Case Report
An 18-year-old female patient presented with lump hypogastrium since one month. Lump was initially small in size but increased progressively to attain the present size. She also complained of non-specific, non-localized abdominal pain which was chronic, dull aching in nature, and non-radiating. It was mild in severity with no aggravating or relieving factors. Bladder and bowel habits were normal. She had an irregular menstrual cycle of 30–60 days, 1–2 days duration and scanty flow. She had no history of previous medication or hospitalization. On examination, two discrete tender lumps, 7–9 cm in size and firm in consistency, and well-defined margins present in hypogastrium. Per vaginal examination could not be performed due to denial of consent due to virgin status. All laboratory investigations were within normal limit except hemoglobin which was 5.9 mg% and low T3 0.10 ng/ml (normal 0.7–2.0 ng/ml), low T4 1.2 µg/dl (normal 5.5–13.5 µg/dl), and high TSH 102 µlu/ml (normal 0.3–5.0 µlu/ml) levels. CA 125 and other tumor markers were within normal limits. Ultrasonography at the time of admission showed bilateral enlarged ovaries of size 15.22 × 8.26 cm(Rt. Ovary) and 11.82 × 6.24 cm (Lt. ovary) with multiple cysts of varying sizes in both ovaries, giving a classical ‘spoke wheel-like appearance.’ A diagnosis of bilateral ovarian cysts was made, and diagnostic laparoscopy was planned for further management. On pre-anesthetic cardiopulmonary evaluation, pericardial effusion was suspected. Hence, cardiology opinion was taken and subsequent echocardiogram revealed massive pericardial effusion. Then, on the basis of previous findings and echocardiogram put together, a diagnosis of spontaneous severe ovarian hyper stimulation syndrome (OHSS) was made.
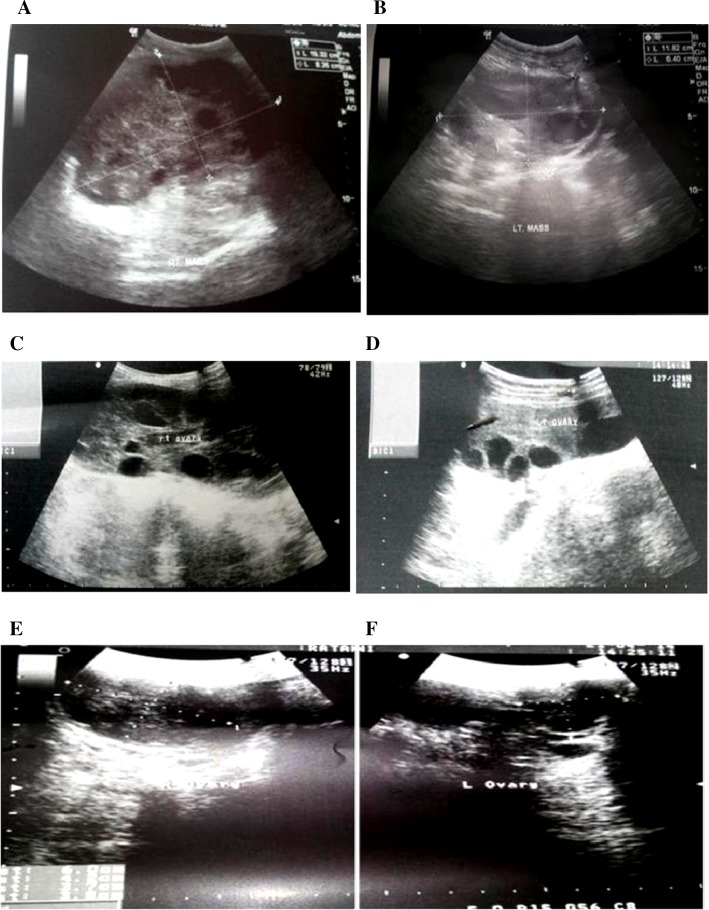
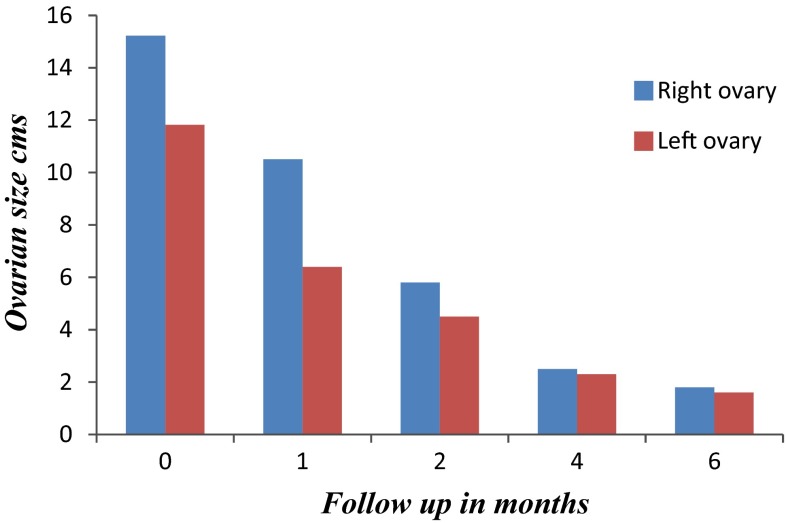
Patient was put on Tab Levothyroxine 100 µgm daily. Patient improved dramatically, and serial ultrasonogram at 1, 2, and 4 months revealed significant reduction in size of both ovaries as well as significant reduction in pericardial effusion. (Figure 1) Patient is still in close follow-up for last 2 months since writing of the case report that shows significant improvement in clinical and radiological profiles. (Graph 1)
Fig. 1.
Follow-up abdominal scan showing significant reduction in ovarian volume and cyst size. a, b on admission; c, d after 2 months; e, f after 4 months
Graph. 1.
Serial regression in ovarian size after levothyroxine therapy
Discussion
OHSS is an iatrogenic, serious complication of controlled ovarian hyper stimulation. Spontaneous OHSS might occur following high levels of human chorionic gonadotropin (HCG) in normal pregnancy, hypothyroidism, or FSH receptor mutation. [1] The pathophysiology of spontaneous OHSS associated with hypothyroidism is not studied well. The explanations given are: (a) Excessive estriol via the 16-hydroxylation pathway instead of the normal 2-hydroxylation that has been demonstrated in hypothyroid patients. Excessive gonadotropin release, due to decreased feedback regulation caused by substitution of estradiol by the less-potent estriol, would result in spontaneous OHSS in those subjects; [2] (b) High levels of thyroid-stimulating hormone can directly stimulate ovaries in women with hypothyroidism and can cause ovarian hyper stimulation; [3] and (c) Activating mutations of the FSHR gene cause ovarian hyper-responsiveness to circulating FSH or even cross-responsiveness of FSHR to hormones having a structure similar to FSH, such as HCG or TSH [4].
The underlying mechanism responsible for the clinical manifestations of OHSS appears to be an increase in capillary permeability of mesothelial surfaces. There is increasing evidence that certain vasoactive substances such as vascular endothelial growth factor (VEGF), cytokines (IL-2, IL-6, and IL-8), tumor necrosis factor-alpha (TNFα), and the ovarian renin–angiotensin system, which are activated by gonadotropin, can lead to increased vascular permeability and extravascular fluid accumulation in OHSS [5].
Symptoms of OHSS usually begin with a sensation of bloating, abdominal discomfort, nausea, vomiting, and diarrhea. As the disease progresses, accumulation of fluid in the third space leads to ascites, pleural and pericardial effusion, hypovolemia, oliguria, hemoconcentration, and electrolyte imbalance. OHSS is classified as mild, moderate, severe, and life threatening stages according to clinical and laboratory parameters (Table 1) [6]. Comparison of some similar cases has been given in (Table 2). Image findings can be similar on ultrasound, CT, and MR imaging; Typically, these findings show bilateral symmetrical enlargement of ovaries with multiple cysts of varying sizes, giving the classic spoke-wheel appearance, which is a characteristic of theca lutein cysts without solid components. It is important to diagnose and manage spontaneous OHSS timely to prevent the occurrence of severe complication. Early diagnosis and appropriate treatment will avoid further complications. The OHSS is managed according to the degree of severity. Patients with mild manifestations can be managed on outpatients’ basis. Treatment only requires oral analgesics and counseling regarding the sign and symptoms progressing illness.
Table 1.
Classification of OHSS (Mathur et al. 2007 [6])
| Mild OHSS | Moderate OHSS | Severe OHSS | Critical OHSS |
|---|---|---|---|
| 1 Abdominal bloating 2 Mild abdominal pain 3 Ovarian size usually <8 cm |
1 Moderate abdominal pain 2 Nausea ± vomiting 3 Ultrasound evidence of ascites 4 Ovarian size, usually 8–12 cm |
1 Clinical ascites (occasionally pleural effusion) 2 Oliguria 3 Hemoconcentration hematocrit (>45 %) 4 Hypoproteinemia 5 Ovarian size, usually >12 cm |
1 Tense ascites or large pleural effusion 2 Hematocrit (>55 %) 3 White-cell count >25,000 4 Oliguria/anuria 5 Thromboembolism 6 Acute respiratory distress syndrome |
Table 2.
Summary of similar case report in literature
| Reference | Age (years) | Hypothyroidism (mIU/l) | Pregnancy | Sonographic report | Follow-up |
|---|---|---|---|---|---|
| Taher et al. [3] | 22 | TSH > 100 | _ | Bilateral multilobulated ovarian mass with cystic component Rt: 90 × 120 Lt: 60 × 40 |
After 3 months: marked reduction |
| R Molaei Langroudi et al. [8] | 15 | TSH > 100 | _ | Enlarged ovaries with multiple ovarian cysts Rt: 150 × 75x62 Lt: 130 × 70x68 |
After 4 months: normal ovary size and regression of cysts |
| 14.5 | TSH = 72.5 | _ | Multiple large cysts with rupture of one cyst Rt: 110 × 65 Lt: 118 × 58 |
After 4 months: Normal | |
| Sultan et al. [9] | 12 | TSH = 1,310 | _ | Large cystic structure | After 3 months: resolution of cysts |
| Mousavi et al. [10] | 26 | TSH > 50 | _ | Bilateral multiseptated ovarian masses Rt: 69 × 63 × 96 Lt: 66 × 63 × 99 |
After 6 months: normal ovary size |
| Singh et al. (present study) | 18 | TSH > 100 | _ | Bilateral cystic enlargement of ovaries Rt: 152 × 82 Lt: 118 × 62 |
After 4 months: resolution of cysts |
Moderate manifestations can still usually be managed on an outpatient basis, but frequent monitoring and evaluation are essential. Serious illness requires hospitalization; patients require IV fluid management to address the acute need of volume expansion. Renal, pulmonary, and cardiac function must be carefully monitored. Ultrasound-guided paracentesis may be indicated for patients with ascites that causes pain, compromised pulmonary function, and renal function that does not improve with appropriate fluid management [7]. Patient with ruptured ovarian cyst with hemorrhage, torsion or ectopic pregnancy requires surgery.
Conclusion
Spontaneous OHSS due to hypothyroidism is a rare entity and it may present as lump abdomen due to bilateral ovarian enlargement in clinical practice. High index of suspicion and thorough investigations including endocrinal workup will lead to definitive diagnosis of OHSS. We recommend very high index of suspicion even in a virgin female as in our case. Once diagnosed erroneous surgical management can be deferred, wise medical management will treat the disease.
Acknowledgments
Compliance with Ethical Requirements and Conflict of Interest
Informed consent is taken before submission of manuscript. Amit singh, Kumkum singh, Radhagovind khandelwal, Prakash choudhary, and Vivek kumar Sharma declares that they have no conflict of interest.
Dr. Amit Singh
completed his M.B.B.S from Dr Sampurnanand Medical College, Jodhpur, 2005, and M.S in general surgery from Jawaharlal Nehru Medical College, Ajmer, 2011. Presently, he is Senior Resident at Jawahar Lal Nehru medical college, Ajmer. His keen area of interest is hepatobiliary and gastrointestinal surgery. He has many international and national publications. 
References
- 1.Debaere A, Smits G, De Leener A, et al. Understanding ovarian hyperstimulation syndrome. Endocrine. 2005;26:285–289. doi: 10.1385/ENDO:26:3:285. [DOI] [PubMed] [Google Scholar]
- 2.Rotmensch S, Scommegna A. Spontaneous ovarian hyperstimulation syndrome associated with hypothyroidism. Am J Obstet Gynecol. 1989;160:1220–1222. doi: 10.1016/0002-9378(89)90196-8. [DOI] [PubMed] [Google Scholar]
- 3.Taher BM, Ghariabeh RA, Jarrah NS, et al. Spontaneous ovarian hyperstimulation syndrome caused by hypothyroidism in an adult. Eur J Obstet Gynecol Reprod Biol. 2004;112:107–109. doi: 10.1016/S0301-2115(03)00283-5. [DOI] [PubMed] [Google Scholar]
- 4.Lussiana C, Guani B, Restagno G, et al. Ovarian hyper-stimulation syndrome after spontaneous conception. Gynecol Endocrinol. 2009;25:455–459. doi: 10.1080/09513590902898213. [DOI] [PubMed] [Google Scholar]
- 5.Rizk B, Aboulghar M, Smitz J, et al. The role of vascular endothelial growth factor and interleukins in the pathogenesis of severe ovarian hyperstimulation syndrome. Hum Reprod Update. 1997;3:255–266. doi: 10.1093/humupd/3.3.255. [DOI] [PubMed] [Google Scholar]
- 6.Mathur R, Kailasam C, Jenkins J. Review of the evidence base strategies to prevent ovarian hyperstimulation syndrome. Hum Fertil. 2007;10:75–85. doi: 10.1080/14647270601111239. [DOI] [PubMed] [Google Scholar]
- 7.Aboulghar MA, Mansour RT, Serour GI, et al. Ultrasonically guided vaginal aspiration of ascites in the treatment of severe ovarian hyperstimulation syndrome. Fertil Steril. 1990;53:933–935. doi: 10.1016/s0015-0282(16)53535-3. [DOI] [PubMed] [Google Scholar]
- 8.R Molaei Langroudi, Ghazanfari Amlashi F, Hedayati Emami MH. Ovarian cyst regression with levothyroxine in ovarian hyperstimulation syndrome associated with hypothyroidism. Endocrinology, diabetes and metabolism case reports ID: 13-0006; July 2013. DOI: 10.1530/EDM-13-0006. [DOI] [PMC free article] [PubMed]
- 9.Sultan A, Velaga MR, Fleet M, et al. Cullen’s sign and massive ovarian enlargement secondary to primary hypothyroidism in a patient with a normal FSH receptor. Arch Dis Child. 2006;91:509–510. doi: 10.1136/adc.2005.088443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Mousavi AS, Behtash N, Hasanzadeh M. Spontaneous ovarian hyperstimulation syndrome caused by hypothyroidism. Cancer Ther. 2005;3:397–400. [Google Scholar]