Abstract
[Purpose] The aim of this study was to investigate the effects of Ving Tsun (VT) Chinese martial art training on radial bone strength, upper- and lower-limb muscular strength, shoulder joint mobility, balance performance, and self-efficacy in elderly participants. [Subjects and Methods] Twelve seniors voluntarily joined the VT training group, and twenty-seven seniors voluntarily joined the control group. The VT group received VT training for three months, while the control group received no training. The bone strength of the distal radius was assessed using an ultrasound bone sonometer. Muscular strength in the limbs was evaluated using a Jamar handgrip dynamometer and the five times sit-to-stand test. Shoulder joint mobility was examined using a goniometer. Balance performance and self-efficacy were evaluated using the Berg Balance Scale and the Chinese version of the Activities-specific Balance Confidence Scale, respectively. [Results] The results revealed a nonsignificant group-by-time interaction effect, group effect, and time effect for all outcome variables. However, general trends of maintenance or improvement in all outcome parameters were observed to a greater extent in the VT group than in the control group. [Conclusion] VT training might be a potential fall-prevention exercise that can be used to maintain general physique, balance, and confidence in the elderly population. A further randomized controlled trial is needed to confirm this postulation.
Key words: Martial arts, Postural balance, Aged
INTRODUCTION
Falls are a common cause of morbidity and mortality among the elderly population. Body balance and lower limb muscular strength are common therapeutic targets to reduce the risk of falls among community-dwelling older adults1,2,3). Balance and strengthening exercises not only reduce the risk of falls and associated injuries but can also improve overall body management, reduce physical impairments, and above all, help to sustain a healthy lifestyle1, 3).
Various fall-prevention programs incorporating static, dynamic, and functional balance activities have been devised for the elderly by physiotherapists4). Nevertheless, conventional physiotherapy practices often vary in frequency, intensity, and duration and are often regarded as single-component and monotonous practices1). For community-dwelling older adults, a progressive exercise program that can strengthen body functions while at the same time adding interest and activity to their sedentary lifestyle would be a more motivating intervention to prevent falls.
In Asian cultures, practising traditional martial arts such as Tai Chi could be a popular means of maintaining general physique5). Martial arts training is regarded as a multicomponent exercise program, unlike single-component interventions that focus on just one of the risk factors associated with the likelihood of falling. A martial arts program integrates multiple components or activities targeting muscular performance, functional balance, postural control, and importantly, cardiovascular endurance1). Nevertheless, only a few studies have used randomized controlled clinical trials to provide evidence for the effects of martial arts training such as Tai Chi6), karate7), judo8), taekwondo9), and kung fu10) on health and fitness.
Invigorated by the strong image of Bruce Lee and Ip Man, Ving Tsun (VT) is another popular traditional Chinese martial art that may improve balance performance, muscular strength, and bone strength in older adults11). VT is characterized by speedy and dynamic yet stable punching techniques and footwork. It comprises three primary elements: structural development forms, reflex-development drills, and tactical development drills. Forms and drills are practised for the initial development of various VT skills in a practical and active way, while tactics are incrementally used to prepare learners for real-life self-defense. The forms are solitary exercises that are designed to sharpen focus and improve body balance, attentiveness, and proprioception. They aim to teach the hand positions, techniques, and defining movements at each level of VT. In conjunction with the forms, the drills instil the principal structure and mechanics; timing, dexterity, and interceptions; and kinesthetic senses12).
Founded on the basis of balance, structure, and stance, VT is a simple fighting skill that can be used to improve consistency, body balance, and simultaneous body movements, mainly through high-impact training practices such as wooden dummy training and sticking-hand exercises12,13,14,15). A previous study found that elderly VT practitioners had higher radial bone and handgrip strengths and better standing balance performance than healthy seniors who were not VT practitioners. These improvements are attributable to the various components of the VT training. First, VT involves repetitive upper limb striking movements that continually load high peak forces and impacts on the forearm bones. The bone strength of the distal radius, therefore, increases to accommodate these mechanical demands. Second, repeated practice of striking and sticking-hand techniques and fundamental standing control requires continuous contraction and relaxation of the upper and lower limb muscles, which should theoretically increase muscle strength. Third, better standing balance control is accredited to the important VT foundation techniques. In practicing static balance control, practitioners sustain postural stability during a variety of upper limb movements11).
In view of the above, we speculated that VT might offer a potential regular physical activity for healthy seniors to sustain better physical functions and balance, and hence to reduce the risk of falls. Building on the pilot study11), this study is the first prospective, non-randomized controlled trial to investigate the effects of short-term VT martial art training on radial bone strength, upper- and lower-limb muscular strength, shoulder joint mobility, balance performance, and self-efficacy in the elderly population.
SUBJECTS AND METHODS
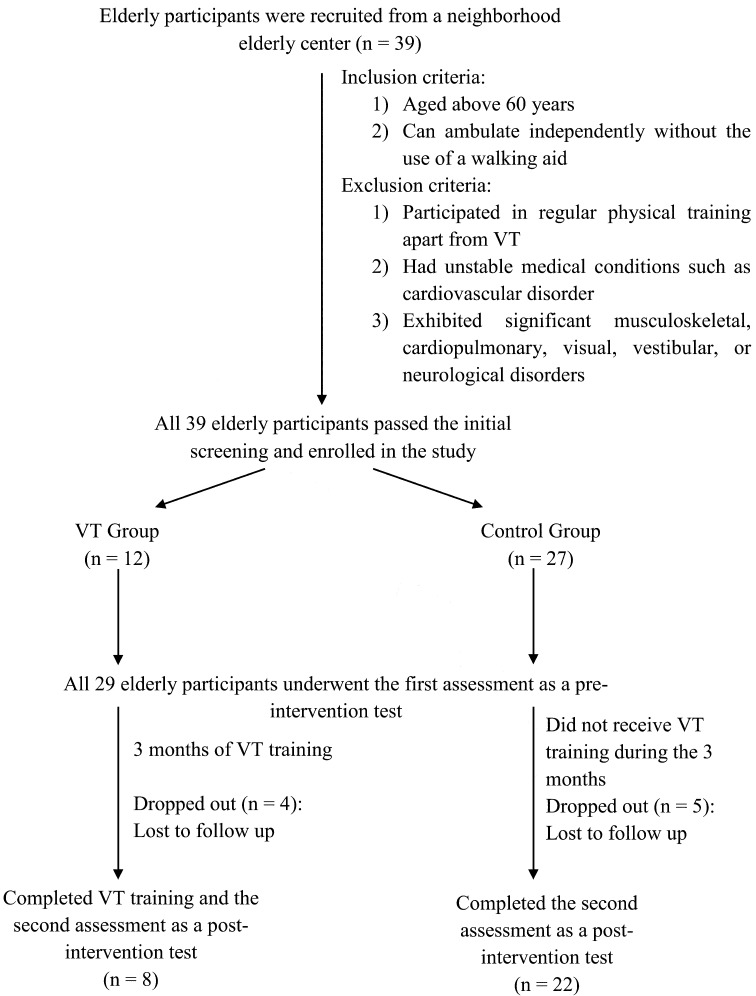
Thirty-nine participants were recruited from a neighborhood elderly center by convenience sampling. Twelve participants joined the VT training group voluntarily, while the other 27 participants acted as controls (Table 1). The inclusion criteria were that participants must be aged 60 years or above, able to ambulate independently without the use of walking aids, and able to communicate and follow verbal commands. Participants were excluded if they participated in regular physical training such as Tai Chi, had unstable medical conditions such as cardiovascular disorders, or exhibited significant cognitive, musculoskeletal, cardiopulmonary, somatosensory, visual, vestibular, or neurological disorders that might affect test performances (Fig. 1). Ethical approval was obtained from the Human Research Ethics Committee of the University of Hong Kong, and Declaration of Helsinki guidelines were followed. The study was explained to each participant, and written informed consent was obtained before data collection.
Table 1. Participants’ characteristics at baseline.
| VT group (n=12) | Control group (n=27) | |
|---|---|---|
| Age (years) | 69.0±7.3* | 74.0±4.7 |
| Sex | ||
| Males (n) | 7* | 1 |
| Females (n) | 5* | 26 |
| Height (cm) | 156.6±6.7* | 150.5±7.5 |
| Weight (kg) | 57.6±9.8 | 56.3±4.1 |
| BMI (kg/m2) | 23.7±4.1 | 24.9±4.0 |
Values represent means ± SD. *p<0.05
Fig. 1.
Study flowchart
The participants in the VT training group were invited to join the community-based VT martial art training program on a weekly basis (one 1-hour face-to-face session per week) for three consecutive months. With reference to the VT curriculum framework, the participants learned, practiced and polished their skills through the two primary elements: forms and drills. They learnt the first and second VT forms, Siu Lim Tau and Chum Kiu, and Chi Sau (sticking-hand exercises) progressively12). The detailed VT training protocol is outlined in Table 2. The participants were instructed to practice the forms and drills repeatedly until they were mildly sweating. They were allowed to rest if absolutely necessary. The VT training session was conducted by an experienced VT coach. The participants were also required to practice the VT exercises at home every day (excluding the VT class days) for an hour, building on those practiced during the face-to-face training sessions. To ensure all participants complied with the home exercises, they were asked to update the coach on their progress before every training session. The control group did not receive VT training within the study period. However, they were invited to join other courses (with no physical training component) at the elderly center.
Table 2. Ving Tsun martial art training protocol and methodology12).
| Exercise or technique | Descriptions |
|---|---|
| Siu Lim Tau “The little idea” |
• Foundation for learning fundamental techniques • Defines the body centreline theory • Consolidates training stance • Teaches VT strikes • Reinforces the proper elbow energy • Introduces fitting coordination of breath |
| Chum Kiu “Seeking the bridge” |
• Emphasizes coordinated movement of the entire body • Infuses generation of power during rapid twisting motions • Teaches the elbow striking and kicking techniques |
| Chi Sau “ Sticking hands” |
• Focuses on maintenance of contact while performing
techniques with a partner • Exemplifies how to sense changes in body mechanics |
| Training methodology Learning Training Feedback |
Participants: • Understood both the mechanical actions and the underlying key concepts • Put into practice by working on the forms, doing solo drills, cooperatively working through partner drills • Guided by coach through the initial rounds of practice and provided ongoing corrections • Self-evaluated and evaluated by coach |
All participants were assessed before the start of the VT intervention and again after the VT training. The participants from both groups underwent pre- and post-intervention assessments in four domains: (1) radial bone strength, (2) upper- and lower-limb muscular strength, (3) shoulder joint mobility, and (4) balance performance and confidence.
The bone strength of the distal radius was assessed using a Sunlight MiniOmni Ultrasound Bone Sonometer (Sunlight, BeamMed Ltd., Petah Tikva, Israel). Several studies have reported that this ultrasound system is both reliable (intra-operator precision at distal radius = 0.36%) and precise (in vivo precision = 0.4% − 0.8%)16,17,18). The detailed assessment procedures have been reported by Fong et al11). In brief, the assessor slowly rotated the ultrasound transducers (within the probe) around the distal radius. The speed of the ultrasound wave (SOS, ms−1) traveling through the outer surface (outer 2–6 mm) of the radial bone was measured. The SOS values were then converted into a T-score immediately using inbuilt computer software19). This score indicates the standard deviation relative to the population reference values of healthy young adults. It reflects the bone’s fragility and is highly correlated with bone strength19, 20). The average SOS T-score of the three trials obtained from the radius of the dominant side was used for analysis.
The handgrip strength of the dominant hand was assessed using a Jamar dynamometer (Sammons Preston, Mississauga, ON, Canada). Standard assessment procedures were followed21), as described in a previous study11). Briefly, participants squeezed the dynamometer as hard as possible three times, and the highest grip-strength value was used for analysis. The inter- and intra-rater reliabilities of this test have been reported to be good to excellent (ICC = 0.94–0.98) in adults21).
The five times sit-to-stand test (FTSTS) was used to functionally assess lower limb muscular strength. This test has good to excellent reliability (ICC = 0.64 − 0.96) and has been widely applied among elderly populations22). The detailed assessment procedures were reported by Ng and colleagues13). In summary, participants were invited to stand up and sit down five times as quickly as possible. Each participant performed the test three times. The average time taken to complete the three trials was used for analysis. A longer FTSTS time denotes weaker lower limb muscles23).
Shoulder joint mobility was assessed through a flexion movement in a seated posture. A universal goniometer was used to measure the active joint range of motion (ROM). The assessor set the goniometer’s stationary arm parallel to the lateral midline of the trunk and the movable arm parallel to the lateral midline of the humerus pointing towards the lateral humeral epicondyle24). The reliability of the ROM measurement depends on the assessor maintaining accurate reference points for the goniometer axes during shoulder movement25). The shoulder flexion ROM of the dominant arm was measured twice, and the mean ROM (degree) of the two trials was used for analysis.
The Berg Balance Scale (BBS) was used to measure the functional balance performance of the participants. The BBS is a 14-item test with a 5-point ordinal scale ranging from 0 to 4. Given that the 14 items are derived from functional movements in everyday life, this assessment was relevant, easy, and safe for the elderly participants to perform. The sum of the item scores (0–56) was used for analysis. A total score of 40 or below indicates the presence of fall risk26).
Fear of falling was measured by the validated Chinese version of the Activities-specific Balance Confidence (ABC) Scale, as it has been demonstrated to have good reliability (ICC = 0.87)27). Participants were invited to rate their self-perceived balance confidence level from 0 (no confidence at all) to 100 (full confidence) when performing 16 daily activities. The 16 item scores were averaged to obtain the mean ABC score (range 0–100), which was used for analysis. A lower mean ABC score indicates greater fear of falling28).
The normality of all continuous data was checked using the Kolmogorov-Smirnov test. Independent t-tests (for continuous data) and χ2 tests (for nominal data) were used to compare the baseline and demographic characteristics of the VT group and the control group. The intention-to-treat principle (last observation carried forward) was applied to deal with missing data. To test the overall time-by-group interaction effects of VT training and to avoid the probability of inflating type I errors, a single two-way repeated measures multivariate analysis of covariance (MANCOVA), incorporating all outcome variables, was performed. The between-subject factor was group, and the within-subject factor was time. If there were significant between-group differences in any of the demographic or outcome variables at baseline, the baseline data for the outstanding demographic or outcome variables were treated as covariates.
After the multivariate analysis, univariate analyses were performed as necessary, using paired and independent t-tests. The significance level was set at 0.05 (two-tailed). All of the statistical analyses were performed using the Statistical Package for the Social Sciences (SPSS) version 20.0 software (IBM, Armonk, NY, USA).
RESULTS
All 39 older adults (VT group, n = 12; control group, n = 27) were eligible to participate in the study (Fig. 1). Overall, 9 (23.1%) dropped out, 4 from the VT group (33.3%) and 5 from the control group (18.5%), due to loss of contact after the intervention period. The demographic and baseline characteristics of the participants are summarized in Tables 1 and 3, respectively. There were significant differences in age, body height, and gender ratio (p<0.05) between the two groups. Significant between-group differences were also found in the pre-test measurements of SOS T-score, handgrip strength, FTSTS time, ABC average score, and BBS total score (p<0.05) (Table 3). Therefore, age, height, and gender, together with the baseline SOS T-score, handgrip strength, FTSTS time, ABC average score, and BBS total score, were treated as covariates in the subsequent analyses.
Table 3. Comparison of outcome measurements between the VT and control groups.
| Measurements | VT group (n=12) | Control group (n=27) | ||
|---|---|---|---|---|
| Pretest (Mean±SD) |
Post-test (Mean±SD) |
Pretest (Mean±SD) |
Post-test (Mean±SD) |
|
| SOS T-score | −2.28±1.32 | −1.62±1.51 | −3.72±1.19 | −3.30±1.28 |
| Handgrip strength (kg) | 26.18±6.04 | 26.45±8.76 | 16.93±5.14 | 17.30±4.21 |
| FTSTS time (s) | 10.12±2.81 | 9.30±2.19 | 14.33±4.62 | 15.09±7.53 |
| Shoulder flexion ROM (degrees) | 170.82±7.53 | 171.55±7.70 | 166.67±12.25 | 164.70±13.12 |
| ABC average score | 87.50±11.65 | 89.60±10.03 | 75.79±11.17 | 75.39±16.73 |
| BBS total score | 48.82±4.33 | 50.36±5.37 | 42.52±7.98 | 43.78±10.25 |
Repeated measures MANCOVA revealed no significant group (p = 0.797), time (p = 0.584), or group-by-time interaction (p = 0.665) effects for any of the outcome variables. Therefore, univariate analysis was not necessary for the individual dependent variables. Despite the insignificant findings, greater trends of improvement were observed in the VT group than in the control group for most of the outcome variables, as follows.
(1) The radial bone strength of the VT group improved by 28.9% over time, whereas the no-training control group improved by only 11.3% (Table 3).
(2) Handgrip strength was similar over time in both groups (Table 3).
(3) The VT group took less time (0.82 s) to complete the FTSTS test after training, indicating possible improvements in lower limb muscular strength. In contrast, the control group required more time (0.76 s) to complete the FTSTS test at the post-intervention assessment compared with at the pre-intervention assessment (Table 3).
(4) Although the improvement in shoulder flexion ROM was minimal (0.4%) after VT training, there was a slight deterioration (1.2%) in the no-training control group over time (Table 3).
(5) A trend of improvement was also observed in the ABC score after VT training. Specifically, balance confidence increased by 2.4% in the VT group but decreased by 0.5% in the control group over time (Table 3).
(6) BBS scores increased by 1.54 units in the VT training group but by only 1.26 units in the control group at the post-intervention assessment (Table 3).
DISCUSSION
To the best of our knowledge, this is the first prospective study to examine the health effects of short-term VT martial art training in an elderly community-dwelling sample. Our findings revealed nonsignificant differences in radial bone strength, limb muscular strength, joint mobility, balance performance, and self-efficacy among the VT group participants. Nevertheless, trends of improvement in these fitness attributes were noticeable in the VT training group.
First, regarding the radial bone strength, participants from the VT group made greater progress than those in the control group. This improvement can be explained by the constant upper limb striking movements throughout the three months of VT training. According to Wolff’s law of bone remodelling29), the repetitive forces and impacts on the forearm bones during sticking-hand drills should enhance distal radial bone strength to accommodate the increased mechanical demands. Hence, the bone is remodelled and becomes stronger to endure this additional load when it encounters increased loading during VT practice29, 30). The improvement in the current study was not as apparent as that reported in a previous study of habitual elderly VT practitioners11). The difference is mainly attributable to the different training periods and VT curricula used in the two studies. In the study by Fong et al., elderly VT practitioners had trained for an average of 16 years and also practised a wide range of forms, drills, and tactics. This long-term regular high-impact training could improve radial bone strength, which could lessen the risk of distal radius fractures as a result of falls11). In this study, the VT participants only trained for a short time (three months). They were also practicing at the beginner level, which focuses on basic techniques and hardly touches upon intensive practices using wooden dummies and sandbags. Therefore, their bones experienced limited exposure to high impact forces, which was insufficient to cause any dramatic improvements in bone strength.
Second, as for the muscular strength in the dominant upper limb, rather stable performances were observed in the handgrip test in both groups over time. In contrast, there was a clear difference in lower limb muscular strength performance between the two groups after the VT training: the VT group had improved, while the control group had deteriorated. Despite this encouraging observation, the between-group difference was not significant. This finding was again contrary to that of the previous study on habitual elderly VT practitioners11), probably for the same reasons as mentioned above. The improvements could also be due to the emphasis on hand forms and footwork in VT training. Repeated practice of the elbow striking and kicking techniques during VT training might strengthen the extrinsic and intrinsic limb muscles as a result of frequent contraction and relaxation31, 32).
Third, similar to muscular strength, shoulder joint mobility improved in the VT group following training, but not in the control group. Although this effect was not significant, there was a clear trend of improvement. As shoulder flexibility is dependent on the physiological adaptation of connective tissues, physical activity consisting of stretching movements would be expected to increase the elasticity of muscle and soft tissues around the joint, rendering a greater ROM33). Therefore, the frequent and unique shoulder stretching movements during VT training (e.g., Bong Sau and Fak Sau)12) might lead to local, if not universal, maintenance or enhancement of shoulder joint mobility.
Finally, concerning balance control and confidence, there were modest improvements in the functional balance task and self-efficacy evaluation in the VT group. This supports the findings of the previous study11). Unlike the sensory organization test used in the previous study11), this study examined participants’ balance control with two well-formulated scales to assess functional balance performance and self-efficacy in the context of the participants’ everyday lives. As suggested in the previous study, the improvement in standing balance control can be attributed to the fundamental balance practice underlying the theory of VT11). Balance, structure, and stance are the basic elements incorporated into every VT form and drill curriculum12). It is unsurprising, therefore, that VT training can strengthen static and anticipatory postural control systems and balance confidence, thereby enhancing postural stability in the course of different functional movements34). Overall, given the trend of improvements demonstrated in this short-term VT intervention, the findings substantiate the use of VT training as a fall-prevention program to strengthen overall physical fitness and improve balance performance and confidence.
There are a number of limitations to the present study. First, as the sample size, particularly in the VT group, was quite small, there was inadequate statistical power to obtain significant results. Second, the attrition rate was quite high, with 33.3% of the subjects from the VT group and 18.5% of the subjects from the control group failing to complete the final assessment. The reasons for drop out are unknown, as the subjects were lost to follow-up, so selective drop out from the VT training was possible. Third, the limited training period may have been insufficient to detect significant improvements in the outcome parameters. Finally, the participants were not randomized and the assessor was not blinded, which may have introduced bias and confounded the results. Based on this study, it is not possible to establish causal relationships between practicing VT martial arts and the aforementioned physical benefits. Further studies should include a larger randomized sample, blind assessments, a comprehensive training protocol and documentation, and a longer VT training period to identify the beneficial effects. Moreover, including older participants may also be appropriate because physical performance declines significantly after 80 years of age35) but fall-prevention exercise programs currently available usually target individuals who are younger than 80 years old36,37,38). Evidence-based VT fall-prevention programs should be developed for people in their 80s.
To conclude, Ving Tsun martial art might be a potential fall-prevention exercise, as it might improve radial bone strength, lower limb muscular strength, functional balance performance, and balance self-efficacy in the elderly population. Further studies with more participants and a longer intervention period are needed to provide more robust evidence of these beneficial effects.
Acknowledgments
We thank the Shun Ching Ving Tsun Martial Arts Association for providing Ving Tsun training and the Evangelical Lutheran Church Kwai Chung Neighborhood Elderly Centre for enabling the recruitment of participants.
REFERENCES
- 1.Shubert TE: Evidence-based exercise prescription for balance and falls prevention: a current review of the literature. J Geriatr Phys Ther, 2011, 34: 100–108. [DOI] [PubMed] [Google Scholar]
- 2.Masud T, Morris RO: Epidemiology of falls. Age Ageing, 2001, 30: 3–7. [DOI] [PubMed] [Google Scholar]
- 3.Weerdesteyn V, Groen BE, van Swigchem R, et al. : Martial arts fall techniques reduce hip impact forces in naive subjects after a brief period of training. J Electromyogr Kinesiol, 2008, 18: 235–242. [DOI] [PubMed] [Google Scholar]
- 4.Sherrington C, Whitney JC, Lord SR, et al. : Effective exercise for the prevention of falls: a systematic review and meta-analysis. J Am Geriatr Soc, 2008, 56: 2234–2243. [DOI] [PubMed] [Google Scholar]
- 5.Bu B, Haijun H, Yong L, et al. : Effects of martial arts on health status: a systematic review. J Evid Based Med, 2010, 3: 205–219. [DOI] [PubMed] [Google Scholar]
- 6.Zeeuwe PE, Verhagen AP, Bierma-Zeinstra SM, et al. : The effect of Tai Chi Chuan in reducing falls among elderly people: design of a randomized clinical trial in the Netherlands [ISRCTN98840266] [ISRCTN98840266] BMC Geriatr, 2006, 6: 6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Chaabène H, Hachana Y, Franchini E, et al. : Physical and physiological profile of elite karate athletes. Sports Med, 2012, 42: 829–843. [DOI] [PubMed] [Google Scholar]
- 8.Wolach B, Falk B, Gavrieli R, et al. : Neutrophil function response to aerobic and anaerobic exercise in female judoka and untrained subjects. Br J Sports Med, 2000, 34: 23–28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Fong SS, Fu SN, Ng GY: Taekwondo training speeds up the development of balance and sensory functions in young adolescents. J Sci Med Sport, 2012, 15: 64–68. [DOI] [PubMed] [Google Scholar]
- 10.Tsang TW, Kohn M, Chow CM, et al. : Health benefits of Kung Fu: a systematic review. J Sports Sci, 2008, 26: 1249–1267. [DOI] [PubMed] [Google Scholar]
- 11.Fong SSM, Guo X, Cheung APM, et al. : Elder Chinese martial art practitioners have higher radial bone strength, hand-grip strength and better standing balance control. ISRN Rehabilitation, 2013. . [Google Scholar]
- 12.Belonoha W: The Wing Chun Compendium. California: Blue Snake Books, 2006. [Google Scholar]
- 13.Green TA: Martial Arts of the World: An Encyclopedia. California: ABCCLIO, 2001. [Google Scholar]
- 14.Yip C: 116 Wing Tsun Dummy Techniques as Demonstrated by Grandmaster Yip Man. Hong Kong: Leung’s Publications, 1981. [Google Scholar]
- 15.Peterson D: Look Beyond the Pointing Finger—the Combat Philosophy of Wong Shun Leung. Victoria: Melbourne Chinese Martial Arts Club, 2001. [Google Scholar]
- 16.Barkmann R, Kantorovich E, Singal C, et al. : A new method for quantitative ultrasound measurements at multiple skeletal sites: first results of precision and fracture discrimination. J Clin Densitom, 2000, 3: 1–7. [DOI] [PubMed] [Google Scholar]
- 17.Drake WM, McClung M, Njeh CF, et al. : Multisite bone ultrasound measurement on North American female reference population. J Clin Densitom, 2001, 4: 239–248. [DOI] [PubMed] [Google Scholar]
- 18.Knapp KM, Blake GM, Spector TD, et al. : Multisite quantitative ultrasound: precision, age- and menopause-related changes, fracture discrimination, and T-score equivalence with dual-energy X-ray absorptiometry. Osteoporos Int, 2001, 12: 456–464. [DOI] [PubMed] [Google Scholar]
- 19.BeamMed Ltd: Sunlight MiniOmni Bone Sonometer User Guide. Israel: BeamMed Ltd, 2010. [Google Scholar]
- 20.Hans D, Schott AM, Meunier PJ: Ultrasonic assessment of bone: a review. Eur J Med, 1993, 2: 157–163. [PubMed] [Google Scholar]
- 21.Peolsson A, Hedlund R, Oberg B: Intra- and inter-tester reliability and reference values for hand strength. J Rehabil Med, 2001, 33: 36–41. [DOI] [PubMed] [Google Scholar]
- 22.Bohannon RW: Test-retest reliability of the five-repetition sit-to-stand test: a systematic review of the literature involving adults. J Strength Cond Res, 2011, 25: 3205–3207. [DOI] [PubMed] [Google Scholar]
- 23.Ng SS, Cheung SY, Lai LS, et al. : Association of seat height and arm position on the Five Times Sit-to-Stand Test times of stroke survivors. Biomed Res Int, 2013, Article ID 642362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Bandy WD, Reese NB: Joint Range of Motion and Muscle Length Testing. Pennsylvania: W.B. Saunders, 2009. [Google Scholar]
- 25.Steultjens MP, Dekker J, van Baar ME, et al. : Range of joint motion and disability in patients with osteoarthritis of the knee or hip. Rheumatology (Oxford), 2000, 39: 955–961. [DOI] [PubMed] [Google Scholar]
- 26.Berg KO, Wood-Dauphinee SL, Williams JI, et al. : Measuring balance in the elderly: validation of an instrument. Can J Public Health, 1992, 83: S7–S11. [PubMed] [Google Scholar]
- 27.Hsu PC, Miller WC: Reliability of the Chinese version of the Chinese version of the activities-specific balance confidence scale. Disabil Rehabil, 2006, 28: 1287–1292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Mak MK, Lau AL, Law FS, et al. : Validation of the Chinese translated activities-specific balance confidence scale. Arch Phys Med Rehabil, 2007, 88: 496–503. [DOI] [PubMed] [Google Scholar]
- 29.Ruff C, Holt B, Trinkaus E: Who’s afraid of the big bad Wolff?: “Wolff’s law” and bone functional adaptation. Am J Phys Anthropol, 2006, 129: 484–498. [DOI] [PubMed] [Google Scholar]
- 30.Jiang Y, Zhao J, Rosen C, et al. : Perspectives on bone mechanical properties and adaptive response to mechanical challenge. J Clin Densitom, 1999, 2: 423–433. [DOI] [PubMed] [Google Scholar]
- 31.Di Monaco M, Di Monaco R, Manca M, et al. : Handgrip strength is an independent predictor of distal radius bone mineral density in postmenopausal women. Clin Rheumatol, 2000, 19: 473–476. [DOI] [PubMed] [Google Scholar]
- 32.Tsuji S, Tsunoda N, Yata H, et al. : Relation between grip strength and radial bone mineral density in young athletes. Arch Phys Med Rehabil, 1995, 76: 234–238. [DOI] [PubMed] [Google Scholar]
- 33.Abernethy B, Kippers V, Hanrahan S, et al. : Biophysical Foundations of Human Movement. Illinois: Human Kinetics, 2013. [Google Scholar]
- 34.Shumway-Cook A, Woollacott MH: Motor Control Translating Research into Clinical Practice. Philadelphia: Lippincott Williams and Wilkins, 2007. [Google Scholar]
- 35.Nakano MM, Otonari TS, Takara KS, et al. : Physical performance, balance, mobility, and muscle strength decline at different rates in elderly people. J Phys Ther Sci, 2014, 26: 583–586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Kim WJ, Chang M, An DH: Effects of a community-based fall prevention exercise program on activity participation. J Phys Ther Sci, 2014, 26: 651–653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Kin S, Li S: Effects of Taijiquan on the physical fitness of elderly Chinese people. J Phys Ther Sci, 2006, 18: 133–136. [Google Scholar]
- 38.Hyun J, Hwangbo K, Lee CW: The effects of pilates mat exercise on the balance ability of elderly females. J Phys Ther Sci, 2014, 26: 291–293. [DOI] [PMC free article] [PubMed] [Google Scholar]