Abstract
Epstein-Barr virus (EBV) has been used as a paradigm for studying host–virus interactions, not only because of its importance as a human oncogenic virus associated with several malignancies including nasopharyngeal carcinoma (NPC) but also owing to its sophisticated strategies to subvert the host antiviral responses. An understanding of the interplay between EBV and NPC is critical for the development of EBV-targeted immunotherapy. Here, we summarize the current knowledge regarding the host immune responses and EBV immune evasion mechanisms in the context of NPC.
Keywords: adaptive immunity, EBV, immune evasion, innate immunity, NPC
INTRODUCTION
Epstein-Barr virus (EBV/HHV-4), which latently infects more than 90% of the world's adult human population, is associated with nasopharyngeal carcinoma (NPC).
In NPC patients, EBV typically exists in a type II latency program (particularly the undifferentiated or poorly differentiated types). Type II latency is characterized by the expression of a subset of latent genes, including EBV-determined nuclear antigen 1 (EBNA1), latent membrane proteins (LMP1, LMP2A, and LMP2B), and several EBV non-coding RNAs (primarily EBER1 and EBER2).1,2,3 In addition, BamHI-A rightward transcripts (BARTs) and BamHI-A rightward frame 1 (BARF1) of EBV are expressed abundantly and detected consistently in NPC.4,5,6
The detection of EBV in NPC and the prominent role of EBV in promoting tumor development support EBV as a potential therapeutic target for NPC. In fact, with the accumulation of knowledge regarding EBV oncogenicity and interactions between EBV and the host immune responses, immunological approaches, such as adoptive T-cell immunotherapy and vaccine-based strategies to induce EBV-specific T-cell responses, are emerging. In this review, we summarize the current understanding of how EBV stimulates the host immunity and the mechanisms exploited by EBV to circumvent immune responses in the context of NPC.
EVIDENCE FOR EBV CONTRIBUTING TO NPC
EBV factors detected in NPC patients
In the 1960s, antibodies against the EBV antigen were first identified in NPC patients,7 and subsequent studies reported higher levels of anti-EBV antibodies in NPC patients than in healthy controls.8,9 More direct and stronger evidence has been obtained regarding the detection of EBV DNA,10,11 protein antigens,2 and miRNA products1 in NPC patients. Viral DNA is considered a specific prognostic marker for both pre- and post-treatment NPC patients,11,12,13,14,15,16,17 regardless of prevalence in the region studied.18 Recent comprehensive profiles with methods that are more sensitive and specific (e.g., multiplexed stem-loop reverse transcription polymerase chain reaction19 and miRNA microarray20) identified panels of upregulated viral miRNAs in both NPC lesions and sera, some of which were shown to function as potential biomarkers for the diagnosis and prognosis of NPC.21
Mechanisms exploited by EBV products to promote NPC
A set of EBV latent genes have been identified that play an important role in NPC development, and multiple mechanisms including the restriction of cell homeostasis, the enhancement of cell mobility, and the induction of stem-like cancer cells were proposed.
EBNA1, which is expressed in all EBV-related tumors, is believed to be one of the most important viral proteins that promote NPC and is required for maintaining the viral latency in NPC.22,23 The introduction of EBNA1 enables EBV-negative NPC cells to grow more rapidly and to achieve increased metastasis in immunodeficiency mice.24 The potential mechanisms of EBNA1 function involve upregulation of tumor angiogenesis cytokines;25 degradation of promyelocytic leukemia (PML) protein, which is associated with p53 activation, DNA repair and cell apoptosis;26 inhibition of the anti-oncogenesis canonical p65 nuclear factor-κB (NF-κB) pathway;27 and induction of metastatic potential proteins28 as well as epithelial–mesenchymal transition (EMT).29
LMP1, another major viral oncoprotein, is closely associated with epithelial transformation30,31 and angiogenesis.32,33,34 LMP1 is detected primarily in preinvasive lesions, including dysplasia and carcinoma in situ, but not in late stage, suggesting that its expression may be an early, initiating event for NPC.35 LMP1 has been shown to promote tumor invasion and metastasis via remodeling actin filaments,36,37,38 inducing EMT39 and upregulating the expression of various matrix metalloproteinases (MMPs).40,41,42 In addition, LPM1 inhibits apoptosis43,44,45 and induces cancer stem/progenitor-like cells in nasopharyngeal epithelial cell lines.46,47
LMP2A and LMP2B are also expressed in NPC.2,48,49 LMP2B negatively regulates LMP2A activity by binding to this protein, preventing its phosphorylation without altering its cellular localization.50 LMP2A possesses the ability to induce stem-like cancer cells,47,51 EMT,51 and MMP expression52 in NPC. No direct evidence has been found for the role of LMP2B in NPC, although LMP2B itself may facilitate the spread and motility of epithelial cells.53
Emerging evidence has revealed that EBERs, BARTs and BARF1 also contribute directly to NPC development. EBERs accelerate the growth of NPC cells54 and confer resistance against apoptotic stress.55 BARF1 is not expressed during EBV infection of the NPC-derived EBV-negative cell lines HONE-1 and CNE-1; however, when infected by a recombinant EBV carrying the BARF1 gene under the control of the SV40 promoter, the infected NPC cells grew faster and were more resistant to apoptosis compared with wild-type EBV-infected cells.56 BARTs are very abundant EBV transcripts in NPC, contain several open reading frames, and are precursors for 22 miRNAs. Their roles in NPC (for instance, miR-BART157 and 358 in cell transformation, miR-BART159 and 560 in anti-apoptotic activity, and miR-BART761,62 and 963 in EMT) were recently reviewed64 (Table 1).
Table 1. A brief summary of mechanisms exploited by EBV latent products to promote NPC formation and development.
| General mechanisms | Viral products | Molecular mechanisms | References |
|---|---|---|---|
| Promotion of transformation and angiogenesis | EBNA1 | Mediates AP-1 to upregulate IL-8, VEGF, HIF-1α | 25 |
| LMP1 | Upregulates the phosphorylation of histone H3; inhibits the LKB1-AMPK pathway | 30,31 | |
| LMP1 | Mediates the NF-κB, MEK-ERK, and JNK pathways to induce endocan; mediates the degradation of prolyl hydroxylases 1 and 3 to upregulate HIF1-α | 32,33,34 | |
| EBERs | Upregulate IGF-1 | 54 | |
| BARF1 | Increases the cell growth rate | 56 | |
| miR-BART1 | Upregulates PSAT1 and PHGDH | 57 | |
| miR-BART3 | Inhibits DICE1 tumor suppressor | 58 | |
| Inhibition of apoptosis | EBNA1 | Disrupts PML nuclear bodies | 26 |
| LMP1 | Inhibits Chk1 to impair the G2 checkpoint; increases p53-mediated survival; mediates EGFR and STAT3 to induce cyclin D1 | 43,44,45 | |
| EBERs | Upregulate Bcl-2 and downregulate caspase-3 and PARP | 55 | |
| miR-BART1 | Inhibits LMP1-mediated apoptosis | 59 | |
| miR-BART5 | Inhibits PUMA | 60 | |
| Induction of stem cell-like phenotype | LMP1 | Induces the CSC/CPC-like phenotype and self-renewal; activates the hedgehog pathway to induce CD44v6, NGFR (p75NTR), and CXCR4 | 46,47 |
| LMP2A | Activates hedgehog to induce CD133 and CXCR4; induces stem-like cells and self-renewal | 47,51 | |
| Enhancement of cell mobility | EBNA1 | Upregulates stathmin 1, aspin, and Nm23-H1 | 28 |
| EBNA1 | Mediates TGF-β1/miR-200/ZEB to induce EMT | 29 | |
| LMP1 | Activates the PI3K/Akt pathway to promote actin stress-fiber formation; interacts with FGD4 to activate Cdc42; mediates the NF-κB pathway to upregulate TNFAIP2 | 36,37,38 | |
| LMP1 | Downregulates E-cadherin to induce EMT | 39 | |
| LMP1 | Upregulates MMPs (e.g., MMP1, 3 and 9) | 40,41,42 | |
| LMP2A | Induces EMT | 51 | |
| LMP2A | Mediates the ERK/Fra-1 pathway to induce MMP9 | 52 | |
| miR-BART7 | Enhances migration and invasion and inhibits PTEN to induce EMT | 61,62 | |
| miR-BART9 | Inhibits E-cadherin to induce EMT | 63 |
AMPK, AMP-activated protein kinase; AP-1, transcription activator-1; Bcl-2, B-cell lymphoma-2; CSC/CPC, cancer stem cells/cancer progenitor cells; CXCR4, C-X-C chemokine receptor type 4; DICE1, deleted in cancer 1; EGFR, epidermal growth factor receptor; HIF-1α, hypoxia-inducible factor 1α IGF-1, insulin-like growth factors-1; JNK, c-Jun N-terminal kinase; LMP1, AMPK-liver kinase B1-AMP-activated protein kinase; NGFR, nerve growth factor receptor; PARP, poly-ADP-ribose polymerase; PHGDH, phosphoglycerate dehydrogenase; PSAT1, phosphohydroxythreonine aminotransferase 1; PTEN, phosphatase and tensin homolog located on chromosome 10; PUMA, p53 upregulated modulator of apoptosis; STAT3, signal transducer and activator of transcription; TNFAIP2, tumor necrosis factor-alpha inducible protein-2; VEGF, vascular endothelial growth factor; MEK-ERK, mitogen-activated protein kinase-extracellular signal-regulated kinase.
THE INTERPLAY BETWEEN HOST INNATE IMMUNITY AND EBV
EBV mounts innate responses
One major characteristic of NPC is the presence of abundant infiltrating leukocytes in tumor stroma where various cell types, including neutrophils,65 natural killer (NK) cells,66,67 monocytes/macrophages, and dendritic cells (DCs),68,69,70 are detected and represent the first defense line for EBV infection. Nevertheless, the interaction between EBV and the host innate immunity system is not fully understood.
Based on flow cytometry, EBV was shown to bind to the neutrophil surface with its major envelope glycoprotein gp350 and subsequently stimulate the production of antiviral cytokines, including interleukin 1α (IL-1α), IL-1β,71 chemokines IL-8, and macrophage inflammatory protein (MIP)-1.72
Conventional DCs (cDCs) and plasmacytoid DCs (pDCs), the two major human DC subsets, sense EBV products through Toll-like receptors. When challenged with either live EBV virions or unmethylated EBV DNA, pDCs were found to produce interferon-α (IFN-α).73 In addition, treatment of cDCs with EBERs induces the production of IFN-β, IFN-γ, and tumor necrosis factors (TNFs).74 EBV-stimulated cDCs and pDCs can promote the cytotoxicity of NK cells through type I IFNs.75 NK cells are potential targets for EBV infection because the gp85-gp25-gp42 complex of EBV can directly combine with human leukocyte antigen (HLA) class II molecules on NK cells.76
EBV can activate monocytes77 and macrophages.78 dUTPase of EBV induces macrophages to express and secrete TNF-α, IL-1β, and IL-6 via the MyD88-dependent activation of NF-κB.78,79 For monocytes, in addition to the inflammatory cytokines that are also produced by activated macrophages,80 EBV also stimulates production of several chemokines, including IFN-inducible protein-10 (IP-10), MIP-1, monocyte chemotactic protein-1 (MCP-1), and IL-8 at the mRNA level.77
Evasion of innate immune responses
The establishment of life-long persistence in more than 90% of the worldwide adult human population clearly indicates that EBV has delicately evolved to evade the innate immune response. In addition to the above-mentioned latent genes, a portion of viral lytic antigens are frequently detected in NPC, probably due to EBV reactivation upon some poorly defined triggers.81,82 Recently, the mechanisms by which individual EBV products (including both lytic and latent genes) evade the innate immune response were reviewed.83 Here, we focus on summarizing two common and efficient strategies to circumvent the innate immune response in the NPC-induced modulation of phagocyte function and blockade of antiviral cytokines.
Modulation of phagocyte apoptosis and maturation
Subsequent to the finding that the binding of EBV to the surface of neutrophils induces inflammatory cytokine expression,71 Gosselin J et al. found that EBV penetrates neutrophils and localizes to their nuclei. After infecting neutrophils, EBV launches apoptosis by modulating the Fas/Fas ligand (L) pathway,84 as indicated by a significant increase in both membrane-bound Fas/Fas-L and soluble Fas-L. This study was the first to explain why EBV cannot establish robust infection in neutrophils. EBV also impairs the phagocytic activity of primary monocytes by inhibiting protein kinase C (PKC) activity.85,86 Monocyte apoptosis caused by EBV contact during DC development results in a reduction in mature DCs.87 This reduction may provide EBV with a time window for productive replication by temporarily delaying the onset of immune responses. In addition to the decrease in the number of pDCs during EBV infection, the maturation of pDCs is also compromised, as indicated by reduced secretion of TNF-α, which could partly facilitate pDC development.88 pDCs have a dual role in defending viral infection, by secreting a high level of type I IFNs to inhibit viral replication directly and by initiating and tuning the specific adaptive immunity. EBV infection undermines the ability of pDCs to mature, thereby preventing these cells from mounting antiviral T-cell responses.88
Blockade of antiviral cytokines
The apoptosis of innate effector cells results in a significant reduction in IFN production. In addition, certain EBV proteins and transcripts, such as EBERs and LMP2, can inhibit the type I IFN responses by disrupting IFN-stimulated transcription89,90 and by targeting IFN receptors for degradation.91
Inducing the innate immune cells to produce antagonistic factors to block the function of those antiviral cytokines demonstrates another strategy by which EBV eludes the immune responses. For example, in addition to IL-1α and IL-1β, EBV also initiates the production of their natural inhibitor IL-1 receptor antagonist (IL-1Ra).71,91,92 IL-1Ra competitively inhibits the binding of IL-1α and IL-1β to their receptors.93 Moreover, IL-Ra is secreted approximately 3200 and 610 times more than IL-1α and IL-1β, respectively, from EBV-stimulated neutrophils,92 indicating another effective mechanism by which EBV counteracts the host innate immune response.
In addition, EBV prevents the production of prostaglandin E2 (PGE2) by monocytes by inhibiting the expression of inducible cyclooxygenase 2 (COX-2), a critical enzyme in the PGE2 biosynthesis pathway. This inhibition of COX-2 may be a result of EBV interfering with the activation of the NF-κB pathway, which plays an important role in COX-2 induction in monocytes.94 NF-κB is also critical for TNF-α induction, and consequently, EBV suppresses TNF-α secretion from lipopolysaccharide-treated monocytes by 70%–90%.95 Because simple contact between EBV and monocytes upregulates TNF-α,80,96 inhibition of the NF-κB pathway after EBV replication in monocytes may be a mechanism by which the virus shuts down further TNF-α production. Additional evidence of this mechanism may be needed. First, TNF-α suppression by EBV was not observed at a basal expression level, and second, the exact mechanism of this suppression may be largely attributable to monocyte apoptosis upon EBV penetration.
THE INTERPLAY BETWEEN HOST ADAPTIVE IMMUNITY AND EBV
Antibodies detected during EBV infection
EBV-specific antibodies, primarily immunoglobulin G (IgG) and IgA, are detected in the sera of NPC patients. These antibodies recognize various EBV targets, including EBV structural antigens (e.g., viral capsid antigen-proteins VCA-p18 and VCA-p40,97 glycoproteins gp350/220,98 and gp7899), lytic antigens (e.g., Bam HI rightward reading frame 1 (BRLF1),82 Bam HI leftward reading frame 1 (BZLF1),100 and EBV-DNase101), and latent antigens (e.g., EBNA1 and LMPs102). One recent study that enrolled a relatively larger number of samples studied the humoral immune response to EBV-encoded tumor-associated proteins in NPC patients. The results indicated that there exists a stronger IgG antibody response to EBNA1 than that of LMP1, LMP2, and BARF1. Except for EBNA1, only low IgA titers against LMP1, LMP2, and BARF1 were present.102 The marginal immunogenicity of LMPs and BARF1 to humoral immune responses may be due to their intrinsic properties (for example, rapid and complete secretion of BARF1 leaves little protein within or on the surfaces of cells for detection103) and to their limited expression on the plasma membrane.
The presence of high titers of antibodies against EBV structural and early lytic antigens97,98,100,101,104 indicates the status of either sporadic reactivation from latency in malignant cells or new infection of naive cells within/surrounding the NPC tumor. However, antibodies may not be able to effectively block EBV infection because EBV has the capacity of spreading through cell–cell contact, which is an efficient mode of infecting the epithelium from reactivating B cells without releasing cell-free virions.105,106
Cellular responses to EBV infection
Cellular immunity is essential for controlling EBV during both primary and persistent phases. The complete view of EBV-specific cellular immunity in NPC patients remains to be elucidated, despite the fact that many novel technical approaches have been introduced to assess CD8+ T and CD4+ T-cell responses to EBV.107,108,109
Circulating EBV-specific cytotoxic lymphocytes (CTLs) can be detected in NPC patients,110,111 and EBV-specific memory CTL responses can be reactivated in vitro after those cells were extracted from blood.112 Nevertheless, the antigen-specific CD8+ CTLs against several consistently expressed viral lytic genes, including BZLF1, BRLF1, BamHI-M leftward frame 1, BamHI-M rightward frame 1, and BamHI-A leftward frame 2, are rarely found in NPC tumor lesions.113,114 In regard to latent antigens, Fogg MH et al. found that CTLs targeting the EBNA1 significantly decrease in EBV-associated NPC patients.115 It is possible that presentation of EBNA1 by major histocompatibility complex (MHC) I molecules is diminished in tumors; however, this interesting finding requires further validation. For the subdominant latent antigens (LMP1, LMP2, and BARF1), CTLs specific to these proteins can be detected in most of NPC patients.111,116,117,118
CD4+ T cells play a pivotal role in supporting the production of high affinity antibodies, maintaining the number and biological function of CTLs, and possessing cytotoxic activities.119 However, the understanding of CD4+ T-cell responses to EBV is less clear due to the small size of the CD4+ compartment because of a lack of detectable CD4+ T-cell expansion during EBV infection.120 Most knowledge concerning CD4+ responses to EBV has been built on observations from either healthy EBV carriers or in vitro experiments. For example, specific CD4+ T-cell clones or T-cell lines against EBV were evaluated by co-culture with autologous B-lymphoblastoid cell lines or DCs infected with recombinant vaccinia virus encoding individual lytic or latent proteins.109 Similar to the CD8+ T-cell response, a hierarchy of immunodominance of EBV antigens has been classified. EBNA1 and EBNA3 are the dominant targets, and LMPs and BARF1 are the subdominant targets.117,121,122 CD4+ T cells specific for EBNA1, LMPs, and BARF1 can be detected in NPC patients, albeit at low levels.111,117
Evasion of adaptive immune responses
Switching off immunodominant viral antigen expression
EBV has developed multiple strategies to evade cellular immune responses during its long-term co-evolution with the host. Like all other herpesviruses, the major strategy EBV uses for establishing and maintaining latency in the face of the cellular immunity, particularly the CD8+ T-cell response, is to switch off the expression of most viral genes, particularly the viral genes with strong immunogenicities or that present a “non-immunogenic” phenotype that makes them invisible to the immune system. For example, several vital latent factors with high immunodominance, such as the EBNA3 family and EBNA2,123 are consistently absent in NPC patients. Nevertheless, when co-cultured in vitro with autologous EBV-transformed lymphoblastoid cell lines, the virus-specific CTLs extracted from NPC patients sufficiently recognize antigens from the EBNA3 family.110
Impairment of the antigen-presenting HLA I or HLA II pathway
NPC cells are positive for both HLA class I and II molecules; thus, these cells may present viral peptides to be recognized by both CD8+ and CD4+ T cells. However, EBV impairs both HLA I and HLA II antigen presentation pathways to circumvent T-cell surveillance. Notably, NPC cells retain their antigen presentation capacity when they are cultured in vitro.110,124
EBNA1 is the primary target for the CD4+-, but not the CD8+-, T-cell response because ENBA1 is highly resistant to proteasomal digestion and thus is protected from being presented by MHC I molecules endogenously.125,126 This strategy is also utilized by latency-associated nuclear antigen 1, a homolog of EBNA1 in Kaposi sarcoma-associated herpes virus, to avoid being presented through the MHC class I pathway.127 Exogenously supplied EBNA1 can be presented by MHC class I molecules through a transporter associated with Ag processing (TAP)-independent pathway, whereas endogenously expressed EBNA1 can only be presented when the glycine-alanine repeat (GAr) domain of EBNA1 is deleted.128,129 Therefore, the GAr domain of EBNA1 is thought to control the presentation of endogenous EBNA1. However, further results have indicated that the GAr domain itself does not completely protect EBNA1 from presentation to CD8+ T cells.130,131,132
The expression of LMP1 in human cells dramatically enhances HLA I processing;133,134 however, LMP1 is a poor CD8+ T-cell target in vivo. Additionally, overall downregulation of HLA class I antigen presentation machinery (APM) was observed in NPC biopsies.135 This discrepancy may be explained by the finding that LMP1 induces c-myelocytomatosis (c-Myc), which has been shown to downregulate HLA class I APM, subsequently counteracting the stimulatory effect of LMP1.135 In addition, the first transmembrane domain of LMP1 is able to mediate self-aggregation to severely impair the cis-presentation of an LMP1-derived epitope,136 demonstrating another novel mechanism of immune evasion.
Among the detectable EBV lytic antigens in NPC patients, BZLF1, BamHI-G leftward frame 5 (BGLF5), and BamHI-N leftward frame 2a (BNLF2a) are able to dysregulate the cellular immune response via various mechanisms. BGLF5, a DNase/alkaline exonuclease (AE) gene, exerts a host shutoff function to block the synthesis of host HLA I, thereby limiting CD8+ T-cell recognition.137 In addition, this shutoff function of BGLF5 is also involved in repressing DNA repair, inducing genomic instability in human epithelial cells.138 BZLF1 inhibits MHC class II expression by suppressing the transcription of the transactivator class II, MHC, transactivator (CIITA),139 a critical transcriptional coactivator of MHC class II expression. BNLF2a specifically affects the presentation of immediate early and early proteins to HLA I molecules by inhibiting TAP and surface HLA I expression.140,141
Regulation of immuno-inhibitory biomolecules
IL-10 is a well-known cytokine with immune-suppressive function. An association between increased IL-10 secretion and a significantly decreased number of cytotoxic T cells was observed in EBV-positive NPCs.142 Both EBV structural proteins and EBV-encoded miRNAs are involved in IL-10 induction. LMP1 was the first identified viral protein responsible for IL-10 induction via the activation of p38/stress-activated protein kinase 2 (SAPK2).143 In addition, EBER1 and EBER2 were shown to be associated with enhanced IL-10 expression at the transcription level through a novel signaling pathway independent of an IFN-inducible protein kinase R (PKR).144
Decoy receptor 3 (DcR3), a recently identified molecule with immune inhibitory function, has the capacity to induce DC apoptosis via the formation of the death domain-containing receptor/death-inducing signaling complex.145 DcR3 also reduces MHC class II expression in tumor-associated macrophages.146 LMP1 was found to upregulate DcR3 expression via the NF-κB and phosphatidyl inositol 3-kinase (PI3K) signaling pathways.147 Because NPC-associated macrophages are positive for EBV,148 DcR3 may also be involved in immune evasion by EBV.
In addition, B7 homolog 1 (B7-H1), a T-cell inhibitory molecule, was upregulated during EBV infection of pDCs88 and NPC cell lines,149 and further studies are required to explore the role of B7-H1 in EBV immune evasion in NPCs.
Induction of T regulatory cell activation and T-cell anergy
T regulatory cells (Tregs), a subset of T cells with immune inhibitory functions, work in a cell-to-cell contact manner and secrete granzyme or cytokines such as IL-10 and transforming growth factor β (TGF-β).150,151,152 Tregs are consistently detected in the circulation and tumor microenvironment in EBV-positive NPC, where approximately 12% of tumor-infiltrating leucocytes (TILs) in NPC harbor a Treg phenotype (CD4+ CD25high forkhead box P3+).153 LMP1 dominantly induces Tregs to secrete IL-10, which suppresses the proliferation of mitogen or the withdrawal of Ag-stimulated T-effector cells and their release of IFN-γ.154 LALLFWL peptides of LMP1 show strong and direct inhibition of T-cell proliferation and NK cytotoxicity. This T-cell anergy is most likely attributable to the enhanced expression of IL-10 and TGF-β, resembling Treg responses.155 Tregs are also involved in the immune evasion of EBNA1 and LMP2 because Treg depletion restores EBNA1- and LMP2-specific CD8+ T-cell responses, as well as the immune control of EBV-infected cells in vitro156 (Table 2).
Table 2. Strategies of cellular response evasion exploited by individual EBV antigens detected in NPC.
| Strategies | Viral antigens | Mechanisms | References |
|---|---|---|---|
| Switch off immunodominant viral antigens | e.g., EBNA2, the EBNA3 family | Not well-known, epigenetic modification? | 123 |
| Impair the HLA I or HLA II pathway | EBNA1 | Blocks proteasomal HLA II pathway degradation via the GAr domain | 128,129 |
| LMP1 | Induces c-Myc via IL6 and the JAK3/STAT3 pathway | 135 | |
| LMP1 | Self-aggregation via its first transmembrane domain | 136 | |
| BZLF1 (Zta) | Suppresses the class II transactivator CIITA | 139 | |
| BGLF5 | Directly shuts off host HLA I synthesis | 137 | |
| BNLF2a | Inhibits TAP and surface HLA I expression | 138,139 | |
| Upregulate immune-inhibitory molecules | LMP1 | Induces IL-10 via p38/SAPK2 | 143 |
| EBERs | Induce IL-10 via PKR-independent pathways | 144 | |
| LMP1 | Induces DcR3 via NF-κB and PI3K pathways | 147 | |
| EBV (specific antigen, not yet determined) | Induces B7-H1 and ICOS-L | 88 | |
| Recruit Tregs and induce T-cell anergy | LMP1 | Induces Tregs via chemokines (e.g., IL-10 and TGF-β) | 155 |
| LMP1 | Directly inhibits T-cell proliferation | 156 |
ICOS-L, inducible costimulatory ligand; JAK3, Janus kinase 3.
CONCLUDING REMARKS
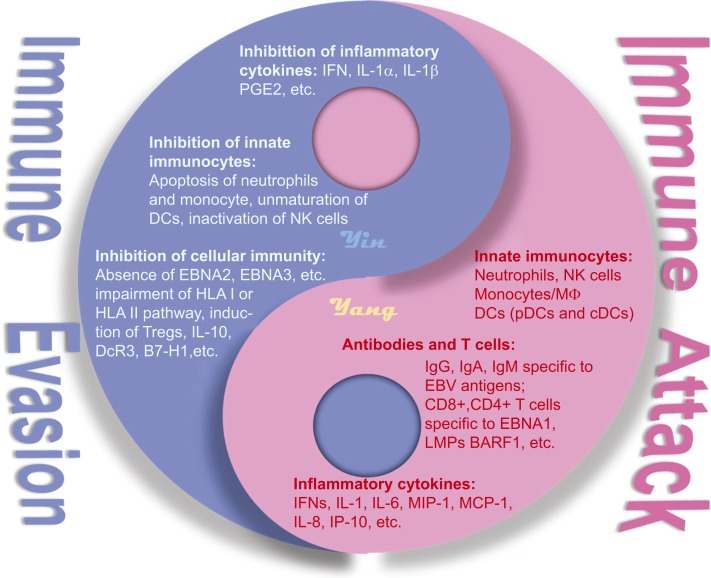
NPC patients maintain efficient immune functions, including innate and adaptive immunities, to address EBV infection. However, this ancient virus has evolved multiple elaborate strategies to counteract and evade the host immunity, leading to its high prevalence among the human population. Seemingly, symbiosis is established between EBV and NPC that EBV facilitates NPC development by promoting the growth of EBV-infected cells and by preventing apoptosis.157,158 EBV also counteracts the host immunity by modulating numerous cellular signaling pathways,159 and an increased number of cancer cells provides more potential neo-hosts for EBV (Figure 1).
Figure 1.
The interaction between EBV and the host immune system in NPC patients. NPC patients preserve efficient anti-EBV immunity while EBV has evolved multiple evasion strategies. A type of balance has been established for this interaction. The anti-EBV immune responses represent the “yang” or “positive” side of the Taiji diagram, and the EBV evasion mechanisms represent the “yin” or “negative” side.
The limited knowledge regarding the virus–host interaction in the NPC environment and in systemic immune responses contributes to the failure or low efficacy of most EBV-targeted immunotherapies. More importantly, selection pressure-driven evolution constantly stimulates the emergence of EBV variants,160,161 which may be more oncogenic and less immunogenic than the parental strain. For instance, a recent study identified an EBV variant from NPC with unusually high tropism for epithelial cells but low tropism for B cells,162 suggesting the existence of EBV variants with increased NPC risk.
To date, the induction of an EBV antigen-specific T-cell response (primarily CD8+ T cells) in patients with vaccines and adoptive T-cell therapy are the two most common strategies for the immunological treatment of EBV-associated cancers. Because targeting only one specific antigen led to limited tumor regression in NPC patients,163,164,165,166 vaccines composed of multiple EBV antigens to activate T-cell responses that are more potent has emerged as a novel strategy. In this respect, two different teams constructed two recombinant viruses. The recombinant virus called Ad-SAVINE incorporates peptide sets from EBNA1, LMP1, and LMP2,167 and the other recombinant virus, called MVA-EL, contains an EBNA1/LMP2 fusion protein.168 Phase I trials in NPC patients showed that both of these vaccinia viruses activate CD4+ and CD8+ T-cell responses; encouraging clinical progress with full tolerance has been made.168,169,170
However, many questions regarding host immunity and EBV remain to be addressed for the development of EBV-targeted therapy. For instance, the immunodominance hierarchy of individual viral antigens (particularly for EBV-encoding RNAs) and the crosstalk among multiple signaling pathways activated by EBV should be addressed. New technologies (for example, a molecular-based tag linkage method our lab developed that enables haplotype phasing greater accuracy and sensitivity for viral quasispecies determination171) with higher sensitivity and precision to examine viral quasispecies in the NPC environment are required to monitor viral evolution. Exploring novel cellular factors or chemical substances that can reactivate EBV from latency will provide a promising strategy for treating EBV-related tumors by inducing cell lysis through viral reactivation. Greater attention should be given to the local suppression of EBV-specific immunity because immunosuppression contributes greatly to NPC development.
Acknowledgments
This work was supported by grants from National Key Basic Research Program of China (2011CB504803 to Ren Sun, 2011CB504305 to Tingting Wu), the National Natural Science Foundation of China (81270063 to Jing Qian), the Natural Science Foundation of Zhejiang Province (LY12H19008 to Jing Qian), the Qianjiang Talent Project of Zhejiang Province (2013R10034 to Jing Qian).
References
- Young LS, Dawson CW, Clark D, et al. Epstein-Barr virus gene expression in nasopharyngeal carcinoma. J Gen Virol. 1988;69 (Pt 5):1051–1065. doi: 10.1099/0022-1317-69-5-1051. [DOI] [PubMed] [Google Scholar]
- Brooks L, Yao QY, Rickinson AB, et al. Epstein-Barr virus latent gene transcription in nasopharyngeal carcinoma cells: coexpression of EBNA1, LMP1, and LMP2 transcripts. J Virol. 1992;66:2689–2697. doi: 10.1128/jvi.66.5.2689-2697.1992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sam CK, Brooks LA, Niedobitek G, et al. Analysis of Epstein-Barr virus infection in nasopharyngeal biopsies from a group at high risk of nasopharyngeal carcinoma. Int J Cancer. 1993;53:957–962. doi: 10.1002/ijc.2910530616. [DOI] [PubMed] [Google Scholar]
- Gilligan KJ, Rajadurai P, Lin JC, et al. Expression of the Epstein-Barr virus BamHI A fragment in nasopharyngeal carcinoma: evidence for a viral protein expressed in vivo. J Virol. 1991;65:6252–6259. doi: 10.1128/jvi.65.11.6252-6259.1991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Decaussin G, Sbih-Lammali F, de Turenne-Tessier M, et al. Expression of BARF1 gene encoded by Epstein-Barr virus in nasopharyngeal carcinoma biopsies. Cancer Res. 2000;60:5584–5588. [PubMed] [Google Scholar]
- Seto E, Yang L, Middeldorp J, et al. Epstein-Barr virus (EBV)-encoded BARF1 gene is expressed in nasopharyngeal carcinoma and EBV-associated gastric carcinoma tissues in the absence of lytic gene expression. J Med Virol. 2005;76:82–88. doi: 10.1002/jmv.20327. [DOI] [PubMed] [Google Scholar]
- Old LJ, Boyse EA, Oettgen HF, et al. Precipitating antibody in human serum to an antigen present in cultured burkitt's lymphoma cells. Proc Natl Acad Sci USA. 1966;56:1699–1704. doi: 10.1073/pnas.56.6.1699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Henle W, Henle G, Ho HC, et al. Antibodies to Epstein-Barr virus in nasopharyngeal carcinoma, other head and neck neoplasms, and control groups. J Natl Cancer Inst. 1970;44:225–231. [PubMed] [Google Scholar]
- Henle G, Henle W. Epstein-Barr virus-specific IgA serum antibodies as an outstanding feature of nasopharyngeal carcinoma. Int J Cancer. 1976;17:1–7. doi: 10.1002/ijc.2910170102. [DOI] [PubMed] [Google Scholar]
- Raab-Traub N, Flynn K. The structure of the termini of the Epstein-Barr virus as a marker of clonal cellular proliferation. Cell. 1986;47:883–889. doi: 10.1016/0092-8674(86)90803-2. [DOI] [PubMed] [Google Scholar]
- Lin JC, Wang WY, Chen KY, et al. Quantification of plasma Epstein-Barr virus DNA in patients with advanced nasopharyngeal carcinoma. N Engl J Med. 2004;350:2461–2470. doi: 10.1056/NEJMoa032260. [DOI] [PubMed] [Google Scholar]
- Lo YM, Chan LY, Chan AT, et al. Quantitative and temporal correlation between circulating cell-free Epstein-Barr virus DNA and tumor recurrence in nasopharyngeal carcinoma. Cancer Res. 1999;59:5452–5455. [PubMed] [Google Scholar]
- Chan AT, Lo YM, Zee B, et al. Plasma Epstein-Barr virus DNA and residual disease after radiotherapy for undifferentiated nasopharyngeal carcinoma. J Natl Cancer Inst. 2002;94:1614–1619. doi: 10.1093/jnci/94.21.1614. [DOI] [PubMed] [Google Scholar]
- Leung SF, Chan AT, Zee B, et al. Pretherapy quantitative measurement of circulating Epstein-Barr virus DNA is predictive of posttherapy distant failure in patients with early-stage nasopharyngeal carcinoma of undifferentiated type. Cancer. 2003;98:288–291. doi: 10.1002/cncr.11496. [DOI] [PubMed] [Google Scholar]
- Wang WY, Twu CW, Chen HH, et al. Plasma EBV DNA clearance rate as a novel prognostic marker for metastatic/recurrent nasopharyngeal carcinoma. Clin Cancer Res. 2010;16:1016–1024. doi: 10.1158/1078-0432.CCR-09-2796. [DOI] [PubMed] [Google Scholar]
- An X, Wang FH, Ding PR, et al. Plasma Epstein-Barr virus DNA level strongly predicts survival in metastatic/recurrent nasopharyngeal carcinoma treated with palliative chemotherapy. Cancer. 2011;117:3750–3757. doi: 10.1002/cncr.25932. [DOI] [PubMed] [Google Scholar]
- Wang WY, Twu CW, Lin WY, et al. Plasma Epstein-Barr virus DNA screening followed by (1)(8)F-fluoro-2-deoxy-D-glucose positron emission tomography in detecting posttreatment failures of nasopharyngeal carcinoma. Cancer. 2011;117:4452–4459. doi: 10.1002/cncr.26069. [DOI] [PubMed] [Google Scholar]
- Desgranges C, de-The G, Wolf H, et al. Further studies on the detection of the Epstein-Barr virus DNA in nasopharyngeal carcinoma biopsies from different parts of the world. IARC Sci Publ. 1975;11 (Pt 2):191–193. [PubMed] [Google Scholar]
- Cosmopoulos K, Pegtel M, Hawkins J, et al. Comprehensive profiling of Epstein-Barr virus microRNAs in nasopharyngeal carcinoma. J Virol. 2009;83:2357–2367. doi: 10.1128/JVI.02104-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wong AM, Kong KL, Tsang JW, et al. Profiling of Epstein-Barr virus-encoded microRNAs in nasopharyngeal carcinoma reveals potential biomarkers and oncomirs. Cancer. 2012;118:698–710. doi: 10.1002/cncr.26309. [DOI] [PubMed] [Google Scholar]
- Zhang G, Zong J, Lin S, et al. Circulating Epstein-Barr virus microRNAs miR-BART7 and miR-BART13 as biomarkers for nasopharyngeal carcinoma diagnosis and treatment. Int J Cancer. 2015;136:E301–E312. doi: 10.1002/ijc.29206. [DOI] [PubMed] [Google Scholar]
- Sivachandran N, Thawe NN, Frappier L. Epstein-Barr virus nuclear antigen 1 replication and segregation functions in nasopharyngeal carcinoma cell lines. J Virol. 2011;85:10425–10430. doi: 10.1128/JVI.05293-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mansouri S, Pan Q, Blencowe BJ, et al. Epstein-Barr virus EBNA1 protein regulates viral latency through effects on let-7 microRNA and dicer. J Virol. 2014;88:11166–11177. doi: 10.1128/JVI.01785-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sheu LF, Chen A, Meng CL, et al. Enhanced malignant progression of nasopharyngeal carcinoma cells mediated by the expression of Epstein-Barr nuclear antigen 1 in vivo. J Pathol. 1996;180:243–248. doi: 10.1002/(SICI)1096-9896(199611)180:3<243::AID-PATH655>3.0.CO;2-7. [DOI] [PubMed] [Google Scholar]
- O'Neil JD, Owen TJ, Wood VH, et al. Epstein-Barr virus-encoded EBNA1 modulates the AP-1 transcription factor pathway in nasopharyngeal carcinoma cells and enhances angiogenesis in vitro. J Gen Virol. 2008;89:2833–2842. doi: 10.1099/vir.0.2008/003392-0. [DOI] [PubMed] [Google Scholar]
- Sivachandran N, Sarkari F, Frappier L. Epstein-Barr nuclear antigen 1 contributes to nasopharyngeal carcinoma through disruption of PML nuclear bodies. PLoS Pathog. 2008;4:e1000170. doi: 10.1371/journal.ppat.1000170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Valentine R, Dawson CW, Hu C, et al. Epstein-Barr virus-encoded EBNA1 inhibits the canonical NF-kappaB pathway in carcinoma cells by inhibiting IKK phosphorylation. Mol Cancer. 2010;9:1. doi: 10.1186/1476-4598-9-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cao JY, Mansouri S, Frappier L. Changes in the nasopharyngeal carcinoma nuclear proteome induced by the EBNA1 protein of Epstein-Barr virus reveal potential roles for EBNA1 in metastasis and oxidative stress responses. J Virol. 2012;86:382–394. doi: 10.1128/JVI.05648-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang L, Tian WD, Xu X, et al. Epstein-Barr virus nuclear antigen 1 (EBNA1) protein induction of epithelial-mesenchymal transition in nasopharyngeal carcinoma cells. Cancer. 2014;120:363–372. doi: 10.1002/cncr.28418. [DOI] [PubMed] [Google Scholar]
- Li B, Huang G, Zhang X, et al. Increased phosphorylation of histone H3 at serine 10 is involved in Epstein-Barr virus latent membrane protein-1-induced carcinogenesis of nasopharyngeal carcinoma. BMC Cancer. 2013;13:124. doi: 10.1186/1471-2407-13-124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lo AK, Lo KW, Ko CW, et al. Inhibition of the LKB1-AMPK pathway by the Epstein-Barr virus-encoded LMP1 promotes proliferation and transformation of human nasopharyngeal epithelial cells. J Pathol. 2013;230:336–346. doi: 10.1002/path.4201. [DOI] [PubMed] [Google Scholar]
- Yu PH, Chou SF, Chen CL, et al. Upregulation of endocan by Epstein-Barr virus latent membrane protein 1 and its clinical significance in nasopharyngeal carcinoma. PLoS One. 2013;8:e82254. doi: 10.1371/journal.pone.0082254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kondo S, Seo SY, Yoshizaki T, et al. EBV latent membrane protein 1 up-regulates hypoxia-inducible factor 1alpha through Siah1-mediated down-regulation of prolyl hydroxylases 1 and 3 in nasopharyngeal epithelial cells. Cancer Res. 2006;66:9870–9877. doi: 10.1158/0008-5472.CAN-06-1679. [DOI] [PubMed] [Google Scholar]
- Aga M, Bentz GL, Raffa S, et al. Exosomal HIF1alpha supports invasive potential of nasopharyngeal carcinoma-associated LMP1-positive exosomes. Oncogene. 2014;33:4613–4622. doi: 10.1038/onc.2014.66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pathmanathan R, Prasad U, Sadler R, et al. Clonal proliferations of cells infected with Epstein-Barr virus in preinvasive lesions related to nasopharyngeal carcinoma. N Engl J Med. 1995;333:693–698. doi: 10.1056/NEJM199509143331103. [DOI] [PubMed] [Google Scholar]
- Dawson CW, Tramountanis G, Eliopoulos AG, et al. Epstein-Barr virus latent membrane protein 1 (LMP1) activates the phosphatidylinositol 3-kinase/Akt pathway to promote cell survival and induce actin filament remodeling. J Biol Chem. 2003;278:3694–3704. doi: 10.1074/jbc.M209840200. [DOI] [PubMed] [Google Scholar]
- Liu HP, Chen CC, Wu CC, et al. Epstein-Barr virus-encoded LMP1 interacts with FGD4 to activate Cdc42 and thereby promote migration of nasopharyngeal carcinoma cells. PLoS Pathog. 2012;8:e1002690. doi: 10.1371/journal.ppat.1002690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen CC, Liu HP, Chao M, et al. NF-kappaB-mediated transcriptional upregulation of TNFAIP2 by the Epstein-Barr virus oncoprotein, LMP1, promotes cell motility in nasopharyngeal carcinoma. Oncogene. 2014;33:3648–3659. doi: 10.1038/onc.2013.345. [DOI] [PubMed] [Google Scholar]
- Tsai CN, Tsai CL, Tse KP, et al. The Epstein-Barr virus oncogene product, latent membrane protein 1, induces the downregulation of E-cadherin gene expression via activation of DNA methyltransferases. Proc Natl Acad Sci USA. 2002;99:10084–10089. doi: 10.1073/pnas.152059399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yoshizaki T, Sato H, Furukawa M, et al. The expression of matrix metalloproteinase 9 is enhanced by Epstein-Barr virus latent membrane protein 1. Proc Natl Acad Sci USA. 1998;95:3621–3626. doi: 10.1073/pnas.95.7.3621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Horikawa T, Yoshizaki T, Sheen TS, et al. Association of latent membrane protein 1 and matrix metalloproteinase 9 with metastasis in nasopharyngeal carcinoma. Cancer. 2000;89:715–723. doi: 10.1002/1097-0142(20000815)89:4<715::aid-cncr1>3.0.co;2-9. [DOI] [PubMed] [Google Scholar]
- Lee DC, Chua DT, Wei WI, et al. Induction of matrix metalloproteinases by Epstein-Barr virus latent membrane protein 1 isolated from nasopharyngeal carcinoma. Biomed Pharmacother. 2007;61:520–526. doi: 10.1016/j.biopha.2007.08.007. [DOI] [PubMed] [Google Scholar]
- Deng W, Pang PS, Tsang CM, et al. Epstein-Barr virus-encoded latent membrane protein 1 impairs G2 checkpoint in human nasopharyngeal epithelial cells through defective Chk1 activation. PLoS One. 2012;7:e39095. doi: 10.1371/journal.pone.0039095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guo L, Tang M, Yang L, et al. Epstein-Barr virus oncoprotein LMP1 mediates survivin upregulation by p53 contributing to G1/S cell cycle progression in nasopharyngeal carcinoma. Int J Mol Med. 2012;29:574–580. doi: 10.3892/ijmm.2012.889. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xu Y, Shi Y, Yuan Q, et al. Epstein-Barr Virus encoded LMP1 regulates cyclin D1 promoter activity by nuclear EGFR and STAT3 in CNE1 cells. J Exp Clin Cancer Res. 2013;32:90. doi: 10.1186/1756-9966-32-90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kondo S, Wakisaka N, Muramatsu M, et al. Epstein-Barr virus latent membrane protein 1 induces cancer stem/progenitor-like cells in nasopharyngeal epithelial cell lines. J Virol. 2011;85:11255–11264. doi: 10.1128/JVI.00188-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Port RJ, Pinheiro-Maia S, Hu C, et al. Epstein-Barr virus induction of the Hedgehog signalling pathway imposes a stem cell phenotype on human epithelial cells. J Pathol. 2013;231:367–377. doi: 10.1002/path.4245. [DOI] [PubMed] [Google Scholar]
- Busson P, McCoy R, Sadler R, et al. Consistent transcription of the Epstein-Barr virus LMP2 gene in nasopharyngeal carcinoma. J Virol. 1992;66:3257–3262. doi: 10.1128/jvi.66.5.3257-3262.1992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heussinger N, Buttner M, Ott G, et al. Expression of the Epstein-Barr virus (EBV)-encoded latent membrane protein 2A (LMP2A) in EBV-associated nasopharyngeal carcinoma. J Pathol. 2004;203:696–699. doi: 10.1002/path.1569. [DOI] [PubMed] [Google Scholar]
- Rovedo M, Longnecker R. Epstein-barr virus latent membrane protein 2B (LMP2B) modulates LMP2A activity. J Virol. 2007;81:84–94. doi: 10.1128/JVI.01302-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kong QL, Hu LJ, Cao JY, et al. Epstein-Barr virus-encoded LMP2A induces an epithelial-mesenchymal transition and increases the number of side population stem-like cancer cells in nasopharyngeal carcinoma. PLoS Pathog. 2010;6:e1000940. doi: 10.1371/journal.ppat.1000940. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lan YY, Hsiao JR, Chang KC, et al. Epstein-Barr virus latent membrane protein 2A promotes invasion of nasopharyngeal carcinoma cells through ERK/Fra-1-mediated induction of matrix metalloproteinase 9. J Virol. 2012;86:6656–6667. doi: 10.1128/JVI.00174-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Allen MD, Young LS, Dawson CW. The Epstein-Barr virus-encoded LMP2A and LMP2B proteins promote epithelial cell spreading and motility. J Virol. 2005;79:1789–1802. doi: 10.1128/JVI.79.3.1789-1802.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Iwakiri D, Sheen TS, Chen JY, et al. Epstein-Barr virus-encoded small RNA induces insulin-like growth factor 1 and supports growth of nasopharyngeal carcinoma-derived cell lines. Oncogene. 2005;24:1767–1773. doi: 10.1038/sj.onc.1208357. [DOI] [PubMed] [Google Scholar]
- Wong HL, Wang X, Chang RC, et al. Stable expression of EBERs in immortalized nasopharyngeal epithelial cells confers resistance to apoptotic stress. Mol Carcinog. 2005;44:92–101. doi: 10.1002/mc.20133. [DOI] [PubMed] [Google Scholar]
- Seto E, Ooka T, Middeldorp J, et al. Reconstitution of nasopharyngeal carcinoma-type EBV infection induces tumorigenicity. Cancer Res. 2008;68:1030–1036. doi: 10.1158/0008-5472.CAN-07-5252. [DOI] [PubMed] [Google Scholar]
- Ye Y, Zhou Y, Zhang L, et al. EBV-miR-BART1 is involved in regulating metabolism-associated genes in nasopharyngeal carcinoma. Biochem Biophys Res Commun. 2013;436:19–24. doi: 10.1016/j.bbrc.2013.05.008. [DOI] [PubMed] [Google Scholar]
- Lei T, Yuen KS, Xu R, et al. Targeting of DICE1 tumor suppressor by Epstein-Barr virus-encoded miR-BART3* microRNA in nasopharyngeal carcinoma. Int J Cancer. 2013;133:79–87. doi: 10.1002/ijc.28007. [DOI] [PubMed] [Google Scholar]
- Lo AK, To KF, Lo KW, et al. Modulation of LMP1 protein expression by EBV-encoded microRNAs. Proc Natl Acad Sci USA. 2007;104:16164–16169. doi: 10.1073/pnas.0702896104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Choy EY, Siu KL, Kok KH, et al. An Epstein-Barr virus-encoded microRNA targets PUMA to promote host cell survival. J Exp Med. 2008;205:2551–2560. doi: 10.1084/jem.20072581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chan JY, Gao W, Ho WK, et al. Overexpression of Epstein-Barr virus-encoded microRNA-BART7 in undifferentiated nasopharyngeal carcinoma. Anticancer Res. 2012;32:3201–3210. [PubMed] [Google Scholar]
- Cai LM, Lyu XM, Luo WR, et al. EBV-miR-BART7-3p promotes the EMT and metastasis of nasopharyngeal carcinoma cells by suppressing the tumor suppressor PTEN Oncogene27 October2014. doi 10.1038/onc.2014.341 [DOI] [PubMed]
- Hsu CY, Yi YH, Chang KP, et al. The Epstein-Barr virus-encoded microRNA MiR-BART9 promotes tumor metastasis by targeting E-cadherin in nasopharyngeal carcinoma. PLoS Pathog. 2014;10:e1003974. doi: 10.1371/journal.ppat.1003974. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xie YJ, Long ZF, He XS. Involvement of EBV-encoded BART-miRNAs and dysregulated cellular miRNAs in nasopharyngeal carcinoma genesis. Asian Pac J Cancer Prev. 2013;14:5637–5644. doi: 10.7314/apjcp.2013.14.10.5637. [DOI] [PubMed] [Google Scholar]
- Chen LC, Wang LJ, Tsang NM, et al. Tumour inflammasome-derived IL-1beta recruits neutrophils and improves local recurrence-free survival in EBV-induced nasopharyngeal carcinoma. EMBO Mol Med. 2012;4:1276–1293. doi: 10.1002/emmm.201201569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ferradini L, Miescher S, Stoeck M, et al. Cytotoxic potential despite impaired activation pathways in T lymphocytes infiltrating nasopharyngeal carcinoma. Int J Cancer. 1991;47:362–370. doi: 10.1002/ijc.2910470309. [DOI] [PubMed] [Google Scholar]
- Hu H, Tang KF, Chua YN, et al. Expression of interleukin-18 by nasopharyngeal carcinoma cells: a factor that possibly initiates the massive leukocyte infiltration. Hum Pathol. 2004;35:722–728. doi: 10.1016/j.humpath.2004.01.026. [DOI] [PubMed] [Google Scholar]
- Giannini A, Bianchi S, Messerini L, et al. Prognostic significance of accessory cells and lymphocytes in nasopharyngeal carcinoma. Pathol Res Pract. 1991;187:496–502. doi: 10.1016/S0344-0338(11)80013-0. [DOI] [PubMed] [Google Scholar]
- Zong YS, Zhang CQ, Zhang F, et al. Infiltrating lymphocytes and accessory cells in nasopharyngeal carcinoma. Jpn J Cancer Res. 1993;84:900–905. doi: 10.1111/j.1349-7006.1993.tb02064.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tang KF, Tan SY, Chan SH, et al. A distinct expression of CC chemokines by macrophages in nasopharyngeal carcinoma: implication for the intense tumor infiltration by T lymphocytes and macrophages. Hum Pathol. 2001;32:42–49. doi: 10.1053/hupa.2001.20886. [DOI] [PubMed] [Google Scholar]
- Beaulieu AD, Paquin R, Gosselin J. Epstein-Barr virus modulates de novo protein synthesis in human neutrophils. Blood. 1995;86:2789–2798. [PubMed] [Google Scholar]
- McColl SR, Roberge CJ, Larochelle B, et al. EBV induces the production and release of IL-8 and macrophage inflammatory protein-1 alpha in human neutrophils. J Immunol. 1997;159:6164–6168. [PubMed] [Google Scholar]
- Fiola S, Gosselin D, Takada K, et al. TLR9 contributes to the recognition of EBV by primary monocytes and plasmacytoid dendritic cells. J Immunol. 2010;185:3620–3631. doi: 10.4049/jimmunol.0903736. [DOI] [PubMed] [Google Scholar]
- Iwakiri D, Zhou L, Samanta M, et al. Epstein-Barr virus (EBV)-encoded small RNA is released from EBV-infected cells and activates signaling from Toll-like receptor 3. J Exp Med. 2009;206:2091–2099. doi: 10.1084/jem.20081761. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Granucci F, Zanoni I, Pavelka N, et al. A contribution of mouse dendritic cell-derived IL-2 for NK cell activation. J Exp Med. 2004;200:287–295. doi: 10.1084/jem.20040370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Isobe Y, Sugimoto K, Yang L, et al. Epstein-Barr virus infection of human natural killer cell lines and peripheral blood natural killer cells. Cancer Res. 2004;64:2167–2174. doi: 10.1158/0008-5472.can-03-1562. [DOI] [PubMed] [Google Scholar]
- Gaudreault E, Fiola S, Olivier M, et al. Epstein-Barr virus induces MCP-1 secretion by human monocytes via TLR2. J Virol. 2007;81:8016–8024. doi: 10.1128/JVI.00403-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ariza ME, Glaser R, Kaumaya PT, et al. The EBV-encoded dUTPase activates NF-kappa B through the TLR2 and MyD88-dependent signaling pathway. J Immunol. 2009;182:851–859. doi: 10.4049/jimmunol.182.2.851. [DOI] [PubMed] [Google Scholar]
- Glaser R, Litsky ML, Padgett DA, et al. EBV-encoded dUTPase induces immune dysregulation: Implications for the pathophysiology of EBV-associated disease. Virology. 2006;346:205–218. doi: 10.1016/j.virol.2005.10.034. [DOI] [PubMed] [Google Scholar]
- Gosselin J, Flamand L, D′Addario M, et al. Infection of peripheral blood mononuclear cells by herpes simplex and Epstein-Barr viruses. Differential induction of interleukin 6 and tumor necrosis factor-alpha. J Clin Invest. 1992;89:1849–1856. doi: 10.1172/JCI115789. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martel-Renoir D, Grunewald V, Touitou R, et al. Qualitative analysis of the expression of Epstein-Barr virus lytic genes in nasopharyngeal carcinoma biopsies. J Gen Virol. 1995;76 (Pt 6):1401–1408. doi: 10.1099/0022-1317-76-6-1401. [DOI] [PubMed] [Google Scholar]
- Feng P, Ren EC, Liu D, et al. Expression of Epstein-Barr virus lytic gene BRLF1 in nasopharyngeal carcinoma: potential use in diagnosis. J Gen Virol. 2000;81:2417–2423. doi: 10.1099/0022-1317-81-10-2417. [DOI] [PubMed] [Google Scholar]
- Ning S. Innate immune modulation in EBV infection. Herpesviridae. 2011;2:1. doi: 10.1186/2042-4280-2-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Larochelle B, Flamand L, Gourde P, et al. Epstein-Barr virus infects and induces apoptosis in human neutrophils. Blood. 1998;92:291–299. [PubMed] [Google Scholar]
- Savard M, Belanger C, Tardif M, et al. Infection of primary human monocytes by Epstein-Barr virus. J Virol. 2000;74:2612–2619. doi: 10.1128/jvi.74.6.2612-2619.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tardif M, Savard M, Flamand L, et al. Impaired protein kinase C activation/translocation in Epstein-Barr virus-infected monocytes. J Biol Chem. 2002;277:24148–24154. doi: 10.1074/jbc.M109036200. [DOI] [PubMed] [Google Scholar]
- Li L, Liu D, Hutt-Fletcher L, et al. Epstein-Barr virus inhibits the development of dendritic cells by promoting apoptosis of their monocyte precursors in the presence of granulocyte macrophage-colony-stimulating factor and interleukin-4. Blood. 2002;99:3725–3734. doi: 10.1182/blood.v99.10.3725. [DOI] [PubMed] [Google Scholar]
- Severa M, Giacomini E, Gafa V, et al. EBV stimulates TLR- and autophagy-dependent pathways and impairs maturation in plasmacytoid dendritic cells: implications for viral immune escape. Eur J Immunol. 2013;43:147–158. doi: 10.1002/eji.201242552. [DOI] [PubMed] [Google Scholar]
- Alcami A, Koszinowski UH. Viral mechanisms of immune evasion. Trends Microbiol. 2000;8:410–418. doi: 10.1016/S0966-842X(00)01830-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Randall RE, Goodbourn S. Interferons and viruses: an interplay between induction, signalling, antiviral responses and virus countermeasures. J Gen Virol. 2008;89:1–47. doi: 10.1099/vir.0.83391-0. [DOI] [PubMed] [Google Scholar]
- Roberge CJ, Larochelle B, Rola-Pleszczynski M, et al. Epstein-Barr virus induces GM-CSF synthesis by monocytes: effect on EBV-induced IL-1 and IL-1 receptor antagonist production in neutrophils. Virology. 1997;238:344–352. doi: 10.1006/viro.1997.8852. [DOI] [PubMed] [Google Scholar]
- Roberge CJ, Poubelle PE, Beaulieu AD, et al. The IL-1 and IL-1 receptor antagonist (IL-1Ra) response of human neutrophils to EBV stimulation. Preponderance of IL-Ra detection. J Immunol. 1996;156:4884–4891. [PubMed] [Google Scholar]
- Hannum CH, Wilcox CJ, Arend WP, et al. Interleukin-1 receptor antagonist activity of a human interleukin-1 inhibitor. Nature. 1990;343:336–340. doi: 10.1038/343336a0. [DOI] [PubMed] [Google Scholar]
- Savard M, Belanger C, Tremblay MJ, et al. EBV suppresses prostaglandin E2 biosynthesis in human monocytes. J Immunol. 2000;164:6467–6473. doi: 10.4049/jimmunol.164.12.6467. [DOI] [PubMed] [Google Scholar]
- Gosselin J, Menezes J, D'Addario M, et al. Inhibition of tumor necrosis factor-alpha transcription by Epstein-Barr virus. Eur J Immunol. 1991;21:203–208. doi: 10.1002/eji.1830210130. [DOI] [PubMed] [Google Scholar]
- D'Addario M, Ahmad A, Morgan A, et al. Binding of the Epstein-Barr virus major envelope glycoprotein gp350 results in the upregulation of the TNF-alpha gene expression in monocytic cells via NF-kappaB involving PKC, PI3-K and tyrosine kinases. J Mol Biol. 2000;298:765–778. doi: 10.1006/jmbi.2000.3717. [DOI] [PubMed] [Google Scholar]
- Fachiroh J, Stevens SJ, Haryana SM, et al. Combination of Epstein-Barr virus scaffold (BdRF1/VCA-p40) and small capsid protein (BFRF3/VCA-p18) into a single molecule for improved serodiagnosis of acute and malignant EBV-driven disease. J Virol Methods. 2010;169:79–86. doi: 10.1016/j.jviromet.2010.07.001. [DOI] [PubMed] [Google Scholar]
- Thorley-Lawson DA, Poodry CA. Identification and isolation of the main component (gp350-gp220) of Epstein-Barr virus responsible for generating neutralizing antibodies in vivo. J Virol. 1982;43:730–736. doi: 10.1128/jvi.43.2.730-736.1982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gu AD, Xie YB, Mo HY, et al. Antibodies against Epstein-Barr virus gp78 antigen: a novel marker for serological diagnosis of nasopharyngeal carcinoma detected by xMAP technology. J Gen Virol. 2008;89:1152–1158. doi: 10.1099/vir.0.83686-0. [DOI] [PubMed] [Google Scholar]
- Joab I, Nicolas JC, Schwaab G, et al. Detection of anti-Epstein-Barr-virus transactivator (ZEBRA) antibodies in sera from patients with nasopharyngeal carcinoma. Int J Cancer. 1991;48:647–649. doi: 10.1002/ijc.2910480503. [DOI] [PubMed] [Google Scholar]
- Chien YC, Chen JY, Liu MY, et al. Serologic markers of Epstein-Barr virus infection and nasopharyngeal carcinoma in Taiwanese men. N Engl J Med. 2001;345:1877–1882. doi: 10.1056/NEJMoa011610. [DOI] [PubMed] [Google Scholar]
- Paramita DK, Fatmawati C, Juwana H, et al. Humoral immune responses to Epstein-Barr virus encoded tumor associated proteins and their putative extracellular domains in nasopharyngeal carcinoma patients and regional controls. J Med Virol. 2011;83:665–678. doi: 10.1002/jmv.21960. [DOI] [PubMed] [Google Scholar]
- de Turenne-Tessier M, Jolicoeur P, Middeldorp JM, et al. Expression and analysis of the Epstein-Barr virus BARF1-encoded protein from a tetracycline-regulatable adenovirus system. Virus Res. 2005;109:9–18. doi: 10.1016/j.virusres.2004.10.003. [DOI] [PubMed] [Google Scholar]
- Paramita DK, Fachiroh J, Artama WT, et al. Native early antigen of Epstein-Barr virus, a promising antigen for diagnosis of nasopharyngeal carcinoma. J Med Virol. 2007;79:1710–1721. doi: 10.1002/jmv.20987. [DOI] [PubMed] [Google Scholar]
- Imai S, Nishikawa J, Takada K. Cell-to-cell contact as an efficient mode of Epstein-Barr virus infection of diverse human epithelial cells. J Virol. 1998;72:4371–4378. doi: 10.1128/jvi.72.5.4371-4378.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shannon-Lowe CD, Neuhierl B, Baldwin G, et al. Resting B cells as a transfer vehicle for Epstein-Barr virus infection of epithelial cells. Proc Natl Acad Sci USA. 2006;103:7065–7070. doi: 10.1073/pnas.0510512103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Altman JD, Moss PA, Goulder PJ, et al. Phenotypic analysis of antigen-specific T lymphocytes. Science. 1996. 274: 94-96. J Immunol. 2011;187:7–9. [PubMed] [Google Scholar]
- Scotet E, Peyrat MA, Saulquin X, et al. Frequent enrichment for CD8 T cells reactive against common herpes viruses in chronic inflammatory lesions: towards a reassessment of the physiopathological significance of T cell clonal expansions found in autoimmune inflammatory processes. Eur J Immunol. 1999;29:973–985. doi: 10.1002/(SICI)1521-4141(199903)29:03<973::AID-IMMU973>3.0.CO;2-P. [DOI] [PubMed] [Google Scholar]
- Landais E, Saulquin X, Houssaint E. The human T cell immune response to Epstein-Barr virus. Int J Dev Biol. 2005;49:285–292. doi: 10.1387/ijdb.041947el. [DOI] [PubMed] [Google Scholar]
- Lee SP, Chan AT, Cheung ST, et al. CTL control of EBV in nasopharyngeal carcinoma (NPC): EBV-specific CTL responses in the blood and tumors of NPC patients and the antigen-processing function of the tumor cells. J Immunol. 2000;165:573–582. doi: 10.4049/jimmunol.165.1.573. [DOI] [PubMed] [Google Scholar]
- Lin X, Gudgeon NH, Hui EP, et al. CD4 and CD8 T cell responses to tumour-associated Epstein-Barr virus antigens in nasopharyngeal carcinoma patients. Cancer Immunol Immunother. 2008;57:963–975. doi: 10.1007/s00262-007-0427-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moss DJ, Chan SH, Burrows SR, et al. Epstein-Barr virus specific T-cell response in nasopharyngeal carcinoma patients. Int J Cancer. 1983;32:301–305. doi: 10.1002/ijc.2910320307. [DOI] [PubMed] [Google Scholar]
- Steven NM, Annels NE, Kumar A, et al. Immediate early and early lytic cycle proteins are frequent targets of the Epstein-Barr virus-induced cytotoxic T cell response. J Exp Med. 1997;185:1605–1617. doi: 10.1084/jem.185.9.1605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Angelini DF, Serafini B, Piras E, et al. Increased CD8+ T cell response to Epstein-Barr virus lytic antigens in the active phase of multiple sclerosis. PLoS Pathog. 2013;9:e1003220. doi: 10.1371/journal.ppat.1003220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fogg MH, Wirth LJ, Posner M, et al. Decreased EBNA-1-specific CD8+ T cells in patients with Epstein-Barr virus-associated nasopharyngeal carcinoma. Proc Natl Acad Sci USA. 2009;106:3318–3323. doi: 10.1073/pnas.0813320106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li J, Zeng XH, Mo HY, et al. Functional inactivation of EBV-specific T-lymphocytes in nasopharyngeal carcinoma: implications for tumor immunotherapy. PLoS One. 2007;2:e1122. doi: 10.1371/journal.pone.0001122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martorelli D, Houali K, Caggiari L, et al. Spontaneous T cell responses to Epstein-Barr virus-encoded BARF1 protein and derived peptides in patients with nasopharyngeal carcinoma: bases for improved immunotherapy. Int J Cancer. 2008;123:1100–1107. doi: 10.1002/ijc.23621. [DOI] [PubMed] [Google Scholar]
- Li J, Chen QY, Mo H, et al. Immunophenotyping at the time of diagnosis distinguishes two groups of nasopharyngeal carcinoma patients: implications for adoptive immunotherapy. Int J Biol Sci. 2011;7:607–617. doi: 10.7150/ijbs.7.607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown DM. Cytolytic CD4 cells: Direct mediators in infectious disease and malignancy. Cell Immunol. 2010;262:89–95. doi: 10.1016/j.cellimm.2010.02.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maini MK, Gudgeon N, Wedderburn LR, et al. Clonal expansions in acute EBV infection are detectable in the CD8 and not the CD4 subset and persist with a variable CD45 phenotype. J Immunol. 2000;165:5729–5737. doi: 10.4049/jimmunol.165.10.5729. [DOI] [PubMed] [Google Scholar]
- Munz C, Bickham KL, Subklewe M, et al. Human CD4(+) T lymphocytes consistently respond to the latent Epstein-Barr virus nuclear antigen EBNA1. J Exp Med. 2000;191:1649–1660. doi: 10.1084/jem.191.10.1649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leen A, Meij P, Redchenko I, et al. Differential immunogenicity of Epstein-Barr virus latent-cycle proteins for human CD4(+) T-helper 1 responses. J Virol. 2001;75:8649–59. doi: 10.1128/JVI.75.18.8649-8659.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Minarovits J. Epigenotypes of latent herpesvirus genomes. Curr Top Microbiol Immunol. 2006;310:61–80. doi: 10.1007/3-540-31181-5_5. [DOI] [PubMed] [Google Scholar]
- Khanna R, Busson P, Burrows SR, et al. Molecular characterization of antigen-processing function in nasopharyngeal carcinoma (NPC): evidence for efficient presentation of Epstein-Barr virus cytotoxic T-cell epitopes by NPC cells. Cancer Res. 1998;58:310–314. [PubMed] [Google Scholar]
- Levitskaya J, Coram M, Levitsky V, et al. Inhibition of antigen processing by the internal repeat region of the Epstein-Barr virus nuclear antigen-1. Nature. 1995;375:685–688. doi: 10.1038/375685a0. [DOI] [PubMed] [Google Scholar]
- Levitskaya J, Sharipo A, Leonchiks A, et al. Inhibition of ubiquitin/proteasome-dependent protein degradation by the Gly-Ala repeat domain of the Epstein-Barr virus nuclear antigen 1. Proc Natl Acad Sci USA. 1997;94:12616–12621. doi: 10.1073/pnas.94.23.12616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zaldumbide A, Ossevoort M, Wiertz EJ, et al. In cis inhibition of antigen processing by the latency-associated nuclear antigen I of Kaposi sarcoma herpes virus. Mol Immunol. 2007;44:1352–13560. doi: 10.1016/j.molimm.2006.05.012. [DOI] [PubMed] [Google Scholar]
- Blake N, Lee S, Redchenko I, et al. Human CD8+ T cell responses to EBV EBNA1: HLA class I presentation of the (Gly-Ala)-containing protein requires exogenous processing. Immunity. 1997;7:791–802. doi: 10.1016/s1074-7613(00)80397-0. [DOI] [PubMed] [Google Scholar]
- Long HM, Taylor GS, Rickinson AB. Immune defence against EBV and EBV-associated disease. Curr Opin Immunol. 2011;23:258–264. doi: 10.1016/j.coi.2010.12.014. [DOI] [PubMed] [Google Scholar]
- Blake N, Haigh T, Shaka'a G, et al. The importance of exogenous antigen in priming the human CD8+ T cell response: lessons from the EBV nuclear antigen EBNA1. J Immunol. 2000;165:7078–7087. doi: 10.4049/jimmunol.165.12.7078. [DOI] [PubMed] [Google Scholar]
- Voo KS, Fu T, Wang HY, et al. Evidence for the presentation of major histocompatibility complex class I-restricted Epstein-Barr virus nuclear antigen 1 peptides to CD8+ T lymphocytes. J Exp Med. 2004;199:459–470. doi: 10.1084/jem.20031219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tellam J, Connolly G, Green KJ, et al. Endogenous presentation of CD8+ T cell epitopes from Epstein-Barr virus-encoded nuclear antigen 1. J Exp Med. 2004;199:1421–1431. doi: 10.1084/jem.20040191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rowe M, Khanna R, Jacob CA, et al. Restoration of endogenous antigen processing in Burkitt's lymphoma cells by Epstein-Barr virus latent membrane protein-1: coordinate up-regulation of peptide transporters and HLA-class I antigen expression. Eur J Immunol. 1995;25:1374–1384. doi: 10.1002/eji.1830250536. [DOI] [PubMed] [Google Scholar]
- Murray PG, Constandinou CM, Crocker J, et al. Analysis of major histocompatibility complex class I, TAP expression, and LMP2 epitope sequence in Epstein-Barr virus-positive Hodgkin's disease. Blood. 1998;92:2477–2483. [PubMed] [Google Scholar]
- Tudor CS, Dawson CW, Eckhardt J, et al. c-Myc and EBV-LMP1: two opposing regulators of the HLA class I antigen presentation machinery in epithelial cells. Br J Cancer. 2012;106:1980–1988. doi: 10.1038/bjc.2012.197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith C, Wakisaka N, Crough T, et al. Discerning regulation of cis- and trans-presentation of CD8+ T-cell epitopes by EBV-encoded oncogene LMP-1 through self-aggregation. Blood. 2009;113:6148–6152. doi: 10.1182/blood-2009-02-203687. [DOI] [PubMed] [Google Scholar]
- Zuo J, Thomas W, van Leeuwen D, et al. The DNase of gammaherpesviruses impairs recognition by virus-specific CD8+ T cells through an additional host shutoff function. J Virol. 2008;82:2385–2393. doi: 10.1128/JVI.01946-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu CC, Liu MT, Chang YT, et al. Epstein-Barr virus DNase (BGLF5) induces genomic instability in human epithelial cells. Nucleic Acids Res. 2010;38:1932–1949. doi: 10.1093/nar/gkp1169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li D, Qian L, Chen C, et al. Down-regulation of MHC class II expression through inhibition of CIITA transcription by lytic transactivator Zta during Epstein-Barr virus reactivation. J Immunol. 2009;182:1799–1809. doi: 10.4049/jimmunol.0802686. [DOI] [PubMed] [Google Scholar]
- Horst D, van Leeuwen D, Croft NP, et al. Specific targeting of the EBV lytic phase protein BNLF2a to the transporter associated with antigen processing results in impairment of HLA class I-restricted antigen presentation. J Immunol. 2009;182:2313–2324. doi: 10.4049/jimmunol.0803218. [DOI] [PubMed] [Google Scholar]
- Croft NP, Shannon-Lowe C, Bell AI, et al. Stage-specific inhibition of MHC class I presentation by the Epstein-Barr virus BNLF2a protein during virus lytic cycle. PLoS Pathog. 2009;5:e1000490. doi: 10.1371/journal.ppat.1000490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yao M, Ohshima K, Suzumiya J, et al. Interleukin-10 expression and cytotoxic-T-cell response in Epstein-Barr-virus-associated nasopharyngeal carcinoma. Int J Cancer. 1997;72:398–402. doi: 10.1002/(sici)1097-0215(19970729)72:3<398::aid-ijc4>3.0.co;2-k. [DOI] [PubMed] [Google Scholar]
- Vockerodt M, Haier B, Buttgereit P, et al. The Epstein-Barr virus latent membrane protein 1 induces interleukin-10 in Burkitt's lymphoma cells but not in Hodgkin's cells involving the p38/SAPK2 pathway. Virology. 2001;280:183–198. doi: 10.1006/viro.2000.0768. [DOI] [PubMed] [Google Scholar]
- Kitagawa N, Goto M, Kurozumi K, et al. Epstein-Barr virus-encoded poly(A)(-) RNA supports Burkitt's lymphoma growth through interleukin-10 induction. EMBO J. 2000;19:6742–50. doi: 10.1093/emboj/19.24.6742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- You RI, Chang YC, Chen PM, et al. Apoptosis of dendritic cells induced by decoy receptor 3 (DcR3). Blood. 2008;111:1480–1488. doi: 10.1182/blood-2007-09-114850. [DOI] [PubMed] [Google Scholar]
- Chang YC, Chen TC, Lee CT, et al. Epigenetic control of MHC class II expression in tumor-associated macrophages by decoy receptor 3. Blood. 2008;111:5054–5063. doi: 10.1182/blood-2007-12-130609. [DOI] [PubMed] [Google Scholar]
- Ho CH, Chen CL, Li WY, et al. Decoy receptor 3, upregulated by Epstein-Barr virus latent membrane protein 1, enhances nasopharyngeal carcinoma cell migration and invasion. Carcinogenesis. 2009;30:1443–1451. doi: 10.1093/carcin/bgp135. [DOI] [PubMed] [Google Scholar]
- Shimakage M, Sakamoto H. Macrophage involvement in Epstein-Barr virus-related tumors. Exp Ther Med. 2010;1:285–291. doi: 10.3892/etm_00000044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fang W, Zhang J, Hong S, et al. EBV-driven LMP1 and IFN-gamma up-regulate PD-L1 in nasopharyngeal carcinoma: Implications for oncotargeted therapy. Oncotarget. 2014;5:12189–12202. doi: 10.18632/oncotarget.2608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gondek DC, Lu LF, Quezada SA, et al. Cutting edge: contact-mediated suppression by CD4+CD25+ regulatory cells involves a granzyme B-dependent, perforin-independent mechanism. J Immunol. 2005;174:1783–1786. doi: 10.4049/jimmunol.174.4.1783. [DOI] [PubMed] [Google Scholar]
- Chen ML, Pittet MJ, Gorelik L, et al. Regulatory T cells suppress tumor-specific CD8 T cell cytotoxicity through TGF-beta signals in vivo. Proc Natl Acad Sci USA. 2005;102:419–424. doi: 10.1073/pnas.0408197102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cao X, Cai SF, Fehniger TA, et al. Granzyme B and perforin are important for regulatory T cell-mediated suppression of tumor clearance. Immunity. 2007;27:635–646. doi: 10.1016/j.immuni.2007.08.014. [DOI] [PubMed] [Google Scholar]
- Lau KM, Cheng SH, Lo KW, et al. Increase in circulating Foxp3+CD4+CD25(high) regulatory T cells in nasopharyngeal carcinoma patients. Br J Cancer. 2007;96:617–622. doi: 10.1038/sj.bjc.6603580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marshall NA, Vickers MA, Barker RN. Regulatory T cells secreting IL-10 dominate the immune response to EBV latent membrane protein 1. J Immunol. 2003;170:6183–6189. doi: 10.4049/jimmunol.170.12.6183. [DOI] [PubMed] [Google Scholar]
- Dukers DF, Meij P, Vervoort MB, et al. Direct immunosuppressive effects of EBV-encoded latent membrane protein 1. J Immunol. 2000;165:663–670. doi: 10.4049/jimmunol.165.2.663. [DOI] [PubMed] [Google Scholar]
- Fogg M, Murphy JR, Lorch J, et al. Therapeutic targeting of regulatory T cells enhances tumor-specific CD8+ T cell responses in Epstein-Barr virus associated nasopharyngeal carcinoma. Virology. 2013;441:107–113. doi: 10.1016/j.virol.2013.03.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fries KL, Miller WE, Raab-Traub N. Epstein-Barr virus latent membrane protein 1 blocks p53-mediated apoptosis through the induction of the A20 gene. J Virol. 1996;70:8653–8659. doi: 10.1128/jvi.70.12.8653-8659.1996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu MY, Shih YY, Li LY, et al. Expression of the Epstein-Barr virus BHRF1 gene, a homologue of Bcl-2, in nasopharyngeal carcinoma tissue. J Med Virol. 2000;61:241–250. doi: 10.1002/(sici)1096-9071(200006)61:2<241::aid-jmv11>3.0.co;2-2. [DOI] [PubMed] [Google Scholar]
- Lo AK, Lo KW, Tsao SW, et al. Epstein-Barr virus infection alters cellular signal cascades in human nasopharyngeal epithelial cells. Neoplasia. 2006;8:173–180. doi: 10.1593/neo.05625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tang YL, Lu JH, Cao L, et al. Genetic variations of EBV-LMP1 from nasopharyngeal carcinoma biopsies: potential loss of T cell epitopes. Braz J Med Biol Res. 2008;41:110–116. doi: 10.1590/s0100-879x2008000200006. [DOI] [PubMed] [Google Scholar]
- Horst D, Burrows SR, Gatherer D, et al. Epstein-Barr virus isolates retain their capacity to evade T cell immunity through BNLF2a despite extensive sequence variation. J Virol. 2012;86:572–577. doi: 10.1128/JVI.05151-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tsai MH, Raykova A, Klinke O, et al. Spontaneous lytic replication and epitheliotropism define an Epstein-Barr virus strain found in carcinomas. Cell Rep. 2013;5:458–470. doi: 10.1016/j.celrep.2013.09.012. [DOI] [PubMed] [Google Scholar]
- Lin CL, Lo WF, Lee TH, et al. Immunization with Epstein-Barr Virus (EBV) peptide-pulsed dendritic cells induces functional CD8+ T-cell immunity and may lead to tumor regression in patients with EBV-positive nasopharyngeal carcinoma. Cancer Res. 2002;62:6952–6958. [PubMed] [Google Scholar]
- Comoli P, Pedrazzoli P, Maccario R, et al. Cell therapy of stage IV nasopharyngeal carcinoma with autologous Epstein-Barr virus-targeted cytotoxic T lymphocytes. J Clin Oncol. 2005;23:8942–8949. doi: 10.1200/JCO.2005.02.6195. [DOI] [PubMed] [Google Scholar]
- Straathof KC, Bollard CM, Popat U, et al. Treatment of nasopharyngeal carcinoma with Epstein-Barr virus-specific T lymphocytes. Blood. 2005;105:1898–1904. doi: 10.1182/blood-2004-07-2975. [DOI] [PubMed] [Google Scholar]
- Louis CU, Straathof K, Bollard CM, et al. Adoptive transfer of EBV-specific T cells results in sustained clinical responses in patients with locoregional nasopharyngeal carcinoma. J Immunother. 2010;33:983–990. doi: 10.1097/CJI.0b013e3181f3cbf4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lutzky VP, Corban M, Heslop L, et al. Novel approach to the formulation of an Epstein-Barr virus antigen-based nasopharyngeal carcinoma vaccine. J Virol. 2010;84:407–417. doi: 10.1128/JVI.01303-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taylor GS, Jia H, Harrington K, et al. A recombinant modified vaccinia ankara vaccine encoding Epstein-Barr Virus (EBV) target antigens: a phase I trial in UK patients with EBV-positive cancer. Clin Cancer Res. 2014;20:5009–5022. doi: 10.1158/1078-0432.CCR-14-1122-T. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hui EP, Taylor GS, Jia H, et al. Phase I trial of recombinant modified vaccinia ankara encoding Epstein-Barr viral tumor antigens in nasopharyngeal carcinoma patients. Cancer Res. 2013;73:1676–1688. doi: 10.1158/0008-5472.CAN-12-2448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith C, Tsang J, Beagley L, et al. Effective treatment of metastatic forms of Epstein-Barr virus-associated nasopharyngeal carcinoma with a novel adenovirus-based adoptive immunotherapy. Cancer Res. 2012;72:1116–1125. doi: 10.1158/0008-5472.CAN-11-3399. [DOI] [PubMed] [Google Scholar]
- Wu NC, De La Cruz J, Al-Mawsawi LQ, et al. HIV-1 quasispecies delineation by tag linkage deep sequencing. PLoS One. 2014;9:e97505. doi: 10.1371/journal.pone.0097505. [DOI] [PMC free article] [PubMed] [Google Scholar]