Abstract
Background
Though gait evaluation is recommended as a core component of fall risk assessments, a systematic examination of the predictive validity of different modes of gait assessments for falls is lacking.
Objective
To compare three commonly employed gait assessments - self-reported walking difficulties, clinical evaluation, and quantitative gait - to predict incident falls.
Material and Methods
380 community-dwelling older adults (mean age 76.5±6.8 y, 55.8% female) were evaluated with three independent gait assessment modes: patient-centered, quantitative, and clinician-diagnosed. The association of these three gait assessment modes with incident falls was examined using Cox proportional hazards models.
Results
23.2% of participants self-reported walking difficulties, 15.5% had slow gait and 48.4% clinical gait abnormalities. 30.3% had abnormalities on only one assessment, whereas only 6.3% had abnormalities on all three. Over a mean follow-up of 24.2 months, 137 participants (36.1%) fell. Those with at least two abnormal gait assessments presented an increased risk of incident falls (HR: 1.61, 95% CI: 1.04-2.49) in comparison to the 169 participants without any abnormalities on any of the three assessments.
Conclusions
Multiple modes of gait evaluation provide a more comprehensive mobility assessment than only one assessment alone, and better identify incident falls in older adults.
Keywords: Gait disorders, clinical assessment, falls, aging
1. Introduction
The clinical examination has evolved over time building on collective clinical experience in disease and risk assessments, but a systematic assessment of its elements is lacking. Gait assessment is a core element of the clinical examination,(1) assisting diagnosis as well as predicting major adverse outcomes such as falls and disability.(2) Clinical guidelines to prevent falls in older adults from various national organizations and expert committees recommend gait assessment as a core element of fall risk screening in older adults, but do not provide guidance on which modes of assessment are optimal.(3-6) Methods employed in clinical practice and in research settings to identify gait disorders include eliciting self-report of mobility difficulties from patients, observation of walking patterns by clinicians, and quantitative gait assessments using instrumented methods.
Self-reported mobility difficulties are an independent predictor of functional impairment, (7) but accuracy depends on intrinsic factors such as visual impairment.(8) Furthermore, aging affects the accuracy of self-reported mobility difficulties in older adults due to cognitive impairment.(9) Clinical gait abnormalities identified by clinicians have been reported to be good predictors of adverse outcomes such as dementia,(10, 11) institutionalization,(12) or mortality.(12) However, the clinical gait assessment is less reliable than quantitative gait evaluation.(13) Quantitative assessment of gait is a strong predictor of cognitive decline,(14) disability (15) and mortality (16) in aging, and is recommended by experts and national organizations as a valid screening measure.(5, 6, 17) Clinical gait evaluations may be combined with quantitative assessments in individuals in order to take into account the intra-individual variability in gait performance.(18) In the specific context of falls, inclusion of self-reported mobility difficulties was reported to improve fall risk assessments. However, independent of abnormal results on other clinical assessments, such as quantitative assessments, self-reported mobility difficulties had a weaker association with falls.(19) Clinicians diagnosed neurologic gait abnormalities and slow gait also were reported to predict falls in older adults.(2, 20) Given the variability in methods used to assess gait function in clinical practice, it would be helpful to know the individual and combined predictive validity of different modes of gait assessment for identifying fall risk.
To address these knowledge gaps, we conducted a prospective study in a community residing cohort of non-demented older adults to compare the predictive validity for falls of three commonly employed, independent gait assessments: self-reported walking difficulties, clinical gait evaluation, and quantitative gait assessment. Identifying efficient methods of using single or combined gait assessment modes can help optimize current fall prediction and refine current clinical guidelines for fall risk assessment.
2. Material and Methods
2.1 Participants
Participants were recruited from the “Central Control of Mobility in Aging” study. The primary goal of the study is to determine clinical predictors of mobility decline and disability in aging.(21, 22) Participants seen in our research center between June 2011 and May 2014 were included in this analysis. Following a screening interview to rule out presence of dementia using two validated cognitive screeners, (23, 24) eligible individuals age 65 and older were scheduled for in-person visits at our research center. Participants received comprehensive neuropsychological, cognitive, psychological, and mobility assessments as well as a neurological examination including gait assessment. Exclusion criteria were: inability to speak English, unable to ambulate independently, dementia, significant loss of vision and/or hearing, and major psychiatric disorders. Informed consents were obtained and study protocols were approved by the local Institutional Review Board.
2.2 Gait assessment modalities
Gait was evaluated by three independent modes of assessments with previously described clinical utility for diagnosis of gait deficits and predicting various adverse outcomes in older patients.(2, 19, 20) Gait assessments included: self-report, clinical evaluation, and quantitative. Each gait assessment was conducted by independent clinicians, blinded to the results of the other two gait assessment methods. Patient centered assessment was based on response to: “Do you have any difficulty walking?” We have reported that this question has moderate reliability in identifying clinical and quantitative gait deficits in older adults.(25) Gait speed (cm/s) was measured while participants walked at their normal pace on an instrumented walkway (180×35.5×0.25 inches) without any attached devices (GAITRite, CIR systems, Havertown, PA). Excellent test-retest reliability has been reported for quantitative gait assessments at our center.(14) Slow gait was defined as one or more standard deviations (SD) below previously defined age and sex-appropriate mean values.(26) We have reported that slow gait predicted incident falls in another aging cohort.(20) While GAITRite provides information on several other gait variables that have been linked to fall risk,(20) we focused on speed for this report, as it is the most widely used gait metric and can be derived without the use of instrumented methods, increasing generalizability of our findings. Participants’ gaits were rated as normal or abnormal (due to neurological or non-neurological diseases) by study clinicians following visual inspection of gait patterns while they walked down a well-lit hallway, as previously described.(10) Our clinical gait classification has been reported to have good inter-rater reliability (kappa 0.8),(12) and neurological gait abnormalities identified by this method has been reported to predict falls in our previous study.(2)
2.3 Falls
Falls were defined as unintentionally coming down to the floor or lower level not due to a major intrinsic or extrinsic event. Subjects were interviewed at baseline and during their annual in-house visit about falls in the previous twelve months. Furthermore, every 2-3 months, the participants were contacted by telephone and asked if they had any falls since their last interview. The consistency between our telephone and in-house interview methods has been reported as highly reliable in a previous study.(27) To improve reliability, three participants diagnosed with dementia following their in-house assessment were excluded from this analysis.
2.4 Statistics
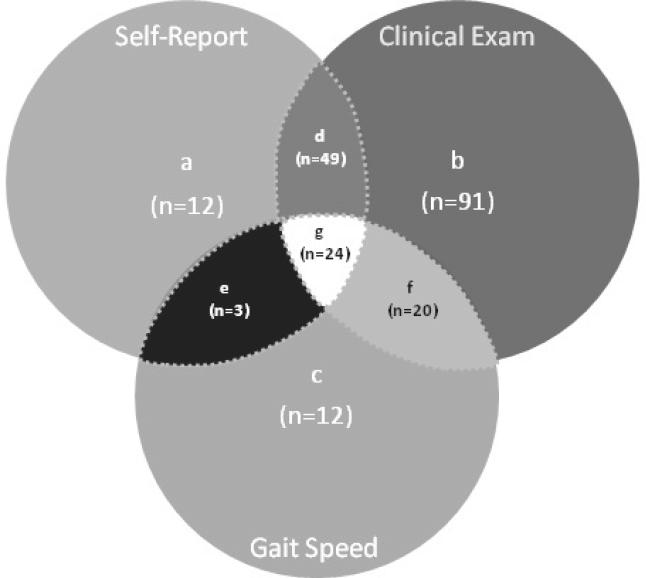
Participants were grouped based on presence of abnormalities on each assessments (Figure 1). Participant characteristics are described using mean and SD or otherwise appropriate values (Table 1). We used Cohen's kappa coefficient to describe the overall agreement between the three classification methods. Cox proportional hazards models were used to compute hazard ratios (HRs) with 95% confidence intervals to predict incident falls based on baseline groups, where we compared participants presenting only one abnormal gait assessment out of the three modes of assessment with those presenting two and three abnormal gait assessments. The 169 participants without abnormality on any of the three modes of gait assessment was the reference group. The models were adjusted for age, gender, education and presence of falls in the year prior to enrollment. Finally, we conducted sensitivity and specificity analyses of the various diagnostic groups for the identification of incident falls. All analyses were performed using SPSS version 20.
Figure 1. Distribution of participants.
Distribution of the study participants in a Venn diagram regarding to their positive answer to the self-reported walking difficulties (self-report), the presence of gait abnormalities during the neurological examination (clinical exam) and the presence of a slow gait velocity (gait speed). The healthy older adults group represents the participant, who did not report any walking difficulties, presented a normal clinical gait assessment and walked at normal gait velocity.
Table 1.
Clinical characteristics (n=380)
| Age (years) | 76.5 ± 6.8 |
| Female (%) | 212 (55.8) |
| Education (years) | 14.5 ±3.1 |
| Slow gaita, n (%) | 59 (15.5) |
| Self-reported walking difficulty, n (%) | 88 (23.2) |
| Clinical gait disorders, n (%) | 184 (48.4) |
| Only 1 abnormal gait features, n (%) | 115 (30.3) |
| Only 2 abnormal gait features, n (%) | 72 (19.0) |
| Only 3 abnormal gait features, n (%) | 24 (6.3) |
| Incident fallsb, n (%) | 137 (36.1) |
Only 1, 2, 3 abnormal gait features: only one, two or three feature(s) among slow gait, self-reported walking difficulty or clinical gait disorders;
Slow gait velocity is defined as one standard deviation or more below age and sex-appropriate mean values;
Any fall during the follow-up period.
3. Results
Clinical characteristics of the 380 non-demented older adults (mean age 76.5±6.8 y, 55.8% female) are summarized in Table 1.
The distribution of diagnostic groupings is illustrated in a Venn diagram (Figure 1). The largest group was the 91 participants that had only gait abnormalities on clinical examination (group b). The smallest group was the 3 participants with the combination of self-reported and quantitative abnormalities (group e).
The overall agreements between clinician assessment and self-report (kappa 0.3), and quantitative evaluation (kappa 0.2) were fair to poor. Agreement between self-report and quantitative evaluation (kappa 0.2) was poor. Of the 380 participants, 169 (44.5%) received normal diagnoses on all three assessments, 115 (30.3%) had abnormalities on only one, 72 (19.0%) on only two, and 24 (6.3%) on all three assessments.
Over a mean follow-up time of 24.2 ± 9.0 months (range: 0-38.2 months), 137 participants (36.1 %) reported an incident fall. Cox proportional hazards model (adjusted for age, gender, education and presence of fall in the past year) showed that participants with at least two abnormal gait assessments presented an increased risk of incident falls (HR: 1.61, 95% CI: 1.04-2.49) in comparison to the 169 participants without any abnormalities on the three modes of assessments, whereas the participants with only one abnormal gait assessment did not show any increased risk of incident falls (HR: 1.33, 95% CI: 0.88-2.01) (Table 2).
Table 2.
Abnormal gait assessments and incident falls (adjusted for age, gender, education and presence of fall in the previous year of enrollment)
| Assessments | N | Fallers (%) | HRs | 95% CI | P-value |
|---|---|---|---|---|---|
| Modes | |||||
| Reference Group* | 169 | 29.6 | |||
| Only one abnormal | 115 | 39.1 | 1.33 | 0.88-2.01 | 0.170 |
| Two or more abnormal | 96 | 43.8 | 1.61 | 1.04-2.49 | 0.032 |
Healthy older adults without any abnormal gait assessment.
Due to small sample size (n=24), the group with abnormalities on all three assessments was examined together with the group with two abnormalities. An unadjusted Cox model showed that the 24 participants with the three abnormal gait assessment had the highest HR for incident falls (HR: 1.93, 95% CI: 1.01-3.71, p =0.049); but this association was no longer significant after adjustments for age, gender, education and presence of fall in the past year.
Increasing the number of abnormal diagnoses on all three assessments from one to three improved the specificity from 72.1 to 95.0 % for identifying incident fallers. Conversely, increasing the requirement from abnormal diagnoses on only one mode to abnormalities on all three modes decreased sensitivity for identifying incident fallers (35.2 to 9.0 %).
4. Discussion
We investigated three independent and widely used approaches to assess gait in older adults. Each method has been independently shown to have value in diagnosing gait deficits and predicting incident falls in aging. However, to our knowledge, this is the first comparative study of these common gait assessment methods in the same prospective cohort.
Our findings indicate considerable variability in diagnosing gait abnormalities using the three modes. Abnormality on only one of the three gait assessments casts the widest net, identifying 30.3% of our sample as abnormal. On the other hand, abnormalities on all three assessments resulted in only 6.3% being classified as abnormal, indicating a considerable lack of overlap between these methods. The results illustrate that reliance on only one method risks failing to capture all participants with gait impairments. Of the 51.6% of participants who were considered normal by a clinician, some of them reported gait difficulties (7.7 %) and/or slow gait (7.7%). This discrepancy may result because the earliest stages of gait dysfunction are associated with subtle changes which may not be obvious to a clinician. Hodt-Billington et al showed that improvement in self-reported gait functioning preceded quantitative gait improvements following hip replacement in 34 patients with hip osteoarthritis.(28) This observation highlights the different facets captured by the three gait assessments; self-report was linked to pain, whereas quantitative gait was associated with recovery.
In clinical practice, identification of older adults with gait disorders constitutes a key element of patient evaluation. Quantitative gait assessment during single tasking(20) and dual tasking(29) has been related independently with incident falls, like clinical gait abnormalities in healthy older adults.(2) The combined clinical gait assessment represents an inexpensive and simple approach with high specificity for incident falls. The comprehensive assessment proposed in this report could be implemented without major resource or time commitments in clinical practice by adding a single question about walking abilities and timing gait over a fixed distance to the standard gait evaluation done by clinicians. While currently not widely used in clinical settings due to mainly resource constraints, highly reliable laboratory based techniques such as footswitches,(30) instrumented walkways,(31) or three dimensional gait analysis (32) that provide a more detailed assessment of gait, may further improve validity of risk stratification in the future.
The low sensitivity and high specificity of this combined gait assessment approach emphasizes its ability to identify patients at the highest risk, who could be targeted for preventive interventions. Several caveats need to be considered while evaluating our specificity and sensitivity results that were primarily done to compare the concurrent validity of the three gait assessments. We studied relatively healthy volunteers, and a higher fall rate will be seen in clinic populations with higher disease burden. Not all diseases or disease stages are associated with gait impairments in older adults. Falls are multifactorial, and may result from mechanisms that are unrelated to gait and balance. Finally, gait is only one aspect of the clinical assessment, and clinicians will utilize the overall examination to diagnose diseases and to assess falls risk in older adults.
Strengths of this study include the use highly reliable and valid methods.(10) While we used quantitative methods, gait speed can also be easily measured over a fixed distance with a stopwatch in clinical settings. A longer follow-up period and an increased sample size would allow us to assess if participants with three abnormal assessments would be at higher risk of falling than participants with only two abnormal tests after adjusting for confounders. We lacked power to examine predictive validity of individual diagnostic groups (Figure 1) due to small sample sizes in these subgroups, and these associations will be explored in future studies.
5. Conclusions
The findings suggest that in addition to observing gait patterns during standard clinical examinations, physicians should also ask patients to report mobility difficulties as well as measure gait velocity to improve the utility of the clinical examination and the identification of patients at high risk of falling. These quick and easy additions to the clinical evaluation could contribute to focus on appropriate interventions in older adults at higher risk of falling.
Highlights.
- Clinical gait abnormalities are noticed in 48.4% of non-demented older adults.
- 6.3% of older adults present abnormalities in the 3 modes of gait assessments.
- Participants with 2 abnormal gait assessments presented an increased risk of falls.
- Combining different modes of gait assessments improves potential faller detection.
ACKNOWLEGMENTS
We thank all of the CCMA study clinicians and research students for their assistance with data collection and Jeannette R. Mahoney for her technical support.
Financial Support: This study was supported by funds from the National Institutes of Health, National Institute on Aging (R01AG036921-01A1: R Holtzer & R01AG044007-01A1: J Verghese). G Allali is supported by a grant from the Geneva University Hospitals and the Resnick Gerontology Center, Albert Einstein College of Medicine, Yeshiva University. The funding sources have no role in the study design; in the collection, analysis and interpretation of data; in the writing of the report; and in the decision to submit the article for publication.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflict of interest: The authors declare that they have no conflict of interest.
References
- 1.Snijders AH, van de Warrenburg BP, Giladi N, Bloem BR. Neurological gait disorders in elderly people: clinical approach and classification. Lancet neurology. 2007;6(1):63–74. doi: 10.1016/S1474-4422(06)70678-0. [DOI] [PubMed] [Google Scholar]
- 2.Verghese J, Ambrose AF, Lipton RB, Wang C. Neurological gait abnormalities and risk of falls in older adults. Journal of neurology. 2010;257(3):392–8. doi: 10.1007/s00415-009-5332-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Panel on Prevention of Falls in Older Persons AGS, British Geriatrics S Summary of the Updated American Geriatrics Society/British Geriatrics Society clinical practice guideline for prevention of falls in older persons. Journal of the American Geriatrics Society. 2011;59(1):148–57. doi: 10.1111/j.1532-5415.2010.03234.x. [DOI] [PubMed] [Google Scholar]
- 4.Lamb SE, Jorstad-Stein EC, Hauer K, Becker C. Prevention of Falls Network E, Outcomes Consensus G. Development of a common outcome data set for fall injury prevention trials: the Prevention of Falls Network Europe consensus. Journal of the American Geriatrics Society. 2005;53(9):1618–22. doi: 10.1111/j.1532-5415.2005.53455.x. [DOI] [PubMed] [Google Scholar]
- 5.National Institute for Clinical Excellence [October 31, 2014];The assessment and prevention of falls in older people. http://www.nice.org.uk/CG021.
- 6.Australian Commission on Safety and Quality in Health Care [October 31, 2014];Falls Prevention. http://www.safetyandquality.gov.au/our-work/falls-prevention.
- 7.Leskinen R, Laatikainen T, Peltonen M, Levalahti E, Antikainen R. Prevalence, predictors and covariates of functional status impairment among Finnish Second World War veterans during 1992-2004. Age and ageing. 2013;42(4):508–14. doi: 10.1093/ageing/aft051. [DOI] [PubMed] [Google Scholar]
- 8.Swenor BK, Bandeen-Roche K, Munoz B, West SK. Does walking speed mediate the association between visual impairment and self-report of mobility disability? The Salisbury Eye Evaluation Study. Journal of the American Geriatrics Society. 2014;62(8):1540–5. doi: 10.1111/jgs.12937. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Abraham P, Ouedraogo N, Tew GA, Vielle B, Leftheriotis G, Mahe G. Aging reduces the accuracy of self-reported walking limitation in patients with vascular-type claudication. Journal of vascular surgery. 2012;56(4):1025–31. doi: 10.1016/j.jvs.2012.03.258. [DOI] [PubMed] [Google Scholar]
- 10.Verghese J, Lipton RB, Hall CB, Kuslansky G, Katz MJ, Buschke H. Abnormality of gait as a predictor of non-Alzheimer's dementia. The New England journal of medicine. 2002;347(22):1761–8. doi: 10.1056/NEJMoa020441. [DOI] [PubMed] [Google Scholar]
- 11.Verghese J, Derby C, Katz MJ, Lipton RB. High risk neurological gait syndrome and vascular dementia. Journal of neural transmission. 2007;114(10):1249–52. doi: 10.1007/s00702-007-0762-0. [DOI] [PubMed] [Google Scholar]
- 12.Verghese J, LeValley A, Hall CB, Katz MJ, Ambrose AF, Lipton RB. Epidemiology of gait disorders in community-residing older adults. Journal of the American Geriatrics Society. 2006;54(2):255–61. doi: 10.1111/j.1532-5415.2005.00580.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Mera TO, Filipkowski DE, Riley DE, Whitney CM, Walter BL, Gunzler SA, et al. Quantitative analysis of gait and balance response to deep brain stimulation in Parkinson's disease. Gait & posture. 2013;38(1):109–14. doi: 10.1016/j.gaitpost.2012.10.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Verghese J, Wang C, Lipton RB, Holtzer R, Xue X. Quantitative gait dysfunction and risk of cognitive decline and dementia. Journal of neurology, neurosurgery, and psychiatry. 2007;78(9):929–35. doi: 10.1136/jnnp.2006.106914. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Cesari M, Kritchevsky SB, Penninx BW, Nicklas BJ, Simonsick EM, Newman AB, et al. Prognostic value of usual gait speed in well-functioning older people--results from the Health, Aging and Body Composition Study. Journal of the American Geriatrics Society. 2005;53(10):1675–80. doi: 10.1111/j.1532-5415.2005.53501.x. [DOI] [PubMed] [Google Scholar]
- 16.Studenski S, Perera S, Patel K, Rosano C, Faulkner K, Inzitari M, et al. Gait speed and survival in older adults. JAMA : the journal of the American Medical Association. 2011;305(1):50–8. doi: 10.1001/jama.2010.1923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Guideline for the prevention of falls in older persons. American Geriatrics Society, British Geriatrics Society, and American Academy of Orthopaedic Surgeons Panel on Falls Prevention. Journal of the American Geriatrics Society. 2001;49(5):664–72. [PubMed] [Google Scholar]
- 18.van Iersel MB, Munneke M, Esselink RA, Benraad CE, Olde Rikkert MG. Gait velocity and the Timed-Up-and-Go test were sensitive to changes in mobility in frail elderly patients. Journal of clinical epidemiology. 2008;61(2):186–91. doi: 10.1016/j.jclinepi.2007.04.016. [DOI] [PubMed] [Google Scholar]
- 19.Simonsick EM, Newman AB, Visser M, Goodpaster B, Kritchevsky SB, Rubin S, et al. Mobility limitation in self-described well-functioning older adults: importance of endurance walk testing. The journals of gerontology Series A, Biological sciences and medical sciences. 2008;63(8):841–7. doi: 10.1093/gerona/63.8.841. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Verghese J, Holtzer R, Lipton RB, Wang C. Quantitative gait markers and incident fall risk in older adults. The journals of gerontology Series A, Biological sciences and medical sciences. 2009;64(8):896–901. doi: 10.1093/gerona/glp033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Holtzer R, Mahoney J, Verghese J. Intraindividual variability in executive functions but not speed of processing or conflict resolution predicts performance differences in gait speed in older adults. The journals of gerontology Series A, Biological sciences and medical sciences. 2014;69(8):980–6. doi: 10.1093/gerona/glt180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Holtzer R, Wang C, Verghese J. Performance variance on walking while talking tasks: theory, findings, and clinical implications. Age. 2014;36(1):373–81. doi: 10.1007/s11357-013-9570-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Lipton RB, Katz MJ, Kuslansky G, Sliwinski MJ, Stewart WF, Verghese J, et al. Screening for dementia by telephone using the memory impairment screen. Journal of the American Geriatrics Society. 2003;51(10):1382–90. doi: 10.1046/j.1532-5415.2003.51455.x. [DOI] [PubMed] [Google Scholar]
- 24.Galvin JE, Roe CM, Powlishta KK, Coats MA, Muich SJ, Grant E, et al. The AD8: a brief informant interview to detect dementia. Neurology. 2005;65(4):559–64. doi: 10.1212/01.wnl.0000172958.95282.2a. [DOI] [PubMed] [Google Scholar]
- 25.Verghese J, Katz MJ, Derby CA, Kuslansky G, Hall CB, Lipton RB. Reliability and validity of a telephone-based mobility assessment questionnaire. Age and ageing. 2004;33(6):628–32. doi: 10.1093/ageing/afh210. [DOI] [PubMed] [Google Scholar]
- 26.Verghese J, Annweiler C, Ayers E, Barzilai N, Beauchet O, Bennett DA, et al. Motoric cognitive risk syndrome: Multicountry prevalence and dementia risk. Neurology. 2014;83(8):718–26. doi: 10.1212/WNL.0000000000000717. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Verghese J, Buschke H, Viola L, Katz M, Hall C, Kuslansky G, et al. Validity of divided attention tasks in predicting falls in older individuals: a preliminary study. Journal of the American Geriatrics Society. 2002;50(9):1572–6. doi: 10.1046/j.1532-5415.2002.50415.x. [DOI] [PubMed] [Google Scholar]
- 28.Hodt-Billington C, Helbostad JL, Vervaat W, Rognsvag T, Moe-Nilssen R. Changes in gait symmetry, gait velocity and self-reported function following total hip replacement. Journal of rehabilitation medicine : official journal of the UEMS European Board of Physical and Rehabilitation Medicine. 2011;43(9):787–93. doi: 10.2340/16501977-0849. [DOI] [PubMed] [Google Scholar]
- 29.Ayers EI, Tow AC, Holtzer R, Verghese J. Walking while talking and falls in aging. Gerontology. 2014;60(2):108–13. doi: 10.1159/000355119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Beauchet O, Herrmann FR, Grandjean R, Dubost V, Allali G. Concurrent validity of SMTEC footswitches system for the measurement of temporal gait parameters. Gait & posture. 2008;27(1):156–9. doi: 10.1016/j.gaitpost.2006.12.017. [DOI] [PubMed] [Google Scholar]
- 31.McDonough AL, Batavia M, Chen FC, Kwon S, Ziai J. The validity and reliability of the GAITRite system's measurements: A preliminary evaluation. Archives of physical medicine and rehabilitation. 2001;82(3):419–25. doi: 10.1053/apmr.2001.19778. [DOI] [PubMed] [Google Scholar]
- 32.Meldrum D, Shouldice C, Conroy R, Jones K, Forward M. Test-retest reliability of three dimensional gait analysis: including a novel approach to visualising agreement of gait cycle waveforms with Bland and Altman plots. Gait & posture. 2014;39(1):265–71. doi: 10.1016/j.gaitpost.2013.07.130. [DOI] [PubMed] [Google Scholar]