Abstract
Obstetric fistula is a debilitating childbirth injury that has been associated with high rates of psychological distress. Global efforts have helped to link women to surgical repair, but thus far no evidence-based interventions exist to address the psychological needs of these women during the hospital stay. In this paper, we describe the development of a psychological intervention for women in Tanzania who are receiving surgical care for an obstetric fistula. The intervention was developed based on theories of cognitive behavioral therapy and coping models. Content and delivery were informed by qualitative data collection with a range of stakeholders including women with fistula, and input from a study advisory board. The resulting intervention was six individual sessions, delivered by a trained community health nurse. The session topics were: 1) recounting the fistula story; 2) creating a new story about the fistula; 3) loss, grief and shame; 4) specific strategies for coping; 5) social relationships; and 6) planning for the future. A trial run of the intervention revealed that the intervention could be delivered with fidelity and was acceptable to patients. A future randomized control trial will evaluate the efficacy of this intervention to address the mental health symptoms of this population.
Keywords: Tanzania, obstetric fistula, mental health, cognitive behavioral therapy, maternal health
1. Introduction
A vaginal fistula is a hole between the vagina and either the bladder or rectum, which causes uncontrollable leaking of urine and/or feces and a persistent bad odor. The majority of women who develop a vaginal fistula do so after obstructed labor that is not relived by a Cesarean section, but there is also growing concern that operative injuries from poorly performed Cesarean sections account for a growing proportion of fistulae (Onsrud, Sjoveian, & Mukwege, 2011; Raassen, Ngongo, & Mahendeka, 2014). A vaginal fistula is also possible from non-obstetric causes, including operative injuries during a hysterectomy or through an act of violent sexual trauma. It is estimated that approximately 2 million women worldwide are living with an obstetric fistula, with up to 100,000 new cases per year, primarily in very low resource and rural settings (Stanton, Holtz, & Ahmed, 2007). For these women, the impact on their lives can be devastating. Fortunately, surgical care is increasingly available for fistula repair. However, there is critical need to also address the psychological morbidity of this patient population. Studies have shown that women with obstetric fistula have high rates of depression (Balogun, 1994; Weston, et al., 2011) and other mental health impairments (Browning, Fentahun, & Goh, 2007; Goh, Sloane, Krause, Browning, & Akhter, 2005), and low quality of life (Pope, Bangser, & Harris Requejo, 2011). Integrating mental health treatment with surgical repair could improve the overall well-being and functioning of these women, but no empirically tested mental health intervention exists for this patient population.
The psychological damage of an obstetric fistula may result from the traumatic childbirth and/or the resulting physical condition itself (Goh, et al., 2005; Semere & Nour, 2008). Women who develop fistulae due to obstructed labor typically experience several days of painful labor, usually ending in stillbirth, and sometimes accompanied by neurological damage and a cluster of other gynecological morbidities (Arrowsmith, Hamlin, & Wall, 1996). These traumas are compounded by the chronic and humiliating condition of leaking urine and/or feces. About two thirds of a Tanzanian sample of women with fistulae reported social isolation due to their leaking (Bangser, et al., 2011), and studies in other settings observed fistula associated with divorce (Ahmed & Holtz, 2007), stigma (Yeakey, Chipeta, Taulo, & Tsui, 2009), depression (Balogun, 1994; Weston, et al., 2011), and general mental health dysfunction (Browning, et al., 2007; Goh, et al., 2005). Our own research has identified rates of depression and post-traumatic stress disorder among fistula patients that are significantly higher than women recruited from other gynecological clinics (Wilson, Sikkema, Watt, & Masenga, 2015).
In Tanzania, it is estimated that approximately 46,000 women are living with obstetric fistula (National Bureau of Statistics of Tanzania & ICF Macro, 2011). Fortunately, for many years, Tanzania has undertaken efforts to identify women living with fistulae and immediately refer them to free surgical repair (Fiander & Vanneste, 2012). The non-governmental organization Comprehensive Community Based Rehabilitation in Tanzania (CCBRT) is conducting a nation-wide effort to identify and refer patients using community ambassadors and mobile phone technology to transfer funds for ambassador incentives and patient transportation (Fiander & Vanneste, 2012). Other hospitals providing fistula repairs in Tanzania are using similar strategies, as well as radio advertisements and community outreach trips to identify and refer women for repair. In 2011, close to 1,000 obstetric fistula repair surgeries were conducted nationally (Ndahani, 2012). While surgery can address the physical symptoms of a fistula (Nielsen, et al., 2009), surgery alone may not end the challenges that women with fistulae face. Although one study demonstrated reductions in depression immediately post-operation (Browning, et al., 2007), other studies have pointed to continued fistula-related stressors and persistent depression after surgical repair, particularly among women who continue to have symptoms or pain related to their condition, and women who had lived with their fistula for a longer time (Elkins, 1994; Muleta, Hamlin, Fantahun, Kennedy, & Tafesse, 2008; Pope, et al., 2011).
Holistic care for obstetric fistula patients should include mental health treatment as a complement to surgery, so that women receive comprehensive treatment and support for their condition. However, thus far, no evidence-based mental health intervention exists for this population. Women who are admitted for repair generally spend several weeks in the hospital, providing a window of opportunity to address the psychological symptoms accumulated from living with this socially marginalizing condition, and to develop coping skills to facilitate reintegration after repair. Although the need to address mental health issues in this population has been recognized (Muleta, 2006; Muleta, et al., 2008; Pope, et al., 2011) and is part of the WHO’s guiding principles of fistula management (World Health Organization, 2006a), to date no intervention studies have evaluated empirically-supported therapies to assist in psychological healing among fistula patients.
Evidence-based psychological treatment, based on cognitive behavioral therapy (CBT) (Beck, 2011) and the theory of stress and coping (Lazarus & Folkman, 1984) has the potential to improve the coping behavior and mental health symptoms of this patient population, and in turn to improve social well-being and functioning to promote successful reintegration to the community post-surgery (Figure 1). In rigorous trials, CBT demonstrates impacts on mental health, quality of life, and shame, in both Western and non-Western contexts (Butler, Chapman, Forman, & Beck, 2006; DeRubeis & Crits-Christoph, 1998; Neuner, et al., 2008; Neuner, Schauer, Klaschik, Karunakara, & Elbert, 2004; Swan, Watson, & Nathan, 2009; Tshabalala & Visser, 2011; Van't Hof, Cuijpers, Waheed, & Stein, 2011). The theory of stress and coping suggests that improvement in coping skills leads to an increase in positive emotionality, reductions in mental health dysfunction, and improvements in self-care (Folkman & Lazarus, 1988; Lazarus & Folkman, 1984; Penley, Tomaka, & Wiebe, 2002). While mental health treatments have been developed for physical disabilities in the United States (Dorstyn, Mathias, & Denson, 2011; Mehta, et al., 2011; Thomas, Thomas, Hillier, Galvin, & Baker, 2006) and in low-resource countries (Daniel & Manigandan, 2005; Lundgren, Dahl, Melin, & Kies, 2006), an intervention for obstetric fistula patients must be tailored specifically to address physical health concerns, trauma history, stigma, and internalized shame. These dimensions of an intervention must, in turn, reflect the context of gender inequalities in which women develop and live with a fistula.
Figure 1.
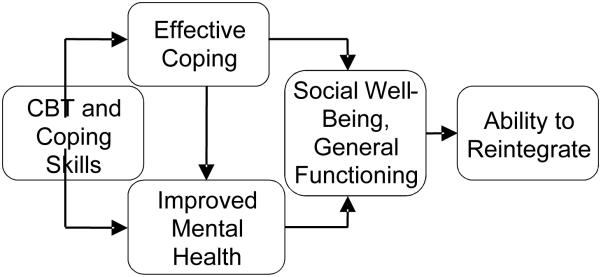
Theoretical Framework
This study aimed to develop a mental health intervention for obstetric fistula patients that can be delivered concurrently with surgical treatment, thereby adding value to clinical services and taking advantage of the “window of opportunity” when patients are in the hospital. The purpose of this paper is to describe the intervention framework and the process of intervention development for the Tanzanian context, and to present results from a small trial run to examine the feasibility and acceptability of this clinic-based intervention for obstetric fistula patients.
2. Methods
2.1 Study site
All study procedures took place at the Kilimanjaro Christian Medical Centre (KCMC) in Moshi, Tanzania. The Department of Obstetrics and Gynecology (OG) at KCMC provides surgical repair of obstetric fistula free of charge and has a dedicated fistula ward. Once admitted to the fistula ward, patients typically undergo reparative surgery within one week and remain on the ward for two to four weeks after the surgery. Approximately 60 patients receive surgical repair for an obstetric fistula at KCMC each year.
2.2 Study overview
The development and feasibility testing of this intervention proceeded in three phases: 1) preliminary intervention development based on psychological theory and empirical research, 2) qualitative data collection to enhance and adapt the intervention curriculum, and 3) a small trial run of the intervention with 6 patients from the KCMC fistula ward. A study advisory board was convened early in the intervention development process, with representatives from fistula care providers, advocacy groups, community health workers, and representatives from the municipal Department of Health. All study procedures were approved by institutional review boards at Duke University, KCMC, and the Tanzanian National Institute for Medical Research.
2.3 Methods for Phase 1: Development of preliminary intervention curriculum
2.3.4 Procedures for Phase 1
Initial intervention development was guided by findings from the investigators’ previous research activities on mental health among obstetric fistula patients at KCMC (Watt, et al., 2014; Wilson, et al., 2015), and resources on CBT and theories of stress and coping. The research team, which included individuals trained in clinical psychology, public health, and obstetrics and gynecology, used their expertise and their experience in this clinical setting to develop the initial intervention curriculum. To accommodate the clinical flow, the team decided that the intervention should be six individual sessions, two prior to surgery and four post-surgery. Sessions combined components of CBT, including coping skills training, relaxation training, identifying thoughts and emotions, cognitive restructuring/reframing, and identifying stressors and effective coping strategies (Beck, 2011). Effective therapeutic techniques, such as medical education, role playing, out-of-session assignments, and validation were used to reinforce concepts and facilitate behavior change (Booth, Beaver, Kitchener, O'Neill, & Farrell, 2005; Miller & Rollnick, 2002). The research team presented the outline of the intervention to the study advisory board, and in a one-day workshop with the board sought feedback on the appropriate session length, suggestions for delivering the intervention to a low-literacy population, and input on the social and cultural acceptance of the content. Breakout sessions during the workshop elicited concrete feedback on the content for each of the six sessions. The research team used the feedback to write an initial draft of the intervention content.
2.4 Methods for Phase 2: Qualitative data collection to refine intervention content and delivery
2.4.1 Participants for Phase 2
After developing the preliminary intervention curriculum, study staff conducted interviews and focus group discussions with a variety of stakeholders to assess the perceived acceptability and feasibility of the intervention and to seek feedback on specific details of the intervention content. In-depth interviews were conducted with six individuals: two patients admitted to KCMC for repair of obstetric fistula (both had lived with a fistula for over 5 years and experienced multiple negative impacts including divorce); two religious leaders (one Muslim imam and one Christian pastor); and, two community outreach workers who specialize in obstetric fistula. Additionally, four focus group discussions (FGDs) were conducted with health care workers at KCMC: two FGDs with nurses in the OG Department who cover the fistula ward; one FGD with medical residents in the OG Department; and, one FGD with nurses in the Community Health Department. A total of 11 individuals participated in the FGDs (3 to 4 per group).
2.4.3 Procedures for Phase 2
Tailored interview guides were developed for the various stakeholder groups (Table 1). The interviews were conducted by either the study coordinator (MM) or the nurse who had been identified to serve as the intervention counselor (PN). The FGDs were facilitated by the study coordinator, and the nurse intervention counselor took notes. The discussions with patients, KCMC staff, and community health workers were conducted in a private room at KCMC, and interviews with the imam and pastor were held at a private location in Moshi convenient for them. After completing each interview and FGD, the interviewer typed notes summarizing the main points discussed for each key area of inquiry. These notes were shared with investigators at Duke University, and the study team together reviewed the data and reached consensus on changes to the intervention curriculum.
Table 1.
Summary of qualitative data collection participants and key areas of inquiry
| Stakeholder Group | Key Areas of Inquiry |
|---|---|
| Obstetric fistula patients (2 in-depth interviews) |
|
| Religious leaders (2 in-depth interviews) |
|
| Community outreach workers (2 in-depth interviews) |
|
| Nurses in obstetrics & gynecology (2 focus group discussions) |
|
| Medical residents (1 focus group discussion) |
|
| Community health nurses (1 focus group discussion) |
|
2.5 Methods for Phase 3: Trial run of the intervention
2.5.1 Staff training for Phase 3
The study coordinator and intervention counselor traveled to Duke University for two weeks in February 2014 to receive training from the study PI (IMW) and experts in clinical psychology (SW and KS). The Duke University investigators provided interactive training on general counseling skills, as well as the theory and principles of cognitive behavioral therapy and stress and coping. The counselor’s training involved role playing delivery of the intervention sessions in both English and Swahili, observation and feedback, and discussion of methods for enhancing fidelity to the curriculum. After the commencement of the trial run of the intervention, training continued via weekly videoconference meetings.
2.5.2 Participants for Phase 3
Trial run participants were recruited from the KCMC fistula ward. Women were eligible for the study if they were at least 18 years old, able to provide informed consent, able to converse comfortably in Swahili, and currently admitted to KCMC for treatment of constant leaking of urine and/or feces due to an obstetric fistula (i.e., a fistula resulting from either obstructed labor or operative injury during Cesarean section). Those who had a fistula due to non-obstetric causes (i.e., hysterectomy and sexual trauma) were not eligible to participate. Patients were identified by a nurse on the fistula ward and screened for eligibility by the study coordinator.
2.5.4 Procedures for Phase 3
Trial run participants completed all six sessions of the curriculum with the nurse counselor. The study coordinator observed about 20% of all sessions to monitor their delivery. Both the counselor and the study coordinator participated in weekly clinical supervision meetings with the study team at Duke University, using Cisco Systems video conferencing technology. A member of the team took notes during the supervision meetings.
The counselor was responsible for filling out clinical notes after each session, detailing fidelity to the curriculum, the participants’ reactions to the sessions, and any challenges she faced in delivering the session. Prior to discharge (approximately 3 days after completing the last intervention session), the study coordinator administered a brief questionnaire to gauge the participant’s experience with the intervention. Participants were asked separate questions about their satisfaction with the intervention and the counselor (response options: very satisfied, satisfied, a little satisfied, not satisfied), and their feedback on the number of sessions and time spent on the intervention (response options: the right amount of time, too little time, too much time). Open ended questions asked about what they liked and did not like about the intervention, what they thought should be changed, and any general feedback about the experience. They were asked to rate the usefulness of each of the six sessions (response options: very useful, somewhat useful, not useful). Finally, they were asked whether they would be willing to take part in the intervention again. The responses to the questionnaire, together with the counselor’s clinical notes, the study coordinator’s observations, and the notes from the clinical supervision meetings were used to assess the preliminary feasibility and acceptability of delivering the intervention in this clinical setting.
3. Results
3.1 Phases 1 & 2: Intervention development
The intervention curriculum built upon techniques of CBT and was developed based on observations from the team’s previous work, feedback from the study advisory board meeting, and findings from qualitative data collection. The final curriculum included six sessions of individual counseling, with each session having a specific topical focus (see Table 2). The first two sessions were intended for delivery before the woman’s surgery, and the remaining four were intended to take place after her surgery. All sessions consisted of approximately 60 minutes of material and were designed for delivery by a non-specialist mental health counselor in an individual, private setting.
Table 2.
Overview of intervention sessions
| Session | Objective |
|---|---|
| Pre-surgery | |
| 1) Recounting the fistula story |
Orient the patient to individual therapy; identify the impact of the woman’s traumatic birth and resulting fistula; highlight goals for discussion and problem-solving within therapy. |
| 2) Creating a new story about your fistula |
Teach medical information on fistula and surgery; validate experience as a normal medical condition; help the patient reframe her personal narrative. |
| Post-surgery | |
| 3) Identifying thoughts and emotions |
Review key emotions; identify negative and problematic thoughts; link thoughts to resulting emotions; begin practicing reframing problematic thoughts. |
| 4) Strategies for coping | Discuss the patient’s negative vs. positive coping strategies; coach patient to recognize stressors and respond by utilizing appropriate and effective coping skills. |
| 5) Social relationships: How they can help and hurt |
Discuss how one’s social network influences thoughts and feelings; formulate strategies to expand and optimize patient’s social support network; review tools to discuss her condition with others; call a support person to practice communication skills. |
| 6) Planning for the future: Realism and hope |
Make practical plans for the patient’s return to her community; discuss the possibility of incomplete cure & post-surgery medical recommendations; mobilize home support through a phone session with a supportive individual in the community. |
Session 1: Recounting the fistula story
The overarching goals of Session 1 are for the counselor to normalize the patient’s experience, to acknowledge the negative and possible positive impacts of the fistula experience on relationships with others, and to begin exploration of how the patient’s experience of an obstetric fistula impacts her feelings and thoughts about herself. During Phase 2 of intervention development (qualitative data collection to inform the intervention), informants had generated a list of common negative and positive impacts that fistula patients often experience (e.g., loss of a child, various impacts on family relationships), which were included in the curriculum as examples. In Session 1, the counselor spends the majority of time hearing the woman’s story of how she developed the fistula, and all the ways that it has impacted her life. The counselor was trained to generate discussion about the impacts that are in the curriculum as examples, but also to allow other impacts to emerge, depending on the patient’s experience. In the course of the patient telling her story, the counselor helps the patient to acknowledge the effects that the fistula has had on her thoughts and emotions. The counselor orients the patient to the intervention by summarizing the curriculum and discussing guidelines for the sessions. Behavior change is emphasized in this session through generating and recording goals for therapy. To conclude the session, the counselor leads the patient through a deep breathing relaxation exercise to reduce muscle tension and decrease distress. The patient is asked to practice this exercise daily before the next session. During Phase 2, this deep breathing exercise was unanimously deemed appropriate and feasible for the patient population, with some noting that it was consistent with women’s use of silent prayer as a way to relax and ease tension.
Session 2: Creating a new story about your fistula
Session 2, and all subsequent sessions, begins with practicing the relaxation exercise and reviewing any assignment from the previous session. The aim of Session 2 is to promote cognitive reframing of the fistula experience through medical education. The counselor educates the patient using drawn handouts of the reproductive system, as well as a life-size anatomical model of the female pelvis. The counselor dispels common myths about fistula, a list of which was generated by key informants during Phase 2. Education involves opportunities for the patient to ask questions, as well as a reverse role-play in which the patient explains to the counselor how a fistula develops. Medical information is solidified when the patient and counselor create a revised story about the patient’s fistula development, incorporating her newly acquired medical knowledge into the story and devoid of any misconceptions she might have spoken about in the original recount of her fistula development. Following this reframing, the counselor provides education to the patient about her upcoming fistula repair surgery, incorporating any relevant information she has received from the patient’s gynecologist outside of sessions. The patient is asked to disclose her hopes, anxieties, and/or questions about treatment. The assigned practice exercise includes the daily relaxation exercise, as well as an assignment to ask a health care provider at least one question (e.g., about the prospects for her surgery), which she identified together with the counselor. This activity is intended to build self-efficacy to engage with providers and increase health literacy, and was incorporated because health care workers reported that women felt very shy to ask questions to providers.
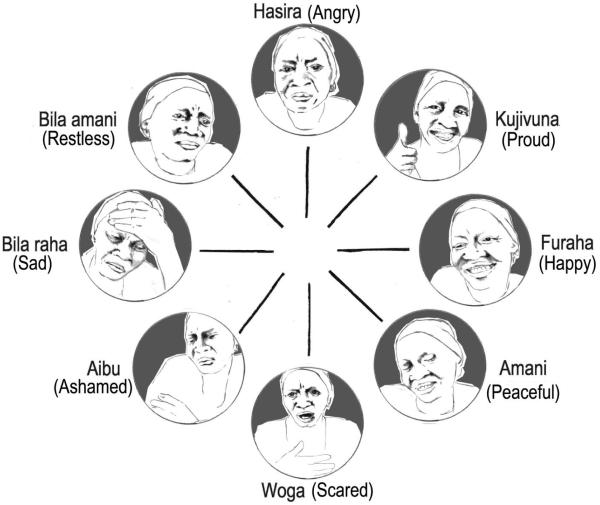
Session 3: Identifying thoughts and emotions
Session 3 is delivered approximately three or four days after the patient’s surgery, or as soon as she is pain-free while sitting. The overall goal of this session is to introduce the patient to the cognitive model, and to begin teaching her how to reframe negative or unhelpful thoughts. Results from Phase 2 revealed that the cognitive model required simplification in order to be covered in a time-limited intervention for a low literacy population. The study advisory board suggested creating a culturally-specific emotion wheel, a commonly used tool in the practice of cognitive behavioral therapy (Arrowsmith, et al., 1996). During Phase 2, the most common emotion words in Swahili were elicited from key informants, and a graphic artist created cartoon faces depicting each emotion (Figure 2). Using the emotion wheel, the patient identifies situations in which she has felt each emotion (e.g., shame in relation to leaking, pride in reaching the hospital). The objective of this exercise is to introduce the patient to the process of identifying and discussing her emotions. After discussing emotions, the counselor defines and discusses thoughts. The counselor asks the patient to endorse which of a list of negative and positive thoughts she has had (e.g., “I am worthless” or “This problem is not my fault”). These thoughts were generated based on our previous qualitative work in this setting, as well as findings from in-depth interviews and focus group discussions in Phase 2. The counselor chooses one negative thought, and works with the patient to reframe the negative thought into a more helpful, positive, and accurate thought. At the end of session, the counselor introduces the “Serenity Prayer” and relates it to the patient’s experience. Previous research has indicated the importance of issues of faith for fistula patients in Tanzania (Creanga & Genadry, 2007), and this prayer was chosen because it reinforces concepts of managing thoughts and emotions, and begins to introduce the idea of coping. In Phase 2 qualitative interviews and focus groups, participants felt that this prayer would resonate with the patient population, and that it would be acceptable for patients of varying faith backgrounds, including both Christian and Muslim faiths. The patient’s homework for this session is to practice reframing another one of her endorsed negative thoughts, and to practice deep breathing daily.
Figure 2.
Emotion wheel
Session 4: Specific strategies for coping
The goal of session 4 is to help the patient to recognize and respond to stressors in her life by utilizing appropriate and effective coping skills. The session begins with the patient creating a list of life stressors, and then categorizing each stressor as changeable or unchangeable. The counselor teaches the patient about coping and discusses how coping behaviors can be helpful (i.e., adaptive) or unhelpful (i.e., maladaptive). The patient then identifies coping strategies she has used the in the past and classifies them as helpful or unhelpful for dealing with her stressors. In order to decrease the use of negative coping, the counselor concludes the session by helping the patient to create a behavioral plan to effectively cope with negative stressors. For the between-session activity, the patient is asked to practice using a helpful coping strategy to deal with something that she finds difficult or stressful.
Session 5: Social relationships - How they can help and hurt
The goal of session 5 is to examine the effect of social relationships on the patient’s life, and to generate specific strategies to strengthen social relationships. The counselor defines social support and guides the patient in identifying primary sources of social support. A handout was developed to aid the counselor in identifying sources of social support (e.g., family, friends, healthcare providers). The counselor and patient categorize types of support (e.g., emotional, financial, practical, informational). They also discuss with whom the patient has talked about her fistula, and the pros and cons of talking about her fistula with others. The counselor and patient role play potential discussions about fistula that she might have with people in her life, referring back to the medical education about fistula. As recommended during Phase 2 qualitative interviews, the counselor emphasizes that disclosure of the patient’s experience is an option but not required. The counselor then facilitates a telephone call between the patient and a chosen social support person, intended to facilitate social support and practical plans for returning home after repair. The study advisory board had advised to try and integrate a supportive person in the therapy sessions, since Tanzanian culture is more communal than individual. Given that fistula patients typically come to the hospital by themselves, telephone was seen as the most appropriate way to engage a support person. If there is no one available for the patient to speak with, then the counselor and patient spend time continuing to discuss opportunities and challenges around social support. For homework, the patient considers her thoughts and feelings about going home.
Session 6: Planning for the future-Realism and hope
The goal of the final intervention session is to prepare the patient for her return home, which maximizes the likelihood of a positive reintegration experience. The session begins with the patient discussing her thoughts and emotions about going home. The counselor discusses these thoughts and feelings, and helps to problem solve strategies to deal with various circumstances and to cope with potential stressors. The information discussed is then used to make a detailed step-by-step action plan for the patient’s first two weeks home after discharge. The counselor then assists the patient to conduct a second phone call with her social support person, where she has the opportunity to share some of her reintegration plans and solidify support. Before concluding the final session, the counselor provides a summary of post-surgery medical recommendations (e.g., 3 months of sexual abstinence, no heavy work). The patient also has an opportunity to ask any additional questions about her fistula, surgery, or health. As recommended by the study advisory board, the patient is provided with realistic information about the possibility of further leaking that might occur due to either an unsuccessful repair or residual stress incontinence, and when it is appropriate to seek further treatment. The session concludes by reviewing the patient’s goals for therapy, discussing her progress in reaching the goals, and making a plan to help her continue working on her goals in the future. The counselor then congratulates the woman on her completion of the intervention, and wishes her well in her reintegration home.
3.2 Phase 3: Lessons learned from trial run of the intervention
3.2.2 Description of the sample
The intervention was delivered with 6 participants between March and July 2014. The women ranged in age from 26 to 46 (mean 37). One woman had lived with a fistula only 4 weeks, while the rest had developed the fistula 1 to 15 years prior (mean 5.7 years). None of the women had education beyond the primary level. Five of the six had a stillbirth at the time of the fistula development, and none reported experiencing divorce or separation due to the fistula.
3.2.3 Intervention feasibility
Six women met eligibility criteria and were invited to participate. The study coordinator explained the intervention, and all agreed to participate. All participants completed the full six sessions, suggesting that the intervention length was feasible in the time that women spent on the ward. In all cases, the intervention was delivered as intended, with two sessions prior to surgery and four sessions following surgery. For one woman, the brief time between hospital admission and surgery required that the first two intervention sessions were delivered on the same day. In several cases, the counselor had to reschedule sessions because the patient had physical symptoms (e.g., headache or pain), which made it difficult for her to attend the therapy session. The nursing staff in the fistula ward collaborated with the counselor to support the intervention, helping her to facilitate scheduling and secure a private space for the sessions.
In clinical supervision meetings, the counselor reported feeling confident in her ability to deliver the sessions as they were intended. She did note, however, some specific areas that she found challenging. These included helping a woman to recognize that her internalized thoughts were changeable and helping her to identify and embrace alternative thoughts; grappling with social relationships that felt unchangeable (e.g., unsupportive parents-in-law); and helping to find solutions to women’s stressors related to poverty and income generation. Depending on the woman’s education and literacy, the counselor found that she had to take more time or simplify concepts even further to ensure that they resonated.
3.3.3 Feedback from participants
In the exit interviews that participants completed, the ratings were very positive (Table 3). Patients were highly satisfied with both the intervention content and the counselor. The assessment of the time spent on the intervention varied; four felt that the number of sessions and time spent on the intervention was the correct amount of time, while two felt that there were both too many sessions and too much time per session. In the open-ended questions, participants reported that they liked participating in the intervention because it helped them “release tensions, thoughts, and fears;” learn more about their fistula treatment and how to care for themselves once they returned home; and learn coping strategies like the “relaxation exercise, serenity prayer” and “breathing exercise.” All six sessions were universally rated as somewhat or very useful to all participants. Session 2 (Creating a new story about your fistula) had the highest rating of usefulness. When asked, all patients said that they would be willing to participate in such an intervention again.
Table 3.
Results of the exit interview with patients (n=6)
| n | |
|---|---|
| Satisfaction with intervention | |
| Very satisfied | 5 |
| Satisfied | 1 |
| A little satisfied | 0 |
| Not satisfied | 0 |
| Satisfaction with counselor | |
| Very satisfied | 6 |
| Satisfied | 0 |
| A little satisfied | 0 |
| Not satisfied | 0 |
| Number of sessions | |
| Right amount | 4 |
| Too little | 0 |
| Too much | 2 |
| Time spent per session | |
| Right amount | 4 |
| Too little | 0 |
| Too much | 2 |
The counselor reported in clinical supervision meetings that she developed warm and supportive relationships with the patients. She expressed sadness when the intervention concluded for patients, and expressed genuine concern for the well-being of the patients she worked with. She expressed that patients similarly expressed warm connections towards her, often promising to visit her again or asking for her phone number so that they could stay in touch.
4. Discussion
This paper described the development and trial run of a mental health intervention for obstetric fistula patients in Tanzania. Building upon psychological theory of CBT and stress and coping, and with input from a range of stakeholders and a study advisory board, we developed a six session intervention delivered to women during the period they were hospital inpatients for fistula surgical repair. We were able to design an intervention that was feasible for delivery in a health care setting, and that was highly regarded by patients. A future randomized control trial will assess the ability for this intervention to improve the mental health of fistula patients and to support the reintegration to their communities after surgery.
The intervention that was developed built upon psychological theory, but required adaptation and tailoring to the specific patient population. One notable adaptation was an overarching emphasis on a woman’s social standing and relationships with others. Unlike Western settings, Tanzanian culture is more communal than individualistic (Velez, Ramsey, & Tell, 2007). While garnering social support is typically included as a target in psychotherapy (Nunez Bragayrac, Azhar, & Sotelo, 2015), our study advisory board and informant interviews were insistent that social identity, as well as social relationships, needed to be a central theme in the intervention. This focus was considered important to both resonate with Tanzanian culture, as well as to address the fact that obstetric fistula typically results in social isolation and loss of standing in the family and community (Lassey, 2007). A focus on social relationships was integrated into several sessions of the intervention. The content on reframing thoughts helped women to rethink their about cognitions about not being a meaningful member of their community due to the fistula. The content on social support helped patients to take stock of the meaningful people in their lives, and identify ways to garner more support and to talk about their fistula condition with these people. The intervention was also guided by the fact that many husbands and family members remain supportive of the woman with fistula (Landry, et al., 2013; Lassey, 2007; Zheng & Anderson, 2009; Zheng, Harrington, Love, Thelemaque, & Anderson, 2013), and it was recommended to us that these individuals should be included in some way in the intervention. Since most women arrived at the hospital by themselves and were typically too far from home to receive visitors, cell phone calls were used as a way to engage support people in the intervention. This approach was feasible given the ubiquity of cell phones in Tanzania. These calls helped to foster support and share information with supporters, reconnect the woman with an important person in her life, and serve as a bridge between the hospital and home environments.
A second modification of the intervention after input in Phase 2 was the integration of religious concepts throughout the curriculum. In Tanzania, religion is an important aspect of culture and life, and studies suggest that Tanzanians rely on religion to cope with adverse medical events (Steglitz, Ng, Mosha, & Kershaw, 2012; Watt, Maman, Jacobson, Laiser, & John, 2009), including obstetric fistula (Creanga & Genadry, 2007). The study advisory board suggested that religious content that would resonate with individuals of both Christian and Muslim faiths would be important to include, and interviews with an imam and a pastor helped to identify opportunities to do so. The counselor was trained to speak openly to the woman about her religious beliefs, and to tailor the curriculum to meet her needs and comfort. This may have included introducing the deep breathing exercise as similar to silent prayer, questioning the woman about her participation in religious activities and how that has changed with her fistula, and suggesting religious engagement as a way to cope with stressors in her life. The serenity prayer was included as a way to introduce a religious message that also reinforced the concepts of recognizing stressors as changeable and unchangeable, and relying on religion as a coping mechanism. Because the prayer includes asking God for “the courage to change the change I can,” it harnesses religion against the idea of fatalism and empowers women to use active coping behaviors.
A third modification of the intervention after input in Phase 2 involved making adjustments to the curriculum to improve integration in the hospital setting. As noted, the time that women spend in the hospital for their surgery is a window of opportunity for the delivery of a psychological intervention. However, the intervention had to be designed in a way that was well integrated with the clinic flow, and flexible enough to be tailored to any unique clinical needs of the patients. At the suggestion of the study advisory board, the intervention was designed to have two sessions that occurred prior to the surgery, and four sessions that occurred after the surgery. Before the surgery, the patient had the opportunity to tell her story developing and living with a fistula and identify some key impacts that she has experienced. She also received comprehensive medical education about her fistula, including about the fistula surgery, and was given the opportunity to ask any questions that she had, reducing anxiety about the surgery. This information was provided in session two, which participants rated as the most useful of all sessions, likely highlighting the perceived utility of medical education at this crucial time prior to surgery. After the surgery, the counselor introduced the ideas of thoughts and emotions, coping, and social relationships, all integrating both the woman’s story and the medical education that had been provided. The final session provided a way to wrap up the content of the intervention and make the transition to thinking about leaving the hospital and going home.
Although a group intervention model was considered at the start of this study, we decided on an individual model for several reasons. First and foremost, we felt that it was important to have the opportunity for the woman to fully share her story developing and living with an obstetric fistula, and to tailor the conversations to address her unique experience. For example, a woman who had lived with a fistula for ten years and suffered serious consequences like divorce would need to address different issues than a woman who had only recently experienced a fistula and was most concerned with her ability to have more children. Another reason that we felt an individual model would be better was unique to the clinical setting where we were working, where the patient load was not consistent enough to form sufficiently sized groups. Lastly, we felt that the progression of topics was important (e.g., starting with telling the story and getting medical education, and ending with discussing reintegration). A drop-in group would not have met that need, and waiting for groups to form would not have been feasible given that intervention delivery had to happen within the time period of the hospital stay. Although we feel that the individual model was best for this population and setting, we recognize that it missed the opportunity to garner support from other women and to normalize the fistula experience. In the intervention session on social support, we encouraged the patient to think about fellow fistula patients on the ward as part of her support system, and we observed women communing and speaking together on the ward.
This study offers some key lessons on choosing and supervising a non-specialist mental health counselor for the delivery of a psychological intervention for this population. Unfortunately, there is very limited psychological training in Tanzania, requiring the use of non-psychiatric providers, an approach known in the global mental health field as “task shifting” (Eaton, et al., 2011; Kakuma, et al., 2011; World Health Organization, 2006b) and practiced in other clinical situations in Tanzania. For this intervention, a community nurse was seen as an appropriate person to serve as the counselor, given her familiarity with obstetric complications, and her ability to converse with patients about issues beyond physical presentation and ailments. Nurse-delivered psychological interventions have been shown to be effective in other low-resource countries (Araya, et al., 2003). Extensive training was provided to the counselor to teach the underlying psychological theory, and to build therapeutic skills such as empathy and active listening, and clinical supervision via video conferencing served to reinforce these concepts. The counselor’s excellent fidelity to the intervention, along with feedback from study participants and the counselor herself about the strong counselor-patient relationships that were developed, suggest a community nurse can serve as a counselor in this setting when she has the appropriate level of training and supervision.
In future examinations of this intervention, greater attention should be paid to how the counselor adapts the intervention content to reflect the heterogeneity of experiences in this participant population (e.g., in the length of time they had been living with a fistula and the impacts of the fistula on their lives). Training of the counselors should emphasize their skills and empowerment to tailor the curriculum to the participant’s unique set of experiences and to address the areas that the participant finds most personally distressing. In a future randomized control trial of this intervention, the impact of the intervention on both psychological and behavioral outcomes should be assessed. Given the importance of psychological state on long-term reintegration and quality of life, outcomes should be assessed several months after discharge to examine whether impacts are sustainable over time. Additionally, data should be disaggregated to examine any differential impact of the intervention based on the time the woman has lived with the fistula and whether or not her child survived the birth.
This study has limitations that must be considered. The intervention was developed for implementation in one hospital, and may not be suitable for other settings without modifications for the unique experiences of the patient population and the clinic flow. The counselor received extensive training on the curriculum, but it is impossible to distinguish the positive feedback about the intervention curriculum content itself from the personality and abilities of the counselor. Although the trial run was intended only to assess the feasibility and acceptability of the intervention, the sample size was nevertheless small, making it difficult to draw definitive conclusions or to assess for any associations. Additionally, the results of the exit questionnaire may have been influenced by social desirability bias, with women reluctant to report any negative impressions of the services they had received. The current study did not include a formal evaluation or include assessments post-discharge; however, an RCT is in progress to assess the impact of the intervention on psychological and behavioral outcomes at discharge and 3-month follow up. Despite its limitations, the current study has notable strengths, including its foundation of psychological theory and the adaptations and modifications that were informed by input from stakeholders including advocates, patients, and health care workers.
4.1 Conclusion
In conclusion, this paper describes a psychological intervention that was developed for obstetric fistula patients in Tanzania. It addresses the dire need for psychological support for fistula patients, given the high rates of distress that have been documented (Balogun, 1994; Browning, et al., 2007; Goh, et al., 2005; Weston, et al., 2011). Although other intervention approaches have been proposed to improve the mental health and well-being of fistula patients (Gerten, Venkatesh, Norman, Shu'aibu, & Richter, 2009; Johnson, et al., 2010; Ojengbede, et al., 2014), this is the first to describe the development of an intervention that is built on psychological theory and informed by stakeholder input.
4.2 Lessons learned
The intervention development process provided some key lessons for the development of mental health interventions for this unique populations: 1) the importance of formative work to adapt and tailor psychological theory to the specific needs and cultural framework of the target population; 2) the importance of designing an intervention curriculum and protocol that is integrated within the clinic flow; and 3) the feasibility of using a non-specialist mental health specialist for delivery of a psychological intervention, with appropriate training and supervision. If this intervention should prove efficacious in a future randomized control trial, then scale up within fistula repair programs should be considered.
Highlights.
We developed a mental health intervention for Tanzanian women with obstetric fistula.
We describe the intervention content and how it was informed by stakeholders.
We demonstrate adaptation of psychological theory for a unique patient population.
A small trial run demonstrated feasibility and acceptability of the intervention.
Acknowledgments
Funding:
This project was supported by the National Institute of Child Health & Human Development, grant R21 HD073681.
Biographies
Melissa H. Watt, Ph.D. is an Assistant Professor of Global Health at Duke University. She brings her training in public health to understand and address the factors that impact women’s health in sub-Saharan Africa. Her research in Tanzania focuses on the mental health needs of women who are seeking surgical care for obstetric fistula.
Sarah M. Wilson, M.A. is a doctoral student in Clinical Psychology at Duke University. Her research interests include the psychological sequelae of obstetric fistula, exploration of trauma and posttraumatic stress disorder (PTSD) cross-culturally, and the intersection of physical and mental health.
Kathleen J. Sikkema, Ph.D. is a Professor of Psychology and Neuroscience and Professor of Global Health at Duke University. She has expertise in the development and evaluation of interventions to address mental health in patient populations.
Jennifer Velloza, M.P.H. conducted this work as a researcher at the Duke Global Health Institute, where she was involved in a range of studies related to mental and physical health in the global context.
Mary Mosha, M.Sc., M.P.H. is a lecturer in community health at the Kilimanjaro Christian Medical College in Moshi, Tanzania, and coordinator of a study on obstetric fistula.
Gileard G. Masenga, M.D. is the chair of Obstetrics and Gynecology and a fistula surgeon at the Kilimanjaro Christian Medical Center in Moshi, Tanzania.
Margaret Bangser, M.P.P.M. is an advocate for maternal health in Tanzania, and a contributor to several programmatic and research efforts to prevent and treat obstetric fistula in East Africa.
Andrew Browning, M.D. is a fistula surgeon at Selian Lutheran Hospital in Arusha, Tanzania, and founder of the non-governmental organization Maternity Africa.
Pilli Nyindo, R.N. is a community health nurse at Kilimanjaro Christian Medical Center and intervention facilitator for a study on mental health of obstetric fistula patients.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Ahmed S, Holtz SA. Social and economic consequences of obstetric fistula: life changed forever? International Journal of Gynaecology and Obstetrics. 2007;99(Suppl 1):S10–15. doi: 10.1016/j.ijgo.2007.06.011. [DOI] [PubMed] [Google Scholar]
- Araya R, Rojas G, Fritsch R, Gaete J, Rojas M, Simon G, Peters TJ. Treating depression in primary care in low-income women in Santiago, Chile: a randomised controlled trial. Lancet. 2003;361:995–1000. doi: 10.1016/S0140-6736(03)12825-5. [DOI] [PubMed] [Google Scholar]
- Arrowsmith S, Hamlin EC, Wall LL. Obstructed labor injury complex: obstetric fistula formation and the multifaceted morbidity of maternal birth trauma in the developing world. Obstetrical and Gynecological Survey. 1996;51:568–574. doi: 10.1097/00006254-199609000-00024. [DOI] [PubMed] [Google Scholar]
- Balogun SK. A comparison of psychological status of vesico vaginal fistula (V. V. F.) sufferers and nonsufferers in southern Nigeria. IFE Psychologia: An International Journal. 1994;2:6–14. [Google Scholar]
- Bangser M, Mehta M, Singer J, Daly C, Kamugumya C, Mwangomale A. Childbirth experiences of women with obstetric fistula in Tanzania and Uganda and their implications for fistula program development. International Urogynecology Journal and Pelvic Floor Dysfunction. 2011;22:91–98. doi: 10.1007/s00192-010-1236-8. [DOI] [PubMed] [Google Scholar]
- Beck JS. Cognitive behavior therapy: Basics and beyond. Guilford Press; 2011. [Google Scholar]
- Booth K, Beaver K, Kitchener H, O'Neill J, Farrell C. Women's experiences of information, psychological distress and worry after treatment for gynaecological cancer. Patient Education and Counseling. 2005;56 doi: 10.1016/j.pec.2004.02.016. [DOI] [PubMed] [Google Scholar]
- Browning A, Fentahun W, Goh JTW. The impact of surgical treatment on the mental health of women with obstetric fistula. Bjog-an International Journal of Obstetrics and Gynaecology. 2007;114:1439–1441. doi: 10.1111/j.1471-0528.2007.01419.x. [DOI] [PubMed] [Google Scholar]
- Butler AC, Chapman JE, Forman EM, Beck AT. The empirical status of cognitive-behavioral therapy: a review of meta-analyses. Clinical Psychology Review. 2006;26:17–31. doi: 10.1016/j.cpr.2005.07.003. [DOI] [PubMed] [Google Scholar]
- Creanga AA, Genadry RR. Obstetric fistulas: A clinical review. International Journal of Gynecology & Obstetrics. 2007;99(Supplement 1):S40–S46. doi: 10.1016/j.ijgo.2007.06.021. [DOI] [PubMed] [Google Scholar]
- Daniel A, Manigandan C. Efficacy of leisure intervention groups and their impact on quality of life among people with spinal cord injury. International Journal of Rehabilitation Research. 2005;28:43–48. doi: 10.1097/00004356-200503000-00006. [DOI] [PubMed] [Google Scholar]
- DeRubeis RJ, Crits-Christoph P. Empirically supported individual and group psychological treatments for adult mental disorders. Journal of Consulting and Clinical Psychology. 1998;66:37–52. doi: 10.1037//0022-006x.66.1.37. [DOI] [PubMed] [Google Scholar]
- Dorstyn DS, Mathias JL, Denson LA. Psychosocial outcomes of telephone-based counseling for adults with an acquired physical disability: A meta-analysis. Rehabilitation Psychology. 2011;56:1–14. doi: 10.1037/a0022249. [DOI] [PubMed] [Google Scholar]
- Eaton J, McCay L, Semrau M, Chatterjee S, Baingana F, Araya R, Ntulo C, Thornicroft G, Saxena S. Scale up of services for mental health in low-income and middle-income countries. The Lancet. 2011;378:1592–1603. doi: 10.1016/S0140-6736(11)60891-X. [DOI] [PubMed] [Google Scholar]
- Elkins TE. Surgery for the obstetric vesicovaginal fistula: a review of 100 operations in 82 patients. American Journal of Obstetrics and Gynecology. 1994;170:1108–1118. doi: 10.1016/s0002-9378(94)70105-9. discussion 1118-1120. [DOI] [PubMed] [Google Scholar]
- Fiander AN, Vanneste T. transportMYpatient: an initiative to overcome the barrier of transport costs for patients accessing treatment for obstetric fistulae and cleft lip in Tanzania. Tropical Doctor. 2012;42:77–79. doi: 10.1258/td.2011.110423. [DOI] [PubMed] [Google Scholar]
- Folkman S, Lazarus RS. Coping as a mediator of emotion. Journal of Personality and Social Psychology. 1988;54:466–475. [PubMed] [Google Scholar]
- Gerten KA, Venkatesh S, Norman AM, Shu'aibu J, Richter HE. Pilot study utilizing a patient educational brochure at a vesicovaginal fistula hospital in Nigeria, Africa. International Urogynecology Journal and Pelvic Floor Dysfunction. 2009;20:33–37. doi: 10.1007/s00192-008-0720-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goh JTW, Sloane KM, Krause HG, Browning A, Akhter S. Mental health screening in women with genital tract fistulae. Bjog-an International Journal of Obstetrics and Gynaecology. 2005;112:1328–1330. doi: 10.1111/j.1471-0528.2005.00712.x. [DOI] [PubMed] [Google Scholar]
- Johnson KA, Turan JM, Hailemariam L, Mengsteab E, Jena D, Polan ML. The role of counseling for obstetric fistula patients: Lessons learned from Eritrea. Patient Education and Counseling. 2010;80:262–265. doi: 10.1016/j.pec.2009.11.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kakuma R, Minas H, van Ginneken N, Dal Poz MR, Desiraju K, Morris JE, Saxena S, Scheffler RM. Human resources for mental health care: current situation and strategies for action. The Lancet. 2011;378:1654–1663. doi: 10.1016/S0140-6736(11)61093-3. [DOI] [PubMed] [Google Scholar]
- Landry E, Frajzyngier V, Ruminjo J, Asiimwe F, Barry TH, Bello A, Danladi D, Ganda SO, Idris S, Inoussa M, Kanoma B, Lynch M, Mussell F, Podder DC, Wali A, Mielke E, Barone MA. Profiles and experiences of women undergoing genital fistula repair: Findings from five countries. Glob Public Health. 2013;8:926–942. doi: 10.1080/17441692.2013.824018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lassey AT. Simple fistulas: Diagnosis and management in low-resource settings—A descriptive report. International Journal of Gynecology & Obstetrics. 2007;99(Supplement 1):S47–S50. doi: 10.1016/j.ijgo.2007.06.025. [DOI] [PubMed] [Google Scholar]
- Lazarus R, Folkman S. Stress, Appraisal and Coping. Springer Publishing Company; New York, NY: 1984. [Google Scholar]
- Lundgren T, Dahl JA, Melin L, Kies B. Evaluation of acceptance and commitment therapy for drug refractory epilepsy: A randomized controlled trial in South Africa - A pilot study. Epilepsia. 2006;47:2173–2179. doi: 10.1111/j.1528-1167.2006.00892.x. [DOI] [PubMed] [Google Scholar]
- Mehta S, Orenczuk S, Hansen KT, Aubut JA, Hitzig SL, Legassic M, Teasell RW. An evidence-based review of the effectiveness of cognitive behavioral therapy for psychosocial issues post-spinal cord injury. Rehabilitation Psychology. 2011;56:15–25. doi: 10.1037/a0022743. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller WR, Rollnick S. Motivational interviewing: Preparing people for change. Guilford press; 2002. [Google Scholar]
- Muleta M. Obstetric fistula in developing countries: a review article. Journal of Obstetrics and Gynaecology Canada. 2006;28:962–966. doi: 10.1016/S1701-2163(16)32305-2. [DOI] [PubMed] [Google Scholar]
- Muleta M, Hamlin EC, Fantahun M, Kennedy RC, Tafesse B. Health and social problems encountered by treated and untreated obstetric fistula patients in rural Ethiopia. Journal of Obstetrics and Gynaecology Canada. 2008;30:44–50. doi: 10.1016/S1701-2163(16)32712-8. [DOI] [PubMed] [Google Scholar]
- National Bureau of Statistics of Tanzania & ICF Macro . Tanzania Demographic and Health Survey 2010. NBC and ICF Macro; Dar es Salaam, Tanzania: 2011. [Google Scholar]
- Ndahani C. Identifying women for fistula repair using transportMYpatient; Addressing the psychosocial needs of obstetric fistula patients in Tanzania: A Duke/KCMC workshop; Moshi, Tanzania. 2012. Publishing. [Google Scholar]
- Neuner F, Onyut PL, Ertl V, Odenwald M, Schauer E, Elbert T. Treatment of posttraumatic stress disorder by trained lay counselors in an African refugee settlement: a randomized controlled trial. Journal of Consulting and Clinical Psychology. 2008;76:686–694. doi: 10.1037/0022-006X.76.4.686. [DOI] [PubMed] [Google Scholar]
- Neuner F, Schauer M, Klaschik C, Karunakara U, Elbert T. A comparison of narrative exposure therapy, supportive counseling, and psychoeducation for treating posttraumatic stress disorder in an african refugee settlement. Journal of Consulting and Clinical Psychology. 2004;72:579–587. doi: 10.1037/0022-006X.72.4.579. [DOI] [PubMed] [Google Scholar]
- Nielsen HS, Lindberg L, Nygaard U, Aytenfisu H, Johnston OL, Sorensen B, Rudnicki M, Crangle M, Lawson R, Duffy S. A community-based long-term follow up of women undergoing obstetric fistula repair in rural Ethiopia. BJOG: An International Journal of Obstetrics and Gynaecology. 2009;116:1258–1264. doi: 10.1111/j.1471-0528.2009.02200.x. [DOI] [PubMed] [Google Scholar]
- Nunez Bragayrac LA, Azhar RA, Sotelo R. Minimally invasive management of urological fistulas. Curr Opin Urol. 2015 doi: 10.1097/MOU.0000000000000144. [DOI] [PubMed] [Google Scholar]
- Ojengbede OA, Baba Y, Morhason-Bello IO, Armah M, Dimiti A, Buwa D, Kariom M. Group psychological therapy in obstetric fistula care: a complementary recipe for the accompanying mental ill health morbidities? African Journal of Reproductive Health. 2014;18:155–159. [PubMed] [Google Scholar]
- Onsrud M, Sjoveian S, Mukwege D. Cesarean delivery-related fistulae in the Democratic Republic of Congo. International Journal of Gynaecology and Obstetrics. 2011;114:10–14. doi: 10.1016/j.ijgo.2011.01.018. [DOI] [PubMed] [Google Scholar]
- Penley JA, Tomaka J, Wiebe JS. The association of coping to physical and psychological health outcomes: A meta-analytic review. Journal of Behavioral Medicine. 2002;25:551–603. doi: 10.1023/a:1020641400589. [DOI] [PubMed] [Google Scholar]
- Pope R, Bangser M, Harris Requejo J. Restoring dignity: Social reintegration after obstetric fistula repair in Ukerewe, Tanzania. Glob Public Health. 2011:1–15. doi: 10.1080/17441692.2010.551519. [DOI] [PubMed] [Google Scholar]
- Raassen TJ, Ngongo CJ, Mahendeka MM. Iatrogenic genitourinary fistula: an 18-year retrospective review of 805 injuries. Int Urogynecol J. 2014;25:1699–1706. doi: 10.1007/s00192-014-2445-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Semere L, Nour NM. Obstetric fistula: living with incontinence and shame. Reviews in Obstetrics and Gynecology. 2008;1:193–197. [PMC free article] [PubMed] [Google Scholar]
- Stanton C, Holtz SA, Ahmed S. Challenges in measuring obstetric fistula. International Journal of Gynecology & Obstetrics. 2007;99(Supplement 1):S4–S9. doi: 10.1016/j.ijgo.2007.06.010. [DOI] [PubMed] [Google Scholar]
- Steglitz J, Ng R, Mosha JS, Kershaw T. Divinity and distress: the impact of religion and spirituality on the mental health of HIV-positive adults in Tanzania. AIDS and Behavior. 2012;16:2392–2398. doi: 10.1007/s10461-012-0261-7. [DOI] [PubMed] [Google Scholar]
- Swan A, Watson HJ, Nathan PR. Quality of Life in Depression: An Important Outcome Measure in an Outpatient Cognitive-Behavioural Therapy Group Programme? Clinical Psychology & Psychotherapy. 2009;16:485–496. doi: 10.1002/cpp.588. [DOI] [PubMed] [Google Scholar]
- Thomas PW, Thomas S, Hillier C, Galvin K, Baker R. Psychological interventions for multiple sclerosis. Cochrane Database of Systematic Reviews. 2006 doi: 10.1002/14651858.CD004431.pub2. CD004431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tshabalala J, Visser M. Developing a cognitive behavioural therapy model to assist women to deal with HIV and stigma. South African Journal of Psychology. 2011;41:17–28. [Google Scholar]
- Van't Hof E, Cuijpers P, Waheed W, Stein DJ. Psychological treatments for depression and anxiety disorders in Low- and middle-income countries: a meta-analysis. Afr J Psychiatry (Johannesbg) 2011;14:200–207. doi: 10.4314/ajpsy.v14i3.2. [DOI] [PubMed] [Google Scholar]
- Velez A, Ramsey K, Tell K. The Campaign to End Fistula: what have we learned? Findings of facility and community needs assessments. International Journal of Gynaecology and Obstetrics. 2007;99(Suppl 1):S143–150. doi: 10.1016/j.ijgo.2007.06.036. [DOI] [PubMed] [Google Scholar]
- Watt MH, Maman S, Jacobson M, Laiser J, John M. Missed opportunities for religious organizations to support people living with HIV/AIDS: Findings from Tanzania. AIDS Patient Care and STDS. 2009;23:389–394. doi: 10.1089/apc.2008.0195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Watt MH, Wilson SM, Joseph M, Masenga G, MacFarlane JC, Oneko O, Sikkema KJ. Religious coping among women with obstetric fistula in Tanzania. Glob Public Health. 2014;9:516–527. doi: 10.1080/17441692.2014.903988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weston K, Mutiso S, Mwangi JW, Qureshi Z, Beard J, Venkat P. Depression among women with obstetric fistula in Kenya. International Journal of Gynaecology and Obstetrics. 2011;115:31–33. doi: 10.1016/j.ijgo.2011.04.015. [DOI] [PubMed] [Google Scholar]
- Wilson SM, Sikkema KJ, Watt MH, Masenga G. Psychological Symptoms among Obstetric Fistula Patients Compared to Gynecology Outpatients in Tanzania. International Journal of Behavioral Medicine. 2015 doi: 10.1007/s12529-015-9466-2. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization . Obstetric fistula: Guiding principles of clinical management and programme development. WHO; Geneva: 2006a. [Google Scholar]
- World Health Organization . The World Health Report 2006 - working together for health. WHO; Geneva: 2006b. [Google Scholar]
- Yeakey MP, Chipeta E, Taulo F, Tsui AO. The lived experience of Malawian women with obstetric fistula. Culture, Health and Sexuality. 2009;11:499–513. doi: 10.1080/13691050902874777. [DOI] [PubMed] [Google Scholar]
- Zheng AX, Anderson FW. Obstetric fistula in low-income countries. International Journal of Gynaecology and Obstetrics. 2009;104:85–89. doi: 10.1016/j.ijgo.2008.09.011. [DOI] [PubMed] [Google Scholar]
- Zheng AX, Harrington AH, Love SA, Thelemaque LD, Anderson FW. Fistula awareness among sisters of women with fistula. International Journal of Gynaecology and Obstetrics. 2013;120:232–235. doi: 10.1016/j.ijgo.2012.09.019. [DOI] [PubMed] [Google Scholar]