Abstract
Aims
To determine the effectiveness of Motivational Enhancement Therapy (MET) for hazardous drinkers in Primary Care Unit (PCU) settings in rural Thailand.
Methods
A randomized controlled trial was conducted in eight PCUs in Ubonratchatanee and Chachoengsao provinces in Thailand. Hazardous drinkers were identified using the World Health Organization-recommended Alcohol Use Disorder Identification Test. Of 117 eligible participants (91% male), 59 were randomized to the intervention group to receive MET in three individual appointments with a trained nurse and 58 to an assessment-only control group. Outcome evaluations were carried out after 6 weeks, 3 months and 6 months.
Results
Follow-up data were available on 84, 94 and 91% of subjects, respectively, at the three intervals. Self-reported drinks per drinking day, frequency of hazardous drinking assessed either on a daily or weekly basis, and of binge drinking sessions were reduced in the intervention group more than in the control group (P < 0.05) after both 3 and 6 months. The groups did not generally differ at 6 weeks. However, although self-reported consumption in both groups fell from baseline to 6-month follow-up, serum gamma-glutamyl transferase increased in both groups, which raises doubts about the validity of this marker in this sample and/or the validity of the self-reported data in this study.
Conclusion
MET delivered by nurses in PCUs in Thailand appears to be an effective intervention for male hazardous drinkers. Uncertainties about the validity of self-reported data jeopardize the safety of this conclusion.
INTRODUCTION
Alcohol consumption has been increasing worldwide, including in Thailand. Morbidity and mortality from alcohol-related problems in Thailand are high and have been increasing over time, making this a major public health problem (Casswell and Thamarangsi, 2009). One study used the World Health Organization-recommended Alcohol Use Disorder Identification Test (AUDIT; Saunders et al., 1993) to assess the prevalence of hazardous and harmful drinking (Assanangkornchai et al., 2003). Approximately 27% of Thai men were found to be hazardous or harmful drinkers, scoring ≥8 on the AUDIT in comparison with ~1% of Thai women.
Brief intervention appears to be a particularly valuable strategy for reducing morbidity in individuals who drink heavily and who have not yet established severe alcohol problems (Bertholet et al., 2005; Kaner et al., 2007; Wilk et al., 1997). However, some studies suggest caution in generalizing from brief intervention studies into practice (Edwards and Rollnick, 1997; Poikolainen, 1999). Motivational Enhancement Therapy (MET) was originally developed as a brief four-session adaptation of Motivational Interviewing in Project MATCH (Miller et al., 1992). This approach uses patient-centred interviewing techniques to enhance patients’ motivation to change their drinking behaviour, and has been widely used in treatment research and demonstrated to be effective for alcohol-dependent patients (for example, Sellman et al., 2001). In this study, MET was selected as a brief intervention for use with hazardous alcohol drinkers who were not dependent. We designed a three-session, 15-min MET counselling schedule especially for use in primary care settings in Thailand, which was evaluated to assess the effectiveness of brief intervention using adapted MET for hazardous alcohol drinkers.
METHODS
Study design and participants
A randomized controlled trial was conducted between July 2003 and April 2004 in eight PCUs in Ubonratchatanee province (Northeast Thailand, a rural area 630 km from Bangkok; n = 7) and Chachoengsao province (Central Thailand, a rural area 200 km from Bangkok; n = 1). Consecutive attenders aged between 18 and 65 years at the PCUs were invited to self-complete the Thai language version of the AUDIT questionnaire (Assanangkornchai et al., 2003). Literacy rates in Thailand are high, and self-completion was thus unproblematic. All patients who had an AUDIT score ≥8, without obvious exclusion criteria, were invited to participate in the study and immediately randomized. The exclusion criteria were as follows:
-
(i)
alcohol-dependent patients (Diagnostic and Statistical Manual of Mental Disorders (DSM-IV) criteria, as applied by a physician)
-
(ii)
patients with a history of any liver disease
-
(iii)
patients with a history of regular alcohol drinking starting early in the morning
-
(iv)
recent consumption of extremely high amounts per day (>120 g for men or >80 g for women)
-
(v)
patients with neurological disease and psychiatric disorders
-
(vi)
pregnant women and
-
(vii)
age <18 years or >65 years.
These criteria were assessed either by a clinician or in baseline data collection. Patients excluded from the study were referred to community hospitals for appropriate treatment. Once patients had completed the AUDIT, they were randomized, completed baseline data collection and, if they had been allocated to the intervention group, received the first intervention session during the same visit. Everyone allocated to intervention subsequently participated in the first session. After collected data were transferred to the coordinating centre, inclusion and exclusion criteria were reviewed again under an established quality control protocol. A small number of patients (n = 9; four in the intervention group and five in the control group) who met criteria for exclusion were inadvertently randomized (see Results) and were withdrawn from the study. Written consent was obtained from each study volunteer at a face-to-face interview. The research protocol was reviewed and approved by the Royal Thai Army Medical Department Ethics Review Committee, Phramongkutklao Army Hospital and College of Medicine.
Baseline assessment
To identify drinking and other health behaviours, interviews with potential study volunteers were conducted by trained personnel (recruited PCU health care workers) using a standardized questionnaire. The questionnaire included not only drinking behaviour but also questions relating to exercise, smoking and eating habits. A history of alcohol consumption during the previous week and month was systematically obtained (one drink = 10 g alcohol, equivalent to an Australian standard drink). Questions included the number of episodes of binge drinking in the previous week, the number of episodes of being drunk in the previous month, the frequency of traffic accidents or other accidents related to alcohol consumption during the previous 6 months, and the frequency of health care utilization attributable to alcohol in the previous 6 months. Additional questions enquired about drinking initiation and family history. Patients who consumed alcohol above specific safety limits were defined as hazardous drinkers (men drinking >14 drinks per week or four drinks per drinking day, or women drinking more than seven drinks a week or three drinks a day (NIAAA, 1995)).
Intervention
Those allocated to the intervention group were individually invited to see a nurse during the initial visit. Nurses had been trained during a single 6-hour session, which included an introduction to the research project, lecture and practice exercises to assess the severity of alcohol problems, the effect of alcohol on the patient’s health and the effect of alcohol on the family and society. According to the Project MATCH MET protocol (Miller et al., 1992), motivation can be enhanced with a patient-centred interviewing style, starting with an evaluation of the patient’s ability to change his drinking habits according to the stage of change. For patients in the pre-contemplation stage, the main technique was feedback, using reflection and questioning skills to elicit self-motivational statements. If change was contemplated, the study nurse would work with the patient’s ambivalence using a pros and cons technique. At the same time, an empathic counselling style and encouragement of the patient’s self-efficacy were used to support change in drinking behaviour. Subsequently, each participant’s readiness to change drinking behaviour was assessed. If in the determination stage, options on how to reduce drinking behaviour were provided. Participants were then asked to commit themselves to try and change their behaviour and to negotiate appropriate goals. A plan was made with measurable goals in changing drinking behaviour during the action phase. Relapse-prevention procedures were used during the maintenance phase. The intervention was composed of three scheduled sessions: on Day 1, at 2 weeks and at 6 weeks after the baseline evaluation. Each session comprised ~15 min of counselling.
Outcome evaluation
A health survey questionnaire administered in a face-to-face interview in scheduled appointments at the PCU was used to collect outcome information. Non-attenders were followed up by telephone and home visits arranged as necessary. The primary outcome was the amount of alcohol consumption during the previous week, measured in four ways and identified in the first four rows of Table 2. Other information assessed by the health survey questionnaire included the consumption of alcohol during the previous month, number of episodes of binge drinking in 7 days and number of episodes of being drunk in previous month, frequency of accidents and traffic accidents due to alcohol drinking during the previous 6 months, and frequency of health care utilization owing to drinking behaviour in the previous 6 months. These were the secondary outcome measures. It was intended to base inferences about effectiveness on the primary outcome measures, taking into account their coherence, whilst also giving attention to any specific effects on secondary outcomes.
Table 2.
Alcohol consumption outcomes
| 6 weeks |
3 months |
6 months |
|||||||
|---|---|---|---|---|---|---|---|---|---|
| Intervention (n = 50) | Control (n = 48) | P-value | Intervention (n = 55) | Control (n = 53) | P-value | Intervention (n = 51) | Control (n = 41) | P-value | |
| Average drinking per drinking day during the previous week (drinks per drinking day) | |||||||||
| Drinks/day | 3.00 ± 3.40 | 4.85 ± 4.15 | 0.017* | 2.73 ± 2.87 | 5.06 ± 4.46 | 0.002* | 2.26 ± 2.70 | 4.02 ± 4.00 | 0.018* |
| Hazardous drinking per drinking day during the previous week (yes/no) | |||||||||
| Yes | 14 | 20 | 0.364 | 12 | 24 | 0.027* | 9 | 15 | 0.040* |
| No | 36 | 28 | 43 | 29 | 42 | 26 | |||
| Average drinking per week during the previous week (drinks/week) | |||||||||
| Drinks/week | 8.30 ± 13.85 | 14.77 ± 21.11 | 0.078 | 6.49 ± 10.63 | 17.00 ± 24.28 | 0.005* | 4.72 ± 8.34 | 11.24 ± 17.74 | 0.035* |
| Hazardous drinking per week during the previous week (yes/no) | |||||||||
| Yes | 13 | 16 | 0.427 | 8 | 18 | 0.018* | 3 | 11 | 0.005* |
| No | 37 | 32 | 47 | 35 | 48 | 30 | |||
| Frequency of binge drinking (past week) | |||||||||
| 0.60 ± 1.39 | 1.20 ± 1.84 | 0.066 | 0.29 ± 0.60 | 1.36 ± 2.33 | 0.002* | 0.45 ± 1.38 | 0.95 ± 1.69 | 0.121 | |
| Frequency of being drunk (past month) | |||||||||
| 0.22 ± 0.58 | 0.54 ± 1.40 | 0.145 | 0.25 ± 1.00 | 0.47 ± 1.22 | 0.314 | 0.76 ± 1.80 | 0.32 ± 0.72 | 0.139 | |
P < 0.05.
Serum gamma-glutamyl transferase (GGT), a biological marker available for evaluation of the severity of current drinking, was used to provide objective evidence of change in alcohol consumption at study entry and at 6 months only. Outcome evaluations were done at 6-week, 3-month and 6-month periods of follow-up. Several features were incorporated to minimize and evaluate biases related to the use of verbal report data. In addition to GGT, parallel interviews with collateral informants were used to assess the honesty and accuracy of the information given by the patients (data not reported).
Sample size
The sample size was calculated based on published data on the effect of brief intervention among hazardous and harmful drinking patients in a provincial hospital in Thailand in 2000 (Chavengchaiyong et al., 2000) in which 66.3% of the treatment group changed their drinking behaviour, by either stopping drinking or reducing alcohol consumption, in comparison to 32% in the control group. It was estimated that at least 76 volunteers would need to be recruited and retained to give the trial 80% power to detect an effect of the intervention of this size at the 5% level of significance, and 98 to give 90% power. A target sample size of 128 subjects to be enrolled at eight PCUs was selected to allow for attrition.
Randomization sequence generation
The unit of randomization was the individual patient. Randomization of subjects to the intervention and control groups was carried out from the Coordinating Centre in Phramongkutklao Hospital in Bangkok using a standard randomization table. Each PCU had both control and intervention groups. In order to keep both groups of similar size, random allocation was done in blocks. On average, the trial was to have 6-8 participants in each study condition in each PCU.
Randomization allocation concealment and implementation
Randomization codes were distributed to each PCU in sealed envelopes. Eligible study participants were enrolled by health personnel when subjects first visited the PCU and were then assigned randomly to either the intervention or control group. The control group completed research assessments only. Both groups were informed that the study was designed to examine change in lifestyle over a 6-month period.
Blinding
In order to minimize the intervention effect of the research procedures, the subjects randomized into the control condition were told that the trial focused on health behaviours, which included questions on smoking, exercise, eating behaviour, weight and alcohol use. The study interviewers at follow-up visits were not aware of the assignment allocation of the study participants.
Statistical methods
Results were analysed on the basis of available outcome data, with all participants with follow-up data at each interval included in all analyses unless specifically indicated otherwise. χ2 and independent t-tests were used for the analyses of categorical and continuous outcomes, respectively. Additional analyses imputed data by the last observation carried forward. The findings of one multiple regression model are reported in which the effect of intervention condition on GGT level at follow-up controlled for the baseline measure of this variable and the one baseline difference between groups that reached statistical significance (risky weekly drinking over the past month, see Table 1), via their inclusion as covariates. Other regression analyses undertaken to further explore study findings were deemed not to add the results presented.
Table 1.
Comparison of intervention and control groups at study entry
| Characteristics | Intervention (N = 59) | Control (N = 58) | P-value |
|---|---|---|---|
| Age (mean ± SD) | 36.83 ± 10.21 | 37.09 ± 9.88 | 0.891 |
| Sex: | |||
| Male | 53 | 54 | 0.527 |
| Female | 6 | 4 | |
| Marital status | |||
| Single | 11 | 10 | 0.868 |
| Married | 45 | 43 | |
| Widowed/separated | 2 | 1 | |
| Education: | |||
| Primary school or less | 26 | 35 | 0.058 |
| Secondary school | 14 | 15 | |
| Graduate or higher | 7 | 1 | |
| Body mass index (kg/m2) | 22.49 ± 3.56 | 22.67 ± 3.19 | 0.797 |
| Regular exercise | 30 | 19 | 0.078 |
| Smoking behaviour | 40 | 42 | 0.486 |
| Average number of cigarettes a day | 8.82 ± 6.74 | 8.86 ± 5.97 | 0.978 |
| Duration of smoking behaviour (years) | 17.45 ± 9.82 | 16.07 ± 9.19 | 0.510 |
| Type of alcoholic beverage | |||
| Beer (6% vol.) | 11 | 13 | 0.614 |
| Spirits (40% vol.) | 48 | 45 | |
| Family history of alcohol abuse | |||
| Yes | 45 | 43 | 0.921 |
| No | 12 | 12 | |
| Family history of alcohol dependence | |||
| Yes | 7 | 6 | 0.821 |
| No | 50 | 49 | |
| Age at onset of drinking | 19.28 ± 4.62 | 19.68 ± 4.27 | 0.633 |
| Duration of drinking | 18.01 ± 8.34 | 17.09 ± 9.29 | 0.572 |
| Average AUDIT score | 18.00 ± 6.82 | 16.77± 6.20 | 0.302 |
| Severity of AUDIT: | |||
| 8–15 | 26 | 30 | 0.765 |
| 16–25 | 25 | 22 | |
| 26–40 | 9 | 8 | |
| History of accident related to alcohol drinking | 12 | 21 | 0.057 |
| History of traffic accident related to alcohol drinking in previous 6 months | 7 | 6 | 0.794 |
During the previous month
|
6.46 ± 4.11 | 6.31 ± 3.86 | 0.842 |
| Yes | 35 | 34 | 0.939 |
| No | 24 | 24 | |
|
17.19 ± 18.85 | 13.07 ± 16.43 | 0.211 |
| Yes | 25 | 13 | 0.021 |
| No | 34 | 45 | |
|
0.46 ± 0.86 | 0.41 ± 0.75 | 0.769 |
During the previous week
|
5.191 ± 4.30 | 4.31 ± 4.23 | 0.269 |
| Yes | 29 | 21 | 0.157 |
| No | 30 | 37 | |
|
13.27 ± 15.40 | 10.55 ± 16.96 | 0.365 |
| Yes | 21 | 13 | 0.116 |
| No | 38 | 45 | |
|
1.00 ± 1.49 | 0.88 ± 1.54 | 0.666 |
| Serum gamma-glutamyl transferase (mg/dl) | 50.90 ± 36.29 | 63.60 ± 50.22 | 0.127 |
RESULTS
Participant flow and follow-up
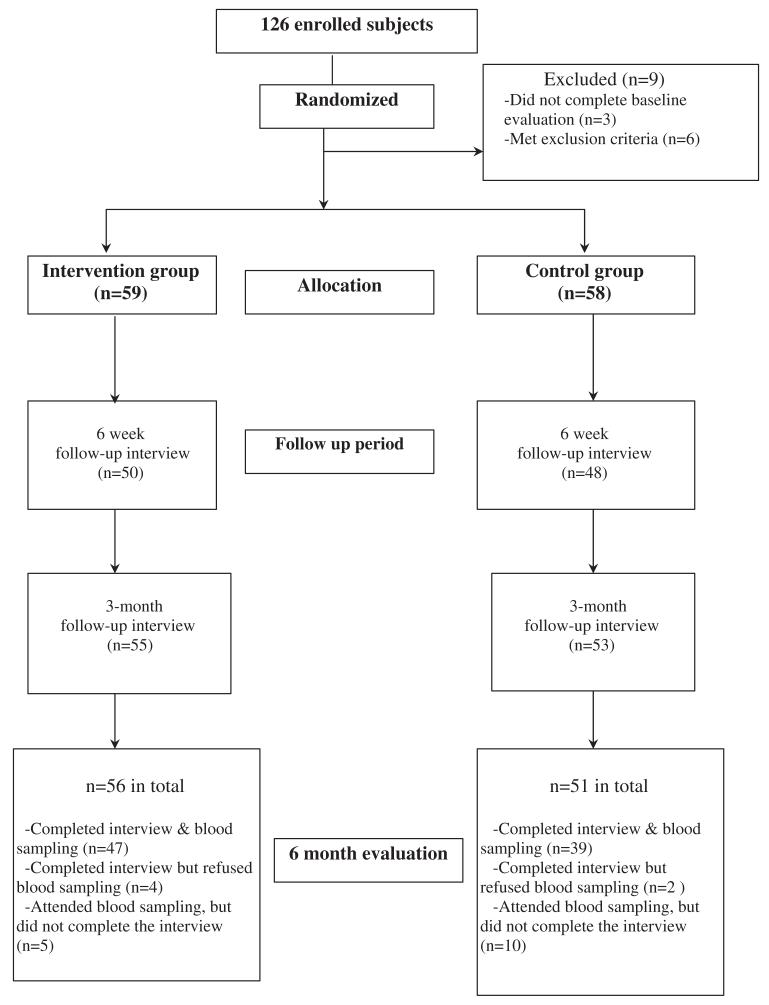
A total of 126 subjects were initially recruited. Of these, nine were subsequently excluded from the study after evaluation of baseline data for exclusion criteria by the data management unit: three (one intervention group and two control group) did not provide any data at the baseline assessment beyond the completion of the AUDIT and six (three in each group) had not met inclusion criteria; two were <18 years of age and four either had a history of liver disease or were judged to be alcohol dependent or both.
Of the remaining 117 subjects, 59 had been randomized to the intervention group and 58 to the control group (see Fig. 1). During the follow-up period after baseline evaluation, one participant from the intervention group died from stroke. At the first follow-up (6 weeks after the baseline), 98 (84%) subjects (50 in intervention and 48 in control groups) completed assessment. At 3 months after baseline, 108 (94%) subjects (55 in intervention and 53 in control groups) attended interviews. At 6 months after baseline 107 (91%), subjects (56 in intervention and 51 in control groups) provided at least some follow-up data (see Fig. 1). Of 107 subjects, 92 subjects completed the full interview; 101 subjects provided blood samples at the 6-month (final) follow-up, with 96 of these also having provided a blood sample at study entry.
Fig. 1.
Participant flow and follow-up.
Baseline data
At the baseline assessment, there were no significant differences between the intervention and the control groups in age, sex and marital status (see Table 1); 107 (91%) participants were male, and this should be borne in mind when examining all further results. Ages of the subjects ranged from 18 to 60 years old. The average age was 37 ± 10 years old. Most of the subjects’ education was at primary school level (62%) and most were current smokers (70%). The mean level of drinking during the previous month was 6.39 ± 3.97 drinks per drinking day or 15.15 ± 17.74 drinks/week. The mean level of drinking in the previous week was 4.75 ± 4.27 drinks per drinking day or 11.92 ± 16.17 drinks per week. The overall mean AUDIT score was 17.4 ± 6.5. Approximately 59% of participants had hazardous drinking behaviour (men >4 drinks/day, women >3 drinks/day) during the previous month. During the previous week, 43% of the participants had hazardous drinking behaviour above this threshold. In terms of alcohol consumption, there was no statistically significant difference between the intervention and control groups, except in the proportions of hazardous drinking in the form of mean alcohol consumption per week during the previous month.
Outcomes
Self-reported drinks per drinking day, frequency of daily and weekly hazardous drinking and of binge drinking sessions were reduced in the intervention group more than the control group (P < 0.05 in 9/10 outcomes assessed) at 3 and 6 months. There was little evidence of any attenuation of these effects between 3 and 6 months. The groups did not differ at 3 or 6 months on self-reported frequency of being drunk (see Table 2). In past week drinking, between-group differences were smaller at the 6-week follow-up, and only in one instance did it reach statistical significance.
The incidence of alcohol-related consequences in the 6-month period was low in both groups, and the differences were not statistically significant: there was one accident in the intervention group compared to four in the control group; three traffic accidents in the intervention group compared to five in the control group; and no visits to PCUs due to alcohol consumption in the intervention group compared to three in the control group.
Blood samples were obtained from 101 participants at 6-month follow-up (52 samples from the intervention group and 49 samples from the control group). These analyses are restricted to the 96 participants (51 intervention group and 45 control group) who provided GGT data at both study entry and at follow-up. The findings are very similar when also including the five cases who did not provide GGT data at baseline. At baseline, mean GGT was a little higher in the control group than in the intervention group, although this difference did not reach statistical significance (62.78 ± 52.04 compared to 48.06 ± 30.20, P = 0.1). GGT levels were higher in both the intervention and control groups at 6-month follow-up than at baseline. However, the mean GGT level of 59.73 ± 36.35 mg/dl in the intervention group was lower than the mean level of 84.11 ± 73.05 mg/dl in the control group to a statistically significant degree (P = 0.038). In the regression model, which explored the robustness of this difference to possible confounding (including the baseline GGT measure and the differential baseline measure of hazardous drinking), this finding was no longer statistically significant (the unstandardized difference in mean GGT levels was 11.0 mg/dl, β = 0.096, P = 0.166). Log-transforming the data to take into account non-normality made no difference to these findings.
Additional analyses
Four sets of additional analyses were undertaken to explore the robustness of the main outcome findings presented in Table 2. These evaluated the four alcohol consumption outcomes: (i) reported within a past month rather than past week timeframe; (ii) used last observation carried forward to construct intention-to-treat analyses (e.g. if baseline data only were available, these were subsequently imputed as outcomes, thus assuming no change); (iii) repeated this analysis also including data from the six excluded cases with baseline assessment data; and lastly (iv) considered outcomes among men only. These additional analyses broadly confirmed the findings reported in Table 2. We report here only those instances where there was a conflict between Table 2 and the additional analyses in the statistical significance of the evaluated outcomes.
For alcohol consumption assessed over the past month, the between-group difference at 6 months in past week drinks per drinking day was no longer statistically significant (intervention group 3.47 ± 3.21 compared to control group 4.61 ± 3.40, P = 0.106). However, two statistically significant differences were reported over the past month at the 6-week interval, which were not reported in the past week timeframe. These were in drinks per week (intervention group 9.20 ± 13.41 compared to control group 16.80 ± 18.59, P = 0.023) and exceeding weekly thresholds for hazardous drinking (11/50 in the intervention group compared to 23/48 in the control group, P = 0.007).
There was a single conflict in statistical significance with Table 2 when the analyses were undertaken in the full eligible sample of 117 with last observations being carried forward. After 6 weeks, the between-group difference in drinks per drinking day was no longer statistically significant (intervention group 3.49 ± 3.57 compared to control group 4.69 ± 4.13, P = 0.096). These analyses were then repeated, also including the six cases who met criteria for exclusion (three other randomized cases were excluded from the study as they did not provide baseline data). The previously identified conflict was found again (intervention group 3.71 ± 3.67 compared to control group 4.85 ± 4.11, P = 0.106). One further conflict was also identified. The difference in the proportions exceeding weekly thresholds for hazardous drinking after 3 months was not statistically significant (14/62 in the intervention group compared to 21/61 in the control group, P = 0.145).
When the analysis was restricted to men only, two differences in Table 2 findings were detected. Again after 6 weeks, the between-group difference in drinks per drinking day was no longer statistically significant (intervention group 3.64 ± 3.60 compared to control group 4.86 ± 4.18, P = 0.104). The difference in the proportions exceeding weekly thresholds for hazardous drinking after 3 months again also did not reach statistical significance (10/53 in the intervention group compared to 19/54 in the control group, P = 0.058).
DISCUSSION
To our knowledge, this is the first randomized trial to evaluate the effectiveness of a brief intervention for hazardous drinkers in primary care in Thailand. Self-reported outcome data strongly suggested that brief intervention with MET can help to reduce levels of alcohol consumption in those attending primary care in Thailand. This study also adds to the international literature in a number of other ways.
The pattern and size of these effects are noteworthy. There was a consistent between-group difference in drinks per week, whether measured over the past week or over the past month, of not less than six standard drinks at all follow-up intervals in all comparisons made. This is higher than the meta-analytic effect size reported by Kaner and colleagues (2007) for brief interventions in primary care. This may be partly explained by the shorter study period used here (Moyer et al., 2002), although there was no substantial evidence of any deterioration in effect over time. Similarly, outcomes in the form of proportions of hazardous drinkers observed here are also broadly equivalent to those found in previous meta-analytic studies. For example, heavy drinkers receiving brief intervention have previously been found to be twice as likely to moderate their drinking to non-hazardous levels 6–12 months after intervention compared to those who receive no intervention (Wilk et al., 1997).
The study showed higher mean GGT levels in both the intervention and control groups at 6-month follow-up relative to the baseline levels, with a larger increase seen in the control group, although these data are quite skewed. This overall increase in GGT levels may be because baseline data were collected immediately after ‘Kao Pansaa’, a 3-month period of Buddhist retreat during which it is customary for people to avoid wrongdoing, including limiting their alcohol drinking. After this period, normal drinking patterns are usually resumed. However, the self-reported data are in conflict here as there was a decrease rather than an increase over time (see below). Nevertheless, there was a difference between the mean GGT levels in the intervention group compared to the control group at follow-up, which fell below the conventional threshold for statistical significance in the regression model. A larger study would be necessary for the possible small effect on this particular outcome to be evaluated and confirmed.
The increased mean levels of GGT at follow-up evaluation in both intervention and control groups are in contrast to the reduced alcohol consumption that was self-reported. Especially given the alcohol consumption reported over the previous month at baseline, this suggests that the use of self-reported data is still liable to social desirability bias. The consensus in the research community that self-reported alcohol consumption is valid derives mainly from conclusions drawn from studies undertaken in treatment contexts. It is not clear whether influences on the validity of self-report in brief intervention contexts may be different, in ways which are important. Any such problem may be exacerbated in Thailand where there is a cultural desire to please. It may be that a more appropriate and instructive comparison can be made to general population surveys in which there are well-known problems with self-reported alcohol consumption data if sales are used as a gold standard (though they are not without their limitations). Data from the present study support further investigation of the measurement of alcohol consumption with biological measures in heavy drinking populations to assess the validity of self-reported outcomes evaluated. Most biological markers have limitations, and it will be worth exploring the validity of self-reported drinking behaviour in other ways.
Studies of brief interventions delivery by primary care nurses are much rarer than by physicians. The findings of the present study mirror those of a small study by Beckham (2007), with which it shares a number of design features. This study explored the effectiveness of motivational interviewing in participants utilizing a low-income community health centre in rural Southern Idaho. AUDIT was used to screen patients, and a single session of motivational interviewing delivered by primary care nurses was contrasted with no intervention, with positive intervention effects on drinking behaviour established after 6 weeks. Trials of brief interventions other than motivational interviewing delivered by nurses have yielded variable results (Holloway et al., 2007; Lock et al., 2006).
There are a number of study limitations that should be borne in mind. The total number of people who were screened using AUDIT was not recorded, and this leads to some uncertainty about the external validity of the study findings. We sought to exclude those who were alcohol dependent by clinician assessment of DSM-IV criteria. The high mean AUDIT scores at baseline strongly suggest that exclusion of those with alcohol dependence was unsuccessful, and we did not measure dependence among trial participants. Because of the small number of women in this study, we could not determine the effect of gender on outcomes, nor indeed be confident that the main findings can be validly applied to women. Fidelity to motivational interviewing was not assessed, so it is unknown to what extent the intervention—as delivered—represents an optimal and valid test of that particular type of brief intervention. Motivational interviewing is complex, and extensive practice is required to reach advanced levels. The extent and nature of training provided in this study are clearly sub-optimal by current international standards. The intervention protocol was based on that used in Project MATCH (Miller et al., 1992), which was in turn adapted from the first edition of ‘Motivational Interviewing’ (Miller and Rollnick, 1991). Subsequent developments in methods of motivational interviewing and enhanced training for its delivery may have the potential to produce superior outcomes than were observed here. The possible significance of urban rural differences in receptivity to brief interventions was not explored here, nor has it been studied anywhere in the international literature as far as we are aware. The longer term course of the effects observed here is also unknown.
Notwithstanding these limitations, this study has important strengths. This study adds a further trial to the many primary studies and systematic reviews that find brief interventions to be effective in reducing self-reported hazardous drinking in primary care populations. The main findings presented in Table 2 have been found to be fairly robust across the various sensitivity analyses of the primary outcome measures. It is noteworthy that this evidence is strongest for an impact on self-reported drinking behaviour at 6 months, being statistically significant in all analyses of all primary outcome measures. Interestingly, there is no consistent evidence of an immediate post-intervention effect at 6 weeks.
The effectiveness of these interventions is likely to depend on the alcohol culture of the society in question as well as on the delivery agent, the setting and the specific approach used. This study provides evidence of effective brief intervention by nurses with male hazardous and harmful drinkers in Thailand, notwithstanding study limitations, most notably including uncertainties about the validity of the self-reported data. The high rates of follow-up maintained to 6 months provide further reasons for confidence in the validity of these effectiveness findings.
Acknowledgements
We would like to thank all the health personnel, nurses, other staff and patients at the eight PCUs for their invaluable help. We are grateful to Sawitri Assanagkornchai, MD, PhD (Prince of Songkla University); Apinun Aramrat, MD, PhD (Chiangmai University); Dr Alan Dellow (FRCGP); and the provincial chief medical officers of Ubon Ratchatani and Chachoengsao for their advice and support. We also acknowledge help from Phramongkutklao laboratories.
Funding — This research was supported by grants from the Thai Health Promotion Foundation.
REFERENCES
- Assanangkornchai S, Pinkaew P, Apakupakul N. Prevalence of hazardous-harmful drinking in a southern Thai community. Drug Alcohol Rev. 2003;22:287–93. doi: 10.1080/0959523031000154427. [DOI] [PubMed] [Google Scholar]
- Beckham N. Motivational interviewing with hazardous drinkers. J Am Acad Nurse Pract. 2007;19:103–10. doi: 10.1111/j.1745-7599.2006.00200.x. [DOI] [PubMed] [Google Scholar]
- Bertholet N, Daeppen JB, Wietlisbach V, et al. Reduction of alcohol consumption by brief alcohol intervention in primary care: systematic review and meta-analysis. Arch Intern Med. 2005;165:986–95. doi: 10.1001/archinte.165.9.986. [DOI] [PubMed] [Google Scholar]
- Casswell S, Thamarangsi T. Reducing harm from alcohol: call to action. Lancet. 2009;373:2247–57. doi: 10.1016/S0140-6736(09)60745-5. [DOI] [PubMed] [Google Scholar]
- Chavengchaiyong W, Foncom A, Chockeard N. The effect of brief intervention to changing behaviour of alcohol disorder patients at Lamphun Hospital. Bull Dept Med Serv. 2000;25:87–95. [Google Scholar]
- Edwards AG, Rollnick S. Outcome studies of brief alcohol intervention in general practice: the problem of lost subjects. Addiction. 1997;92:1699–704. [PubMed] [Google Scholar]
- Holloway AS, Watson HE, Arthur AJ, et al. The effect of brief interventions on alcohol consumption among heavy drinkers in a general hospital setting. Addiction. 2007;102:1762–70. doi: 10.1111/j.1360-0443.2007.01968.x. [DOI] [PubMed] [Google Scholar]
- Kaner EF, Beyer F, Dickonson HO, et al. Effectiveness of brief alcohol interventions in primary care populations. Cochrane Database Syst Rev. 2007 doi: 10.1002/14651858.CD004148.pub3. Art. No.: CD004148. DOI: 10.1002/14651858.CD004148.pub3. [DOI] [PubMed] [Google Scholar]
- Lock CA, Kaner E, Heather N, et al. Effectiveness of nurseled brief alcohol intervention: a cluster randomized controlled trial. J Adv Nurs. 2006;54:426–39. doi: 10.1111/j.1365-2648.2006.03836.x. [DOI] [PubMed] [Google Scholar]
- Miller WR, Rollnick S. Motivational Interviewing: Preparing People to Change Addictive Behavior. Guilford Press; New York, NY: 1991. [Google Scholar]
- Miller WR, Zweben A, Diclemente CC, et al. Project MATCH Motivational Enhancement Therapy Manual. NIAAA; Maryland: 1992. [Google Scholar]
- Moyer A, Finney JW, Swearingen CE, et al. Brief interventions for alcohol problems: a meta-analytic review of controlled investigations in treatment-seeking and non-treatment-seeking populations. Addiction. 2002;97:279–292. doi: 10.1046/j.1360-0443.2002.00018.x. [DOI] [PubMed] [Google Scholar]
- NIAAA . The Physicians’ Guide to Helping Patients with Alcohol Problems. National institutes of Health; Washington, DC: 1995. pp. NIH Publication No 95-3769. [Google Scholar]
- Poikolainen K. Effectiveness of brief interventions to reduce alcohol intake in primary health care populations: a meta-analysis. Prev Med. 1999;28:503–9. doi: 10.1006/pmed.1999.0467. [DOI] [PubMed] [Google Scholar]
- Saunders JB, Aasland OG, Babor TF, et al. Development of the Alcohol Use Disorders Identification Test (AUDIT): WHO Collaborative Project on Early Detection of Persons with Harmful Alcohol Consumption—II. Addiction. 1993;88:791–804. doi: 10.1111/j.1360-0443.1993.tb02093.x. [DOI] [PubMed] [Google Scholar]
- Sellman JD, Sullivan PF, Dore GM, et al. A randomized controlled trial of motivational enhancement therapy (MET) for mild to moderate alcohol dependence. J Stud Alcohol Drugs. 2001;62:389–96. doi: 10.15288/jsa.2001.62.389. [DOI] [PubMed] [Google Scholar]
- Wilk AI, Jensen NM, Havighurst TC. Meta-analysis of randomized control trials addressing brief interventions in heavy alcohol drinkers. J Gen Intern Med. 1997;12:274–283. doi: 10.1046/j.1525-1497.1997.012005274.x. [DOI] [PMC free article] [PubMed] [Google Scholar]