Abstract
Background
The authors undertook a study involving members of a dental practice-based research network to determine the outcome and factors associated with success and failure of endodontic therapy.
Methods
Members in participating practices (practitioner-investigators [P-Is]) invited the enrollment of all patients seeking treatment in the practice who had undergone primary endodontic therapy and restoration in a permanent tooth three to five years previously. If a patient had more than one tooth so treated, the P-I selected as the index tooth the tooth treated earliest during the three- to five-year period. The authors excluded from the study any teeth that served as abutments for removable partial dentures or overdentures, third molars and teeth undergoing active orthodontic endodontic therapy. The primary outcome was retention of the index tooth. Secondary outcomes, in addition to extraction, that defined failure included clinical or radiographic evidence (or both) of periapical pathosis, endodontic retreatment or pain on percussion.
Results
P-Is in 64 network practices enrolled 1,312 patients with a mean (standard deviation) time to follow-up of 3.9 (0.6) years. During that period, 3.3 percent of the index teeth were extracted, 2.2 percent underwent retreatment, 3.6 percent had pain on percussion and 10.6 percent had periapical radiolucencies for a combined failure rate of 19.1 percent. The presence of preoperative periapical radiolucency with a diagnosis of either irreversible pulpitis or necrotic pulp was associated with failure after multivariate analysis, as were multiple canals, male sex and Hispanic/Latino ethnicity.
Conclusions
These results suggest that failure rates for endodontic therapy are higher than previously reported in general practices, according to results of studies based on dental insurance claims data.
Clinical Implications
The results of this study can help guide the practitioner in deciding the most appropriate course of therapy for teeth with irreversible pulpitis, necrotic pulp or periapical periodontitis.
Keywords: Endodontic therapy, root canal, practice-based research, treatment outcome
Practice-based research networks (PBRNs) enable groups of practitioners to conduct clinical studies while providing care for their patients. Questions for PBRN studies commonly arise from the practitioners themselves and address questions of significance in clinical practice. One decision frequently confronted in general dental practice arises when the clinician is presented with a diagnosis of irreversible pulpitis, necrotic pulp or periapical periodontitis: whether to perform endodontic therapy followed by restoration or to extract the tooth and place an implant-supported restoration or a fixed prosthesis. Results of the many clinical studies reported to date regarding these three modes of treatment should guide the clinician when making this common decision; however, the reported outcomes of endodontic therapy and subsequent restoration vary widely.
This variation in reported outcomes is the result of several factors, including varying criteria used to define success or failure, the interval of follow-up after therapy, the operators’ level of experience and whether or not the restoration outcome was included in the analysis. For example, a meta-analysis of 40 studies involving the use of the absence or reduction in perapical pathosis as a measure of success for primary endodontic therapy reported a pooled success rate of 74.7 percent (95 percent confidence interval [CI], 69.8–79.5), with follow-up taking place from six months to as long as 30 years after treatment.1 However, investigators in a second meta-analysis of 18 studies involving the use of various clinical and radiographic criteria for primary endodontic therapy reported pooled success rates of 90 percent (95 percent CI, 88–92) for two to four years, 93 percent (95 percent CI, 87–97) for four to six years and 84 percent (95 percent CI, 82–87) for more than six years after primary endodontic therapy.2 In addition, most studies cited in both meta-analyses were derived from academic or specialty practices, making the results of these studies difficult to apply in the general dental practice setting.
Researchers have used dental insurance claims data to evaluate the outcome of primary endodontic therapy in general as well as specialty private practices. The results of these studies suggest that the outcomes of primary endodontic therapy performed by general dentists are equivalent to those of treatment provided by specialists, although specialists tend to treat more complex cases. Lazarski and colleagues3 retrospectively analyzed selected outcomes after primary endodontic therapy by using an insurance company database of 110,766 cases that were completed by endodontists and the referring general dentists. In a subset of 44,613 cases, with a minimum follow-up of two years, the reported incidence of extraction, retreatment and periapical surgery was 5.6 percent, 2.5 percent and 1.4 percent, respectively. Overall, 94.4 percent of nonsurgically treated teeth remained in function during an average follow-up period of 3.5 years. The authors noted that the incidence of extraction after endodontic therapy increased with patients’ age, and teeth that were not restored after endodontic therapy were significantly more likely to be extracted than were restored teeth. Although endodontists treated a significantly higher proportion of molars (48 percent more; P < .001) and a lower proportion of anterior teeth (43 percent fewer; P < .001) than did general dentists, the two provider groups had comparable success rates.
Even higher rates of endodontic success were reported in the insurance database study by Salehrabi and Rotstein,4 in which the majority of adverse events occurred in the first three years after endodontic therapy and, overall, 97 percent of teeth were retained eight years after initial nonsurgical endodontic therapy. The results of another study, in which investigators drew on the Taiwan National Health Insurance database to examine outcomes for 1,557,547 teeth that had received primary endodontic therapy performed by both general dentists and specialists, showed a 92.9 percent retention rate after five years. In that period, 111,348 teeth (7.1 percent) were extracted and 55,089 (3.5 percent) were retreated or had periapical surgery, resulting in a combined failure rate of 10.6 percent for primary endodontic therapy.5 It should be noted that several reasons for extraction subsequent to, but not directly linked with, endodontic therapy—including root fracture, advanced periodontitis and trauma—are included in many outcome studies of primary endodontic therapy.
In view of the varying outcomes reported for primary endodontic therapy and the questionable applicability of the results of past studies conducted in specialty or academic settings to decisions faced in general practice, we conducted a retrospective study to determine the outcomes of primary endodontic therapy in a network of private general dental practices. Our working hypothesis was the outcomes for endodontic therapy and subsequent restoration would not differ from those in published studies involving the use of dental insurance claim databases. Our secondary aim was to define factors associated with success and failure of endodontic therapy and subsequent restoration in general dental practices. In this article, we present success rates for endodontic therapy and factors associated with success and failure. (A subsequent article reporting outcomes for single-tooth restorations after endodontic therapy has been developed and is undergoing review.)
METHODS
Study design and inclusion criteria
The study was conducted by the Practitioners Engaged in Applied Research and Learning (PEARL) Network, a PBRN funded by the National Institute of Dental and Craniofacial Research and established in 2005.6 The PEARL Network’s approximately 230 member dentists are primarily general practitioners located in the northeastern United States. We used a retrospective study design to assess the outcome of primary, nonsurgical endodontic therapy and factors associated with success or failure of that therapy.
Patients seeking care from PEARL Network practices for any reason who had undergone endodontic therapy and subsequent restoration three to five years previously were invited by practitioner-investigators (P-Is) to enroll in the study. If more than one tooth was treated, the P-I selected as the index (study) tooth the tooth that had been treated earliest during the three-to five-year period. We allowed that endodontic therapy could have been performed by either the general dentist or a specialist; however, we required that the restoration have been placed by the general dentist. Included in the analysis were 11 teeth that had been planned to receive, but had not yet received, a definitive restoration. Additional inclusion criteria required the index tooth to be a permanent tooth with a fully formed apex at the time of endodontic treatment. Patients also had to be 70 years or younger when endodontic therapy was performed. We excluded teeth that served as an abutment for a removable partial denture or overdenture, third molars and teeth undergoing active orthodontic treatment. We permitted as many as 100 participants to be enrolled from a single practice. The New York University School of Medicine Institutional Review Board, New York City, reviewed and approved the study protocol.
Study protocol and data collection
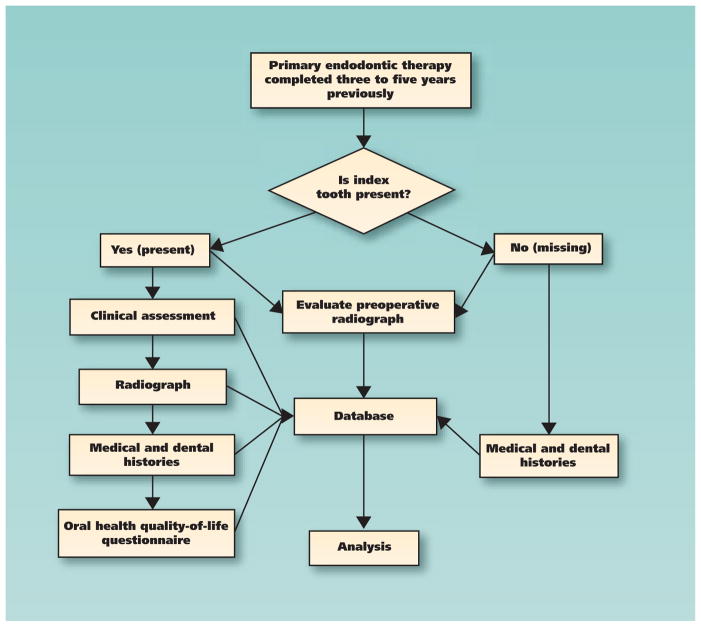
Figure 1 shows the flow of our data collection process. After each participant provided written informed consent, P-Is completed a demographic form documenting the participant’s age, sex, and ethnicity and race. In addition, the practitioner recorded the presence or absence of the index tooth and, if it was absent, the reason for extraction.
Figure 1.
Study data collection flowchart.
If the index tooth was present, the clinical data recorded included pain on percussion (recorded dichotomously, according to patient report), whether the restoration had been or needed to be replaced and reason for replacement, the number of proximal contacts, cracking or fracturing of the tooth, presence of primary or secondary caries and extent of periodontitis as measured by means of probing depth and mobility. If the index tooth had received secondary endodontic treatment, the dentist was to record the reason and type of treatment (retreatment or periapical surgery). If a periapical radiograph of the index tooth had not been obtained within the preceding seven months, the P-I obtained and examined a new one for periapical pathosis, widening of the periodontal ligament space or radiographic suggestion of root fracture. The participant also completed a tooth sensitivity assessment and an oral health inventory questionnaire.
For all index teeth, the P-I recorded whether the tooth was vital or nonvital before endodontic therapy began, whether a general dentist or a specialist had performed the endodontic therapy, the type of endodontic technique used (compaction technique and materials), whether the preoperative radiograph demonstrated periapical pathosis, whether the dentist had prescribed antibiotics, and the number of visits required to complete endodontic therapy. The P-I also recorded whether the patient received a post and, if so, reported the type of post, the type of coronal restoration placed, the date of final restoration placement, whether the restoration was replaced and, if so, the reason for replacement.
Participating practices submitted all data electronically to the central PEARL Network data coordinating center (The EMMES Corp., Rockville, Md.) by means of a proprietary electronic data capture software program (AdvantageEDC, EMMES). Source documents, work sheets and case report forms remained at the practices until the conclusion of the study. PEARL Network P-Is used a Web-based module to undergo training and technique calibration regarding the characterization of radiographic periapical lesions and all aspects of data collection for this study. The PEARL Network also supplied a chairside reference guide that provided inclusion-exclusion check-off questions and radiographic examples of periapical pathosis. Once the P-Is completed online training, a certified PEARL Network clinical research associate traveled to the practice to initiate the study, review the case report forms and ensure the practice staff’s competence in using the AdvantageEDC data capture software. Clinical research associates also were available if questions arose at practice sites during the study, and they monitored sites for data quality assurance.
The participating practice sent a duplicate periapical radiograph of the index tooth at follow-up to the PEARL Network administrative center. Two of the authors, a board-certified periodontist (R.G.C.) and an endodontist (D.F.), made the determination of periapical pathosis if they clearly observed a lesion that corresponded to a score of 3 or higher on a periapical index (PAI) developed by Orstavik and colleagues.7 Both reviewers were masked as to practitioner-reported outcome before undertaking the evaluation.
Statistical analysis
Our specific aims in this study were to examine the outcome of primary endodontic therapy in the general practice setting three to five years after endodontic treatment and to evaluate risk factors associated with adverse outcomes. We used logistic regression to evaluate the relationship between the primary and secondary dependent variables and the independent variables listed below. The primary dependent variable was the presence or absence of the index tooth. Secondary dependent variables were additional variables that defined endodontic failure: presence of clinical or radiographically visible periapical pathosis, endodontic retreatment of the index tooth and pain on percussion. The independent variables were the initial condition of the tooth, as assessed retrospectively by the dentist, combined with preoperative periapical pathosis; whether a general dentist or a specialist performed endodontic therapy; the number of visits needed to complete the endodontic therapy; endodontic restoration (whether the index tooth had single or multiple canals); tooth type; use of antibiotics; restoration type (resin-based composite or amalgam restoration versus full or partial crown or onlay); post replacement; existing proximal contacts; time to coronal restoration; patients’ demographic data (age, sex, and race and ethnicity) and periodontal involvement (yes or no).
The study was powered assuming a 95 percent tooth retention rate to detect a 75 percent increase in risk associated with binary, relatively nonskewed covariates. We included factors significant at P = .10 in the univariate setting in the multivariate model with backward elimination at P = .05 for variable selection. In the case of correlated factors, we included only one of the factors in the multivariate model.
RESULTS
From May 2007 through September 2010, P-Is enrolled in the study 1,323 patients who had undergone primary endodontic therapy and restoration. Of the patients enrolled, we deemed 11 ineligible because their endodontic therapy had been completed outside the three- to five-year requirement (n = 6), a radiograph had not been obtained at the study visit (n = 4) or the index tooth served as an abutment for a removable partial denture (n = 1). This left 1,312 participants for analysis—and then one patient withdrew from the study before the outcome assessment phase. The mean (standard deviation) time to follow-up after completion of primary endodontic therapy was 3.9 (0.6) years. The median age of the participants at enrollment was 52 years (age range, 14–74 years), and 58 percent were female. Participant-reported race was 86 percent white, 4 percent African American, 5 percent Asian, 0.5 percent Hawaiian/Pacific Islander, 0.4 percent Alaska Native or American Indian and 3 percent unknown. Participant-reported ethnicity was 7 percent Hispanic/Latino, 89 percent not Hispanic/Latino and 4 percent unknown. Participants were enrolled from 64 sites; the median enrollment was 11 participants per site (range, 1–100). The distribution of enrolling sites was 69 percent suburban, 19 percent urban and 12 percent rural. The median number of years in practice for enrolling dentists was 23 (range, 2–35 years).
The distribution of endodontically treated teeth was 11 percent incisors, 5 percent canines, 28 percent premolars and 56 percent molars. Specialists treated 32 percent of the teeth, 80 percent of which had multiple canals. The pre-operative diagnosis of 60 percent of the index teeth was irreversible pulpitis; that of the remainder was necrotic pulp. Practitioners used lateral compaction in 51 percent, thermal compaction in 41 percent and thermoplastic injection in 5 percent of the index teeth; they used other methods in the other 3 percent of index teeth. Practitioners prescribed antibiotics in 30 percent of the procedures, with penicillin, erythromycin, clindamycin and cephalosporin (first generation) prescribed in 70 percent, 11 percent, 10 percent and 6 percent of these procedures, respectively. The majority of teeth (69 percent) received full-coverage restorations, whereas most of the remaining teeth (26 percent) received composite or amalgam restorations. Practitioners placed posts in 56 percent of treated teeth.
Table 1 shows the outcomes of endodontic therapy. The percentage of index teeth extracted (primary outcome) was 3.3 percent. Reasons for extraction of 43 index teeth were root fractures (57 percent), endodontic failure (24 percent), advanced periodontitis (9 percent), recurrent caries (9 percent) and other (2 percent). The other three index teeth were recoded to forms of restorative failure rather than extraction. Multivariate analysis showed an association between extraction of index teeth and the absence of a post (odds ratio [OR], 5.74; 95 percent CI, 2.62–12.57), teeth with multiple versus single canals (OR, 2.79; 95 percent CI, 1.20–6.49), teeth diagnosed as having necrotic pulp (OR, 2.48; 95 percent CI, 1.30–4.74) and older patient age (OR, 1.05; 95 percent CI, 1.01–1.08).
TABLE 1.
Outcomes of primary endodontic therapy in index teeth three to five years after treatment in general practice (N = 1,311*).
| TYPE OF FAILURE | NO. (PERCENTAGE) | 95% CONFIDENCE INTERVAL |
|---|---|---|
| Extraction | 43 of 1,311 (3.3) | 2.3–4.2 |
| Endodontic Retreatment | 29 of 1,311 (2.2) | 1.4–3.0 |
| Pain on Percussion | 45 of 1,265 (3.6) | 2.5–4.6 |
| Periapical Pathosis | 134 of 1,265 (10.6) | 8.7–12.0 |
| TOTAL | 251 of 1,311 (19.1) | 17.0–21.3 |
Denominator is 1,311 rather than 1,312 because one participant exited the study before undergoing evaluation of the index tooth.
Secondary adverse outcomes for endodontic therapy included endodontic retreatment (2.2 percent), pain on percussion (3.6 percent) or periapical pathosis (10.6 percent), for a combined adverse outcome rate of 19.1 percent (95 percent CI, 17.0–21.3). Five of the 11 nonrestored endodontically treated teeth were in this category.
Table 2 shows the distribution of patient characteristics and associations with adverse outcomes after endodontic therapy. Male patients were at greater risk of experiencing failure than were female patients (OR, 1.35; P = .032) and Hispanic or Latino patients were at greater risk than those who were not Hispanic or Latino or were of unknown ethnicity (OR, 1.88; P < .01). We found no association for patient’s age or for race.
TABLE 2.
Distribution of participants’ characteristics and univariate associations with adverse outcomes after primary endodontic therapy (N = 1,311*).
| FACTOR | ADVERSE OUTCOME
|
ODDS RATIO | CONFIDENCE INTERVAL | P VALUE | OVERALL P VALUE | |
|---|---|---|---|---|---|---|
| Yes | No | |||||
|
| ||||||
| Sex, No. (%) | ||||||
| Female | 130 (17.2) | 628 (82.8) | 1.00 | —† | — | .03 |
| Male | 121 (21.9) | 432 (78.1) | 1.35 | 1.03–1.78 | .03 | |
|
| ||||||
| Race, No. (%) | ||||||
| White | 215 (19.0) | 916 (81.0) | 1.00 | — | — | .75 |
| Not white/unknown | 36 (20.0) | 144 (80.0) | 1.07 | 0.72–1.58 | .75 | |
|
| ||||||
| Ethnicity, No. (%) | ||||||
| Not Hispanic/Latino | 224 (18.4) | 996 (81.6) | 1.00 | — | — | < .01 |
| Hispanic/Latino | 27 (29.7) | 64 (70.3) | 1.88 | 1.17–3.01 | .01 | |
|
| ||||||
| Age in Years, Mean/Median (Standard Deviation) | 49.1/51.0 (251/12.7) | 50.2/52.0 (1,060/11.4) | 0.99 | 0.98–1.00 | .17 | .17 |
Denominator is 1,311 rather than 1,312 because one participant exited the study before undergoing evaluation of the index tooth.
Reference group.
Table 3 shows the univariate associations between clinical characteristics and endodontic therapy failure. A tooth with a periapical pathosis with either a diagnosis of irreversible pulpitis (OR, 2.24; P < .01) or necrotic pulp (OR, 2.68; P < .01 was at significantly greater risk of experiencing failure. Among tooth types, molars had the greatest risk of experiencing failure, whereas teeth with multiple canals had a greater risk of experiencing failure than did teeth with single canals (OR, 1.60; P < .01). Teeth with periodontal connective tissue attachment loss also were associated with failure (OR, 1.89; P < .01). We found none of the following to be associated with increased risk of experiencing failure: the type of provider (whether generalist or specialist), the number of visits required to complete endodontic therapy, the endodontic technique used, the type of restoration placed, the time to restoration, whether antibiotics were prescribed or placement of posts.
TABLE 3.
Univariate associations between clinical characteristics and adverse outcomes three to five years after primary endodontic therapy in general practice.
| FACTOR | YES NO. (%) |
NO NO. (%) |
ODDS RATIO | CONFIDENCE INTERVAL | P VALUE | OVERALL P VALUE |
|---|---|---|---|---|---|---|
|
| ||||||
| Initial Diagnosis and Periapical Pathosis (PP) | ||||||
| Irreversible pulpitis without PP | 78 (13.3) | 508 (86.7) | 1.00 | —* | — | |
| Necrotic pulp without PP | 30 (14.2) | 182 (85.8) | 1.07 | 0.68–1.69 | .76 | < .01 |
| Irreversible pulpitis with PP | 51 (25.6) | 148 (74.4) | 2.24 | 1.51–3.34 | < .01 | |
| Necrotic pulp with PP | 91 (29.2) | 221 (70.8) | 2.68 | 1.91–3.77 | < .01 | |
|
| ||||||
| Type of Provider | ||||||
| General practitioner | 174 (19.5) | 717 (80.5) | 1.00 | — | — | .61 |
| Specialist | 77 (18.3) | 343 (81.7) | 0.93 | 0.69–1.25 | .61 | |
|
| ||||||
| Visits Required to Complete Endodontic Therapy | ||||||
| One | 119 (18.0) | 543 (82.0) | 1.00 | —* | —* | .41 |
| Two | 105 (21.0) | 395 (79.0) | 1.21 | 0.91–1.63 | .120 | |
| Three or more | 27 (18.1) | 122 (81.9) | 1.01 | 0.64–1.60 | .97 | |
|
| ||||||
| Tooth Type | ||||||
| Canine | 7 (11.7) | 53 (88.3) | 1.00 | — | — | |
| Incisor | 26 (17.9) | 119 (82.1) | 1.65 | 0.68–4.05 | .27 | < .01 |
| Premolar | 55 (14.7) | 319 (85.3) | 1.31 | 0.56–3.02 | .53 | |
| Molar | 163 (22.3) | 569 (77.7) | 2.17 | 0.97–4.86 | .06 | |
|
| ||||||
| Number of Canals | ||||||
| Single canal | 58 (14.4) | 344 (85.6) | 1.00 | — | — | < .01 |
| Multiple canals | 193 (21.2) | 716 (78.8) | 1.60 | 1.16–2.20 | < .01 | |
|
| ||||||
| Antibiotic Prescribed | ||||||
| No | 162 (17.8) | 748 (82.2) | 1.00 | — | — | .06 |
| Yes | 89 (22.3) | 310 (77.7) | 1.33 | 0.99–1.77 | .06 | |
|
| ||||||
| Restoration Type | ||||||
| Full/partial crown or onlay | 166 (17.8) | 766 (82.2) | 1.00 | — | — | .12 |
|
| ||||||
| Composite/amalgam restoration | 80 (21.6) | 291 (78.4) | 1.27 | 0.94–1.71 | .12 | |
| Post Replaced | ||||||
| Yes | 126 (17.3) | 602 (82.7) | 1.00 | — | — | .06 |
| No | 125 (21.4) | 458 (78.6) | 1.30 | 0.99–1.72 | .06 | |
|
| ||||||
| Periodontal Involvement | ||||||
| No | 175 (15.4) | 961 (84.6) | 1.00 | — | — | < .01 |
| Yes | 33 (25.6) | 96 (74.4) | 1.89 | 1.23–2.89 | < .01 | |
|
| ||||||
| Time to Restoration, Mean/Median (No. [Standard Deviation]) | 5.3/1.7 (246 [8.9]) | 5.2/1.8 (1,054 [8.8]) | 1.00 | 0.99–1.02 | .88 | .88 |
Reference group.
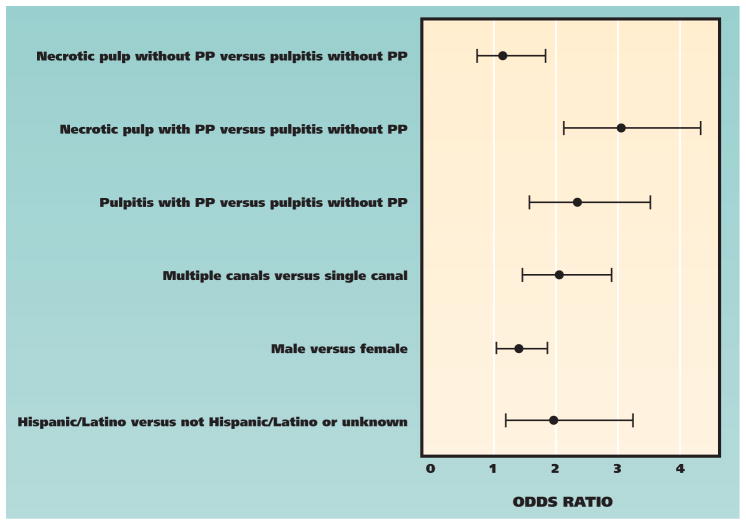
Figure 2 shows factors associated with failure after multivariate analyses. The predictive model for the odds of failure involved the following covariates: teeth with multiple canals (OR, 2.05; P < .01); presence of preoperative periapical pathosis with either a diagnosis of irreversible pulpitis (OR, 2.34; P < .01) or necrotic pulp (OR, 3.03; P < .01); male sex (OR, 1.40; P < .05); and Hispanic or Latino ethnicity (OR, 1.97; P < .01).
Figure 2.
Factors associated (by means of multivariate analysis) with adverse outcomes after primary endodontic therapy, shown as odds ratios with 95 percent Wald confidence limits. PP: Periapical pathosis.
DISCUSSION
The primary objective of this study was to determine the three- to five-year outcome of primary endodontic therapy in private general dental practices. The intent was to help provide an evidence base to guide the general practitioner when he or she is attempting to determine the most favorable course of treatment for a tooth with irreversible pulpitis, periapical periodontitis or necrotic pulp. In our study, 19.1 percent of teeth receiving primary endodontic therapy were classifiable as failures after an average follow-up of 3.9 years. This adverse outcome is at a considerably higher degree than those reported by Lazarski and colleagues,3 Salehrabi and Rotstein4 and Chen and colleagues5—all of whom used dental insurance claims databases—and was principally the result of the strict criteria for success we used in this study. Dental insurance claims databases typically do not include clinical or radiographic status at follow-up (such as the presence of periapical pathosis, which was the most common reason for failure in our study) or loss of patients to recall or patient-centered outcomes such as pain on percussion. Dental claims databases typically contain information regarding procedures performed in endodontically treated teeth for which a claim was previously submitted. Therefore, dental insurance claims data report rates of survival (that is, presence of the tooth) rather than success (that is, free of detectable pathology and patient discomfort) for primary endodontic therapy, the latter being more encompassing and of greater interest to the general dental practitioner and the patient.
Investigators have questioned the lack of periapical pathosis or the reduction in radiographic periapical lesion size across time as a criterion for endodontic success, chiefly owing to limitations in interpretation with the use of two-dimensional periapical radiographs but also with the advent of the increased sensitivity afforded by three-dimensional cone-beam computed tomography (CBCT).8 The incidence of periapical pathosis in endodontic outcomes studies undoubtedly will increase in the future with the growing use of CBCT.
Our study included pain on percussion as a criterion for failure, although many endodontics outcomes studies do not (especially in the absence of periapical pathosis9–12) because of the subjective nature of the patient’s response. We included it in our study because it may signal the presence of periapical inflammation not apparent on conventional radiographs. In addition, from a practice management viewpoint, it is important that the patient be satisfied and comfortable with the outcome of therapy, especially if other treatment options exist.
Although systematic reviews regarding the outcome of primary endodontic therapy have been published, the results of most studies included in those reviews, which usually are conducted in academic or specialty settings, are not entirely applicable to private general practice. Nevertheless, they provide a range of outcomes for comparison with those of our study. A 2007 systematic review and meta-analysis of 13 studies from an initial screening of 430 reports published between 1966 and 2006 showed a survival rate of 97.7 percent 36 months after primary endodontic therapy.2 However, the investigators did not include in the analysis the clinical or radiographic status of the endodontically treated teeth. At six or more years, researchers in two combined studies reported a success rate of 84 percent (95 percent CI, 82–87) after meta-analysis2; however, patient-centered outcomes, such as pain on percussion, were not part of the success criteria. Results of a second systematic review and meta-analysis of 63 outcome studies from 1922 to 2002 showed pooled success rates at least one year after primary endodontic therapy to average 74.7 percent, with a range of 68 to 85 percent, when researchers applied “strict” criteria (that is, lack of periapical radiolucencies) and to average 85.2 percent with a range of 60 to 100 percent when researchers applied “loose” criteria (that is, reduction in periapical radiolucency).1 Endodontic outcome results of Ng and colleagues’1 meta-analysis involving the use of strict criteria more closely approximate the results of our study, in which 19.1 percent failed three to five years after treatment. Ng and colleagues1 also noted that during the period from 1922 to 2002, reported success rates of primary endodontic therapy generally did not increase, even in view of advances in restorative materials and techniques, including microsurgery.1 Lastly, investigators in a systematic review and meta analysis of 14 studies published between 1993 and 2007 reported tooth survival after endodontic therapy to be 86 percent after two to three years, 93 percent after four to five years and 87 percent after eight to 10 years.13
Results of outcome studies of primary endodontic therapy conducted by specialists reflect the upper limits of outcomes provided in a highly standardized and controlled environment. Investigators in a recent comparison of single-unit restorations for implant versus primary endodontically treated teeth from an endodontic private group practice, a study involving 143 teeth, reported a success rate of 90.2 percent at an average of 22 months (range, 18–59 months) after primary endodontic therapy. Failure criteria included extraction, retreatment, PAI score of 3 or higher or need for periapical surgery.14 Researchers in the postgraduate endodontics program at the University of Toronto published a series of prospective studies regarding the four- to six-year outcomes of primary endodontic therapy.9–12 They classified teeth as healed if the teeth had a PAI score of 2 or higher, with no signs or symptoms other than tenderness on percussion, which more closely approximates the strict criteria for success in our study. In total, the investigators classified 439 (86 percent) of 510 teeth as healed and 71 (14 percent) of 510 teeth as diseased.12 Of note was the 41 percent recall rate for all endodontically treated teeth, which underscores the difficulty in performing prospective outcomes assessment studies in an institutional environment with a transient patient base.
A secondary objective of our study was to identify factors associated with success or failure three to five years after primary endodontic therapy in general practices. The primary outcome was extraction of the index tooth. As noted in the Results section, multivariate analysis found absence of a post, teeth with multiple canals, a diagnosis of necrotic pulp and older patient age to be associated with extraction. These results confirm those of earlier primary endodontic therapy outcome studies indicating that preoperative periapical pathosis or teeth with necrotic pulp or multiple canals are associated with subsequent extraction.3,5,9,10–13 In our study, when we combined primary and secondary outcomes, results of multivariate analysis demonstrated an increased risk of experiencing an adverse outcome after endodontic therapy in teeth with preoperative periapical pathosis and a diagnosis of either irreversible pulpitis or necrotic pulp; in teeth with multiple canals; and in patients who were male or of Hispanic or Latino ethnicity.
Most of the factors we found in our study were reported in earlier studies conducted mainly in academic or specialty settings. Results of the fourth phase of the Toronto endodontic therapy outcomes studies cited earlier showed, after multivariate analysis, that a preoperative periapical pathosis (OR, 2.86; 95 percent CI, 1.56–5.24; P < .01) and teeth with multiple canals (OR, 2.53; 95 percent CI, 1.25–5.13; P = .10) were associated with treatment failure.12 For teeth with preoperative periapical pathosis, the presence of an intraoperative complication (OR, 2.27; 95 percent CI, 1.05–4.89; P = .037) and use of a lateral versus vertical filling technique (OR, 1.88; 95 percent CI, 1.01–3.53; P = .049) were associated with failure.12 Results of a systematic review and meta-analysis of 63 studies showed the following factors to be associated with success of primary endodontic therapy: teeth other than mandibular molars, a vital preoperative diagnosis (OR, 1.77; 95 percent CI, 1.35–2.31), absence of preoperative periapical pathosis, root canal filling without radiographically apparent voids, root canals filled within 2 millimeters of the radiographic apex and a satisfactory coronal restoration.14 Investigators in another systematic review and meta-analysis of 19 studies involving 3,891 teeth treated with primary endodontic therapy from 1966 to 2000 who used loose radiographic criteria reported a mean (SD) cumulative success rate of 82.8 (1.19) percent for teeth with a preoperative diagnosis of vital versus necrotic pulp (OR = 1.18; 95 percent CI, 1.06–1.32). Mean (SD) success rates for teeth without preoperative periapical pathosis were 82.0 (1.24) percent, whereas the rates for teeth with a preoperative periapical pathosis were 71.5 (1.60) percent. The difference between teeth with and without periapical pathosis was significant (OR, 2.79; 95 percent CI, 2.44–3.20).15
Investigators in several endodontic therapy outcomes studies reported differences between the sexes,16,17 but several have not18–20; however, these findings have not held up under meta-analysis.13,21 The greater failure rate in Hispanic or Latino patients reported in this study was unexpected and difficult to explain, especially since this group constituted only 7 percent of the study population. Although the 91 Hispanic or Latino patients in this study were enrolled from 22 sites, one site enrolled 37 Hispanic or Latino patients and had an overall higher failure rate. Maximum enrollment of Hispanic or Latino patients at any other site was eight, suggesting the results may be due to a site effect. Alternatively, both the sex and ethnicity effects may be caused by residual confounding variables not accounted for in our analysis or by racial or ethnic anatomical anomalies in this population.
Study strengths
Our study has several strengths that arise directly from its having been performed in a PBRN. First, we conducted it in established private general practices with patients treated in those practices. The results of therapy provided by the practitioner were recorded rigorously, although the specifics of that therapy could not be influenced retroactively. A second strength of the study is the relatively large sample size (1,312 index teeth) enrolled from 64 private practices. Investigators in PBRN effectiveness studies typically enroll a small number of patients from a relatively large number of practices to be able to generalize results better. Third is the use of electronic data capture and data quality assurance procedures, including formal study closeout and physical site audits conducted by study clinical research associates. Together, the results reported in our study tend to reflect those expected in real-life practice, or at least those in the PEARL Network private practices that enrolled patients in the study. We are aware of only two earlier studies of primary endodontic therapy outcomes conducted solely in general practices. A prospective study of teeth receiving endodontic therapy was reported from private practices in Florida.22 Inclusion criteria included follow-up of at least one year or, in the case of extraction, an average follow-up of 24.8 months. Of the 74 teeth included in the study, 19 percent ultimately were extracted. Investigators in a second retrospective study recorded the outcome of primary endodontic therapy for 174 teeth from 13 practices.23 Average follow-up was 8.6 years, and permanent restorations were placed in 89 percent of the teeth with a mean time to restoration of 214.4 days. The authors reported that 18 percent of endodontically treated teeth ultimately were extracted and that time to restoration was a major factor in endodontic treatment failure.23
Study limitations
Our study’s limitations include the predominance of white patients (86 percent), which reflects the practice characteristics of the 64 sites that enrolled patients in the study. Most of the practitioners who participated in the study were experienced clinicians (median 23 years in practice) with well-established practices and stable patient bases. However, these characteristics potentially limit generalization of the results to the nation at large. But in light of the large patient population (n = 1,312) and number of enrolling practices (n = 64), our results probably reflect the outcomes of primary endodontic therapy expected in established practices in the northeastern United States. Also, the P-I submitted a single radiograph on each patient’s enrollment; therefore, some of the periapical pathoses noted in this study actually may have been resolving lesions, because multiple radiographs were not obtained across time to prove otherwise.
CONCLUSIONS
We oversaw a retrospective study of the three- to five-year outcomes of primary endodontic therapy for 1,312 permanent teeth conducted in 64 private practices of the PEARL Network. Overall, 19.1 percent of the treated teeth were classified as failures, with 3.3 percent being extracted, 2.2 percent receiving retreatment, 3.6 percent having pain on percussion and 10.4 percent having periapical pathosis. Strongly associated with failure were preoperative periapical pathosis with a diagnosis of either irreversible pulpitis or necrotic pulp and teeth with multiple canals. The PEARL Network now is conducting a parallel study to examine the outcome of implant therapy and single-unit restoration. The results of both studies should help guide the clinician when deciding the most appropriate course of therapy for teeth with irreversible pulpitis, necrotic pulp or periapical periodontitis.
Acknowledgments
This study was funded by grant U-01-DE016755 awarded to New York University College of Dentistry by the National Institute of Dental and Craniofacial Research, National Institutes of Health, Bethesda, Md.
ABBREVIATION KEY
- CBCT
Cone-beam computed tomography
- PAI
Periapical index
- PBRN
Practice-based research network
- PEARL
Practitioners Engaged in Applied Research and Learning
- P-I
Practitioner-investigator
- PP
Periapical pathosis
Footnotes
Disclosure. None of the authors reported any disclosures.
Contributor Information
Dr. Susan D. Bernstein, Dr. Bernstein maintains a private practice in general dentistry in Cincinnati and is a practitioner-investigator in the Practitioners Engaged in Applied Research and Learning (PEARL) Network, New York City.
Dr. Allan J. Horowitz, Dr. Horowitz maintains a private practice in general dentistry in King of Prussia, Pa., and is a practitioner-investigator in the Practitioners Engaged in Applied Research and Learning (PEARL) Network, New York City.
Dr. Martin Man, Dr. Man maintains a private practice in general dentistry in New York City and is a practitioner-investigator in the Practitioners Engaged in Applied Research and Learning (PEARL) Network, New York City.
Ms. Hongyu Wu, Ms. Wu is a statistician for The EMMES Corporation, Rockville, Md.
Dr. Denise Foran, Dr. Foran is an assistant professor, Department of Endodontics, College of Dentistry, New York University, New York City.
Mr. Donald A. Vena, Mr. Vena is a statistician, The EMMES Corporation, Rockville, Md.; and the principal investigator, Practitioners Engaged in Applied Research and Learning (PEARL) Network Coordinating Center, New York City.
Mr. Damon Collie, Mr. Collie is a project manager for The EMMES Corporation, Rockville, Md.
Dr. Abigail G. Matthews, Dr. Matthews is a biostatistician, The EMMES Corporation, Rockville, Md.
Dr. Frederick A. Curro, Dr. Curro is a clinical professor of pharmacology and oral medicine, Department of Oral and Maxillofacial Pathology, Radiology and Medicine, College of Dentistry, New York University, New York City; the director, Clinical Pharmacology/Regulatory Affairs, College of Dentistry, New York University, New York City; and the director, Recruitment, Retention and Operations Core, Practitioners Engaged in Applied Research and Learning (PEARL) Network, New York City.
Dr. Van P. Thompson, Dr. Thompson is a professor and the chair, Department of Biomaterials and Biomimetics, College of Dentistry, New York University, New York City; and the director, Protocol Development and Training Core, Practitioners Engaged in Applied Research and Learning (PEARL) Network, New York City.
Dr. Ronald G. Craig, Dr. Craig is an associate professor, Department of Basic Sciences and Craniofacial Biology and Department of Periodontology and Implant Dentistry, New York University College of Dentistry, New York City; and the director, Information Dissemination Core, Practitioners Engaged in Applied Research and Learning (PEARL) Network, College of Dentistry, New York University, New York City.
References
- 1.Ng YL, Mann V, Rahbaran S, Lewsey J, Gulabivala K. Outcome of primary root canal therapy: systematic review of the literature, part 1: effects of study characteristics on probability of success (published online ahead of print Oct. 10, 2007) Int Endod J. 2007;40(12):921–939. doi: 10.1111/j.1365-2591.2007.01322.x. [DOI] [PubMed] [Google Scholar]
- 2.Torabinejad M, Anderson P, Bader J, et al. Outcomes of root canal treatment and restoration, implant-supported single crowns, fixed partial dentures, and extraction without replacement: a systematic review. J Prosthet Dent. 2007;98(4):285–311. doi: 10.1016/S0022-3913(07)60102-4. [DOI] [PubMed] [Google Scholar]
- 3.Lazarski MP, Walker WA, 3rd, Flores CM, Schindler WG, Hargreaves KM. Epidemiological evaluation of the outcomes of nonsurgical root canal treatment in a large cohort of insured dental patients. J Endod. 2001;27(12):791–796. doi: 10.1097/00004770-200112000-00021. [DOI] [PubMed] [Google Scholar]
- 4.Salehrabi R, Rotstein I. Endodontic treatment outcomes in a large patient population in the USA: an epidemiological study. J Endod. 2004;30(12):846–850. doi: 10.1097/01.don.0000145031.04236.ca. [DOI] [PubMed] [Google Scholar]
- 5.Chen SC, Chueh LH, Hsiao CK, Tsai MY, Ho SC, Chiang CP. An epidemiologic study of tooth retention after nonsurgical endodontic treatment in a large population in Taiwan (published online ahead of print Jan. 22, 2007) J Endod. 2007;33(3):226–229. doi: 10.1016/j.joen.2006.11.022. [DOI] [PubMed] [Google Scholar]
- 6.Pihlstrom BL, Tabak L. The National Institute of Dental and Craniofacial Research: research for the practicing dentist. JADA. 2005;136(6):728–737. doi: 10.14219/jada.archive.2005.0256. [DOI] [PubMed] [Google Scholar]
- 7.Orstavik D, Kerekes K, Eriksen HM. The periapical index: a scoring system for radiographic assessment of apical periodontitis. Endod Dent Traumatol. 1986;2(1):20–34. doi: 10.1111/j.1600-9657.1986.tb00119.x. [DOI] [PubMed] [Google Scholar]
- 8.Wu MK, Shemesh H, Wesselink PR. Limitations of previously published systematic reviews evaluating the outcome of endodontic treatment (published online ahead of print June 22, 2009) Int Endod J. 2009;42(8):656–666. doi: 10.1111/j.1365-2591.2009.01600.x. [DOI] [PubMed] [Google Scholar]
- 9.Friedman S, Abitbol S, Lawrence HP. Treatment outcome in endodontics: the Toronto Study, phase 1—initial treatment. J Endod. 2003;29(12):787–793. doi: 10.1097/00004770-200312000-00001. [DOI] [PubMed] [Google Scholar]
- 10.Farzaneh M, Abitbol S, Lawrence HP, Friedman S. Toronto Study. Treatment outcome in endodontics: the Toronto Study, phase II—initial treatment. J Endod. 2004;30(5):302–309. doi: 10.1097/00004770-200405000-00002. [DOI] [PubMed] [Google Scholar]
- 11.Marquis VL, Dao T, Farzaneh M, Abitbol S, Friedman S. Treatment outcome in endodontics: the Toronto Study, phase III—initial treatment. J Endod. 2006;32(4):299–306. doi: 10.1016/j.joen.2005.10.050. [DOI] [PubMed] [Google Scholar]
- 12.de Chevigny C, Dao TT, Basrani BR, et al. Treatment outcome in endodontics: the Toronto Study, phase 4—initial treatment (published online ahead of print Dec. 21,2007) J Endod. 2008;34(3):258–263. doi: 10.1016/j.joen.2007.10.017. [DOI] [PubMed] [Google Scholar]
- 13.Ng YL, Mann V, Gulabivala K. Tooth survival following non-surgical root canal treatment: a systematic review of the literature. Int Endod J. 2010;43(3):171–189. doi: 10.1111/j.1365-2591.2009.01671.x. [DOI] [PubMed] [Google Scholar]
- 14.Hannahan JP, Eleazer PD. Comparison of success of implants versus endodontically treated teeth (published online ahead of print Sept. 19, 2008) J Endod. 2008;34(11):1302–1305. doi: 10.1016/j.joen.2008.08.011. [DOI] [PubMed] [Google Scholar]
- 21.Ng YL, Mann V, Rahbaran S, Lewsey J, Gulabivala K. Outcome of primary root canal treatment: systematic review of the literature, part 2: influence of clinical factors (published online ahead of print Oct. 10, 2007) Int Endod J. 2008;41(1):6–31. doi: 10.1111/j.1365-2591.2007.01323.x. [DOI] [PubMed] [Google Scholar]
- 15.Kojima K, Inamoto K, Nagamatsu K, et al. Success rate of endodontic treatment of teeth with vital and nonvital pulps: a meta-analysis. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2004;97(1):95–99. doi: 10.1016/j.tripleo.2003.07.006. [DOI] [PubMed] [Google Scholar]
- 16.Swartz DB, Skidmore AE, Griffin JA., Jr Twenty years of endodontic success and failure. J Endod. 1983;9(5):198–202. doi: 10.1016/S0099-2399(83)80092-2. [DOI] [PubMed] [Google Scholar]
- 17.Smith CS, Setchell DJ, Harty FJ. Factors influencing the success of conventional root canal therapy: a five-year retrospective study. Int Endod J. 1993;26(6):321–333. doi: 10.1111/j.1365-2591.1993.tb00765.x. [DOI] [PubMed] [Google Scholar]
- 18.Hoskinson SE, Ng YL, Hoskinson AE, Moles DR, Gulabivala K. A retrospective comparison of outcome of root canal treatment using two different protocols. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2002;93(6):705–715. doi: 10.1067/moe.2001.122822. [DOI] [PubMed] [Google Scholar]
- 19.Cheung GS. Survival of first-time nonsurgical root canal treatment performed in a dental teaching hospital. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2002;93(5):596–604. doi: 10.1067/moe.2002.120254. [DOI] [PubMed] [Google Scholar]
- 20.Benenati FW, Khajotia SS. A radiographic recall evaluation of 894 endodontic cases treated in a dental school setting. J Endod. 2002;28(5):391–395. doi: 10.1097/00004770-200205000-00011. [DOI] [PubMed] [Google Scholar]
- 22.Tilashalski KR, Gilbert GH, Boykin MJ, Shelton BJ. Root canal treatment in a population-based adult sample: status of teeth after endodontic treatment. J Endod. 2004;30(8):577–581. doi: 10.1097/01.don.0000125874.80753.f3. [DOI] [PubMed] [Google Scholar]
- 23.Gilbert GH, Tilashalski KR, Litaker MS, McNeal SF, Boykin MJ, Kessler AW DPBRN Collaborative Group. Outcomes of root canal treatment in Dental Practice-Based Research Network practices. Gen Dent. 2010;58(1):28–36. [PMC free article] [PubMed] [Google Scholar]