Abstract
Background
Smartphone applications can potentially provide recovery monitoring and support in real-time, real-life contexts. Study aims included determining feasibility of: a) Adolescents completing ecological momentary assessments (EMA) and utilizing phone-based ecological momentary interventions (EMI); and b) Using EMA and EMI data to predict substance use in the subsequent week.
Methods
Twenty-nine adolescents were recruited at discharge from residential treatment, regardless of their discharge status or length of stay. During the 6-week pilot, youth were prompted to complete an EMA at 6 random times per day and were provided access to a suite of recovery support EMI. Youth completed 87% of the 5,580 EMAs. Based on use in the next 7 days, EMA observations were classified into 3 risk groups: “Current Use” in the past 30 minutes (3% of observations), “Unrecognized Risk” (42%), or “Recognized Risk” (55%). All youth had observations in 2 or more risk groups and 38%, in all three. Youth accessed an EMI on-average 162 times each week.
Results
Participants were: 31% female, 48% African American, 21% Caucasian, 7% Hispanic, 24% Mixed/Other, average age 16.6 years. During the 90 days prior to entering treatment, youth reported using alcohol (38%), marijuana (41%), and other drugs (7%). When compared to the “Recognized Risk” group’s use in the following week (31%), both the “Unrecognized Risk” (50%, OR=2.08) and “Current Use” (96%, OR=50.30) groups reported significantly higher rates of use in the next week. When an EMI was accessed 2 or more times within the hour following an EMA, the rate of using during the next week was significantly lower than when EMIs were not accessed (32% vs. 43%, OR=0.62).
Conclusions
Results demonstrate the feasibility of using smartphones for recovery monitoring and support with adolescents, with potential to reduce use.
Keywords: Adolescent, Substance Use Disorders, Recovery Management, Smartphones, Mobile Phones
INTRODUCTION
The 20,175 (17% of all admissions in the U.S.) adolescents admitted to residential substance use treatment are typically among the most severe in terms of both substance use disorders and co-occurring problems. Yet 77 % complete less than the 90 days of treatment recommended by experts, and 50–70% relapse within the first 90 days after discharge from residential treatment1–6. While continuing care and recovery support services after residential discharge have been demonstrated to reduce relapse4,7–10 and are recommended by expert groups5,11,12, only 18% of the youth discharged from publicly funded treatment receive aftercare; even fewer access recovery support services6. One promising way to address this service gap is the use of smartphones to: 1) Teach adolescents how to better self-monitor risk and protective factors associated with relapse, and 2) Provide adolescents with immediate interventions that remind them of their motivation for recovery, prompting them to seek support from others, distract themselves from urges or cravings, and connect with others in pro-social ways8.
The use of smartphone technology and the Addiction Comprehensive Health Enhancement Support System (ACHESS) has been demonstrated by Gustafson and colleagues to help reduce risky drinking days among adults discharged from residential treatment,13 but has not yet been used to provide recovery support for adolescents post-treatment. Study aims included determining feasibility of: a) Adolescents completing ecological momentary assessments (EMA) and recovery support ecological momentary interventions (EMI) via smartphones; and b) Using EMA and EMI data to predict substance use in the subsequent week.
METHODS
Recruitment and Design
Adolescents were recruited from residential treatment between November of 2012 and April of 2013. Over a 6 week period, adolescents were provided a smartphone with an unlimited calling/data plan, the study’s mobile applications, and training on how to use them. They were then asked to: a) complete a 2–3 minute EMAs at 6 randomly prompted times per day, b) meet with research staff at the research office twice during each 7 day period and provide a urine sample, and c) return the phone in its original condition. Adolescents could earn up to $50 per week for completing all study requirements, which included answering at least 5 of the 6 EMAs per day, providing a urine sample and meeting with research staff twice a week in the research office. If an adolescent missed more than 2 EMA’s in a 24-hour period, research staff would contact him/her to determine if there were technical issues with the phone. Phones were preinstalled with all phone and web applications to support the EMAs and a suite of recovery support EMIs that were available 24/7. Participation was voluntary, requiring both the assent of the youth and parental consent. The study was conducted in accord with the Helsinki Declaration of 1975 and under the supervision of Chestnut Human Subject Institutional Review Board (IRB).
Eligibility
Eligibility criteria for the current pilot included: a) discharge from residential treatment (regardless of discharge status or length of stay), b) being age 18 or under at the time of recruitment, and c) assent to participate from the youth, plus consent to participate from a parent or guardian. Of the 43 adolescents meeting the first two criteria and invited to participate, 32 (74%) agreed to participate in the pilot study and showed up for training. Participation was terminated early for 3 adolescents: the first was unable to attend both trainings, the second became frustrated with the software problems that occurred and chose to withdraw early, and the third was incarcerated during the 6 week period of the pilot and was not released before the end of the 6 week period. Of those who initially agreed to participate, the remaining 29 (90%) completed all requirements for both trainings and the pilot.
Instruments and Other Data Sources
At the beginning of the pilot, participant characteristics and clinical problems were collected using the Global Appraisal of Individual Needs – Quick version 3 (GAIN-Q3)14. For adolescents (n = 10,625), the GAIN-Q3’s 53 item total disorder screener has excellent internal consistency (Cronbach’s alpha=.90), is highly correlated (r=.96), and also predictive (Area under the curve [AUC] =.99), with the 220 item total disorder scale in the full GAIN. The GAIN-Q3’s nine 4–10 item short screeners (school, work, stress, health, HIV risk behavior, internalizing mental health, externalizing mental health, substance use, and crime/violence) were selected based on a Rasch measurement model, so that while the short screeners only have fair to good internal consistency (alpha .56 to .79), they are highly correlated (r=.86 to .92) and predictive (AUC=.92 to .98) of the interpretative cut points in the respective 8 to 43 item longer versions in the full GAIN. In each case, having over 90% of the people self-reporting 0 symptoms on a given screener do not have a problem on the corresponding full GAIN measures and over 90% of the people self-reporting 3 or more symptoms on the screener have a problem on the corresponding full GAIN measure. Of those reporting 1–2 symptoms, about half have problems on the full measure and half do not.
The EMAs which adolescents were asked to perform 6 times a day incorporated several items modeled after ones used by Epstein and colleagues15 and are available from the authors. All EMA questions referenced the “past 30 minutes” and content focused on the adolescent’s current feelings, activities, and location, as well as on the persons present. Adolescents were also asked to rate the degree to which the internal and external factors they endorsed made them want to use drugs or alcohol, supported their recovery, or had no impact. Respondents were also asked about their ability during the past 30 minutes to resist using drugs and alcohol, the extent of their cravings, and exposure to drugs, alcohol, or illegal activity. Positive ratings (supporting recovery, self-efficacy) were reversed and combined with negative ratings (e.g., making you want to use alcohol or drugs, access, craving, pain, withdrawal) to make a unidimensional scale (alpha=.93) ranging from 0 to 100, with higher scores representing greater perceived risk and less perceived support. ACHESS13 recorded the date, time, location and responses to all EMAs.
The EMIs which adolescents could access at any time included: a) recovery support (discussion groups, support team, reaching out to others via text, listening to recovery stories, on-line self-help meetings, in person self-help meeting locator, linking to sponsor), b) relaxation (guided relaxation, playing games, listening to music, learn/reading, physical exercise), c) recovery motivation (motivational text messaging, recovery words, recovery profiles and pictures), and d) social networking (Facebook, contacting friends). This included all of the EMI previously provided in ACHESS13, plus additional links to existing mobile and web applications for on-line self-help, relaxation, games, music, and exercise. ACHESS recorded the date and time that the youth used it to access each of the EMIs.
The urine samples which adolescents were asked to provide twice a week were tested on-site with CLIAA waived QuikScreen cups using an immunochromatographic assay for rapid (2–5 minute) qualitative results based on SAMHSA-standard cutoffs for alcohol (20mg/dL or 0.02% BAC), amphetamine/ methamphetamine (1,000 ng/ml), cannabis (50 ng/ml), cocaine/ benzoylecgonine (300 ng/ml), and opiates/ morphine (2000 ng/ml). Of the 316 urine tests, 33% were positive (32% Cannabis, 3% Amphetamines, 1% Cocaine, 1% Opioid, and 0% Alcohol).
The primary outcomes were time to first alcohol or drug use in the next 7 days (for survival analysis) and any use in the next 7 days (for logistic regression). The date and time of first use was based on the first of the next 42 EMA where they self-report alcohol or drug use, or, the date of the first urine tested that was positive for urine alcohol or drug use. The rate of agreement between the urine tests and self- reports on the EMA were excellent for the past month (Kappa=.70) and past day (Kappa=.57) and are similar to earlier adolescent studies16,17.
Training
Two 4-hour trainings were provided, and adolescents were trained in 5 cohorts by members of the research team. The first training focused on education about recovery support, how to use the study phones, and how to complete the EMAs. Each adolescent was asked to select a 15-hour time period during the day in which they could receive the 6 randomly scheduled EMAs for the 6-week study. The EMAs had to be a minimum of 90 minutes apart or a maximum of 6 hours apart. This schedule provided participants with 9 hours for uninterrupted sleep. Participants had 30 minutes to complete an EMA before it deactivated. The second training focused on EMIs, how they could help with recovery, and procedures for accessing them.
Data Collection
During week one, adolescents completed a 2–3 minute EMA at 6 randomly selected times and participated in 2 one-hour office visits to ensure that they could operate the phone efficiently and complete the surveys. After the second training, adolescents continued to complete the EMAs and could access the EMIs at any time. EMA responses were saved in real-time via a web application, and every webpage or phone application was recorded as it was accessed. The youth also attended two office visits per week to a) check their proficiency on using the smartphone and applications, b) complete a survey and c) provide urine samples. The proficiency check required them to demonstrate the use of any application they had not used 5 or more times in the past week. The 5-minute survey asked about their experience using the phone, completing the EMAs (burden), use of each EMI, and the effectiveness of each EMI. Urine was tested on-site with CLIAA waived QuikScreen cups as described above.
Classification of EMA Observation Risk Groups
IBM’s SPSS version 22 Chi-square Automatic Interaction Detection (CHAID) was then used to identify subgroups which best predicted subsequent substance use in the next 7 days. Considering all of the items in the EMA and the summary scale, this analysis revealed three main observation risk groups:
Current Use (3% of observations): When youth self-reported alcohol or drug use in the 30 minutes prior to the EMA;
Unrecognized Risk (42% of observations): When youth reported no alcohol or drug use, reported no risk from any internal or external factors, and reported that these factors supported their recovery (i.e., summary score=0); and
Recognized Risk (55% of observations): When youth reported no alcohol or drug use, but recognized and reported that at least one of the internal or external factors was making them want to use, or less than perfect support for recovery (i.e., summary score =1 to 100).
The order of the risk groups above is ranked based on their actual rates of use in the next 7 days (discussed further in Results section). The patterns across observations is 5 (17%) adolescents with all observations in Recognized Risk Group, 13 (45%) with observations in both the Unrecognized and Recognized Risk, and 11 (38%) that had observations in all 3 observation risk groups. The later includes all of the youth reporting any use during the pilot.
EMI Utilization
The pre-installed Addiction Comprehensive Health Enhancement Support System (ACHESS) application on the smartphone connected users to the ACHESS webserver, other Internet sites, and/or other mobile applications on the phone. The server logged the person, date, time and URL each time adolescents accessed a web page. Multiple URL hits in a short period of time were considered evidence of more active usage. For the predictive analysis, we focused on EMI use during the hour after the referent EMA in order to maintain temporal precedence before the subsequent EMA was used for dependent variables (which per above had to be at least an hour later).
Analyses
All analyses were completed using IBM SPSS version 22. As noted above, identification of sub-groups based on subsequent actual use was done with a series of exploratory CHAID. Time to first-use was analyzed using Kaplan-Meier methods overall, and Wilcoxon (Gehen) from Life-Tables analysis for pairwise comparisons of sub-groups. Differences in next 7-day use by Observation Risk Groups and EMI utilization were evaluated also by using logistic regression analysis. For all analyses, data were arranged into sequences of 1 week of observations that included a referent EMA (from which all predictors came) and two dependent variables (time to first use and any first use in the next week) calculated from the ~ 42 EMA and 1–2 urine tests in the week that followed it. Thus, any given EMA was used both to predict dependent variables based on the EMA for the week that followed it, and also to help calculate the dependent variables for observations in the week before it. This produced 3,640 overlapping sets of observations for the analysis.
RESULTS
Participant Characteristics
The adolescents were 31% female, 48% African American, 21% Caucasian, 7% Hispanic, and 24% mixed races. There were 28% between 14–15 years of age, 45% were 16–17, and 28% were age 18. Most had a lifetime history of victimization (76%) and involvement with the juvenile justice system (69%). Regarding substance use during the 90 days prior to treatment intake, 41% reported using marijuana, 38% reported using alcohol (31% heavy use), and 7% reported using other drugs. This included weekly use of any substance (21%), marijuana (17%), and heavy alcohol use (3%). The most common major clinical problems were substance use disorders (90%), internalizing or externalizing mental health disorders (83%), school problems (79%), HIV risk behaviors including sexual risk, needle use and victimization (76%), crime or violence towards others (72%), psycho-social stress (69%), physical health problems (65%), and work problems (17%).
Feasibility and Acceptability of Using EMAs with Adolescents
During the first week, adolescents were trained by staff on using the EMA and EMI and were tested to determine proficiency of using the phones, accessing and completing the EMAs, and accessing the EMIs. This testing ruled out the possibility of low utilization rates attributable to lack of skill. During the pilot, adolescents completed 4,860 (89%) of the total 5,460 EMAs. Of the 29 participants, 18 completed over 90% of the EMAs, 10 completed 80–89%, and one completed 77%. In the office visit survey, the majority of adolescents felt that the EMA “was not too long” (95%), “very easy” or “easy to learn how to do” (100%), and that it was “very easy” or “easy to complete 6 EMAs per day” (94%).
Feasibility of Using EMA Data to Predict Risk of Use in the Subsequent 7 Days
Data from this pilot was used to explore ways of combining multiple factors that influence recovery and predict future use (~31% overall). Not surprisingly, substance use in the past 30 minutes (vs. not) was the single best predictor of any subsequent use in the next 7 days (96% vs. 39%; X2(1) = 120.45, p<.001). The next best predictor involved combining 20 ratings of internal and external risk and protective factors from the EMA (e.g., people, places, feelings, activities, current use, exposure to substances, pain, withdrawal, craving, ability to resist using). These ratings varied along a common latent dimension for risk of future use (alpha =.93) on a scale of 0 to 100 (no risk /highest support to highest risk /no support). Based on a series of analyses using IBM SPSS's chi-square automated detection (CHAID), the best breaking point on this scale was between those who "Recognized" some risk or limits in their support (scores of 1 to 100) vs. those with "Unrecognized" risks or limits in their support (score=0) (31% vs. 50%; X2(1) = 122.06, p<.001).
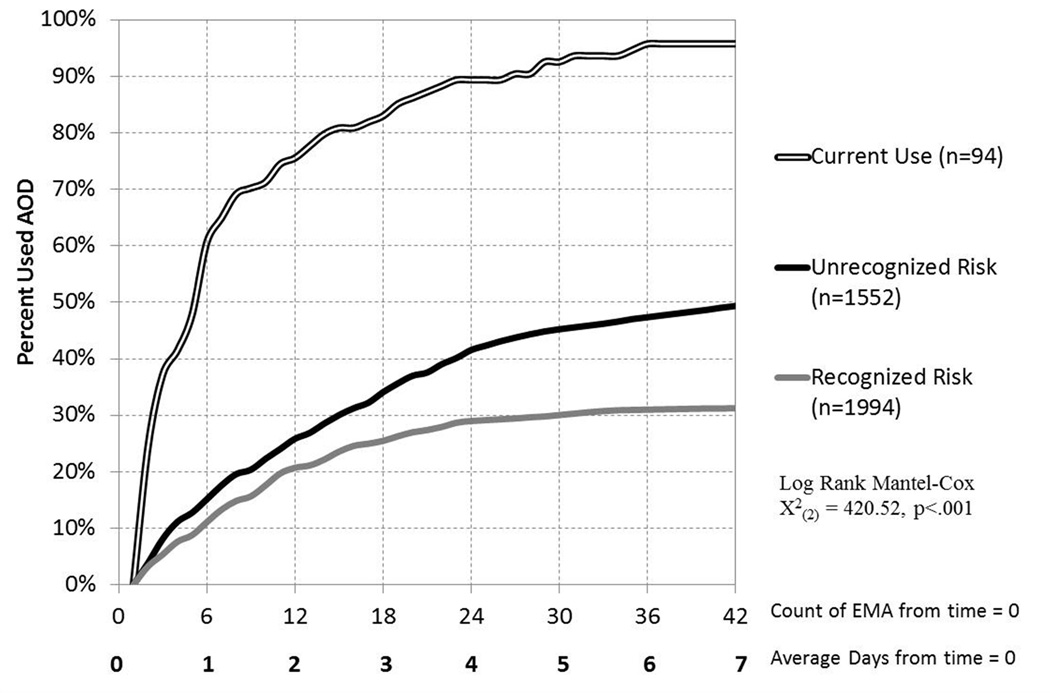
Figure 1 shows the time from the referent EMA to the first subsequent use. The x-axis shows the number of EMAs and average days between the referent EMA and the first EMA in which the participant reported alcohol or drug use during the subsequent 7 days. Separate survival curves are shown for each of the Adolescent EMA Observation Risk Groups. Using Kaplan-Meir life tables, EMA Observation Risk Groups were significantly related to the time to subsequent use (Log Rank Mantel-Cox X2(2) = 420.52, p<.001). Weighting by number of surviving observations (e.g., Breslow X2) or the squared number of surviving observations (e.g., Tarone-Ware X2) and all pairwise comparisons of survival curves (e.g., Wilcoxon-Ghen), all are statistically significant at p<.001. Substantively, when adolescents were in the “current use” EMA observation risk group, 96% of the time alcohol or drug use was reported again during the next 7 days (24% of the time at the very next EMA, 65% within approximately one day). For referent EMA where adolescents had not used in the past 30 minutes, the time to first use was longer and the rate of use in the next week was lower after EMAs with Unrecognized Risk (50%) and Recognized Risk (31%).
Figure 1.
Alcohol or Drug Use in the Next 7 Days by Adolescent EMA Observation Risk Group
Utilization, Acceptability, and Impact of EMIs
Table 1 shows the percentage of adolescents who used one or more EMIs at any time, followed by the mean number of times per day, week, and over the course of the pilot study. Excluding time in training, 100% of the adolescents accessed EMIs during the pilot. They averaged 23.5 EMIs per day (SD=12.7), which is 162 per week and 847 over the course of the pilot. Adolescents accessed EMIs on 78% of the days, with a third accessing EMIs on 95–100% of the days. The average time spent per access of EMI was just over 3 minutes, with 2.8 minutes for relaxation, 5.2 minutes on recovery motivation, and almost 10 minutes per social network access. Adolescents accessed 2 or more EMIs within one hour of an EMA an average of 27 times during the pilot and 1 or more times per day. This is important because adolescents using 2 or more EMI within an hour of the EMA were significantly less likely than those who did not to use drugs or alcohol within the 7 days, based on self-report or urine tests (32% vs. 43%; odds ratio [OR] = 0.62, 95% confidence interval of 0.52 to 0.74). While the selection of specific EMIs was NOT associated with any additional differences in subsequent use, below we have provided further detail on the contents of what was utilized and how useful youth rated each type of application.
TABLE 1.
Ecological Momentary Interventions (EMI) Utilization
| Class of EMI Specific Type of EMI |
% of Clients with 1+ |
Mean per day |
SD per day |
Mean per week |
Mean Total |
% 4/5 Usefulnessa |
|---|---|---|---|---|---|---|
| Any EMI | 100% | 23.5 | 12.7 | 162 | 847 | |
| Recovery Support | 100% | 5.7 | 5.5 | 40.1 | 206.4 | |
| Discussion Groups | 100% | 2.7 | 2.0 | 18.8 | 97 | 91% |
| Reach out to others | 86% | 1.8 | 4.3 | 12.4 | 62 | NA |
| Support Team | 100% | 1.0 | 0.7 | 6.8 | 36 | 94% |
| Listen to Recovery Stories | 90% | 0.1 | 0.2 | 1.0 | 6 | 96% |
| Meeting Locator | 79% | 0.1 | 0.1 | 0.8 | 4 | 77% |
| Linking to Sponsor | 34% | 0.0 | 0.1 | 0.3 | 2 | NA |
| Recovery Motivation | 100% | 3.1 | 1.7 | 21.9 | 115.6 | |
| Motivational Messaging | 100% | 2.2 | 1.7 | 15.1 | 81 | NA |
| My Recovery Profile | 97% | 0.2 | 0.1 | 1.1 | 6 | 95% |
| My Recovery Motivation | 83% | 0.7 | 0.4 | 5.2 | 26 | NA |
| Recovery Words | 59% | 0.1 | 0.1 | 0.5 | 2 | 100% |
| Recovery Pictures | 28% | 0.0 | 0.1 | 0.1 | 1 | 84% |
| Relaxation | 100% | 1.6 | 1.2 | 11.1 | 57.5 | |
| Guided Relaxation | 97% | 0.7 | 0.6 | 4.7 | 24 | 93% |
| Listen to Music | 83% | 0.5 | 0.7 | 3.3 | 17 | 90% |
| Play Games | 72% | 0.2 | 0.3 | 1.5 | 8 | 97% |
| Learn/Read | 69% | 0.2 | 0.1 | 1.1 | 6 | NA |
| Exercise | 62% | 0.1 | 0.1 | 0.5 | 3 | 71% |
| Social Networking | 90% | 1.6 | 2.6 | 11.1 | 55.1 | |
| Go on Facebook | 78% | 0.9 | 3.0 | 6.4 | 31.7 | 76% |
| Socialb | 83% | 0.6 | 0.8 | 4.5 | 22.7 | NA |
| Contact Your Friends | 35% | 0.0 | 0.1 | 0.1 | 0.7 | 98% |
NA - not available
Based on ratings given during weekly office visits for those EMIs they had used.
Were unable to separate Facebook from Contact Friends for first cohort.
Recovery support (average of 5.7 times per day, 40.1 times per week – see table for SD) was the most commonly used suite of EMIs. This included participation in recovery support discussion groups (3 times per day), reaching out to others (2 times per day), and contacting members of their peer-support team (1 time per day). Though less common, adolescents also listened to recovery story recordings, located self-help meetings via the meeting locator and/or linked to their sponsor. During each office visit, the adolescents were asked to rate the usefulness (1 “not at all useful” to 5 “very useful”) of the EMIs which they reported using since the previous office visit. The last column includes the usefulness ratings. All ratings were over 77%, with most over 90%. The slightly lower rating for the meeting locator is likely due to the limited and sometimes dated information available on local meetings via Google and the lack of information on the degree of adolescent involvement in many meetings.
Recovery motivation (3.1 times per day, 21.9 per week) was the second most commonly used suite of EMIs. This included daily motivational messages sent 15 times per week, reviewing their personal profile, which included photos, stories, reminders, and poems that adolescents had identified as recovery supports. All were rated as “useful” or “very useful” by 84 to 100% of those that accessed them.
Relaxation (1.6 times per day, 11.1 times per week) was the third most commonly used suite of EMIs, with guided relaxation tapes being the most frequently utilized (5 times per week). Though they were less commonly utilized, other EMIs included listening to music, playing games, learning/reading and physical exercise. All were rated as “useful” or “very useful” by 96 to 100% of the adolescents.
Social networking (11.1 times per week) was the fourth most commonly used suite of EMIs, with the most common being to access to Facebook (6 times per week) and contacting their friends. Note the standard deviation is much larger than the mean because the utilization of social networks was primarily driven by a subset of the youth. The social networking EMI, phone, text and availability of the browser were rated as “useful” or “very useful” by 76 to 98%.
Note that the rates of using relaxation tapes, music, games and social networking are likely an underestimate, as the web-based ACHESS system only recorded times the adolescent accessed other mobile applications on the phone, web-sites or social networking on the internet from within the ACHESS application. If the youth called, texted, or accessed EMIs without going through ACHESS, the system did not record it.
Interaction of EMA Risk Groups & EMI Utilization
The study addressed whether there was an interaction between EMA Observation Risk Groups and EMI utilization within the subsequent hour and how they were associated with alcohol or drug use over the next 7 days. Table 2 reports the prevalence of use in the next week by risk group (rows) and EMI utilization (columns), along with the respective odds ratios (OR) and their 95% confidence intervals. Bold ORs and confidence intervals indicate significance at p < .01. Relative to the Recognized Risk observations (where youth had not been using and recognized the risks in their environment), there were significantly higher rates of substance use in the next 7 days after observations classified as Unrecognized Risk (OR =2.08) and Current Use (OR = 50.30). Accessing EMIs 2 or more times within one hour of the current EMA significantly decreased the likelihood of using in the next week overall (OR=0.62), within Unrecognized Risk observation group (OR = 0.69) and within the Recognized Risk observation group (OR = 0.54). While it is in a similar direction and magnitude of the second group, the effect within the smaller Current Use observation group did not reach statistical significance.
TABLE 2.
Effects of EMI Utilization and Adolescent EMA Observation Risk Groups on Alcohol or Drug Use in the Next Week
| Adolescent EMA Observation Risk Group |
Effect of EMA Observation Risk Group relative to Recognized Riska |
Effect of Accessing EMI 2+ times within Risk Group |
|||||
|---|---|---|---|---|---|---|---|
| Use in the Next Week |
OR | 95% CI | Use in the next week by Utilization |
OR | 95% CI | ||
| 0–1 Time | 2+ | ||||||
| Across | 38% | -- | -- | 43% | 32% | 0.62 | (0.62, 0.74) |
| Current Use | 96% | 50.30 | (15.80, 160.17) | 96% | 93% | 0.55 | (0.05, 5.70) |
| Unrecognized Risk | 50% | 2.08 | (1.79, 2.42) | 51% | 42% | 0.69 | (0.53, 0.90) |
| Recognized Risk | 31% | -- | -- | 33% | 21% | 0.54 | (0.41, 0.71) |
OR = Odds ratio, CI = Confidence Interval,Bold indicates p < .01
Rate of use in the next week regardless of EMI use were relative to those who self-monitor and acknowledge their risk
DISCUSSION
These results demonstrate the feasibility of using smartphones with adolescents to provide recovery monitoring and support services following treatment. Youth successfully completed EMAs 6 times a day to self-monitor the risk and protective factors associated with relapse and utilized a wide range of EMIs delivered via smartphones on a regular basis. Self-reported EMA data could be used to classify observations based on the rate of use in the next 7 days and EMI utilization was associated with reduced rates of use. The fact that over 97% of the observations occurred prior to substance use – means that this approach provides real and timely opportunities for relapse prevention. Moreover, the need to provide youth assistance with self-monitoring is evident in that over half the time, adolescents did not recognize their risks or lack of support for recovery. This highlights the potential value of using EMAs via smartphones to get ahead of relapse and help youth self-monitor their risks. Though only observational, the pilot also provides promising evidence of the potential effectiveness of getting youth to use EMIs to reduce the risk of relapse. To the extent that substance use disorders are a chronic condition, it also helps to establish the value of providing youth with self-management tools.
Relative to the earlier ACHESS study with adults13, with adolescents here we achieved higher rates of the “average EMI utilization per day” (8 vs 23 times per day) or “any EMI utilization per day” (41% vs 78% of days). This coincides with an increased investment by Chestnut and ACHESS staff in training, expanded EMI content and high ratings of usefulness. It may also be due, in part, to the change in population and greater amenability to using smartphone by youth. Either way, it is important because in both earlier and this work, higher EMI utilization is associated with reduced use.
It is also important to acknowledge some key limitations of the study, including a relatively small number of youth, recruited from residential programs in one state, followed for a relatively short duration, and the lack of a randomized control group. Thus, it will be important to replicate this study with a larger number of youth, from a more diverse of set of programs, over a longer duration, and in an experimental study. A more subtle limit of the pilot was that when the youth completed the EMA, they were simply “left” at the main menu for the EMI. In future work, we may be able to further increase adolescents’ utilization of EMIs by providing them with immediate feedback at the end of the EMA on their risk of relapse and the potential for immediate EMI utilization to reduce risk.
While the use of incentives is common place in research, the use of them here likely impacts the high response rate to the EMAs. A study to look at adherence to EMA without incentives is also warranted.
Finally, while use of urine test results as part of the dependent variable provides an additional unbiased source of information, marijuana (the primary substance the adolescents used) has a long latency (7–30 days) in urine tests and may have potentially inflated the rates of subsequent use. Reanalysis without urine data lowered the total rates slightly, but did not substantively change the pattern of results.
In conclusion, this pilot provides strong support for the feasibility of conducting a larger study that provides recovery support services via EMA and EMI on a smartphone. It now needs to be replicated in a larger randomized trial.
ACKNOWLEDGEMENTS
The authors thank Dr. Dave Gustafson and his staff for adding our EMAs and additional EMIs to their existing Addiction Comprehensive Health Enhancement Support System (ACHESS) system and allowing us to use it as a platform for conducting the pilot study. We also thank Anthony Abrams for his work with the adolescents, Brittany Callahan and Belinda Willis for assistance with preparation of the manuscript; special appreciation also goes to the programs, staff, and adolescents who participated in the study and without whom this original research would not have been possible.
FUNDING
The proposed work was supported by NIDA grants no. R37 DA11323 and R01 DA021174. The opinions here are those of the authors and do not reflect the positions of the funding agency or government.
Footnotes
AUTHOR CONTRIBUTIONS
Drs. Dennis and Scott both: a) designed the study and ecological momentary assessment (EMA), and identified several of the EMIs for inclusion in this pilot; b) trained the staff and oversaw implementation of the pilot study; and c) led the analysis, interpretation and writing-up of the results. Mr. Funk cleaned the data, conducted the analysis, and contributed to the write-up of the methods and results. Mrs. Nicholson led the adolescent recruitment, training, day-to-day implementation, and helped write the manuscript.
REFERENCES
- 1.Brown SA, Vik PW, Creamer VA. Characteristics of relapse following adolescent substance abuse treatment. Addict Behav. 1989;14:291–300. doi: 10.1016/0306-4603(89)90060-9. [DOI] [PubMed] [Google Scholar]
- 2.Dennis ML, Dawud-Noursi S, Muck RD, McDermeit (Ives) M. The need for developing and evaluating adolescent treatment models. In: Stevens SJ, Morral AR, editors. Adolescent substance abuse treatment in the United States: Exemplary models from a National Evaluation Study. Binghamton, NY: Haworth Press; 2003. pp. 3–34. [Google Scholar]
- 3.Godley MD, Godley SH, Dennis ML, Funk R, Passetti L. Preliminary outcomes from the assertive continuing care experiment for adolescents discharged from residential treatment. J Subst Abuse Treat. 2002;23(1):21–32. doi: 10.1016/s0740-5472(02)00230-1. [DOI] [PubMed] [Google Scholar]
- 4.Godley MD, Godley SH, Dennis ML, Funk RR, Passetti LL, Petry NM. A randomized trial of Assertive Continuing Care and Contingency Management for adolescents with substance use disorders. J Consult Clin Psychol. 2014;82(1):40–51. doi: 10.1037/a0035264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.NIDA. Rockville, MD: National Institutes of Health; 2014. [Retrieved on 4/2/14]. Principles of adolescent substance use disorder treatment: A research-based guide. NIH Pub Number: 14-795 from http://www.drugabuse.gov/publications/principles-adolescent-substance-use-disorder-treatment-research-based-guide. [Google Scholar]
- 6.Substance Abuse and Mental Health Services Administration. Ann Arbor, MI: Inter-university Consortium for Polication and Social Research [distributor]; 2013. Nov 21, Center for Behavioral Health Statistics and Quality. Treatment Episode Data-set – Discharges (TEDS-D) 2010. ICPSR34898-v1. [Google Scholar]
- 7.Godley MD, Godley SH, Dennis ML, Funk RR, Passetti LL. The effect of Assertive Continuing Care on continuing care linkage, adherence and abstinence following residential treatment for adolescents with substance use disorders. Addiction. 2007;102(1):81–93. doi: 10.1111/j.1360-0443.2006.01648.x. [DOI] [PubMed] [Google Scholar]
- 8.Dennis ML, Scott CK, Laudet A. Beyond bricks and mortar: Recent research on substance use disorder recovery management. Curr Psychiatry Rep. 16.4. 2014:1–7. doi: 10.1007/s11920-014-0442-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.McKay J. Continuing care research: What we've learned and where we're going. J Subst Abuse Treat. 2009;36:131–145. doi: 10.1016/j.jsat.2008.10.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Winters KC, Stinchfield R, Latimer WW, Lee S. Long-term outcome of substance-dependent youth following 12-step treatment. J Subst Abuse Treat. 2007;33:61–69. doi: 10.1016/j.jsat.2006.12.003. [DOI] [PubMed] [Google Scholar]
- 11.Brannigan R, Schackman BR, Falco M, Millman RB. The quality of highly regarded adolescent substance abuse treatment programs: Results of an in-depth national survey. Arch of Pediatr and Adoles Med. 2004;158(9):904–909. doi: 10.1001/archpedi.158.9.904. [DOI] [PubMed] [Google Scholar]
- 12.Dennis ML, Scott CK. Managing addiction as a chronic condition. Addict Sci and Clin Pract. 2007;4(1):45–55. doi: 10.1151/ascp074145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Gustafson DH, McTavish FM, Chih M-Y, et al. A smartphone application to support recovery from alcoholism: A randomized clinical trial. JAMA Psychiatry. 2014;71(5):445–572. doi: 10.1001/jamapsychiatry.2013.4642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Titus JC, Feeney T, Smith DC, Rivers TL, Kelly LL, Dennis MD. Normal, IL: Chestnut Health Systems; 2012. [Retrieved on 4/2/14]. GAIN-Q3 3.1: Administration, clinical interpretation, and brief intervention. from http://gaincc.org/GAINQ3. [Google Scholar]
- 15.Epstein DH, Willner-Reid J, Vahabzadeh M, Mezghanni M, Lin J, Preston KL. Real-time electronic diary reports of cue exposure and mood in the hours before cocaine and heroin craving and use. Arch of Gen Psychiatry. 2009;66(1):88–94. doi: 10.1001/archgenpsychiatry.2008.509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Buchan BJ, Dennis ML, Tims FM, Diamond GS. Cannabis use: Consistency and validity of self report, on-site urine testing, and laboratory testing. Addiction. 2002;97(suppl. 1):s98–s108. doi: 10.1046/j.1360-0443.97.s01.1.x. [DOI] [PubMed] [Google Scholar]
- 17.Dennis ML, Godley SH, Diamond G, Tims FM, Babor T, Donaldson J, et al. The Cannabis Youth Treatment (CYT) Study: Main findings from two randomized trials. J Subst Abuse Treat. 2004;27(3):197–213. doi: 10.1016/j.jsat.2003.09.005. [DOI] [PubMed] [Google Scholar]