Up to 13% of women experience a major depressive episode during pregnancy, with an even greater proportion reporting clinically significant depressive symptom elevations (Gavin et al., 2005). Numerous studies have documented adverse outcomes associated with antenatal depression (Davalos, 2012; Grigoriadis et al., 2013). Compared to non-depressed women, depressed pregnant women experience higher rates of pre-eclampsia (Cripe, Frederick, Qiu, & Williams, 2011), spontaneous abortion (Sugiura-Ogasawara et al., 2002), and pre-birth complications (Palladino et al., 2011), and infants of depressed mothers are at higher risk of pre-term delivery and low birth weight (Grote et al., 2010). Antenatal depression often precedes postpartum depression, which is associated with cognitive and emotional problems in children (Beebe, 2008; Murray, 2003).
Lack of acceptable treatments for antenatal depression
Although pharmacological and non-pharmacologic interventions have been developed to treat depression in the general population, fewer clinical trials have examined the efficacy and safety of depression interventions during pregnancy. Pregnant women have unique concerns that influence their treatment decisions, and the most available depression treatment in the community, antidepressant medication, is viewed by many women to be unacceptable during pregnancy (Battle, Salisbury, Schofield, & Ortiz-Hernandez, 2013). Fetal exposure concerns are common among both women and providers, and risk / benefit decision-making can be complex due to the large and at times conflicting literature addressing the safety of prenatal antidepressant use (Chaudron, 2013). Psychotherapeutic approaches such as interpersonal psychotherapy and cognitive behavioral psychotherapy have shown promise in the treatment of perinatal depression (Sockol, Epperson, & Barber, 2011), but engagement in psychotherapy is often hampered by logistical or attitudinal barriers (Kim et al., 2010; O'Mahen, 2008). Some pregnant women may be reluctant to seek mental health care due to stigma; others may have less available due to increased medical appointments necessary for routine prenatal care, or other tasks related to preparing for a new baby.
New treatments are needed
Although public awareness of perinatal mental health issues has increased, the majority of depressed pregnant and postpartum women do not receive mental health care (Flynn, 2006). Due to the high public health cost of untreated antenatal depression, there is a need to develop more acceptable strategies to treat mood symptoms during pregnancy (Battle, Uebelacker, & Magee, 2012; Freeman, 2011).
Prenatal yoga: A promising approach
Prenatal yoga, a form of yoga tailored to be safe, gentle, and particularly helpful for pregnant women, represents a promising strategy for the treatment of maternal depression. One of the ways in which prenatal yoga may have an impact on depression is by increasing mindfulness, or nonjudgmental attention to the present moment. Mindfulness is directly taught in many yoga classes. This skill many generalize beyond classes, thereby reducing (negative) self-judgment, and/or increasing focus on the present moment rather than ruminating about the past or future. Yoga has been increasingly studied in non-perinatal populations as a potential treatment for physical health conditions, including back pain, cardiovascular disease, and discomfort associated with cancer (Sherman, 2012). Although limited, some trials have examined yoga as a depression treatment. To date, randomized controlled trials (RCTs) evaluating yoga for depression have been generally positive (Uebelacker et al., 2010); however, most have had significant methodological limitations, limiting firm conclusions that may be drawn.
Because prenatal yoga differs from yoga geared towards the general population in content, pace, and use of modifications, and because pregnant women have unique physiological needs, it is important to examine yoga specifically designed for the prenatal period. Although research has documented interest in prenatal yoga among pregnant women seeking depression treatment (Battle, Uebelacker, Howard, & Castaneda, 2010), little research has examined the efficacy of prenatal yoga in reducing symptoms among clinically depressed pregnant women. Most published prenatal yoga RCTs have focused on physical health outcomes rather than psychological wellbeing (Curtis, Weinrib, & Katz, 2012). One RCT with depressed women did find positive outcomes in the group receiving biweekly prenatal yoga classes for 12 weeks relative to a routine prenatal care group (Field et al., 2012). Another study of the same intervention (Field, Diego, Delgado, & Medina, 2013) found that improvements in depression were similar to those in a brief social support condition over a period of 12 weeks. However, generalizability of results for both trials are limited by reliance upon self-report scales, and use of a non-standard, brief (20 minute) class format inconsistent with yoga classes offered in the community (Sherman, 2012). Further, although it is clear that the yoga intervention included a series of asanas (postures), there was no discussion of the style or tone of the classes (e.g., whether mindfulness was emphasized) and presence or absence of adverse events was not discussed. A recent small non-randomized trial (n=18) tested a 10-week mindfulness-based prenatal yoga intervention that utilized a more typical (90 minute) class format, finding that self-reported depression was significantly reduced by post-intervention (Muzik, Hamilton, Lisa Rosenblum, Waxler, & Hadi, 2012). The intervention included a series of asanas and a clear focus on mindfulness. Although promising, a standard interviewer-rated depression scale was not used, and the mixed psychiatric sample included only a small number of women with a current depression diagnosis. In sum, initial studies provide encouragement regarding prenatal yoga as a strategy to lower symptoms among depressed pregnant women, but are not definitive.
The current study
The goal of the current study was to develop a prenatal yoga intervention for clinically depressed women using a class structure and content that is consistent with prenatal yoga taught in the community, and to evaluate the acceptability, feasibility and preliminary efficacy of the intervention in an open pilot trial. In addition to careful measurement of changes in depression, we examined pre-post changes in mindfulness, a possible mechanism by which yoga may potentially lower depressive symptoms (Uebelacker et al., 2010). In the current study, we expected that mindfulness would increase over time and depression would decrease over time.
Method
This study was approved for human subjects protections by our institution's Institutional Review Board.
Participants
Eligibility
Participants met the following criteria: 12-26 weeks gestation with a singleton pregnancy; absence of medical problems for which prenatal yoga is contraindicated; 18 or older; English-speaking; not a regular yoga practitioner; available to attend at least one class time; absence of significant alcohol or drug use during pregnancy; presence of a major or minor depressive episode during the pregnancy; absence of significant suicidality; absence of bipolar disorder, schizophrenia, or a chronic psychotic condition; absence of severe post-traumatic stress disorder, obsessive compulsive disorder, or panic disorder; and a Quick Inventory of Depressive Symptomatology (QIDS) (A. J. Rush et al., 2005) score between 7-20. We judged 7 to be the minimum score for which we might see clinically important change; scores over 20 represent severe depression that merits more extensive treatment and oversight.
Demographic, pregnancy, and psychiatric characteristics
We enrolled 34 participants. Please see Table 1 for demographic, pregnancy and psychiatric characteristics. The sample was diverse with respect to race and ethnicity. Many had had a college education, yet were fairly low-income. Half of participants reported having an unplanned pregnancy; less than half had at least one child. The majority of women met criteria for current major depressive disorder (MDD). Baseline depression symptom severity ranged from mild to moderate. Four women were engaged in other depression treatment at baseline; the majority (n = 29; 85%) did not engage in any standard depression treatment at any time during the trial.
Table 1.
Characteristics of the study sample.
| N (%) or Mean(SD) and range | |
|---|---|
| Demographics | |
| Age in years | 28 (5.4); range =19-40 |
| Marital status | |
| Married/ living with partner | 23 (68%) |
| Single/ divorced | 11 (32%) |
| Ethnicity | |
| Latina/ Hispanic | 14 (41%) |
| Not Latina/ Hispanic | 20 (59%) |
| Race | |
| Black / African American | 5 (15%) |
| White | 14 (41%) |
| Multiracial | 2 (6%) |
| Other/ race not specified | 11 (32%) |
| Educational attainment | |
| High school not completed | 3 (9%) |
| High school degree | 5 (15%) |
| Some college | 9 (26%) |
| Completed bachelor's degree | 17 (50%) |
| Yearly Combined Family Income | |
| < $25,000 | 11 (32%) |
| $25,000 - $50,000 | 12 (35%) |
| $50,000 or greater | 9 (26%) |
| Declined to specify | 2 (6%) |
| Employment status | |
| Full time | 15 (44%) |
| Part-time | 5 (15%) |
| Full-time parent/ homemaker | 0 |
| Student | 6 (18%) |
| Unemployed | 7 (21%) |
| Declined to specify | 1 (3%) |
|
Pregnancy characteristics at baseline | |
| Average weeks gestation | 19.0 (4.7); range = 12-26.5 |
| Pregnancy planning | |
| Pregnancy planned | 16 (47%) |
| Pregnancy not planned | 17 (50%) |
| Declined to specify | 1 (3%) |
| Prior live births | |
| None | 22 (65%) |
| One or more | 12 (45%) |
|
Psychiatric characteristics | |
| Diagnosis | |
| Current major depressive disorder (MDD) | 25 (74%) |
| MDD earlier in pregnancy | 4 (12%) |
| Current minor depressive disorder | 4 (12%) |
| Minor depressive disorder earlier in preg. | 1 (3%) |
| Baseline QIDS score | 12.6 (3.2); range = 7- 18 |
| Baseline EPDS score | 13.0 (5.3); range = 2-23 |
| Baseline depression treatment | |
| Taking an antidepressant | 1 (3%) |
| Engaged in psychotherapy | 4 (12%) |
Procedures
Participants entered the study on a continual basis. We advertised at local OB/GYN practices and other locations serving perinatal women. Women who called expressing interest completed a screening interview that included the Patient Health Questionnaire – 9 (PHQ9) (Kroenke, Spitzer, & Williams, 2001) to assess depressive symptoms. If participants did not at least have a low level of depression symptoms (i.e., a PHQ-9 total score ≥ 5 and a “1” on the mood or anhedonia item), we judged that they would be unlikely to meet eligibility criteria. If judged potentially eligible, the caller was scheduled for an in-person assessment. At that interview, if she appeared eligible, we requested permission to contact her obstetric provider to gain medical clearance for participation. Once we received written clearance, participants could start attending prenatal yoga classes.
Participants completed assessments at baseline and endpoint (10 weeks). In addition, we conducted phone assessments throughout the 10-week period. The schedule for interim assessments shifted mid-way through the trial in response to participant feedback; initially these were scheduled at weeks 2, 4, 6, and 8; however, we moved to assessments to weeks 3.3 and 6.6 only. Fewer assessments enabled us to monitor participant safety and symptoms while minimizing burden.
Because this was a pilot treatment development study, we monitored participant adherence carefully. Initially, we did not question women about availability of transportation for class. We paid women for attendance at assessments but not classes; women could earn a total of $80 for assessments including $40 for the initial assessment. After the first 25 participants enrolled, we observed that some women enrolled, yet experienced difficulty getting to class. In response, we put increased emphasis on the need for reliable transportation. To decrease the possibility that women attended the initial assessment simply to be paid, we decreased the amount paid for baseline and follow up assessments (to $20 rather than $40). We added a small incentive ($10) each time a participant attended one class per week for two consecutive weeks. Thus, the total amount a woman could earn remained $80.
Measures
Demographics and pregnancy characteristics
We assessed the following via patient self-report: age, relationship status, race, ethnicity, education, family income, work status, pregnancy history, gestation.
Depression diagnosis
The Structured Clinical Interview for DSM-IV Axis I Disorders- Patient Version, Mood Module and Psychotic Screen SCID-IP; (First, Spitzer, Gibbon, & Williams, 2001) was used at baseline to diagnose mood disorders. Interviews were administered by trained research assistants; questions about diagnosis were resolved by licensed psychologists (the first or second author).
Depression severity
We used the interviewer-rated QIDS (A. J. Rush, et al., 2005) both to determine presence of depressive symptoms for study eligibility and to assess change in depression severity over time. The QIDS is a psychometrically strong measure that is widely used in depression treatment trials. Scores of 0-5 represent no depression, 6-10 mild depression, and 11-15 moderate depression (A J Rush et al., 2003; Trivedi et al., 2004). We also administered the Edinburgh Postnatal Depression Scale (EPDS) (Cox, 1987) to assess change in depression severity over time. The EPDS is a widely-used, 10-item self-report scale for perinatal populations with established validity and reliability. Both were administered at all assessment points.
Mental health treatment
The Treatment Response to Antidepressant Questionnaire (TRAQ; (Posternak et al., 2004) was used to assess antidepressant usage. We used a brief structured interview to collect information about other mental health treatments. Measures were administered at baseline and 10 weeks.
Expectations and satisfaction with treatment
Treatment credibility and patient expectations for treatment success were measured at baseline with the Credibility Expectancy Questionnaire (Devilly & Borkovec, 2000). Scores on the two subscales – i.e., credibility and expectancy-- range from 1 (not at all) to 9 (very much). The Client Satisfaction Questionnaire-8 (CSQ-8; (Larsen, Attkisson, Hargreaves, & al., 1979) is an 8-item scale that yields a score ranging from 8-32, with 32 indicating highest satisfaction. This scale has acceptable psychometric properties (Nguyen, Attkisson, & Stegner, 1983). The CSQ-8 was administered at endpoint.
Exercise/ prenatal yoga
The International Physical Activity Questionnaire (IPAQ) (Craig et al., 2003) is a self-report measure of physical activity that was administered at all timepoints. We added questions to assess number of prenatal yoga classes attended, amount of home yoga practice, and overall minutes per week spent practicing yoga. We also used data from class attendance sheets.
Mindfulness
The Five-Facet Mindfulness Questionnaire (FFMQ; (Baer, Smith, Hopkins, Krietemeyer, & Toney, 2006) is a 39-item questionnaire measuring five aspects of mindfulness: non-reactivity to inner experience, observing, acting with awareness, describing with words, and non-judging of experience. Higher scores reflect more mindfulness. The FFMQ was administered at baseline and endpoint.
Description of prenatal yoga classes
Prenatal yoga classes occurred twice per week, with one daytime class and one evening class offered. Women were invited to attend twice per week; however, we understood that most women would only be able to attend once per week. We provided women with a yoga mat and a prenatal yoga DVD and encouraged them to practice at home. Classes were 75 minutes long, gentle in nature, and designed to be safe for pregnant women, including frequent use of props and modifications of poses. Consultation with experts in prenatal yoga helped to ensure that class content and format was consistent with prenatal yoga classes typically offered in the community. Class content was documented in a detailed intervention manual, and included the following components: an opening greeting; pranayama, breath awareness or meditation; a warm-up that included gentle, breath-linked movement; standing poses; floor poses; a final resting pose; pranayama or meditation; and a brief class closing, including discussion of homework. Yoga teachers were Registered Yoga Teachers (RYTs) who had prenatal yoga training prior to the study, as well as further study-specific training. Consistent with common principles of yoga practice, instructors were asked to: (1) demonstrate and encourage a nonjudgmental focus on sensation experienced in the present moment (i.e., mindfulness); (2) emphasize breathing awareness; (3) have an open and non-judgmental attitude toward pregnancy and birth-related choices; and (4) to keep in mind that participants could potentially have both positive and negative reactions to their pregnancy, and that participants may vary in degree of attachment to the developing baby.
Data analysis
We used descriptive statistics to characterize the sample. In order to examine change in depression over time, we employed multilevel linear models, with depression symptoms as the outcome variable and time (i.e., weeks) as the sole predictor variable. The intercept was specified as random. A multilevel modeling approach is advantageous in that, compared to a pre-post t-test, the multilevel model results in increased power because it uses all available data at each timepoint when the outcome variable is measured. Further, the model can accommodate varying interim assessment timepoints. In order to understand the association between minutes per week of yoga and depression symptoms, we conducted a similar multilevel analysis in which we examined whether minutes of yoga in the previous week was associated with depression severity in the previous week. Again, only the intercept was specified as random. We did not include the baseline timepoint in the model as inclusion of this timepoint could artificially inflate the association between the two variables of interest. Depression severity (ie., QIDS) served as the outcome variable. Time and minutes per week of yoga were time-varying predictors. Finally, to examine changes in mindfulness over time, we conducted paired t-tests.
Results
Acceptability and feasibility of the intervention
Recruitment
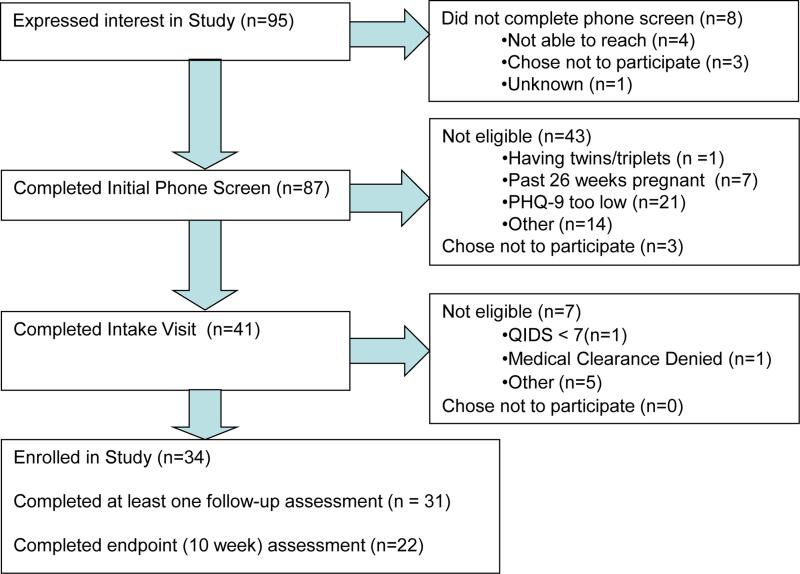
See Figure 1. We recruited 34 participants over a 14-month period. Of 95 women who initially called, only 6 chose not to participate after hearing the study description. Ultimately one third of women who called about the study were enrolled.
Figure 1.
Flow Chart of Participants in Prenatal Yoga Open Trial
Retention
We collected at least partial follow-up assessment data from 31 of the 34 participants; 22 (65%) provided data at specifically at endpoint. Overall, we were able to collect data at approximately 75% of all scheduled data collection timepoints. One woman did not provide follow-up data and did not attend classes because she terminated her pregnancy soon after enrollment.
Number of classes attended
Twenty-nine participants attended one or more classes; 5 did not attend any classes. The mean number of classes attended for those who attended classes was 5.2 (see Table 2) over the 9 weeks they were eligible to attend. As discussed in the Methods, we made protocol changes after the first 25 participants were enrolled. We examined adherence before and after these protocol changes and found that the number of classes attended increased from a mean of 3.8 classes in the initial group of participants (n=25) to a mean of 6.4 classes among the final group of enrolled participants (n=9); t=-1.82, df=32, p<.10.
Table 2.
Indices of acceptability and feasibility
| N | Mean(SD) | Range | |
|---|---|---|---|
| Number of classes attended | 34 | 5.2 (3.7) | 1-16 |
| Average minutes per week practicing yoga in class | 30 | 51.3 (41.6) | 0-182 |
| Average minutes per week practice yoga at home | 30 | 32.7 (55.2) | 0-260 |
| Average minutes per week practicing yoga at home and in class | 30 | 83.9 (75.3) | 0-345 |
| Expectancy (CEQ) prior to beginning classes | 34 | 7.0 (1.1) | 5-9 |
| Credibility (CEQ) prior to beginning classes | 34 | 7.7 (0.9) | 5.3 -9 |
| Satisfaction (CSQ-8) at endpoint | 23 | 29.3 (2.9) | 23-32 |
T p < .10.
Class and home practice
Please see Table 2 for descriptive statistics with regard to amount of yoga practiced. Number of classes attended as assessed by attendance records showed a large correlation with self-report minutes per week in class (r = 0.85, p < .01).
Other mental health treatment
Very few treatment changes were observed. Of the four women in psychotherapy at baseline, three continued during the trial. Another woman started therapy while in the trial. The one participant taking antidepressants at baseline continued on a consistent dose throughout the trial.
Expectancy, credibility, and participant satisfaction
Please see Table 2. Overall, participants expected that prenatal yoga would improve their symptoms, and believed that prenatal yoga was a credible intervention for depression. After taking classes, participants, on average, rated their satisfaction with classes as high.
Injuries due to yoga
At all interim and endpoint assessments, we asked participants if they had experienced any injuries due to participation in yoga classes, or during home yoga practice. No injuries were reported.
Change in depression severity
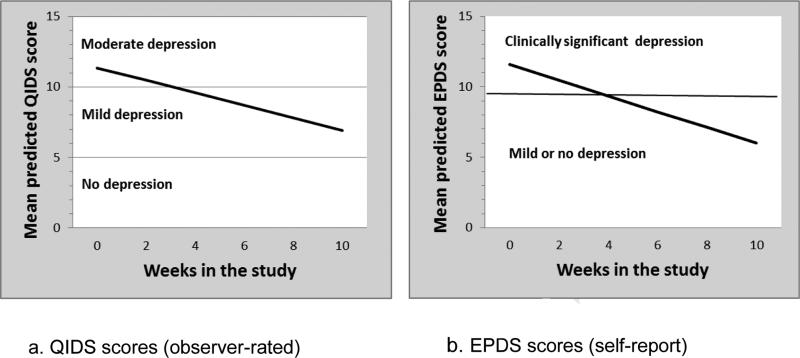
We conducted multilevel models to examine changes in depression symptoms over time. Please see Table 3. Participants experienced significant decreases in depression symptoms over time on both the QIDS and the EPDS. Over 10 weeks, women's symptoms decreased, on average, 4.4 points on the QIDS (1.4 standard deviations) and 5.5 points on the EPDS (1.0 standard deviation), a clinically meaningful reduction. See Figure 2. This degree of change is similar to that seen in more established treatments for antenatal depression (Spinelli & Endicott, 2003), and represents a large effect size (Cohen, 1988).
Table 3.
Multilevel models predicting change in depression severity over time.
| Parameter | Estimate (SE) | 95% CI | t (df) |
|---|---|---|---|
| Outcome = QIDS | |||
| Intercept | 11.34 (0.52) | 10.31, 12.37 | 21.82 (89.4)* |
| Time | −0.44 (0.08) | −0.60, −0.28 | −5.45 (107.7)* |
|
Outcome = EPDS | |||
| Intercept | 11.57 (0.86) | 9.84, 13.31 | 13.42 (48.2)* |
| Time | −0.55 (0.97) | −0.75, −0.36 | −5.69 (97.2)* |
|
Outcome = QIDS (Not including baseline timepoint) | |||
| Intercept | 10.07 (0.90) | 8.29, 11.85 | 11.25 (85.9)* |
| Time | −0.16 (0.11) | −3.67, 0.05 | −1.49 (72.1) |
| Minutes per week in class | −0.010 (.004) | −.0187, −0.001 | −2.22 (74.9)* |
p < 05.
Figure 2.
Change in depression severity over time on the QIDS and EPDS
We examined the association between minutes per week of yoga and depression symptoms in the previous week. As reported in Table 3, we found that more time spent practicing yoga during a given week was significantly associated with lower levels of depression during that week.
Mindfulness
In Table 4, we present correlations between baseline depression and baseline mindfulness. As we expected, higher levels of mindfulness were generally associated with lower levels of depression. Next, we used paired t-tests to assess pre-post changes in aspects of mindfulness. All changes were in the expected direction, and improvements in two aspects of mindfulness (increased awareness, increased non-judgment) reached statistical significance. Effect sizes were in the moderate range (Cohen, 1988).
Table 4.
Change in mindfulness over time on the FFMQ
| Pre-treatment Mean (SD) | Post-treatment Mean (SD) | Paired t-test (df) | Cohen's d | Correlation between baseline mindfulness and depressionc | |
|---|---|---|---|---|---|
| Observe | 22.2 (7.1) a | 24.0 (6.1) a | −1.21 (19) | 0.27 | −0.05 |
| Describe | 26.5 (6.9) b | 27.6 (6.5) b | −1.06 (20) | 0.16 | −0.36* |
| Awareness | 25.8 (5.5) b | 28.8 (6.2) b | −2.84* (20) | 0.51 | −0.42* |
| Nonjudge | 26.2 (7.9) a | 29.9 (5.7) a | −3.71* (19) | 0.54 | −0.44* |
| Nonreact | 20.3 (4.8) b | 22.5 (4.4) b | −1.88 (20) | 0.48 | −0.36* |
n = 20
n = 21
n = 33.
p < 05.
Discussion
This treatment development study sought to evaluate whether prenatal yoga could represent a viable treatment option for antenatal depression. We developed a 10-week prenatal yoga program for depressed women with no prior yoga experience, and tested the intervention in an open pilot trial with 34 women. We found that the intervention was feasible to administer and acceptable to both patients, who voiced high levels of satisfaction, and to prenatal care providers, who welcomed study recruitment and provided medical clearance for appropriate patients. We designed the program to be consistent with prenatal yoga classes offered in the community. Women engaged in the program by attending classes and practicing yoga at home. Classes were gentle in nature and no injuries or safety concerns were reported. Significant reductions in depression severity were observed from pre to post treatment. We also collected data on a potential mechanism of change, mindfulness. We observed that mindfulness was correlated with depression at baseline, and that there were increases in mindfulness over time as women participated in the trial.
These findings contribute to the small but growing literature suggesting that prenatal yoga may be useful as a treatment for antenatal depression. Consistent with findings of Muzik et al., we showed that a standard length (i.e., 75-90 minute) prenatal yoga class may be acceptable to women with elevated depression, and that mindfulness increases over the course of a prenatal yoga intervention. Also like Muzik, we did not observe any adverse events due to prenatal yoga practice. Because the present study utilized a rigorous assessment strategy including diagnostic assessment at baseline as well as repeated administration of a standard, interview-based measure of depression severity as the outcome - and because the majority of our sample had a current major depressive episode - our findings extend previous research by indicating that standard prenatal yoga classes may be effective in reducing depressive symptoms, even among women experiencing a current major depressive episode. Further, this is the first study to demonstrate that amount of yoga practice (i.e., number of minutes practicing prenatal yoga each week) was significantly associated with women's depressive severity that week.
This study was intended to develop and evaluate the content and format of the prenatal yoga program so that the intervention could be evaluated in a subsequent, well-powered RCT. While the design was ideal for assessing feasibility, acceptability, and safety of the program, the current trial did not have the design necessary to definitively evaluate the efficacy of prenatal yoga in reducing depression. Without randomization to a prenatal yoga condition vs. a comparison condition, we cannot be certain that observed reductions in depression were attributable to prenatal yoga practice. Another limitation includes the small number of women enrolled after procedural changes were made to help increase attendance rates. Because we employed several protocol changes to increase attendance, including small financial incentives, we do not know if increased attendance rates would have occurred without financial incentives. Finally, the sample size prohibited examination of differences in outcomes by demographic or clinical subgroup.
Future Research
Several studies now suggest that prenatal yoga may be a viable treatment for antenatal depression, likely to be safe, feasible to administer, and acceptable to women and providers. However, critical questions remain. In addition to a well-designed, fully powered RCT to evaluate efficacy, future studies should examine potential mechanisms of action. Mechanisms may be conceptualized on the biologic level (e.g., decreased sympathetic nervous system arousal) or on the psychological level (e.g., increased mindfulness/ non-judgment).
In addition, future studies should include longitudinal designs, and evaluate not only maternal outcomes, but also associated pregnancy and infant outcomes. Prior studies with healthy, non-depressed samples suggest that yoga may improve overall maternal health and wellbeing, as it is associated with lower lumbo-pelvic pain (Martins & Pinto, 2013), better quality of life (Rakhshani, Maharana, Raghuram, Nagendra, & Venkatram, 2010), lower stress (Satyapriya, Nagendra, Nagarathna, & Padmalatha, 2009), and decreased delivery pain (Chuntharapat, Petpichetchian, & Hatthakit, 2008). Further, women with high risk pregnancies who practiced yoga are less likely to develop pregnancy-induced hypertension or pre-eclampsia (Jayashree et al., 2013), and had fewer preterm births (Rakhshani et al., 2012). However, no studies to date have evaluated pregnancy and birth outcomes among depressed women practicing yoga.
While our data provide some indication that prenatal yoga may be acceptable to women across a range of racial/ ethnic sub-groups, future research with larger and more diverse samples will be important to examine this question more carefully.
Implementation challenges
Pregnant women have unique concerns in accessing depression treatment, and often face barriers to care (Goodman, 2009). Although prenatal yoga may represent a more acceptable option for many women, logistical issues may still limit access. For example, although prenatal yoga is increasingly popular (Wang et al., 2005), not all communities offer it. Even when available, some women may have difficulty attending classes at times offered. Prenatal yoga DVDs may increase access, yet relying on home practice alone may be challenging for depressed women who experience lower levels of motivation and energy. Should future research demonstrate efficacy of prenatal yoga for depression, greater efforts should be made to minimize barriers for pregnant women. This may include making prenatal yoga available onsite at OB/Gyn clinics, establishing yoga programs reimbursable by insurance policies, and providing childcare. In the current study, we found that increasing emphasis on adherence and providing small incentives for regular adherence increased number of classes attended. Though provision of financial incentives may not always be feasible, use of such incentives has been built in to “real world” wellness programs offered by some employers and insurers.
Implications for Practice and/ or Policy
In light of the high cost to women, families, and society of not treating antenatal depression, more resources should be devoted to testing novel interventions that may have broader reach than current depression treatment options. Prenatal yoga is particularly promising because the current results, and the burgeoning literature, suggest prenatal yoga may lead to improvements in depression and also bring about a wider range of health benefits.
Further, emerging data suggest that pregnant women are interested in trying alternative treatment approaches. As findings support new approaches to care, insurers and policy-makers must consider making non-traditional treatments with demonstrated efficacy eligible for insurance payment. This will ensure that these therapies are available to groups likely to experience the greatest health disparities, such as low income and racial minority women (Segre, Losch, & O'Hara, 2006) (Shankardass et al., 2014).
Highlights.
We evaluated feasibility of prenatal yoga as a treatment for antenatal depression.
34 depressed pregnant women were enrolled in a 10-week open trial of prenatal yoga.
Findings suggested that the yoga intervention was feasible, acceptable, and safe.
In addition, women had significant reductions in depressive symptoms.
These data provide initial support for prenatal yoga as a viable treatment option.
Acknowledgments
Funding Source
NIH/ NIMH Grant no. R34 MH085053
Biography
Cynthia L. Battle is a clinical psychologist and Associate Professor (Research) of Psychiatry & Human Behavior at Alpert Medical School of Brown University. Her research is focused on women's perinatal mental health, including development of novel behavioral intervention approaches.
Lisa A. Uebelacker, a clinical psychologist, is Associate Professor (Research) of Psychiatry & Human Behavior and Family Medicine at Brown University's Alpert Medical School. Her research interests include innovative behavioral interventions for depression and integration of behavioral interventions into primary care.
Susanna R. Magee, a board-certified family physician, is Director of the Maternal-Child Health Program at Memorial Hospital of Rhode Island, and Assistant Professor in the Department of Family Medicine at Alpert Medical School of Brown University.
Kaeli Sutton is a registered yoga teacher who has extensive training and experience with prenatal and postpartum yoga. She is founder and Co-Director of the Motion Center, a yoga center in Providence, Rhode Island that specializes in classes for perinatal women.
Ivan Miller is a clinical psychologist and Professor of Psychiatry & Human Behavior at Alpert Medical School of Brown University. His research involves the development and evaluation of interventions for depression and suicidal behavior.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Baer RA, Smith GT, Hopkins J, Krietemeyer J, Toney L. Using self-report assessment methods to explore facets of mindfulness. Assessment. 2006;13:27–45. doi: 10.1177/1073191105283504. [DOI] [PubMed] [Google Scholar]
- Battle CL, Salisbury AL, Schofield CA, Ortiz-Hernandez S. Perinatal antidepressant use: understanding women's preferences and concerns. J Psychiatr Pract. 2013;19(6):443–453. doi: 10.1097/01.pra.0000438183.74359.46. doi: 10.1097/01.pra.0000438183.74359.46 00131746-201311000-00002 [pii] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Battle CL, Uebelacker LA, Howard M, Castaneda M. Prenatal yoga and depression during pregnancy. Birth. 2010;37(4):353–354. doi: 10.1111/j.1523-536X.2010.00435_1.x. doi: 10.1111/j.1523-536X.2010.00435_1.x. [DOI] [PubMed] [Google Scholar]
- Battle CL, Uebelacker LA, Magee SR. Patient-centered care for antenatal depression. Am J Obstet Gynecol. 2012;207(5):e10–11. doi: 10.1016/j.ajog.2012.06.062. author reply e11. doi: 10.1016/j.ajog.2012.06.062 S0002-9378(12)00716-8 [pii] [DOI] [PubMed] [Google Scholar]
- Beebe B, Jaffe J, Buck L, Chen H, Cohen P, Feldstein S, Andrews H. Six-week postpartum maternal depressive symptoms and 4-month mother-infant self and interactive contingency. Infant Mental Health Journal. 2008;29(4):442–471. doi: 10.1002/imhj.20191. [DOI] [PubMed] [Google Scholar]
- Chaudron LH. Complex challenges in treating depression during pregnancy. Am J Psychiatry. 2013;170(1):12–20. doi: 10.1176/appi.ajp.2012.12040440. doi: 10.1176/appi.ajp.2012.12040440 1555607 [pii] [DOI] [PubMed] [Google Scholar]
- Chuntharapat S, Petpichetchian W, Hatthakit U. Yoga during pregnancy: effects on maternal comfort, labor pain and birth outcomes. Complementary Therapies in Clinical Practice. 2008;14:105–115. doi: 10.1016/j.ctcp.2007.12.007. [DOI] [PubMed] [Google Scholar]
- Cohen J. Statistical power analysis for the behavioral sciences. 2nd ed. Lawrence Erlbaum Associates; Hillsdale, NJ: 1988. [Google Scholar]
- Cox JL, Holden JM, Sagovsky R. Detection of postnatal depression: Development of the Edinburgh Postnatal Depression Scale. British Journal of Psychiatry. 1987;((150):782–786. doi: 10.1192/bjp.150.6.782. [DOI] [PubMed] [Google Scholar]
- Craig CL, Marshall AL, Sjostrom M, Bauman AE, Booth ML, Ainsworth BE, Oja P. International physical activity questionnaire: 12-country reliability and validity. Med Sci Sports Exerc. 2003;35(8):1381–1395. doi: 10.1249/01.MSS.0000078924.61453.FB. doi: 10.1249/01.MSS.0000078924.61453.FB. [DOI] [PubMed] [Google Scholar]
- Cripe SM, Frederick IO, Qiu C, Williams MA. Risk of preterm delivery and hypertensive disorders of pregnancy in relation to maternal co-morbid mood and migraine disorders during pregnancy. Paediatr Perinat Epidemiol. 2011;25(2):116–123. doi: 10.1111/j.1365-3016.2010.01182.x. doi: 10.1111/j.1365-3016.2010.01182.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Curtis K, Weinrib A, Katz J. Systematic review of yoga for pregnant women: current status and future directions. Evid Based Complement Alternat Med. 2012;2012:715942. doi: 10.1155/2012/715942. doi: 10.1155/2012/715942. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davalos D, Yadon CA, Tregellas HC. Untreated prenatal maternal depression and the potential risks to offspring; A review. Arch Women's Mental Health. 2012;15:1–14. doi: 10.1007/s00737-011-0251-1. [DOI] [PubMed] [Google Scholar]
- Devilly GJ, Borkovec TD. Psychometric properties of the credibility/expectancy questionnaire. Journal of Behavior Therapy and Experimental Psychiatry. 2000;31:73–86. doi: 10.1016/s0005-7916(00)00012-4. [DOI] [PubMed] [Google Scholar]
- Field T, Diego M, Delgado J, Medina L. Yoga and social support reduce prenatal depression, anxiety and cortisol. J Bodyw Mov Ther. 2013;17(4):397–403. doi: 10.1016/j.jbmt.2013.03.010. doi: 10.1016/j.jbmt.2013.03.010 S1360-8592(13)00059-4 [pii] [DOI] [PubMed] [Google Scholar]
- Field T, Diego M, Hernandez-Reif M, Medina L, Delgado J, Hernandez A. Yoga and massage therapy reduce prenatal depression and prematurity. J Bodyw Mov Ther. 2012;16(2):204–209. doi: 10.1016/j.jbmt.2011.08.002. doi: 10.1016/j.jbmt.2011.08.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- First MB, Spitzer RL, Gibbon M, Williams JBW. Structured clinical interview for DSM-IV-TR Axis I disorders, Research version, Patient edition with Psychotic Screen (SCID-I/P W/ PSY SCREEN) Biometrics Research, New York State Psychiatric Institute; New York: 2001. [Google Scholar]
- Flynn HA, Blow FC, Marcus SM. Rates and predictors of depression treatment among pregnant women in hospital-affiliated obstetrics practices. Gen Hosp Psychiatry. 2006;(28):289–295. doi: 10.1016/j.genhosppsych.2006.04.002. [DOI] [PubMed] [Google Scholar]
- Freeman MP. Antidepressant medications treatment during pregnancy: prevalence of use, clinical implications, and alternatives. J Clin Psychiatry. 2011;72:7. doi: 10.4088/JCP.11f07206. [DOI] [PubMed] [Google Scholar]
- Gavin NI, Gaynes BN, Lohr KN, Meltzer-Brody S, Gartlehner G, Swinson T. Perinatal depression: Systemmatic review of prevalence and incidence. Obstetrics and Gynecology. 2005;106(5):1071–1083. doi: 10.1097/01.AOG.0000183597.31630.db. [DOI] [PubMed] [Google Scholar]
- Goodman JH. Women's Attitudes, Preferences, and Perceived Barriers to Treatment for Perinatal Depression. Birth: Issues in Perinatal Care. 2009;36:60–69. doi: 10.1111/j.1523-536X.2008.00296.x. [DOI] [PubMed] [Google Scholar]
- Grigoriadis S, VonderPorten EH, Mamisashvili L, Tomlinson G, Dennis CL, Koren G, Ross LE. The impact of maternal depression during pregnancy on perinatal outcomes: a systematic review and meta-analysis. J Clin Psychiatry. 2013;74(4):e321–341. doi: 10.4088/JCP.12r07968. doi: 10.4088/JCP.12r07968. [DOI] [PubMed] [Google Scholar]
- Grote NK, Bridge JA, Gavin AR, Melville JL, Iyengar S, Katon WJ. A meta-analysis of depression during pregnancy and the risk of preterm birth, low birth weight, and intrauterine growth restriction. Arch Gen Psychiatry. 2010;67(10):1012–1024. doi: 10.1001/archgenpsychiatry.2010.111. doi: 10.1001/archgenpsychiatry.2010.111 67/10/1012 [pii] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jayashree R, Malini A, Rakhshani A, Nagendra H, Gunasheela S, Nagarathna R. Effect of the integrated approach of yoga therapy on platelet count and uric acid in pregnancy: A multicenter stratified randomized single-blind study. Int J Yoga. 2013;6(1):39–46. doi: 10.4103/0973-6131.105945. doi: 10.4103/0973-6131.105945. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jeffery RW, Wing RR, Thorson C, Burton LR. Use of personal trainers and financial incentives to increase exercise in a behavioral weight-loss program. J Consult Clin Psychol. 1998;66(5):777–783. doi: 10.1037//0022-006x.66.5.777. [DOI] [PubMed] [Google Scholar]
- Kim JJ, La Porte LM, Corcoran M, Magasi S, Batza J, Silver RK. Barriers to mental health treatment among obstetric patients at risk for depression. Am J Obstet Gynecol. 2010;202(3):312, e311–315. doi: 10.1016/j.ajog.2010.01.004. doi: 10.1016/j.ajog.2010.01.004 S0002-9378(10)00005-0 [pii] [DOI] [PubMed] [Google Scholar]
- Kroenke K, Spitzer RL, Williams JBW. The PHQ-9: Validity of a brief depression severity measure. J Gen Intern Med. 2001;16:606–613. doi: 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Larsen DL, Attkisson CC, Hargreaves WA, et al. Assessment of client/ patient satisfaction: development of a general scale. Evaluation and Program Planning. 1979;2:197–207. doi: 10.1016/0149-7189(79)90094-6. [DOI] [PubMed] [Google Scholar]
- Martins RF, Pinto ESJL. Treatment of Pregnancy-Related Lumbar and Pelvic Girdle Pain by the Yoga Method: A Randomized Controlled Study. J Altern Complement Med. 2013 doi: 10.1089/acm.2012.0715. doi: 10.1089/acm.2012.0715. [DOI] [PubMed] [Google Scholar]
- Murray LC, P.J., Wilson A, Romaniuk H. Controlled trial of the short- and long-term effect of psychological treatment of postpartum depression. 2. Impact on the mother-child relationship and child outcome. Br J Psychiatry. 2003;182:420–427. [PubMed] [Google Scholar]
- Muzik M, Hamilton SE, Lisa Rosenblum K, Waxler E, Hadi Z. Mindfulness yoga during pregnancy for psychiatrically at-risk women: preliminary results from a pilot feasibility study. Complement Ther Clin Pract. 2012;18(4):235–240. doi: 10.1016/j.ctcp.2012.06.006. doi: 10.1016/j.ctcp.2012.06.006 S1744-3881(12)00048-5 [pii] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nguyen TD, Attkisson CC, Stegner BL. Assessment of patient satisfaction: development and refinement of a service evaluation questionnaire. Evaluation and Program Planning. 1983;6:299–313. doi: 10.1016/0149-7189(83)90010-1. [DOI] [PubMed] [Google Scholar]
- O'Mahen HAF, H.A. Preferences and Perceived Barriers to Treatment for Depression during the Perinatal Period. Journal of Women's Health. 2008;17(8):1301–1309. doi: 10.1089/jwh.2007.0631. [DOI] [PubMed] [Google Scholar]
- Palladino CL, Flynn HA, Richardson C, Marcus SM, Johnson TR, Davis MM. Lengthened predelivery stay and antepartum complications in women with depressive symptoms during pregnancy. J Womens Health (Larchmt) 2011;20(6):953–962. doi: 10.1089/jwh.2010.2380. doi: 10.1089/jwh.2010.2380. [DOI] [PubMed] [Google Scholar]
- Posternak MA, Young D, Sheeran T, Chelminski I, Franklin CL, Zimmerman M. Assessing past treatment history: test-retest reliability of the Treatment Response to Antidepressant Questionnaire. J Nerv Ment Dis. 2004;192(2):95–102. doi: 10.1097/01.nmd.0000110280.19284.47. [DOI] [PubMed] [Google Scholar]
- Rakhshani A, Maharana S, Raghuram N, Nagendra HR, Venkatram P. Effects of integrated yoga on quality of life and interpersonal relationship of pregnant women. Qual Life Res. 2010;19(10):1447–1455. doi: 10.1007/s11136-010-9709-2. doi: 10.1007/s11136-010-9709-2. [DOI] [PubMed] [Google Scholar]
- Rakhshani A, Nagarathna R, Mhaskar R, Mhaskar A, Thomas A, Gunasheela S. The effects of yoga in prevention of pregnancy complications in high-risk pregnancies: a randomized controlled trial. Prev Med. 2012;55(4):333–340. doi: 10.1016/j.ypmed.2012.07.020. doi: 10.1016/j.ypmed.2012.07.020. [DOI] [PubMed] [Google Scholar]
- Rush AJ, Bernstein IH, Trivedi MH, Carmody TJ, Wisniewski S, Mundt JC, Fava M. An Evaluation of the Quick Inventory of DepressiveSymptomatology and the Hamilton Rating Scale for Depression: A Sequenced Treatment Alternatives to Relieve Depression Trial Report. Biol Psychiatry. 2005 doi: 10.1016/j.biopsych.2005.08.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rush AJ, Trivedi MH, Ibrahim HM, Carmody TJ, Arnow B, Klein DN, Keller M. The 16-item Quick Inventory of Depressive Symptomatology (QIDS) Clinician Rating (QIDS-C) and Self-Report (QIDS-SR): a psychometric evaluation in patients with chronic major depression. Biol Psychiatry. 2003;54:573–583. doi: 10.1016/s0006-3223(02)01866-8. [DOI] [PubMed] [Google Scholar]
- Satyapriya M, Nagendra HR, Nagarathna R, Padmalatha V. Effect of integrated yoga on stress and heart rate variability in pregnant women. Int J Gynaecol Obstet. 2009;104(3):218–222. doi: 10.1016/j.ijgo.2008.11.013. doi: 10.1016/j.ijgo.2008.11.013. [DOI] [PubMed] [Google Scholar]
- Segre LS, Losch ME, O'Hara MW. Race/ethnicity and perinatal depressed mood. Journal of Reproductive and Infant Psychology. 2006;24(2):99–106. doi: Doi 10.1080/02646830600643908. [Google Scholar]
- Shankardass K, O'Campo P, Dodds L, Fahey J, Joseph K, Morinis J, Allen VM. Magnitude of income-related disparities in adverse perinatal outcomes. BMC Pregnancy Childbirth. 2014;14:96. doi: 10.1186/1471-2393-14-96. doi: 10.1186/1471-2393-14-961471-2393-14-96 [pii] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sherman KJ. Guidelines for developing yoga interventions for randomized trials. Evid Based Complement Alternat Med. 2012;2012:143271. doi: 10.1155/2012/143271. doi: 10.1155/2012/143271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sockol LE, Epperson CN, Barber JP. A meta-analysis of treatments for perinatal depression. Clin Psychol Rev. 2011;31(5):839–849. doi: 10.1016/j.cpr.2011.03.009. doi: 10.1016/j.cpr.2011.03.009 S0272-7358(11)00057-2 [pii] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spinelli MG, Endicott J. Controlled clinical trial of interpersonal psychotherapy versus parenting education program for depressed pregnant women. Am J Psychiatry. 2003;160(3):555–562. doi: 10.1176/appi.ajp.160.3.555. [DOI] [PubMed] [Google Scholar]
- Sugiura-Ogasawara M, Furukawa TA, Nakano Y, Hori S, Aoki K, Kitamura T. Depression as a potential causal factor in subsequent miscarriage in recurrent spontaneous aborters. Hum Reprod. 2002;17(10):2580–2584. doi: 10.1093/humrep/17.10.2580. [DOI] [PubMed] [Google Scholar]
- Trivedi MH, Rush AJ, Ibrahim HM, Carmody TJ, Biggs MM, Suppes T, Kashner TM. The Inventory of Depressive Symptomatology, Clinician Rating (IDS-C) and Self-Report (IDS-SR), and the Quick Inventory of Depressive Symptomatology, Clinician Rating (QIDS-C) and Self-Report (QIDS-SR) in public sector patients with mood disorders: a psychometric evaluation. Psychol Med. 2004;34(1):73–82. doi: 10.1017/s0033291703001107. [DOI] [PubMed] [Google Scholar]
- Uebelacker LA, Epstein-Lubow G, Gaudiano BA, Tremont G, Battle CL, Miller IW. Hatha yoga for depression: critical review of the evidence for efficacy, plausible mechanisms of action, and directions for future research. J Psychiatr Pract. 2010;16(1):22–33. doi: 10.1097/01.pra.0000367775.88388.96. doi: 10.1097/01.pra.0000367775.88388.9600131746-201001000-00004 [pii] [DOI] [PubMed] [Google Scholar]
- Wang S, DeZinno P, Fermo L, William K, Caldwell-Andrews AA, Bravemen F, Kain ZN. Complementary and alternative medicine for low-back pain in pregnancy: a cross-sectional survey. Journal of Alternative and Complementary Medicine. 2005;11:459–464. doi: 10.1089/acm.2005.11.459. [DOI] [PubMed] [Google Scholar]