Abstract
In college and university residence halls, resident assistants (RAs) are expected to serve as first-aid providers to students who may have alcohol, other drug, mental health, and academic problems. Despite this responsibility, evidence-based, first-aid programs have not been developed and tested for the RA workforce. The current study examined effects of an investigational first-aid program designed specifically for RAs. The online Peer Hero Training program is a novel approach to RA training in its use of interactive video dramatizations of incidents involving substance-using or distressed residents. A 9-month randomized trial conducted on 8 U.S. campuses compared RAs who participated in the Peer Hero Training program to RAs who received training-as-usual. Participation in the Peer Hero Training program significantly increased RA first-aid efforts for residential students who may have had alcohol, other drug, mental health, or academic problems six months after baseline. Compared to those in the training-as-usual condition, RAs in the Peer Hero Training program made more than 10 times as many first-aid efforts for possible alcohol problems, almost 14 times the number of first-aid efforts for possible drug use, almost 3 times the number of first-aid efforts for possible mental health problems, and 3 times the number of first-aid efforts for academic problems. There was no evidence that measured RA attitudes mediated the effects of the intervention. Results of this preliminary evaluation trial suggest that online training using interactive video dramatizations is a viable approach to strengthening RAs’ ability to provide alcohol, other drug, and mental health first-aid to undergraduates.
Keywords: resident assistants, alcohol and other drugs, mental health first-aid, longitudinal research, intervention evaluation
Alcohol use, drug use, and mental health disorders are not rare in the U.S. college student population. In a national probability sample that used DSM-IV nomenclature of the American Psychiatric Association (2000), Blanco et al. (2008) found the following proportions of 19- to 25-year-old U.S. college students met criteria for certain conditions: 18% for any personality disorder, 13% for alcohol dependence, 12% for any anxiety disorder, 11% for any mood disorder, 8% for alcohol abuse, 4% for drug abuse, and 1% for drug dependence. Another national study found that in the past school year, 43% of college students “felt so depressed it was difficult to function,” 9% seriously considered suicide, and 1% attempted suicide (American College Health Association, 2009). The 2012 college student results from the Monitoring the Future Study indicated that past 30-day rates for drunkenness and marijuana/hashish smoking were 40% and 21%, respectively (Johnston, O'Malley, Bachman, & Schulenberg, 2013).
Most college students who experience mental health problems, including alcohol and drug use disorders, do not receive early intervention or treatment services. For example, only about 34% of college students with a mood disorder (Blanco et al., 2008) and 4% to 5% of those with an alcohol or alcohol/drug use disorder (Wu, Pilowsky, Schlenger, & Hasin, 2007) reported receiving treatment in the past 12 months. These findings are consistent with concerns of campus mental health professionals who have noted that college students often do not identify their behaviors or mood states as problematic and therefore do not seek help on their own (Buscemi et al., 2010; Kadison, 2004).
U.S. colleges and universities employ approximately 60,000 resident assistants (RAs) to work and live in student residence halls each year (U.S. Census, 2010). Although they have several roles, RAs are expected to serve as first-responders when acute or chronic mental health problems and academic problems appear in students living in residence halls (Blimling, 2003; Elleven, Allen, & Wircenski, 2001; Sharkin, Plageman, & Mangold, 2003; Taub et al., 2013). The vast majority of undergraduate RAs hold these positions for only one or two academic years. Thus, the annual turnover in the RA workforce is substantial, making RA training and supervision an ongoing task in residence life/housing departments. At most campuses, RA training programs devote minimal time to alcohol, drug, and mental health first-aid, including teaching RAs effective referral skills for these problems (Taub & Servaty-Seib, 2011; Taub et al., 2013). Moreover, the first-aid training conducted by departments of residence life/housing is locally devised and not evidence-informed (Owens, 2011; Taub & Servaty-Seib, 2011; Taub et al., 2013). Although there are no available data, more RA training time may focus on helping students with academic problems than with alcohol, drug, and mental health first-aid (Reingle, Thombs, Osborn, Saffian, & Oltersdorf, 2010).
Over the past decade, there has been a significant increase in research seeking to develop and test approaches for improving the mental health first-aid in the public and in the workplace, for specific mental health conditions, and in specific professions (Gratwick-Sarll, & Bentley, 2014; Kelly et al., 2011; Kitchener & Jorm, 2004; 2006; Pekevski, 2013; Svensson & Hansson, 2014). This response is driven by the belief that early intervention optimizes treatment success and by the recognition that many individuals with mental health problems, including alcohol and other drug abuse, will not seek treatment on their own (Buscemi et al., 2010; Rossetto, Jorm, & Reavley, 2014). Thus, mental health first-aid programs are designed to teach skills in recognizing and effectively responding to behavioral problems in other persons (Kingston et al., 2009, 2011). Training focuses on helping those who may be developing a mental health condition, are in psychological crisis, or are exhibiting signs of problematic substance use.
The aim of the current study was to test the effects of an alcohol, other drug, mental health, and academic first-aid program designed specifically for RAs. To our knowledge, this is only the second study (following Taub et al., 2013) to develop an evidence-based approach to training RAs in these first-aid practices. The primary intervention goal was to increase the number of first-aid efforts carried out by RAs for alcohol, other drug, mental health, and academic problems in their living units during one academic year.
Known as Peer Hero, this online training program used a novel, story-based approach involving interactive video dramatizations of residence life incidents. The program was designed to change four RA attitudinal constructs: perceived referral barriers, referral self-efficacy, anticipatory anxiety, and perceived referral norms. Each construct was hypothesized to mediate intervention effects on first-aid efforts. Longitudinal analyses examined which constructs changed over the course of the Peer Hero Training program and mediated the effects of the intervention during this nine-month randomized trial conducted on 8 U.S. campuses.
There were two study hypotheses. First, we hypothesized that compared to RAs receiving training-as-usual, RAs participating in the Peer Hero Training program would engage in a significantly greater number of first-aid efforts for alcohol, other drug, and mental health problems in their living units. Second, we hypothesized that results of mediation analyses would provide evidence that perceived referral barriers, referral self-efficacy, referral anticipatory anxiety, and perceived referral norms act as mechanisms of change in the Peer Hero Training program.
Methods
Participants and Procedure
In August 2012, the Peer Hero Training program trial was implemented at 8 higher education institutions in the U.S. The campuses included two large public universities and one historically black university in the Southeast; two small private colleges and two medium-size public universities in the Midwest; and one private university in the Pacific Northwest. The size of the campus RA staffs ranged from 25 to 204 (mean = 86.9). The RAs oversaw residents living in traditional dorm-style residence halls, suites, and on-campus apartments. All RAs at each institution were required to participate in the training condition to which their campus was randomly assigned (training-as-usual, or Peer Hero + training-as-usual) as a part of their employment.
Through an international professional association of residence life and housing officers, offers to participate in the investigational training study were extended to the directors of 13 departments of residence life/housing, and eight agreed to participate. After each director agreed to participate, the principal investigator and each director reviewed the details of study participation, and written consent was obtained from the director at that time. The campuses were then randomized to either the Peer Hero Training program condition or the training-as-usual condition after informed consent was obtained from all 8 directors. Each campus assigned a senior staff member to serve as study liaison.
During the 2012-13 academic year (9 months), 652 RAs or 100% of the sampling frame participated in the training study. A total of 86 RAs (13.2%) did not complete the trial as a result of leaving their employed position during the school year (due to mid-year graduation, studying abroad during the Spring Semester, academic problems, job performance issues, or other reasons). These cases were excluded from data analyses because of different ways in which the departments of residence life/housing replaced and trained these employees. Thus, this study reports results from 566 RAs.
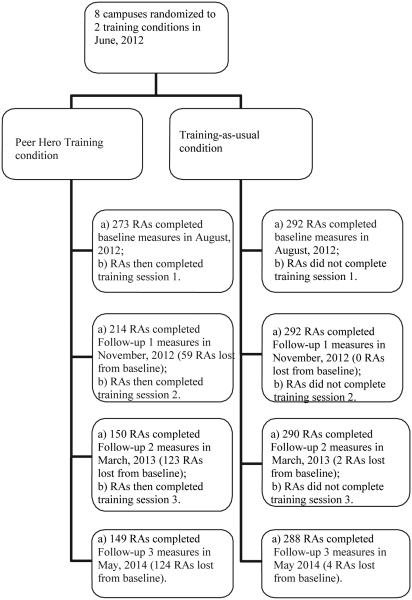
RAs assigned to the investigational training program participated in the Peer Hero Training program as well as their institution’s training-as-usual. As shown in Figure 1, online Peer Hero Training sessions took place immediately after completing the baseline assessment (training session 1), follow-up 1 (training session 2), and follow-up 2 (training session 3) measures. Each Peer Hero Training session could be completed in 15 to 25 minutes. In the training-as-usual condition, RAs were provided the standard, annual training offered by their institution (no Peer Hero Training was offered). At all 8 campuses, training-as-usual included some education on alcohol, other drugs, mental health, and academic problems in the college student population. This education was delivered prior to the start of the academic year.
Figure 1.
Depiction of RA assignment to training condition and retention during study.
Institutional Review Board (IRB) approval was obtained from the principal investigator’s institution and from IRBs at each of the 8 participating campuses. Informed consent was obtained from the directors of residence life/housing at each of the eight campuses. The directors were free to withdraw their departments and RAs from the study at any time without penalty. Informed consent was not sought from RAs because the IRBs considered study participation, consisting of training and completion of online surveys, to be a condition of employment rather than voluntary activity. It should be noted that all survey items included the response option “no answer” for which there was no penalty. RAs were informed throughout the study that their confidential responses would not be shared with any official at their institution.
To reduce respondent burden, all survey measures were administered online at four specific times in the 9-month academic year to accommodate the major examination periods and holiday breaks of RAs. Baseline measures were collected in August of 2012, prior to residents returning to campus for Fall Semester. Follow-up 1 measures were obtained in November of 2012, prior to Thanksgiving Break. Follow-up 2 measures were collected prior to Spring Break in March of 2013, and follow-up 3 measures were obtained in May of 2013 (prior to final examinations).
Figure 1 depicts RA assignment to training condition and retention during the study. Randomization to study condition (Peer Hero Training vs. training-as-usual) took place at the campus level. RA attrition was much greater in the Peer Hero Training condition because after follow-up 1 (and training session 2), the department director at one university opted to withdraw from the study due to the level of staff effort needed to monitor and follow-up on RA participation.
Peer Hero Training Program
Supported by small business technology transfer research funding (STTR), a computer technology firm developed the online Peer Hero Training program. Content for the program was developed by a team of senior professional staff in campus residence life/housing, RA supervisors, RAs, campus mental health professionals, other student affairs professionals, and health behavior researchers. A 2-year iterative process was used to design and test the functionality of the training program. Residence life stakeholders from a number of U.S. campuses contributed to its content and provided feedback in its development. The resultant online product was named “Peer Hero Training” to emphasize that RAs are expected to exercise courage in carrying out their responsibilities as mental health and alcohol/other drug first-aid providers.
The online Peer Hero Training program has three components, all in video format: (1) three separate RA demonstration episodes, (2) a counseling session segment, and (3) a series of parent and “pro hero” interviews. The first two parts are fictional, follow a story line (e.g., titled “Low and Away”), were filmed on an actual college campus, and feature culturally diverse professional actors portraying RAs (e.g., “Derek”), RA supervisors, and undergraduate student residents (e.g., “Rob”). The third part of the program features actual parents of undergraduate students residing in residence halls, as well as a variety of student affairs/residence life personnel describing the role and responsibilities of the RA and recommendations for RA approach and referral behaviors. The same technology firm filmed all videos, which have high production quality to optimize their credibility and to retain the interest of RA trainees.
The RA demonstration episodes showcase RA attempts to approach residents with alcohol, other drug, mental health, and academic problems, as well as RA methods for referring residents for professional assistance (e.g., only after consulting with RA supervisors). Each of the three episodes contains three interactive decision points, where the RA trainee selects among four possible responses to a situation involving the featured RA and the distressed resident. At these points, the online scene freezes and four options appear on the screen, each a one-line text of what the RA may say next in the story (e.g., “It’s my job to be concerned”). Once an option is selected, the video resumes with the RA dramatizing the selected response. Following each of the video selected responses, a commentator appears on screen, informing the RA trainee whether the response selected and dramatized by the RA is very helpful, helpful, somewhat helpful, or not at all helpful. The commentator then provides an explanation describing why the response was or was not helpful in the situation. The episode and its story did not resume until the RA trainee had selected the correct response, the very helpful response. They were encouraged, however, to explore all four responses at each interactive decision point, regardless of their initial selection. Each of the RA demonstration segments, including the interactive decision points, are between 10 and 15 minutes in length.
A two-part counseling session segment features resident “Rob” meeting with a professional counselor at a college counseling center for two individual counseling sessions that follow a story line and appear in training sessions 2 and 3. It is “Rob” who has been referred to counseling by his RA, “Derek,” in the demonstration episode “Low and Away” that RA trainees had already viewed. Again, as in the RA demonstration episodes, persons featured in the counseling session segment are professional actors. The purpose of this part of the Peer Hero Training program is to highlight for RA trainees what residents referred to counseling might expect to encounter (e.g., review of confidentiality and its limits), thus addressing one aspect of perceived norms in RA approach and referral behaviors.
The third and final part of the Peer Hero Training program is a series of parent and “pro hero” interviews. These brief interviews are with actual parents of undergraduate students and actual senior residence life professionals (the latter referred to as “pro heroes”). The names and titles/positions of the “pro heroes” appear on screen while they discuss the range of resident problems that RAs routinely see in their living units. These professionals emphasize that RAs are expected to make resident referrals to professional counseling services on campus in accordance with their department’s protocol, and they caution against ignoring or overlooking residents’ needs. They also provide specific advice on how to approach residents with an observed behavioral problem. They emphasize the need for RAs to be sincere and empathic, and to maintain confidentiality. In the Peer Hero Training program, these interviews appeared before and after each of the three RA demonstration episodes.
A distinctive feature of the Peer Hero Training program is that all three of its parts address four attitudes the research team identified as critical mechanisms for strengthening RA first-aid efforts: perceived referral barriers, referral self-efficacy, referral anticipatory anxiety, and perceived referral norms (Glanz, Rimer, & Viswanath, 2008). First, in an effort to reduce perceived barriers to making campus referrals, RAs are shown taking specific steps to approach residents in a sensitive and respectful manner and consulting their supervisor and campus mental health professionals. Second, to strengthen RA trainee self-efficacy, all RAs are depicted as positive, confident and empathic, and not deterred by residents reluctant to accept help. To reduce the anticipatory anxiety that may precede a first-aid effort, the videos also include scenes of the RAs preparing themselves to effectively approach residents to discuss a problem. The fourth and final attitude addressed in the Peer Hero Training program is that of perceived referral norms. To reinforce these norms, RA trainees are exposed to interviews with parents of residents and with “peer heroes,” and also to RA demonstration episodes that include RA supervisors expressing their expectations about helping residents in need.
Instrumentation
Survey items were pre-tested using RA supervisors from a number of campuses (none of the campuses in the present study participated in pre-testing). In addition to assessing demographic characteristics, online survey items measured the number of four different types of first-aid efforts RAs made: (1) During the past 30 days, how many residents have you talked with about an alcohol problem?; (2) During the past 30 days, how many residents have you referred to your immediate supervisor about an alcohol problem?; and, (3) During the past 30 days, how many residents have you referred to a counseling service for assistance with an alcohol problem? In addition, RAs responded to separate sets of parallel items for other drug, mental health, and academic first-aid efforts. The scores from each three-item set of past 30-day first-aid efforts were summed to form four first-aid indicators for each RA. The rationale for this scoring approach was twofold. First, first-aid efforts for a single resident referral may be process involving several meetings by an RA, and possibly their immediate supervisor, over the course of a semester (or longer). To address the complexity of these situations, items were constructed to assess the number of residents involved, rather than the number of meetings with a resident. Second, there was a need for multiple first-aid effort items for each problem type because campuses and RA supervisors had different protocols for how RAs were expected to provide first-aid. At some campuses in the study, RAs were supported in making direct referrals to campus counseling centers, whereas at other campuses, RAs were expected to make referrals to their immediate supervisor or another professional staff member.
A total of eight items were used to measure perceived referral barriers. Using five-point Likert scales ranging from strongly disagree (scored as 1) to strongly agree (scored as 5), responses indicated the extent of agreement with statements about negative aspects of making referrals (e.g., a negative aspect of approaching and possibly referring a resident is that they will become defensive or angry with me). Comprised of three items, referral self-efficacy relied on the same 5-point Likert scale. An example of an item used to measure referral self-efficacy was: I feel confident in my ability to discuss with a resident those concerns I may have about their behavior. Referral anticipatory anxiety was measured using 4 items on the same 5-point Likert scale. One of these items was: If I were to suggest that a resident see a professional at the counseling center, I would be afraid that he or she would become angry with me or dismiss the idea as ridiculous. Perceived referral norms for alcohol referrals, other drug referrals, and mental health referrals were measured by separate sets of parallel items. RAs responded to two separate alcohol, other drug, and mental health questions: What would the following people think of you if you referred a resident to the campus counseling center for a possible alcohol (or drug/mental health) problem? Using 5-point Likert scales ranging from strongly disapprove (scored as 1) to strongly approve (scored as 5), responses were provided for 5 referents: (1) RAs on your hall staff; (2) your immediate supervisor; (3) your director of residence life/housing; (4) residents in your living unit; and, (5) parents of residents in your living unit. A longstanding and accepted role for RAs is to help link residents to services of campus learning assistance centers. As such, the Peer Hero Training program was not expected to strengthen perceived referral norms for academic problems. Thus, this measure was not used in the study.
Items comprising the referral self-efficacy, perceived alcohol referral norms, drug referral norms, and mental health referral norms scales had good internal consistency across each of the three time points in both training conditions, with Cronbach’s alphas ranging from 0.82 to 0.94. Items comprising referral anticipatory anxiety and perceived referral barriers had moderately high internal consistency (i.e., alphas ranging from 0.75 to 0.86). Intra-class correlations for participants (nested within schools) across time points were high (ICC > 0.50) for perceived barriers and referral self-efficacy. The correlations were moderately high for anticipatory anxiety (ICC = 0.48) and alcohol referral norms (ICC = 0.49) across time. They were substantially lower for perceived drug and mental health referral norms (ICC = 0.29 and ICC = 0.33, respectively). Despite the relatively low correlations for these latter two variables over time, these correlations were significantly higher in the training-as-usual condition compared with the Peer Hero Training program condition.
Analytic Methods
The numbers of first-aid efforts made by the RA within each of four categories (alcohol, other drug, mental health, and academic) were treated as the primary outcome measures. Descriptive statistics were calculated to show the proportion of RAs making at least one referral effort at baseline and each of the three follow-ups for the Peer Hero Training condition and the training-as-usual condition. Additionally, means and standard errors were computed for the attitudinal measures for each group at each time point. To investigate the longitudinal effects of the Peer Hero Training program while controlling for the nested effects of campuses, a multilevel Poisson regression model was used. We conducted sensitivity analyses by excluding one campus that withdrew from the study after the first follow-up survey. However, the results from all eight campuses initially in this trial are included in the final analyses. Maximum likelihood imputation was used to address missing data. All analyses were conducted using STATA 13 (College Station, TX).
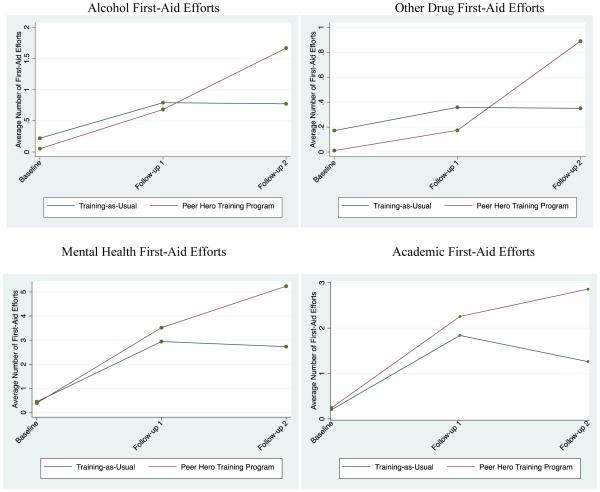
We created figures depicting the past 30-day effects of the Peer Hero Training program over time. Although we initially included all four waves of data, the consistent convergence of all four RA first-aid efforts between the Peer Hero Training and training-as-usual conditions at the final follow-up (i.e., the end of the academic year) led us to exclude the final follow-up from the primary analysis for two reasons. First, by the second follow-up (just prior to Spring Break, which occurs during the Spring semester), a RA, in most cases, would have already identified and extended first-aid efforts to residents they were concerned about. Second, at the end of the academic year, RAs tend to refocus their energy from their residence life responsibilities to their own end-of-semester academic work, graduation, moving plans and the upcoming summer break, job searches, and/or other activities. Therefore, the present analyses report the effects of the training conditions over three time points (prior to the beginning of the Fall semester, 2012 through the midpoint of the spring semester; with 2- to 3-month intervals between each follow-up). All follow-up 2, surveys were completed prior to each campus’ Spring Break.
Each of the four outcome variables were assessed independently for direct Peer Hero Training program effects. We expected that the Peer Hero Training program to have more robust past 30-day effects on alcohol, drug, and mental health first-aid efforts as compared with academic referrals because conventional RA training programs (training-as-usual) have traditionally focused on helping students with academic problems.
Results
Past 30-day RA first-aid efforts and attitudinal measures for each time point are summarized in Table 1. Briefly, the sample included 566 RAs from eight colleges and universities in the U.S. The sample was predominately male (59%), White (78%), and the mean age was 20 years in both the Peer Hero Training program and training-as-usual conditions. As a result of the random assignment of campuses to intervention condition, slightly more than one-half (52%) of the participating RAs were assigned to the training-as-usual control condition. Less than one-half (45%) of the participating RAs were returning to their RA positions from a previous year at the baseline interview. There were no differences in the attitudinal variables across training groups at baseline (i.e., perceived referral barriers, anticipatory anxiety, self-efficacy, and perceived alcohol, other drug, and mental health referral norms). However, the number of returning RAs who reported making an effort to provide first-aid to students at baseline for all four outcomes (alcohol, other drug, mental health, and academic problems) was consistently higher in the training-as-usual condition.
Table 1.
Description of measures by investigational training condition, N = 566.
|
Peer Hero
Training (1+ referral actions at Baseline) |
Training-as-
Usual (1+ referral actions at Baseline) |
Peer Hero Training
(1+ referral actions in past 30 days at follow-ups: F1-F3) |
Training-as-Usual
(1+ referral actions in past 30 days at follow-ups: F1-F3) |
|||||||
|---|---|---|---|---|---|---|---|---|---|---|
| N | % | N | % | F1% | F2% | F3% | F1% | F2% | F3% | |
| Referral problem | ||||||||||
| Alcohol | 6 | 2.3% | 23 | 8.0% | 25.3% | 27.4% | 20.9% | 29.3% | 24.9% | 20.1% |
| Marijuana | 2 | 0.7% | 10 | 3.5% | 7.9% | 18.0% | 9.8% | 13.6% | 14.9% | 14.1% |
| Mental health | 25 | 9.5% | 55 | 19.2% | 78.4% | 85.7% | 72.8% | 76.8% | 71.8% | 61.7% |
| Academic | 13 | 4.9% | 29 | 10.1% | 63.0% | 62.2% | 56.3% | 58.0% | 46.0% | 43.8% |
| Mean(SE) | Mean(SE) | Mean(SE) | Mean(SE) | |||||||
| Attitudinal Measures | ||||||||||
| Perceived referral barriers (range: 8-40) |
25.9(0.3) | 25.4(0.3) | 26.0(0.4) | 24.9(0.5) | 23.7(0.6) | 24.9(0.3) | 24.6(0.3) | 23.0(0.6) | ||
| Referral self-efficacy (range: 3-15) |
10.3(0.1) | 11.1(0.1) | 10.6(0.1) | 10.9(0.2) | 11.1(0.3) | 11.0(0.1) | 10.9(0.1) | 10.8(0.3) | ||
| Referral anticipatory anxiety (range: 4-20) |
8.2(0.2) | 8.4(0.2) | 8.4(0.2) | 8.4(0.3) | 8.8(0.4) | 8.5(0.1) | 8.8(0.2) | 9.0(0.2) | ||
| Perceived referral norms – alcohol use (range: 5-25) |
19.6(0.3) | 19.3(0.2) | 19.1(0.3) | 18.5(0.4) | 18.2(0.4) | 18.6(0.2) | 18.1(0.2) | 17.5(0.3) | ||
| Perceived referral norms – drug use (range: 5-25) |
10.4(0.3) | 10.7(0.2) | 10.9(0.3) | 11.5(0.4) | 11.8(0.6) | 11.4(0.2) | 11.9(0.3) | 12.5(0.5) | ||
| Perceived referral norms – mental health (range 5-30) |
23.3(0.2) | 23.3(0.2) | 23.0(0.2) | 22.8(0.4) | 23.0(0.06) | 22.9(0.2) | 22.4(0.2) | 22.2(0.06) | ||
The trajectories in Figure 2 depict the average number of first-aid efforts reported by RAs in the Peer Hero Training program condition compared with the training-as-usual condition. Although the number of RA first-aid efforts in both conditions increased over time for each outcome (see Figure 2), these effects were more robust in the Peer Hero Training program condition. At the baseline assessment, RAs in the training-as-usual condition had a slightly higher number of other drug first-aid efforts; however, the number of alcohol, mental health and academic first-aid efforts were similar across groups. The number of first-aid efforts increased for all outcomes across groups at follow-up 1; however, the Peer Hero Training program condition surpassed the training-as-usual condition across all first-aid effort outcomes at follow-up 2.
Figure 2.
Effect of training conditions on RA first-aid effort from baseline to follow-up 2.
The direct relationship between the Peer Hero Training program and each type of first-aid effort is displayed in Table 2. We expected that the Peer Hero Training program would have a positive effect on each type of RA first-aid effort. Indeed, as judged by the incidence rate ratios (IRRs), the program had a significant, positive effect on all four past 30-day first-aid efforts at follow-up 2 as well as a positive past 30-day effect on alcohol and mental health first-aid efforts at both follow-up 1 and 2 time points. At follow-up 1, RAs in the Peer Hero Training program were more likely to have made past 30-day first-aid efforts for alcohol problems (IRR = 5.21; 95% CI 2.38 - 11.42), and mental health problems (IRR = 1.80; 95% CI 1.26 - 2.57). At follow-up 2, the RAs in the Peer Hero Training program made more than 10 times as many past 30-day first-aid efforts for alcohol as RAs in the training-as-usual condition during the same time period (IRR = 10.70; 95% CI 4.83 - 23.70). RAs in the Peer Hero Training program were also more likely to have made past 30-day first-aid efforts for drug problems (IRR = 13.94; 95% CI 3.69 - 52.62), mental health problems (IRR = 2.96; 95% CI 2.05 - 4.26), and academic problems (IRR = 3.43; 95% CI 2.11 - 5.57) compared to RAs assigned to the training-as-usual condition at follow-up 2.
Table 2.
Direct effects of Peer Hero Training Program on first-aid efforts over time, N = 566.
| Alcohol First-Aid Efforts |
Drug First-Aid Efforts | Mental Health First-Aid Efforts |
Academic First-Aid Efforts |
|
|---|---|---|---|---|
| IRR (95% CI) | IRR (95% CI) | IRR (95% CI) | IRR (95% CI) | |
| Investigational Training Program Effects over Time | ||||
| Baseline -> Follow-up 1 | 5.21(2.38 - 11.42)*** | 2.38(0.63 - 8.99) | 1.80(1.26 - 2.57)** | 1.57(0.98 - 2.52) |
| Baseline -> Follow-up 2 | 10.70(4.83 - 23.70)*** | 13.94(3.69 - 52.62)*** | 2.96(2.05 - 4.26)*** | 3.43(2.11 - 5.57)*** |
| Attitudinal Measures | ||||
| Perceived Referral Barriers | 0.97(0.94 - 0.99)* | 0.94(0.89 - 0.98)* | 1.01(0.99 - 1.02) | 1.01(0.99 - 1.03) |
| Referral Anticipatory Anxiety | 1.00(0.95 - 1.06) | 1.04(0.96 - 1.13) | 0.96(0.92 - 0.97)* | 0.97(0.94 - 1.01) |
| Referral Self-efficacy | 0.93(0.87 - 0.99)* | 1.00(0.91 - 1.10) | 0.98(.94 - 1.01) | 0.96(0.92 - 0.99)* |
| Perceived Referral Norms- Alcohol Use |
1.03(0.99 - 1.06) | -- | -- | -- |
| Perceived Referral Norms- Drug Use |
-- | 0.95(0.91 - 0.99)* | -- | -- |
| Perceived Referral Norms- Mental Health |
-- | -- | 1.03(1.01 - 1.05)** | -- |
| Covariates (Baseline) | ||||
| Gender (male) | 0.97(0.61 - 1.55) | 2.77(1.41 - 5.46)** | 0.62(0.50 - 0.77)*** | 0.93(0.69 - 1.25) |
| Race (White) | 0.86(0.51 - 1.45) | 0.31(0.15 - 0.63)** | 1.05(0.83 - 1.33) | 0.61(0.44 - 0.83)** |
| Age | 1.16(0.93 - 1.46) | 1.14(0.82 - 1.58) | 1.18(1.06 - 1.32)** | 1.13(0.97 - 1.31) |
| Returning RA Status | 0.91(0.56 - 1.49) | 1.66(0.82 - 3.36) | 1.64(1.30 - 2.06)*** | 1.86(1.35 - 2.56)*** |
p < 0.05,
p < 0.01,
p < 0.001
Note: No assessment was made of perceived referral norms for academic problems.
IRR = Incidence Rate Ratio.
Sensitivity analyses demonstrated that these results were highly stable, despite the inclusion of one campus that did not participate in the Peer Hero Training program after follow-up 1. When this campus was excluded from analyses, the significant effects of Peer Hero Training program remained in place for each of the four RA first-aid efforts at each follow-up (results not shown).
The observed training effects were independent of the attitudinal variables that the research team theoretically linked to RA first-aid efforts; that is, the four attitudes did not mediate between training condition and first-aid efforts. Therefore, these measures were treated as covariates. Independent of their training condition, RAs with lower perceived referral barriers had higher rates of first-aid efforts for alcohol (IRR = 0.97; 95% CI 0.94 - 0.99) and other drugs (IRR = 0.94; 95% CI 0.89 - 0.98). RAs with higher levels of anticipatory anxiety were less likely to make first-aid efforts for mental health problems (IRR = 0.96; 95% CI 0.92 - 0.97), and RAs with higher referral self-efficacy were less likely to make first-aid efforts for alcohol (IRR = 0.93; 95% CI 0.87 - 0.99) and academic problems (IRR = 0.96; 95% CI .92 - .99). RAs who perceived drug-related referrals to be less normative were more likely to make first-aid efforts for drug problems compared to those who perceived these referrals to be more normative (IRR = 0.95; 95% CI 0.91 - 0.99). RAs who perceived mental health first-aid efforts to be more normative were more likely to make such efforts (IRR = 1.03; 95% CI 1.01 - 1.05) than RAs who perceived mental health referrals to be less normative. Male RAs were more likely to make first-aid efforts for drug problems (IRR = 2.77; 95% CI 1.41 - 5.46), whereas female RAs were more likely to make first-aid efforts for mental health problems (IRR = 0.62; 95% CI 0.50 - 0.77). White RAs were less likely than non-White RAs to make first-aid efforts for drug problems (IRR = .31; 95% CI .15 - .63) and academic problems (IRR = 0.61; 95% CI 0.44 - 0.83). Older RAs were more likely to make first-aid efforts for mental health problems (IRR = 1.18; 95% CI 1.06 - 1.32). RAs who had served as an RA prior to the baseline assessment were more likely than RAs who were new at baseline to make first-aid efforts for mental health (IRR = 1.64; 95% CI 1.30 - 2.06) and academic problems (IRR = 1.86; 95% CI 1.35 - 2.56).
Discussion
Historically, the training of RAs has not been an evidence-informed practice. The lack of investment in systematic development and testing of alcohol, other drug, and mental health first-aid training is surprising given the longstanding recognition that RAs are not well-prepared to address the challenging situations they encounter in their living units (Dodge, 1990; Rubington, 1996). More recently, Owens (2011) concluded that the current demands of the RA staff position require a transformation in the type of pre-service and in-service training on most campuses. Findings from the present study offer initial steps towards the strengthening of first-aid training for RAs.
We hypothesized that RAs assigned to the Peer Hero Training program would engage in a significantly greater number of first-aid efforts for alcohol, other drug, and mental health problems in their living units compared to RAs assigned to a training-as-usual condition. Although there was a convergence of training condition effects at the end of the academic year, the trial outcomes observed prior to Spring Break of the Spring Semester provided support for this hypothesis. More specifically, positive Peer Hero Training effects were observed prior to Spring Break for drug and academic first-aid efforts, indicating a lagged effect of the program, possibly related to the follow-up Peer Hero Training sessions and/or slower emergence of these two problems in the resident population. In a qualitative study of RAs, Reingle et al. (2010) found that RAs tended to be slow or hesitant to discuss concerns they may have about alcohol, drug, or mental health conditions with residents. Nevertheless, positive Peer Hero Training effects were observed prior to both Thanksgiving and Spring Breaks for alcohol and mental health first-aid efforts. In summary, the Peer Hero Training program had significant, positive effects on first-aid efforts for alcohol, drug, mental health, and academic problems.
We did not expect to find a significant Peer Hero Training effect on first-aid efforts for academic problems. One possible explanation is that increases in academic first-aid efforts resulted from RAs attempting to help residents who had co-occurring problems that involved not only academics, but alcohol, other drug, or mental health problems as well. Existing research does support the contention that academic problems co-occur with alcohol (Wechsler & Nelson, 2008), other drug (Arria et al., 2013), and mental health problems (Hysenbegasi, Hass, & Rowland, 2005) in the college student population.
We also hypothesized that perceived referral barriers, referral self-efficacy, referral anticipatory anxiety, and perceived referral norms would mediate between training condition and first-aid outcomes. We found no evidence to support this hypothesis. The four attitudinal measures did not fluctuate drastically over time across groups, regardless of training condition. However, these measures often had direct effects on first-aid efforts, that is, independent of training condition assignment. For instance, greater perceived barriers to making first-aid efforts were associated with fewer first-aid efforts RAs made for alcohol and other drug problems. Similarly, higher levels of referral anticipatory anxiety were associated with fewer first-aid efforts for mental health conditions. In the case of referral self-efficacy and referral norms, the observed associations were in theoretically unexpected directions. These findings suggest that self-efficacy and referral norms may be artifacts of previous first-aid efforts. First-aid actions could potentially erode the RA’s own referral self-efficacy, thereby weakening perceptions that helping residents is an expected practice. A more intensive evaluation of the Peer Hero Training program might include qualitative methods (e.g., RAs’ reflections on the training program) to determine how, if, and/or why the training program influenced RAs’ first aid-efforts.
The study has a number of strengths. First, the Peer Hero Training program offers an innovative approach to training RAs based on interactive video dramatizations of residence life events. The video content engage RAs through story-telling and interactive features that require RAs to make decisions about how to approach and discuss their concerns with residents. Therefore, we expect that the training content will be more readily retained than that provided by traditional didactic training programs. Second, RAs were asked to report their first-aid efforts prior to completing each training session. This design removed potential biases associated with the administration of a survey after the implementation of a training session. Third, the Peer Hero Training program includes three training sessions over the course of the academic year (baseline and two follow-ups), compared to RA training-as-usual on alcohol, other drug, and mental health problems that takes place only once prior to the beginning of an academic year. Fourth, the online format of the Peer Hero Training program facilitates the delivery of standardized first-aid training to multiple campus locations, including those with insufficient local resources for training RAs on alcohol, other drug, and mental health issues. Finally, given that the RA plays a pivotal role in linking college students to treatment resources that they may need, the Peer Hero Training program advances the science of prevention by addressing a substantial gap in evidence-based, first-aid training. However, as noted earlier, one campus in the Peer Hero Training condition elected to dropout prior to the end of the trial even though the burden of participation was relatively low (given the online format). Thus, for these programs to be successful, they must be adequately funded and be endorsed by senior residence life administrators.
Limitations
This study has three specific limitations. First, only 8 campuses were included in this preliminary trial. This may raise questions about sample adequacy. However, we observed consistent and strong program effects for alcohol, other drug use, mental health, and academic first-aid outcomes. Second, this study did not measure the alcohol and other drug use, or the mental health problems, of the RAs who participated in this trial. It might be expected that these problems exist at lower rates among RAs than in the general student population. However, very little is known about their prevalence in the RA population, and how their presence affects training impact. Third, the study did not include an evaluation of the effects on residents who were the recipients of RA first-aid. Thus, nothing is known about the outcomes of RA first-aid efforts.
Conclusions and Recommendations for Future Research
Future research should test the Peer Hero Training program in an expanded trial involving a greater number of campuses and a more comprehensive, mixed-methods evaluation of RA behavior, the living environment, the content of “training-as-usual,” and include measures from RA supervisors and residents. In an expanded trial, assessments should be made of RAs’ personal alcohol and other drug use, as well as their history of mental health problems. The expectations and practices of RA supervisors, with respect to first-aid efforts, should be evaluated in future studies as they may moderate the effects of the Peer Hero Training program. First-aid recipients should be evaluated in future trials to determine the rate at which they obtain and benefit from professional mental health treatment. Finally, the effects of the Peer Hero Training program on living environments should be conducted to evaluate potential impacts of the program on academic norms and achievement, student retention, social cohesion, and quality of residential living. Further, iterative feedback to the RA could be incorporated into this program based on each RA’s responses to attitudinal measures, which may increase first-aid efforts as the academic year progresses. This initial evaluation demonstrated the potential utility of an automated, engaging, easily disseminated, and standardized RA training tool that could be readily disseminated across diverse college and university campuses.
Acknowledgments
This research was supported by the National Institutes of Health, National Institute on Alcohol Abuse and Alcoholism 5R42AA016990, Co-PIs: Dennis L. Thombs, PhD and Doug Olson.
The authors thank Gary Kimble, Dan Oltersdorf, Steve Saffian, Doug Olson, and Noah Sodano for their important contributions to this study.
Footnotes
The authors declare that they have no conflict of interest.
Contributor Information
Dennis L. Thombs, Department of Behavioral and Community Health, Texas Prevention Institute, University of North Texas Health Science Center.
Jennifer M. Reingle Gonzalez, Division of Epidemiology, Human Genetics, and Environmental Sciences, University of Texas School of Public Health, Dallas Regional Campus.
Cynthia J. Osborn, Counseling and Human Development Services, Kent State University.
Matthew E. Rossheim, Department of Behavioral and Community Health, University of North Texas Health Science Center.
Sumihiro Suzuki, Department of Biostatistics and Epidemiology, University of North Texas Health Science Center.
References
- American College Health Association American College Health Association – National College Health Assessment Spring 2008 reference group data report (abridged) Journal of American College Health. 2009;57:477–488. doi: 10.3200/JACH.57.5.477-488. [DOI] [PubMed] [Google Scholar]
- American Psychiatric Association . Diagnostic and statistical manual of mental disorders. 4th Author; Washington, D.C.: 2000. [Google Scholar]
- Arria AM, Wilcox HC, Caldeira KM, Vincent KB, Garnier-Dykstra LM, O'Grady KE. Dispelling the myth of "smart drugs": cannabis and alcohol use problems predict nonmedical use of prescription stimulants for studying. Addictive Behaviors. 2013;38:1643–1650. doi: 10.1016/j.addbeh.2012.10.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blanco C, Okuda M, Wright C, Hasin DS, Grant B, Liu SM, Olfson M. Mental health of college students and their non-college-attending peers. Archives of General Psychiatry. 2008;65:1429–1437. doi: 10.1001/archpsyc.65.12.1429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blimling G. The resident assistant. 6th Kendall Hunt Publishing; Dubuque, IA: 2003. [Google Scholar]
- Buscemi J, Murphy JG, Martens MP, McDevitt-Murphy ME, Dennhardt AA, Skidmore JR. Help-seeking for alcohol-related problems in college students: Correlates and preferred resources. Psychology of Addictive Behaviors. 2010;24:571–580. doi: 10.1037/a0021122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dodge S. The demanding job of resident assistant: Has it grown too big for students? Chronicle of Higher Education. 1990 Feb 21; Available: chronicle.com/article/The- Demanding-Job-of-Resident/69138/. Accessed July 19, 2014. [Google Scholar]
- Elleven RK, Allen J, Wircenski M. Resident assistant training: A southwest perspective. College Student Journal. 2001;35:609–616. [Google Scholar]
- Glanz K, Rimer BK, Viswanath KV. Health behavior and health education: Theory, research, and practice. 4th Wiley, John & Sons; Hoboken, NJ: 2008. [Google Scholar]
- Gratwick-Sarll K, Bentley C. Improving eating disorders mental health literacy: A preliminary evaluation of the "Should I Say Something?" workshop. Eating Disorders. 2014;25:1–15. doi: 10.1080/10640266.2014.925764. [DOI] [PubMed] [Google Scholar]
- Hysenbegasi A, Hass SL, Rowland CR. The impact of depression on the academic productivity of university students. Journal of Mental Health Policy and Economics. 2005;8:145–151. [PubMed] [Google Scholar]
- Johnston LD, O'Malley PM, Bachman JG, Schulenberg JE. Institute for Social Research, University of Michigan; Ann Arbor, MI: 2013. Monitoring the Future National Survey results on drug use, 1975-2012. Volume II: College students and adults ages 19-50. Available: http://www.monitoringthefuture.org//pubs/monographs/mtf-vol2_2012.pdf. Accessed June 28, 2014. [Google Scholar]
- Kadison RD. The mental health crisis: What colleges must do. The Chronicle of Higher Education. 2004;51(16):B20. Available: http://chronicle.com/article/The-Mental-Health-Crisis-What/1712. Accessed July 1, 2014. [Google Scholar]
- Kelly CM, Mithen JM, Fischer JA, Kitchener BA, Jorm AF, Lowe A, Scanlan C. Youth mental health first aid: A description of the program and an initial evaluation. International Journal of Mental Health Systems. 2011;5:4–12. doi: 10.1186/1752-4458-5-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kingston AH, Jorm AF, Kitchener BA, Hides L, Kelly CM, Morgan AJ, Hart LM, Lubman DI. Helping someone with problem drinking: Mental health first aid guidelines - A Delphi expert consensus study. BMC Psychiatry. 2009;9:79. doi: 10.1186/1471-244X-9-79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kingston AH, Morgan AJ, Jorm AF, Hall K, Hart LM, Kelly CM, Lubman DI. Helping someone with problem drug use: A Delphi consensus study of consumers, carers, and clinicians. BMC Psychiatry. 2011;11:3. doi: 10.1186/1471-244X-11-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kitchener BA, Jorm AF. Mental health first aid training in a workplace setting: A randomized controlled trial. BMC Psychiatry. 2004;4:23–28. doi: 10.1186/1471-244X-4-23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kitchener BA, Jorm AF. Mental health first aid training: review of evaluation studies. Australian and New Zealand Journal of Psychiatry. 2006;40:6–8. doi: 10.1080/j.1440-1614.2006.01735.x. [DOI] [PubMed] [Google Scholar]
- Owens EW. The resident assistant as paraprofessional counselor and crisis Interventionist: A study of lived experience. 2011. Doctoral Dissertation. Duquesne University. ProQuest UMI Number: 3443375.
- Pekevski J. First responders and psychological first aid. Journal of Emergency Management. 2013;11(1):39–48. doi: 10.5055/jem.2013.0126. [DOI] [PubMed] [Google Scholar]
- Reingle J, Thombs D, Osborn C, Saffian S, Oltersdorf D. Mental health and substance use: A qualitative study of resident assistants’ attitudes and referral practices. Journal of Student Affairs Research and Practice. 2010;47:325–342. [Google Scholar]
- Rossetto A, Jorm AF, Reavley NJ. Quality of helping behaviours of members of the public towards a person with a mental illness: A descriptive analysis of data from an Australian national survey. Annals of General Psychiatry. 2014;13(1):1–21. doi: 10.1186/1744-859X-13-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rubington E. The ethic of “responsible drinking.”. Deviant Behavior: An Interdisciplinary Journal. 1996;17:319–335. [Google Scholar]
- Sharkin BS, Plageman PM, Mangold SL. College student response to peer in distress: An exploratory study. Journal of College Student Development. 2003;44:691–698. [Google Scholar]
- Svensson B, Hansson L. Effectiveness of mental health first aid training in Sweden. A randomized controlled trial with a six-month and two-year follow-up. PLoS One. 2014;9(6):e100911. doi: 10.1371/journal.pone.0100911. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taub DJ, Servaty-Seib HL. Training resident assistants to make effective referrals to counseling. Journal of College and University Student Housing. 2011;37(2):10–25. [Google Scholar]
- Taub DJ, Servaty-Seib HL, Miles N, Lee J, Wachter Morris CA, Prieto-Welch SL, Werden D. The impact of gatekeeper training for suicide prevention on university resident assistants. Journal of College Counseling. 2013;16(1):64–78. [Google Scholar]
- U.S. Census Bureau Group quarters population in college/university housing; 2010 Census Congressional District Summary File (113th Congress); 2010. Available: http://factfinder2.census.gov. Accessed June 27, 2014. [Google Scholar]
- Wechsler H, Nelson TF. What we have learned from the Harvard School Of Public Health College Alcohol Study: Focusing attention on college student alcohol consumption and the environmental conditions that promote it. Journal of Studies on Alcohol and Drugs. 2008;69:481–90. doi: 10.15288/jsad.2008.69.481. [DOI] [PubMed] [Google Scholar]
- Wu LT, Pilowsky DJ, Schlenger WE, Hasin D. Alcohol use disorders and the use of treatment services among college-age young adults. Psychiatric Services. 2007;58:192–200. doi: 10.1176/appi.ps.58.2.192. [DOI] [PMC free article] [PubMed] [Google Scholar]