Abstract
AIM: To investigate the inhibitory effects of emodin, baicalin, etc. on the hefA gene of multidrug resistance (MDR) in Helicobacter pylori (H. pylori).
METHODS: The double dilution method was used to screen MDR H. pylori strains and determine the minimum inhibitory concentrations (MICs) of emodin, baicalin, schizandrin, berberine, clarithromycin, metronidazole, tetracycline, amoxicillin and levofloxacin against H. pylori strains. After the screened MDR stains were treated with emodin, baicalin, schizandrin or berberine at a 1/2 MIC concentration for 48 h, changes in MICs of amoxicillin, tetracycline, levofloxacin, metronidazole and clarithromycin were determined. MDR strains with reduced MICs of amoxicillin were selected to detect the hefA mRNA expression by real-time quantitative PCR.
RESULTS: A total of four MDR H. pylori strains were screened. Treatment with emodin, baicalin, schizandrin and berberine significantly decreased the MICs of amoxicillin and tetracycline against some strains, decreased by 1 to 2 times, but did not significantly change the MICs of clarithromycin, levofloxacin, and metronidazole against MDR strains. In the majority of strains with reduced MICs of amoxicillin, hefA mRNA expression was decreased; one-way ANOVA (SPSS 12.0) used for comparative analysis, P < 0.05.
CONCLUSION: Emodin, baicalin, schizandrin and berberine significantly decreased the MICs of amoxicillin and tetracycline against some H. pylori strains, possibly by mechanisms associated with decreasing hefA mRNA expression.
Keywords: Traditional Chinese medicine, Multidrug resistance, Helicobacter pylori, Efflux pump, hefA
Core tip: Clinical signs of Helicobacter pylori (H. pylori)-induced drug resistance have become more and more prevalent, thus resulting in reduced cure rates. In this study, we used herbal extracts, such as berberine, to inhibit multidrug resistance in H. pylori. The results indicated that the minimum inhibitory concentration of amoxicillin and tetracycline was lowered after the intervention; the regulatory mechanism was related to down-regulation of efflux pump hefA mRNA expression. This suggests a novel strategy for prophylaxis and treatment of H. pylori-induced resistance.
INTRODUCTION
Helicobacter pylori (H. pylori) is the pathogen of multiple digestive system diseases including chronic active gastritis and peptic ulcer, and has been categorized as a class I carcinogen by the World Health Organization[1,2]. Globally, the rate of H. pylori infection is as high as 50%[3-5], and it is even higher in developing countries. In China, the rate of H. pylori infection is 60%-90%[6,7]. Studies have found that 15% of clinical isolates of H. pylori develop multiple drug resistance (MDR; resistance to three or more antibiotics)[8-11], and this causes a decline in H. pylori eradication rate, posing a serious threat to human health. Therefore, the mechanism of MDR of H. pylori has become a hot research topic. Bacterial efflux pumps play an important role in the development of MDR. Liu et al[12] found that high expression of the hefA gene, which encodes a member of the active efflux system, resulted in the development of MDR in H. pylori. Zhang et al[13] artificially induced MDR and, for the first time, found that efflux pump inhibitors could partially reverse MDR. Studies have shown that traditional Chinese medicines emodin and baicalin have an obvious inhibitory effect on H. pylori[14-17]. The present study investigated the possible inhibitory effect of emodin, baicalin, schizandrin and berberine on MDR of H. pylori strains and the relationship between efflux pump hefA mRNA expression and reduced minimum inhibitory concentrations (MICs) of antibiotics, with an aim to explore the effect of Chinese herbs on H. pylori efflux pumps and to provide a theoretical basis for reversing MDR.
MATERIALS AND METHODS
Materials
H. pylori strains were obtained from the Department of Gastroenterology, Affiliated Hospital of Youjiang Medical University for Nationalities. For isolating H. pylori strains, gastric mucosal specimens were collected, ground, inoculated on Columbia blood agar plates containing 5% fresh rabbit blood, and cultured at 37 °C under micro-aerobic conditions (850 mL/L N2, 100 mL/L CO2, 50 mL/L O2) in > 98% relative humidity for 3 to 5 d. The isolated strains were confirmed as H. pylori by biochemical tests (urease, catalase, oxidase), hematoxylin and eosin staining, and morphological analysis. Antibiotics used in this study included: amoxicillin (Lot No. 10807; Sichuan Pharmaceutical, Inc., China), clarithromycin (Lot No. 111202; Harbin Pharmaceutical Group Sixth Pharm Factory, China), levofloxacin (Lot No. 120120, Xinchang Pharmaceutical Factory of Zhejiang Pharmaceutical Co., LTD., China), tetracycline (Lot No. 20110902, Guangdong Taicheng Pharmaceutical Co., LTD., China), and metronidazole (Lot No.10091544, Zhejiang Jimin Pharmaceutical Co., LTD., China). Emodin (Lot No. 120908; purity, 98%), berberine (Lot No. 120810; purity, 97%), schizandrin (Lot No. 120908; purity, 98%), and baicalin (Lot No. 120908; purity, 90%) were purchased from Shaanxi Angsheng Biological Technology Co., LTD (China). Other reagents or kits used included Trizol reagent kit (Shanghai Invitrogen, China); RevertAid First Strand cDNA Synthesis Kit and DNase I (Fermentas); 2 × SYBRGreen quantitative PCR (qPCR) Mix (Beijing Zhuangment Co., LTD, China). PCR primers were designed based on the H. pylori hefABC gene sequences deposited in GenBank. Through sequence homology analysis, the primers were selected in the conserved region. 16S rRNA was used as an internal control. The primers were synthesized by Shanghai Sangon Biotech (China).
Screening of MDR strains
The double dilution method was used to determine the MICs of emodin, baicalin, schizandrin, berberine, clarithromycin, metronidazole, tetracycline, amoxicillin and levofloxacin against H. pylori strains. According to the Clinical and Laboratory Standards Institute (NCCLS) criteria, H. pylori strains that could grow in medium containing three or more of amoxicillin (≥ 4 μg/mL), levofloxacin (≥ 8 μg/mL), clarithromycin (≥ 1 μg/mL), metronidazole (≥ 8 μg/mL), and tetracycline (≥ 4 μg/mL) were identified as MDR strains.
Determination of antibiotic susceptibility of MDR strains before and after treatment with traditional Chinese medicines
Based on the method described previously[18], the MICs of the traditional Chinese medicines against MDR strains were calculated, and the next concentration below MIC was 1/2 MIC. The screened MDR stains were treated with emodin, baicalin, schizandrin or berberine at a 1/2 MIC concentration for 48 h to determine their effect on the MICs of amoxicillin, tetracycline, levofloxacin, metronidazole and clarithromycin. A positive control (10 mg/mL pantoprazole) and a negative control (culture medium) were also run at the same time.
Reverse transcription-PCR for detection of hefA mRNA expression in MDR strains with reduced MICs of amoxicillin
MDR strains with reduced MICs of amoxicillin after treatment with emodin, baicalin, schizandrin and berberine at a 1/2 MIC concentration were screened, and total RNA was prepared with Trizol reagent according to the manufacturer’s instructions. Reverse transcription was then performed in a 20-μL system containing 5 μL total RNA, 1 μL random primer p(dN)6 (0.2 μg/μL), 5 μL RNase-free ddH2O, 4.0 μL, 5 × reaction buffer, 2.0 μL dNTP mix (10 mmol/L), 1.0 μL Rnase inhibitor (20 U/μL) and 2.0 μL AMV reverse transcriptase (10 U/μL). The reaction parameters were 37 °C for 5 min, 42 °C for 60 min, and 70 °C for 10 min. PCR was then performed in a 20-μL system containing 10 μL SybrGreen qPCR Master Mix, 1 μL forward primer (10 μmol/L), 1 μL reverse primer (10 μmol/L), 7 μL ddH20, and 1 μL template (cDNA; 1:6 dilution). Cycling parameters were pre-denaturation at 95 °C for 2 min, and 40 cycles of denaturation at 95 °C for 10 s and annealing at 60 °C for 40 s.
Statistical analysis
Statistical analyses were performed using SPSS12.0. The differences in hefA mRNA expression were compared using analysis of variance (ANOVA) and Tukey tests.
RESULTS
Screening of MDR strains
A total of four MDR strains were screened, of which two were resistant to amoxicillin, clarithromycin, levofloxacin, tetracycline, and metronidazole, one was resistant to amoxicillin, clarithromycin, tetracycline, and metronidazole, and one was resistant to amoxicillin, levofloxacin, tetracycline, and metronidazole. These MDR strains are shown in Table 1.
Table 1.
Resistance of multidrug resistance strains to the five antibiotics
| No. | Levofloxacin | Amoxicillin | Clarithromycin | Tetracycline | Metronidazole |
| 23 | R | R | R | R | R |
| 40 | R | R | R | R | R |
| 41 | S | R | R | R | R |
| 42 | R | R | I | R | R |
R: Resistant; S: Sensitive; I: Intermediate.
MICs of the four traditional Chinese medicines against MDR strains
The MICs of emodin, baicalin, schizandrin and berberine against MDR strains are shown in Table 2.
Table 2.
Minimum inhibitory concentrations of the four Chinese medicines against multidrug resistance strains (mg/mL)
| No. | Emodin | Berberine | Berberine | Schizandrin |
| 23 | 12.5 | 50 | 200 | 50 |
| 40 | 12.5 | 100 | 100 | 100 |
| 41 | 12.5 | 100 | 100 | 100 |
| 42 | 12.5 | 25 | 100 | 50 |
Changes in MICs of the determined antibiotics against MDR strains after treatment with the four traditional Chinese medicines
After the four MDR strains were treated with emodin, baicalin, schizandrin and berberine at a 1/2 MIC concentration or pantoprazole, the MICs of amoxicillin and tetracycline against some strains were decreased compared with before treatment or the negative control group. Compared with 10 mg/mL pantoprazole, the effects of the traditional Chinese medicines were comparable or superior (Tables 3 and 4). However, the MICs of clarithromycin, levofloxacin, and metronidazole against MDR strains showed no significant changes (Tables 5, 6 and 7).
Table 3.
Minimum inhibitory concentrations of amoxicillin against the four multidrug resistance strains after treatment with the four traditional Chinese medicines (μg/mL)
| No. | Emodin | Berberine | Berberine | Schizandrin | Pantoprazole | NC |
| 23 | 32 | 16 | 64 | 32 | 32 | 64 |
| 40 | 16 | 8 | 16 | 16 | 16 | 32 |
| 41 | 64 | 64 | 21 | 64 | 32 | 64 |
| 42 | 32 | 16 | 32 | 32 | 32 | 32 |
Pantoprazole was used as a positive control, and culture medium was used as a negative control. NC: Negative control.
Table 4.
Minimum inhibitory concentrations of tetracycline against the four multidrug resistance strains after treatment with the four traditional Chinese medicines (μg/mL)
| No. | Emodin | Berberine | Berberine | Schizandrin | Pantoprazole | NC |
| 23 | 64 | 32 | 64 | 64 | 32 | 64 |
| 40 | 16 | 16 | 32 | 32 | 32 | 32 |
| 41 | 32 | 32 | 32 | 64 | 16 | 32 |
| 42 | 32 | 16 | 32 | 32 | 32 | 32 |
NC: Negative control.
Table 5.
Minimum inhibitory concentrations of metronidazole against the four multidrug resistance strains after treatment with the four traditional Chinese medicines (μg/mL)
| No. | Emodin | Berberine | Berberine | Schizandrin | Pantoprazole | NC |
| 23 | 128 | 128 | 128 | 128 | 64 | 128 |
| 40 | 64 | 64 | 64 | 64 | 32 | 64 |
| 41 | 64 | 64 | 64 | 64 | 32 | 64 |
| 42 | 64 | 64 | 64 | 64 | 64 | 64 |
NC: Negative control.
Table 6.
Minimum inhibitory concentrations of clarithromycin against the four multidrug resistance strains after treatment with the four traditional Chinese medicines (μg/mL)
| No. | Emodin | Berberine | Berberine | Schizandrin | Pantoprazole | NC |
| 23 | 64 | 64 | 64 | 64 | 32 | 64 |
| 40 | 32 | 32 | 32 | 32 | 16 | 32 |
| 41 | 32 | 32 | 32 | 32 | 16 | 32 |
| 42 | 32 | 32 | 32 | 32 | 32 | 32 |
NC: Negative control.
Table 7.
Minimum inhibitory concentrations of levofloxacin against the four multidrug resistance strains after treatment with the four traditional Chinese medicines (μg/mL)
| No. | Emodin | Berberine | Berberine | Schizandrin | Pantoprazole | NC |
| 23 | 64 | 64 | 64 | 64 | 32 | 64 |
| 40 | 32 | 32 | 32 | 32 | 16 | 32 |
| 41 | 32 | 32 | 32 | 32 | 16 | 32 |
| 42 | 64 | 64 | 64 | 64 | 64 | 64 |
NC: Negative control.
Expression of hefA mRNA in MDR strains with significantly changed MICs of amoxicillin
Sixteen sub-cultured strains with significantly reduced MICs of amoxicillin after treatment with emodin, baicalin, schizandrin, berberine or pantoprazole (Table 3) were selected and used to detect the hefA mRNA expression by reverse transcription-PCR. After No. 23 MDR strain was treated with emodin, schizandrin or berberine, both MICs of amoxicillin and hefA mRNA expression were decreased. After No. 40 MDR strain was treated with emodin, baicalin, schizandrin and berberine, both MICs of amoxicillin and hefA mRNA expression were decreased. For No. 41 MDR strain, treatment with baicalin decreased MIC of amoxicillin but increased hefA mRNA expression. For No. 42 MDR strain, treatment with berberine decreased MIC of amoxicillin but increased hefA mRNA expression, while treatment with pantoprazole did not significantly change MIC of amoxicillin but increased hefA mRNA expression. The amplification curves, melting curves, PCR products and quantitative results for the 16 sub-cultured strains are shown in Figures 1, 2, 3 and Table 8, respectively.
Figure 1.
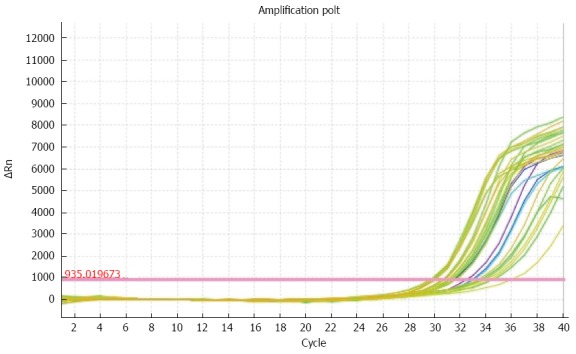
Amplification curves for the hefA gene in 16 sub-cultured strains with significantly changed minimum inhibitory concentration of amoxicillin.
Figure 2.
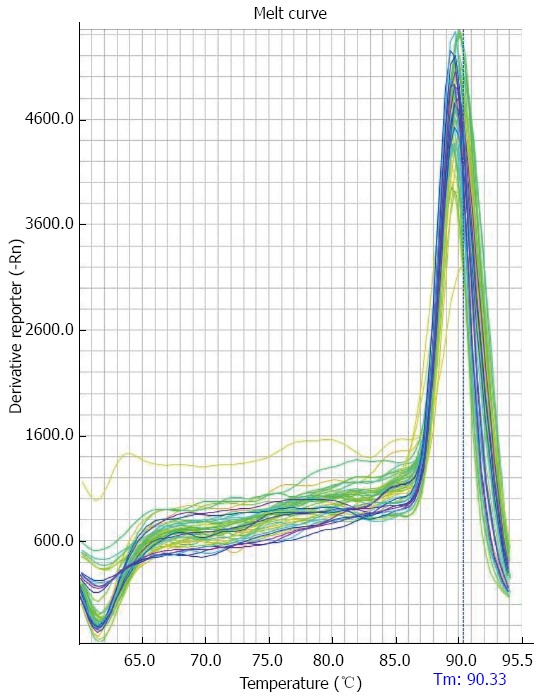
Melting curves for the hefA gene in 16 sub-cultured strains with significantly changed minimum inhibitory concentration of amoxicillin.
Figure 3.
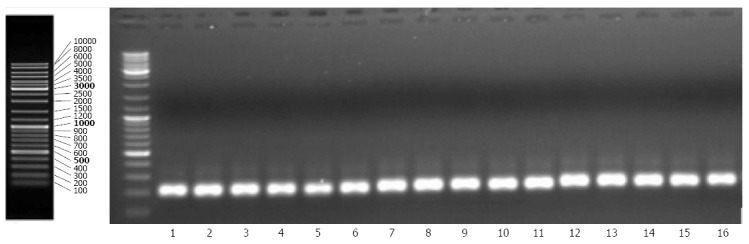
Agarose gel electrophoresis analysis of PCR products for hefA in 16 sub-cultured strains with significantly changed minimum inhibitory concentration of amoxicillin.
Table 8.
Real-time PCR quantitative results for hefA gene expression in 16 sub-cultured strains with significantly changed minimum inhibitory concentration of amoxicillin
| No. | hefA | 16S rRNA | ∆Ct | ∆∆Ct | 2-(∆∆Ct) |
| 1 | 31.0933170 | 14.457372 | 16.63595 | 0 | 1 |
| 2 | 30.2871494 | 15.427569 | 14.85958 | -1.77637 | 3.425620 |
| 3 | 29.8203506 | 16.133926 | 13.68642 | -2.94952 | 7.724926 |
| 4 | 30.2641807 | 16.449774 | 13.81441 | -2.82154 | 7.069158 |
| 5 | 33.8933296 | 15.226003 | 18.66733 | 2.031382 | 0.244621 |
| 6 | 32.0969762 | 15.256840 | 16.84014 | 0.204191 | 0.868025 |
| 7 | 29.9665985 | 15.307595 | 14.65900 | -1.97694 | 3.936578 |
| 8 | 31.2955170 | 14.817378 | 16.47814 | -0.15781 | 1.115590 |
| 9 | 31.6979313 | 14.758531 | 16.93940 | 0.303455 | 0.810309 |
| 10 | 30.7486935 | 14.488201 | 16.26049 | -0.37545 | 1.297247 |
| 11 | 34.3626747 | 18.408577 | 15.95410 | -0.68185 | 1.604193 |
| 12 | 36.2199669 | 18.414414 | 17.80555 | 1.169608 | 0.444542 |
| 13 | 33.9337616 | 17.102884 | 16.83088 | 0.194932 | 0.873614 |
| 14 | 31.4263000 | 14.820235 | 16.60606 | -0.02988 | 1.020928 |
| 15 | 32.9468956 | 14.884178 | 18.06272 | 1.426772 | 0.371962 |
| 16 | 31.6464024 | 15.465043 | 16.18136 | -0.45459 | 1.370390 |
DISCUSSION
In recent years, there have been more and more studies on traditional Chinese medicines. As a result, the mechanisms of action of many traditional Chinese medicines have been gradually elucidated. Heat-clearing and detoxicating Chinese medicines have strong antibacterial effects and are therefore called plant antibiotics; these include Rhizoma coptidis, Radix scutellariae, Andrographis paniculata, rhubarb, and Radix isatidis[17,19-24]. Baicalin is the main effective ingredient of Radix scutellariae, and its bacteriostatic mechanisms include destroying bacterial cell membrane, inhibition of bacterial DNA, RNA and protein biosynthesis, and degradation of endotoxins[25]. Berberine, also called berberine hydrochloride, is the main ingredient of Rhizoma coptidis. It exerts bacteriostatic effects probably by inhibiting bacterial growth and respiration, suppressing the oxidation of glucose and sugar metabolic intermediates, especially deoxidization reactions[26]. Rhubarb consists mainly of anthraquinone compounds including emodin, rhein, and chrysophanol. Emodin has purgative, antibacterial, antitumor and hemostatic effects, and its antibacterial effects are associated with inhibiting bacterial nucleic acid biosynthesis and breathing processes, because it can cause bacterial DNA damage and result in the production of small pieces of DNA[27,28]. However, some studies found that the inhibitory effect of emodin on H. pylori is related to the inhibition of aromatic amine-N-acetyl transferase activity[29]. Berberine, emodin, schizandrin, and baicalin have inhibitory and killing effects against H. pylori, even in drug-resistant strains. Currently, there have been no other reports of the effects of traditional Chinese medicines on MDR and the underlying mechanisms.
The results of the present study, together with our previous findings, showed that berberine, emodin, schizandrin, and baicalin have certain inhibitory and killing effects against MDR H. pylori strains. Additionally, emodin, baicalin, schizandrin or berberine at a 1/2 MIC concentration could reduce the MICs of amoxicillin and tetracycline against some MDR strains. Compared with 10 mg/mL pantoprazole, the effects of the traditional Chinese medicines were comparable or superior; however, they could not reduce the MICs of clarithromycin, levofloxacin, and metronidazole against MDR strains. The possible reasons are: (1) different MDR strains may have different drug resistance patterns, thus resulting in different MICs; (2) different traditional Chinese medicine ingredients have different bacteriostatic effects. Berberine has obvious, relatively stable bacteriostatic effects, while the other three medicines have unobvious, unstable antibacterial effects; and (3) bacterial strains came from different sources and had different growth environments, which may also affect MICs.
While exploring the mechanism by which emodin, baicalin, schizandrin, berberine and pantoprazole reduced the MICs of amoxicillin against MDR strains, we found that both MICs of amoxicillin and hefA mRNA expression were reduced in No. 23 and No. 40 MDR strains, suggesting that hefA mRNA expression may be positively correlated with the effects of emodin, baicalin, schizandrin, berberine and pantoprazole in reducing the MICs of amoxicillin against MDR strains. However, in No. 41 MDR strain, treatment with baicalin decreased the MIC but increased hefA mRNA expression; for No. 42 MDR strain, treatment with berberine decreased the MIC but increased hefA mRNA expression, and treatment with pantoprazole did not significantly change the MIC but increased hefA mRNA expression. On one hand, this may be associated with drug resistance patterns of MDR strains. Both No. 23 and No 40 MDR strains had the same pattern of resistance to levofloxacin, clarithromycin, amoxicillin, tetracycline, and metronidazole, while No. 41 was sensitive to levofloxacin, and No. 42 was moderately sensitive to clarithromycin. On the other hand, the existence of multiple efflux pump gene families may result in the above discrepancy. Since the hefA gene is only one member of one of the five efflux pump families, other members of the five efflux pump families may mediate the MIC reduction.
The present study showed that berberine, baicalin, emodin, and schizandrin all have antibacterial activities against MDR, and can reduce the MICs of amoxicillin and tetracycline, possibly via mechanisms associated with altering hefA gene expression. These findings provide a new idea and new method for solving the problem of increasingly serious MDR. However, it remains to be investigated why these Chinese medicines only reduced the MICs of amoxicillin and tetracycline, and did not alter those of levofloxacin, clarithromycin and metronidazole, and why hefA gene expression was not correlated with MIC reduction in some strains.
COMMENTS
Background
There are different mechanisms of Helicobacter pylori (H. pylori)-induced resistance to various antibiotics, but its multidrug resistance may be closely linked to the activity of efflux pumps. However, there is not yet an accredited method to prevent or reverse multidrug-resistance induced by H. pylori. Our research group has found that herbal extracts (especially emodin) have an effective inhibitory effect on H. pylori-induced multi-drug resistance, and that they reduced the minimum inhibitory concentration (MIC) of some antibiotics. Thus, the authors further explored the molecular mechanism of emodin lowering of antibiotic MIC by assessing the expression of the efflux pump gene hefA.
Research frontiers
The issue of H. pylori-induced drug resistance has become one of the current research directions, and seeking to optimally measure its resistance is an urgent scientific project. Chinese herbal medicine has pronounced characteristics, such as anti-inflammatory, immunomodulatory, anti-tumor roles and it lowers side effects. Therefore, developing some substitutes extracted from Chinese herbals would provide new ideas or methods to solve the drug resistance.
Innovations and breakthroughs
A class of fever-reducing and detoxification herbals generally has antibacterial effects, and some herbals, such as berberine, play an inhibitory role against H. pylori-induced drug resistance; however, its mechanism remains unclear. This study found that berberine had an effective inhibitory effect on H. pylori-induced drug resistance and decreased the MIC of amoxicillin antibiotic, etc. The authors also report that the mechanism may be related to reduction of efflux pump hefA gene expression.
Applications
This study found that berberine has an effective inhibitory effect on H. pylori-induced multi-drug resistance, and lowered the MIC of amoxicillin antibiotic etc. The findings suggest new ideas or methods to solve the drug-resistance induced by H. pylori, thereby aiming to cure this disease.
Terminology
Minimum inhibitory concentration is the lowest antimicrobial concentration that can inhibit the growth of bacteria; Multidrug resistance is a condition enabling disease-causing microorganisms (bacteria, viruses, fungi or parasites) to resist distinct antimicrobials.
Peer-review
The present study revealed that berberine etc. has an effective inhibitory effect on H. pylori-induced multi-drug resistance and lowered the MIC of amoxicillin antibiotic etc.; the mechanism may be related to down-regulation of efflux pump hefA gene expression. The findings demonstrate that use of berberine has a relatively large practical value, and it would provide the scientific theory for developing effective medication against resistance induced by H. pylori.
Footnotes
Supported by Grants from Guangxi Key Discipline Fund (Pathogenic Microbiology), No. [2013]16; Key Laboratory Fund of Colleges and Universities in Guangxi, No. Gui Jiao Ke Yan [2014]6; National Natural Science Foundation of China, No. 31460023; and Natural Science Foundation of Guangxi, No. 2014GXNSFAA118206.
Ethics approval: The study was reviewed and approved by the Youjiang Medical College Institutional Review Board.
Institutional animal care and use committee: All procedures involving animals were reviewed and approved by the Institutional Animal Care and Use Committee of the Guangxi Zhuang Autonomous Region Science and Technology Agency (IACUC protocol number: SCXK 2012-0003).
Conflict-of-interest: The authors declare no conflicts of interest to disclose.
Data sharing: No additional data are available.
Open-Access: This article is an open-access article which was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: http://creativecommons.org/licenses/by-nc/4.0/
Peer-review started: November 2, 2014
First decision: December 2, 2014
Article in press: February 5, 2015
P- Reviewer: Miller C, Miller JS, Schaffellner S S- Editor: Yu J L- Editor: Logan S E- Editor: Ma S
References
- 1.Wang H, Liu J, Dai DF, Guan XW, Ding J, Shao SL. Construction of cagL gene mutant in Helicobacter pylori. Zhongguo Mianyixue Zazhi. 2012;28:775–778. [Google Scholar]
- 2.Gisbert JP. [Helicobacter pylori-related diseases] Gastroenterol Hepatol. 2012;35 Suppl 1:12–25. doi: 10.1016/S0210-5705(12)70030-4. [DOI] [PubMed] [Google Scholar]
- 3.Cid TP, Fernández MC, Benito Martínez S, Jones NL. Pathogenesis of Helicobacter pylori infection. Helicobacter. 2013;18 Suppl 1:12–17. doi: 10.1111/hel.12076. [DOI] [PubMed] [Google Scholar]
- 4.Thirumurthi S, Graham DY. Helicobacter pylori infection in India from a western perspective. Indian J Med Res. 2012;136:549–562. [PMC free article] [PubMed] [Google Scholar]
- 5.Vilaichone RK, Yamaoka Y, Shiota S, Ratanachu-ek T, Tshering L, Uchida T, Fujioka T, Mahachai V. Antibiotics resistance rate of Helicobacter pylori in Bhutan. World J Gastroenterol. 2013;19:5508–5512. doi: 10.3748/wjg.v19.i33.5508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Malfertheiner P, Megraud F, O’Morain CA, Atherton J, Axon AT, Bazzoli F, Gensini GF, Gisbert JP, Graham DY, Rokkas T, et al. Management of Helicobacter pylori infection--the Maastricht IV/ Florence Consensus Report. Gut. 2012;61:646–664. doi: 10.1136/gutjnl-2012-302084. [DOI] [PubMed] [Google Scholar]
- 7.Gao HJ, Sheng HH. Drug resistance related gene detection and Helicobacter pylori eradication. Zhonghue Yixue Zazhi. 2012;92:657–658. [PubMed] [Google Scholar]
- 8.Abdollahi H, Savari M, Zahedi MJ, Moghadam SD, Hayatbakhsh Abasi M. Detection of A2142C, A2142G, and A2143G Mutations in 23s rRNA Gene Conferring Resistance to Clarithromycin among Helicobacter pylori Isolates in Kerman, Iran. Iran J Med Sci. 2011;36:104–110. [PMC free article] [PubMed] [Google Scholar]
- 9.Vega AE, Cortiñas TI, Puig ON, Silva HJ. Molecular characterization and susceptibility testing of Helicobacter pylori strains isolated in western Argentina. Int J Infect Dis. 2010;14 Suppl 3:e85–e92. doi: 10.1016/j.ijid.2009.11.022. [DOI] [PubMed] [Google Scholar]
- 10.Kim MS, Kim N, Kim SE, Jo HJ, Shin CM, Lee SH, Park YS, Hwang JH, Kim JW, Jeong SH, et al. Long-term follow-up Helicobacter pylori reinfection rate and its associated factors in Korea. Helicobacter. 2013;18:135–142. doi: 10.1111/hel.12018. [DOI] [PubMed] [Google Scholar]
- 11.Wueppenhorst N, Stueger HP, Kist M, Glocker E. Identification and molecular characterization of triple- and quadruple-resistant Helicobacter pylori clinical isolates in Germany. J Antimicrob Chemother. 2009;63:648–653. doi: 10.1093/jac/dkp003. [DOI] [PubMed] [Google Scholar]
- 12.Liu ZQ, Zheng PY. Important role of efflux pump gene hefA in multidrug resistance of Helicobacter pylori. Shijie Huaren Xiaohu Zazhi. 2008;14:5217–5222. doi: 10.3748/wjg.14.5217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Zhang Z, Liu ZQ, Zheng PY, Tang FA, Yang PC. Influence of efflux pump inhibitors on the multidrug resistance of Helicobacter pylori. World J Gastroenterol. 2010;16:1279–1284. doi: 10.3748/wjg.v16.i10.1279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Zou SP, Lian JG. Jiawei Banxia Xiexin decoction for treatment of chronic atrophic gastritis: analysis of 35 cases. Dangdai Yixue. 2013;19:155–156. [Google Scholar]
- 15.Zhu FY, Wu JL, Xu S. Scanning electron microscopic observation of effect of Leweiyin on the gastric mucosa of rats with chronic atrophic gastritis. JTCM. 2012;18:269–270. [Google Scholar]
- 16.Wang WH, Hu FL. A multicenter study of Chinese patent medicine Wenweishu /Yangweishu in the treatment of Helicobacter pylori positive patients with chronic gastritis and peptic ulcer. Zhonghua Yixue Zazhi. 2010;90:75–78. [PubMed] [Google Scholar]
- 17.Ma F, Chen Y, Li J, Qing HP, Wang JD, Zhang YL, Long BG, Bai Y. Screening test for anti-Helicobacter pylori activity of traditional Chinese herbal medicines. World J Gastroenterol. 2010;16:5629–5634. doi: 10.3748/wjg.v16.i44.5629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Wu J, Hu D, Wang KX. In vitro antibacterial activity of radix scutellariae and baicalin against Helicobacter pylori. Zhongyaocai. 2008;31:707–710. [PubMed] [Google Scholar]
- 19.Lin J, Huang WW. A systematic review of treating Helicobacter pylori infection with Traditional Chinese Medicine. World J Gastroenterol. 2009;15:4715–4719. doi: 10.3748/wjg.15.4715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Bu Y, Lee K, Jung HS, Moon SK. Therapeutic effects of traditional herbal medicine on cerebral ischemia: a perspective of vascular protection. Chin J Integr Med. 2013;19:804–814. doi: 10.1007/s11655-013-1341-2. [DOI] [PubMed] [Google Scholar]
- 21.Chang CH, Huang WY, Lai CH, Hsu YM, Yao YH, Chen TY, Wu JY, Peng SF, Lin YH. Development of novel nanoparticles shelled with heparin for berberine delivery to treat Helicobacter pylori. Acta Biomater. 2011;7:593–603. doi: 10.1016/j.actbio.2010.08.028. [DOI] [PubMed] [Google Scholar]
- 22.Sun YX. Treatment of 60 cases of chronic atrophic gastritis based on syndrome differentiation. Hunan Zhongyi Zazhi. 2010;26:71–72. [Google Scholar]
- 23.Zhang L. Relationship between Helicobacter pylori and chronic atrophic gastritis and its prevention and treatment. Zhongguo Zhongxiyi Jiehe Zazhi. 2008;12:521–523. [PubMed] [Google Scholar]
- 24.Huang YQ, Huang GR, Li XH, Huang XF, Wei LD, Wei HY, Chen YH, Tang HY, Yang S, Qin YC. Effect of traditional Chinese medicine extracts on bio-membrane formation in drug-resistant Helicobacter pylori. Zhongguo Yiyao Daobao. 2013;32:1407–1409. [Google Scholar]
- 25.Wu ZB. Pharmacological mechanism of heat-clearing effects of baicalin. Anmo yu Kangfu Yixue. 2011:2. [Google Scholar]
- 26.Wang JP, Peng XW. Single Chinese herb for treatment of Helicobacter pylori infection in animal models. Weichangbingxue He Ganbingxue Zazhi. 2010;19:345–7. [Google Scholar]
- 27.Peng RJ, Peng XW. In vitro antibacterial activity of vitamin C, resveratrol and emodin against Helicobacter pylori. JTCM. 2011;3:51–52. [Google Scholar]
- 28.Hsu SC, Chung JG. Anticancer potential of emodin. BioMedicine. 2012;2:108–16. doi: 10.1016/j.biomed.2012.03.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Huang XM, Huang H, Ou LM, Li J. In vitro activity of rhubarb against non-spore-forming anaerobes. Zhongguo Zhongyiyao Xinxi Zazhi. 2001;8:41–42. [Google Scholar]


