Abstract
The aim of the present study was to investigate the clinical efficacy of herbal medicines (1 gm tulsi and 1 gm turmeric mixed in glycerine base) for the treatment of oral submucous fibrosis (OSMF). Forty-one patients in the age group of 17- 56 years without any systemic complications were included in the study. The patients were treated with medicines, which were to be applied 3-4 times a day. Blood samples were collected before and after treatment to screen for any systemic changes due to these medications. Burning sensation and mouth opening were recorded before and after treatment. Patients were followed up on monthly subsequent visits for three months. Changes in the burning sensation on visual analogue scale (VAS) scale and difference in the mouth opening were analyzed statistically. A statistically significant improvement was seen in both burning sensation and mouth opening. Tulsi and turmeric offers a safe and efficacious combination of natural products available for symptomatic treatment of OSMF.
Keywords: Burning sensation, Curcuma longa, mouth opening, Ocimum sanctum, oral sub-mucous fibrosis, tulsi, turmeric
INTRODUCTION
Oral Submucous Fibrosis (OSMF) is defined as an insidious chronic condition of unknown etiology affecting the oral mucosa characterized by dense collagen tissue deposition within submucosa, occasionally extending to the pharynx and esophagus.,[1] The disease is characterized by blanching and stiffness of oral mucosa, trismus, burning sensation, loss of mobility of tongue and loss of gustatory sensation. Majority of these cases are seen in Indian population.[2] The prevalence varies from 0.20-0.5% in India with a higher percentage being found in the southern parts of the country.[3]
A variety of physiological factors have been associated with it including betel nut chewing, capsasin, autoimmunity and genetic predisposition. The OSMF, if not treated can progress to oral cancer. The conversion rate is about 2-10%.[4] It is the major health issue affecting 2.5 million Indian population under the age of 40 years.[1] OSMF is the most poorly understood and unsatisfactorily treated disease. The younger the age, the more rapid is the progression of disease. All the available treatments give only symptomatic relief which is short lived.[5] The incidence of OSMF still rising alarmingly and there is a dire need to search for an effective and safe remedy because of lack of present therapies to either provide a complete cure or treating the patients at the cost of adverse effects.[1,4] Comprehensive search of scientific literature has shown only limited ayurvedic preparations being used in the treatment of OSMF, though their efficacies have to be evaluated in a proper clinical trial. Natural ayurvedic treatment of OSMF along with life style modification can help in lowering the symptoms of OSMF and may help in curing the disease.
Turmeric (Curcuma longa Linn) is the perennial plant, when dried rhizomes, it is made into a yellow powder with a bitter yet sweet taste.[6] It has a wide range of therapeutic actions. It protects against free radical damage as it is a strong antioxidant, helps in reducing inflammation by lowering histamine levels and also increases the production of natural cortisone.[7,8] In addition, it also helps in increasing the blood circulation and is known to be anti-mutagenic.[8,9,10] The plant was included as one of the active ingredients in the present study because of all these properties.
Tulsi (Ocimum sanctum Linn) ‘basil’ is a plant with many medicinal values. Ayurveda recommends tulsi in several formulations to enhance immunity and metabolic functions. It helps in reducing inflammation by inhibiting the inflammation-causing enzymes.[11]
Due to all these properties, a synergistic approach using both tulsi and turmeric was planned in the treatment of OSMF with prior ethical clearance from the institute. Reason for selecting these two drugs was that there were no clinical trials on OSMF in spite of their proven efficacy as anti-metabolite and anti-inflammatory actions.[12]
MATERIALS AND METHODS
It was a prospective observational study conducted at Faculty of Dental Sciences, Institute of Medical Sciences, Banaras Hindu University, Varanasi. Institutional ethical committee approval was taken before starting the study. Informed consent was taken from each patient for participation in the study. Forty-five patients of recently diagnosed OSMF were selected, which were to be followed up after giving them the above mentioned treatment. The study was completed with 41 patients as 4 patients did not turn up for follow-up. As the study was done in a government institute, with patients coming from low socio-economic status with low literacy, they may not aware of the importance of follow-up visits and hence there were the drop out cases in the study.
Patients were involved irrespective of age, gender, occupation, social status, ethnicity, and stages of OSMF. The condition was diagnosed clinically, as OSMF has characteristic clinical features. All the patients who were already undergoing some OSMF treatment and some systemic diseases were excluded from the study. For accessing their eligibility all patients underwent a complete blood investigation and only patients with values within normal limits were included in the study. Incision biopsies from all the selected patients were obtained to rule out any dysplasia or frank malignancy as such cases had to be excluded from the study.
All patients were motivated for life style modifications and advised to quit the habitual use of tobacco and alcohol. Habits included smoking cigarette and bidis, chewing tobacco, gutkha, betel nut, areca nut and alcohol. All patients had some or other habit but most patients had the habit of chewing tobacco and gutkha. Life style modifications included yoga, meditation, behavioral therapy and relaxation therapy.
The herbs were procured from Gola Deenanath herbal drug market, Varanasi and identified by ayurvedic specialist by conducting pharmacognosy study. They were powdered by pulverizer machine in ayurvedic pharmacy, BHU. The rhizomes of curcuma and leaves of tulsi were used. The herbs were prescribed by researchers in consultation with ayurvedic physicians.
The patients were advised to mi × 1 gm of turmeric powder and 1 gm of tulsi powder in glycerine to make a paste. The patients were instructed to apply this paste all over the oral mucosa 4-5 times per day and not to eat or drink anything for next 15 minutes. On follow-up visits, the patients were asked to bring the used packets back to check their compliance and to see whether all the powder was used or not. Pretreatment burning sensation was measured on visual analogue scale (VAS) scale and inter-incisal distance was measured in millimeters (mm), to assess the mouth opening. All patients were advised to come for follow-up visits at 1-month interval for 3 months. Each time, the burning sensation on VAS scale and inter-incisal distance was recorded. No biopsy was taken after the treatment, only clinical improvement i.e. mouth opening, burning sensation etc., were taken into account.
Results were statistically analyzed at the end of the study by paired ‘t’ test to find out the efficacy of the treatment.
RESULTS
Forty-one patients completed the study. Patients were within the age group of 17-56 years. The mean age of the patients was 31.93 ± 10.92 years with 17 patients below 25 years and 24 patients above 25 years. There were 34 male and 7 female patients.
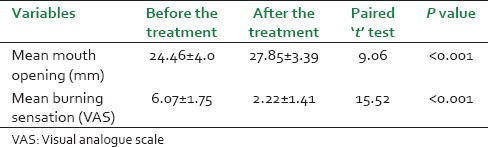
On the first visit, the means of the mouth opening and burning sensation recorded. At the end of therapy, there was statistically significant improvement in burning sensation and mouth opening. Mean burning sensation was [Table 1] 6.07 ± 1.75 before the treatment and 2.22 ± 1.41 after the treatment (t = 15.52; P < 0.001). Mean mouth opening [Table 1] was 24.46 ± 4.0 mm before the treatment and 27.85 ± 3.39 mm after the treatment (t = 9.06; P < 0.001).
Table 1.
Improvement in mouth opening and burning sensation
Gender wise comparison for the changes in burning sensation and mouth opening was also analyzed by paired ‘t’ test and was found to be statistically significant.
The mean burning sensation on VAS scale before the treatment in males was 5.94 ± 1.79, which was reduced after therapy to 2.12 ± 1.45. The improvement was statistically significant (t = 13.58; P < 0.001). Similarly, in females, the mean burning sensation on VAS scale before the treatment was 6.71 ± 1.50, which was improved up to the mean 2.71 ± 1.11 [Table 2]. The improvement observed was statistically significant (t = 7.48; P < 0.001).
Table 2.
Gender wise variation in mouth opening and burning sensation
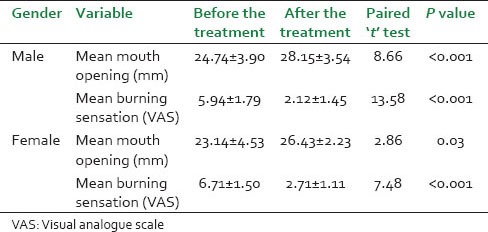
The mean mouth opening before the treatment in males was 24.74 ± 3.90 mm, which was increased after therapy to 28.15 ± 3.54 mm. The improvement was significant (t = 8.66; P < 0.001). Likewise, in females, the mean mouth opening before the treatment was 23.14 ± 4.53 mm, which was improved to the mean 26.43 ± 2.23 mm [Table 2]. The improvement observed was statistically significant (t = 2.86; P = 0.03).
The results of the study showed that gender did not appear to affect the responsiveness of the treatment. No clinically significant adverse reactions to the treatment were seen in patients taking the same mentioned treatment. Out of 41 patients, 3 patients experienced bad taste.
DISCUSSION
In spite of various present treatment modalities practiced for OSMF, not a single is totally effective in every case. Many pharmaceutical products have been proven to be successful in treating OSMF but found to have adverse effects and recurrences.[1,2] Recently, interest in herbal medicines have been increased and various studies are being carried out to explore clinical efficacy of compound preparations. The trial drugs, turmeric and tulsi were tried because of the drawback of conventional OSMF treatment. Turmeric is known to be strong antioxidant and reduces inflammation. It increases blood circulation and is anti-mutagenic.[6]
Turmeric constituents include three curcuminoids: Curcumin, demethoxycurcumin and bisdemethoxycurcumin. Curcumin (diferuloylmethane), an anti-inflammatory agent used in traditional medicine, has been shown to suppress cellular transformation, proliferation, invasion, angiogenesis, and metastasis. Curcumin suppresses tumor necrosis factor (TNF)-induced NF-κB activation and NF-κB-dependent reporter gene expression. Such products which are involved in cellular proliferation (COX-2, cyclin D1, and c-myc), anti-apoptosis (IAP1, IAP2, XIAP, Bcl-2, Bcl-xL, Bfl-1/A1, TRAF1, and cellular cFLIP), and metastasis (VEGF, MMP-9, ICAM-1) were down regulated by curcumin.[13]
Tulsi enhances immunity and improves metabolic functions. Their extract has been found to reduce inflammation by inhibiting enzymes. It also lowers the stress and has antioxidant property.[11,12]
Ursolic acid (UA), a pentacyclic triterpene acid from O. sanctum has been reported to suppress NF-κB activation induced by various carcinogens including TNF, phorbol ester, okadaic acid, H2O2 and cigarette smoke. UA inhibits degradation and phosphorylation of IκBα, IκB-kinase activation, p65 phosphorylation, p65 nuclear translocation and NF-κB-dependent reporter gene expression. Finally, UA inhibits proliferation and induces apoptosis and the accumulation of cells in G1-G0 phase of the cell cycle.[13]
The results of the study showed that the synergistic action of these two herbs results in higher efficacy and highly potent anti-OSMF treatment. Treatment with these drugs produces an early, sustained and significant fall in burning sensation, clinically and statistically as soon as one month. Mouth opening was also significantly improved. Results were better in severe cases reflecting its higher efficacy. Age or gender did affect the response.
Emphasis was also given on life style modification by motivating all patients before, during and after the study to discontinue tobacco, beetle nut and alcohol. Life style modification along with these drugs can be attributed to dramatic improvement in OSMF cases.
The results of the present study were compared with the results of documented outcomes of other therapeutic procedures. In the study, conducted by Alam S et al., the efficacy of aloe-vera gel as an adjuvant therapy of OSMF has been assessed on 60 subjects. They were divided into two categories; medicinal treatment (submucosal injection of hyaluronidase and dexamethasone, n = 30) and surgical treatment (n = 30). Each category was randomly divided into Aloe vera and without Aloe vera groups (with 15 patients in each category).[14]
The results showed that the groups receiving aloe vera had a significant improvement in most symptoms of OSMF (P < 0.01) compared with the non-Aloe vera groups in both the medicinal and surgical categories.[14] Nichlani SS et al., assessed the Benefit of Using Muscle Relaxants in the Routine Treatment Protocol of Oral Submucosal Fibrosis: Beneficial uses of muscle relaxants in the routine treatment protocol of OSMF. The study was conducted on 40 patients with grade 3 (<19 mm) mouth opening. Twenty of these patients underwent the routine treatment protocol of weekly injection of hyaluronidase with hydrocortisone and antioxidant capsules with added lycopene for 1 month. The remaining 20 test subjects, in addition to the routine injections and antioxidants, were given skeletal muscle relaxants like thiocolchicoside or chlorzoxazone.[15] Seventeen out of the 20 test patients who received muscle relaxants in addition to the routine protocol showed marked improvement with shift from grade 3 (<19 mm) to grade 1 (>40 mm) that is a greater than 20 mm improvement in mouth opening.[15] Karemore TV et al., evaluated the effect of newer antioxidant lycopene in the treatment of oral submucous fibrosis. The study group included 92 patients with OSMF. Out of the 92 patients, 46 patients were given lycopene and remaining 46 were on placebo drug. Lycopene group patients received 8 mg Lycored™ per day in two divided doses of 4 mg each, while placebo group patients received placebo tablet twice a day.[16] Lycopene was found to be significantly efficacious as the percentage of the cases with improved maximal mouth opening, was 69.56% (P < 0.05). It was observed that an increase in the mean mouth opening was 4.46 ± 3.65 mm in the lycopene group while 1.16 ± 1.3 mm in the placebo group.[16]
Although there was significant improvement in the mouth opening in the first two studies, the treatment modalities (Aloe vera and muscle relaxants) were just an adjuvant therapies while herbs used in the present study are the main therapy for management of OSMF in all clinical stages. In addition, the role of Aloe vera and muscle relaxants per se in the treatment of OSMF has not been established in these studies. Another disadvantage of their study was that Aloe vera gel and muscle relaxants were used with invasive techniques (injections and surgery) whereas our treatment modality needs no invasion. Besides, muscle relaxants have many side effects such as gastric irritation, drowsiness, lethargy etc., whereas treatment with turmeric and tulsi has no side effects. The results of the third study (lycopene treatment) are comparable to the results of present study as the improvement in the mean mouth opening was 3.41 mm and 3.29 mm in males and females, respectively in present study. The improvements observed are statistically significant. However, the drug used (lycored) in the study was synthetically manufactured while tulsi and turmeric used in this study are freely available in India. Therefore, this treatment modality can be used by masses at a low cost. Present study not only demonstrated superior rate in relieving symptoms in OSMF patients but also was associated with minimal side effects such as bad taste, mild headache, which disappeared after treatment. Major drawback of study was that no controls were taken to compare efficacy. This can be explained by the fact that this is a primary study using ayurvedic medications. Further studies to assess the comparative efficacy with already existing OSMF treatment modalities are required.
CONCLUSION
Tulsi and turmeric along with life style modification is safe and efficacious remedy for the treatment of all grades of OSMF in all age groups with no limitation to its use. Tulsi and turmeric can provide a safer, low cost, and effective alternative to the present conventional treatment, which can be useful in a country like India. Further studies will be followed to access the comparative efficacy with already existing treatment for OSMF.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Borle RM, Borle SR. Management of oral submucous fibrosis: A conservative approach. J Oral Maxillofac Surg. 1991;49:788–91. doi: 10.1016/0278-2391(91)90002-4. [DOI] [PubMed] [Google Scholar]
- 2.Scully C. The oral cavity. In: Champion RH, Burton IL, Ebling FJ, editors. Textbook of Dermatology. 5th ed. London: Oxford Blackwell Scientific Publication; 1992. pp. 2689–276. [Google Scholar]
- 3.Saraswathi TR, Ranganathan K, Shanmugam S, Sowmya R, Narasimhan PD, Gunaseelan R. Prevalence of oral lesions in relation to habits: Cross-sectional study in South India. Indian J Dent Res. 2006;17:121–5. doi: 10.4103/0970-9290.29877. [DOI] [PubMed] [Google Scholar]
- 4.Canniff JP, Harvey W, Harris M. Oral submucous fibrosis: Its pathogenesis and management. Br Dent J. 1986;160:429–34. doi: 10.1038/sj.bdj.4805876. [DOI] [PubMed] [Google Scholar]
- 5.Gupta D, Sharma SC. Oral submucous fibrosis: A new treatment regimen. J Oral Maxillofac Surg. 1988;46:830–3. doi: 10.1016/0278-2391(88)90043-2. [DOI] [PubMed] [Google Scholar]
- 6.Chaturvedi TP. Uses of turmeric in dentistry: An update. Indian J Dent Res. 2009;20:107–9. doi: 10.4103/0970-9290.49065. [DOI] [PubMed] [Google Scholar]
- 7.Ramirez-Bosca A, Soler A, Gutierrez MA. Antioxidant curcuma extracts decreases the blood lipid peroxide levels of human subjects. Age. 1995;18:167–9. [Google Scholar]
- 8.Ammon HP, Safayhi H, Mack T, Sabieraj J. Mechanism of anti-inflammatory actions of curcumine and boswellic acids. J Ethnopharmacol. 1993;38:113–9. doi: 10.1016/0378-8741(93)90005-p. [DOI] [PubMed] [Google Scholar]
- 9.Srivastava R, Puri V, Srimal RC, Dhawan BN. Effect of curcumin on platelet aggregation and vascular prostacyclin synthesis. Arzneimittelforschung. 1986;36:715–7. [PubMed] [Google Scholar]
- 10.Menon LG, Kuttan R, Kuttan G. Anti-metastatic activity of curcumin and catechin. Cancer Lett. 1999;141:159–65. doi: 10.1016/s0304-3835(99)00098-1. [DOI] [PubMed] [Google Scholar]
- 11.Prakash P, Gupta N. Therapeutic uses of Ocimum sanctum linn (Tulsi) with a note on eugenol and its pharmacological actions: A short review. Indian J Physiol Pharmacol. 2005;49:125–31. [PubMed] [Google Scholar]
- 12.Kelm MA, Nair MG, Strasburg GM, DeWitt DL. Antioxidant and cyclo-oxygenase inhibitory phenolic compounds from Ocimum sanctum Linn. Phytomedicine. 2000;7:7–13. doi: 10.1016/S0944-7113(00)80015-X. [DOI] [PubMed] [Google Scholar]
- 13.Aggarwal BB, Prasad S, Reuter S, Kannappan R, Yadev VR, Park B, et al. Identification of novel anti-inflammatory agents from ayurvedic medicine for prevention of chronic diseases: “Reverse pharmacology” and “bedside to bench” approach. Curr Drug Targets. 2011;12:1595–653. doi: 10.2174/138945011798109464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Alam S, Ali I, Giri KY, Gokkulakrishnan S, Natu SS, Faisal M, et al. Efficacy of aloe vera gel as an adjuvant treatment of oral submucous fibrosis. Oral Surg Oral Med Oral Pathol Oral Radiol. 2013;116:717–24. doi: 10.1016/j.oooo.2013.08.003. [DOI] [PubMed] [Google Scholar]
- 15.Nichlani SS, Jagade MV, Ganeshan A. Benefit of using muscle relaxants in the routine treatment protocol of oral submucous fibrosis: A pilot study. Indian J Otolaryngol Head Neck Surg. 2011;63:317–20. doi: 10.1007/s12070-011-0234-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Karemore TV, Motwani M. Evaluation of the effect of newer antioxidant lycopene in the treatment of oral submucous fibrosis. Indian J Dent Res. 2012;23:524–8. doi: 10.4103/0970-9290.104964. [DOI] [PubMed] [Google Scholar]


