Abstract
Background
Although increases in obesity over the past 30 years have adversely affected the health of the U.S. population, there have been concomitant improvements in health because of reductions in smoking. Having a better understanding of the joint effects of these trends on longevity and quality of life will facilitate more efficient targeting of health care resources.
Methods
For each year from 2005 through 2020, we forecasted life expectancy and quality-adjusted life expectancy for a representative 18-year-old, assuming a continuation of past trends in smoking (based on data from the National Health Interview Survey for 1978 through 1979, 1990 through 1991, 1999 through 2001, and 2004 through 2006) and past trends in body-mass index (BMI) (based on data from the National Health and Nutrition Examination Survey for 1971 through 1975, 1988 through 1994, 1999 through 2002, and 2003 through 2006). The 2003 Medical Expenditure Panel Survey was used to examine the effects of smoking and BMI on health-related quality of life.
Results
The negative effects of increasing BMI overwhelmed the positive effects of declines in smoking in multiple scenarios. In the base case, increases in the remaining life expectancy of a typical 18-year-old are held back by 0.71 years or 0.91 quality-adjusted years between 2005 and 2020. If all U.S. adults became nonsmokers of normal weight by 2020, we forecast that the life expectancy of an 18-year-old would increase by 3.76 life-years or 5.16 quality-adjusted years.
Conclusions
If past obesity trends continue unchecked, the negative effects on the health of the U.S. population will increasingly outweigh the positive effects gained from declining smoking rates. Failure to address continued increases in obesity could result in an erosion of the pattern of steady gains in health observed since early in the 20th century.
Trends in behavioral risk factors can have a profound effect on population health.1,2 Estimates suggest that obesity accounts for 5 to 15% of deaths each year in the United States2–5 and smoking for 18%.1 Eliminating smoking could increase population life expectancy by as much as 1 to 2 years.6,7 In contrast, if obesity rates continue to grow as they have historically, a leveling off, or even a reversal, of past life expectancy trends has been predicted.8
In addition to their effect on mortality, obesity and smoking affect quality of life.9–14 Smoking is a major risk factor for cardiovascular disease, chronic lung disease, and several cancers. Obesity leads to cardiovascular disease, diabetes, and joint problems.
Recent U.S. trends in smoking and obesity have moved in opposite directions: over the past 15 years, smoking rates have declined by 20%, whereas obesity rates have increased by 48%.15 Estimating the joint effect of the trends in smoking and obesity on both mortality and quality of life is important if we are to create a complete picture of their effects on population health. Although previous studies have examined the joint effect of obesity and smoking on mortality, they have neither used nationally representative data nor examined quality of life.
This study forecasts the effect of trends in obesity and smoking on future U.S. life expectancy and quality-adjusted life expectancy. We use data from the past three decades to forecast future rates of obesity and smoking and estimate their effects on length and quality of life.
Methods
Data Sources and Definitions
Three surveys, each nationally representative of the civilian, noninstitutionalized U.S. population,16–19 were used to measure the prevalence of risk factors and their effect on mortality and quality of life in adults. Data on body-mass index (BMI, the weight in kilograms divided by the square of the height in meters) were obtained from physical measures recorded in the National Health and Nutrition Examination Survey (NHANES).17 Respondents were classified with the use of World Health Organization (WHO) criteria20 as having normal weight (BMI, 18.5 to 24.9), being overweight (BMI, 25.0 to 29.9), or being obese (BMI, 30.0 to 34.9; obesity class I) or morbidly obese (BMI ≥35.0; obesity classes II and III). Those with a BMI of less than 18.5 were excluded because a low BMI can be indicative of preexisting illness.21 To measure historical trends, the mean BMI was calculated according to age and sex for four time periods: 1971 through 1975 (NHANES I, 4992 respondents),22 1988 through 1994 (NHANES III, 17,689 respondents), 1999 through 2002 (the first two waves of continuous data from NHANES, 10,132 respondents), and 2003 through 2006 (two subsequent waves of continuous data from NHANES, 10,436 respondents).
Smoking trends were obtained from the National Health Interview Survey.18,23 The population was divided into four groups: current smokers, former smokers who had smoked within the previous 10 years, former smokers who had not smoked for 10 years or more, and people who had never smoked. Smoking rates were examined according to age and sex for four time periods: 1978 through 1979 (23,488 respondents), 1990 through 1991 (83,770 respondents), 1999 through 2001 (95,623 respondents), and 2004 through 2006 (86,069 respondents).
The effects of smoking status and BMI on quality of life were estimated with the use of data from the 2003 Medical Expenditure Panel Survey,16,24 which included a self-rating of health on a scale from 0 (worst health imaginable) to 1.0 (best).25 Analyses included the 80% of respondents (18,913 in total) for whom there were complete data on smoking, BMI, and self-rated health.
Risks of death from any cause for the joint categories of smoking and BMI were calculated with the use of follow-up data on mortality from NHANES I, II, and III (a combined total of 24,758 respondents). Life tables for the U.S. population were obtained from the National Center for Health Statistics and the Social Security Administration (for ages top-coded in tables from the National Center for Health Statistics; for details see the Supplementary Appendix, available with the full text of this article at NEJM.org).26,27
Approach to Forecasting
Our analysis proceeded in four parts. First, we forecasted future prevalence of smoking and obesity by simulating a continuation of past trends. Historical changes in smoking and BMI were calculated going back approximately 15 years. Respondents were divided into 4 categories for smoking and 4 categories for BMI, which were then combined to produce a total of 16 groups. To control for changing demographic characteristics, the 16 categories of smoking and BMI in each year were weighted according to the national distribution of age and sex for the year 2000.28
Using NHANES data for the years 2003 through 2006 as a baseline, we then forecasted the joint distribution of future smoking and BMI categories. An annual percentage increase in BMI that was consistent with historical change was simulated for each person. To simulate a continuation of past rates of change for smoking, we probabilistically assigned a percentage of current smokers to become former smokers and a percentage of current and short-term former smokers to become long-term quitters or lifetime nonsmokers in each year. We then recalculated annual population shares in each of the 16 categories for smoking and obesity. Finally, for each future year we smoothed the population distribution by regressing an indicator for being in each joint BMI and smoking category on the basis of age and age squared.
The second step was to estimate the relative risks of death from any cause for each of the 16 groups, applying Cox proportional-hazards models to combined follow-up data from NHANES I, II, and III. We used attained age as the time scale.29 Covariates were baseline age in 5-year intervals, sex, and race.
The third step was to generate life tables for each smoking and BMI category. We began with age-specific mortality rates from 2004 life tables. Using the relative risks of death calculated for each of the 16 groups and our forecasts of population shares of smoking and BMI at each age, we calculated mortality rates at each age for each of the 16 groups. These rates were used to simulate life expectancy for each group.
The effect of smoking and BMI on quality of life was estimated using a regression analysis30 relating self-rated health to smoking–BMI category and sociodemographic variables. Because the Medical Expenditure Panel Survey asks only about current smoking status, we assumed that the quality of life for former smokers was the same as that for people who had never smoked. Predicted summary health scores were then estimated for each of the 16 categories of smoking and BMI by age. These quality-of-life scores were weighted by our population forecasts to estimate the effects of obesity and smoking on quality-adjusted life expectancy for each future year.
To estimate the effect these risk factors may already have had on life expectancy, we forecasted the change in life expectancy between 1990 and 2004, holding rates of smoking and obesity constant at 1990 levels. We then compared the forecasted change in life expectancy with the observed change in life expectancy over the interval.
Sensitivity Analyses
Our baseline simulation assumed that trends in smoking and obesity through 2020 would be equal to the change occurring over the 15 years preceding 2020. We formed alternative projections using historical changes from longer (30-year) and shorter (5-year) periods. Also, since evidence suggests that the growth in the rate of obesity may be decelerating,31,32 we estimated the threshold rate of increase in BMI above which its adverse effects begin to surpass the beneficial effects of declines in the rate of smoking. We also simulated the effects of eliminating smoking and obesity (i.e., reducing BMI to <25) by 2020. Finally, we performed sensitivity analyses using alternative relative risks of death from any cause, obtained from two prospective studies of health professionals that, although not nationally representative, consider the joint effects of smoking and BMI on mortality.21,33
Results
Rates of Change in Smoking and Obesity
On average, the prevalence of smoking declined by 1.4% per year and BMI increased by 0.5% per year over the 15 years before 2005 (Table 1). Over the 30-year and 5-year historical periods, the annual rate of decline in smoking was higher (1.7% and 2.0%, respectively), and the annual rate of increase in BMI was lower (0.4% and 0.3%, respectively).
Table 1.
Historical Trends in Smoking Prevalence and Mean BMI among U.S. Adults, 1973–2005.*
| Variable | Period | Approximate Annual Rate of Change before 2005 | |||||
|---|---|---|---|---|---|---|---|
| 1973–1979 | 1990 | 2000 | 2005 | Over 30 yr | Over 15 yr | Over 5 yr | |
| Smoking status (%) | |||||||
| Current smoker | 33.3 | 25.7 | 23.1 | 20.9 | −1.7 | −1.4 | −2.0 |
| Former smoker | |||||||
| Has not smoked for <10 yr | 11.5 | 12.7 | 8.5 | 7.5 | −1.6 | −3.6 | −2.4 |
| Has not smoked for ≥10 yr | 8.2 | 12.6 | 13.8 | 13.1 | 1.6 | 0.3 | 0.9 |
| Mean BMI | 25.2 | 26.5 | 27.9 | 28.3 | 0.4 | 0.5 | 0.3 |
All prevalence estimates and means are weighted according to the distribution of age and sex in the 2000 census population. Rates of change are percentages. Smoking data are from the National Health Interview Survey for the years that the survey had questions on smoking, including amount of time passed since quitting: 1978 through 1979, 1990 through 1991, 1999 through 2001, and 2004 through 2006. The periods covered for smoking are thus 26.5 years, 14.5 years, and 5 years. Data on body-mass index (BMI, the weight in kilograms divided by the square of the height in meters) are from the National Health and Nutrition Examination Survey (NHANES) I (1971 through 1975), NHANES III (1988 through 1994), and continuous NHANES data from 1999 through 2002 and 2003 through 2006. The periods covered for BMI, which are based on the midpoints of the periods covered by these surveys, are 31.5 years, 13.5 years, and 4 years.
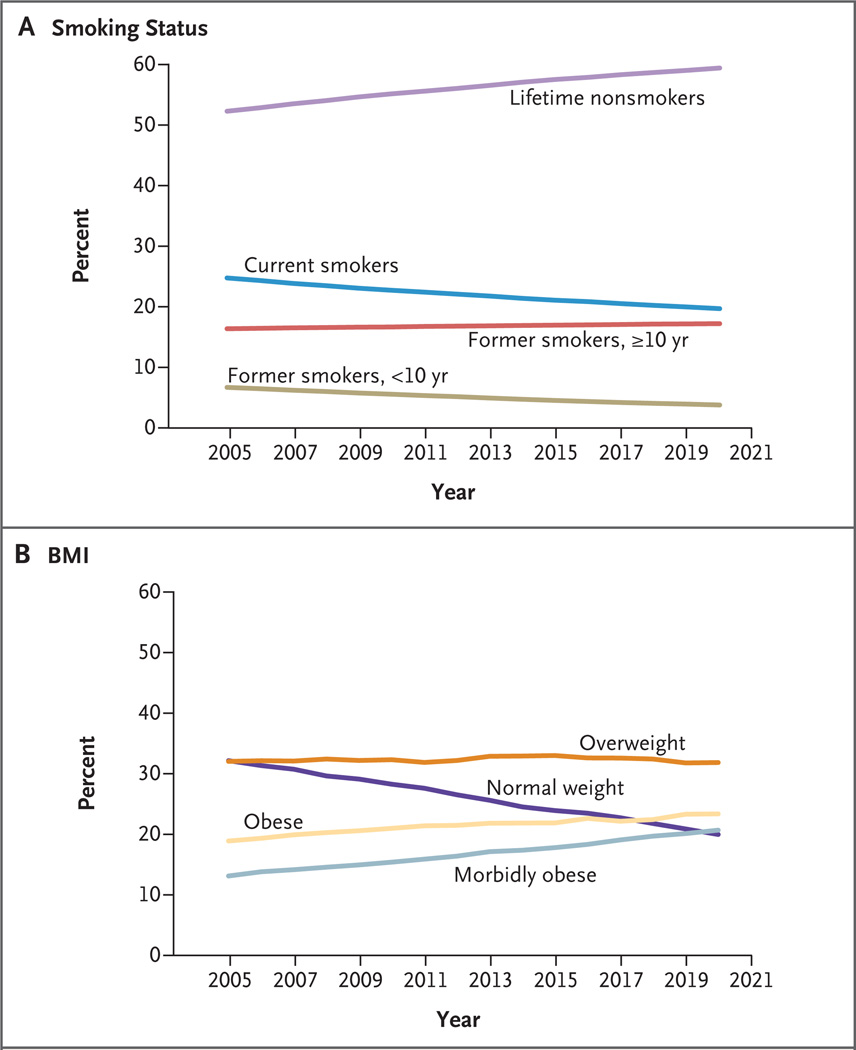
Our forecasted trends in the prevalence of smoking and the distribution of BMI assume that historical 15-year trends will continue over the course of our projection period, from 2005 through 2020 (Fig. 1) (smoothing details are provided in the Supplementary Appendix). Over those 15 years, we project that the share of the population that is currently smoking will decline by 21%, the share that stopped for less than 10 years will decline by 44%, and the share that stopped smoking for 10 years or more will increase by 5%. Over that same time frame, the share of the population that has a normal weight is projected to decline by 35%. Nearly half the population (45%) is expected to be obese by 2020.
Figure 1. Forecasted Distribution of Risk Factors, 2005 through 2020.
The projected rates of change in the categorical distribution of smoking status (Panel A) and body-mass index (BMI) (Panel B) from 2005 to 2020 are shown, assuming a continuation of trends occurring over the 15 years preceding 2005. The categories for weight were defined according to the World Health Organization criteria: normal weight (BMI [the weight in kilograms divided by the square of the height in meters], 18.5 to 24.9), overweight (BMI, 25.0 to 29.9), obese (BMI, 30.0 to 34.9; obesity class I), and morbidly obese (BMI, ≥35.0; obesity classes II and III). Historical trends for smoking were measured with the use of the National Health Interview Survey (1990 through 1991 and 2004 through 2006) and historical trends for BMI with the use of the National Health and Nutrition Examination Survey (1988 through 1994 and 1999 through 2002).
Health Outcomes
In the analyses of the risks of death associated with BMI and smoking, mortality was higher among current smokers and those with a higher BMI (consistent with the findings by Flegal and colleagues).3 In the analyses of quality of life, smokers had a lower quality than nonsmokers at all ages, and quality declined with increasing BMI across age groups (Table 2). (The relative risks of death from smoking and BMI status and the results of regression analysis for quality of life appear in the Supplementary Appendix.)
Table 2.
Summary of Quality-of-Life Scores According to Level of Risk.*
| Smoking Status and Age | Quality-of-Life Score | |||
|---|---|---|---|---|
| Normal Weight (BMI, 18.5–24.9) |
Overweight (BMI, 25.0–29.9) |
Obese (BMI, 30.0–34.9) |
Morbidly Obese (BMI, ≥35.0) |
|
| Former smoker or lifetime nonsmoker | ||||
| 18–24 yr | 0.90 | 0.89 | 0.86 | 0.80 |
| 25–34 yr | 0.88 | 0.88 | 0.84 | 0.78 |
| 35–44 yr | 0.86 | 0.85 | 0.82 | 0.76 |
| 45–54 yr | 0.84 | 0.84 | 0.80 | 0.75 |
| 55–64 yr | 0.82 | 0.81 | 0.78 | 0.72 |
| 65–74 yr | 0.78 | 0.77 | 0.74 | 0.68 |
| ≥75 yr | 0.72 | 0.71 | 0.68 | 0.64 |
| Current smoker | ||||
| 18–24 yr | 0.84 | 0.83 | 0.81 | 0.74 |
| 25–34 yr | 0.82 | 0.81 | 0.78 | 0.72 |
| 35–44 yr | 0.79 | 0.79 | 0.76 | 0.70 |
| 45–54 yr | 0.78 | 0.77 | 0.74 | 0.69 |
| 55–64 yr | 0.76 | 0.75 | 0.72 | 0.67 |
| 65–74 yr | 0.72 | 0.71 | 0.66† | 0.61† |
| ≥75 yr | 0.67 | 0.67 | 0.66† | 0.61† |
Quality-of-life scores range from 0 to 1, with 0 representing the worst health imaginable and 1 the best. Scores were predicted on the basis of a regression of scores on the European Quality of Life–5 Dimensions (EQ-5D) visual-analogue scale available in the Medical Expenditure Panel Survey, 2003.
BMI denotes body-mass index.
The quality of life for obese and morbidly obese smokers was estimated jointly for all respondents who were 65 years of age or older, since the number of respondents in these groups was small.
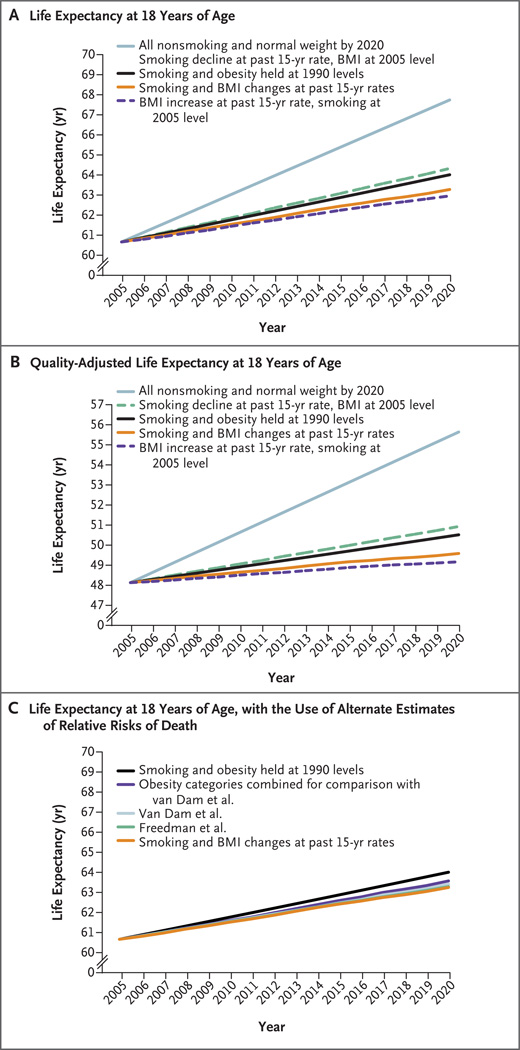
Fifteen-year forecasts for a typical 18-year-old in terms of life expectancy and quality-adjusted life expectancy, accounting for changes in smoking status alone, in BMI alone, and in both combined, are shown in Table 3 and Figure 2. For smoking status alone, continued declines in smoking at rates seen over the past 15 years would lead to an increase in life expectancy of 0.31 years and an increase in quality-adjusted life expectancy of 0.41 years (over and above the trend in life expectancy resulting from other factors). In contrast, a continuation of the increases seen in BMI alone would reduce gains in life expectancy by 1.02 years and reduce quality-adjusted gains in life expectancy by 1.32 years relative to the trend. The net effect of the declines in smoking and the increases in BMI is a reduction in life expectancy of 0.71 years and a reduction in quality-adjusted life expectancy of 0.91 years relative to the trend. This pattern of results is seen for every year between 2005 and 2020 and becomes more pronounced over time. Sensitivity analyses based on alternative estimates of the risks of death, obtained from prospective studies, yielded similar results (Fig. 2C).
Table 3.
Effect of Alternative Assumptions about Trends in Smoking and BMI on Life Expectancy and Quality-Adjusted Life Expectancy for a Typical 18-Year-Old.*
| Scenario | Change, 2005–2020 | |||||
|---|---|---|---|---|---|---|
| Smoking Status Alone† | BMI Alone‡ | Both Smoking Status and BMI§ | ||||
| life expectancy |
quality-adjusted life expectancy |
life expectancy |
quality-adjusted life expectancy |
life expectancy |
quality-adjusted life expectancy |
|
| years | ||||||
| Historical 15-year rate of change (baseline) | 0.31 | 0.41 | −1.02 | −1.32 | −0.71 | −0.91 |
| Historical 30-year rate of change | 0.32 | 0.43 | −0.76 | −1.00 | −0.43 | −0.56 |
| Historical 5-year rate of change | 0.41 | 0.52 | −0.58 | −0.75 | −0.10 | −0.17 |
| All persons become nonsmokers of normal weight¶ | 1.73 | 2.17 | 1.40 | 2.44 | 3.76 | 5.16 |
BMI denotes body-mass index.
This category shows the effect of continuing trends in smoking status with BMI remaining at 2005 levels.
This category shows the effect of continuing trends in BMI with smoking status remaining at 2005 levels.
This category shows the effect of continuing trends in both smoking status and BMI.
In this scenario, current and former smokers were classified as former smokers who had not smoked for 10 years or more.
Figure 2. Forecasted Life Expectancy and Quality-Adjusted Life Expectancy at 18 Years of Age from 2005 through 2020, Considering Trends in Smoking Alone, Body-Mass Index Alone, and Smoking and Body-Mass Index Combined.
The life expectancy (Panel A) and quality-adjusted life expectancy (Panel B) for a typical 18-year-old are depicted in accordance with the following simulation scenarios: entire population classified as having normal weight and all current and former smokers classified as former smokers who have not smoked for 10 years or more by 2020 (blue line); declines in smoking set to the rate of the past 15 years with body-mass index (BMI) remaining at 2005 levels (green line); continuation of the rates of increase in life expectancy from 1990 through 2004, independent of changes in smoking and BMI over that time period (black line); trends in smoking and BMI continued at the rate of the past 15 years (brown line); and increases in BMI continued at the rate of the past 15 years (purple line). Panel C shows life expectancy for a typical 18-year-old, forecasted on the basis of relative risks of death from different studies. Two of the forecasts shown here are from Panel A (based on the relative risks of death calculated in this study with the use of the National Health and Nutrition Examination Surveys [NHANES] I, II, and III), with one forecast continuing the rates of increase in life expectancy from 1990 through 2004, independent of changes in smoking and BMI over that period (black line) and the other forecast a continuation of the trends in smoking and BMI at the rates of the past 15 years (brown line). For the sake of comparison with these forecasts, we also included forecasts based on relative risks of death as reported in prospective studies by Freedman and colleagues in 200621 (green line, hidden beneath brown line) and by van Dam and colleagues in 200833 (women only, blue line), assuming a continuation of the trends in smoking and BMI at the rates of the past 15 years. To obtain relative risks for the joint categories of smoking and obesity from the study by van Dam and colleagues, a multiplicative relationship between smoking and obesity was assumed. Since, unlike our study, the van Dam study combined the categories of obese and morbidly obese when calculating risks of death, we performed an alternate forecast for the sake of comparison in which these categories were combined, using mortality data from NHANES (purple line).
Historical trends from the years 1990 through 2004 show that the life expectancy of a typical 18-year-old increased by 2.44 years as compared with our forecasted increase of 2.98 years, assuming no change in smoking and obesity rates from 1990 levels. Thus, adverse trends in obesity reduced, but did not overwhelm, the positive effects of other factors during the years 1990 through 2004 (Fig. 2).
Sensitivity Analyses
Forecasts based on alternative assumptions about changes in smoking and BMI (Table 3) projected slightly more rapid declines in smoking and less rapid increases in BMI. However, even in these scenarios, the negative effect of increasing BMI surpassed the positive effect of declines in smoking rates, eroding growth in both life expectancy and quality-adjusted life expectancy. In fact, the negative effect of increasing BMI on life expectancy and quality-adjusted life expectancy would persist as long as the rate of increase exceeded 0.15% per year.
The hypothetical elimination of smoking by 2020 would increase the life expectancy and quality-adjusted life expectancy of an 18-year-old by 1.73 years and 2.17 years, respectively; returning the entire population to normal weight would have similar effects. The combined effect of eliminating both smoking and obesity made for a net gain of 3.76 life-years and 5.16 quality-adjusted life-years (Table 3 and Fig. 2A and 2B).
Discussion
The negative effects of increasing obesity rates on the health of the U.S. population are forecasted to outweigh the benefits resulting from continued reductions in the prevalence of smoking during the next decade. In addition, these adverse health effects are forecasted to increase over time. The magnitude is large. A reduction in life expectancy of 0.71 years — our estimate of the combined effects of reduced smoking and increased obesity — is about one quarter of the 2.98-year increase in life expectancy at age 18 that we forecast would have occurred between 1990 and 2004 without changes in these risk factors. Our results do not imply that life expectancy will fall; more likely, life expectancy will continue to rise but less rapidly than it otherwise would.
The hypothetical scenario in which everyone is a nonsmoker of normal weight by 2020, though perhaps not achievable, illustrates the dramatic toll these behavioral risk factors can take when combined. Perfect control of these risk factors would add more than 5 years of quality-adjusted life.
Our forecasts suggest that if past trends continue, almost half the U.S. adult population will meet the WHO criteria for obesity by 2020, a prediction consistent with that made by Wang and colleagues.34 That said, it is difficult to predict future trends in smoking and obesity with accuracy. Risk-factor trends are susceptible to policy and environmental factors, and there is evidence that the rate of increase in BMI may be decelerating.31,32 However, increases in BMI among adults are likely to occur with the maturation of the current cohort of U.S. children, among whom obesity rates are at a historical high.22 In addition, sensitivity analyses using different historical rates of change in risk factors show that the negative effects of trends in obesity continue to outweigh the positive effects of declines in smoking as long as the increases in BMI exceed even minimal levels.
Although adverse behavioral risk factors cannot be completely eliminated, even modest weight loss35 and reductions in smoking at the individual level12 can have substantial effects on population health. Research has shown the clinical efficacy of several interventions in achieving smoking cessation36 and weight control.35,37–39 The challenge is to increase the use of these interventions40 while continuing to develop and test others. Effective public health and behavioral interventions are crucial for fostering continued efforts to curtail smoking41 and addressing the roots of obesity, which include sedentary lifestyles, the widespread availability of high-calorie food in large portions, and reduced time for the preparation of food at home.32,42–45
Since most of the negative effects of obesity on health are manifested in chronic diseases, it is encouraging that control of other risk factors for cardiovascular disease, such as high cholesterol and hypertension, has improved over the past 40 years, particularly among those who are overweight or obese.46 An important exception to this trend is diabetes,46,47 the prevalence of which is at an all-time high and continues to increase rapidly. Improved treatment of obesity-related diseases is thus vital to improving the nation’s health.
Our study examined the joint effect of trends in obesity and smoking on length and quality of life in the United States. In another study, investigators estimated the effect of these trends on disability-adjusted life expectancy in the Netherlands.48 Their findings were similar in magnitude and direction to ours, despite the marked difference in their methods, which were based on a microsimulation model of chronic disease. An important strength of our study was the use of nationally representative data as a base for forecasts and underlying rates. Basing our projections on simultaneous historical trends in smoking and obesity, we were able to incorporate factors such as the weight gain among smokers who quit.49
Our study also has some limitations. Although it quantifies the effects of obesity and smoking, it cannot account for the many other factors that determine life expectancy and quality of life, such as advances in medicine and public health. Historically, the positive effects of these factors have overwhelmed the negative effects of smoking and obesity; our results are depicted relative to an assumed continuation of this trend. There is ongoing debate about the effect of different BMI levels on the risk of death.5,50 However, the relative risks of death in our study come directly from nationally representative data, and sensitivity analyses using other published data on relative risks show that our findings are robust.21,48 As with past studies,3,4,21,33 our mortality analyses did not include socioeconomic status, although alternative analyses controlling for education yielded very similar results (see Table A3 in the Supplementary Appendix). Our quality-of-life estimates are cross-sectional, since prospective studies were not available to measure the joint effects of smoking and obesity in a nationally representative sample. Comparison with data from a prospective study of quality of life and weight loss suggests that the actual changes in quality of life associated with weight loss or gain may be greater than we estimate.51
The forecasts reported are at a population level and do not apply to a particular person who loses weight or stops smoking. We also made some assumptions that are typical for population-level estimates.1–4,8,11 For example, we assume that the risk of death increases instantaneously when a BMI threshold is crossed. However, because the baseline risk is relatively low, actual increases in mortality are not observed right away. In addition, although we simulate changes in smoking and BMI in each future year, our forecasts for each year assume that smoking and obesity status remain unchanged throughout a person’s life. Finally, our forecasts are not stratified by socioeconomic status or race.8,32,52,53 BMI has increased disproportionately among blacks, which may further heighten disparities in the future.
In conclusion, the detrimental effect of increases in obesity rates on population health is tempered only somewhat by the decline in the prevalence of smoking. Efforts to improve health should focus on stabilization or reversal of trends in BMI, continued reductions in tobacco use, and better control of the clinical risk factors associated with obesity and smoking. Inadequate progress in these areas could result in an erosion of the pattern of steady gains in health observed in the United States since the early 20th century.
Supplementary Material
Acknowledgments
Supported by grants from the National Institute on Aging (P01AG031098, P30AG012810, and P01AG005842), the Harvard Interfaculty Program for Health Systems Improvement, and the Lasker Foundation.
We thank Raghunathan Trivellore for advice on statistical analysis and Marcelo Coca and Jean Roth for assistance with portions of data analysis.
Footnotes
No potential conflict of interest relevant to this article was reported.
References
- 1.Mokdad AH, Marks JS, Stroup DF, Gerberding JL. Actual causes of death in the United States, 2000. JAMA. 2004;291:1238–1245. doi: 10.1001/jama.291.10.1238. [DOI] [PubMed] [Google Scholar]
- 2.Idem. Correction: actual causes of death in the United States, 2000. JAMA. 2005;293:293–294. doi: 10.1001/jama.293.3.293. [DOI] [PubMed] [Google Scholar]
- 3.Flegal KM, Graubard BI, Williamson DF, Gail MH. Excess deaths associated with underweight, overweight, and obesity. JAMA. 2005;293:1861–1867. doi: 10.1001/jama.293.15.1861. [DOI] [PubMed] [Google Scholar]
- 4.Allison DB, Fontaine KR, Manson JE, Stevens J, VanItallie TB. Annual deaths attributable to obesity in the United States. JAMA. 1999;282:1530–1538. doi: 10.1001/jama.282.16.1530. [DOI] [PubMed] [Google Scholar]
- 5.Manson JE, Bassuk SS, Hu FB, Stampfer MJ, Colditz GA, Willett WC. Estimating the number of deaths due to obesity: can the divergent findings be reconciled? J Womens Health (Larchmt) 2007;16:168–176. doi: 10.1089/jwh.2006.0080. [DOI] [PubMed] [Google Scholar]
- 6.Silverstein MD, Nietert PJ, Zoller JS, Silvestri GA. Predicted impact of attaining smoking reduction goals on mortality. South Med J. 2001;94:176–183. [PubMed] [Google Scholar]
- 7.Warner KE. Health and economic implications of a tobacco-free society. JAMA. 1987;258:2080–2086. [PubMed] [Google Scholar]
- 8.Olshansky SJ, Passaro DJ, Hershow RC, et al. A potential decline in life expectancy in the United States in the 21st century. N Engl J Med. 2005;352:1138–1145. doi: 10.1056/NEJMsr043743. [DOI] [PubMed] [Google Scholar]
- 9.Groessl EJ, Kaplan RM, Barrett-Connor E, Ganiats TG. Body mass index and quality of well-being in a community of older adults. Am J Prev Med. 2004;26:126–129. doi: 10.1016/j.amepre.2003.10.007. [DOI] [PubMed] [Google Scholar]
- 10.Jia H, Lubetkin EI. The impact of obesity on health-related quality-of-life in the general adult US population. J Public Health (Oxf) 2005;27:156–164. doi: 10.1093/pubmed/fdi025. [DOI] [PubMed] [Google Scholar]
- 11.Kaplan RM, Anderson JP, Kaplan CM. Modeling quality-adjusted life expectancy loss resulting from tobacco use in the United States. Soc Indic Res. 2007;81:51–64. [Google Scholar]
- 12.Wilson D, Parsons J, Wakefield M. The health-related quality-of-life of never smokers, ex-smokers, and light, moderate, and heavy smokers. Prev Med. 1999;29:139–144. doi: 10.1006/pmed.1999.0523. [DOI] [PubMed] [Google Scholar]
- 13.Lakdawalla DN, Goldman DP, Shang B. The health and cost consequences of obesity among the future elderly. Health Aff (Millwood) 2005;24(Suppl 2):W5R30–W5R41. doi: 10.1377/hlthaff.w5.r30. [DOI] [PubMed] [Google Scholar]
- 14.Atlanta: Centers for Disease Control and Prevention; [Accessed September 30, 2009]. Chronic disease prevention and health promotion: chronic disease overview. (at http://www.cdc.gov/nccdphp/overview.htm#2.) [Google Scholar]
- 15.Ogden CL, Yanovski SZ, Carroll MD, Flegal KM. The epidemiology of obesity. Gastroenterology. 2007;132:2087–2102. doi: 10.1053/j.gastro.2007.03.052. [DOI] [PubMed] [Google Scholar]
- 16.Rockville, MD: Agency for Healthcare Research and Quality; [Accessed September 30, 2009]. Medical Expenditure Panel Survey: background. (at http://www.meps.ahrq.gov/mepsweb/about_meps/survey_back.jsp.) [Google Scholar]
- 17.Atlanta: Centers for Disease Control and Prevention; [Accessed September 30, 2009]. National Health and Nutrition Examination Survey: questionnaires, datasets, and related documentation. (at http://www.cdc.gov/nchs/nhanes/nhanes_questionnaires.htm.) [Google Scholar]
- 18.Atlanta: Centers for Disease Control and Prevention; [Accessed September 30, 2009]. National Health Interview Survey: questionnaires, datasets, and related documentation. (at http://www.cdc.gov/nchs/nhis/nhis_questionnaires.htm.) [Google Scholar]
- 19.Ezzati-Rice TM, Rohde F, Greenblatt J. Methodology report no. 22. March 2008. Rockville, MD: Agency for Healthcare Research and Quality; 2008. Mar, [Accessed September 30, 2009]. Sample design of the Medical Expenditure Panel Survey household component, 1998–2007. (at http://www.meps.ahrq.gov/mepsweb/data_files/publications/mr22/mr22.pdf.) [Google Scholar]
- 20.Geneva: World Health Organization; 2000. Obesity: preventing and managing the global epidemic. [PubMed] [Google Scholar]
- 21.Freedman DM, Sigurdson AJ, Rajaraman P, Doody MM, Linet MS, Ron E. The mortality risk of smoking and obesity combined. Am J Prev Med. 2006;31:355–362. doi: 10.1016/j.amepre.2006.07.022. [DOI] [PubMed] [Google Scholar]
- 22.Ogden C, Fryar C, Carroll M, Flegal K. Mean body weight, height, and body mass index, United States 1960–2002. Hyattsville, MD: National Center for Health Statistics; 2004. [PubMed] [Google Scholar]
- 23.National Health Interview Survey: adult tobacco use information, smoking status recodes. [Accessed November 4, 2009]; (at http://www.cdc.gov/nchs/nhis/tobacco/tobacco_recodes.htm.)
- 24.Rockville, MD: Agency for Healthcare Policy and Research; 1997. [Accessed November 5, 2009]. Methodology report #1: design and methods of the Medical Expenditure Panel Survey household component. (at http://www.meps.ahrq.gov/mepsweb/data_files/publications/mr1/mr1.shtml.) [Google Scholar]
- 25.Brooks R, Rabin RE, de Charro F, editors. The measurement and valuation of health status using EQ-5D: a European perspective. Dordrecht, the Netherlands: Kluwer Academic; 2003. [Google Scholar]
- 26.United States life tables, 2004. Natl Vital Stat Rep. 2007;56(9):1–39. [PubMed] [Google Scholar]
- 27.Baltimore: Social Security Administration; [Accessed November 5, 2009]. Social Security Administration annual statistical supplement, 2008. (at http://www.ssa.gov/policy/docs/statcomps/supplement/2008/4c.pdf.) [Google Scholar]
- 28.U.S. Census Bureau. Census 2000, summary file 1: sex by age, total population. [Accessed September 30, 2009]; (at http://factfinder.census.gov.)
- 29.Korn EL, Graubard BI, Midthune D. Time-to-event analysis of longitudinal follow-up of a survey: choice of time scale. Am J Epidemiol. 1997;145:72–80. doi: 10.1093/oxfordjournals.aje.a009034. [DOI] [PubMed] [Google Scholar]
- 30.Stewart ST, Woodward RM, Rosen AB, Cutler DM. The impact of symptoms and impairments on overall health in US national health data. Med Care. 2008;46:954–962. doi: 10.1097/MLR.0b013e318179199f. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Ogden C, Carroll M, McDowell M, Flegal K. Obesity among adults in the United States — no change since 2003– 2004. Hyattsville, MD: National Center for Health Statistics; 2007. [Google Scholar]
- 32.Komlos J, Breitfelder A, Sunder M. The transition to post-industrial BMI values among US children. Am J Hum Biol. 2009;21:151–160. doi: 10.1002/ajhb.20806. [DOI] [PubMed] [Google Scholar]
- 33.van Dam RM, Li T, Spiegelman D, Franco OH, Hu FB. Combined impact of lifestyle factors on mortality: prospective cohort study in US women. BMJ. 2008;337:a1440. doi: 10.1136/bmj.a1440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Wang YC, Colditz GA, Kuntz KM. Forecasting the obesity epidemic in the aging U.S. population. Obesity (Silver Spring) 2007;15:2855–2865. doi: 10.1038/oby.2007.339. [DOI] [PubMed] [Google Scholar]
- 35.Orzano AJ, Scott JG. Diagnosis and treatment of obesity in adults: an applied evidence-based review. J Am Board Fam Pract. 2004;17:359–369. doi: 10.3122/jabfm.17.5.359. [DOI] [PubMed] [Google Scholar]
- 36.Fiore M, Jaén C, Baker T, et al. Treating tobacco use and dependence: 2008 update. Rockville, MD: Department of Health and Human Services; 2008. May, [Google Scholar]
- 37.Eckel RH. Nonsurgical management of obesity in adults. N Engl J Med. 2008;358:1941–1950. doi: 10.1056/NEJMcp0801652. [DOI] [PubMed] [Google Scholar]
- 38.Clinical guidelines on the identification, evaluation, and treatment of overweight and obesity in adults — the Evidence Report. Obes Res. 1998;6(Suppl 2):51S–209S. [Erratum, Obes Res 1998;6:464.] [PubMed] [Google Scholar]
- 39.Volpp KG, John LK, Troxel AB, Norton L, Fassbender J, Loewenstein G. Financial incentive-based approaches for weight loss: a randomized trial. JAMA. 2008;300:2631–2637. doi: 10.1001/jama.2008.804. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Fiore MC, Jaén CR. A clinical blue-print to accelerate the elimination of tobacco use. JAMA. 2008;299:2083–2085. doi: 10.1001/jama.299.17.2083. [DOI] [PubMed] [Google Scholar]
- 41.Warner KE, editor. Tobacco control policy. San Francisco: Jossey-Bass; 2006. [Google Scholar]
- 42.Cutler DM, Glaeser EL, Shapiro JM. Why have Americans become more obese? J Econ Perspect. 2003;17:93–118. [Google Scholar]
- 43.Bleich S, Cutler D, Murray C, Adams A. Why is the developed world obese? Annu Rev Public Health. 2008;29:273–295. doi: 10.1146/annurev.publhealth.29.020907.090954. [DOI] [PubMed] [Google Scholar]
- 44.Swinburn BA. Obesity prevention: the role of policies, laws and regulations. Aust New Zealand Health Policy. 2008;5:12. doi: 10.1186/1743-8462-5-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.James WP. The epidemiology of obesity: the size of the problem. J Intern Med. 2008;263:336–352. doi: 10.1111/j.1365-2796.2008.01922.x. [DOI] [PubMed] [Google Scholar]
- 46.Gregg EW, Cheng YJ, Cadwell BL, et al. Secular trends in cardiovascular disease risk factors according to body mass index in US adults. JAMA. 2005;293:1868–1874. doi: 10.1001/jama.293.15.1868. [Erratum, JAMA 2005;294:182.] [DOI] [PubMed] [Google Scholar]
- 47.Mokdad AH, Bowman BA, Ford ES, Vinicor F, Marks JS, Koplan JP. The continuing epidemics of obesity and diabetes in the United States. JAMA. 2001;286:1195–1200. doi: 10.1001/jama.286.10.1195. [DOI] [PubMed] [Google Scholar]
- 48.van Baal PH, Hoogenveen RT, de Wit GA, Boshuizen HC. Estimating health-adjusted life expectancy conditional on risk factors: results for smoking and obesity. Popul Health Metr. 2006;4:14. doi: 10.1186/1478-7954-4-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Flegal KM. The effects of changes in smoking prevalence on obesity prevalence in the United States. Am J Public Health. 2007;97:1510–1514. doi: 10.2105/AJPH.2005.084343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Flegal KM, Graubard BI, Williamson DF, Gail MH. Weight-associated deaths in the United States. J Womens Health (Larchmt) 2007;16:1368–1370. doi: 10.1089/jwh.2007.0547. [DOI] [PubMed] [Google Scholar]
- 51.Hertzman P. The cost effectiveness of orlistat in a 1-year weight-management programme for treating overweight and obese patients in Sweden: a treatment responder approach. Pharmacoeconomics. 2005;23:1007–1020. doi: 10.2165/00019053-200523100-00004. [DOI] [PubMed] [Google Scholar]
- 52.Freedman DS, Khan LK, Serdula MK, Ogden CL, Dietz WH. Racial and ethnic differences in secular trends for childhood BMI, weight, and height. Obesity (Silver Spring) 2006;14:301–308. doi: 10.1038/oby.2006.39. [DOI] [PubMed] [Google Scholar]
- 53.Wang Y, Beydoun MA, Liang L, Caballero B, Kumanyika SK. Will all Americans become overweight or obese? Estimating the progression and cost of the US obesity epidemic. Obesity (Silver Spring) 2008;16:2323–2330. doi: 10.1038/oby.2008.351. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.