Abstract
Objective
To examine whether experiencing a traumatic brain injury (TBI) on a recent combat deployment was associated with postdeployment binge drinking, independent of posttraumatic stress disorder (PTSD).
Methods
Using the 2008 Department of Defense Survey of Health Related Behaviors among Active Duty Military Personnel, an anonymous survey completed by 28,546 personnel, the study sample included 6,824 personnel who had a combat deployment in the past year. Path analysis was used to examine whether PTSD accounted for the total association between TBI and binge drinking.
Main Measures
The dependent variable, binge drinking days, was an ordinal measure capturing the number of times personnel drank 5+ drinks on one occasion (4+ for women) in the past month. TBI-level captured the severity of TBI after a combat injury event exposure: TBI-AC (altered consciousness only), TBI-LOC≤20 (loss of consciousness up to 20 minutes), and TBI-LOC>20 (loss of consciousness greater than 20 minutes). APTSD positive screen relied on the standard diagnostic cutoff of 50+ on the PCL-C.
Results
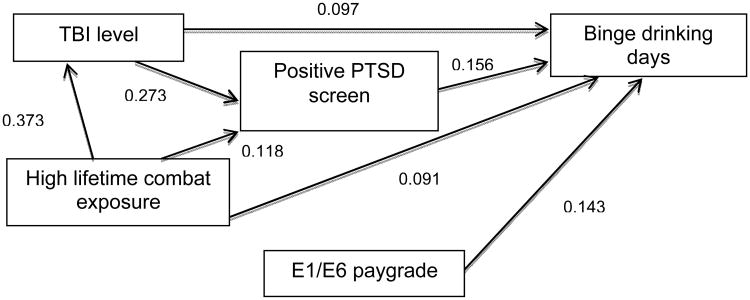
The final path model found that while the direct effect of TBI (0.097) on binge drinking was smaller than that of PTSD (0.156), both were significant. Almost 70% of the total effect of TBI on binge drinking was from the direct effect; only 30% represented the indirect effect through PTSD.
Conclusion
Further research is needed to replicate these findings and to understand the underlying mechanisms that explain the relationship between TBI and increased postdeployment drinking.
Keywords: traumatic brain injury, combat, military personnel, alcohol drinking, posttraumatic stress disorder, path analysis
1. Introduction
The association between posttraumatic stress disorder (PTSD) and unhealthy drinking among military personnel has been well studied.1-4 In contrast, research on the relationship between combat-acquired traumatic brain injury (TBI) and unhealthy alcohol use among military personnel is in early development.5 While recent studies of military personnel returning from Operation Enduring Freedom (OEF) and Operation Iraqi Freedom (OIF) suggest that TBI is independently associated with unhealthy alcohol consumption after a deployment, independent of PTSD,6,7 other studies found that the apparent association between TBI and problematic drinking is explained by PTSD.8,9
Reports of at least monthly binge drinking, and heavy drinking (at least weekly binge episodes in the past month), are associated with negative drinking-related consequences among military personnel, including job-performance problems, driving while under the influence, and being hurt in a drinking-related accident.10-13 Unhealthy alcohol consumption is associated with combat exposure and deployment.14-17 It has been posited that for some, drinking is a learned coping mechanism to self-medicate in response to the stresses of combat and to suppress the memories of traumatic events.18-23 Yet, combat alone does not explain the historic high levels of drinking among military personnel.22,24,25
While both PTSD and TBI may be risk factors for increased alcohol use among military personnel who have served in OEF/OIF, the relationship between these problems is complex. Combat-acquired TBI is often experienced during a traumatizing event, such as a blast, in which personnel may fear for their own life, witness death or injury to others, or experience injuries. The etiology that contributes to a TBI may be the same that contributes to the development of PTSD.3,26-30 Hence, it is logical that TBI and PTSD are correlated among those returning from OEF/OIF.8,31-34 Studies have found that mild TBI, defined as an alteration or loss of consciousness of up to 30 minutes after an injury event,35,36 may increase the likelihood of developing PTSD,31,37 or complicate recovery from PTSD.38 One study of 52 OEF/OIF veterans found that PTSD severity was related to underlying structural brain changes revealed through anatomical magnetic resonance imaging (MRI) and diffusion tensor imaging (DTI) scanning of the brain, rather than clinical diagnoses of mild TBI, suggesting a biological model.39 Further, the presence of PTSD among military personnel with a TBI may exacerbate or prolong the occurrence of TBI symptoms.3,40 While many with combat-acquired TBI do not experience long-term cognitive impairment,41 others do report ongoing postconcussive symptoms.42 Among those with comorbid TBI and PTSD, it may be difficult to identify the source of postconcussive symptoms since both problems have symptoms in common (i.e., insomnia, irritability).29,43-45
The purpose of this study is to use path analysis to delineate the relative contributions of TBI and PTSD to postdeployment binge drinking among active duty personnel returning from a past year combat deployment. This study builds on prior analysis with a similar study population that used multivariate logistic regression.6 We hypothesize that both TBI and PTSD are associated with binge drinking and that experiencing a TBI is independently associated with increased binge drinking days. Support for the hypothesis will be inferred if both TBI and PTSD have a significant direct effect on binge drinking days in the path model. Research that informs our understanding of risk factors for unhealthy alcohol consumption is an important public health topic with implications for the wellbeing and readiness of the Armed Forces. Better understanding of the complex relationship of TBI and PTSD in relation to unhealthy drinking is critical information for the Department of Defense (DoD) and the Veterans Administration (VA).43
2. Method
2.1 Data Source
The 2008 Department of Defense Survey of Health Related Behaviors among Active Duty Military Personnel (HRB Survey) is an anonymous, population-based assessment of the active duty component of the U.S. military.24 The survey was completed by 28,546 military personnel from all service branches between May-June of 2008, utilizing a dual-mode administration to capture the worldwide distribution of the U.S. Armed Forces. The respondent sample was weighted to reflect the composition of the active duty military. Details of the stratified multi-stage sampling design, data collection methods, and the procedure for calculating weights have been published elsewhere.46 For more detail, see the supplemental digital content.
The HRB Survey was conducted with approval by the DoD/DHA and RTI International Institutional Review Boards. This study was conducted with approval from Brandeis University's Committee for Protection of Human Subjects, and the Human Research Protection Program at the OASD/DHA at the DoD. The DHA Privacy and Civil Liberties Office executed a Data Sharing Agreement for use of the 2008 HRB Survey public-use file to ensure compliance with DoD privacy and security regulations.
2.2 Analysis Sample
To examine the hypothesis, we selected from all HRB respondents those who reported being on a combat deployment during the past 12 months, allowing us to identify those with a recent combat-acquired TBI as well as postdeployment drinking behaviors. Of all respondents, 7,169 met these criteria and 354 were excluded because they did not complete necessary information on binge drinking. The final study sample was 6,824.
2.3 Measures
The HRB survey includes items on drinking behaviors, as well as measures of demographics, deployment history, combat exposure, psychological health issues, and TBI screening questions.
2.3.1 Past Month Binge Drinking Days (Dependent Variable)
Binge drinking days was assessed on the HRB Survey by asking respondents on how many days in the past 30 days (month) they drank five or more drinks on the same occasion, or four or more for women, consistent with guidelines from the National Institute on Alcohol Abuse and Alcoholism.47 Based on the response categories, we constructed an ordinal measure to capture maximum variation for the number of past month binge drinking days: 0) non-drinkers, 1) no binge drinking, 2) once a month, 3) 2-3 days a month, 4) 1-2 days a week, 5) 3-4 days a week, 6) 5-6 days a week, and 7) daily. Respondents that either left the question blank, or were logically assigned as drinkers in the past month with level unknown, were coded as missing.
As an alternative representation of unhealthy drinking behavior, we constructed a variable using the Alcohol Use Disorders Identification Test (AUDIT) which uses 10 questions (score range of 0-40) to identify hazardous drinkers (score 8-15), harmful drinkers (score 16-19), and those at risk for possible alcohol dependence (score of 20-40).48 Because of the AUDIT's known psychometric properties,48 we examined the correlation of the AUDIT score and binge drinking days to establish the construct validity of the binge drinking days measure.
2.3.2 Traumatic Brain Injury-level
The HRB survey asked respondents, “During your last deployment, did you experience any of the following events? - blast or explosion (IED, RPG, land mine, grenade, etc.); vehicular accident/crash (any vehicle, including aircraft); fragment wound above the shoulders; bullet wound above the shoulders; fall; or other.” This was followed by a question to establish whether the definition of TBI is satisfied, and if so, at what level, “Did any injury you received while on your last deployment result in any of the following? – lost consciousness or got “knocked out” for less than a minute; lost consciousness or got “knocked out” for 1 to 20 minutes; lost consciousness or got “knocked out” for more than 20 minutes; felt dazed, confused, or “saw stars;” didn't remember the event; had a concussion of symptoms of a concussion; or had a head injury.”
Based on positive responses to these two items, excluding self-report of concussion or head injury because they require a clinical interview, we constructed a 4-level TBI variable guided by the Ohio State University TBI Identification Method:49 1) altered consciousness (AC) but no actual loss of consciousness (LOC) (TBI-AC), 2) LOC up to and including 20 minutes (TBI-LOC≤20), or 3) LOC of more than 20 minutes (TBI-LOC>20). When the level of TBI might derive from multiple reports of alterations or loss of consciousness, the resulting TBI classification was based on a hierarchy with TBI-LOC>20 having precedence over TBI-LOC≤20, which in turn had precedence over TBI-AC. The reference group (no TBI) was comprised of either those with no exposure to an injury event, or those with exposure but no self-reported AC or LOC. Self-reported TBI is based on the respondent's most recent deployment, because TBIs that occurred on prior deployments or during non-deployment periods were not queried on the HRB instrument. TBI-level was defined with self-report elicited by the HRB survey and does not represent a clinical diagnosis or observed event.
The TBI screening items on the HRB survey are based on the Brief Traumatic Brain Injury Screen (BTBIS),50 consistent with other military studies conducted at the time of the 2008 HRB survey development,32,51 and similar to those used by the DoD in its routine postdeployment health assessments.52 Because the HRB Survey TBI screening questions were modeled after the BTBIS, there was insufficient information to code TBI-level using the American Congress of Rehabilitation Medicine's definition, which defines a mild TBI as an AC or LOC of up to 30 minutes.35 Therefore, the TBI-LOC>20 group may include an unknown number of respondents who experienced a moderate or severe TBI.
2.3.3 Posttraumatic Stress Disorder (PTSD)
Current posttraumatic stress disorder was assessed using the PTSD Checklist-Civilian (PCL-C), which assesses the presence of 17 symptoms over the previous 30 days, which trace to trauma events during military or non-military experiences. The validated standard diagnostic cutoff score of 50 or greater was used to classify a positive screen for current PTSD.53,54
2.3.4 High Lifetime Combat Exposure
Lifetime combat exposure was assessed with 17 questions modified from the Deployment Risk and Resilience Inventory (DRRI)55 about different combat experiences including, but not limited to, witnessing or handling dead bodies, witnessing members of a unit being killed, firing a weapon upon the enemy, caring for injured/dying people, or being injured in combat. Respondents reported the number of times (0, 1-3, 4-12, 13-50, or 51+) they experienced each of the 17 items on all previous deployments. A summary score was calculated for the 17 items based on the following values: 4=51+, 3=13-50, 2=4-12, 1=1-3, and 0=0. We classified respondents as reporting high lifetime combat exposure based on a dichotomous variable of those with a summary score of 10+.46,56 Subsequent factor analyses of the combat exposure items confirmed that this scoring cut point correctly classified respondents as having high combat exposure.
2.3.5 Pay-grade – Enlisted/E1-E6
We constructed a dichotomous variable characterizing those who were junior enlisted personnel at the E1/E6 levels compared to all other pay-grades (senior enlisted and officers) as a covariate in this analysis. Because pay-grade was correlated with age and education level, we could not use all characteristics due to their multicollinearity. We opted to use pay-grade because it is a measure of socioeconomic status, is commonly used in military studies, and provides policy-relevant information for military leadership.
2.4 Analysis
All analyses were based on weighted data to account for the complex sampling design of the HRB Survey. Table 1 shows the distributions of average AUDIT scores within separate intervals of the dependent variable, past month binge drinking days, using a Bonferroni correction to assess for multiple comparisons. Table 2 in the digital supplemental content includes the correlation matrix for the variables included in the path analysis model.
Table 1. Average AUDIT Score (0-40) of Active Duty Military Personnel Returning from a Past Year Combat Deployment, by Binge Drinking Level, (N=6,824)a, b.
| Total Study Sample, Unweighted N | Unweighted Percentages | Weighted Percentages | Average AUDIT Score, 95% CI c (N=6,234) | |
|---|---|---|---|---|
|
| ||||
| Binge Drinking Days, past 30 days | ||||
| Non-Drinker | 1,340 | 19.6% | 18.4% | 0.4 (0.3 – 0.6) |
| Drinker, no binge days | 2,084 | 30.5% | 27.9% | 3.2 (3.1 – 3.3) |
| Once per month | 897 | 13.1% | 13.1% | 5.5 (5.0 – 6.0) |
| 2-3 days per month | 906 | 13.3% | 13.8% | 7.8 (7.4 – 8.3) |
| 1-2 days per week | 836 | 12.3% | 13.9% | 10.9 (10.5 – 11.3) |
| 3-4 days per week | 412 | 6.0% | 6.8% | 13.3 (12.7 – 14.0) |
| 5-6 days per week | 142 | 2.1% | 2.4% | 16.4 (14.8 –18.0) |
| Daily | 207 | 3.0% | 3.7% | 20.1 (19.0 – 21.2) |
Abbreviations: CI, confidence interval; AUDIT, Alcohol Use Disorders Identification Test.
AUDIT assessment reflects past year and binge drinking days reflects past 30 days.
All differences between adjacent categories of binge drinking days had significantly different average AUDIT scores at the p<.05 level.
590 sample participants did not answer all relevant questions for the AUDIT and therefore were excluded from this bivariate analysis. Sums may not add to 100% due to rounding.
Path analysis was performed to model the effects of independent variables and covariates to predict past month binge drinking days. The independent variables and covariates were selected according to theory, time precedence, and prior research.23,57 Path correlation coefficients, including direct, indirect, and total effects, were estimated in standardized form to facilitate comparisons among paths. A recursive path analysis model was estimated, implying that the paths, and presumed causes, were in one direction only without any feedback loops in the model.57 Assessment of model adequacy and choice of models from alternative specifications were based on the standardized root mean squared residual (SRMR), using the criteria that a good fit is indicated by a value under 0.08;58 the coefficient of determination (CD) or overall R2 for the model, in which a larger CD indicates a better explanatory model. Both tests represent the variance in the dependent variable explained by the set of independent variables in the model.57 Additional fit statistics that rely on a true log-likelihood were not available because we were using weighted complex survey data, which relies on a pseudo log-likelihood.
Path analysis limits itself to the structural equation and determines relationships among observables. We did not use full structural equation modeling (SEM), which poses corresponding measurement equations to account for how well observed measures (e.g., TBI, PTSD) reflect their underlying concepts. Given the size of our sample and the potential multicollinearity among concepts, path analysis was considered appropriate for a first modeling effort.
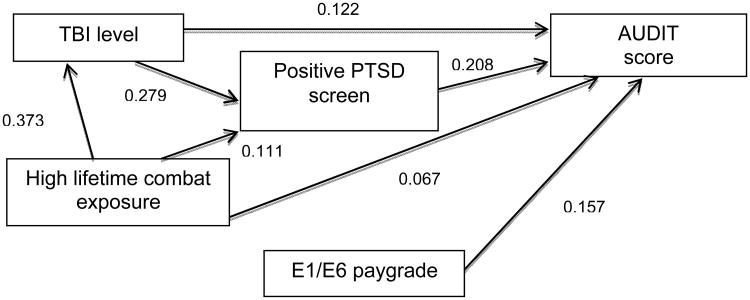
We conducted post hoc sensitivity analyses to better understand the results of the analysis, which included estimation of an additional path model with total AUDIT score as the dependent variable. To the extent that the results of these additional path models confirm our main results, they provide evidence of their robustness. All analyses were conducted in STATA 12 using its set of survey (svy) commands to account for weighted data and stratification, and maximum pseudolikelihood estimation for path analysis.59
3. Results
3.1 Sample Characteristics
The study population (N=6,824) was comprised of mostly males (88.8%), White/non-Hispanics (63.6%), those who were married/living as married (61.4%), with less education than a college degree (80.7%), and an average age of 28.5 years. In terms of military characteristics, the majority was enlisted personnel/E1-E6 (75.2%), with just over half (55.1%) having had two or more combat deployments since September 11th, 2001, and 39.9% reporting high lifetime combat exposure. The majority were in the Army (37.3%) and the Navy (27.0%). Over one-tenth (13.4%) had a positive screen for past month PTSD. Overall, 14.0% of the study population reported experiencing a TBI during the most recent deployment. The most common type of TBI was TBI-AC (7.6%), followed by TBI-LOC≤20 (4.9%), and TBI-LOC>20 (1.5%). Among those with TBI, 82.6% reported an injury event that included a blast or explosion, with the majority of those individuals (84.8%) reporting both a blast or explosion and another injury event (i.e, a fall) (data not shown).
3.2 Binge Drinking Days and Total AUDIT Score
As described in Table 1, the majority of the sample consists of current drinkers in the past 30 days (81.6%). The average AUDIT score was 6.6 (CI 6.0-7.1) and the range was 0-40 (data not shown). The majority of the study sample reported some binge drinking (53.7%); among current drinkers the percentage was 62.0%. Further, 23.4% of the study sample (29.1% of current drinkers) reported frequent binge drinking, defined as binge drinking at least weekly. Over 6% of the study sample reported binge drinking at extremely high frequency, 5-6 days per week (2.4%) or daily (3.7%).
Table 1 demonstrates the strong correlation between the constructed binge drinking days measure and total AUDIT score. For each successive category of binge drinking days, the average total AUDIT score increased. All differences between adjacent categories of binge drinking days had significantly different average AUDIT scores at the p<.05 level. Respondents who reported not drinking at all in the past month, reported a very low AUDIT score (under 1), likely reflecting drinking that occurred in the past year but prior to the past month. Current drinkers, who had no binge days, as well as those who reported binge drinking once or 2-3 days per month, had average AUDIT scores below the hazardous range. Current drinkers, who reported binge drinking at least weekly, averaged scores in the hazardous range or above, and those who reported binge drinking daily often had scores indicating possible alcohol dependence.
3.3 Bivariate Associations among Variables
With the exception of the relationship between high lifetime combat exposure and E1/E6 pay-grade, all correlations in the matrix were significant at the p≤.01 level. The two strongest associations involved the variable for TBI-level, which had a .373 correlation with high lifetime combat exposure and a .317 correlation with a positive PTSD screen (see Table 2 in the digital supplemental content). In path analysis it is common, indeed expected, that the variable of interest will have significant correlation with other variables in the model. It is through such relationships that the total effect of the variable on the outcome will come to differ from the direct effect.
3.4 Path Analysis Results
The initial path model (data not shown) included all variables, as well as paths from E1/E6 to all other measures in the model (R2=0.04, SRMR=0.00). Because the correlations between E1/E6 and the three independent measures in the model were low, as depicted in Table 2, these three paths were omitted from the final model.
Figure 1 depicts the final path model with direct effects displayed as standardized correlation coefficients. All direct, indirect, and total effects were statistically significant at the p≤.01 level (SRMR=0.04, R2=0.18). The direct effect of TBI-level on binge drinking days was 0.097 and the direct effect from PTSD on binge drinking days was 0.156. High lifetime combat exposure and enlisted E1/E6 personnel also had significant direct effects, 0.091 and 0.143 respectively. The total effect of TBI-level on binge drinking days was 0.139. Of this total effect, 69.4% was accounted for by the direct effect, with the indirect effect through PTSD accounting for the remaining 30.6%. The largest total effect from any variable was from lifetime combat exposure (0.161) with contributions of the indirect paths through PTSD and TBI, as well as the direct effect (0.067). PTSD (0.156) and E1/E6 (0.143) had total effects similar to TBI-level.
Figure 1. Final Path Model to Predict Binge Drinking Days among Active Duty Military Personnel Returning from a Past Year Combat Deploymenta, b, c.
a Path coefficients report direct effects and are displayed in standardized format.
b All direct, indirect, and total effects were statistically significant at the p≤.01 level.
c Some participants did not complete all relevant questions.
While not the main focus of this study, the path model also revealed that TBI-level had a larger direct effect on PTSD (0.273) than the direct effect from lifetime combat exposure to PTSD (0.118). Nonetheless, the total effect of lifetime combat exposure on PTSD (0.220) was close to that of TBI-level on PTSD (0.273), because of the indirect effect of combat exposure to PTSD through TBI-level (0.102).
The post hoc sensitivity analyses provide confirmatory evidence to the main results of the path analyses, as shown in Figure 2(R2=0.18, SRMR=0.3).The total effects on total AUDIT score of most independent variables were higher than on binge drinking days: TBI-level (0.180 vs. 0.139), PTSD (0.208 vs. 0.156), high lifetime combat exposure (0.158 vs. 0.161), and E1/E6 (0.157 vs. 0.143).
Figure 2. Sensitivity Analysis - Path Model to Predict Total AUDIT Score among Active Duty Military Personnel Returning from a Past Year Combat Deploymenta, b, c.
Abbreviations: AUDIT score = total AUDIT score (0-40)
a Path coefficients report direct effects and are displayed in standardized format.
b All direct, indirect, and total effects were statistically significant at the p≤.01 level.
c Some participants did not complete all relevant questions.
4. Discussion
While previous studies have examined the relationship between combat-acquired TBI and PTSD,31,38,60,61 as well as the role of risk factors, including TBI, for unhealthy alcohol use among military personnel,6,8,14,62,63 this study is significant because, to our knowledge, it is the first to test a theoretical model using path analysis techniques to assess direct and indirect associations of TBI and PTSD on postdeployment alcohol use. This study is strengthened by the use of a population-based survey of all active duty military, the anonymous nature of the survey when assessing sensitive behavioral health issues,64 and the use of a hierarchal variable that captures variation in severity of TBI-level.
The final path model confirms the study hypothesis that both TBI and PTSD have direct effects on past month binge drinking days. The direct effect of TBI (0.097) was somewhat smaller than the direct effect from PTSD to binge drinking days (0.156); yet, the direct effect of TBI on binge drinking days was almost 70% of the total effect, with the remaining 30% from an indirect effect through PTSD. High lifetime combat exposure also had a total effect on binge drinking days comparable to those of TBI and PTSD, suggesting that there may be a cumulative effect of overall combat exposure contributing to unhealthy alcohol consumption among military personnel. As enlisted personnel (E1/E6) are also younger compared to those at higher pay-grades, the finding that they constitute a risk group for increased binge drinking days is expected because of younger age. Further, because officers and senior enlisted personnel have commanding responsibilities, and may consequently face more severe repercussions for misconduct compared to junior enlisted personnel, being from a higher pay-grade may serve as a deterrent for binge drinking.
This study also revealed the relative contributions of TBI and lifetime combat exposure on a past-month positive screen for PTSD. Our final path model showed that the total effect of lifetime combat exposure on PTSD was 0.273, with a little more than half of the association accounted for by a direct effect, and the other 46.3% from the indirect paths through PTSD or TBI-level.
This study was conducted to explore previous findings based upon multivariate logistic regression models which found that personnel with TBI had increased odds of frequent binge drinking (at least weekly) compared to those without a TBI.6 This path analysis explores the possibility that the effect of TBI on binge drinking is further explained by an indirect effect through PTSD, and that TBI and PTSD are not independent of one another, as well as other covariates in a path model. Both studies rely on cross sectional data, limiting the ability to draw causal inferences, yet the path nature of the model does suggest that TBI might be an independent driver of unhealthy alcohol use. These findings are in contrast to those found by Polusny et al.,8 which showed that among National Guard Army personnel from one brigade combat team returning from Iraq, the association between TBI and problematic drinking (using AUDIT score) became insignificant after controlling for PTSD. Further studies are needed to explore this relationship.
We can only speculate as to why having experienced a TBI may increase the frequency of unhealthy binge drinking postdeployment. One theory is that having experienced a TBI while deployed is a stressful combat injury in which drinking may be used to self-medicate from any unmeasured factors associated with TBI postdeployment.23 Similarly, TBI may lead to somatic pains that lead to excessive alcohol use.65 Another theory is that damage to the frontal circuits during a TBI may disrupt executive functions, such as emotional and behavioral self-regulation, increasing the potential to drink with less inhibition.65,66 Disinhibition could affect either the desire to drink or the amount consumed in a session of drinking.
We made several choices to strengthen the study design. The selection of the study sample and the HRB items ensured that personnel were reporting on a recent combat deployment with a probable TBI that would have occurred while deployed, thus before any self-report of binge drinking days in the past month. This supports the temporal precedence of our path model, a key condition of path analysis methods.57 Even though path analysis techniques allowed us to conduct simultaneous and sequential theorized regressions, and by design the TBI reported occurred during the previous combat deployment, we still do not know whether any ongoing symptoms or problems may be a result of the TBI or PTSD.29,43-45 Thus, if personnel are self-medicating with alcohol it is difficult to determine the source of this need to self-medicate. This is a limitation in military studies and one that is inherently hard to disentangle, particularly when relying solely on self-report and cross-sectional data.67
This study was also limited by our reliance on self-report of sensitive drinking behaviors, which may lead to biased responses; however, this may have been reduced due to the anonymous nature of the HRB survey. Further, we do not know history of drinking prior to joining the military, or before the TBI, and if drinking prior to a TBI may make someone more vulnerable to unhealthy drinking post-injury. Personnel that served in OEF/OIF who return with co-occurring mild TBI and PTSD often have other comorbid conditions, including pain and sleep disturbances not measured in this study.68-70 Additionally, we do not capture those personnel who may have separated from the Armed Forces or been dishonorably discharged within the past year. All of these omitted variables could be explored in future studies.
This study relies on retrospective self-reported TBI rather than a clinical diagnosis which may introduce false positives,71 yet this is a limitation of most studies of combat-acquired TBI,31,51 and personnel were reporting on events that occurred during their most recent deployment in the past year, helping to reduce recall bias. We do not know lifetime history of TBI, how many TBIs may have occurred on the most recent deployment, or how much time had elapsed since a prior TBI and the most recent one reported, all of which may complicate recovery from the current TBI.72-75 Lifetime TBI may be of particular importance in this population, as one study of 377 personnel medically evacuated from OEF in 2010 found that 70% reported experiencing at least one concussion before their medical evacuation.76 Similarly, we do not know prior history of PTSD. Also, the HRB survey did not allow us isolate those personnel that experienced an injury on their most recent deployment, which would have been a useful comparison group to those with probable TBI.77
Because the response categories for TBI were modeled after the BTBIS, one response category on the instrument was an “LOC of 20 minutes or greater,” and therefore did not allow us to isolate moderate or severe TBIs from mild TBIs, routinely defined as up to 30 minutes.35 However, many personnel with more severe TBI and other injuries were likely medically evacuated or still in rehabilitation and therefore less likely to be eligible for the HRB survey at the time it was administered. Also modeled after the BTBIS, the wording of the TBI items on the HRB survey did not ask that the “definitional symptoms of TBI” (i.e., altered consciousness, lost consciousness) have occurred in relation to any injury event reported in the previous question (i.e., blast). This raises the possibility that there may have been some false positives in our TBI group; however, by definition any loss of consciousness would be considered a TBI, thus this would only raise concerns in the TBI-AC group.78 Further, more examination of the BTBIS's reliability and validity is needed.79
Path models are designed to estimate the indirect effect of one variable acting through another. Since the goal is to determine the full contributions of all variables in the model, path models are generally constructed to be as parsimonious as possible. As a result, important variables may inadvertently be omitted and thereby bias the estimates of effects, both direct and indirect. Since our path model included important covariates of prior analyses,6 we hope that we have not overlooked omitted variables, but there is always the possibility. Further, even though the R2 for the final path model appears low(0.18), this is likely adequate when the dependent variable is measuring person-level behaviors.
4.1 Implications and Conclusions
On September 18th, 2012, the DOD issued DoD Instruction 6490.11, replacing the Directive-Type Memorandum 09-033 created in June 2010,80 to establish policies, procedures, and responsibilities for management of mild TBI in deployed settings.81 This policy reflects a shift to incident-based screening for personnel involved in a potentially concussive event, removing the burden to seek help from personnel themselves.82 This intervention may provide an opportunity for a targeted prevention effort. It would be useful to replicate this study after the implementation of this policy because we would expect the long-term symptoms associated with TBI to decrease if more personnel who experienced a TBI while deployed are given mandatory rest immediately after the event.83
Studies have shown that PTSD is a risk factor for unhealthy alcohol consumption among military personnel and veterans.1-3 This study extends that knowledge and suggests that experiencing a combat-acquired TBI is also a risk factor for increased binge drinking among military personnel postdeployment. Thus, it is important for the DoD to continue conducting preventive screening assessments for TBI and PTSD, both in deployed settings and postdeployment, and to implement evidence-based screening and brief interventions for problem alcohol use to those with either or both conditions.22,84,85 Future studies should examine if these evidence-based methods of screening and brief intervention need to be tailored to the distinct needs of those with TBI and/or PTSD.86 Personnel, who experienced a TBI, or those with a history of alcohol use-related problems, should be identified as particularly vulnerable to high-risk drinking, and provided with ongoing clinical interventions continuing throughout the risky postdeployment months. More research is needed with longitudinal data to better understand the relative associations of TBI and PTSD with unhealthy alcohol consumption.
Supplementary Material
Acknowledgments
Disclaimers: The Office of the Assistant Secretary of Defense for Health Affairs/Defense Health Agency (OASD HA/DHA) of the United States Department of Defense (DOD) provided access to these data. The opinions or assertions herein are those of the authors and do not necessarily reflect the view of the United States Department of Defense or of the National Institutes of Health. This research has been conducted in compliance with all applicable federal regulations governing the protection of human subjects. Dr. Thomas V. Williams is the DHA/DOD Government Project Manager. NIAAA had no role in the study design, collection, analysis or interpretation of the data, writing the manuscript, or the decision to submit the paper for publication.
Funding Sources: Funding for this study was provided by NIAAA Grant F31AA021030 and NIAAA institutional training grant T32AA007567.
Footnotes
Conflict of Interest: There are no conflicts of interest.
Contributor Information
Rachel Sayko Adams, The Heller School for Social Policy & Management, Institute for Behavioral Health, Brandeis University, Waltham, MA.
Mary Jo Larson, The Heller School for Social Policy & Management, Institute for Behavioral Health, Brandeis University, Waltham, MA.
John D. Corrigan, Department of Physical Medicine & Rehabilitation, The Ohio State University, Columbus, OH, USA.
Grant A. Ritter, The Heller School for Social Policy & Management, Schneider Institutes for Health Policy, Brandeis University, Waltham, MA.
Constance M. Horgan, The Heller School for Social Policy & Management, Institute for Behavioral Health, Brandeis University, Waltham, MA.
Robert M. Bray, RTI International, Research Triangle Park, NC, USA.
Thomas V. Williams, Defense Health Cost Assessment and Program Evaluation, Defense Health Agency, Department of Defense, Falls Church, VA, USA.
References
- 1.Ramchand R, Miles J, Schell T, Jaycox L, Marshall GN, Tanielian T. Prevalence and Correlates of Drinking Behaviors Among Previously Deployed Military and Matched Civilian Populations. Military Psychology. 2011;23(1):6–21. doi: 10.1080/08995605.2011.534407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Barry AE, Whiteman SD, MacDermid Wadsworth SM. Implications of Posttraumatic Stress Among Military-Affiliated and Civilian Students. Journal of American College Health. 2012;60(8):562–573. doi: 10.1080/07448481.2012.721427. 2012/11/01. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Institute of Medicine. Treatment for Posttraumatic Stress Disorder in Military and Veteran Populations: Initial Assessment. Washington, D.C.: The National Academies Press; 2012. [PubMed] [Google Scholar]
- 4.Jakupcak M, Tull M, McDermott M, Kaysen D, Hunt S, Simpson T. PTSD symptom clusters in relationship to alcohol misuse among Iraq and Afghanistan war veterans seeking post-deployment VA health care. Addictive Behaviors. 2010;35(9):840–843. doi: 10.1016/j.addbeh.2010.03.023. [DOI] [PubMed] [Google Scholar]
- 5.Adams RS, Corrigan JD, Larson MJ. Alcohol Use after Combat-Acquired Traumatic Brain Injury: What We Know and Don't Know. Journal of Social Work Practice in the Addictions. 2012;12(1):28–51. doi: 10.1080/1533256X.2012.647580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Adams RS, Larson MJ, Corrigan JD, Horgan CM, Williams TV. Frequent Binge Drinking After Combat-Acquired Traumatic Brain Injury Among Active Duty Military Personnel With a Past Year Combat Deployment. Journal of Head Trauma Rehabilitation. 2012;27(5):349–360. doi: 10.1097/HTR.0b013e318268db94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Rona RJ, Jones M, Fear NT, et al. Mild Traumatic Brain Injury in UK Military Personnel Returning From Afghanistan and Iraq: Cohort and Cross-sectional Analyses. The Journal of Head Trauma Rehabilitation. 2012;27(1):33–44. doi: 10.1097/HTR.0b013e318212f814. [DOI] [PubMed] [Google Scholar]
- 8.Polusny MA, Kehle SM, Nelson NW, Erbes CR, Arbisi PA, Thuras P. Longitudinal Effects of Mild Traumatic Brain Injury and Posttraumatic Stress Disorder Comorbidity on Postdeployment Outcomes in National Guard Soldiers Deployed to Iraq. Archives of General Psychiatry. 2011;68(1):79–89. doi: 10.1001/archgenpsychiatry.2010.172. [DOI] [PubMed] [Google Scholar]
- 9.Kelley AM, Athy JR, Cho TH, Erickson B, King M, Cruz P. Risk propensity and health risk behaviors in U.S. army soldiers with and without psychological disturbances across the deployment cycle. Journal of psychiatric research. 2012;46(5):582–589. doi: 10.1016/j.jpsychires.2012.01.017. [DOI] [PubMed] [Google Scholar]
- 10.Adams RS, Larson MJ, Corrigan JD, Ritter GA, Williams TV. Traumatic Brain Injury among US Active Duty Military Personnel and Negative Drinking-Related Consequences. Substance Use & Misuse. 2013;48:821–836. doi: 10.3109/10826084.2013.797995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Mattiko MJ, Olmsted KLR, Brown JM, Bray RM. Alcohol use and negative consequences among active duty military personnel. Addictive Behaviors. 2011;36(6):608–614. doi: 10.1016/j.addbeh.2011.01.023. [DOI] [PubMed] [Google Scholar]
- 12.Santiago PN, Wilk JE, Milliken CS, Castro CA, Engel CC, Hoge CW. Screening for Alcohol Misuse and Alcohol-Related Behaviors Among Combat Veterans. Psychiatric Services. 2010 Jun 1;61(6):575–581. doi: 10.1176/ps.2010.61.6.575. 2010. [DOI] [PubMed] [Google Scholar]
- 13.Stahre MA, Brewer RD, Fonseca VP, Naimi TS. Binge Drinking Among U.S. Active-Duty Military Personnel. American Journal of Preventive Medicine. 2009;36(3):208–217. doi: 10.1016/j.amepre.2008.10.017. [DOI] [PubMed] [Google Scholar]
- 14.Spera C, Thomas RK, Barlas F, Szoc R, Cambridge MH. Relationship of Military Deployment Recency, Frequency, Duration, and Combat Exposure to Alcohol Use in the Air Force. Journal of Studies on Alcohol and Drugs. 2010;72(1):5–14. doi: 10.15288/jsad.2011.72.5. [DOI] [PubMed] [Google Scholar]
- 15.Larson MJ, Wooten NR, Adams RS, Merrick EL. Military Combat Deployments and Substance Use: Review and Future Directions. Journal of Social Work Practice in the Addictions. 2012;12(1):6–27. doi: 10.1080/1533256X.2012.647586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Bogner J, Corrigan JD. Reliability and Predictive Validity of the Ohio State University TBI Identification Method With Prisoners. The Journal of Head Trauma Rehabilitation. 2009;24(4):279–291. doi: 10.1097/HTR.0b013e3181a66356. [DOI] [PubMed] [Google Scholar]
- 17.Jacobson IG, Ryan MAK, Hooper TI, et al. Alcohol Use and Alcohol-Related Problems Before and After Military Combat Deployment. Journal of the American Medical Association. 2008 Aug 13;300(6):663–675. doi: 10.1001/jama.300.6.663. 2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Lande RG, Marin BA, Chang AS, Lande GR. Survey of Alcohol Use in the U.S. Army. J Addict Dis. 2008;27(3):115–121. doi: 10.1080/10550880802122711. [DOI] [PubMed] [Google Scholar]
- 19.Ames G, Cunradi C. Alcohol Use and Preventing Alcohol-Related Problems Among Young Adults in the Military. Alcohol Research & Health. 2004;28(4):252–257. [Google Scholar]
- 20.Board DH, editor. Department of Defense Task Force on Mental Health. An Achievable Vision: Report of the Department of Defense Task Force on Mental Health. Falls Church, VA: 2007. [Google Scholar]
- 21.Dolan CA, Ender MG. The Coping Paradox: Work, Stress, and Coping in the U.S. Army. Military Psychology. 2008;20(3):151–169. [Google Scholar]
- 22.Institute of Medicine. Substance Use Disorders in the U S Armed Forces. Washington D.C.: The National Academies Press; 2012. [Google Scholar]
- 23.Colder C. Life Stress, Physiological and Subjective Indexes of Negative Emotionality, and Coping Reasons for Drinking: Is There Evidence for a Self-Medication Model of Alcohol Use? Psychology of Addictive Behaviors. 2001;15(3):237–245. [PubMed] [Google Scholar]
- 24.Bray R, Pemberton M, Lane M, Hourani L, Mattiko M, Babeu L. Substance use and mental health trends among U.S. military active duty personnel: key findings from the 2008 DoD Health Behavior Survey. Military Medicine. 2010;175(6):390–399. doi: 10.7205/milmed-d-09-00132. [DOI] [PubMed] [Google Scholar]
- 25.Hatch SL, Harvey SB, Dandeker C et al. Life in and after the Armed Forces: social networks and mental health in the UK military. Sociology of health & illness. 2013 doi: 10.1111/1467-9566.12022. [DOI] [PubMed] [Google Scholar]
- 26.Vasterling JJ, Bryant RA, Keane TM. Understanding the Interface of Traumatic Stress and Mild Traumatic Brain Injury: Background and Conceptual Framework. In: Vasterling JJ, Bryant RA, Keane TM, editors. PTSD and Mild Traumatic Brain Injury. New York, NY: The Guilford Press; 2012. pp. 3–14. [Google Scholar]
- 27.Pietrzak R, Whealin J, Stotzer R, Goldstein M, Southwick S. An Examination of the Relation between Combat Experiences and Combat-Related Posttraumatic Stress Disorder in a Sample of Connecticut OEF-OIF Veterans. Journal of Psychiatric Research. 2011;45(12):1579–1584. doi: 10.1016/j.jpsychires.2011.07.010. [DOI] [PubMed] [Google Scholar]
- 28.Smith TC, Ryan MAK, Wingard DL, et al. New onset and persistent symptoms of post-traumatic stress disorder self reported after deployment and combat exposures: prospective population based US military cohort study. BMJ. 2008 Feb 16;336(7640):366–371. doi: 10.1136/bmj.39430.638241.AE. 2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Bryant RA. Disentangling Mild Traumatic Brain Injury and Stress Reactions. New England Journal of Medicine. 2008;358(5):525–527. doi: 10.1056/NEJMe078235. [DOI] [PubMed] [Google Scholar]
- 30.Williams JL, McDevitt-Murphy ME, Murphy JG, Crouse EM. Deployment Risk Factors and Postdeployment Health Profiles Associated With Traumatic Brain Injury in Heavy Drinking Veterans. Military Medicine. 2012;177(7):789–796. doi: 10.7205/milmed-d-12-00019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Hoge CW, McGurk D, Thomas JL, Cox AL, Engel CC, Castro CA. Mild Traumatic Brain Injury in US Soldiers Returning from Iraq. New England Journal of Medicine. 2008 Jan;358(5):453–463. doi: 10.1056/NEJMoa072972. [DOI] [PubMed] [Google Scholar]
- 32.Schneiderman AI, Braver ER, Kang HK. Understanding Sequelae of Injury Mechanisms and Mild Traumatic Brain Injury Incurred during the Conflicts in Iraq and Afghanistan: Persistent Postconcussive Symptoms and Posttraumatic Stress Disorder. American Journal of Epidemiology. 2008 Jun 15;167(12):1446–1452. doi: 10.1093/aje/kwn068. 2008. [DOI] [PubMed] [Google Scholar]
- 33.Hill J, Mobo BHP, Cullen M. Separating Deployment-Related Traumatic Brain Injury and Posttraumatic Stress Disorder in Veterans: Preliminary Findings from the Veterans Affairs Traumatic Brain Injury Screening Program. American Journal of Physical Medicine & Rehabilitation. 2009;88(8):605–614. doi: 10.1097/PHM.0b013e3181ae0f83. [DOI] [PubMed] [Google Scholar]
- 34.Kennedy J, Jaffee M, Leskin G, Stokes J, Leal F, Fitzpatrick P. Posttraumatic Stress Disorder and Posttraumatic Stress Disorder-like Symptoms and Mild Traumatic Brain Injury. Journal of Rehabilitation Research and Development. 2007;44(7):895–920. doi: 10.1682/jrrd.2006.12.0166. [DOI] [PubMed] [Google Scholar]
- 35.Kay T, Harrington DE, Adams R, et al. Definition of Mild Traumatic Brain Injury. Journal of Head Trauma Rehabilitation. 1993;8(3):86–87. [Google Scholar]
- 36.Centers for Disease Control and Prevention National Center for Injury Prevention and Control. Report to Congress on Mild Traumatic Brain Injury in the United States: Steps to Prevent a Serious Public Health Problem. Atlanta, GA: Centers for Disease Control and Prevention; 2003. [Google Scholar]
- 37.Bryant R, O'Donnell M, Creamer M, McFarlane A, Clark CR, Silove D. The psychiatric sequelae of traumatic injury. The American Journal of Psychiatry. 2010;167(3):312–320. doi: 10.1176/appi.ajp.2009.09050617. [DOI] [PubMed] [Google Scholar]
- 38.Vanderploeg RD, Belanger HG, Curtiss G. Mild Traumatic Brain Injury and Posttraumatic Stress Disorder and Their Associations With Health Symptoms. Archives of Physical Medicine and Rehabilitation. 2009;90(7):1084–1093. doi: 10.1016/j.apmr.2009.01.023. [DOI] [PubMed] [Google Scholar]
- 39.Bazarian JJ, Donnelly K, Peterson DR, Warner GC, Zhu T, Zhong J. The Relation Between Posttraumatic Stress Disorder and Mild Traumatic Brain Injury Acquired During Operations Enduring Freedom and Iraqi Freedom. The journal of head trauma rehabilitation. 2013;28(1):1–12. doi: 10.1097/HTR.0b013e318256d3d3. [DOI] [PubMed] [Google Scholar]
- 40.Brenner LA, Ivins BJ, Schwab K, et al. Traumatic Brain Injury, Posttraumatic Stress Disorder, and Postconcussive Symptom Reporting Among Troops Returning From Iraq. The Journal of Head Trauma Rehabilitation. 2010;25(5):307–312. doi: 10.1097/HTR.0b013e3181cada03. [DOI] [PubMed] [Google Scholar]
- 41.Ivins BJ, Kane R, Schwab KA. Performance on the Automated Neuropsychological Assessment Metrics in a Nonclinical Sample of Soldiers Screened for Mild TBI After Returning From Iraq and Afghanistan: A Descriptive Analysis. Journal of Head Trauma Rehabilitation. 2009 Jan-Feb;24(1):24–31. doi: 10.1097/HTR.0b013e3181957042. [DOI] [PubMed] [Google Scholar]
- 42.Carlson K, Nelson D, Orazem R, Nugent S, Cifu D, Sayer N. Psychiatric Diagnoses Among Iraq and Afghanistan War Veterans Screened for Deployment-Related Traumatic Brain Injury. Journal of Traumatic Stress. 2010;23(1):17–24. doi: 10.1002/jts.20483. [DOI] [PubMed] [Google Scholar]
- 43.Brady K, Tuerk P, Back S, Saladin M, Waldrop A, Myrick H. Combat Posttraumatic Stress Disorder, Substance Use Disorders, and Traumatic Brain Injury. Journal of Addiction Medicine. 2009;3(4):179–188. doi: 10.1097/ADM.0b013e3181aa244f. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Stein MB, McAllister TW. Exploring the Convergence of Posttraumatic Stress Disorder and Mild Traumatic Brain Injury. American Journal of Psychiatry. 2009 Jul 1;166(7):768–776. doi: 10.1176/appi.ajp.2009.08101604. 2009. [DOI] [PubMed] [Google Scholar]
- 45.Hoge CW, Goldberg HM, Castro CA. Care of War Veterans with Mild Traumatic Brain Injury--Flawed Perspectives. The New England Journal of Medicine. 2009;360(16):1588–1591. doi: 10.1056/NEJMp0810606. [DOI] [PubMed] [Google Scholar]
- 46.Bray RM, Pemberton MR, Hourani LL, et al. 2008 Department of Defense Survey of Health Related Behaviors Among Active Duty Military Personnel RTI International. 2009 [Google Scholar]
- 47.National Institute on Alcohol Abuse and Alcoholism [NIAAA] Helping Patients Who Drink Too Much: A Clinician's Guide. NIH Publication No 07-3769. 2005 [Google Scholar]
- 48.Babor TF, Higgins-Biddle JC, Saunders JB, Monteiro MG. The Alcohol Use Disorders Identification Test: Guidelines for Use in Primary Care. Geneva, Switzerland: 2001. [Google Scholar]
- 49.Corrigan JD, Bogner J. Initial Reliability and Validity of the Ohio State University TBI Identification Method. The Journal of Head Trauma Rehabilitation. 2007;22(6):318–329. doi: 10.1097/01.HTR.0000300227.67748.77. [DOI] [PubMed] [Google Scholar]
- 50.Schwab KA, Ivins B, Cramer G, et al. Screening for Traumatic Brain Injury in Troops Returning From Deployment in Afghanistan and Iraq: Initial Investigation of the Usefulness of a Short Screening Tool for Traumatic Brain Injury. The Journal of Head Trauma Rehabilitation. 2007;22(6):377–389. doi: 10.1097/01.HTR.0000300233.98242.87. [DOI] [PubMed] [Google Scholar]
- 51.Tanielian T, Jaycox L, editors. Invisible Wounds of War: Psychological and Cognitive Injuries, Their Consequences, and Services to Assist Recovery. Santa Monica, CA: RAND Corporation; 2008. [Google Scholar]
- 52.DOD Deployment Health Clinical Center. [Accessed October 1, 2010];Enhanced Post-Deployment Health Assessment (PDHA) Process (DD Form 2796) 2010 http://www.pdhealth.mil/dcs/DD_form_2796.asp.
- 53.Weathers FW, Litz BT, Herman DS, Huska JA, Keane TM. Annual Meeting of International Society for Traumatic Stress Studies. San Antonio, TX: 1993. The PTSD Checklist (PCL): Reliability, Validity, and Diagnostic Utility. [Google Scholar]
- 54.Bliese PD, Wright KM, Adler AB, Cabrera O, Castro CA, Hoge CW. Validating the Primary Care Posttraumatic Stress Disorder Screen and the Posttraumatic Stress Disorder Checklist with Soldiers Returning from Combat. J Consult Clin Psychol. 2008 Apr;76(2):272–281. doi: 10.1037/0022-006X.76.2.272. [DOI] [PubMed] [Google Scholar]
- 55.King L, King D, Vogt D, Knight J, Samper R. Deployment Risk and Resilience Inventory: A collection of measures for studying deployment related experiences of military personnel and veterans. Military Psychology. 2006;18:89–120. [Google Scholar]
- 56.Brown JM, Bray RM, Calvin SL, et al. 2006 Unit Level Influences on Alcohol and Tobacco Use. 2007 Project Number 0209842. [Google Scholar]
- 57.Keith TZ. Multiple Regression and Beyond. Boston: Pearson Education, Inc.; 2006. [Google Scholar]
- 58.Hu L, Bentler PM. Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Structural Equation Modeling: A Multidisciplinary Journal. 1999 Jan 01;6(1):1–55. 1999. [Google Scholar]
- 59.Stata Corp Stata Statistical Software: Release 12[computer program] College Station, TX: StataCorp LP; 2011. [Google Scholar]
- 60.Morissette SB, Woodward M, Kimbrel NA, et al. Deployment-related TBI, Persistent Postconcussive Symptoms, PTSD, and Depression in OEF/OIF Veterans. Rehabilitation Psychology. 2011;56(4):340–350. doi: 10.1037/a0025462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.MacGregor A, Dougherty A, Tang J, Galarneau M. Postconcussive symptom reporting among US combat veterans with mild traumatic brain injury from Operation Iraqi Freedom. The journal of head trauma rehabilitation. 2013;28(1):59–67. doi: 10.1097/HTR.0b013e3182596382. [DOI] [PubMed] [Google Scholar]
- 62.Foran HM, Heyman RE, Slep AMS, Usaf Hazardous Drinking and Military Community Functioning: Identifying Mediating Risk Factors. J Consult Clin Psychol. 2011 Aug;79(4):521–532. doi: 10.1037/a0024110. [DOI] [PubMed] [Google Scholar]
- 63.Wilk J, Bliese P, Kim P, Thomas J, McGurk D, Hoge C. Relationship of Combat Experiences to Alcohol Misuse among US Soldiers Returning from the Iraq War. Drug and Alcohol Dependence. 2010;108(1-2):115–121. doi: 10.1016/j.drugalcdep.2009.12.003. [DOI] [PubMed] [Google Scholar]
- 64.Warner CH, Appenzeller GN, Grieger T, et al. Importance of Anonymity to Encourage Honest Reporting in Mental Health Screening after Combat Deployment. Archives of General Psychiatry. 2011;68(10):1065–1071. doi: 10.1001/archgenpsychiatry.2011.112. [DOI] [PubMed] [Google Scholar]
- 65.Halbauer JD, Ashford JW, Zeitzer JM, Adamson MM, Lew H, Yesavage J. Neuropsychiatric Diagnosis and Management of Chronic Sequelae of War-Related Mild to Moderate Traumatic Brain Injury. Journal of Rehabilitation Research and Development. 2009;46(6):757–796. doi: 10.1682/jrrd.2008.08.0119. [DOI] [PubMed] [Google Scholar]
- 66.Corrigan JD, Cole TB. Substance Use Disorders and Clinical Management of Traumatic Brain Injury and Posttraumatic Stress Disorder. Journal of the American Medical Association. 2008 Aug 13;300(6):720–721. doi: 10.1001/jama.300.6.720. 2008. [DOI] [PubMed] [Google Scholar]
- 67.Carlson KF, Kehle SM, Meis LA, et al. Prevalence, Assessment, and Treatment of Mild Traumatic Brain Injury and Posttraumatic Stress Disorder: A Systematic Review of the Evidence. The journal of head trauma rehabilitation. 2011;26(2):103–115. doi: 10.1097/HTR.0b013e3181e50ef1. [DOI] [PubMed] [Google Scholar]
- 68.Lew HL, Vanderploeg RD, Moore DF, et al. Overlap of Mild TBI and Mental Health Conditions in Returning OIF/OEF Service Members and Veterans. Journal of Rehabilitation Research & Development. 2008;45(3):347–347. [PubMed] [Google Scholar]
- 69.Sayer NA, Rettmann NA, Carlson KF, et al. Veterans with History of Mild Traumatic Brain Injury and Posttraumatic Stress Disorder: Challenges from Provider Perspective. Journal of Rehabilitation Research & Development. 2009;46(6):703–715. doi: 10.1682/jrrd.2009.01.0008. [DOI] [PubMed] [Google Scholar]
- 70.Lang KP, Veazey-Morris K, Andrasik F. Exploring the role of insomnia in the relation between PTSD and pain in veterans with polytrauma injuries. Journal of Head Trauma Rehabilitation. 2013 doi: 10.1097/HTR.0b013e31829c85d0. Publish ahead of print. [DOI] [PubMed] [Google Scholar]
- 71.Iverson GL. Clinical and Methodological Challenges With Assessing Mild Traumatic Brain Injury in the Military. The journal of head trauma rehabilitation. 2010;25(5):313–319. doi: 10.1097/HTR.0b013e3181d6f9bd. [DOI] [PubMed] [Google Scholar]
- 72.Corrigan JD, Bogner J, Holloman C. Lifetime history of traumatic brain injury among persons with substance use disorders. Brain Injury. 2012;26(2):139–150. doi: 10.3109/02699052.2011.648705. [DOI] [PubMed] [Google Scholar]
- 73.McKinlay A, Grace R, Horwood J, Fergusson D, MacFarlane M. Adolescent Psychiatric Symptoms Following Preschool Childhood Mild Traumatic Brain Injury: Evidence from a Birth Cohort. The Journal of Head Trauma Rehabilitation. 2009;24(3):221. doi: 10.1097/HTR.0b013e3181a40590. [DOI] [PubMed] [Google Scholar]
- 74.McCrory P, Meeuwisse W, Johnston K, et al. Consensus statement on concussion in sport: the 3rd International Conference on Concussion in Sport held in Zurich, November 2008. Journal of Athletic Training. 2009;44(4):434–448. doi: 10.4085/1062-6050-44.4.434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Miller K, Ivins B, Schwab K. Self-reported mild TBI and postconcussive symptoms in a peacetime active duty military population: effect of multiple TBI history versus single mild TBI. The journal of head trauma rehabilitation. 2013;28(1):31–38. doi: 10.1097/HTR.0b013e318255ceae. [DOI] [PubMed] [Google Scholar]
- 76.Kennedy CH, Porter Evans J, Chee S, Moore JL, Barth JT, Stuessi KA. Return to Combat Duty after Concussive Blast Injury. Archives of Clinical Neuropsychology. 2012 Dec 1;27(8):817–827. doi: 10.1093/arclin/acs092. 2012. [DOI] [PubMed] [Google Scholar]
- 77.Miller S, Baktash S, Webb T, et al. Risk for addiction-related disorders following mild traumatic brain injury in a large cohort of active-duty U.S. airmen. The American Journal of Psychiatry. 2013;170(4):383–390. doi: 10.1176/appi.ajp.2012.12010126. [DOI] [PubMed] [Google Scholar]
- 78.Centers for Disease Control and Prevention. DoD/VA Code Proposal Final - 508 Compliant: DoD/VA Common Definition of TBI. Atlanta, GA: 2008. [Google Scholar]
- 79.Donnelly KT, Donnelly JP, Dunnam M, et al. Reliability, sensitivity, and specificity of the VA traumatic brain injury screening tool. The Journal of Head Trauma Rehabilitation. 2011;26(6):439–453. doi: 10.1097/HTR.0b013e3182005de3. [DOI] [PubMed] [Google Scholar]
- 80.Deployment Health Clinical Center. Traumatic Brain Injury. 2011 http://www.pdhealth.mil/TBI.asp.
- 81.Department of Defense. DoD Policy Guidance for Management of Mild Traumatic Brain Injury/Concussion in the Deployed Setting. 2012 [Google Scholar]
- 82.Helmick K, Baugh L, Lattimore T, Goldman S. Traumatic Brain Injury: Next Steps, Research Needed, and Priority Focus Areas. Military Medicine. 2012;177(8):86–92. doi: 10.7205/milmed-d-12-00174. [DOI] [PubMed] [Google Scholar]
- 83.Silverberg ND, Iverson GL. Is Rest After Concussion “The Best Medicine?”: Recommendations for Activity Resumption Following Concussion in Athletes, Civilians, and Military Service Members. The journal of head trauma rehabilitation. 2013;28(4):250–259. doi: 10.1097/HTR.0b013e31825ad658. [DOI] [PubMed] [Google Scholar]
- 84.Bliese PD, Wright KM, Hoge CW. Preventive Mental Health Screening in the Military. In: Adler AB, Bliese PD, Castro CA, editors. Deployment Psychology: Evidence-Based Strategies to Promote Mental Health in the Military. Washington D.C.: American Psychological Association; 2011. pp. 175–194. [Google Scholar]
- 85.Corrigan JD, Adams RS, Larson MJ. When Addiction Co-Occurs with Traumatic Brain Injury. American Journal of Psychiatry. 2013;170(4):351–354. doi: 10.1176/appi.ajp.2012.12121602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Zatzick D, Donovan DM, Jurkovich G, et al. Disseminating Alcohol Screening and Brief Intervention at Trauma Centers: A Policy Relevant Cluster Randomized Effectiveness Trial. Addiction. 2014 doi: 10.1111/add.12492. Epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.