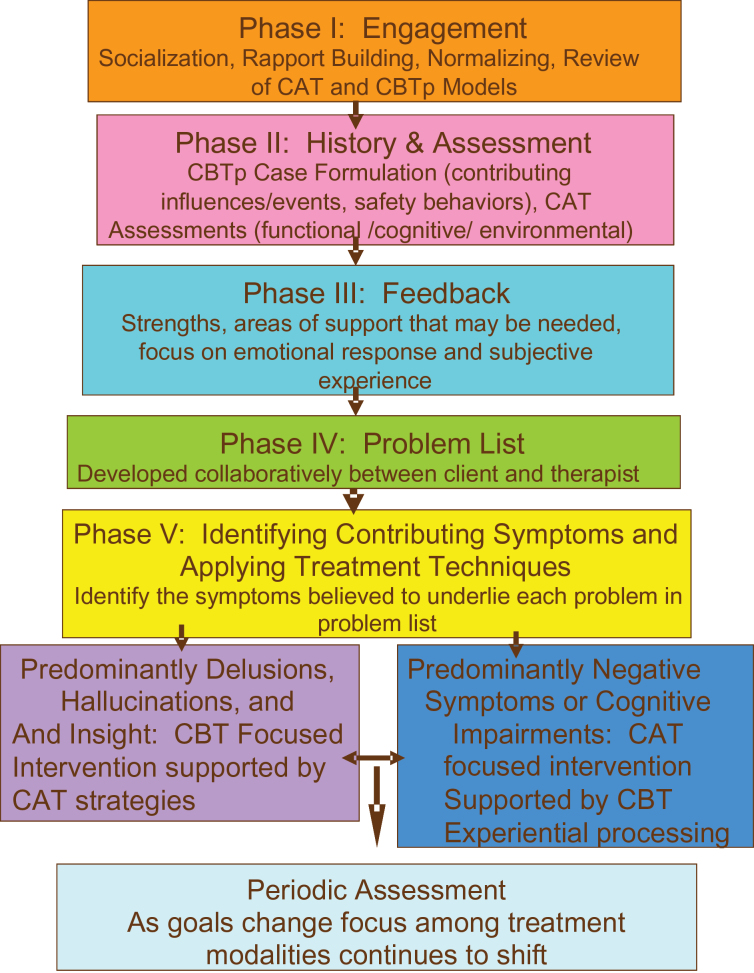
Mcog (CBTp + CAT).
This was an integrated, manual-driven treatment developed by Drs Turkington, Tai, and Velligan involving both a formal case formulation based on history to plan CBT interventions and the cognitive and functional assessments necessary to plan CAT interventions. Following initial engagement and normalizing of symptoms, participants received feedback regarding assessments and worked with the Mcog therapist on the formulation of a problem list. If problems listed were influenced more by neurocognitive impairments, negative symptoms, or disorganization, CAT strategies were used initially, supported by CBT techniques. For example, signs and alarms were used to prompt specific behaviors including reminding the person to catch and write down automatic thoughts. If problems listed were influenced more by delusions or hallucinations, CBT techniques were used initially and these were supported by CAT strategies. For example, pie charts showing alternative explanations for people coughing including “secret communication, colds, allergies, and heavy smoking” were made on large paper and pasted on the wall to continue reminding the person to generate alternatives. If problems listed were influenced by both positive symptoms and cognitive impairments, the treatment would address each contributing factor in a rational order. For example, if an individual with very poor hygiene was fearful of interacting with others due to paranoid thinking, hygiene issues would be addressed prior to any behavioral experiments involving others. Without addressing hygiene first (using CAT strategies), behavioral experiments could result in negative social consequences and reinforce paranoid thinking. A graphic depicting the therapy process is illustrated in figure 2.
Fig. 2.
The Mcog therapy process.
The problem list initially agreed upon was reviewed regularly, and interventions were adjusted accordingly. All therapists performing Mcog were trained in both CBT for psychosis and CAT as described earlier. They were then trained in the integrated Mcog model and participated in supervision with Drs Velligan, Tai, and Turkington. Fidelity was rated by Drs Tai and Velligan.
TAU.
TAU consisted of case management and medication follow up appointments provided by the local community mental health center. Medication follow-up visits occurred approximately every 3 months and caseloads varied from 40 to 150 patients per case.
Assessments
Symptoms and Community Functioning.
Symptom and functional assessments were administered by bachelor’s, master’s, or doctoral level psychologists or social workers required to reach a criterion of 0.80 intraclass correlation coefficient on a series of interviews. We conducted checks on rater competency throughout the study and provided on-going training and regular assessment of inter-rater reliability to prevent rater/scorer drift.10 All raters were blind to treatment condition.
Symptomatology
Symptoms over the past week were assessed using the expanded version of the BPRS.10,11 The psychosis factor score, the mean of items assessing hallucinations, unusual thought content, suspiciousness and conceptual disorganization, was a measure of positive symptoms.12,13 Higher scores indicate greater psychotic symptomatology. Scores on each item are rated based on frequency and severity of the symptom as well as impairment in functioning due to the symptom. Secondary measures of symptomatology included the Auditory Hallucination Rating Scale (AHRS) and the Delusion Rating Scale (DRS).14 These latter instruments separately rate frequency, intensity, and the distress caused by psychotic symptoms.
Functional Outcome
The primary measure of functional outcome was the Multnomah Community Ability Scale (MCAS).15 The MCAS is a 17-item scale assessing a variety of domains of community adjustment including interference with functioning, adjustment to living, social competence, and behavioral problems. Scores rate functioning over the past 3 months. Higher scores reflect better community functioning.
Data Analysis
All analyses were intent-to-treat including all patients who had a baseline and at least 1 follow-up assessment. Primary outcomes were changes in the psychosis factor from the BPRS and the mean score for the MCAS during the treatment period. Secondary outcomes included the AHRS and DRS, as well as changes in symptoms and community functioning through the follow-up period. We examined group differences in symptomatology (BPRS positive symptom score, AHRS, DRS) and functioning (MCAS score) over time during the active treatment period (3, 6, and 9 months) by treatment group using mixed effects regression with repeated measures using a 2 (CAT/no CAT) × 2 (CBT/no CBT) factorial design, covarying the baseline scores.1 All analyses were intent-to-treat. This procedure makes use of all available data, fits the covariance of repeated measures, adjusts for missing values, and allows us to examine the points at which groups began to diverge with respect to outcome measures. For significant effects, we report effect size as Cohen’s d and number needed to treat (NNT).16,17 We repeated these analyses including the 6-month post-treatment follow-up period.
Power was estimated using RMASS2 software for longitudinal data18 at >0.95 to detect a main effect of treatment type (treatments containing CAT vs those not containing CAT and treatments containing CBT vs those not containing CBT). Assumptions were a medium effect (Cohen’s d = 0.50) with a baseline covariate and 3 postbaseline measures, all normally distributed with equal variances and constant effect size over time.
Results
There were no statistically significant group differences with respect to demographic or clinical data at baseline (table 1). The number of subjects with data at each time point was as follows: baseline n = 142; 3 months, n = 142; 6 months, n = 117; 9 months, n = 108. For the follow-up period at months 12 and 15, there were 102 and 97 individuals available for analysis. Reasons for drop out appear in the consort diagram. The mean number of sessions for CAT, CBTp, and Mcog were 27.5 (S D = 7.20), 26.6 (S D = 9.55), and 27.5 (S D = 8.19), respectively; P > .80.
Table 1.
Baseline Characteristics by Treatment Group
| CAT (n = 33) | CBT (n = 37) | Mcog (n = 35) | TAU (n = 37) | |
|---|---|---|---|---|
| % Male | 54.0 (n = 18) | 45.9 (n = 17) | 54.3 (n = 19) | 54.05 (n = 20) |
| % Hispanic | 45.2 (n = 14) | 54.0 (n = 20) | 37.1 (n = 13) | 48.65 (n = 18) |
| % Non-Hispanic White | 22.6 (n = 7) | 21.6 (n = 8) | 40.0 (n = 14) | 27.0 (n = 10) |
| % African American | 33.0 (n = 11) | 24.2 (n = 9) | 17.1 (n = 6) | 24.3 (n = 9) |
| Age | 43.47 (SD = 10.7) | 39.2 (SD = 12.5) | 39.5 (SD = 12.8) | 40.3 (SD = 11.1) |
| Education | 11.8 (SD = 2.1) | 11.5 (SD = 2.0) | 11.1 (SD = 2.3) | 11.9 (SD = 2.3) |
| Mean BPRS psychosis factor | 4.0 (SD = 1.0) | 4.1 (SD = 0.9) | 3.9 (SD = 0.9) | 4.1 (SD = 1.0) |
| Mean AHRS | 1.9 (SD = 1.0) | 1.9 (SD = 1.0) | 2.0 (SD = 0.9) | 2.1 (SD = 0.7) |
| Mean DRS | 2.0 (SD = 1.1) | 2.1 (SD = 0.7) | 2.0 (SD = 1.0) | 1.6 (SD = 1.3) |
| Mean MCAS | 3.7 (SD = 0.4) | 3.8 (SD = 0.3) | 3.7 (SD = 0.3) | 3.8 (SD = 0.4) |
Note: AHRS, Auditory Hallucination Rating Scale; BPRS, Brief Psychiatric Rating Scale; CAT, Cognitive Adaptation Training; CBT, Cognitive Behavior Therapy; DRS, Delusion Rating Scale; MCAS, Multnomah Community Ability Scale; TAU, Treatment as Usual.
Symptoms
For the BPRS psychosis score, the mixed effects regression model yielded nonsignificant main effects for CAT, CBTp, and time, and nonsignificant interactions (all F’s < 1.12 all P’s > .29). For the AHRS, results of the mixed effects regression indicated a significant main effect of CAT treatment (F(1, 138) = 4.38; P <.04), and nonsignificant main effects for CBTp (F(1, 138) = 0.02; P <.88), and time (F(2, 233) = 2.26; P < .11). All interaction terms were nonsignificant (F-ratios <1.62, all P’s >.20). A significant main effect of CAT treatment with no treatment by time interaction means that the effect of CAT was stable throughout treatment, with no differences in slope. An inspection of means indicated that patients improved to a greater extent in terms of severity and distress resulting from auditory hallucinations in treatments containing CAT (ie, CAT and Mcog). Averaged across the time points, the effect size for CAT vs non-CAT treatments was ~0.36 which corresponds to a NNT of 6.17 According to Cohen’s conventions,19 this represents a small treatment effect. For the DRS, there were no statistically significant main effects or interactions (all F’s <2.4, all P’s >.13).
Functioning
Results of a mixed effects regression model examining treatment group differences over time on MCAS scores indicated a main effect for CAT (F(1, 133) = 5.65; P < .02) with nonsignificant CBTp, time, and treatment by time effects (all F < 2.71; all P’s >.10). An inspection of means indicated that individuals in treatments that included CAT did better than those in treatments that did not include CAT. Averaged across the time points, the effect size for CAT treatment as compared to no CAT treatment was 0.41 which corresponds to a NNT of 5. According to Cohen’s conventions,19 this is a small to moderate treatment effect of CAT on functional outcome.
Additional Analyses
We repeated the analyses including the time points following treatment termination (months 12 and 15), and essentially found the same results. Main effects of CAT treatment on the AHRS and the MCAS were slightly weaker when the follow-up data were included (P-values < .06). No other trends or statistically significant main effects or interactions were found. Because CBTp is designed to address multiple problems and symptoms, we examined the total score from the BPRS and found no significant main effects or interactions.
Discussion
As in earlier studies, CAT improved community functioning. CAT patients also benefited modestly in terms of decreases in auditory hallucinations and related distress in comparison to non-CAT patients. This finding is consistent with 2 other studies demonstrating decreases in positive symptoms with CAT.7,8 However, the results of the study did not support the hypothesis that combining CAT treatment and CBT for psychosis would produce improved outcomes. There was no evidence that CBTp improved positive symptoms and associated distress. These results stand in stark contrast to multiple published studies and meta-analyses of CBT for psychosis. We describe later possible explanations for the greater impact of CAT vs CBTp on treatment outcomes. It is important to note that although CAT did outperform CBTp, effect sizes for CAT were notably smaller in this sample selected for high levels of positive symptoms in comparison to previous studies.
It is possible that CAT outcomes were better in this trial in part because CAT was developed at our site in South Texas. Cognitive Behavior Therapy for psychosis was less familiar to our therapists. That being said, training and supervision was rigorous and fidelity measures supported the competence of therapists. Patient demographic factors may have impacted the outcome. Patients in published studies of CBT for psychosis had mean education levels ranging from 11.3 to 16.5 with a weighted mean of 12.95. On average, our participants had less than a high school education. Recent evidence indicates that better educational attainment and cognitive functioning predict better CBT outcomes.20
There was also no guarantee that patients were taking oral medications as prescribed during the trial. Medication ingestion was not observed. If medication was not consistent, fluctuations in symptoms may have created sufficient noise so as to obscure any treatment effects. This may be why CAT, which focuses on taking medication as directed, as one of its treatment targets, may have reduced auditory hallucinations and associated distress. Nonadherence has a negative impact on the delivery of psychological treatments, and CAT was less likely to be affected by this factor. Now that there are multiple second generation antipsychotics available in long-acting form, a study design that provides injectable medication to all participants would be important to be considered for future studies examining the efficacy of psychosocial treatments. However, inconsistent adherence is a fact of life in the current treatment environment and studying psychosocial treatments in this context makes results more generalizable.
In this study, clinics provided medication management but far less support than is available on average to patients in the United Kingdom. Clinics are generally understaffed and underfunded. According to the State Mental Health Agency, in 2010, Texas ranked 49th out of 50 states and Puerto Rico in terms of the amount of money spent per person for mental health services.
There is also an issue that patients admitted to the study were not necessarily seeking treatment for either their persisting symptoms or functional impairments. Some individuals may have agreed to participate to receive compensation for assessments or simply to have something to do. This may lower motivation for change. Because CAT treatment is highly directive and designed to overcome problems in initiating behavior, lower motivation may be a less significant factor in patients randomized to CAT than for those randomized to CBTp, which is patient directed to a much greater extent.
Cognitive Behavior Therapy for psychosis in our trial was highly individualized for each patient such that the target goals varied substantially from one participant to another. Some individuals selected to work on sleep issues, others on feeling less paranoid taking the bus, and others on coping with anxiety. Some of these targets may not have been well reflected in aggregate scores on the BPRS and measures of positive symptoms. Studying CBTp with more homogenous groups (eg, patients with auditory hallucinations) may achieve more positive results. CAT treatment is also individualized, but the prompts and cues vary rather than the overall treatment goal of improving everyday functional behaviors.
In summary, results demonstrated overall poor improvement of participants, small to moderate effects of CAT treatment on auditory hallucinations and related distress and functional outcome, with no significant impact of CBT for psychosis.
Funding
National Institute of Mental Health (5R01MH082793).
Acknowledgments
The authors have declared that there are no conflicts of interest in relation to the subject of this study.
References
- 1.Maples NJ, Miller AL, Evans L, et al. Translating evidence-based practices into community treatment settings. Schizophr Bull. 2007;33:595. [Google Scholar]
- 2.Zimmermann G, Favrod J, Trieu VH, Pomini V. The effect of cognitive behavioral treatment on the positive symptoms of schizophrenia spectrum disorders: a meta-analysis. Schizophr Res. 2005;77:1–9. [DOI] [PubMed] [Google Scholar]
- 3.Velligan DI, Turkington D, Tai S. Multi-modal cognitive therapy for schizophrenia: Addressing cognitive impairment and dysfunctional cognitive schemas. Schizophr Bull. 2009;35(suppl 1):345–346. [Google Scholar]
- 4.O’Connor R, Herrman H. Assessment of contributions to disability in people with schizophrenia during rehabilitation. Aust N Z J Psychiatry. 1993;27:595–600. [DOI] [PubMed] [Google Scholar]
- 5.Kingdon DG, Turkington D. Guides to Individualized Evidence-Based Treatment. Cognitive Therapy of Schizophrenia. New York, NY: The Guildford Press; 2005. [Google Scholar]
- 6.Granholm E, McQuaid JR, McClure FS, et al. A randomized, controlled trial of cognitive behavioral social skills training for middle-aged and older outpatients with chronic schizophrenia. Am J Psychiatry. 2005;162:520–529. [DOI] [PubMed] [Google Scholar]
- 7.Velligan DI, Bow-Thomas CC, Huntzinger C, et al. Randomized controlled trial of the use of compensatory strategies to enhance adaptive functioning in outpatients with schizophrenia. Am J Psychiatry. 2000;157:1317–1323. [DOI] [PubMed] [Google Scholar]
- 8.Velligan DI, Prihoda TJ, Ritch JL, Maples N, Bow-Thomas CC, Dassori A. A randomized single-blind pilot study of compensatory strategies in schizophrenia outpatients. Schizophr Bull. 2002;28:283–292. [DOI] [PubMed] [Google Scholar]
- 9.Velligan DI, Diamond PM, Maples NJ, et al. Comparing the efficacy of interventions that use environmental supports to improve outcomes in patients with schizophrenia. Schizophr Res. 2008;102:312–319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Brabban A, Tai S, Turkington D. Predictors of outcome in brief cognitive behavior therapy for schizophrenia. Schizophr Bull. 2009;35:859–864. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ventura J, Lukoff D, Nuechterlein KH, Liberman RP, Green MF, Shaner A. Manual for the expanded brief psychiatric rating scale. Int J Methods Psychiatr Res. 1993;3:227–244. [Google Scholar]
- 12.Drury V, Birchwood M, Cochrane R, MacMillan F. Cognitive therapy and recovery from acute psychosis: A controlled trial. Br J Psychiatry. 1996;169:593–601. [DOI] [PubMed] [Google Scholar]
- 13.Turkington D, Kingdon D, Rathod S, Hammond K, Pelton J, Mehta R. Outcomes of an effectiveness trial of cognitive-behavioural intervention by mental health nurses in schizophrenia. Br J Psychiatry. 2006;189:36–40. [DOI] [PubMed] [Google Scholar]
- 14.Haddock G, McCarron J, Tarrier N, Faragher EB. Scales to measure dimensions of hallucinations and delusions: the psychotic symptom rating scales (PSYRATS). Psychol Med. 1999;29:879–889. [DOI] [PubMed] [Google Scholar]
- 15.Barker S, Barron N, McFarland BH, Bigelow DA. A community ability scale for chronically mentally ill consumers: Part I. Reliability and validity. Community Ment Health J. 1994;30:363–383. [DOI] [PubMed] [Google Scholar]
- 16.Jones C, Cormac I, Silveira da Mota Neo JI, Campbell C. Cognitive behaviour therapy for schizophrenia. Cochrane Database Syst Rev (Online). 2005;4:1–57. [DOI] [PubMed] [Google Scholar]
- 17.Granholm E, McQuaid JR, McClure FS, et al. A randomized, controlled trial of cognitive behavioral social skills training for middle-aged and older outpatients with chronic schizophrenia. Am J Psychiatry. 2005;162:520–529. [DOI] [PubMed] [Google Scholar]
- 18.Hedeker D, Gibbons RD, Waternaux C. Sample size estimation for longitudinal designs with attrition: Comparing time-related contrasts between two groups. J Educ Behav Stat. 1999;24:70–93. [Google Scholar]
- 19.Cohen J.Statistical Power Analysis for the Behavioral Sciences. 2nd ed.Hillsdale, NJ: Lawrence Erlbaum Associates; 1988. [Google Scholar]
- 20.Kukla M, Davis LW, Lysaker PH. Cognitive behavioral therapy and work outcomes: Correlates of treatment engagement and full and partial success in schizophrenia. Behav Cogn Psychother. 2013;21:1–16. [DOI] [PubMed] [Google Scholar]