Abstract
Synchronous intracranial germ cell tumor in the pineal and suprasellar region is rare. They represent only 5–10% of all intracranial germinomas. They are also known by the entity “double midline atypical teratoma” and are common in the second decade of life. We report a case of an 11-year-old girl having dual midline intracranial lesions with obstructive hydrocephalus treated by ventriculo-peritoneal shunt. Diagnosis of germinoma was made on the basis of imaging and elevated beta-human chorionic gonadotropin in cerebrospinal fluid. Radiotherapy was instituted, which resulted in the total disappearance of both the lesions. Clinical expression, diagnosis and management strategies are discussed.
Keywords: Alpha feto protein, beta-human chorionic gonadotropin, germinomas, radiotherapy, synchronous lesions
Introduction
Germinomas accounts for 2–5% of all central nervous system malignancies in the pediatric population out of which synchronous lesion in the pineal and suprasellar region accounts for only 5% of such lesions.[1,2] Diagnosis is made by polymorphic clinical expression with neuroimaging and biopsy. Elevation of alpha feto protein (AFP) and beta-human chorionic gonadotropin (β-HCG) in the serum and cerebrospinal fluid (CSF) is reliable for diagnosis of germinoma, which obviates the need for biopsy.
We report a rare case of dual midline germinomas in pineal and suprasellar region presented with obstructive hydrocephalus. Diagnosis was made on the basis of increased β-HCG and imaging characteristics. Ventriculo-peritoneal shunt relieved symptoms of raised intracranial pressure. Radiotherapy resulted in the total disappearance of both the lesions. Clinical manifestations, diagnostic methods and treatment strategy are discussed.
Case Report
An 11-year-old girl presented with a history of headache and vomiting of 1-month duration. Parents also noticed altered sensorium and diminution of vision 5 days prior to admission. On examination, child was drowsy but arousable. Fundoscopic examination revealed bilateral papilledema. Additional neurological and general physical examination revealed no abnormalities. Magnetic resonance imaging brain revealed dual lesion in the pineal and suprasellar region, which were hypointense to isointense on T1-weighted and hyperintense on T2-weighted images, and there was marked enhancement on contrast administration. There was obstructive hydrocephalus [Figure 1]. Serum tumor markers like β-HCG and AFP were within normal limit. Other routine investigations were also normal. Ventriculo-peritoneal shunt placement was done to relieve raised pressure symptoms. CSF analysis was done, which revealed raised β-HCG level while AFP level was normal.
Figure 1.
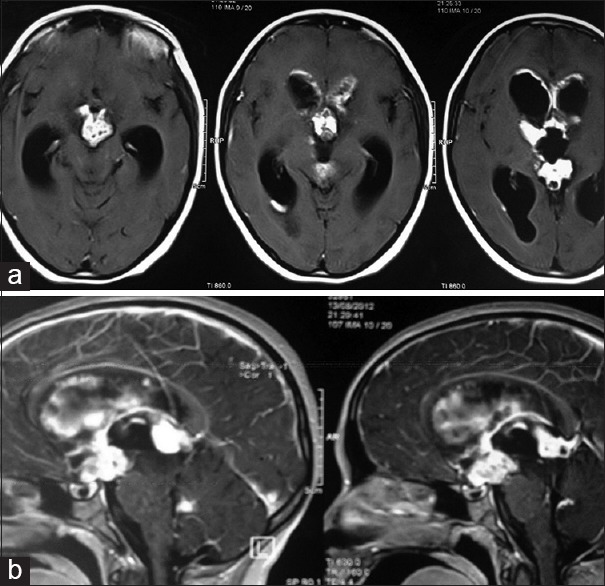
T1-weighted gadolinium enhanced magnetic resonance imaging scan axial image (a) and sagittal image (b) 2 lesions in the suprasellar and pineal regions
Diagnosis of germinoma was made on the basis of raised β-HCG level in CSF and characteristic radiological imaging findings. Radiotherapy was instituted, which resulted in the total disappearance of both the lesions [Figure 2]. There was no recurrence after 1-year of follow-up.
Figure 2.
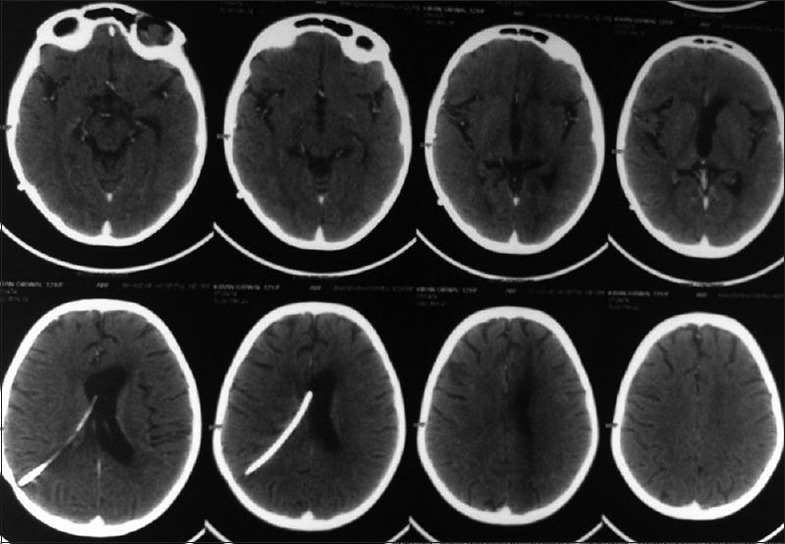
Contrast-enhanced computed tomography scan brain 6 months after radiotherapy-both the lesions disappeared with ventriculo-peritoneal shunt in situ
Discussion
On an average 5–10% of all germinomas present as dual lesions in the pineal and suprasellar region and are also known by the entity “double midline atypical teratoma.” This is common in the second decade of life with a male preponderance,[2] while our patient is a female. Patient usually present with polymorphic clinical expression. Pineal region tumor causes symptoms associated with increased intracranial pressure resulting from obstructive hydrocephalus and may exhibit Parinaud's syndrome, papilledema, obtundation, and ataxia.[2,3] Suprasellar tumor commonly presents with visual field defect due to optic chiasma compression and hypothalamic pituitary axis dysfunction particularly diabetes insipidus. Presentation may also include delayed secondary sexual features, hypopituitarism and/or isolated growth failure.[2,3] In the series of six cases reported by Sugiyama et al. initial symptoms were attributable to suprasellar region and symptoms due to the pineal region tumor developed later, whereas in our case patient presented with obstructive hydrocephalus due to pineal region tumor and no signs and symptoms pertaining to suprasellar lesion. Typical clinical presentation with radiological imaging of dual lesion raises suspicion of germinoma, but either histological verification or elevated tumor marker like β-HCG and AFP in serum or CSF is necessary for diagnosis. In our case diagnosis was established on the basis of increased β-HCG in CSF. Empirical therapy is rarely advisable now a days.[4] Tissue diagnosis may be done by stereotactic biopsy, craniotomy or neuroendoscopy.[5]
Various treatment options like radiotherapy, chemotherapy and surgery are available to manage these lesions. Sugiyama et al. noted that tumors of both pineal and suprasellar region disappeared after irradiation, similarly our case also demonstrated disappearance of both the lesions after radiation therapy.[6] Radiotherapy remains the treatment of choice as germinomas are highly radiosensitive tumors.[4,6] Some reports suggest that in patients with germinoma 5 years survival rate is 90% and 20 years survival rate is 80%.[7] Kaprelyan et al. noticed that the best survival and least long term morbidity is achieved with a combination of both chemotherapy and radiotherapy.[2] Neo-adjuvant chemotherapy may allow for a reduction in the dose for the local (from 5000 to 3000 cGy) and for craniospinal (from 3600 cGy to 2100 cGy) with good disease control.[3] New treatment technologies such as intensity-modulated radiotherapy or proton therapy reduces the risk of radiation to nontarget brain.[8] Surgery is mainly done for hydrocephalus. Endoscopic third ventriculostomy, ventriculo-peritoneal shunt or external drainage may be done for CSF diversion. Surgical decompression of the tumor is rarely needed. Regular blood and CSF β-HCG and AFP level monitoring are useful markers for follow-up of response to therapy and tumor recurrence.[9] Intracranial germinoma can be diagnosed on the basis of radiological imaging and elevated tumor markers in CSF and blood - thus obviating the need for biopsy.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
References
- 1.Haque F, Zahid M, Ahmad SA, Naseem S. Synchronous germinomas in the pineal and suprasellar region. Indian Pediatr. 2005;42:376–9. [PubMed] [Google Scholar]
- 2.Kaprelyan AG, Deleva N, Tzoukeva A, Balev B, Metodiev KT, Kyuchukov GN. CNS germinoma with synchronous lesios in the suprasellar and pineal regions: Clinical, CT and immunological follow-up. J IMAB. 2006;12:41–6. [Google Scholar]
- 3.Packer RJ, Cohen BH, Cooney K. Intracranial germ cell tumors. Oncologist. 2000;5:312–20. [PubMed] [Google Scholar]
- 4.Van Battum P, Huijberts MS, Heijckmann AC, Wilmink JT, Nieuwenhuijzen Kruseman AC. Intracranial multiple midline germinomas: Is histological verification crucial for therapy? Neth J Med. 2007;65:386–9. [PubMed] [Google Scholar]
- 5.De Silva JC, de Melo F, de Lima T, Faquini IV, Costa LF, Valença MM. Multiple midline intracranial germinoma managed by neuroendoscopy. Arq Neuropsiquiatr. 2009;67:125–6. doi: 10.1590/s0004-282x2009000100033. [DOI] [PubMed] [Google Scholar]
- 6.Sugiyama K, Uozumi T, Kiya K, Mukada K, Arita K, Kurisu K, et al. Intracranial germ-cell tumor with synchronous lesions in the pineal and suprasellar regions: Report of six cases and review of the literature. Surg Neurol. 1992;38:114–20. doi: 10.1016/0090-3019(92)90088-5. [DOI] [PubMed] [Google Scholar]
- 7.Hadjikoutis S, Hughes T. Germinoma with synchronous involvement of the pineal gland and the suprasellar region: A treatable cause of visual failure in a young adult. Eye (Lond) 2004;18:525–6. doi: 10.1038/sj.eye.6700715. [DOI] [PubMed] [Google Scholar]
- 8.Kortmann RD. Current concepts and future strategies in the management of intracranial germinoma. Expert Rev Anticancer Ther. 2014;14:105–19. doi: 10.1586/14737140.2014.856268. [DOI] [PubMed] [Google Scholar]
- 9.Pollack IF, Jakacki RI. 6th ed. Ch. 204. Philadelphia, PA: Elsevier Saunders; 2011. Youman's Neurological Surgery, Intracranial Germ Cell Tumors; pp. 2121–7. [Google Scholar]


