Abstract
Background:
Increasing awareness around patient safety and efforts to reduce medical errors has become a priority in the modern health care system. Losing needles during laparoscopic procedures is an uncommon occurrence; however, it poses a significant dilemma for the operating surgeon because retrieval can be a major challenge even for highly skilled and experienced operators.
Objective:
The objective of this paper was to review the current literature and highlight this potentially serious issue and suggest a method of dealing with this uncommon occurrence.
Methods:
A comprehensive literature search was conducted using several Internet search engines including PubMed, Google Scholar, and ScienceDirect.
Conclusions:
The risks associated with retained small foreign bodies remains unknown, and there are few reports and little consensus on how surgeons should manage retained needles or other small foreign bodies during laparoscopic surgery. We propose an algorithm that may be implemented as a standard operating procedure in surgical theatres when a surgeon is faced with such a dilemma.
Keywords: Lost needles, Laparoscopy
INTRODUCTION
The benefits of laparoscopic surgery are well documented,1 and minimal-access surgery is now widely practiced in most surgical specialties. However, laparoscopic procedures are not without risk. Specifically, laparoscopic techniques may lead to trocar and “off camera” injuries, as well as port site hernia. Moreover, lost needles in the laparoscopic setting, as well as mislaid swabs, can pose a significant laparoscopic challenge, and important decisions on the optimum method of retrieval need to be made.
Reduction of medical errors remains a significant clinical priority. Retained foreign surgical bodies can have serious clinical and medico-legal consequences. Abdominal procedures (approximately 50%) followed by gynecological and urological procedures seem to present the most risk of retaining a foreign body.2 Retained foreign bodies after operations are estimated to affect between 0.3 and 1 per 1000 procedures performed on the abdomen.3 Lincourt et al reported that 83% of patients with retained foreign bodies required reoperation.4
Lost needles or broken equipment during laparoscopic operations are an uncommon but potentially serious problem. Retrieval can be a major challenge even for highly skilled and experienced operators.5
Intraabdominal retained foreign objects such as needles, swabs, and other equipment can cause infections, delayed hemorrhage, pain, and even bowel obstruction.6 This can apparently occur even with very small retained objects. Huntington and Klomp7 reported a case of a patient who underwent laparoscopic-assisted vaginal hysterectomy. Several weeks after the operation, she developed mechanical small bowel obstruction caused by the presence of a free staple intraperitoneally creating an obstructing band. A loose staple as a cause of mechanical small bowel obstruction after laparoscopic appendectomy has also been reported by Lorken et al.8
Preventive measures are the best way to ensure that foreign bodies are not retained after any operation (laparoscopic or open). This includes accurately counting the instruments and equipment used at the start and the conclusion of the operation. Any discrepancy should lead to a recount. If there is missing equipment, then either imaging should be used or re-exploration of the surgical site considered.
Several factors have been cited as increasing the chance of losing foreign bodies during an operation; these include a high body mass index, using a large number of surgical instruments, involvement of more than one surgical team, complex and/or prolonged operations, and emergency surgical procedures.3,9
The objective of this paper was to review the current literature on the management of missing needles during laparoscopic procedures and highlight this potentially serious issue. Moreover, we propose an algorithm that may be adopted as a way of trying to deal with this uncommon occurrence.
METHODS
A comprehensive literature search was conducted using a number of Internet search engines including PubMed, Google Scholar, and ScienceDirect. A combination of the following terms was searched: lost needles/sutures, missing needles, laparoscopy/laparoscopic operations, and retained surgical foreign body.
DISCUSSION
What is the best course of action if a needle is lost during laparoscopic surgery? Should the operation be converted into a laparotomy immediately to retrieve the missing object? Should an image intensifier be used intraoperatively to search for and retrieve the foreign body? Or should the operation continue as planned and the foreign body simply ignored? The literature on how to actually manage lost foreign bodies such as needles during laparoscopic operations is scarce.
Ostrzenski10 reported a method of detecting a missing needle or instrument fragment intraoperatively during laparoscopy. A plain abdominal radiograph may show the missing equipment, but it is challenging to actually find it with a laparoscope. His method used radiopaque threads removed from radiograph-detectable sponges to create a “net” or “grid” on the abdomen. A metallic instrument was then used to pinpoint the missing fragment more accurately. In this manner, the surgeon was able to localize and retrieve the missing fragment without having to convert to open surgery.
Lynch and Powers11 described the retrieval of a 2-mm fragment of a broken needle in a patient undergoing a laparoscopic-assisted vaginal hysterectomy. They also suggested using radiopaque materials such as graspers or staples to aid in locating a small object.
Small fragments or needles, however, can be extremely difficult to locate because they are often buried between loops of intestine. Kandioler-Eckersberger et al12 described the use of a novel magnetic probe to retrieve broken metallic parts during laparoscopy. The probe is a 6-cm long magnetic Teflon-coated tip attached to a semiflexible Teflon rod. The flexibility of the rod ensures it can be maneuvered without the risk of causing bowel injury. They described two cases in which the magnetic probe and fluoroscopy were used together to grasp the missing fragment, thus avoiding a laparotomy and additional trocar placement.
Macilquham et al13 carried out a study to ascertain the minimum needle size that can be identified using a variety of radiographic techniques. These techniques included using departmental radiography equipment, using a portable radiograph machine, and using a mobile image intensifier. Surgeons, radiologists, and radiographers were asked to review the resultant images. All observers were able to identify needles larger than 19 mm. Only 13% of their observers were able to identify the 13-mm needle on radiographs, with no observer identifying needles smaller than this size. The smallest sized needle seen by most of their observers (84%) was 17 mm; 3% identified the 19-mm needle as the smallest seen. They concluded that for needles smaller than 13 mm, obtaining radiographs to search for the needle is probably superfluous because it exposes patients to unnecessary radiation with little or no gain. In such circumstances, accurate postoperative documentation would probably be adequate.
However, this study is not without its limitations, and there are other conflicting reports in the literature regarding the size of needles that can be identified on radiographs.14
In a survey study carried out by Ruscher at al6 to ascertain the attitudes and approaches toward retained foreign bodies, health care professionals were asked how they would manage a retained needle during an elective laparoscopic operation. They analyzed 255 complete responses. Fifty-five percent of respondents in this study replied that they would convert to an open operation (laparotomy) to retrieve a retained needle, whereas 45% stated they would continue with the operation and leave the needle in situ. However, the size of the needle was not specified in the question.
Sixty-eight percent of respondents felt that retained needles would place patients at some risk of harm in the future but 89.4% thought the complications of converting a laparoscopic operation to an open operation outweighed the presence of a retained surgical body. Approximately 90% of respondents felt surgeons were always obliged to inform the patient if an object was lost or possibly left inside the patient.
CONCLUSIONS
There is currently no consensus in the literature on how one should manage retained needles during laparoscopic operations.6 Aside from sporadic reports of postoperative complications, the true risks and adverse events associated with retained small foreign bodies remains unknown.
Retained needles causing pain and discomfort to patients and necessitating a further operation have been highlighted.15,16 In these reports, the needles tended to be large (>17 mm) or present in small cavities such as the eye. Needles smaller than 17 mm are difficult to detect on plain radiographs, and there is no good evidence suggesting they would cause harm in larger body cavities.14
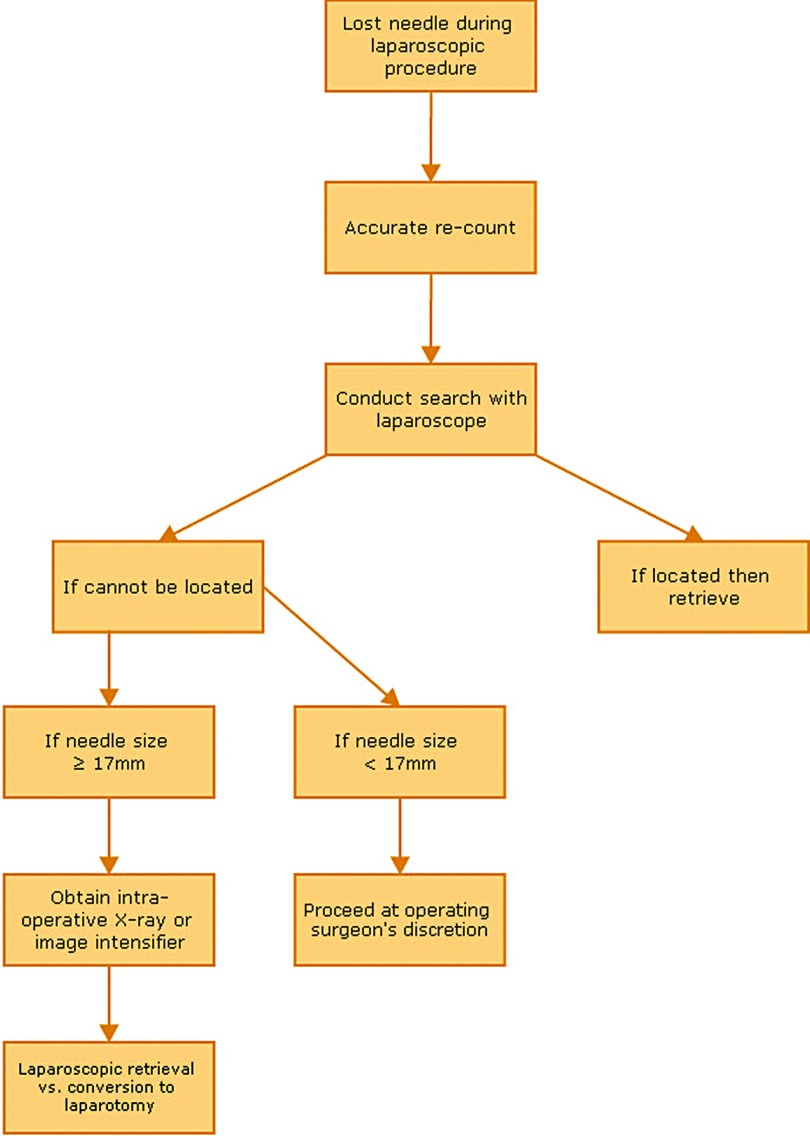
We therefore propose the following algorithm when a laparoscopic surgeon is faced with such a dilemma (Figure 1).
Figure 1.
A proposed algorithm for the management of a lost needle during laparoscopic surgery.
The operating surgeon needs to weigh the risk of a retained needle against converting a laparoscopic operation into an open laparotomy and the disadvantages associated with this in each individual patient. The role of new technologies and devices such as magnetic probes needs to be explored further because these may provide a useful solution to this challenging problem.
In accordance with good medical practice, however, in all cases, full disclosure concerning the lost needle must be given to the patient and the event documented in the medical notes. This might have important implications for the patient in the future (eg, in the use of imaging such as magnetic resonance imaging scans).
Lost foreign bodies and retained needles remain contentious and important issues. The surgeon must have a clear and safe plan when it occurs, resulting in an outcome that puts the patient at the least risk. Ultimately as surgeons, we must be able to justify our actions and be completely honest with the patient.
Contributor Information
Shafquat Zaman, Heart of England NHS Foundation Trust, Bordesley Green, Birmingham, UK..
Robert Clarke, Shrewsbury and Telford NHS Trust, Mytton Oak Road, Shrewsbury, UK..
Andrew Schofield, Shrewsbury and Telford NHS Trust, Mytton Oak Road, Shrewsbury, UK..
References:
- 1. Swanton A, Slack A, McVeigh E. Laparoscopy and laparoscopic surgery. Obstet Gynecol Reprod Med. 2010;20(2):33–40. [Google Scholar]
- 2. Mouhsine E, Halkic N, Garofalo R, et al. Soft-tissue textiloma: a potential diagnostic pitfall. Can J Surg. 2005;48:495–496. [PMC free article] [PubMed] [Google Scholar]
- 3. Stawicki SP, Evans DC, Cipolla J, et al. Retained surgical foreign bodies: a comprehensive review of risks and preventive strategies. Scand J Surg. 2009;98(1):8–17. [DOI] [PubMed] [Google Scholar]
- 4. Lincourt AE, Harrell A, Cristiano J, Sechrist C, Kercher K, Heniford BT. Retained foreign bodies after surgery. J Surg Res. 2007;138(2):170–174. [DOI] [PubMed] [Google Scholar]
- 5. Barto W, Yazbek C, Bell S. Finding a lost needle in laparoscopic surgery. Surg Laparosc Endosc Percutan Tech. 2011;21(4):163–165. [DOI] [PubMed] [Google Scholar]
- 6. Ruscher KA, Modeste KA, Papasavas PK, Tishler S. Retained needles in laparoscopic surgery. Open or observe? Poster presented at: Society of American Gastrointestinal and Endoscopic Surgeons (SAGES) 2011 Annual Meeting; March 30-April 2, 2011; San Antonio, TX. [Google Scholar]
- 7. Huntington TR, Klomp GR. Retained staples as a cause of mechanical small-bowel obstruction. Surg Endosc. 1995;9(3)353–354. [DOI] [PubMed] [Google Scholar]
- 8. Lorken M, Marnitz U, Schumpelick V. Free intraperitoneal clip as the cause of mechanical ileus of the small intestine. Chirurgie. 1999;70:1492–1493. [DOI] [PubMed] [Google Scholar]
- 9. Gawande AA, Studdert DM, Orav EJ, Brennan TA, Zinner MJ. Risk factors for retained instruments and sponges after surgery. N Engl J Med. 2003;348:229–235. [DOI] [PubMed] [Google Scholar]
- 10. Ostrzenski A. An intraoperative method of localising a missing piece of a broken laparoscopic instrument. Am J Obstet Gynecol. 1997;176(3)726–727. [DOI] [PubMed] [Google Scholar]
- 11. Lynch CM, Powers AK. Management of a broken needle at the time of laparoscopic burch. JSLS. 2000;4(3):275–276. [PMC free article] [PubMed] [Google Scholar]
- 12. Kandioler-Eckersberger D, Niederle B, Herbst F, Wenzl E. A magnetic probe to retrieve broken metallic parts of instruments during laparoscopic procedures. Surg Endosc. 2002;16:208–209. [DOI] [PubMed] [Google Scholar]
- 13. Macilquham MD, Riley RG, Grossberg P. Identifying lost surgical needles using radiographic techniques. AORN J. 2003;78(1):73–78. [DOI] [PubMed] [Google Scholar]
- 14. Barrow CJ. Use of x-ray in the presence of an incorrect needle count. AORN J. 2001;74(1):80–81. [DOI] [PubMed] [Google Scholar]
- 15. NoThing Left Behind: A national surgical patient-safety project to prevent retained surgical items. Available at: http://www.nothingleftbehind.org Accessed December 6, 2012.
- 16. Gibbs VC. Retained surgical items and minimally invasive surgery. World J Surg. 2011;35(7):1532–1539. [DOI] [PMC free article] [PubMed] [Google Scholar]