Abstract
We examine how families influence mental health service (MHS) utilization among African Americans by drawing on the concept of family ambivalence, which encompasses both family support and stress, and by placing utilization within the context of family histories of psychiatric disorder and treatment. Data are from the 2001–2003 National Survey of American Life, a nationally representative sample of African American adults (n = 3,149), including a clinical need subsample (n = 605) of respondents with a disorder. Negative family interactions have indirect positive effects on use of any MHS through need for care, whereas family social support lacks any effect. Although poor self-rated mental health (SRMH) is associated with greater utilization of any and specialty MHS given family histories of no disorder or treated disorder, utilization is low given a family history of untreated disorder, irrespective of SRMH. Screening for family histories of psychiatric disorder in primary care is recommended.
Keywords: African Americans, disparities, family, mental health need, mental health services
Effective treatments exist for many mental disorders, but less than half of persons who have a mental disorder, an indicator of need for mental health services (MHS), receive any treatment (Wang et al. 2005). This underutilization is more pronounced among African Americans than non-Hispanic whites (e.g., Harris, Edlund, and Larson 2005; Wang et al. 2005).1 Although African Americans have similar or lower prevalence rates for many disorders than non-Hispanic whites (e.g., Breslau et al. 2006; Williams et al. 2007), treatment disparities typically persist when differences in prevalence are controlled (e.g., Alegría et al. 2002; Harris et al. 2005). Moreover, African Americans have relatively high rates of disorders that carry substantial need for treatment including severe, disabling, persistent, and chronic disorders (e.g., Breslau et al. 2005; Williams et al. 2007; for an exception, see Harris et al. 2005). Therefore, it is of great consequence to identify sources of underutilization of MHS within this population.
Several qualitative studies identify the family as a key influence on MHS use among African Americans, facilitating treatment by making recommendations to seek help, for instance, or inhibiting utilization by expressing negative attitudes about treatment (e.g., Hines-Martin, Brown-Martin, et al. 2003; Hines-Martin, Malone, et al. 2003; Lindsey, Joe, and Nebbitt 2010). Although suggestive, these studies do not assess the determinants of utilization because only persons who have used services are studied and select convenience samples limit generalizability. Surveys of large national probability samples of African Americans address these limitations and point to the crucial role played by family, demonstrating relationships such as the inverse association between family closeness and the exclusive use of professional services (Woodward et al. 2008). However, these studies typically: (1) examine one aspect of family functioning, usually social support, but neglect other aspects such as stress, potentially exaggerating the role of social support; (2) misinterpret direct effects of family functioning as if they were total effects, which may understate its full role; and/or (3) implicitly assume that family effects are uniform throughout the population, a problematic assumption because families differ in their prior experience with psychiatric disorder and treatment. The current study provides a more complete view of the impact of family functioning on MHS utilization among African Americans by comparing the effects of social support and stress, including their indirect effects via need for services, and by testing whether these connections are contingent upon family history of psychiatric disorder and treatment.
BACKGROUND
The Role of Family Functioning in MHS Utilization
Pescosolido and Boyer (2010:432) describe help seeking for mental health problems as being “as much a process of social influence as it is a result of individual action.” These social influences range from suggestions to persuasion and coercion, with many people “muddling” through, neither actively resisting nor accepting recommendations from social network members (Pescosolido, Gardner, and Lubell 1998), although family and friends also may normalize signs and symptoms of mental disorder and delay or oppose treatment (Clausen and Yarrow 1955). As a case in point, family members rarely identified MHS as a possible resource early in the help-seeking process of African Americans entering treatment in the public sector, even though patients reported that family members were able to recognize changes in their behaviors as mental health problems (Hines-Martin, Brown-Piper, et al. 2003). When family did recommend treatment, however, it facilitated obtaining treatment, especially when family members had prior positive experiences with treatment (Hines-Martin, Brown-Piper, et al. 2003).
Research on social network influences in general and the family in particular has focused most often on one aspect of these relationships: social support. Thoits (2011a, 2011b) maintains that social support obviates the need for care because it benefits mental health directly and buffers the mental health effects of exposure to stressors. According to Thoits’ (1985, 2011b) self-labeling theory, individuals recognize that something is wrong with them when their emotional reactions to stressful situations are inappropriate—too intense, recurrent, or prolonged—and this self-labeling leads to seeking help from important members of their social networks. When support is forthcoming and effective, symptoms decline and people are less likely to think they need help from professionals (Thoits 2011b). In this manner, social support functions as a substitute for formal care. However, when support is lacking, symptoms may persist or worsen, leading people to seek professional care (Thoits 2011b). These considerations imply that some or all of the effect of family social support on utilization is indirect and is transmitted through better mental health, that is, reduced need.
A recent study validates the supposition that family support sometimes substitutes for formal services among African Americans insofar as frequent contact with family was associated with using informal support as the sole source of help (Woodward et al. 2008). Frequent contact was also associated with using both informal and formal sources of help, suggesting that family support also complements formal services. However, the study examined these relationships only among those with diagnostically evaluated need and therefore did not address potential indirect effects of support on utilization through need.
In contrast to social support, the consequences of problematic family relationships have been neglected, especially the possibility that negative family interactions act as social stressors that generate disorder (Wheaton et al. 2013) and thereby lead to utilization of MHS. August, Rook, and Newsom (2007) characterize these negative social interactions—including insensitivity, criticism, and excessive demands—as being among the most distressing stressors people experience on an everyday basis. Thus, the beneficial effects of supportive social ties on mental health may be offset by negative social interactions, which often occur with the same network members (August et al. 2007; Lincoln, Taylor, and Chatters 2003; Rook 1998).
Lincoln and associates (2012) invoke the concept of ambivalence—the coexistence of negative and positive feelings toward the same person—to explain why contradictions like the co-occurrence of support and stress are built into the nature of families. They link ambivalence among African Americans to strong family identification and social networks that are largely comprised of blood and fictive kin2 and to: (1) heavy reliance on these networks for instrumental and tangible aid, which can create conflict if assistance is frequently sought; (2) violations of reciprocity norms if someone is unable to give in return; and (3) extended and multigenerational family structures that may present conflicting norms. The investigators find that African Americans report more emotional support than negative interactions but that some report high levels of both. Therefore, drawing on the concept of family ambivalence, we examine each of these aspects of family functioning on utilization.
There is some evidence that stressful family relationships may be more important than supportive ones for MHS use among African Americans. Among depressed blacks, problematic relationships with relatives and friends were found to be the only aspect of social relationships associated with treatment seeking, an association not present for whites (Sussman, Robins, and Earls 1987). More recently, Abe-Kim, Takeuchi, and Hwang (2002) reported that family conflict is predictive of MHS utilization for Chinese Americans, whereas supportive ties are not. While noting that harmonious family relationships are highly valued among this population, the investigators conclude that the effect of family conflict on utilization is unlikely to be unique to this population. Given the centrality of family to African Americans just described, problematic family relationships may result in higher utilization regardless of any influence of family support. These considerations lead to the following:
Hypothesis 1: Family support has a negative association with MHS utilization that is mediated at least in part by diminished need for services.
Hypothesis 2: Family stress has a positive association with MHS utilization that is mediated at least in part by increased need for services.
Family Histories of Psychiatric Disorder and Treatment
Treatment for psychiatric disorders appears to cluster in families, at least in part because disorders aggregate in families as a result of genetic and shared environmental factors. Schor and colleagues (1987) found that family members resemble one another in their utilization of medical services for psychological problems.3 Also, having depressed relatives is positively associated with treatment seeking for depression (Kendler 1995). Treatment among depressed persons, especially outpatient treatment and psychotropic medication, is substantially greater when there is a family history of depression than when there is not (Prokofyeva et al. 2013). Moreover, having a family member or friend who has used MHS in the past makes it more likely that someone who is symptomatic will seek and receive treatment (Yokopenic, Clark, and Aneshensel 1983).
The influence of having a family history of treatment on MHS utilization seems to represent the confluence of several social psychological processes. Family histories of treatment may facilitate other relatives’ entry into treatment through greater awareness of depressive symptoms and knowledge about seeking and obtaining treatment, which Prokofyeva and colleagues (2013) identify as a form of “family mental health literacy.” Schor and associates (1987) maintain that families establish patterns of health behaviors, including service use, based on a shared environment and belief system. Relatives who have used services in the past appear to communicate social norms that are perceived by others as being favorable toward treatment, including expectations that significant others would approve of one seeking help for a personal problem and would seek help themselves for similar problems (Vogel et al. 2007). Persons who have relatives who have had psychiatric disorders also may use MHS as a means of prevention even in the absence of mental health problems (i.e., the worried well). Thus, family histories of treated disorders may increase an individual’s insight into and responsiveness to their own mental health problems.
However, the role of family histories of untreated psychiatric disorder has been overlooked. Families with untreated disorder histories have role models for the nonuse of formal services, which may communicate unfavorable social norms regarding treatment, even if that is not the intended message, and lack experience in accessing treatment. Relatives also may hold stigmatized attitudes toward treatment and, therefore, actively discourage other relatives from seeking formal help. In this manner, family members with mental health problems may come to believe that professional intervention is not an appropriate or effective solution to their problems. As a result, family history of untreated disorder may be one means through which low utilization of MHS among African Americans is perpetuated.
In the absence of a known family history of psychiatric disorder, relatives lack experience with responding to the occurrence of mental illness within the boundaries of their families, which may interfere with recognizing signs and symptoms among their relatives and reduce their ability to facilitate access to care. In this scenario, the family’s reaction to the emergence of mental illness is not filtered by past experiences and may lead to attitudes and beliefs about treatment that are similar to the average views of the African American population overall, in contrast to families with histories of treated or untreated disorder, which may hold views that are more and less favorable than average, respectively. These considerations lead to the following:
Hypothesis 3: Compared to a family history of untreated disorder, having a known history of treated disorder: (a) amplifies the impact of family stress on utilization—because it fosters the belief that treatment is a valid means of coping with problems; (b) dampens the effect of family support—because treatment is seen as a legitimate source of help; and (c) intensifies the effect of need—because the affected individual and/or relatives are able to recognize that something is wrong that requires intervention and know how to access care.
DATA AND METHODS
Sample and Data Collection
The National Survey of American Life was conducted with a national household probability sample of African American (N = 3,570), non-Hispanic white (N = 891), and Afro-Caribbean (N = 1,438) adults 18 years of age and older residing in the contiguous United States. A four-stage area probability sampling design was used: U.S. Metropolitan Statistical Areas and counties, area segments, housing units, and respondents within housing units (Heeringa et al. 2004). The current study is restricted to the African American subsample (response rate 70.7 percent) and excludes Afro-Caribbeans because of physical distance from relatives and non-Latino whites because they were sampled from high-density African American areas. After dropping respondents with missing data or no family (n = 19), the analytic sample size is 3,149. A clinical need subsample (n = 605) consists of respondents meeting past-year diagnostic criteria for one or more mood, anxiety, or substance use disorders (see the following). The analysis of the full sample permitted assessment of the indirect effects of family functioning on utilization through need— which has been overlooked in previous research— while the clinical need subsample is informative about those who most need treatment, in keeping with previous research. Although family functioning characteristics may not play a direct role in formal help-seeking beyond affecting need, family history of disorder and treatment is thought to influence utilization among persons with need through awareness of and responsiveness to mental health problems.
Most respondents were interviewed face to face (others by telephone) using a computer-assisted structured questionnaire. Psychiatric disorder was assessed with the World Health Organization version of the Composite International Diagnostic Interview (WHO-CIDI) (Williams et al. 2007). The survey also collected information relevant to this study on self-rated mental health, MHS utilization, family characteristics and functioning, and socioeconomic and demographic characteristics. Data collection occurred between February 2001 and June 2003.
Measures
Service Utilization
The dependent variables of MHS utilization are defined as making at least one visit within the 12 months preceding the interview with a provider specifically for “problems with emotions, mental health, or use of alcohol or drugs” and/or positive responses to separate questions about self-help and support groups. Specialty MHS use is scored 1 if the respondent saw a psychiatrist, psychologist, social worker, counselor, other mental health professional (e.g., psychotherapist), and/ or used a mental health hotline; else = 0. General medical service use is scored 1 if the respondent reported seeing a medical doctor (e.g., general practitioner), nurse, occupational therapist, or other health professional; else = 0. Any MHS use combines specialty and medical services with religious or spiritual advisors, online support groups, self-help groups, and any other healer (e.g., herbalist).
We examine medical services and specialty MHS separately because some, although not all, studies find that African Americans are more likely than non-Hispanic whites to use medical services for mental health treatment and less likely to use specialty MHS (e.g., Alegría et al. 2002; Snowden 2001; Snowden and Pingitore 2002). Their use of medical services versus specialty MHS for mental health treatment is problematic because African Americans are less likely to receive minimally adequate mental health care in the medical sector than the specialty sector (Neighbors et al. 2007).
Family Functioning and History
Consistent with existing research, we examine family social support using three measures. First, the family social support scale is comprised of three items asking how often relatives: “make you feel loved and cared for,” “listen to you talk about your private problems and concerns,” and “express interest and concern in your well-being,” with response codes ranging 1 = never to 4 = very often. Summated scores range from 3 to 12 with good reliability (α = .73). Second, family helpfulness is a single item, “How often do people in your family help you?” with responses of 1 = never to 4 = very often. Finally, a parallel measure of fictive kin helpfulness is also used (along with an indicator of having no fictive kin). In addition to family social support, we operationalize family stress with a three-item scale tapping negative interactions with family members. The questions asked how often relatives: “make too many demands on you?”; “criticize you and the things you do?”; and “try to take advantage of you?” Responses range from 1 = never to 4 = very often. Summated scores range from 3 to 12 with good reliability (α = .74).
Family history of psychiatric disorder/treatment is based on questions asking whether any parents, siblings, or children (over age 13) had ever had “problems” with symptoms of depression, mania, panic attack, phobias, drug and alcohol use disorders, and/or schizophrenia. Those responding affirmatively were then asked if professional treatment was received. Three mutually exclusive histories are distinguished: no history of psychiatric disorder (the mode and referent), untreated disorder only, and any treated disorder.4
Need for Services
Diagnostically evaluated need for MHS was assessed with the WHO-CIDI, using research-based diagnostic criteria from the Diagnostic and Statistical Manual of Mental Health Disorders, Fourth Edition (DSM-IV) (American Psychiatric Association 2000). Diagnostic status is scored as 1 if the respondent meets diagnostic criteria for any past year mood (depression, dysthymia, or bipolar disorder; 6.6 percent), anxiety (panic attack, posttraumatic stress disorder, social phobia, agoraphobia, or generalized anxiety disorder; 14.7 percent), or substance use (alcohol/drug abuse or dependence; 2.8 percent) disorder; 0 = none of these disorders. The prevalence of these disorders is substantially higher among the clinical need subsample (see appendix), which consists of persons that meet criteria for one or more disorders. Equating need with diagnosis is imperfect because some disorders are mild, non-disabling, and self-limiting; by contrast some persons without a diagnosable disorder still have substantial disability (Mechanic 2003).5 Nevertheless, diagnosis is the most common operationalization of need, and its use is substantiated with the current data: compared to those without a diagnosis, the clinical need subsample has significantly (p < .001) poorer self-rated mental health, more suicide attempts and ideation, and more mentally unhealthy days. For the clinical need subsample, the past year number of disorders is used as a measure of severity; although the mode is one disorder (43.7 percent), the majority has two or more disorders (see appendix). We also use the person’s subjective appraisal measured as self-rated mental health (SRMH) with 1 = excellent through 5 = poor. The overall mode is very good (35.5 percent) compared to good (29.3 percent) among the clinical need subsample.
Control Variables
Standard survey measures were used to assess demographic and socioeconomic characteristics, including: age scored in years, gender (0 = female, 1 = male), education in years, poverty index—an income to needs ratio of household income divided by the poverty threshold (Proctor and Dalaker 2002), and employment status (three categories: employed—reference group, unemployed, and not in labor force). Two indicators of social resources are also controlled: marital status (three categories: married/cohabiting—reference group; previously married—divorced, separated, or widowed; and never married) and whether the person lives alone = 1, else = 0. Insurance status is categorized as follows: uninsured—omitted reference, insured with mental health coverage, and insured with no or unknown mental health coverage.
Analysis
Sample design variables and weights developed by Heeringa and colleagues (2004) were used in all models to correct for stratification, clustering, unequal selection probabilities, and nonresponse. The STATA SE 12 survey procedures were used to calculate descriptive statistics and estimate logistic regression models (StataCorp 2011). Wald tests with Bonferroni correction for multiple comparisons were performed for comparisons between the clinical need subsample and the remainder of the sample.
A sequential series of logistic regression models were tested for each utilization dependent variable: (A) a restricted model that contained the set of family functioning variables along with the control variables; (B) a full model that added diagnostic status, SRMH, and family history; and (C) a set of conditional models separately tested the interaction of family history with (1) support, (2) stress, (3) diagnostic status, and (4) SRMH. Continuous measures were mean-deviated. Product interaction terms were tested as a set by comparing the conditional and full models using a Wald test.
We subsequently tested the hypothesized mediation of family functioning through need using a probit model following MacKinnon’s (2008) recommendations for the case of a dichotomous mediator (diagnostic status) and a dichotomous outcome (MHS utilization). The logistic regression results indicated potential mediation only for negative family interactions for any MHS (total sample) and also pointed to possible moderation of the mediated effect. Therefore, we tested whether (1) diagnostic status mediates the effect of negative interactions on use, (2) SRMH mediates the effects of diagnostic status and negative interactions on use, and (3) family history moderates the effects of SRMH on use. The model was estimated using Mplus 6.1 with weighted least squares estimation.
RESULTS
Sample and Clinical Need Subsample Characteristics
As shown in Table 1, participants are middle aged, on average, and there are considerably more women than men. Three out of four participants have at least a high school education, and two out of three are employed. The mean poverty index indicates low income on average. The married/cohabiting comprise a plurality, but one in four is previously married and one in three is never married. The majority has health insurance and 59.8 percent know they have mental health coverage. Most have employer-sponsored insurance (59.6 percent), followed by public insurance (e.g., Medicaid; 31.9 percent) and/ or private insurance (8.9 percent; not mutually exclusive and not shown).
Table 1.
Sample Distribution of Socioeconomic and Demographic Characteristics by Diagnostic Status: African American Adults, 2001–2003, NSAL (Weighted).
| Total |
Diagnosis Status, Past Yeara |
||
|---|---|---|---|
| (N = 3,149) |
Positive (N = 2,544) |
Negative (N = 605) |
|
| Mean/(SD) or Percentag | Mean/(SD) or Percentage | Mean/(SD) or Percentage | |
| Age (years) | 41.59 (17.82) | 42.22 (18.16) | 38.82 (15.77) |
| F(1, 34) = 32.07*** | |||
| Male | 43.7 | 46.1 | 33.0 F(1, 34) = 24.43*** |
| Marital status | |||
| Married/cohabiting | 42.3 | 44.0 | 34.8 |
| Previously married | 26.0 | 25.0 | 30.6 |
| Never married | 31.7 | 31.0 | 34.6 F(2, 33) = 8.24** |
| Lives alone (/no) | 20.0 | 20.0 | 19.4 F(1, 34) = 0.12 |
| Employment status | |||
| Employed | 68.0 | 69.3 | 62.6 |
| Unemployed | 10.2 | 9.0 | 15.3 |
| Not in labor force | 21.8 | 21.7 | 22.1 F(2, 33) = 7.67** |
| Years of Education | |||
| Less than 12 years | 23.5 | 22.3 | 29.1 |
| 12 years | 37.8 | 38.2 | 36.0 |
| 13–15 years | 24.3 | 24.5 | 23.1 |
| 16+ years | 14.4 | 15.0 | 11.7 F(3, 32) = 4.70** |
| Poverty Index | 2.68 (2.72) | 2.76 (2.69) | 2.30 (2.84) F(1, 34) = 8.70** |
| Uninsured | 17.8 | 16.6 | 23.4 F(2, 33) = 4.71* |
| Family support (3 = low to 12 = high) | 9.74 (2.40) | 9.83 (2.29) | 9.34 (2.80) |
| F(1, 34) = 10.58** | |||
| Negative family interactions (3 = low to 12 = high) | 5.53 (2.57) | 5.33 (2.44) | 6.42 (2.89) F(1, 34) = 79.56*** |
| Family helpfulness (1 = never to 4 = very often) | 2.74 (1.20) | 2.73 (1.20) | 2.77 (1.19) F(1, 34) = 0.49 |
| Fictive kin helpfulness (1 = never to 4 = very often) | 2.35 (1.37) | 2.33 (1.35) | 2.40 (1.46) F(1, 34) = 1.13 |
| No fictive kin | 8.7 | 8.4 | 10.3 F(1, 34) = 1.76 |
| Family history of disorder/t | |||
| No disorder | 46.3 | 50.2 | 29.2 |
| Untreated disorder only | 24.8 | 23.9 | 28.9 |
| Any treated disorder | 28.9 | 25.9 | 41.9 F(2, 33) = 29.76*** |
| Self-rated mental health (1 = excellent to 5 = poor) | 2.13 (1.12) | 2.02 (1.04) | 2.67 (1.27) F(1, 34) = 168.04*** |
| Past year service utilization | |||
| Any mental health service (/no) | 9.8 | 4.9 | 31.1 F(1, 34) = 100.49*** |
| Specialty mental health services (/no) | 4.3 | 1.6 | 16.2 F(1, 34) = 53.72*** |
| General medical services (/no) | 5.2 | 2.6 | 16.7 F(1, 34) = 43.66*** |
Note: NSAL = National Survey of American Life.
Met DSM-IV diagnostic criteria for one or more mood, anxiety, or substance use disorders in the past 12 months.
p < .05,
p < .01,
p < .001, Wald tests for differences by diagnostic status.
Those who meet criteria for a psychiatric diagnosis are younger and more likely to be female than those who do not meet criteria. The diagnostic groups differ significantly on marital status, with more married/cohabiting persons among those without a disorder, and more previously married and never married persons among those with a disorder. Employment status differs by diagnostic status too, with more employed persons among those without a diagnosis and more unemployed persons among persons with a diagnosis. The two groups differ significantly on education and insurance status, with the clinical need subsample less likely than others to have at least a high school education or health insurance.
Overall, family support is high and negative family interactions are low among this sample of African Americans; however, those in the clinical need subsample have lower support and higher negative interaction scores, on average, than the remainder of the sample. Levels of family and fic-tive kin helpfulness are moderate irrespective of diagnostic status. Stark differences in family history of disorder and treatment are seen between the clinical need subsample and the remainder of the sample. About half of African Americans without a diagnosis report no history of disorder within their families compared to one-third of those with a diagnosis. Among those with a history of disorder, more report some treated disorder than only untreated disorder. Thus, a substantial majority of persons with a diagnostically evaluated need have a family history of disorder, and among these persons, a history of treated disorder predominates.
Mental Health Services Utilization among African Americans
For the total sample, less than 10 percent used any service in the past year, and utilization rates for medical services and specialty MHS are similarly low (4.3 percent vs. 5.2 percent, respectively). Rates for the clinical subsample are substantially higher, but still absolutely low: 31.1 percent, 16.2 percent, and 16.7 percent, respectively. As a reference point, data from the National Comorbidity Survey-Replication show that 41.1 percent of the U.S. population who met 12-month diagnostic criteria received any treatment during that time, with 22.8 percent using medical services and 21.7 percent using specialty MHS (Wang et al. 2005). The low rates among African Americans substantiate the merit of explaining underutilization within this population, and the unexpected comparability of utilization across the two service sectors underscores the value of identifying similarities and differences in their determinants. Although the utilization rate for any MHS is very low among persons without a diagnosis (4.9 percent), a substantial portion (40.0 percent) of those using any MHS did not have a diagnosable psychiatric disorder.
The proportion of African Americans from the total sample using any MHS use is extremely low given no family history of psychiatric disorder (5.3 percent), somewhat higher for untreated disorder (9.7 percent) and highest for treated disorder (17.0 percent; all groups differ at p < .05). A similar pattern is observed for medical services (2.4 percent, 3.5 percent, and 8.1 percent, respectively) and specialty MHS (2.9 percent, 3.9 percent, and 10.0 percent, respectively), although the no disorder versus untreated disorder contrast is not significant. Similar patterns emerge for the clinical need subsample, apart from substantially higher MHS utilization rates across all family history groups (e.g., for any MHS: 27.7 percent, 25.2 percent, and 37.5 percent, respectively). These differences are consistent with the idea that treatment clusters in families.
Family and MHS Utilization among African Americans
The results of the logistic regression model-building process for the total sample appear in Table 2. All three models are presented for any MHS use because there is evidence of moderated mediation. The conditional model is presented for specialty MHS because the interaction of SRMH and family history is statistically significant. The unconditional full model is presented for medical services because none of the interactions are significant.
Table 2.
Logistic Regressions (Odds Ratio (SE)) of Past Year Mental Health Service Utilization on Family, Mental Health, Socioeconomic, and Demographic Characteristics: Total Sample (N = 3,149).
| I. Any Mental Health Service |
II. Specialty Mental Health Services |
III. General Medical Services |
||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Characteristics | A. Reduced Model |
B. Full Mo del |
C. Conditional Model |
C. Conditional Model |
B. Full Model |
|||||
| Male | .607** | (.088) | .807 | (.128) | .805 | (.131) | 1.118 | (.285) | .803 | (.194) |
| Age (years) | .993 | (.006) | .997 | (.007) | .997 | (.007) | .990 | (.010) | 1.022 | (.012) |
| Years of education | ||||||||||
| Less than 12 years | 1.000 | 1.000 | 1.000 | 1.000 | 1.000 | |||||
| 12 years | 1.075 | (.193) | 1.261 | (.228) | 1.266 | (.235) | 1.818 | (.536) | .931 | (.288) |
| 13 to 15 years | 1.357 | (.285) | 1.650* | (.350) | 1.622* | (.352) | 2.729** | (.946) | 1.571 | (.596) |
| 16 or more years | 1.894** | (.412) | 2.258** | (.518) | 2.294** | (.560) | 4.763*** | (1.853) | 1.475 | (.604) |
| Poverty Index | .937 | (.042) | .947 | (.039) | .941 | (.040) | .917 | (.062) | .947 | (.052) |
| Marital status | ||||||||||
| Married/cohabiting | 1.000 | 1.000 | 1.000 | 1.000 | 1.000 | |||||
| Previously married | 1.516* | (.243) | 1.303 | (.237) | 1.303 | (.240) | 1.248 | (.284) | 1.015 | (.341) |
| Never married | 1.128 | (.252) | 1.275 | (.314) | 1.322 | (.316) | 1.474 | (.476) | 1.257 | (.506) |
| Lives alone (/no) | .746 | (.138) | .700 | (.136) | .687 | (.137) | .729 | (.201) | .524* | (.166) |
| Employment status | ||||||||||
| Employed | 1.000 | 1.000 | 1.000 | 1.000 | 1.000 | |||||
| Unemployed | 1.194 | (.424) | .962 | (.348) | .945 | (.340) | 1.236 | (.560) | 1.295 | (.476) |
| Not in labor force | 1.757* | (.363) | 1.431 | (.323) | 1.430 | (.333) | 1.544 | (.438) | 1.221 | (.403) |
| Insurance status | ||||||||||
| Uninsured | 1.000 | 1.000 | 1.000 | 1.000 | 1.000 | |||||
| Insured, no or unknown MHCa | .545* | (.159) | .645 | (.212) | .647 | (.213) | .598 | (.271) | .760 | (.314) |
| Insured, with MHC | 1.448 | (.327) | 1.764* | (.393) | 1.785* | (.395) | 2.032* | (.702) | 1.832 | (.573) |
| Family support | .958 | (.043) | 1.004 | (.045) | 1.011 | (.044) | 1.091 | (.064) | 1.011 | (.067) |
| Negative family interactions | 1.103** | (.032) | 1.020 | (.035) | 1.017 | (.034) | 1.032 | (.042) | 1.026 | (.055) |
| Family helpfulness 1.009 | (.087) | 1.021 | (.095) | 1.019 | (.095) | .956 | (.127) | 1.015 | (.113) | |
| Fictive kin helpfulness | 1.149 | (.100) | 1.119 | (.106) | 1.122 | (.102) | .998 | (.115) | .950 | (.136) |
| No fictive kin | 1.504 | (.536) | 1.303 | (.492) | 1.322 | (.496) | .958 | (.380) | .895 | (.452) |
| Family history of disorder/treatment | ||||||||||
| No disorder | — | — | 1.000 | 1.000 | 1.000 | 1.000 | ||||
| Untreated disorder only | — | — | 1.562 | (.352) | 2.251** | (.600) | 1.874 | (.711) | 1.133 | (.365) |
| Any treated disorder | — | — | 2.506*** | (.431) | 3.539*** | (.841) | 3.811*** | (1.187) | 2.189** | (.532) |
| Diagnosis statusb | — | — | 6.087*** | (1.015) | 6.031*** | (1.006) | 4.579*** | (1.276) | 8.368*** | (2.236) |
| Self-rated mental health (SRMH) | — | — | 1.629*** | (.130) | 2.472*** | (.302) | 2.978*** | (.430) | 1.596*** | (.130) |
| Interaction: SRMH× family history | ||||||||||
| SRMH × no disorder | — | — | — | — | 1.000 | 1.000 | — | — | ||
| SRMH × untreated disorder only | — | — | — | — | .524** | (.120) | .425* | (.135) | — | — |
| SRMH × any treated disorder | — | — | — | — | .578*** | (.079) | .592** | (.109) | — | — |
| Omnibus test of interaction (df) |
F(2, 33) = 8.71*** |
F(2, 33) = 5.14* |
||||||||
Note: Utilization: Specialty = psychiatrist, psychologist, social worker, counselor, other mental health professional, and/or mental health hotline. General medical = medical doctor, nurse, occupational therapist, or other health professional. Any service = specialty, general medical, and/or religious or spiritual advisors, informal services (e.g. online support groups, self-help groups), and any other healer.
MHC = mental health coverage.
Meets DSM-IV diagnostic criteria for one or more mood, anxiety, or substance use disorder in the past 12 months.
p < .05,
p < .01,
p < .001.
Any MHS Use
The use of any MHS by African Americans is significantly associated with negative family interactions but not any of the family support variables when these variables are considered simultaneously and in conjunction with the control variables (Model IA). Furthermore, negative interactions are not significant when need and family history are included in the full model (Model IB, Table 2).6
Over and above need, having a family history of treated disorder more than doubles the odds of using any MHS compared to a history of no disorder; however, the comparison of histories of no disorder and untreated disorder only approaches significance (p = .056). This pattern is consistent with the supposition that a family’s prior experience with treatment shapes the utilization of individual family members. Both diagnostic status and SRMH are significantly associated with substantially increased odds of using any MHS, other factors held constant.
However, the association between SRMH and use of any MHS is contingent upon family history (Model IC, Table 2). This association is significantly weaker among those with histories of untreated and treated disorder than among those with histories of no disorder. Although the effect of SRMH on utilization is statistically significant for histories of no disorder (p < .001) and treated disorder (p < .01), it is not significant when previous instances of psychiatric disorder in the family have not been treated (p = .181; post-estimation tests).
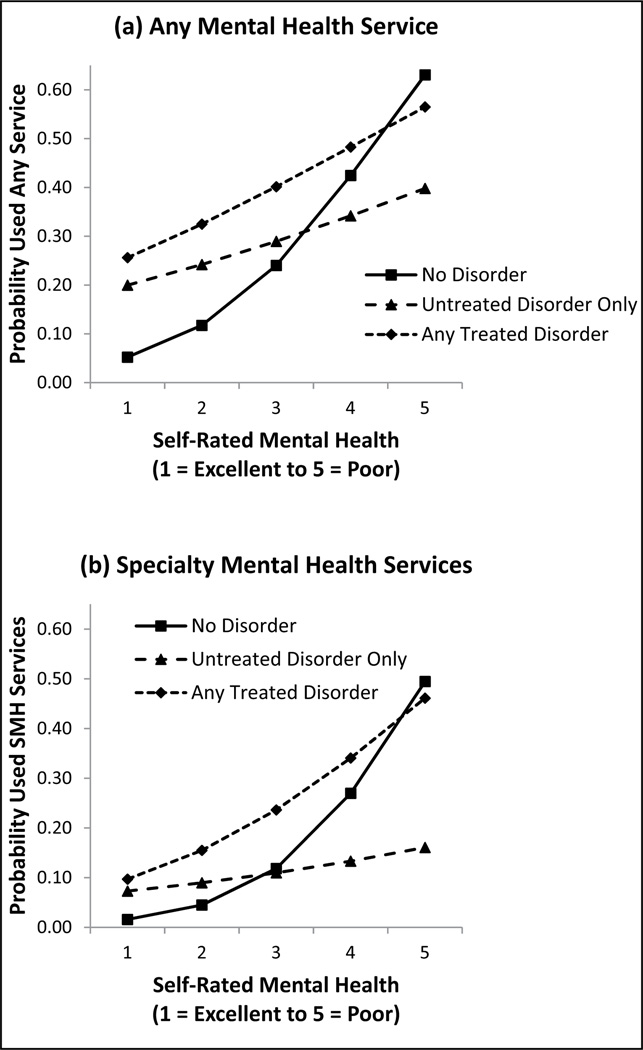
The predicted probabilities for this interaction are plotted in Figure 1(a). As SRMH goes from excellent to poor, the probability of any MHS use increases most among persons with family histories of no disorder. As a result, this group has the lowest probability of use when mental health is rated as excellent, but the highest probability when mental health is rated as poor.
Figure 1.
Predicted Probability of Any Mental Health Service Utilization by Self-Rated Mental Health and Family History: Total Sample (N = 3,149).
When SRMH is excellent, the probability of using any MHS is slightly higher among the treated than untreated disorder groups, but the magnitude of this difference widens as SRMH worsens. Consequently, at a rating of poor, the probability of use is considerably lower for histories of untreated than treated disorder. This pattern is consistent with the proposition that the presence of prior untreated disorder in the family deters utilization when another family member subsequently has mental health problems.
The results of the moderated mediation probit model provide additional insight into the impact of negative family interactions on use of any MHS. As shown in the top panel of Table 3, negative interactions do not have a significant direct effect on any MHS use, but it does have a significant positive total effect as a result of a significant positive indirect effect that is transmitted through diagnostic status and SRMH. The lower panel of the table shows that the largest component of the indirect effect is through diagnostic status. The smaller indirect effect through SRMH differs by family history, being substantially smaller for a history of no disorder than a history of untreated or treated disorder. This pattern is the same for the indirect effect through diagnostic status and SRMH; these effects are small, however, although statistically significant.
Table 3.
Direct, Indirect, and Total Effects of Family Stress on Any Past Year Mental Health (MH) Service Utilization Via Need: Total Sample (N = 3,149).
| Negative Family Interactions |
|
|---|---|
| Estimate (SE) | |
| Total effect | .049 (.023)* |
| Total indirect effect | .062 (.011)*** |
| Direct effect | −.013 (.021) |
| Specific indirect effects | |
| Via diagnostic statusa | .051 (.011)*** |
| Via self-rated mental health (SRMH) | |
| Moderated by family history | |
| No disorder | .006 (.002)** |
| Untreated disorder only | .011 (.004)** |
| Any treated disorder | .013 (.004)** |
| Via diagnostic status and self-rated mental health | |
| Moderated by family history | |
| No disorder | .004 (.001)*** |
| Untreated disorder only | .007 (.002)*** |
| Any treated disorder | .008 (.002)*** |
Note: Model contains all terms in Model IC, Table 2; indirect effect of negative family interactions through diagnostic status and SRMH; indirect effect of diagnostic status through SRMH; and interaction of SRMH and family history.
Meets DSM-IV diagnostic criteria for one or more mood, anxiety, or substance use disorder in the past 12 months.
p < .05,
p < .01,
p < .001.
Socioeconomic and demographic characteristics play a very limited role in the use of any MHS among African Americans when considered simultaneously with family variables and need, as also shown in Table 2 (Model IC). Having more than a high school education (relative to less than a high school) increases the odds of any MHS use, and health insurance enables utilization (relative to no insurance), but only when the person knows it covers MHS.
Specialty MHS Use
None of the family functioning variables are statistically significant in the restricted model for this outcome (not shown), negating the possibility of mediated effects for this outcome. Otherwise, the results for this outcome are isomorphic to those for any MHS in that the conditional model provides the best fit to the data, as shown in Table 2 (Model IIC). Specifically, the impact of SRMH on use of specialty MHS differs significantly across the family history groups, with SRMH having a significant and strong association with utilization among those with histories of no disorder (p < .001) and a significantly weaker association among those with histories of treated disorder that is nevertheless significantly different from zero (p < .001). The association between SRMH and use of specialty MHS is not significant (p = .369), however, among those with histories of untreated disorder.
As shown in Figure 1(b), the probability of using this type of service at excellent SRMH approaches zero for family histories of no disorder and is somewhat higher for histories of treated or untreated disorder. In contrast, among those who describe their mental health as poor, the probability of using specialty MHS remains low among the untreated disorder group and is similarly higher among the no disorder and treated disorder groups.
High levels of education are associated with greater odds of using specialty MHS services among African Americans, as is having health insurance with known mental health coverage (Model IIC, Table 2).
General Medical Services Use
None of the family functioning variables are statistically significant in the restricted model for this outcome (not shown), meaning that there are no independent effects of support or negative interactions to be mediated by need. None of the tested interaction terms are statistically significant for this outcome.
When need is taken into consideration, the only aspect of family that matters is having a history of treated disorder, which doubles the odds of using medical services for psychological problems compared to a history of no disorder (Model IIIB, Table 2). Family history of untreated disorder is not significantly different from history of no disorder.
Diagnostic status and SRMH substantially increase the odds of utilization of medical services. The only other factor that is statistically significant is living alone, which lowers these odds. Thus, use of medical services among African Americans appears to be primarily a function of having a psychiatric disorder, evaluating one’s mental health unfavorably, belonging to a family that has a history of treated disorder, and not living alone.
Family and Utilization among African Americans with Clinical Need
The results of the logistic regression model-building process for the clinical need subsample of persons with at least one past-year disorder appear in Table 4. The family functioning variables are not associated with utilization in any of the models tested and do not interact with family history. However, family history moderates the effect of SRMH on any MHS and has main effects for specialty MHS but not medical services. Therefore, the conditional model is presented for any MHS and the full model is presented for specialty MHS and medical services.
Table 4.
Logistic Regressions (Odds Ratio (SE)) of Past Year Mental Health Service Utilization on Family, Mental Health, Socioeconomic, and Demographic Characteristics: Clinical Need Subsample (N = 605).
| Characteristics | I. Any Mental Health Service |
II. Specialty Mental Health Services |
III. General Medical Services |
|||
|---|---|---|---|---|---|---|
| Male | .891 | (.226) | 1.195 | (.456) | .908 | (.284) |
| Age (years) | 1.029** | (.010) | 1.025* | (.012) | 1.050** | (.015) |
| Years of education | ||||||
| Less than 12 years | 1.000 | 1.000 | 1.000 | |||
| 12 years | 1.470 | (.371) | 2.837* | (1.437) | 1.334 | (.410) |
| 13 to 15 years | 2.361* | (.830) | 5.010** | (2.724) | 2.565* | (.980) |
| 16 or more years | 2.757** | (1.013) | 6.569** | (3.903) | 1.163 | (.506) |
| Poverty Index | 1.015 | (.048) | 1.006 | (.051) | 1.003 | (.049) |
| Marital status | ||||||
| Married/cohabiting | 1.000 | 1.000 | 1.000 | |||
| Previously married | .929 | (.270) | .955 | (.281) | .730 | (.353) |
| Never married | 1.742 | (.654) | 2.253* | (.858) | 1.278 | (.545) |
| Lives alone (/no) | .340** | (.106) | .383** | (.121) | .437* | (.165) |
| Employment status | ||||||
| Employed | 1.000 | 1.000 | 1.000 | |||
| Unemployed | 1.043 | (.435) | 1.365 | (.693) | 1.480 | (.726) |
| Not in labor force | 1.627 | (.505) | 1.270 | (.435) | 1.244 | (.540) |
| Insurance status | ||||||
| Uninsured | 1.000 | 1.000 | 1.000 | |||
| Insured, no or unknown MHCa | .805 | (.338) | 1.018 | (.659) | .672 | (.330) |
| Insured, with MHC | 1.172 | (.374) | 1.964 | (.845) | 1.579 | (.604) |
| Family support | 1.054 | (.069) | 1.139 | (.102) | 1.067 | (.083) |
| Negative family interactions | .989 | (.048) | 1.075 | (.057) | 1.046 | (.068) |
| Family helpfulness | .955 | (.097) | .938 | (.152) | 1.009 | (.126) |
| Fictive kin helpfulness | 1.170 | (.129) | 1.057 | (.169) | .785 | (.146) |
| No fictive kin | .826 | (.392) | 1.036 | (.520) | .297 | (.220) |
| Family history of disorder/treatment | ||||||
| No disorder | 1.000 | 1.000 | 1.000 | |||
| Untreated disorder only | 1.452 | (.456) | .409** | (.122) | .776 | (.319) |
| Any treated disorder | 1.832* | (.517) | 1.518 | (.420) | 1.333 | (.443) |
| Number of DSM-IV diagnoses | ||||||
| 1.000 | 1.000 | 1.000 | 1.000 | |||
| 2.000 | 2.336* | (.748) | 2.089 | (.999) | 2.262* | (.801) |
| 3 or more | 4.497*** | (1.369) | 3.263** | (1.291) | 3.290** | (1.233) |
| Self-rated mental health (SRMH) | 1.920*** | (.343) | 1.640*** | (.223) | 1.350* | (.193) |
| Interaction: SRMH × family history | ||||||
| SRMH × no disorder | 1.000 | |||||
| SRMH × untreated disorder only | .553* | (.156) | – | – | – | – |
| SRMH × any treated disorder | .685* | (.106) | – | – | – | – |
| Omnibus test of interaction (df) | F(2, 33) = 3.67* | |||||
Note: Utilization: Specialty = psychiatrist, psychologist, social worker, counselor, other mental health professional, and/or mental health hotline. General medical = medical doctor, nurse, occupational therapist, or other health professional. Any service = specialty, general medical, and/or religious or spiritual advisors, informal services (e.g. online support groups, self-help groups), and any other healer.
MHC = mental health coverage.
p < .05,
p < .01,
p < .001.
Any MHS Use
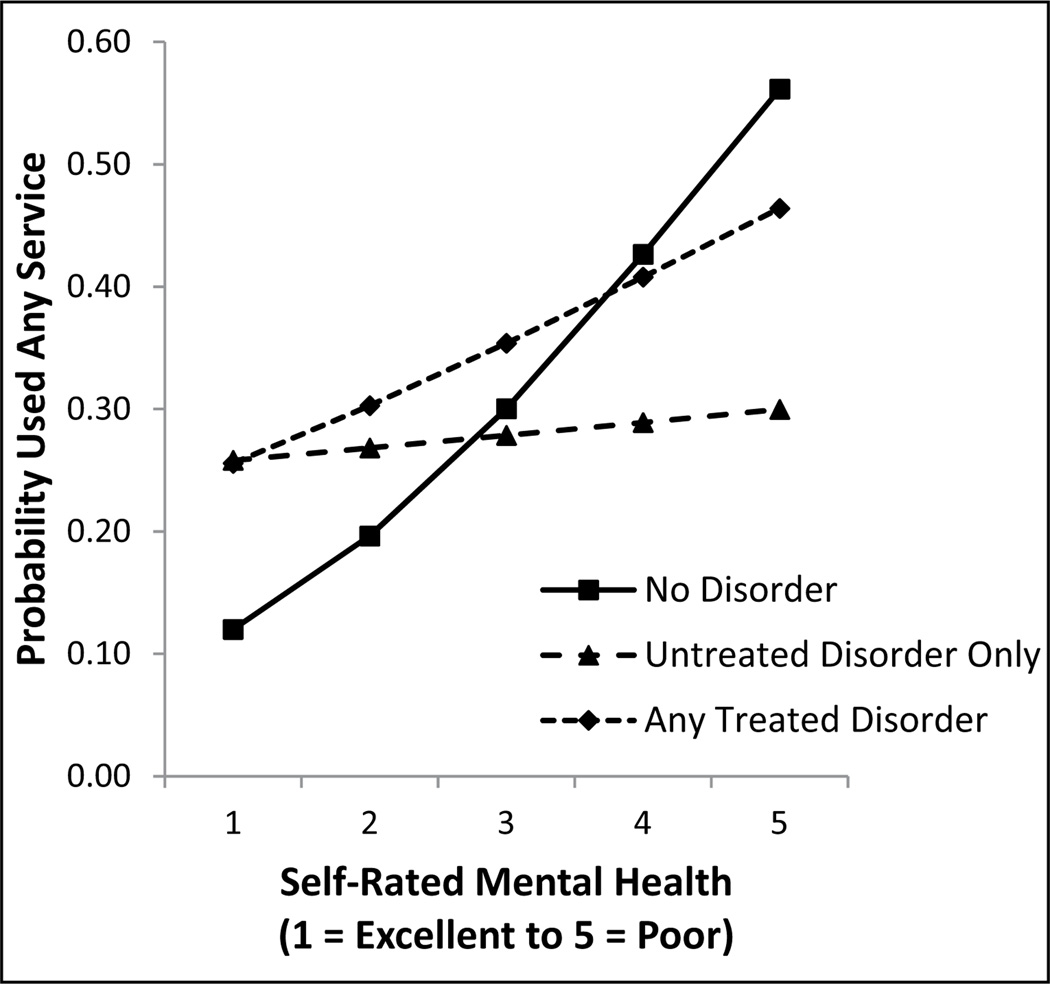
The impact of SRMH on this outcome is significantly weaker among persons with family histories of untreated and treated disorder than persons with histories of no disorder, net of other variables in the model (see Table 4). Although the effect of SRMH on utilization is statistically significant for no disorder, its moderate effect in the treated disorder group only approaches significance (p = .09), and is weak and nonsignificant in the untreated group (p = .76).
The predicted probabilities for this conditional relationship are plotted in Figure 2. Although utilization is relatively low at excellent, this probability is noteworthy in the absolute, especially among those with family histories of disorder. The history of no disorder group has the lowest probability of utilization at excellent, but the highest probability at poor, surpassing the untreated and treated histories. At excellent, the probability of utilization is similar for the treated and untreated history groups, but at poor this probability is much higher among the treated than untreated group because utilization does not vary much in the untreated group as a function of how the person rates his or her mental health.
Figure 2.
Predicted Probability of Any Mental Health Service Utilization by Self-rated Mental Health and Family History: Clinical Need Subsample (N = 605).
Number of diagnoses is strongly associated with utilization of any MHS in a dose-response manner. Education also has strong positive effects, while living alone is associated with low odds of utilization, and these odds increase as age increases.
Specialty MHS Use
Unlike the total sample, the impact of SRMH on use of specialty MHS services among the clinical need subsample is not conditional upon family history: instead, these two variables have independent effects on utilization (see Table 4). The odds of using specialty MHS increase as SRMH worsens, and a history of untreated disorders substantially lowers these odds relative to a history of no disorder, other things being equal, although these odds do not differ significantly for the no disorder and treated disorder groups. In addition, multiple comorbidities increase these odds.
The use of specialty MHS also increases steadily as education and age increase. The never married have twice the odds of using specialty services compared to the married/cohabiting. In contrast, persons who live alone have lower odds of utilization relative to those who live with others. Other characteristics are not statistically significant.
General Medical Services
For this outcome, SRMH has a main effect, but family history is not statistically significant, although number of diagnoses progressively increase the odds of using medical services. Like the other two outcomes, use of medical services increases as age increases and living alone decreases these odds. With regard to socio-economic variables, only one contrast is significant: those with 13 to 15 years of education have twice the odds of using medical services than those with less than high school education.
DISCUSSION
Based on these results, Hypothesis 1 for family support is rejected, while Hypothesis 2 for family stress receives partial support insofar as the effect of negative interactions is mediated by diagnosis status and SRMH, although only for any MHS (total sample only). For Hypothesis 3, there is: no support for Hypothesis 3a for family support, partial support for Hypothesis 3b in the form of the moderated mediated effect of negative family interactions for any MHS (total sample only), and partial support for Hypothesis 3c insofar as SRMH is moderated by family history for any MHS and specialty MHS (total sample only).
Unlike the total sample, for the clinical need subsample, the only family variable that matters is family history. Sherbourne (1988) suggests that family influences on formal MHS utilization may not persist once a need for care has been established. This interpretation implies that families only indirectly affect utilization by influencing need, which is consistent with our results. However, we find that persons with family histories of untreated disorder are especially unlikely to use specialty MHS. They have a low probability of using any MHS irrespective of how they rate their mental health, a pattern that also is observed for the total sample.
In both the total sample and clinical need subsample, utilization rates for medical services and specialty MHS are roughly the same, which was unanticipated because some existing studies report that African Americans are more likely than non-Hispanic whites to use medical services and less likely to use specialty services. The observed similarity between these service sectors among African Americans may be associated with the steady increase in the use of these services across the U.S. population. Between 1990 and 2003, there was a substantial increase in the use of psychiatric services and the use of medical services for mental health problems and a somewhat smaller increase in the use of other mental health services (Kessler et al. 2005). These changes may have led to a narrowing over time of the gap between sectors among African Americans.
Turning to the results for the total sample and other outcomes, we find that family history alters the impact of a key element in the help-seeking process—the realization that something is wrong, as indexed by SRMH—on the use of any and specialty MHS. Utilization is particularly low among persons with family histories of untreated disorder irrespective of how they rate their mental health, suggesting that these individuals encounter deterrents to utilization that are of sufficient magnitude to override their awareness of having mental health problems. Obstacles to service use often arise outside of the family, but the lack of responsiveness to perceived mental health problems is specific to having relatives who have not used services when they had similar problems. This connection calls attention to intrafamilial factors that may have kept family members with mental health problems from seeking professional help in the past and continue to do so, such as having relatives persistently express stigmatized attitudes toward MHS (e.g., Lindsey et al. 2010). This also might reflect lack of familiarity with the treatment system among relatives, which may interfere with them functioning as navigators of this system (e.g., Hines-Martin, Brown-Piper, et al. 2003; Pescosolido 1992). Alternately, this nonuse of services among persons who see their mental health as poor may be a direct result of a relative’s earlier untreated disorder; for example, a disorder that resolved itself without treatment may lead to an expectation this will happen for oneself too. However, we do not have information that can be used to sort out these possibilities, making these interpretations speculative.
For other family histories, SRMH is associated with utilization, more so among persons with family histories of no disorder than histories of treated disorder. We had reasoned that family members with treated disorders normalize treatment, reduce stigma and provide information about how to identify resources and access services, thereby increasing utilization of MHS (Vogel et al. 2007). In retrospect, our hypothesis that families with past treatment experience would foster help-seeking did not give sufficient consideration to the impact of negative past treatment experiences in some families, which is likely to offset the impact of positive experiences in other families, generating a small average effect. African Americans who use MHS for a mental health problem tend to be less satisfied with their care than non-Latino whites (e.g., Diala et al. 2000), which supports this interpretation.
Very low rates of utilization are expected for persons who perceive their mental health as excellent or very good, and although this is the case for persons without a history of psychiatric disorder, those with a history of treated disorder have a noteworthy chance of using services. This pattern sheds light on the use of services by people who do not appear to have a need for treatment MHS (Meadows et al. 2000). This seemingly excess use may be among the “worried well,” whose worry stems from knowing relatives with prior psychiatric disorders. It should be noted, however, that persons without a diagnosable disorder often have substantial psychological distress that warrants treatment (Mechanic 2003).
Although family functioning plays a prominent role in theories about the etiology of mental illness, our findings show that these influences extend to utilization of MHS. Existing research has focused almost exclusively on examining family support in help-seeking, but our findings indicate that family stress is more consequential to use of any MHS among African Americans. Specifically, negative family interactions appear to increase utilization by influencing need and leading people to see themselves as having mental health problems. However, these indirect influences are limited to the composite category of any MHS, suggesting that family functioning plays a role in moving a person from no service use to any of a number of services, but not in differentiating among these services. Given these indirect effects, we infer that the impact of family on utilization is likely to be underestimated by the common practice of misinterpreting the direct effect of family (net of need and other potential mediators) as if it were the total effect.
When negative family interactions are taken into consideration, family support lacks any effect on utilization of specialty MHS, medical services, or any MHS. Studies that overlook problematic aspects of family relationships, therefore, may well overestimate the impact of support. We recommend that future research spell out more fully the impact of adverse dimensions of family relationships.
We hypothesized that the impact of family functioning is conditional upon family history, but these interactions were not statistically significant. However, as a result of the interaction of family history and SRMH, negative family interactions have a greater indirect effect on the use of any MHS among persons with a history of disorder than among persons with a history of no disorder. This pattern may occur because the past occurrence of disorder in the family predisposes people to interpret stress-induced psychological distress as signs and symptoms of mental disorder because they know that disorder “runs” in their families (e.g., Prokofyeva et al. 2013).
Similar to previously published studies, we find that predictors of greater MHS utilization include: (1) two social resources—being married (total sample) and not living alone (clinical need subsample), (2) more years of education, and (3) insurance with mental health coverage (total sample). Being married and living with others are social contexts in which others can observe on a day-to-day basis changes in behavior or emotions that may signal mental health problems and can help to facilitate access to care, while marital dissolution like divorce or separation may intensify stress and need for care, thereby influencing use of MHS. Education increases knowledge about mental illness and treatment, while insurance eases financial constraints. Unlike previous studies (e.g., Albizu-Garcia et al. 2001; Neighbors et al. 2008), we did not find gender differences net of the other variables in the analysis, although in bivariate analyses men used MHS less often than women. The lack of a net gender effect appears to be due to the inclusion of need and family history variables: Compared to women, men have significantly (p < .05): better SRMH, less disorder, more family histories of no disorder, and fewer histories of treated disorder. We did not find age effects for most outcomes, perhaps because, in contrast to previous studies, we treated age as a continuous variable and not as categorical because of data sparseness concerns with multiple categorical variables.
Several limitations of this study merit mention. First, reported family histories may be imprecise because respondents lack the requisite information or give socially desirable responses. If so, then some people with positive histories are likely to be misclassified as having negative histories, which would tend to attenuate observed associations. However, these concerns are mitigated somewhat because our approach emphasizes histories that are known to the person and others in the family, following the sociological dictum “if men define situations as real, they are real in their consequences” (Thomas and Thomas, 1928:571–72). Also, our history questions ask about symptoms and whether any professional treatment was obtained, whereas diagnostic status and detailed data about service sectors would permit more refined analysis, as would information about whether the previous treatment was viewed in positive terms. Second, our mediation analysis assumes that negative interactions are causally antecedent to need and that need influences utilization. However, there are other possibilities: the use of services may lessen negative interactions with family members, and treatment presumably leads to remission or recovery, that is, reciprocal or reverse causation. More generally, the cross-sectional data mean that we cannot unequivocally infer causality. Longitudinal data would allow us to use the time-ordering of events to help establish the direction of causal influence. Longitudinal effects might be smaller to the extent that causal influence flows from utilization to need or family functioning. Additionally, we cannot rule out the possibility that a shared environment accounts for the correspondence between family history and the person’s mental health status and use of services. Third, our measures of need are not optimal for reasons given by Mechanic (2003), including the mild and transient nature of some psychiatric disorders and the substantial distress experienced by some persons who do not meet diagnostic criteria. Furthermore, culture bias in the measure may misclassify persons as not having a disorder, for example, does not capture nonpsychothat offer alternativelogical idioms of distress that may be disproportionately found in the African American population (e.g., Snowden 2001). Fourth, our focus on the family necessarily means that we have omitted many extrafamilial influences on utilization, including those that systematically deter utilization in general and among African Americans in particular. Finally, because this analysis is restricted to African Americans, it is not possible to determine the extent to which the results are specific to this population or apply to the population in general. This determination awaits research on these relationships using other data sets and racial/ethnic groups.
These limitations notwithstanding, the current study has a number of notable strengths, including the large national probability sample of African Americans, which yields excellent external validity and permits generalization to the population. In addition, although many disorders were not assessed in the NSAL, the most common disorders were measured and assessed with a standardized instrument that has been widely applied in existing research. Furthermore, the study provides a level perspective on family functioning as encompassing both positive and negative features and in doing so demonstrates the relevance of family stress to utilization. The mediation analysis attests to the value of identifying the pathways that connect the family to utilization. Additionally, the use of family history as a context suggests that the population may be comprised of distinct subgroups that differ not only in their use of services but also in the process leading to utilization, thereby introducing a potentially productive new line of research in this area.
Our results point toward three other areas for future research. The first is to examine the extent to which a family history of disorder/treatment explains differences in MHS utilization between African Americans and non-Latino whites. These histories are likely to differ between these groups as a consequence of the low prevalence and treatment rates among African Americans compared to non-Latino whites. Second, the indirect effects of family functioning on utilization merit further examination because the absence of direct effects might otherwise be misconstrued as meaning that these factors are unimportant and because existing research has focused on direct effects (insofar as indirect and total effects have not been estimated). Finally, although extant research has emphasized the explanation of underutilization among those with a mental disorder, future research also should address the use of services among persons who do not have a disorder because this group comprises a substantial portion of all African Americans who use services.
The distinctive family effects observed in this study yield specific policy implications. First, the family history results suggest that patients in primary care settings be screened not only for their own mental health, but also for family histories of mental illness, much like routine screening for family histories of cancer and heart disease, to identify patients who may be at risk of untreated mental health problems. Schor and colleagues (1987) recommend that family health data be used to inform selective interventions by health care providers, a recommendation that we endorse. Second, the indirect effects of family stress suggest interventions that focus on decreasing negative family interactions and increasing positive interactions may help reduce need for care. Finally, this study does not address a wide range of social, cultural, economic, and psychological factors that may lessen utilization among African Americans, such as racism, mistreatment in the health care system, lack of accessible and culturally appropriate treatment facilities, and cultural insensitivity of mental health professionals that may lead to inadequate detection of mental health problems and improper diagnosis and treatment (Alegría et al. 2002; Lindsey et al. 2010; Wang et al. 2005)—factors that offer alternative explanations for our findings. Our focus on the family should not deflect attention from policy initiatives to reduce these systematic barriers to services based on race.
In conclusion, problematic family relationships appear to have a greater influence than supportive ones on MHS use among African Americans in general and especially among those with a family history of disorder. Having a relative with a psychiatric disorder, and whether that disorder is treated or untreated, are consequential for the use of services. In particular, utilization is affected by a person’s perceived mental health, as indexed by SRMH, except when there is a family history of untreated disorder. Family history also influences treatment for African Americans with a clinical need. Thus, a family history of untreated disorder may be an important mechanism through which the underutilization of MHS among African Americans is passed down from generation to generation within a family or spread laterally within a generation.
Acknowledgments
FUNDING
The authors disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: The National Survey of American Life (NSAL) is supported by the National Institute of Mental Health (NIMH; grant U01-MH577616) with supplemental support from the Office of Behavioral and Social Science Research at the National Institutes of Health (NIH) and the University of Michigan. The preparation of this article was partially supported by a fellowship from the Graduate Division of the University of California, Los Angeles (UCLA) and the NIH/National Center for Advancing Translational Science UCLA Clinical and Translational Science Institute grant (TL1 TR000121). The content is solely the responsibility of the authors and does not represent the official views of UCLA or NIH.
Biographies
Alice P. Villatoro is a PhD candidate in the Department of Health Policy and Management at the UCLA Fielding School of Public Health. Her research primarily focuses on understanding racial-ethnic disparities in access and utilization of mental health services. She is currently working on completing her doctoral dissertation, which examines racial-ethnic variation in perceptions of need for mental health care. Her dissertation research is support by the UCLA TL1 Clinical and Translational Science Fellowship.
Carol S. Aneshensel is professor of Community Health Sciences at the UCLA Fielding School of Public Health. Her research concerns the ways in which social inequality becomes mental health disparities with a focus on the unequal distribution of stressors and resources. Most recently, her work has focused on the impact of the social stratification of neighborhoods on the mental health of older persons. She is the past Chair of the Sociology of Mental Health Section of the American Sociological Association (ASA) and recipient of its Leonard I. Pearlin Award for Distinguished Contributions to the Sociological Study of Mental Health, and past Chair of the Medical Sociology Section of ASA and recipient of its Leo G. Reeder Award for Distinguished Contributions.
APPENDIX
Percentage Distribution of Past Year DSM-IV Mental Disorders for the Total and Clinical Need Subsample, African American Adults, 2001–2003, NSAL (weighted).
| Total Sample (N = 3,149) | Clinical Need Sample (N = 605) | |
|---|---|---|
| DSM-IV past year disorder | ||
| Major depressive disorder | 5.1 | 27.6 |
| Major depressive episode | 6.3 | 33.8 |
| Dysthymia | 2.3 | 12.6 |
| Bipolar disorder | 1.1 | 5.8 |
| Panic attack | 7.9 | 42.5 |
| Panic disorder | 2.2 | 11.7 |
| Social phobia | 4.2 | 22.6 |
| Agoraphobia without panic | 1.6 | 8.5 |
| Agoraphobia with panic | 1.0 | 5.2 |
| Generalized anxiety disorder | 2.1 | 11.5 |
| Posttraumatic stress disorder | 3.7 | 20.0 |
| Alcohol abuse | 2.1 | 11.1 |
| Alcohol dependence | 1.0 | 5.6 |
| Drug abuse | 1.2 | 6.3 |
| Drug dependence | .6 | 3.2 |
| Type of DSM-IV past year disorder | ||
| Mood disordera | 6.6 | 35.6 |
| Anxiety disorderb | 14.7 | 79.1 |
| Substance use disorderc | 2.8 | 15.0 |
| Number of DSM-IV past year disorders | ||
| None | 81.5 | — |
| One | 8.1 | 43.7 |
| Two | 4.7 | 25.2 |
| Three or more | 5.8 | 31.1 |
Mood disorder = includes major depression disorder, major depressive episode, dysthymia, and bipolar disorder.
Anxiety disorder = includes panic attack, panic disorder, social phobia, agoraphobia, generalized anxiety disorder, and PTSD.
Substance use disorder = includes alcohol abuse/dependence and drug abuse/dependence.
Footnotes
We use the terminology of the cited study for race-ethnicity.
Fictive kin are people who are not related by blood or marriage, but who are treated just like a relative (Taylor and Chatters 1991).
Hereafter, we refer to general medical services as simply medical services.
Although the items ask about symptoms of psychiatric disorder not diagnosed disorder per se, we use psychiatric disorder as shorthand because this appears to be the intent of the questions.
Hereafter the term diagnosis means meeting research diagnostic criteria for a psychiatric disorder based on a computer scored algorithm applied to data collected with a standardized survey instrument.
We do not test for mediation by comparing the reduced and full model using the difference of coefficient methods because coefficients cannot be compared across logistic models as variables are added (Mood 2010). Instead, we use the product of coefficient method.
REFERENCES
- Abe-Kim Jennifer, Takeuchi David, Hwang Wei-Chin. Predictors of Help Seeking for Emotional Distress Among Chinese Americans: Family Matters. Journal of Consulting and Clinical Psychology. 2002;70(5):1186–1190. [PubMed] [Google Scholar]
- Albizu-Garcia Carmen E, Alegría Margarita, Freeman Daniel, Vera Mildred. Gender and Health Services Use for a Mental Health Problem. Social Science & Medicine. 2001;53(7):865–878. doi: 10.1016/s0277-9536(00)00380-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alegría Margarita, Canino Glorisa, Rios Ruth, Vera Mildred, Calderon Jose, Rusch Dana, Ortega Alexander N. Inequalities in Use of Specialty Mental Health Services among Latinos, African Americans, and Non-Latino Whites. Psychiatric Services. 2002;53(12):1547–1555. doi: 10.1176/appi.ps.53.12.1547. [DOI] [PubMed] [Google Scholar]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 4th ed. Washington, DC: Author; 2000. [Google Scholar]
- August Kristin J, Rook Karen S, Newsom Jason T. The Joint Effects of Life Stress and Negative Social Exchanges on Emotional Distress. Journal of Gerontology. 2007;62B(5):S304–S314. doi: 10.1093/geronb/62.5.s304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Breslau Joshua, Aguilar-Gaxiola Sergio, Kendler Kenneth S, Su Maxwell, Williams David, Kessler Ronald C. Specifying Race-ethnic Differences in Risk for Psychiatric Disorder in a USA National Sample. Psychological Medicine. 2006;36(1):57–68. doi: 10.1017/S0033291705006161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Breslau Joshua, Kendler Kenneth S, Su Maxwell, Gaxiola-Aguilar Sergio, Kessler Ronald C. Lifetime Risk and Persistence of Psychiatric Disorders across Ethnic Groups in the United States. Psychological Medicine. 2005;35(3):317–327. doi: 10.1017/s0033291704003514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clausen John A, Yarrow Marian Radke. Mental Illness and the Family. Journal of Social Issues. 1955;11:3–5. [Google Scholar]
- Diala Chamberlain, Muntaner Carles, Walrath Christine, Nickerson Kim J, LaVeist Thomas A, Leaf Philip J. Racial Differences in Attitudes Towards Professional Mental Health Care and in the Use of Services. American Journal of Orthopsychiatry. 2000;70(4):455–464. doi: 10.1037/h0087736. [DOI] [PubMed] [Google Scholar]
- Harris Katherine M, Edlund Mark J, Larson Sharon. Racial and Ethnic Differences in the Mental Health Problems and Use of Mental Health Care. Medical Care. 2005;43(8):775–784. doi: 10.1097/01.mlr.0000170405.66264.23. [DOI] [PubMed] [Google Scholar]
- Heeringa Steven G, Wagner James, Torres Myriam, Duan Naihua, Adams Terry, Berglund Patricia. Sample Designs and Sampling Methods for the Collaborative Psychiatric Epidemiology Studies (CPES) International Journal of Methods in Psychiatric Research. 2004;13(4):221–240. doi: 10.1002/mpr.179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hines-Martin Vicki, Brown-Piper Ada, Kim Sanggil, Malone Mary. Enabling Factors of Mental Health Service Use among African Americans. Archives of Psychiatric Nursing. 2003;17(5):197–204. doi: 10.1016/s0883-9417(03)00094-3. [DOI] [PubMed] [Google Scholar]
- Hines-Martin Vicki, Malone Mary, Kim Sanggil, Brown-Piper Ada. Barriers to Mental Health Care Access in an African American Population. Issues in Mental Health Nursing. 2003;24(3):237–256. doi: 10.1080/01612840305281. [DOI] [PubMed] [Google Scholar]
- Kendler Kenneth S. Is Seeking Treatment for Depression Predicted by a History of Depression in Relatives? Implications for Family Studies of Affective Disorder. Psychological Medicine. 1995;25:807–814. doi: 10.1017/s0033291700035054. [DOI] [PubMed] [Google Scholar]
- Kessler Ronald C, Demler Olga, Frank Richard G, Olfson Mark, Pincus Harold Alan, Walters Ellen E, Wang Philip, Wells Kenneth B, Zaslavsky Alan M. Prevalence and Treatment of Mental Disorders, 1990–2003. The New England Journal of Medicine. 2005;352(24):2515–2523. doi: 10.1056/NEJMsa043266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lincoln Karen D, Taylor Robert Joseph, Chatters Linda M. Correlates of Emotional Support and Negative Interaction among Older Black Americans. Journal of Gerontology. 2003;58B(4):S225–S233. doi: 10.1093/geronb/58.4.s225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lincoln Karen D, Taylor Robert Joseph, Chatters Linda M. Correlates of Emotional Support and Negative Interaction among African Americans and Caribbean Blacks. Journal of Family Issues. 2012:1–29. doi: 10.1177/0192513X12454655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lindsey Michael, Joe Sean, Nebbitt Von. Family Matters: The Role of Mental Health Stigma and Social Support on Depressive Symptoms and Subsequent Help Seeking among African American Boys. Journal of Black Psychology. 2010;36(4):458–482. doi: 10.1177/0095798409355796. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MacKinnon David P. Introduction to Statistical Mediation Analysis. New York: Taylor & Francis Group, LLC; 2008. [Google Scholar]
- Meadows G, Burgess P, Fossey E, Harvey C. Perceived Need for Mental Health Care, Findings from the Australian National Survey of Mental Health and Well-being. Psychological Medicine. 2000;30(3):645–656. doi: 10.1017/s003329179900207x. [DOI] [PubMed] [Google Scholar]
- Mechanic David. Is the Prevalence of Mental Disorders a Good Measure of the Need for Services? Health Affairs. 2003;22:8–20. doi: 10.1377/hlthaff.22.5.8. [DOI] [PubMed] [Google Scholar]
- Mood Carina. Logistic Regression: Why We Cannot Do What We Think We Can Do, and What We Can Do about It. European Sociological Review. 2010;26(1):67–82. [Google Scholar]
- Neighbors Harold W, Caldwell Cleopatra, Williams David R, Nesse Randolph, Taylor Robert Joseph, Bullard Kai McKeever, Torres Myriam, Jackson James S. Race, Ethnicity, and the Use of Services for Mental Disorders: Results from the National Survey of American Life. Archives of General Psychiatry. 2007;64(4):485–494. doi: 10.1001/archpsyc.64.4.485. [DOI] [PubMed] [Google Scholar]
- Neighbors Harold W, Woodward Amanda Toler, Bullard Kai McKeever, Ford Briggett C, Taylor Robert Joseph, Jackson James S. Mental Health Service Use among Older African Americans: The National Survey of American Life. The American Journal of Geriatric Psychiatry. 2008;16(12):948–956. doi: 10.1097/JGP.0b013e318187ddd3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pescosolido Bernice A. Beyond Rational Choice: The Social Dynamics of How People Seek Help. AJS. 1992;97:1096–1138. [Google Scholar]
- Pescosolido Bernice A, Boyer Carol A. Understanding the Context and Dynamic Social Processes of Mental Health Treatment. In: Scheid TL, Brown TN, editors. A Handbook for the Study of Mental Health. Cambridge: Cambridge University Press; 2010. pp. 420–438. [Google Scholar]
- Pescosolido Bernice A, Gardner Carol Brooks, Lubell Keri M. How People Get into Mental Health Services: Stories of Choice, Coercion and 'Muddling Throught' from 'First Timers.'. Social Science & Medicine. 1998;46(2):275–286. doi: 10.1016/s0277-9536(97)00160-3. [DOI] [PubMed] [Google Scholar]
- Proctor Bernadette D, Dalaker Joseph. Poverty in the United States: 2001. Washington, DC: U.S. Census Bureau; 2002. [Google Scholar]
- Prokofyeva Elena, Martins Silvia S, Younès Nadia, Surkan Pamela J, Melchior Maria. The Role of Family History in Mental Health Service Utilization for Major Depression. Journal of Affective Disorders. 2013;151:461–466. doi: 10.1016/j.jad.2013.06.025. [DOI] [PubMed] [Google Scholar]
- Rook Karen S. Investigating the Positive and Negative Sides of Personal Relationships: Through a Lens Darkly? In: Spitzberg BH, Cupach WR, editors. The Dark Side of Close Relationships. Mahwah, NJ: Lawrence Erlbaum Associates Publishers; 1998. pp. 369–393. [Google Scholar]
- Schor Edward, Starfield Barbara, Stidley Christine, Hankin Janet. Family Health: Utilization and Effects of Family Membership. Medical Care. 1987;25(7):616–626. [PubMed] [Google Scholar]
- Sherbourne Cathy Donald. The Role of Social Support and Life Stress Events in Use of Mental Health Services. Social Science & Medicine. 1988;27:1393–1400. doi: 10.1016/0277-9536(88)90205-5. [DOI] [PubMed] [Google Scholar]
- Snowden Lonnie R. Barriers to Effective Mental Health Services for African Americans. Mental Health Services Research. 2001;3(4):181–187. doi: 10.1023/a:1013172913880. [DOI] [PubMed] [Google Scholar]
- Snowden Lonnie R, Pingitore David. Frequency and Scope of Mental Health Service Delivery to African Americans in Primary Care. Mental Health Services Research. 2002;4(3):123–130. doi: 10.1023/a:1019709728333. [DOI] [PubMed] [Google Scholar]
- StataCorp. Stata Statistical Software: Release 12. College Station, TX: StataCorp LP; 2011. [Google Scholar]
- Sussman Linda K, Robins Lee N, Earls Felton. Treatment-seeking for Depression by Black and White Americans. Social Science & Medicine. 1987;24(3):187–196. doi: 10.1016/0277-9536(87)90046-3. [DOI] [PubMed] [Google Scholar]
- Taylor Robert Joseph, Chatters Linda M. Extended Family Networks of Older Black Adults. Journal of Gerontology. 1991;46(4):S210–S217. doi: 10.1093/geronj/46.4.s210. [DOI] [PubMed] [Google Scholar]
- Thoits Peggy A. Self-labeling Processes in Mental Illness: The Role of Emotional Deviance. AJS. 1985;91:221–249. [Google Scholar]
- Thoits Peggy A. Mechanisms Linking Social Ties and Support to Physical and Mental Health. Journal of Health and Social Behavior. 2011a;52(2):145–161. doi: 10.1177/0022146510395592. [DOI] [PubMed] [Google Scholar]
- Thoits Peggy A. Perceived Social Support and the Voluntary, Mixed, or Pressured Use of Mental Health Services. Society and Mental Health. 2011b;1(1):4–19. [Google Scholar]
- Thomas William Isaac, Thomas Dorothy Swaine. The Child in America: Behavior Problems and Programs. New York: Knopf; 1928. [Google Scholar]
- Vogel David L, Wade Nathaniel G, Wester Stephen R, Larson Lisa, Hackler Ashley H. Seeking Help from a Mental Health Professional: The Influence of One’s Social Network. Journal of Clinical Psychology. 2007;63(3):233–245. doi: 10.1002/jclp.20345. [DOI] [PubMed] [Google Scholar]
- Wang Philip S, Lane Michael, Olfson Mark, Pincus Harold A, Wells Kenneth B, Kessler Ronald C. Twelve-month Use of Mental Health Services: Results from the National Comorbidity Survey Replication. Archives of General Psychiatry. 2005;62(6):629–640. doi: 10.1001/archpsyc.62.6.629. [DOI] [PubMed] [Google Scholar]
- Wheaton Blair, Young Marisa, Montazer Shirin, Stuart-Lahman Katie. Social Stress in the Twenty-First Century. In: Aneshensel CS, Phelan JC, Bierman A, editors. Handbook of the Sociology of Mental Health. New York: Springer; 2013. [Google Scholar]
- Williams David R, Gonzalez Hector M, Neighbors Harold, Nesse Randolph, Abelson Jamie M, Sweetman Julie, Jackson James S. Prevalence and Distribution of Major Depressive Disorder in African American, Caribbean Blacks, and Non-Hispanic Whites: Resutls from the National Survey of American Life. Archives of General Psychiatry. 2007;64(3):305–315. doi: 10.1001/archpsyc.64.3.305. [DOI] [PubMed] [Google Scholar]
- Woodward Amanda Toler, Taylor Robert Joseph, Bullard Kai McKeever, Neighbors Harold W, Chatters Linda M, Jackson James S. Use of Professional and Informal Support by African Americans and Caribbean Blacks with Mental Disorders. Psychiatric Services. 2008;59(11):1292–1298. doi: 10.1176/appi.ps.59.11.1292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yokopenic Patricia A, Clark Virginia A, Aneshensel Carol S. Depression, Problem Recognition, and Professional Consultation. The Journal of Nervous and Mental Disease. 1983;171(1):15–23. doi: 10.1097/00005053-198301000-00004. [DOI] [PubMed] [Google Scholar]