Abstract
Objective
Several studies have examined the relationships between dietary potassium and sodium and hypertension, but few have evaluated the association between serum potassium or sodium and risk of incident hypertension. We therefore investigated the associations between serum potassium and sodium and risk of incident hypertension in a Chinese community-based population.
Methods
A total of 839 normotensive individuals without cardiovascular disease from the Chinese Multi-Provincial Cohort Study who took part in the baseline examination in 2007–2008 and the follow-up survey in 2012–2013 were included in this study. Odds ratios (OR) and 95% confidence intervals (95%CI) for baseline serum potassium and sodium in relation to the risk of new-onset hypertension were evaluated using multivariate logistic regression models.
Results
During five years of follow-up, 218 (26.0%) individuals progressed to hypertension. Logistic regression adjusting for multiple confounders showed that every 1 mEq/L increment in baseline serum potassium level was associated with a 75% increased risk of hypertension (OR: 1.75; 95%CI: 1.01–3.04; P = 0.04). Compared with adults with serum potassium level of 4.20–4.79 mEq/L, adults with level ≥ 4.80 mEq/L had an 84% increased risk of hypertension (OR: 1.84; 95%CI: 1.14–2.96; P = 0.01). There was no significant association between serum sodium and risk of hypertension (OR: 0.96; 95%CI: 0.89–1.04; P = 0.33).
Conclusions
Baseline serum potassium level, but not baseline serum sodium level, was positively related to the risk of incident hypertension in the Chinese population.
Keywords: Hypertension, Potassium, Serum, Sodium
1. Introduction
Hypertension is recognized as a major risk factor for cardiovascular disease (CVD), and represents a worldwide public health challenge. Known risk factors for hypertension include genetic and environmental factors, such as family history, age, unhealthy diet, overweight, reduced physical activity, and excess alcohol intake.[1],[2] Although previous studies have shown that inadequate intake of potassium or excess intake of sodium may elevate blood pressure, the associations between dietary potassium and sodium and blood pressure in normotensive participants remain unclear. A meta-analysis performed by Aburto et al.[3] in 2013 analyzed data from 22 randomized controlled trials and concluded that potassium supplementation did not lower blood pressure in individuals with normal blood pressure. However, Zhang, et al.[4] reported that higher sodium and lower potassium consumption were associated with hypertension. Another cross-sectional study by Sharma, et al.[5] indicated that dietary potassium and sodium were not associated with elevated blood pressure in individuals with no prior history of hypertension.
However, dietary potassium and sodium do not necessarily reflect their levels in extracellular fluids. Serum potassium and sodium represent the internal environment of the body, and play an important role in the regulation of blood pressure.[6],[7] Existing studies rarely investigate the associations between serum potassium and sodium and hypertension, and the results are sometimes conflicting. The Framingham Heart Study suggested that serum potassium level ≥ 5.2 mEq/L or ≤ 4.0 mEq/L may increase the risk of hypertension, though the association was not significant, and serum sodium level was not related to hypertension.[8],[9] The NHANES and British Regional Heart Study suggested that elevated serum potassium level increased CVD mortality.[10],[11] A cross-sectional study conducted by Kesteloot and Joossens revealed that serum potassium and sodium levels were negatively related to blood pressure.[12]
Increased dietary intake of potassium and sodium may subsequently increase potassium and sodium levels in blood.[13]–[16] The safety of salt substitutes containing potassium chloride needs to be evaluated if higher serum potassium may increase the risk of hypertension or other diseases.
This study aimed to evaluate the associations between serum potassium and sodium levels and risk of incident hypertension during a 5-year follow-up period in a community-based population of Chinese adults without diagnosed hypertension.
2. Methods
2.1. Study population
The study population was recruited from the large Chinese Multi-Provincial Cohort Study (CMCS) in the Beijing, China. The design and selection criteria of the CMCS have been described previously.[17] We selected participants who had took part in the baseline examination at 2007–2008 and follow-up survey at 2012–2013 in Beijing as the baseline population (n = 1991). Participants who were lack of blood pressure (n = 5) or baseline potassium or sodium levels (n = 66), or who had CVD (n = 56) or hypertension (n = 1023), or with an estimated glomerular filtration rate (eGFR) < 60 (n = 2) were excluded. A total of 839 participants were thus finally included in the study.
The study protocol was approved by the Ethics Committee of Beijing Anzhen Hospital, Capital Medical University and all participants provided written informed consent.
2.2. Risk factor measurements
Baseline and follow-up surveys of CVD risk factors were based on the WHO-MONICA project.[18] All investigators in the surveys had been properly trained according to the WHO-MONICA research protocol. Data were recorded using a standardized questionnaire including age, sex, smoking status, alcohol consumption, physical activity and medical history. Current smoking was defined as at least one cigarette per day in the past year. Alcohol consumption was defined as drinking more than three times a week. Physical activity was categorized as no activity, occasional activity (exercise 1-2 sessions a week lasting on average 30 min per session) and regular activity (exercise more than 3 sessions a week lasting on average 30 min per session).
Physical examinations included measurements of height, weight and blood pressure. Blood pressure was measured on the right arm using a standard electronic sphygmomanometer (OMRON, HEM-770A, Japan) with the participant seated quietly for at least 5 min. The mean value of three consecutive readings (an interval of 30 s) was used both at the baseline and the follow-up surveys. Hypertension was defined as a mean systolic blood pressure ≥= 140 mmHg, and/or a mean diastolic blood pressure ≥ 90 mmHg, and/or taking antihypertensive medication.[19] Optimal blood pressure was defined as a mean systolic blood pressure < 120 mmHg and a mean diastolic blood pressure < 80 mmHg. Normal blood pressure was defined as a mean systolic blood pressure of 120–129 mmHg and a mean diastolic blood pressure of 80–84 mmHg. Pre-hypertension was defined as a mean systolic blood pressure of 130–139 mmHg and a mean diastolic blood pressure of 85–89 mmHg. The new-onset hypertension was defined as normotensive at baseline examination and progressed to hypertension in the follow-up survey. Body mass index (BMI) was calculated as the weight in kilograms divided by the square of the height in meters. The eGFR was calculated according to the modification of diet in renal disease.[20] Diabetes mellitus was defined as fasting blood glucose ≥ 126 mg/dL (7.0 mmol/L) or the use of antidiabetic drugs.
Overnight fasting venous blood samples were collected for the measurements of serum glucose, blood lipid, albumin, creatinine, insulin and electrolyte concentrations. Serum potassium and sodium levels were measured by the ion-selective electrode method.[21] Fasting blood glucose and creatinine were measured by enzymatic methods. High-density lipoprotein and low-density lipoprotein were measured by homogeneous assay. Fasting insulin was measured using a microparticle enzyme immunoassay and albumin level was measured by the bromocresol green method. Quality control of laboratory tests was performed by the WHO Regional Lipid Reference Center.[22]
2.3. Statistical analysis
With the actual sample size of 839, hypertension incidence of 26.0%, α of 5% and statistical power of 80%, we can test a statistically significant association if the odds ratios were lower than 0.79 or higher than 1.27 with serum potassium or sodium levels as continuous variables or if the odds ratios were lower than 0.51 or higher than 1.74 with serum potassium or sodium levels as categorical variables.
Serum potassium and sodium levels were expressed as means ± SD. Categorical variables were presented as percent (%). For comparison, serum potassium level was classified into five groups according to 0.20 mEq/L intervals (< 4.20 mEq/L, 4.20–4.39 mEq/L, 4.40–4.59 mEq/L, 4.60– 4.79 mEq/L and ≥ 4.80 mEq/L). Serum sodium was classified into five groups according to 1 mEq/L intervals (< 140, 141, 142, 143, and ≥ 144 mEq/L). The incidence of hypertension was calculated according to baseline serum potassium and sodium levels, classified as above. Univariate and multivariate logistic regression models were used to evaluate the associations between baseline serum potassium and sodium levels and risk of incident hypertension. The multivariate model was adjusted for factors that may affect blood pressure or serum potassium and sodium including age, sex, BMI, systolic blood pressure, high-density lipoprotein (HDL-C), low-density lipoprotein (LDL-C), insulin, albumin, eGFR, diabetes mellitus, smoking, alcohol consumption, physical activity, family history of hypertension, and levels of serum calcium and magnesium ions. The associations between baseline potassium and sodium and the incidence of hypertension were expressed as OR and 95% confidence intervals (95%CI). Potential increased risk for hypertension with higher or lower serum potassium and sodium levels was further assessed by combining the second, third and fourth groups as reference groups.
We tested for interactions between serum potassium and sodium and sex, BMI, smoking, alcohol consumption, diabetes, and physical activity by including the interaction terms in the logistic models. P < 0.05 was considered statistically significant and analyses were identified as two-tailed. Data were analyzed using Statistical Package for the Social Sciences (SPSS) version 20.0 (SPSS Inc., Chicago, IL, USA).
3. Results
A total of 839 participants were included in the analysis, including 300 men (35.8%) and 539 women (64.2%), aged 45–79 years. The mean baseline serum potassium and sodium levels were 4.47 ± 0.35 mEq/L and 142.67 ± 2.64 mEq/L, respectively. A total of 3.8% of participants had serum potassium level above the normal range (normal: 3.5–5.1 mEq/L), while 0.8% and 6.7% had lower and higher serum sodium level, respectively (normal: 136–146 mEq/L).
The baseline serum potassium and sodium levels according to the different characteristics of the study population are presented in Table 1. Serum potassium level was higher in smokers (P < 0.01), participants with more physical activity (P < 0.01) and participants with lower eGFR (P < 0.01). Serum sodium level was higher in younger individuals (P = 0.01), and those with lower eGFR (P < 0.001).
Table 1. Baseline serum potassium and sodium levels of participants.
| Characteristics | Total, n = 839 |
Men, n = 300 |
Women, n = 539 |
||||||||
| Potassium, mEq/L | Sodium, mEq/L | n | Potassium, mEq/L | Sodium, mEq/L | n | Potassium, mEq/L | Sodium, mEq/L | n | |||
| Age, years | |||||||||||
| 45−59 | 4.47 ± 0.33 | 142.85 ± 2.72 | 508 | 4.48 ± 0.33 | 142.37 ± 2.49 | 142 | 4.47 ± 0.34 | 143.03 ± 2.78 | 366 | ||
| 60−69 | 4.48 ± 0.34 | 142.62 ± 2.48 | 225 | 4.44 ± 0.33 | 142.53 ± 2.64 | 96 | 4.51 ± 0.35 | 142.68 ± 2.37 | 129 | ||
| 70−79 | 4.46 ± 0.40 | 142.02 ± 2.43 | 106 | 4.47 ± 0.42 | 141.77 ± 2.72 | 62 | 4.46 ± 0.37 | 142.36 ± 1.93 | 44 | ||
| P | 0.92 | 0.01 | 0.63 | 0.18 | 0.45 | 0.16 | |||||
| BMI, kg/m2 | |||||||||||
| < 24 | 4.46 ± 0.37 | 142.53 ± 2.55 | 414 | 4.44 ± 0.35 | 142.15 ± 2.51 | 135 | 4.47 ± 0.37 | 142.71 ± 2.55 | 279 | ||
| ≥ 24 | 4.49 ± 0.32 | 142.83 ± 2.71 | 425 | 4.48 ± 0.35 | 142.42 ± 2.66 | 165 | 4.49 ± 0.31 | 143.09 ± 2.71 | 260 | ||
| P | 0.30 | 0.10 | 0.28 | 0.37 | 0.59 | 0.09 | |||||
| Smoking | |||||||||||
| Yes | 4.57 ± 0.35 | 142.29 ± 2.74 | 105 | 4.56 ± 0.34 | 142.20 ± 4.56 | 97 | 4.67 ± 0.38 | 143.38 ± 2.07 | 8 | ||
| No | 4.46 ± 0.34 | 142.74 ± 2.61 | 734 | 4.42 ± 0.34 | 142.34 ± 2.51 | 203 | 4.48 ± 0.34 | 142.89 ± 2.64 | 531 | ||
| P | < 0.01 | 0.10 | < 0.01 | 0.64 | 0.11 | 0.60 | |||||
| Alcohol consumption | |||||||||||
| Yes | 4.47 ± 0.35 | 142.70 ± 2.64 | 770 | 4.45 ± 0.35 | 142.28 ± 2.61 | 236 | 4.48 ± 0.34 | 142.89 ± 2.63 | 534 | ||
| No | 4.52 ± 0.33 | 142.48 ± 2.58 | 69 | 4.52 ± 0.34 | 142.38 ± 2.57 | 64 | 4.48 ± 0.12 | 143.80 ± 2.59 | 5 | ||
| P | 0.24 | 0.51 | 0.13 | 0.79 | 0.99 | 0.44 | |||||
| Physical activity | |||||||||||
| No activity | 4.43 ± 0.38 | 142.43 ± 2.72 | 102 | 4.43 ± 0.38 | 141.65 ± 2.72 | 31 | 4.43 ± 0.39 | 142.78 ± 2.66 | 71 | ||
| Occasional activity | 4.45 ± 0.33 | 142.71 ± 2.74 | 479 | 4.42 ± 0.32 | 142.25 ± 2.59 | 174 | 4.47 ± 0.34 | 142.98 ± 2.79 | 305 | ||
| Regular activity | 4.53 ± 0.34 | 142.72 ± 2.40 | 258 | 4.57 ± 0.38 | 142.59 ± 2.54 | 95 | 4.51 ± 0.32 | 142.79 ± 2.31 | 163 | ||
| P | < 0.01 | 0.60 | < 0.01 | 0.20 | 0.30 | 0.72 | |||||
| Diabetes | |||||||||||
| Yes | 4.47 ± 0.35 | 142.73 ± 2.62 | 761 | 4.46 ± 0.35 | 142.35 ± 2.57 | 264 | 4.48 ± 0.35 | 142.94 ± 2.63 | 497 | ||
| No | 4.50 ± 0.31 | 142.17 ± 2.72 | 78 | 4.50 ± 0.32 | 141.89 ± 2.75 | 36 | 4.50 ± 0.31 | 142.40 ± 2.70 | 42 | ||
| P | 0.45 | 0.07 | 0.49 | 0.32 | 0.67 | 0.21 | |||||
| BP category | |||||||||||
| Optimal | 4.44 ± 0.33 | 4.44 ± 0.33 | 277 | 4.46 ± 0.33 | 4.46 ± 0.33 | 77 | 4.44 ± 0.33 | 4.44 ± 0.33 | 200 | ||
| Normal | 4.50 ± 0.35 | 4.50 ± 0.35 | 270 | 4.48 ± 0.39 | 4.48 ± 0.39 | 99 | 4.51 ± 0.32 | 4.51 ± 0.32 | 171 | ||
| Pre-hypertension | 4.48 ± 0.36 | 4.48 ± 0.36 | 292 | 4.46 ± 0.33 | 4.46 ± 0.33 | 124 | 4.50 ± 0.37 | 4.50 ± 0.37 | 168 | ||
| P | 0.20 | 0.80 | 0.88 | 0.94 | 0.13 | 0.67 | |||||
| eGFR, 60 mL/min per 1.73 m2 | |||||||||||
| < 80 | 4.55 ± 0.41 | 143.71 ± 3.01 | 79 | 4.54 ± 0.43 | 143.38 ± 2.67 | 45 | 4.56 ± 0.38 | 144.15 ± 3.39 | 34 | ||
| 80−120 | 4.49 ± 0.34 | 142.83 ± 2.48 | 602 | 4.46 ± 0.34 | 142.31 ± 2.50 | 229 | 4.50 ± 0.35 | 143.14 ± 2.42 | 373 | ||
| > 120 | 4.39 ± 0.30 | 141.60 ± 2.67 | 158 | 4.38 ± 0.29 | 140.27 ± 2.09 | 26 | 4.39 ± 0.31 | 141.86 ± 2.70 | 132 | ||
| P | < 0.01 | < 0.001 | 0.18 | < 0.001 | < 0.01 | < 0.001 | |||||
Values are means and standard deviations. BMI: body mass index; BP: blood pressure; eGFR: estimated glomerular filtration rate.
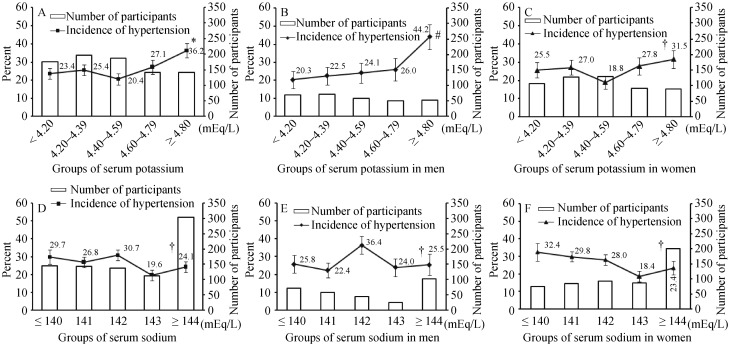
Among the 839 participants, 218 (26.0%, 80 men) developed hypertension during the 5-year follow-up period. There was no statistical difference between sexes (P = 0.74), of the cumulative incidences of hypertension, with 26.7% in men and 25.6% in women. The cumulative incidence rates of new-onset hypertension according to baseline serum potassium and sodium groups are presented in Figure 1. The incidence of hypertension was highest in the group of serum potassium ≥ 4.80 mEq/L and lowest in the group of serum potassium of 4.40–4.59 mEq/L in the whole population and the females, and the incidence of hypertension rises with the increase of serum potassium levels in males. Although the incidence of hypertension was highest in the group of serum sodium of 142 mEq/L in the whole population and the males, the incidence of hypertension decreased with the increase of serum sodium levels in females. The P for trends of incident hypertension was 0.02 for serum potassium and 0.10 for serum sodium.
Figure 1. Incidence of hypertension according to baseline serum potassium or sodium levels.
(A): Incidence of hypertension for all study subjects according to baseline serum potassium; (B): Incidence of hypertension in men according to baseline serum potassium; (C): Incidence of hypertension in women according to baseline serum potassium; (D): Incidence of hypertension for all study subjects according to baseline serum sodium; (E): Incidence of hypertension in men according to baseline serum sodium; (F): Incidence of hypertension in women according to baseline serum sodium. Error bars represent standard errors. *P for trends = 0.021. #P for trends = 0.006. †P for trends > 0.05.
Baseline serum potassium level was positively associated with the risk of hypertension when analyzed as a continuous variable in univariate analysis (OR: 1.86; 95%CI: 1.20–2.90; P < 0.01) and in multivariate analysis (OR: 1.75; 95%CI: 1.01–3.04; P = 0.04). However, there was no significant association between baseline serum sodium level and risk of hypertension in either univariate analysis (OR: 0.98; 95%CI: 0.92–1.04; P = 0.41) or multivariate analysis (OR: 0.96; 95%CI: 0.89–1.04; P = 0.33) (Table 2). The highest category of serum potassium (≥ 4.80 mEq/L) was positively associated with risk of hypertension compared with the reference group (OR: 1.84; 95%CI: 1.14–2.96; P = 0.01), and there was a non-significant increase in risk of hypertension in the lowest serum-potassium group (< 4.20 mEq/L) compared with the reference group (OR: 1.06; 95%CI, 0.66–1.70; P = 0.81). Neither the lowest nor the highest category of serum sodium was significantly associated with risk of hypertension (Table 2).
Table 2. Baseline serum potassium and sodium levels and risk of incident hypertension.
| No. at risk | No. of hypertension, n (%) | Non-adjusted |
Fully-adjusted* |
||||
| OR (95%CI) | P | OR (95%CI) | P | ||||
| Potassium, mEq/L | |||||||
| Continuous variable | 839 | 218 (26.0) | 1.86 (1.20−2.90) | < 0.01 | 1.75 (1.01−3.04) | 0.04 | |
| Categorical variable | |||||||
| < 4.20 | 175 | 41 (23.4) | 0.96 (0.64−1.44) | 0.86 | 1.06 (0.66−1.70) | 0.81 | |
| 4.20−4.79 | 523 | 126 (24.1) | 1.00 | 1.00 | |||
| ≥ 4.80 | 141 | 51 (36.2) | 1.79 (1.20−2.66) | < 0.01 | 1.84 (1.14−2.96) | 0.01 | |
| Sodium, mEq/L | |||||||
| Continuous variable | 839 | 218 (26.0) | 0.98 (0.92−1.04) | 0.41 | 0.96 (0.89−1.04) | 0.33 | |
| Categorical variable | |||||||
| < 141 | 145 | 43 (29.7) | 1.19 (0.78−1.82) | 0.41 | 1.11 (0.67−1.85) | 0.68 | |
| 141−143 | 391 | 102 (26.1) | 1.00 | 1.00 | |||
| ≥ 144 | 303 | 73 (24.1) | 0.90 (0.64−1.27) | 0.55 | 0.82 (0.54−1.26) | 0.37 | |
*Adjusted for age, sex, body mass index, systolic blood pressure, high-density lipoprotein, low-density lipoprotein, eGFR, albumin, diabetes mellitus, smoking, alcohol consumption, physical activity, family history of hypertension, serum calcium and magnesium levels. We further adjusted for serum sodium level when analyzing the relationship between serum potassium and hypertension, and further adjusted for serum potassium level when analyzing the relationship between serum sodium and hypertension.
We found no significant interactions between serum potassium or sodium levels and selected covariates (P > 0.05). Other risk factors for hypertension included BMI (OR: 1.09; 95%CI, 1.02–1.16; P = 0.01), systolic blood pressure (OR: 1.12; 95%CI, 1.09–1.14; P < 0.001) and family history of hypertension (OR: 1.60; 95%CI: 1.11–2.31; P = 0.01) at baseline.
4. Discussion
Individuals in this Chinese, community-based cohort study showed interindividual variations in serum potassium and sodium levels. Baseline serum potassium level was positively associated with the risk of incident hypertension (OR: 1.75; 95%CI: 1.01–3.04; P = 0.04) after adjusting for potential confounding factors. In contrast, there was no significant association between baseline serum sodium level and hypertension risk (OR: 0.96; 95%CI: 0.89–1.04; P = 0.33).
As far as we know, there are few epidemiological studies investigating the association between serum potassium level and hypertension with only one cohort study among them.[9] The Framingham Heart Study found that adults with serum potassium ≥ 5.2 mEq/L had increased risk of hypertension, though the difference was not significant.[9] Higher serum potassium level was also associated with increased risk of CVD. The results of Fang, et al.[11] suggested that there was an increase in CVD mortality among the population with serum potassium ≥ 4.5 mEq/L, after adjusting for other CVD risk factors. Wannamethee, et al.[10] reported an increase in mortality risk of 70% in male smokers with serum potassium ≥ 5.2 mEq/L. The results of cross-sectional and case-control studies of serum potassium and hypertension were not consistent with our study. Kesteloot, et al.[12], Pikilidou, et al.[23] and Rinner, et al.[24] found that serum potassium level was negatively associated with blood pressure. Hu, et al.[6] suggested that serum potassium level was lower in hypertension group compared with non-hypertension group. However, it is insufficient to infer causality of serum potassium level on future risk of hypertension based on results from cross-sectional and case-control studies.
We found an 84% increased risk of hypertension in individuals with baseline serum potassium level ≥ 4.80 mEq/L compared with level of 4.20–4.79 mEq/L, in accordance with the trend shown by Framingham Heart Study.[9] Our study was similar to that of the Framingham Heart Study with respect to follow-up years, but the participants in our study were older. In addition, the Framingham Heart Study excluded participants with creatinine levels ≥ 2.0 mg/dL and potassium levels > 6.3 mEq/L, however, all participants had creatinine levels < 2.0 mg/dL and potassium levels ≤ 6.3 mEq/L in our study. We excluded individuals with eGFR < 60 mL/min per 1.73 m2 and adjusted for eGFR in multivariate analyses, given that renal function may influence serum potassium and sodium levels.
There was no significant association between baseline serum sodium level and risk of hypertension, which was consistent with Framingham Heart Study.[8] While a cross-sectional study from Kesteloot, et al.[12] found a negative correlation between serum sodium level and blood pressure. And Hu, et al.[6] found no significant difference in serum sodium level between hypertension and non-hypertension groups.
Potassium and sodium play important roles in the maintenance of cellular functions, and raised or lowered serum potassium level may be harmful to health.[25] Our results found that elevated serum potassium could increase the risk of hypertension. The physiological mechanisms by which higher serum potassium level increase hypertension risk are not fully understood. Renal function may affect the level of serum potassium,[25] however, the association was not altered after adjusting for eGFR in multivariate analysis. This indicated that the association between serum potassium and hypertension risk was independent of renal function. Our study found no association between serum sodium and risk of hypertension. The regulation of blood pressure by sodium may be based on dietary intake and renal excretion, independent of serum sodium level.[8] In addition, it is important to note that the incidence of hypertension may be affected by other unknown risk factors that may affect serum potassium and sodium levels.
Increased dietary intake of potassium and sodium may subsequently increase potassium and sodium levels in blood.[13],[14],[26] The Atherosclerosis Risk in Communities (ARIC) Study[26] measured the dietary and serum potassium levels in 12,209 participants, and showed that serum potassium level was higher in the group of high potassium intake. In this study, serum potassium level was divided into 4 groups < 4.0, 4.0–4.5, 4.5–5.0 and 5.0–5.5 mEq/L, and the dietary potassium intake were 1.63 ± 0.43, 1.65 ± 0.42, 1.68 ± 0.41 and 1.70 ± 0.41 mg/kcal (P < 0.01), respectively. Another research among normotensive individuals showed that with the salt intake from 10 mmol/day increased to 250 mmol/day, plasma sodium levels changed from 138.5 ± 0.7 mmol/day to 141.5 ± 1.1 mmol/day.[14]
Salt substitute containing 25% potassium chloride, 65% sodium chloride and 10% magnesium sulfate to replace 100% sodium chloride are currently used in China to reduce sodium intake and increase potassium intake.[27] However, our results suggested that an increase in serum potassium might also increase the risk of hypertension. Individuals with normal blood pressure who use such salt substitute over a long period may thus be at increased risk of hypertension. In fact, the results from studies with health outcomes were insufficient to draw a conclusion whether low sodium intake is associated with an increased or reduced risk of CVD in general population.[28]–[30] Further studies on the safety of long-term intake of salt substitute are therefore required.
There were several limitations to our study. First, our study based on the Chinese population and the results may therefore not be applicable to other populations. Second, baseline levels of serum potassium and sodium cannot represent the values of serum potassium and sodium throughout the study period. Third, our study may have insufficient statistical power to detect a relatively modest association between serum sodium and hypertension. In addition, we cannot get more details about other variables such as heart function and the quantitative data of alcohol consumption. Additional cohort studies with larger sample size and which monitor 24-h potassium and sodium excretion as well as potassium and sodium levels in blood may be necessary.
This study was among the few cohort studies to investigate the relationships between serum potassium and sodium levels and the risk of hypertension in normotensive adults. In conclusion, the results of this community-based study indicated that elevated serum potassium level might increase the risk of incident hypertension, while serum sodium level was unrelated to hypertension risk. These findings suggested that potassium might not always be beneficial in terms of reducing the risk of hypertension. However, further studies with larger sample size and wider age ranges are needed to clarify the relationships between serum potassium and sodium and the risk of hypertension.
Acknowledgments
This work was supported by a grant from the National Program on Key Basic Research Project of China (2012CB517806, Zhi-Ming ZHU) and the Key Laboratory of Remodeling-related Cardiovascular Diseases, Beijing Anzhen Hospital, Capital Medical University, Ministry of Education, Beijing, China. The sponsor had no role in the design and conduct of the study. The authors declared no conflict of interest.
References
- 1.Chobanian AV, Bakris GL, Black HR, et al. Seventh report of the Joint National Committee on Prevention, detection, evaluation, and treatment of high blood rressure. Hypertension. 2003;42:1206–1252. doi: 10.1161/01.HYP.0000107251.49515.c2. [DOI] [PubMed] [Google Scholar]
- 2. World Health Organization A global brief on hypertension. Silent killer, global public health crisis 2013. World Health Organization Web site. http://www.who.int/cardiovascular_diseases/publications/global_brief_hypertension/en/ (accessed April 2013)
- 3.Aburto NJ, Hanson S, Gutierrez H, et al. Effect of increased potassium intake on cardiovascular risk factors and disease: systematic review and meta-analyses. BMJ. 2013;346:f1378. doi: 10.1136/bmj.f1378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Zhang Z, Cogswell ME, Gillespie C, et al. Association between usual sodium and potassium intake and blood pressure and hypertension among U.S. adults: NHANES 2005–2010. PLoS One. 2013;8:e75289. doi: 10.1371/journal.pone.0075289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Sharma S, McFann K, Chonchol M, et al. Dietary sodium and potassium intake is not associated with elevated blood pressure in US adults with no prior history of hypertension. J Clin Hypertens (Greenwich) 2014;16:418–423. doi: 10.1111/jch.12312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hu G, Xu X, Liang X, et al. Associations of plasma atrial natriuretic peptide and electrolyte levels with essential hypertension. Exp Ther Med. 2013;5:1439–1443. doi: 10.3892/etm.2013.991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Carlos MI. Calcium, hypertension and target organ damage: from prevention to regression. Rev Latinoam Hiperte. 2007;2:24–28. [Google Scholar]
- 8.Lago RM, Pencina MJ, Wang TJ, et al. Interindividual variation in serum sodium and longitudinal blood pressure tracking in the Framingham Heart Study. J Hypertens. 2008;26:2121–2125. doi: 10.1097/HJH.0b013e32830fe4a5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Walsh CR, Larson MG, Vasan RS, et al. Serum potassium is not associated with blood pressure tracking in the Framingham Heart Study. Am J Hypertens. 2002;15:130–136. doi: 10.1016/s0895-7061(01)02293-2. [DOI] [PubMed] [Google Scholar]
- 10.Wannamethee SG, Lever AF, Shaper AG, et al. Serum potassium, cigarette smoking, and mortality in middle-aged men. Am J Epidemiol. 1997;145:598–606. doi: 10.1093/oxfordjournals.aje.a009156. [DOI] [PubMed] [Google Scholar]
- 11.Fang J, Madhavan S, Cohen H, et al. Serum potassium and cardiovascular mortality. J Gen Intern Med. 2000;15:885–890. doi: 10.1046/j.1525-1497.2000.91021.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kesteloot H, Joossens JV. Relationship of serum sodium, potassium, calcium, and phosphorus with blood pressure. Belgian Interuniversity Research on Nutrition and Health. Hypertension. 1988;12:589–593. doi: 10.1161/01.hyp.12.6.589. [DOI] [PubMed] [Google Scholar]
- 13.de Wardener HE, He FJ, MacGregor GA. Plasma sodium and hypertension. Kidney Int. 2004;66:2454–2466. doi: 10.1111/j.1523-1755.2004.66018.x. [DOI] [PubMed] [Google Scholar]
- 14.He FJ, Markandu ND, Sagnella GA, et al. Plasma sodium: ignored and underestimated. Hypertension. 2005;45:98–102. doi: 10.1161/01.HYP.0000149431.79450.a2. [DOI] [PubMed] [Google Scholar]
- 15.Overlack A, Conrad H, Stumpe KO. The influence of oral potassium citrate/bicarbonate on blood pressure in essential hypertension during unrestricted salt intake. Klin Wochenschr. 1991;69:79–83. [PubMed] [Google Scholar]
- 16.Siani A, Strazzullo P, Russo L, et al. Controlled trial of long term oral potassium supplements in patients with mild hypertension. Br Med J (Clin Res Ed) 1987;294:1453–1456. doi: 10.1136/bmj.294.6585.1453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Liu J, Hong Y, D'Agostino RB, Sr, et al. Predictive value for the Chinese population of the Framingham CHD risk assessment tool compared with the Chinese Multi-Provincial Cohort Study. JAMA. 2004;291:2591–2599. doi: 10.1001/jama.291.21.2591. [DOI] [PubMed] [Google Scholar]
- 18.Wu Z, Yao C, Zhao D, et al. Sino-MONICA project: a collaborative study on trends and determinants in cardiovascular diseases in China, Part i: morbidity and mortality monitoring. Circulation. 2001;103:462–468. doi: 10.1161/01.cir.103.3.462. [DOI] [PubMed] [Google Scholar]
- 19.Liu LS. 2010 Chinese guidelines for the management of hypertension. Zhonghua Xin Xue Guan Bing Za Zhi. 2011;39:579–615. [PubMed] [Google Scholar]
- 20.Zhang L, Wang F, Wang L, et al. Prevalence of chronic kidney disease in China: a cross-sectional survey. Lancet. 2012;379:815–822. doi: 10.1016/S0140-6736(12)60033-6. [DOI] [PubMed] [Google Scholar]
- 21.Worth HG. A comparison of the measurement of sodium and potassium by flame photometry and ion-selective electrode. Ann Clin Biochem. 1985;22:343–350. doi: 10.1177/000456328502200402. [DOI] [PubMed] [Google Scholar]
- 22.Liu J, Wang W, Wang M, et al. Impact of diabetes, high triglycerides and low HDL cholesterol on risk for ischemic cardiovascular disease varies by LDL cholesterol level: a 15-year follow-up of the Chinese Multi-provincial Cohort Study. Diabetes Res Clin Pract. 2012;96:217–224. doi: 10.1016/j.diabres.2011.12.018. [DOI] [PubMed] [Google Scholar]
- 23.Pikilidou MI, Lasaridis AN, Sarafidis PA, et al. Blood pressure and serum potassium levels in hypertensive patients receiving or not receiving antihypertensive treatment. Clin Exp Hypertens. 2007;29:563–573. doi: 10.1080/10641960701744103. [DOI] [PubMed] [Google Scholar]
- 24.Rinner MD, Spliet-van Laar L, Kromhout D. Serum sodium, potassium, calcium and magnesium and blood pressure in a Dutch population. J Hypertens. 1989;7:977–981. doi: 10.1097/00004872-198912000-00008. [DOI] [PubMed] [Google Scholar]
- 25.Foringer JR, Norris C, Finkel KW. In: Evidence-Based Nephrology. Molony DA, Craig JC, editors. Blackwell Publishing Ltd; 2008. pp. Chapter 56; 633–641. [Google Scholar]
- 26.Chatterjee R, Yeh HC, Shafi T, et al. Serum and dietary potassium and risk of incident type 2 diabetes mellitus: The Atherosclerosis Risk in Communities (ARIC) study. Arch Intern Med. 2010;170:1745–1751. doi: 10.1001/archinternmed.2010.362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.China Salt Substitute Study Collaborative Group Salt substitution: a low-cost strategy for blood pressure control among rural Chinese. A randomized, controlled trial. J Hypertens. 2007;25:2011–2018. doi: 10.1097/HJH.0b013e3282b9714b. [DOI] [PubMed] [Google Scholar]
- 28.Oparil S. Low sodium intake—cardiovascular health benefit or risk? N Engl J Med. 2014;371:677–679. doi: 10.1056/NEJMe1407695. [DOI] [PubMed] [Google Scholar]
- 29.Stolarz-Skrzypek K, Kuznetsova T, Thijs L, et al. Fatal and nonfatal outcomes, incidence of hypertension, and blood pressure changes in relation to urinary sodium excretion. JAMA. 2011;305:1777–1785. doi: 10.1001/jama.2011.574. [DOI] [PubMed] [Google Scholar]
- 30.O'Donnell MJ, Yusuf S, Mente A, et al. Urinary sodium and potassium excretion and risk of cardiovascular events. JAMA. 2011;306:2229–2238. doi: 10.1001/jama.2011.1729. [DOI] [PubMed] [Google Scholar]