Introduction
Parental stress resulting from experiences with infants hospitalized in the NICU is well documented.1–5 Stress emanating from the birth of a premature or sick neonate has received considerable attention and is associated with concurrent parental anxiety and depression.1,6–9 Less well studied is the relationship of parental NICU stress with fatigue and sleep disruption. Lee and others report high rates of sleep disturbance, including average sleep duration less than 7 hours/night, in mothers of infants hospitalized in the NICU, as well as elevated fatigue and reduced wellbeing.10,11 The National Sleep Foundation cites 7–8 hours/night as the basic sleep need in adults.12 Sleep is a particular concern given the prevalence of postpartum sleep problems (57.7%) and complex relationship between postpartum sleep and depression.13
Parental stress emanating from the NICU experience is important, potentially impacting parenting behavior as well as producing long term emotional problems and health alteration. Early work by Miles14 provides a model of pathways influencing parental responses and parenting premature infant. Parent stress, anxiety, depression, and fatigue alter parenting behavior and perception of parental competence, parent-infant interaction, and ultimately infant outcomes such as cognitive development, emotional regulation, and health.4,15–19 Miles7 identified increased odds of depression related to parental role alteration and worry about child health among NICU parents. In this same study, although depression declined over time following the infant’s discharge from the NICU, 13% of mothers remained depressed 27 months following birth and individual trajectories were noted. In work by Holditch-Davis and others individual patterns of maternal distress following the birth a premature infant did not consistently decline over time and there were distinct groups of mothers with differing trajectories of distress and subsequent effects on parenting.1 Combined, these findings not only document stress experienced by parents of NICU infants but also highlight emotional consequences and the individual nature of parent response to the NICU experience.
Notably the NICU experience is associated with long term parent emotional effects. Research suggests parent responses are not limited to the period of hospitalization and that the NICU experience is associated with disorders such as acute stress disorder (ASD) and post-traumatic stress disorder (PTSD).20,21 In one study 15% of mothers and 8% of fathers demonstrated evidence of PTSD when evaluated 30 days after their infants’ NICU admission.22 Mothers of preterm infants demonstrate significant stress reactions 6 months following the infants’ expected due date.20 and in another study mothers continued to experience distress and evidenced alterations in parenting 24 months after the infant’s due date.1 When compared with low-income mothers of healthy infants, low-income NICU mothers demonstrated an increased rate of ASD (3% vs. 23%).23
Evidence suggests that emotional stress may not abate over time and that parents are at risk for delayed response.4,22–24 Further, the pattern of stress experienced may differ for mothers and fathers. In a study of PTSD occurrence following parental NICU experience, measured using the Stanford Acute Stress Reaction Questionnaire, fathers had increased PTSD scores at four months following their child’s birth. In this same study 33% of fathers, compared with 9% of mothers, met criteria for diagnosis of PTSD.24
Based on current knowledge, evaluation of parents during infant NICU hospitalization is needed to assess current responses to stress associated with the NICU experience and to identify parents at risk for extended physical and emotional consequences. Such clinical evaluation requires instrumentation that not only is both psychometrically solid but also offers straightforward administration and scoring as well as providing population norms for comparison. An instrument that meets psychometric measurement requirements must be valid and reliable. Instruments available from the NIH funded Patient Reported Outcomes Measurement Information System (PROMIS) are valid, reliable, and efficient and meet these requirements.25–27
The purpose of this study was to test the relationship between stress associated with hospitalization of an infant in the neonatal intensive care unit (NICU) and parent responses. Studied parent responses were anxiety, depression, fatigue, and sleep disruption measured using PROMIS (Patient Reported Outcomes Measurement Information System) instruments. Research questions included: (1) What are the relationships among parental sources of stress (infant behavior and appearance, NICU sights and sounds, and alteration of parental role)? (2) What are the relationships among parental responses to NICU stress (sleep disturbance, fatigue, anxiety, and depression)? (3) What is the relationship of NICU parent stress (infant behavior and appearance, NICU sights and sounds, and alteration of parental role) with anxiety, depression, fatigue, and sleep disruption?
Materials and Method
Design and Subjects
Data were collected in a 32-bed, Level III NICU using an exploratory design. The study was approved by the University of Washington institutional review board. Parents who were age ≥ 18 years, literate in English or Spanish, and whose infant was hospitalized in the unit were invited to participate. Parents of infants considered in medical crisis (i.e., life-threatening circumstance) per determination of the charge nurse were not approached for participation. These parents were excluded to avoid unnecessary burden during a particularly challenging time.
Instruments
Parental Stressor Scale
Sources of parent stress were measured using the Parental Stressor Scale: Neonatal Intensive Care Unit (PSS: NICU, 2002), a well-established self report survey in which parents rated sources of stress using a Likert scale (1 = not at all stressful, 5 = extremely stressful) within three domains – Infant Behavior and Appearance (17 items), Sights and Sounds (6 items), Parental Role Alteration (11 items).28 Parents were asked to mark only those events they had experienced or that were relevant to their NICU stay per standard administration protocol. Construct validity of the PSS:NICU has been demonstrated through correlation with measures of state anxiety (r = 0.46–0.61, p < 0.001).5 Internal consistency of the PSS:NICU is reported as alpha > 0.70 for all domain scales and alpha = 0.89–0.90 for the entire instrument.28 Mean scores were calculated within domains.
PROMIS
The Patient Reported Outcomes Measurement Information System (PROMIS) was developed by a consortium of investigators working at twelve primary research sites across the country to provide unified, efficient, reliable, and valid measures of self-reported health for use by clinicians and researchers.26 PROMIS instruments assess self-reported health in three primary areas and seven subdomains: Physical Health – symptoms, function; Mental Health – affect, behavior, cognition, and Social Health – relationship, function.26 PROMIS instruments are available for online use or as printed hard copy and include short form or computerized adaptive tests (CAT). Although the majority of current PROMIS instruments are designed for adults, a number are available for pediatric applications and a number of instruments have been translated for non-English speaking respondents. The PROMIS short form instruments range from four to ten items and cover a wide range of outcomes such as cognition, pain, emotional distress, physical function, sexual function, social role participation, and illness impact. The following PROMIS short forms were utilized to quantify health outcomes: Sleep-Disturbance (8 items), Fatigue (7 items), Anxiety (7 items), Depression (8 items). Development of the PROMIS instruments, along with validity and reliability testing, have been reported.25,27,29–31 PROMIS measures have been tested extensively in large diverse samples drawn from the general population and clinical groups and validity has been demonstrated by correlation with well-standardized measures.25; 32 Results of such testing follow: PROMIS depression test bank items correlation with the Center for Epidemiological Studies-Depression (CESD) r = 0.83 (n = 782); PROMIS anxiety test bank items correlation with the Mood and Anxiety Symptom Questionnaire (MASQ) r = 0.80 (n = 788); PROMIS sleep disturbance test bank items correlated with the Pittsburgh Sleep Quality Index (PSQI) r = 0.85 (n = 2252); short form PROMIS fatigue scale correlated with the FACIT-Fatigue Scale r = 0.91 (n = 9047). Responses for each PROMIS measure were summed to form a raw score and converted to a T score (standardized score) using tables available through the PROMIS web site. For all PROMIS instrument T-scores the population mean = 50 and standard deviation = 10. Thus a T-score of 60 indicates a score 1 standard deviation about the population mean.
Demographic survey
Respondents provided information about their infant’s birth and health status, age, marital status, ethnicity and race, education, occupation, residence distance from the NICU and time spent with the infant, and family members. Additionally parents added comments in an open ended portion of the demographic survey.
Procedure
Investigators made biweekly rounds and approached eligible parents, using an approved script, to elicit possible interest in the study. Parents were then provided with a packet containing an information sheet describing the study, study instruments, and an envelope to be used in returning responses anonymously to a drop box at the unit front desk. The packet also contained a $5 gift card for the hospital coffee shop. Spanish speaking parents were offered instruments in Spanish; approach and consent discussions occurred in Spanish provided by a Spanish-speaking investigator. Official Spanish versions of the PSS:NICU and PROMIS instruments, available from the PROMIS website, were employed;26 other study materials were translated into Spanish by a Spanish-speaking member of the research team and back translated for accuracy. For back translation, the Spanish versions of the instruments were translated into English and this English version was then compared with the original English text.
Results
Demographic characteristics describing the 30 parents who participated in the project are provided in Table 1. Four respondents chose to complete the survey in Spanish. The sample was predominantly married or partnered (n = 26, 86.7%), white, and educated (n = 27, 75.9 % high school or higher level of education). A third of the sample lived greater than 50 miles from the medical center. The majority of parent respondents (n = 24, 80%) reported coming to the NICU more than 5 times per week, and spending more than 30 hours per week (n = 19, 63.4%) with their infant. Thirteen respondents (43.3%) had one or more children at home (range 1 to 6 other children). The majority of infants were 28 to 36 weeks gestation at birth (n = 20, 66.7%; mean 30.2 wks), hospitalized from 4 to 110 days (mean (SD) = 24.7 (17)), and born by cesarean birth (n = 20, 66.7%).
Table 1.
Demographic characteristics (N = 30).
| Variable | n | Mean (SD) | Min, Max |
|---|---|---|---|
| Parent age (yrs) | 30 | 32.17 (7.49) | 18, 44 |
| Time in unit (days) | 29 | 24.66 (17.0) | 4,110 |
| % | |||
| Parent | 22 | Mother | 73.3 |
| 8 | Father | 26.7 | |
| Race, ethnicity | 20 | White | 66.7 |
| 6 | Hispanic | 20.7 | |
| 2 | Asian | 6.9 | |
| 1 | Native American | 3.4 | |
| Marital status | 26 | Married/partnered | 86.7% |
| Education | 2 | < high school | 6.9 |
| 10 | High school | 34.5 | |
| 17 | > high school | 41.4 | |
| Distance from hospital | 4 | 0–10 mile | 13.3 |
| 8 | 11–20 | 26.7 | |
| 3 | 21–30 | 10 | |
| 5 | 31–40 | 16.7 | |
| 10 | > 50 miles | 33.3 | |
| Visits to NICU (fr) | 1 | 0–2/wk | 3.3 |
| 5 | 3–5/wk | 16.7 | |
| 24 | > 5/wk | 80 | |
| Visits (hrs/wk) | 1 | 0–5 | 3.3 |
| 3 | 6–10 | 10 | |
| 4 | 11–20 | 13.3 | |
| 3 | 21–30 | 10 | |
| 8 | 31–40 | 26.7 | |
| 11 | > 40 | 36.7 | |
| Gestational age | 8 | < 28 wks | 26.7 |
| 20 | 28–36 wks | 66.7 | |
| 2 | 37–42 | 6.7 | |
Instrument reliability, determined using Cronbach’s alpha, was as follows for the PROMIS scales: Sleep Disturbance 0.897, Fatigue 0.879, Anxiety 0.890, and Depression 0.891. PSS:NICU subscale reliability was: Sights and Sounds 0.738, Infant Behavior and Appearance 0.861, Parental Role Alteration 0.847. Note that reliability for the PSS was calculated using coding Metric 2 (“not applicable” coded as 1; represents the overall stress level related to the NICU environment) as described by the tool’s author.28
The relationships among sample characteristics, PROMIS scales, and the PSS:NICU were assessed using correlation. The convenience sample of n = 30 provided power of 0.90 to detect a large effect size (r = 0.50) at a 0.05 significance level. The analysis was focused on large effect size and resultant ability to explain a large proportion of variance which increases the clinical significance of findings. Before addressing the research questions, the correlations between sample characteristics, PROMIS scales, and the PSS: NICU were evaluated. There were no significant correlations of responding parents’ age, education, language, length of hospitalization, and infant gestational age with PSS:NICU or PROMIS scores. Fatigue was correlated with sample characteristics as follows: increased fatigue was associated with shorter distance from the medical center (r = −0.418, p = 0.021), increased number of trips to the unit (r = 0.410, p = 0.024), and increased hours spent in the unit (r = 0.417, p = 0.022). Other children in the family was correlated with anxiety (r = 0.439, p 0.022) but not with any other outcome variable. Respondents completing instruments were both mothers 22 (73.3%) and fathers 8 (26.7%).
Descriptive information for study variables along with the correlation structure among anxiety, depression, fatigue, sleep disturbance and parent stress are provided in Table 2. The relationships among parental sources of stress (research question 1) are shown in the correlations among the subscales of the PSS: NICU. Alteration in parenting role was the largest source of parental stress (mean score 3.25 (SD 0.99)) (Table 2) while sights and sounds of the NICU ranked lowest as a source of stress (mean score 2.374 (0.81)). All of the PSS: NICU subscales (infant behavior and appearance, NICU sights and sounds, and alteration of parental role) are significantly correlated (r = 0.719 to 0.941). The second research question focuses on the relationships among parents’ responses to NICU stress. Parents reported experiences of anxiety, depression, fatigue, and sleep disturbance (Table 2, Figure 1). There was significant correlation among all of the PROMIS scales (sleep disturbance, depression, anxiety, fatigue) (r = 0.424 to 0.735).
Table 2.
Descriptive data and correlation of PROMIS and PSS:NICU (N = 30).
| Descriptive Statistics | PROMIS Subscale Correlation (r) | PSS: NICU × PROMIS Correlation (r) | |||||||
|---|---|---|---|---|---|---|---|---|---|
| PROMIS (raw scores) | Mean (SD) | Min, max | Depression | Fatigue | Sleep disturbance | Sights & sounds | Infant appearance | Parent role | Total stress |
| Anxiety1 | 21.96 (4.97) | 12, 32 | 0.735** | 0.427* | 0.509** | 0.377 | 0.615** | 0.602** | 0.606** |
| Depression | 17.77 (6.92) | 8, 33 | – | 0.424* | 0.446* | 0.158 | 0.373* | 0.387* | 0.361* |
| Fatigue | 20.80 (6.18) | 10, 34 | – | – | 0.439* | 0.144 | 0.257 | 0.370* | 0.333 |
| Sleep disturbance | 27.17 (6.26) | 16, 40 | – | – | – | 0.303 | 0.595** | 0.600** | 0.595** |
| PSS: NICU | Mean (SD) | Min, max | PSS: NICU Subscale Correlation (r) | ||||||
| Sights & sounds | 2.37 (0.81) | 1.00, 3.83 | – | – | – | – | 0.719** | 0.719** | 0.837** |
| Infant appearance | 3.09 (0.88) | 1.5, 4.5 | – | – | – | – | – | 0.822** | 0.941** |
| Role | 3.25 (0.99) | 1.13, 5.0 | 0.941** | ||||||
| Total stress | 3.01 (0.83) | 1.29, 4.29 | – | ||||||
≤ .05
< .01
n = 27, all other scales N = 30
Figure 1.
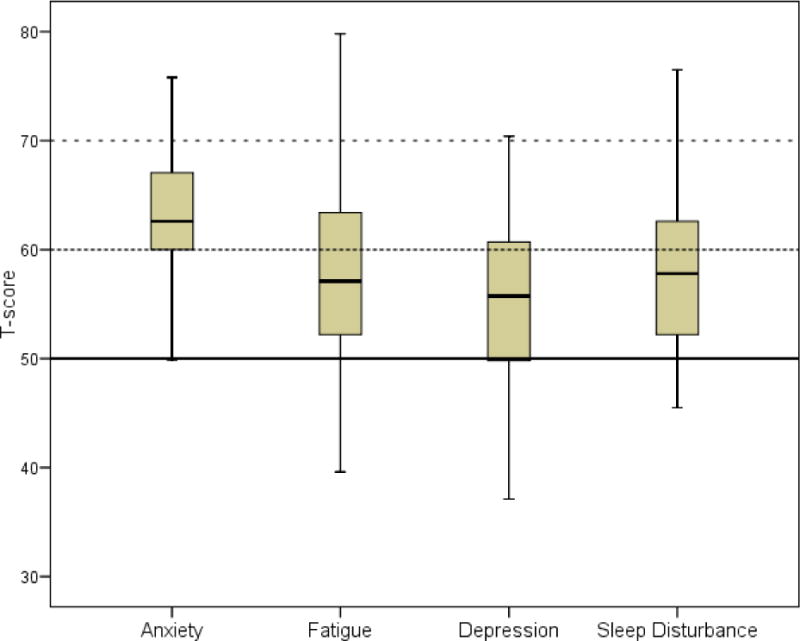
Boxplot of parent PROMIS T-Scores evaluated against general populations scores.
Note: Boxplot of parent scores, median = line within box, interquartile range = shaded box, vertical lines = minimum, and maximum. Population horizontal lines, mean = 50 (solid horizontal line) and mean plus 1 SD (60, dotted line) and mean plus 2 SD’s (70, dashed line).
The correlations between the PSS: NICU and PROMIS scales were examined to answer the third research question, the relationship between parent stress and parent responses. While NICU Sights and Sounds were not significantly correlated with parent outcomes, Infant Behavior and Appearance, Parental Role Alteration, and Total Score were significantly correlated with anxiety, depression, and sleep disturbance and Parental Role Alteration was significantly related with fatigue (Table 2).
Parents’ PROMIS raw scores were converted into T-scores using the table of published values32 and plotted to illustrate anxiety, depression, fatigue, and sleep disturbance compared to national values (Figure 1). Population T-scores are centered with a mean of 50 and standard deviation (SD) of 10 (i.e. mean + 1 SD = 60; mean + 2 SD’s = 70). Sample median values for anxiety, depression, fatigue, and sleep disturbance all exceeded the population mean. Parent anxiety is clearly evident, with the entire sample above the population mean. The frequency (and percentage) of subjects with PROMIS T-scores greater than one and two SD above the population are provided in Table 3. The distribution of parent responses was further explored using cluster analysis, a type of exploratory analysis that identifies groups within a sample demonstrating similar characteristics. Using cluster analysis the parents fell into two groups differentiated by high (n = 16) and low (n = 14) T-scores for depression, anxiety, fatigue, and sleep disturbance. In cluster analysis the metric distance measures the dissimilarity between groups. The distance between the above two clusters of parents was 19.52.
Table 3.
Parent PROMIS T-scores larger than general population mean.
| > 1 SD | > 2 SD | |||
|---|---|---|---|---|
| Variable | n | % | n | % |
| Anxiety | 15 | 55.6 | 3 | 11.1 |
| Depression | 8 | 26.7 | 2 | 6.7 |
| Fatigue | 12 | 40.0 | 3 | 10.0 |
| Sleep disturbance | 11 | 36.7 | 1 | 3.3 |
Discussion
The philosophy of family-centered care in the NICU hinges on parent involvement in care and support for parents.33 Identification of parents at risk for severe responses is essential to direct nursing actions that may reduce parental stress, decrease untoward responses and improve both parental health and parenting behavior.
The magnitude of parent sources of stress in the current study, assessed by the PSS:NICU, was similar to that reported in previous publications, with alteration in parenting role a leading source of stress also detected in these studies.3,5,28,34 Simply stated, parents find it difficult to carry out parenting activities in the critical care setting. The occurrence of anxiety, depression, fatigue, and sleep disturbance among parents of NICU infants, demonstrated in prior studies,1,6–11 was also revealed in the PROMIS measures used in the current study. Parents of NICU patients experience a combination of related emotional responses and alteration in sleep. The current study is unique in utilizing the clinically relevant PROMIS measures to document these responses and in providing evidence of the constellation of anxiety, depression fatigue, and sleep disruption experienced by parents in the NICU. Our data from the PROMIS measures show that parents experience a combination of responses and PROMIS T scores illustrate that these responses exceed national values.
The PROMIS instruments are publically available, easily administered and scored, and interpretable. The PROMIS instruments provide clinicians with outcome measures that may be used to evaluate care as well as provide benchmarks for quality improvement. In addition to research applications, findings illustrate how the PROMIS instruments and T scores could be used clinically to identify parents experiencing heightened responses and to provide intervention and referral for services, particularly for treatment for anxiety and depression. Fatigue and sleep disturbance scores could guide parent support measures delivered by critical care nurses as well as counseling parents on self-care. Although clinical cut-off scores have not been developed for the PROMIS instruments, use of the T-scores and comparison to national statistics allows identification of scores one or two standard deviations above the mean. Nurses may assist parents in developing a visiting pattern that promotes attachment with the infant while assuring adequate rest for parents. Assurance that the nurse will phone parents if the infant’s condition deteriorates may increase parents’ comfort when unable to be at the infant’s bedside, particularly at night. As possible, providing parents with in-unit napping opportunities may reduce fatigue. Provision of competent care in a calm and reassuring manner as well as clear communication and careful explanations geared to parental comprehension capability may reduce parental anxiety. Interventions addressing NICU parent stress, depression, and anxiety have been shown to not only improve parent outcomes but infant outcomes as well.15,35
Limitations
These exploratory findings are taken from a study within a single NICU and involved a limited sample size. Given the small sample size and the fact that only one parent per infant provided data, differences between father and mother responses and differences within couples could not be determined. Because prior research has shown discrepancies between the magnitude and pattern of mother and father responses24 future research should evaluate the constellation of responses experienced by both parents. Further study should include a broader range of units. Parents of infants experiencing life-threatening conditions were not included. This at risk group requires additional consideration.
Conclusion
In conclusion, stress experienced by parents whose infant is hospitalized in the NICU is strongly correlated with anxiety, fatigue, depression, and sleep disruption. Knowledge of these relationships can be used to guide family-focused nursing care in the NICU.
Acknowledgments
The authors appreciate support and guidance provided by the NICU nursing local practice council.
Supported by: Pacific Northwest Association of Neonatal Nurses; P30 NR011400 (Thomas) and F31-NR011365 (Thorngate) awarded by National Institute for Nursing Research.
Biography
Morgan Busse and Kayleigh Stromgren are 2011 BSN graduates of the University of Washington School of Nursing. Ms Busse is currently a staff nurse in a maternal-infant unit at Group Health Cooperative and Ms Stromgren is staff nurse in neonatal intensive care at University of Washington Medical Center. Lauren Thorngate is a doctoral candidate studying effects of opioid administration on premature infant neural organization and Karen Thomas is a faculty member, both at the University of Washington Department of Family and Child Nursing
Footnotes
Conflict of Interest
The authors have no conflict of interest.
Contributor Information
Morgan Busse, Staff Nurse, Group Health Cooperative, Seattle, WA 98101; Home address: 1722 13th Avenue S #C, Seattle, WA 98144.
Kayleigh Stromgren, Staff Nurse, University of Washington Medical Center NICU, Seattle, WA 98195; Home address: 4277 East Lake Sammamish Shore Lane SE, Sammamish, WA 98075.
Lauren Thorngate, Doctoral Student, Department of Family and Child Nursing, University of Washington, Seattle, WA 98195-7262; Home address: 14044 22nd Avenue NE, Seattle, WA 98125.
Karen A. Thomas, Professor, Department of Family and Child Nursing, University of Washington, Seattle, WA 98195-7262; Home address: 24227 26th Avenue SE, Bothell, WA 98021.
References
- 1.Holditch-Davis D, Miles MS, Weaver MA, et al. Patterns of distress in African-American mothers of preterm infants. J Dev Behav Pediatr. 2009 Jun;30(3):193–205. doi: 10.1097/DBP.0b013e3181a7ee53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Trombini E, Surcinelli P, Piccioni A, Alessandroni R, Faldella G. Environmental factors associated with stress in mothers of preterm newborns. Acta Paediatr. 2008 Jul;97(7):894–898. doi: 10.1111/j.1651-2227.2008.00849.x. [DOI] [PubMed] [Google Scholar]
- 3.Dudek-Shriber L. Parent stress in the neonatal intensive care unit and the influence of parent and infant characteristics. Am J Occup Ther. 2004 Sep-Oct;58(5):509–520. doi: 10.5014/ajot.58.5.509. [DOI] [PubMed] [Google Scholar]
- 4.Olshtain-Mann O, Auslander GK. Parents of preterm infants two months after discharge from the hospital: are they still at (parental) risk? Health Soc Work. 2008 Nov;33(4):299–308. doi: 10.1093/hsw/33.4.299. [DOI] [PubMed] [Google Scholar]
- 5.Franck LS, Cox S, Allen A, Winter I. Measuring neonatal intensive care unit-related parental stress. J Adv Nurs. 2005 Mar;49(6):608–615. doi: 10.1111/j.1365-2648.2004.03336.x. [DOI] [PubMed] [Google Scholar]
- 6.Beck CT. Recognizing and screening for postpartum depression in mothers of NICU infants. Adv Neonatal Care. 2003 Feb;3(1):37–46. doi: 10.1053/adnc.2003.50013. [DOI] [PubMed] [Google Scholar]
- 7.Miles MS, Holditch-Davis D, Schwartz TA, Scher M. Depressive symptoms in mothers of prematurely born infants. J Dev Behav Pediatr. 2007 Feb;28(1):36–44. doi: 10.1097/01.DBP.0000257517.52459.7a. [DOI] [PubMed] [Google Scholar]
- 8.Paulson JF, Dauber S, Leiferman JA. Individual and combined effects of postpartum depression in mothers and fathers on parenting behavior. Pediatrics. 2006 Aug;118(2):659–668. doi: 10.1542/peds.2005-2948. [DOI] [PubMed] [Google Scholar]
- 9.Mew AM, Holditch-Davis D, Belyea M, Miles MS, Fishel A. Correlates of depressive symptoms in mothers of preterm infants. Neonatal Netw. 2003 Sep-Oct;22(5):51–60. doi: 10.1891/0730-0832.22.5.51. [DOI] [PubMed] [Google Scholar]
- 10.Lee SY, Kimble LP. Impaired sleep and well-being in mothers with low-birth-weight infants. J Obstet Gynecol Neonatal Nurs. 2009 Nov-Dec;38(6):676–685. doi: 10.1111/j.1552-6909.2009.01064.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lee SY, Lee KA, Rankin SH, Weiss SJ, Alkon A. Sleep disturbance, fatigue, and stress among Chinese-American parents with ICU hospitalized infants. Issues Ment Health Nurs. 2007;28(6):593–605. doi: 10.1080/01612840701354505. [DOI] [PubMed] [Google Scholar]
- 12.National Sleep Foundation. How much sleep do we really need? 2011. 2012 http://www.sleepfoundation.org/article/how-sleep-works/how-much-sleep-do-we-really-need. Accessed July 3, 2012.
- 13.Dorheim SK, Bondevik GT, Eberhard-Gran M, Bjorvatn B. Sleep and depression in postpartum women: a population-based study. Sleep. 2009 Jul 1;32(7):847–855. doi: 10.1093/sleep/32.7.847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Miles MS, Holditch-Davis D. Parenting the prematurely born child: pathways of influence. Semin Perinatol. 1997 Jun;21(3):254–266. doi: 10.1016/s0146-0005(97)80067-5. [DOI] [PubMed] [Google Scholar]
- 15.Melnyk BM, Crean HF, Feinstein NF, Fairbanks E. Maternal anxiety and depression after a premature infant’s discharge from the neonatal intensive care unit: explanatory effects of the creating opportunities for parent empowerment program. Nurs Res. 2008 Nov-Dec;57(6):383–394. doi: 10.1097/NNR.0b013e3181906f59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Feldman R, Eidelman AI. Maternal postpartum behavior and the emergence of infant-mother and infant-father synchrony in preterm and full-term infants: the role of neonatal vagal tone. Dev Psychobiol. 2007 Apr;49(3):290–302. doi: 10.1002/dev.20220. [DOI] [PubMed] [Google Scholar]
- 17.Righetti-Veltema M, Conne-Perreard E, Bousquet A, Manzano J. Postpartum depression and mother-infant relationship at 3 months old. J Affect Disord. 2002;70(3):291–306. doi: 10.1016/s0165-0327(01)00367-6. [DOI] [PubMed] [Google Scholar]
- 18.Dunkel Schetter C, Tanner L. Anxiety, depression and stress in pregnancy: implications for mothers, children, research, and practice. Curr Opin Psychiatry. Mar;25(2):141–148. doi: 10.1097/YCO.0b013e3283503680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Field T. Postpartum depression effects on early interactions, parenting, and safety practices: a review. Infant Behav Dev. Feb;33(1):1–6. doi: 10.1016/j.infbeh.2009.10.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Holditch-Davis D, Bartlett TR, Blickman AL, Miles MS. Posttraumatic stress symptoms in mothers of premature infants. J Obstet Gynecol Neonatal Nurs. 2003 Mar-Apr;32(2):161–171. doi: 10.1177/0884217503252035. [DOI] [PubMed] [Google Scholar]
- 21.Shaw RJ, Deblois T, Ikuta L, Ginzburg K, Fleisher B, Koopman C. Acute stress disorder among parents of infants in the neonatal intensive care nursery. Psychosomatics. 2006 May-Jun;47(3):206–212. doi: 10.1176/appi.psy.47.3.206. [DOI] [PubMed] [Google Scholar]
- 22.Lefkowitz DS, Baxt C, Evans JR. Prevalence and correlates of posttraumatic stress and postpartum depression in parents of infants in the Neonatal Intensive Care Unit (NICU) J Clin Psychol Med Settings. 2010 Sep;17(3):230–237. doi: 10.1007/s10880-010-9202-7. [DOI] [PubMed] [Google Scholar]
- 23.Vanderbilt D, Bushley T, Young R, Frank DA. Acute posttraumatic stress symptoms among urban mothers with newborns in the neonatal intensive care unit: a preliminary study. J Dev Behav Pediatr. 2009 Feb;30(1):50–56. doi: 10.1097/DBP.0b013e318196b0de. [DOI] [PubMed] [Google Scholar]
- 24.Shaw RJ, Bernard RS, Deblois T, Ikuta LM, Ginzburg K, Koopman C. The relationship between acute stress disorder and posttraumatic stress disorder in the neonatal intensive care unit. Psychosomatics. 2009 Mar-Apr;50(2):131–137. doi: 10.1176/appi.psy.50.2.131. [DOI] [PubMed] [Google Scholar]
- 25.Cella D, Riley W, Stone A, et al. The Patient-Reported Outcomes Measurement Information System (PROMIS) developed and tested its first wave of adult self-reported health outcome item banks: 2005–2008. J Clin Epidemiol. 2010 Nov;63(11):1179–1194. doi: 10.1016/j.jclinepi.2010.04.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.PROMIS: Dynamic Tools to Measure Health Outcomes from the Patient Perspective. http://www.nihpromis.org/Measures/DomainFramework. Accessed October 13, 2011.
- 27.Pilkonis PA, Choi SW, Reise SP, Stover AM, Riley WT, Cella D. Item Banks for Measuring Emotional Distress From the Patient-Reported Outcomes Measurement Information System (PROMIS(R)): Depression, Anxiety, and Anger. Assessment. 2011 Sep;18(3):263–283. doi: 10.1177/1073191111411667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Miles MS, Funk SG, Carlson J. Parental Stressor Scale: neonatal intensive care unit. Nurs Res. 1993 May-Jun;42(3):148–152. [PubMed] [Google Scholar]
- 29.Buysse DJ, Yu L, Moul DE, et al. Development and validation of patient-reported outcome measures for sleep disturbance and sleep-related impairments. Sleep. 2010 Jun 1;33(6):781–792. doi: 10.1093/sleep/33.6.781. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Riley WT, Rothrock N, Bruce B, et al. Patient-reported outcomes measurement information system (PROMIS) domain names and definitions revisions: further evaluation of content validity in IRT-derived item banks. Qual Life Res. 2010 Nov;19(9):1311–1321. doi: 10.1007/s11136-010-9694-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Gershon RC, Rothrock N, Hanrahan R, Bass M, Cella D. The use of PROMIS and assessment center to deliver patient-reported outcome measures in clinical research. J Appl Meas. 2010;11(3):304–314. [PMC free article] [PubMed] [Google Scholar]
- 32.PROMIS Scoring Manuals. http://www.assessmentcenter.net/Manuals.aspx. Accessed October 14, 2011.
- 33.Gooding JS, Cooper LG, Blaine AI, Franck LS, Howse JL, Berns SD. Family support and family-centered care in the neonatal intensive care unit: origins, advances, impact. Semin Perinatol. 2011 Feb;35(1):20–28. doi: 10.1053/j.semperi.2010.10.004. [DOI] [PubMed] [Google Scholar]
- 34.Schenk LK, Kelley JH. Mothering an extremely low birth-weight infant: a phenomenological study. Adv Neonatal Care. 2010 Apr;10(2):88–97. doi: 10.1097/ANC.0b013e3181d28330. [DOI] [PubMed] [Google Scholar]
- 35.Turan T, Basbakkal Z, Ozbek S. Effect of nursing interventions on stressors of parents of premature infants in neonatal intensive care unit. J Clin Nurs. 2008 Nov;17(21):2856–2866. doi: 10.1111/j.1365-2702.2008.02307.x. [DOI] [PubMed] [Google Scholar]


