ABSTRACT
Objective
Optimism is associated with reduced cardiovascular mortality, but its impact on recovery after acute coronary syndrome (ACS) is poorly understood. We hypothesized that greater optimism would lead to more effective physical and emotional adaptation after ACS and would buffer the impact of persistent depressive symptoms on clinical outcomes.
Methods
This prospective observational clinical study took place in an urban general hospital and involved 369 patients admitted with a documented ACS. Optimism was assessed with a standardized questionnaire. The main outcomes were physical health status, depressive symptoms, smoking, physical activity, and fruit and vegetable consumption measured 12 months after ACS, and composite major adverse cardiac events (cardiovascular death, readmission with reinfarction or unstable angina, and coronary artery bypass graft surgery) assessed over an average of 45.7 months.
Results
We found that optimism predicted better physical health status 12 months after ACS independently of baseline physical health, age, sex, ethnicity, social deprivation, and clinical risk factors (B = 0.65, 95% confidence interval [CI] = 0.10–1.20). Greater optimism also predicted reduced risk of depressive symptoms (odds ratio = 0.82, 95% CI = 0.74–0.90), more smoking cessation, and more fruit and vegetable consumption at 12 months. Persistent depressive symptoms 12 months after ACS predicted major adverse cardiac events over subsequent years (odds ratio = 2.56, 95% CI = 1.16–5.67), but only among individuals low in optimism (optimism × depression interaction; p = .014).
Conclusions
Optimism predicts better physical and emotional health after ACS. Measuring optimism may help identify individuals at risk. Pessimistic outlooks can be modified, potentially leading to improved recovery after major cardiac events.
Key words/Abbreviations: myocardial infarction, optimism, depression, recovery, ACS = acute coronary syndrome, CI = confidence interval, GRACE = Global Registry of Acute Coronary Events, BDI = Beck Depression Inventory, CHD = coronary heart disease, SES = socioeconomic status, SF-12 = 12-Item Short Form Health Survey
INTRODUCTION
Optimism is a psychological trait characterized by positive expectations about future outcomes. Optimistic dispositions seem to be associated with reduced cardiovascular mortality and morbidity (1–3). This relationship could be due to associations between optimism and the incidence of cardiovascular disease, or to more effective recovery after cardiovascular events in people with advanced disease. Optimism has been linked with lower levels of biomarkers such as interleukin-6 and C-reactive protein (4,5), better endothelial function (6), favorable lipid profiles (7), and slower progression of carotid atherosclerosis (8). Optimism has also been associated with lower risk of incident heart failure (9), has been shown to predict rehospitalization after coronary artery bypass graft surgery (10), and fewer cardiac events after percutaneous coronary interventions (11). However, the impact of optimism on recovery after acute coronary syndrome (ACS) is not known.
Optimism is not a passive trait because more optimistic individuals are proactive and exert effort to achieve positive outcomes compared with less optimistic individuals (12). In this study, we investigated the relationship between optimistic dispositions and physical health status and psychological well-being 12 months after ACS, testing the hypothesis that optimistic patients would be less depressed and have better physical health status. We also measured health behaviors including smoking, fruit and vegetable intake, and physical activity, reasoning that more optimistic patients would be more likely to stop smoking, change to a healthier diet and become more physically active than would less optimistic individuals.
Depressive symptoms after ACS have been consistently associated with recurrent cardiac events and greater morbidity (13). Optimism may protect against the adverse impact of depression. We therefore tested whether high levels of optimism buffered the effects of persistent depressive symptoms on long-term cardiac health.
METHODS
Patients and Procedure
These data are derived from two longitudinal studies of biobehavioral aspects of ACS carried out at St George’s Hospital in South London (14–16). Recruitment to the first study was carried out between December 2001 and August 2004, and the second between June 2007 and September 2008. Inclusion criteria were identical, with patients being invited to participate if they had a diagnosis of ACS based on the presence of chest pain plus verification by diagnostic electrocardiogram changes, troponin T, or troponin I ≥99th percentile of the upper reference limit. Patients were required to be 18 years or older, not to have comorbid conditions that might influence either symptom presentation or mood (e.g., neoplasia, unexplained anemia, immunotherapy, and critical ischemia), and ability to complete interviews and questionnaires in English. Patients were interviewed in the hospital when demographic data were collected together with information about symptom onset. In the first study, optimism and baseline measures of depressive symptoms and health status were assessed 7 to 10 days after ACS, whereas in the second study, measures were taken during a home visit carried out an average of 21.6 days after ACS. There were, however, no differences in levels of optimism between the two studies. Follow-up assessments of depressive symptoms, physical health status, and health behaviors were made by structured telephone interviews and questionnaires 12 months after discharge, and major adverse cardiac events were identified from hospital clinical records. The studies were approved by the National Research Ethics Service, and all patients gave signed consent.
Measures
Dispositional optimism was assessed using the revised Life Orientation Test, a widely used measure of optimistic traits that evaluates generalized expectations of positive and negative outcomes (17). Participants were asked to indicate the extent of their agreement with each item (e.g., “In uncertain times, I usually expect the best”) from 0 (strongly disagree) to 4 (strongly agree). Six items are used to derive the optimism score, so ratings can range from 0 to 24, with higher scores indicating higher levels of optimism.
The Beck Depression Inventory (BDI) was used to assess depressive symptoms (18), as recommended by an expert group in 2006 (19). This consists of 21 items rated on a scale of 0 to 3, so maximum scores can range from 0 to 63. The standard threshold of 10 or higher was used to define clinically significant depressive symptoms (20), but similar results were obtained when the BDI was analyzed as a continuous measure. Physical health status was assessed with the physical health component score from the 12-Item Short Form Health Survey (21). Limitations in physical functioning, effective role fulfillment, bodily pain, and general health perceptions contribute to total scores that can range from 0 to 100, with higher scores indicating better physical health status.
Smoking was assessed as a binary variable (current smoker/nonsmoker), and physical activity was assessed in terms of the number of times over the past week the patient had exercised vigorously (enough to make them out of breath) and the minutes of brisk walking per day. We also measured whether or not the patient had eaten at least five daily servings over the previous week of fruit and vegetables, using a biochemically validated measure (22). Major adverse cardiac events were defined as cardiovascular death, readmission with reinfarction or unstable angina, and coronary artery bypass graft surgery. This information was obtained from clinical records with an average follow-up of 45.7 (14.9) months after ACS.
Admission electrocardiograms were reviewed for presentation as ST-elevation myocardial infarction or non–ST elevation myocardial infarction or unstable angina. Cardiovascular history, clinical factors during admission, and management were obtained from clinical notes, and the extent of significant stenosis of coronary arteries and left ventricular function were obtained from angiography records. Clinical risk was assessed using the Global Registry of Acute Coronary Events (GRACE) risk score, which combines nine indices to define risk of postdischarge death after ACS (23). Lifetime history of depressive illness was assessed using standard methods (24). Socioeconomic status (SES) affects survival after ACS (25), so was assessed using a deprivation index based on three criteria: living in a crowded household, renting as opposed to owning a home, and not having use of a motor vehicle (car or van) (16). Patients were classified as low deprivation (negative on all items), medium deprivation (one positive), high (two positive), and very high (three positive).
Statistical Analysis
We analyzed optimism as a continuous variable and modeled associations between optimism and outcomes at 12 months using logistic regression for depressive symptoms, smoking status, and fruit and vegetable consumption, and linear regression for physical health status and physical activity. We included factors that might potentially confound associations with outcomes, including age, sex, ethnicity, social deprivation, history of depression, and GRACE risk score. Study sample was modeled as a dummy variable to take account of any differences between the two investigations contributing to this analysis. We also included the baseline value (obtained in the month after ACS) of each dependent variable as an additional covariate. Results are presented as adjusted odds ratios or unstandardized regression coefficients with 95% confidence intervals (CIs). We illustrate the significant associations at 12 months by comparing the outcomes in patients in the lowest and highest tertiles of optimism, after adjustment for covariates.
Information on long-term major adverse cardiac events was missing for 52 (14.1%) of the 369 patients because records could not be traced due to patient relocation or transfer to another hospital. A further 62 cases had a cardiac event before 12 months (n = 32) or failed to complete the BDI at 12 months (n = 30), so they could not be included in analyses combining optimism with persistent depression. There were no differences between patients who were included and patients who were omitted from the analysis of long-term adverse events in terms of age, sex, ethnicity, history of ACS, GRACE risk score, or optimism. We therefore tested the association between optimism and long-term clinical cardiac outcomes in the full sample for which data were available (n = 317), and the interaction between optimism and persistent depression (clinically significant symptoms at 12 months) in 255 cases. The odds of major adverse cardiac events were calculated, adjusting for age, sex, ethnicity, social deprivation, history of depression, GRACE risk score, and study sample. When testing the interaction between optimism and depression, we computed the cross-product between continuous optimism (reverse scored) and depressive symptom ratings and entered it into a regression on major adverse cardiac events. The significant interaction was illustrated by dividing the sample into higher and lower optimism subgroups by binary split and creating four categories of patient: higher optimism/low depressive symptoms, higher optimism/high depressive symptoms, lower optimism/low depressive symptoms, and lower optimism/high depressive symptoms. In supplementary analyses, we added history of ACS and number of coronary arteries with significant stenosis to all the analyses, but the findings were unchanged (results not shown).
RESULTS
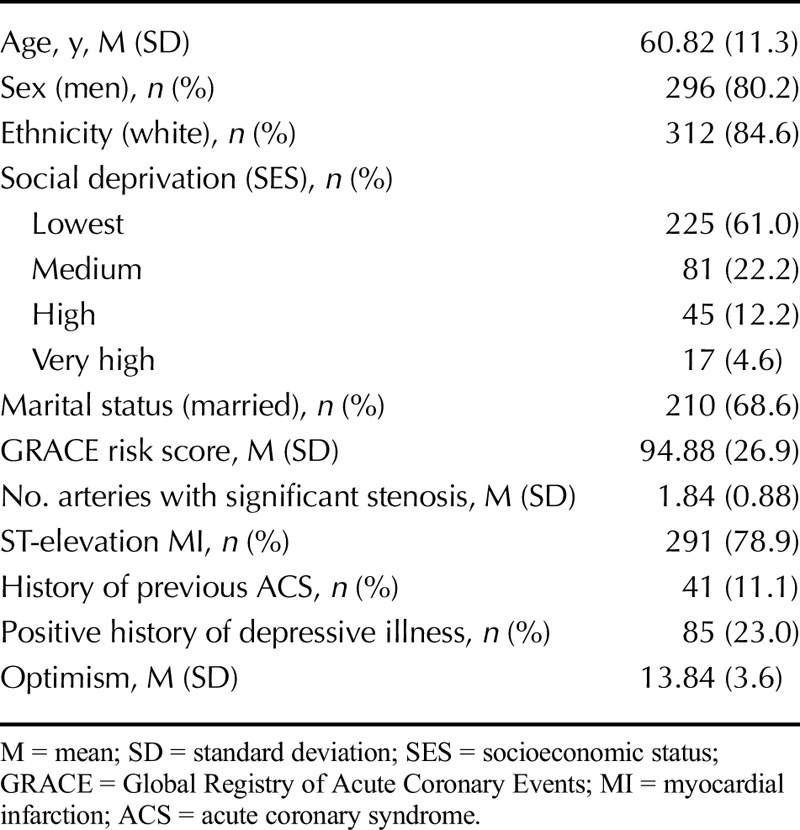
The study group consisted of 296 male and 73 female ACS patients, as detailed in Table 1. Most patients were white men who had experienced an ST-elevation myocardial infarction. Optimism was not related to age, sex, ethnicity, social deprivation, ACS type, GRACE risk score, number of arteries with significant stenosis, history of ACS, severity of CAD, or left ventricular function.
TABLE 1.
Characteristics of Study Participants
Depressive symptoms increased from 3 weeks to 12 months after ACS, and the proportion of patients with clinically significant symptoms rose from 24.6% to 31.7% (p = .011), whereas physical health status improved from a mean of 49.3 (20.0) to 52.5 (21.4) over the same period (p < .001). Smoking prevalence fell from 36.9% to 10.9% at 12 months (p < .001), whereas at 12 months, 30.5% consumed five or more servings of fruit and vegetables per day. There was no change in vigorous physical activity, but patients reported increasing brisk walking from 11.76 to 27.80 min/d (p = .027). There were 85 (26.8%) major adverse cardiac events over the follow-up period between 12 and 45.7 months.
Optimism and Recovery After ACS
We found an inverse cross-sectional association between optimism and depressive symptoms measured at baseline immediately after ACS (r = −0.39, p < .001). Optimism also predicted low risk of depressive symptoms after 12 months, with an odds ratio of 0.82 (95% CI = 0.74–0.90, p < .001) after adjusting statistically for baseline depression level, age, sex, ethnicity, SES, history of clinical depression, GRACE risk score, and study sample. As illustrated in Figure 1, clinically significant depressive symptoms were twice as common in the low than high optimism tertiles after adjusting for covariates. The adjusted BDI scores averaged 6.99 (4.71), 8.19 (5.81), and 10.67 (11.46) in the low, medium, and high optimism tertiles, respectively (p < .001).
FIGURE 1.
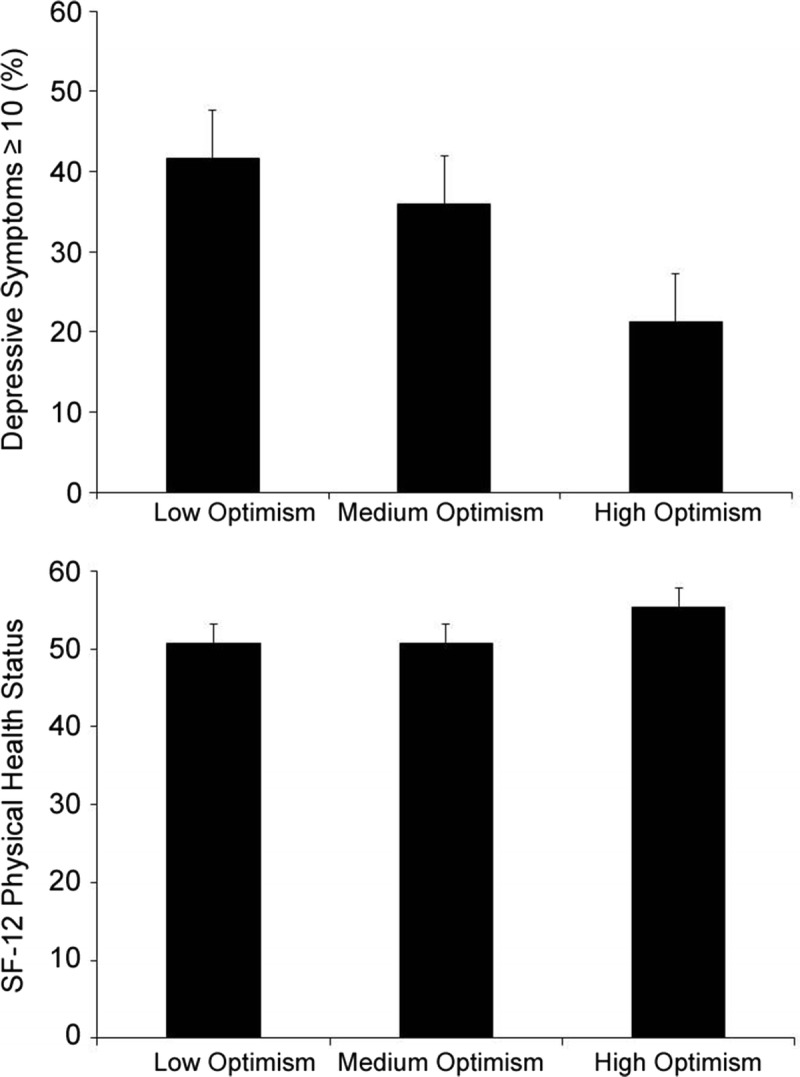
Upper panel: proportion of patients with depressive symptoms ≥10 at 12 months after ACS in the low, medium, and high tertiles of optimism, adjusted for depressive symptoms at baselines, age, sex, ethnicity, SES, history of depression, and GRACE risk scores. The adjusted difference was significant at p < .001. Error bars are SEM. Lower panel: mean SF-12 physical health status scores at 12 months after ACS in the low, medium, and high tertiles of optimism, adjusted for baseline physical health status and the other covariates listed above. The adjusted difference was significant at p = .05. Error bars indicate SEM. ACS = acute coronary syndrome; SES = socioeconomic status; GRACE = Global Registry of Acute Coronary Events; SEM = standard error of the mean; SF-12 = 12-Item Short Form Health Survey.
We found that optimism was not related to physical health status in the month after ACS (p = .50). However, after 12 months, physical health status scores were more positive in optimistic patients (B = 0.65, 95% CI = 0.10–1.20, p = .022) after adjusting for baseline health status, clinical, and sociodemographic covariates, and study sample. The adjusted physical health status scores averaged 4.6 points higher in the high than low optimism tertile (Fig. 1), although the association was not linear, with individuals in the medium tertile having similar ratings to those in the low tertile.
Optimism and Health Behavior 12 Months After ACS
Optimism was not related to smoking status, fruit and vegetable intake, or physical activity in the month after ACS, but we found that optimism predicted a reduction in smoking after 12 months independently of age, sex, ethnicity, SES, history of depression, GRACE risk score, and study sample (odds ratio = 0.84. 95% CI = 0.73–0.96, p = .01). After 12 months, 47.9% of smokers at baseline in the low tertile of optimism continued to smoke, compared with only 15.3% of patients in the high optimism tertile (Fig. 2). The proportion of patients eating five or more servings of fruit and vegetables per day was positively associated with optimism (adjusted odds ratio = 1.13, 95% CI = 0.13–1.23, p = .007), with twice as many patients in the high than low optimism tertile eating adequate fruit and vegetables (Fig. 2). By contrast, changes in physical activity were not related to optimism.
FIGURE 2.
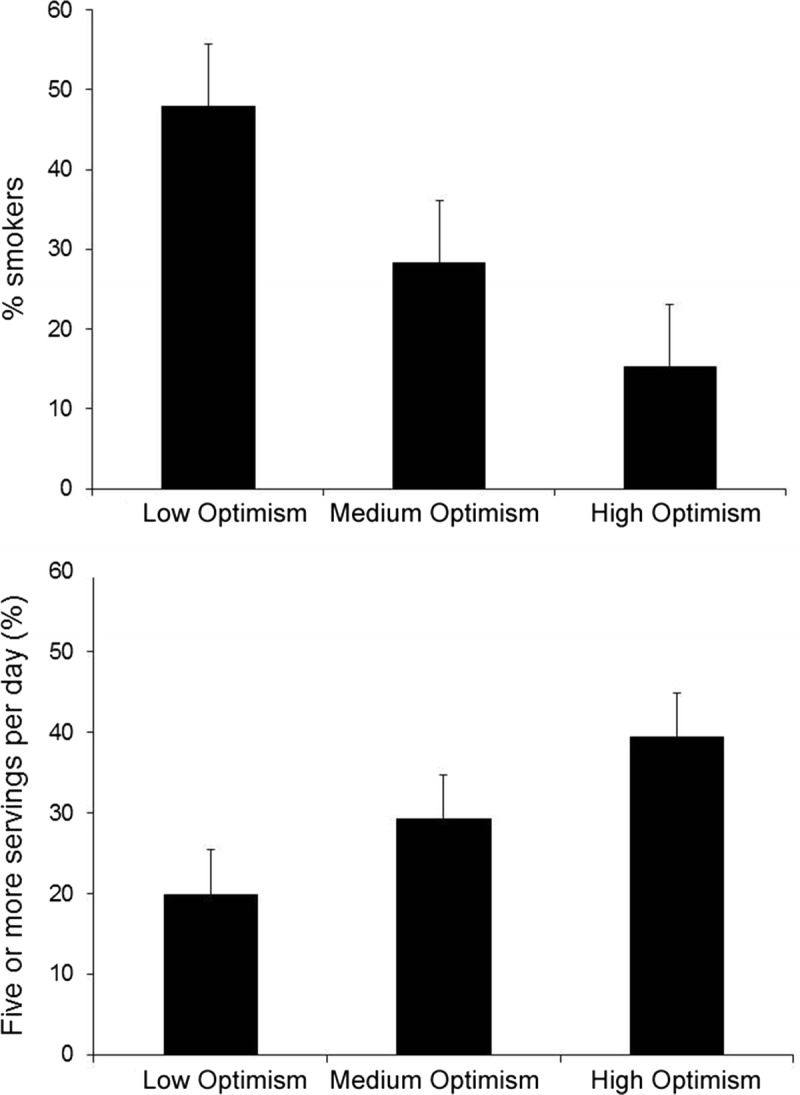
Upper panel: proportion of smokers at the time of ACS who were still smoking 12 months later in the low, medium, and high tertiles of optimism, adjusted for the covariates listed for Figure 1. The adjusted difference was significant at p = .004. Error bars indicate SEM. Lower panel: proportion of patients eating five or more servings of fruit and vegetables per day at 12 months after ACS in the low, medium, and high tertiles of optimism, adjusted for the covariates listed for Figure 1. The adjusted difference was significant at p = .009. Error bars are SEM. ACS = acute coronary syndrome; SEM = standard error of the mean.
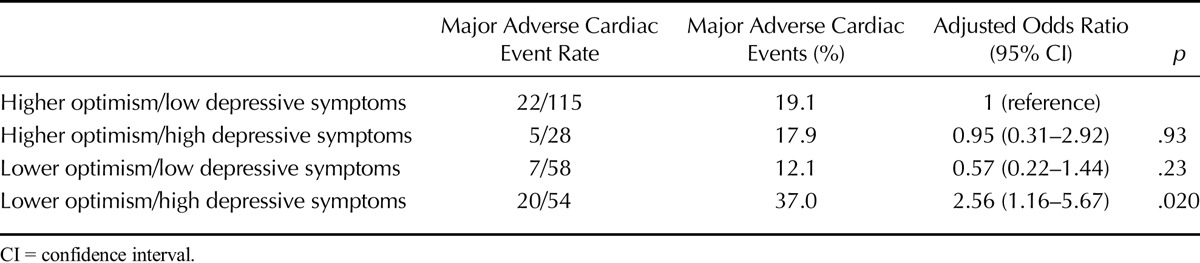
Optimism, Depression, and Long-Term Clinical Outcome
The odds of major adverse cardiac events were reduced for every unit increase in optimism score (odds ratio = 0.97, 95% CI = 0.90–1.05), but the association was not significant. However, the cross-product of optimism (reverse scored) and depression at 12 months (both measured as continuous variables) was associated with the occurrence of major adverse cardiac events after adjusting for covariates (odds ratio = 1.13, 95% CI = 1.03–1.2, p = .014). In this model examining the interaction, the main effect for optimism (odds ratio = 0.80, 95% CI = 0.67–0.96, p = .017) was significant, but not the main effect for depression (odds ratio = 0.98, 95% CI = 0.92–1.05, p = .54). In addition, patients reporting low optimism coupled with high depressive symptoms were at increased risk. This association is illustrated by analysis of patients’ higher and lower in optimism defined by binary split, and with and without clinically significant depressive symptoms. It should be noted that although four groups were created using this method, the proportion of patients in the higher optimism/high depressive symptom category is small (n = 5; see Table 2). Nonetheless, 37% patients with clinically significant depressive symptoms at 12 months who were low in optimism had a further cardiac event or death, compared with 19.1% in the higher optimism/low depressive symptom category (Table 2). The odds of a major adverse event in the lower optimism/high depressive symptom category were 2.56 (95% CI = 1.16–5.67, p = .020) adjusted for age, sex, ethnicity, SES, history of depression, GRACE risk score, and study sample. Optimism seemed to protect against the impact of persistent depressive symptoms because patients in the higher optimism/high depressive symptom category did not show an elevated major adverse cardiac event rate.
TABLE 2.
Optimism, Persistent Depressive Symptoms, and Clinical Cardiac Outcome
DISCUSSION
Our study found that optimistic patients showed better recovery 12 months after an ACS, as evidenced by fewer depressive symptoms and better physical health status. These associations were independent of demographic and clinical factors. We also hypothesized that optimistic patients would be more likely to stop smoking, improve their diet, and become more physically active than patients low in optimism. Our results were moderately supportive, in that patients higher in optimism were more likely to stop smoking and eat more fruit and vegetables. There was, however, no association between optimism and changes in physical activity. In addition, we found that optimism seemed to protect against the long-term adverse effects of depression on cardiac morbidity and mortality. With the exception of physical health status, the associations were linear across the optimism distribution.
It has previously been reported that optimism is associated with reduced cardiovascular mortality. For example, Giltay et al. (1) found that older men without previous cardiovascular disease in the upper tertile of optimism had a hazard ratio of 0.45 (95% CI = 0.29–0.68) for cardiovascular mortality over the next 15 years compared with those in the lowest optimism tertile. In the Women’s Health Initiative, optimists had reduced all-cause and cardiovascular mortality over an average of 8-year period, independently of covariates (2), whereas optimism was associated with reduced coronary heart disease (CHD) risk in the Whitehall II study (26) and reduced incident heart failure in the Health and Retirement Study (9). Such effects could be the result of optimism affecting the incidence of cardiovascular disease, or because optimism is associated with better recovery after acute cardiac events. Associations with CHD incidence have been somewhat inconsistent, showing positive associations with level of optimism in some studies but not others (27,28). With regard to adaptation after cardiac events, associations between dispositional optimism and more effective recovery from cardiac surgery have been described, with lower rates of rehospitalization after coronary artery bypass graft in more optimistic individuals (10,29). Associations between optimism and recovery after ACS have not been described before, but our results suggest that the favorable effects of optimism extend to recovery after acute cardiac events as well.
Not only was optimism associated with better physical health status 12 months after ACS, it also seemed to predict greater psychological well-being. Depressive symptoms are common after cardiovascular events (30) and are associated with poor recovery and quality of life as well as mortality among ACS patients (13,31). Dispositional optimism may protect against depression in people with serious physical illness, and inverse associations between optimism and depressive symptoms have been described after breast cancer surgery (32) and in CHD patients (33). Our analyses document a substantial protective effect, with a two-fold difference in elevated depressive symptoms at 12 months in patients in the highest versus lowest tertile of optimism, even after controlling for depressive symptoms at baseline.
Our results also suggest that more optimistic patients actively promote recovery after ACS by making changes toward healthier life-styles. Smoking cessation was more common among optimists, who also reported greater consumption of fruit and vegetables. Together with the difference in psychological well-being, these behaviors may contribute to enhanced recovery. The one behavior that was not related to optimism was physical activity. Patients reported that they carried out more brisk walking at 12 months compared with the month after ACS, but the effect was not associated with optimism. The reasons are not clear, but a previous study of elderly patients with a history of CHD also showed no association (34). The limited reliability, validity, and sensitivity to change of self-report measures of physical activity in this population may be relevant, and objective measures would provide a stronger test of the association between optimism and physical activity.
There was a small increase in the prevalence of clinically significant depressive symptoms between 3 weeks and 12 months after ACS. Although decreases are sometime recorded (35), previous findings have been quite varied, with stable levels in some clinical cohorts (36,37) and increases due to new-onset symptoms in others (38,39). The explanation for these variations is not clear.
Our study did not demonstrate that optimism in isolation was associated with reduced risk of major adverse cardiac events; although the odds ratio was reduced among patients with greater optimism, the effect was not significant. Hence, low optimism in itself was not detrimental to cardiac health in this sample. However, we did find that optimism seemed to buffer the impact of persistent depression on cardiac outcomes. This suggests that optimism may ameliorate the negative influence of depressive symptoms, possibly through the enhancement of protective health behaviors. The primary evidence for this association emerged from analyses using the cross-product of optimism and 12-month depressive symptom scores, but effects were corroborated by division of the cohort into four categories based on optimism and depression ratings. It should be noted that the average optimism ratings were relatively low; unpublished ratings from more than 500 healthy men and women of a similar age to these patients have an average of 15.72 (4.0) compared with 13.84 (3.6) in our ACS patients. As would be expected, the combination of higher optimism and high depressive symptoms was relatively rare, being observed in only 19% of respondents in the higher optimism category.
Strengths of this study include the longitudinal design, with assessments soon after hospitalization with ACS, at 12 months after the cardiac event, and with longer-term cardiac outcomes. We used standardized and well-established measures of optimism, physical health status, and depressive symptoms, and we were able to control statistically for clinical cardiologic factors.
There are also a number of limitations. Optimism was assessed over the month after ACS and at different average time intervals since ACS in the two longitudinal studies on which the analyses are based. These ratings may, in part, reflect patients’ perceptions of their recovery and prognosis, rather than more general psychological dispositions. We did not record physician-patient interactions but conjectured that if this was the explanation, then less optimistic patients would have poorer physical health status in the month after ACS; this was not the case. However, optimism is a moderately stable trait (1), so it is unlikely to have changed after ACS. We failed to track all the patients for long-term adverse cardiac events. However, there were no striking differences between patients who were included and missing from long-term follow-up. We ascertained clinical outcomes from hospital notes without independent adjudication and used a composite end point because there were insufficient cases for analysing separate outcomes. We were not able to assess other causes of death such as cancer, although other studies have suggested associations with low optimism (40). The measures of health behavior, depressive symptoms, and physical health status were collected by self-report and were not corroborated with objective assessments. This was an observational study, so we cannot infer a causal association between optimism and cardiac outcomes.
In conclusion, our results indicate that optimistic dispositions predict better recovery after ACS in terms of physical health status, depressive symptoms, and behaviors relevant to long-term prognosis, and that these effects are independent of demographic and clinical factors. These effects are consistent with previous studies of patients undergoing cardiac surgical interventions. Optimism also seems to buffer the adverse impact of persistent depressive symptoms on long-term cardiac outcomes. Measurement of optimism might lead to more accurate identification of individuals at risk for poor adaptation. In addition, cognitive-behavioral interventions can increase optimism (41), so it is possible that less optimistic perspectives in cardiac patients are malleable, potentially leading to improved adaptation after major cardiac events.
Acknowledgments
Source of Funding and Conflicts of Interest: This study was supported by the British Heart Foundation (RG/05/006). The authors report no conflicts of interest. The funders of this work were not involved with the analyses of these data or production of this paper.
REFERENCES
- 1. Giltay EJ, Kamphuis MH, Kalmijn S, Zitman FG, Kromhout D. Dispositional optimism and the risk of cardiovascular death: the Zutphen Elderly Study. Arch Intern Med 2006; 166: 431– 6. [DOI] [PubMed] [Google Scholar]
- 2. Tindle HA, Chang Y-F, Kuller LH, Manson JE, Robinson JG, Rosal MC, Siegle GJ, Matthews KA. Optimism, cynical hostility, and incident coronary heart disease and mortality in the Women’s Health Initiative. Circulation 2009; 120: 656– 62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Nabi H, Koskenvuo M, Singh-Manoux A, Korkeila J, Suominen S, Korkeila K, Vahtera J, Kivimäki M. Low pessimism protects against stroke: the Health and Social Support (HeSSup) prospective cohort study. Stroke 2010; 41: 187– 90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Brydon L, Walker C, Wawrzyniak AJ, Chart H, Steptoe A. Dispositional optimism and stress-induced changes in immunity and negative mood. Brain Behav Immun 2009; 23: 810– 6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Roy B, Diez-Roux AV, Seeman T, Ranjit N, Shea S, Cushman M. Association of optimism and pessimism with inflammation and hemostasis in the Multi-Ethnic Study of Atherosclerosis (MESA). Psychosom Med 2010; 72: 134– 40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Ikeda A, Schwartz J, Peters JL, Fang S, Spiro A, Sparrow D, Vokonas P, Kubzansky LD. Optimism in relation to inflammation and endothelial dysfunction in older men: the VA Normative Aging Study. Psychosom Med 2011; 73: 664– 71. [DOI] [PubMed] [Google Scholar]
- 7. Boehm JK, Williams DR, Rimm EB, Ryff C, Kubzansky LD. Relation between optimism and lipids in midlife. Am J Cardiol 2013; 111: 1425– 31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Matthews KA, Räikkönen K, Sutton-Tyrrell K, Kuller LH. Optimistic attitudes protect against progression of carotid atherosclerosis in healthy middle-aged women. Psychosom Med 2004; 66: 640– 4. [DOI] [PubMed] [Google Scholar]
- 9. Kim ES, Smith J, Kubzansky LD. A prospective study of the association between dispositional optimism and incident heart failure. Circ Heart Fail 2014; 7: 394– 400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Scheier MF, Matthews KA, Owens JF, Schulz R, Bridges MW, Magovern GJ, Carver CS. Optimism and rehospitalization after coronary artery bypass graft surgery. Arch Intern Med 1999; 159: 829– 35. [DOI] [PubMed] [Google Scholar]
- 11. Helgeson VS, Fritz HL. Cognitive adaptation as a predictor of new coronary events after percutaneous transluminal coronary angioplasty. Psychosom Med 1999; 61: 488– 95. [DOI] [PubMed] [Google Scholar]
- 12. Carver CS, Scheier MF, Segerstrom SC. Optimism. Clin Psychol Rev 2010; 30: 879– 89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Lichtman JH, Froelicher ES, Blumenthal JA, Carney RM, Doering LV, Frasure-Smith N, Freedland KE, Jaffe AS, Leifheit-Limson EC, Sheps DS, Vaccarino V, Wulsin L. Depression as a risk factor for poor prognosis among patients with acute coronary syndrome: systematic review and recommendations: a scientific statement from the American Heart Association. Circulation 2014; 129: 1350– 69. [DOI] [PubMed] [Google Scholar]
- 14. Bhattacharyya MR, Perkins-Porras L, Wikman A, Steptoe A. The long-term effects of acute triggers of acute coronary syndromes on adaptation and quality of life. Int J Cardiol 2010; 138: 246– 52. [DOI] [PubMed] [Google Scholar]
- 15. Steptoe A, Molloy GJ, Messerli-Bürgy N, Wikman A, Randall G, Perkins-Porras L, Kaski JC. Fear of dying and inflammation following acute coronary syndrome. Eur Heart J 2011; 32: 2405– 11. [DOI] [PubMed] [Google Scholar]
- 16. Strike PC, Perkins-Porras L, Whitehead DL, McEwan J, Steptoe A. Triggering of acute coronary syndromes by physical exertion and anger: clinical and sociodemographic characteristics. Heart 2006; 92: 1035– 40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Scheier MF, Carver CS, Bridges MW. Distinguishing optimism from neuroticism (and trait anxiety, self-mastery, and self-esteem): a reevaluation of the Life Orientation Test. J Pers Soc Psychol 1994; 67: 1063– 78. [DOI] [PubMed] [Google Scholar]
- 18. Beck AT, Steer RA, Carbin MG. Psychometric properties of the Beck Depression Inventory: twenty-five years of evaluation. Clin Psychol Rev 1988; 8: 77– 100. [Google Scholar]
- 19. Davidson KW, Kupfer DJ, Bigger JT, Califf RM, Carney RM, Coyne JC, Czajkowski SM, Frank E, Frasure-Smith N, Freedland KE, Froelicher ES, Glassman AH, Katon WJ, Kaufmann PG, Kessler RC, Kraemer HC, Krishnan KRR, Lespérance F, Rieckmann N, Sheps DS, Suls JM. Assessment and treatment of depression in patients with cardiovascular disease: National Heart, Lung, and Blood Institute Working Group Report. Psychosom Med 2006; 68: 645– 50. [DOI] [PubMed] [Google Scholar]
- 20. Zuidersma M, Conradi HJ, van Melle JP, Ormel J, de Jonge P. Self-reported depressive symptoms, diagnosed clinical depression and cardiac morbidity and mortality after myocardial infarction. Int J Cardiol 2013; 167: 2775– 80. [DOI] [PubMed] [Google Scholar]
- 21. Gandek B, Ware JE, Aaronson NK, Apolone G, Bjorner JB, Brazier JE, Bullinger M, Kaasa S, Leplege A, Prieto L, Sullivan M. Cross-validation of item selection and scoring for the SF-12 Health Survey in nine countries: results from the IQOLA Project. J Clin Epidemiol 1998; 51: 1171– 8. [DOI] [PubMed] [Google Scholar]
- 22. Cappuccio FP, Rink E, Perkins-Porras L, McKay C, Hilton S, Steptoe A. Estimation of fruit and vegetable intake using a two-item dietary questionnaire: a potential tool for primary health care workers. Nutr Metab Cardiovasc Dis 2003; 13: 12– 9. [DOI] [PubMed] [Google Scholar]
- 23. Eagle KA, Lim MJ, Dabbous OH, Pieper KS, Goldberg RJ, Van de Werf F, Goodman SG, Granger CB, Steg PG, Gore JM, Budaj A, Avezum A, Flather MD, Fox KAA. A validated prediction model for all forms of acute coronary syndrome: estimating the risk of 6-month postdischarge death in an international registry. JAMA 2004; 291: 2727– 33. [DOI] [PubMed] [Google Scholar]
- 24. Freedland KE, Skala JA, Carney RM, Raczynski JM, Taylor CB, de Leon CFM, Ironson G, Youngblood ME, Krishnan KRR, Veith RC. The Depression Interview and Structured Hamilton (DISH): rationale, development, characteristics, and clinical validity. Psychosom Med 2002; 64: 897– 905. [DOI] [PubMed] [Google Scholar]
- 25. Alter DA, Chong A, Austin PC, Mustard C, Iron K, Williams JI, Morgan CD, Tu JV, Irvine J, Naylor CD. Socioeconomic status and mortality after acute myocardial infarction. Ann Intern Med 2006; 144: 82– 93. [DOI] [PubMed] [Google Scholar]
- 26. Boehm JK, Peterson C, Kivimaki M, Kubzansky LD. Heart health when life is satisfying: evidence from the Whitehall II cohort study. Eur Heart J 2011; 32: 2672– 7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Hansen JD, Shimbo D, Shaffer JA, Hong S, Borda T, Ventura A, Scwartz JE, Harlapur M, Davidson KW. Finding the glass half full? Optimism is protective of 10-year incident CHD in a population-based study: the Canadian Nova Scotia Health Survey. Int J Cardiol 2010; 145: 603– 4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Kubzansky LD, Sparrow D, Vokonas P, Kawachi I. Is the glass half empty or half full? A prospective study of optimism and coronary heart disease in the normative aging study. Psychosom Med 2001; 63: 910– 6. [DOI] [PubMed] [Google Scholar]
- 29. Tindle H, Belnap BH, Houck PR, Mazumdar S, Scheier MF, Matthews KA, He F, Rollman BL. Optimism, response to treatment of depression, and rehospitalization after coronary artery bypass graft surgery. Psychosom Med 2012; 74: 200– 7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Thombs BD, Bass EB, Ford DE, Stewart KJ, Tsilidis KK, Patel U, Fauerbach JA, Bush DE, Ziegelstein RC. Prevalence of depression in survivors of acute myocardial infarction. J Gen Intern Med 2006; 21: 30– 8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Dickens C, Cherrington A, McGowan L. Depression and health-related quality of life in people with coronary heart disease: a systematic review. Eur J Cardiovasc Nurs 2012; 11: 265– 75. [DOI] [PubMed] [Google Scholar]
- 32. Schou I, Ekeberg Ø, Ruland CM, Sandvik L, Kåresen R. Pessimism as a predictor of emotional morbidity one year following breast cancer surgery. Psychooncology 2004; 13: 309– 20. [DOI] [PubMed] [Google Scholar]
- 33. Shnek ZM, Irvine J, Stewart D, Abbey S. Psychological factors and depressive symptoms in ischemic heart disease. Health Psychol 2001; 20: 141. [DOI] [PubMed] [Google Scholar]
- 34. Rius-Ottenheim N, Geleijnse JM, Kromhout D, van der Mast RC, Zitman FG, Giltay EJ. Physical activity after myocardial infarction: is it related to mental health? Eur J Prev Cardiol 2013; 20: 399– 408. [DOI] [PubMed] [Google Scholar]
- 35. Thombs BD, Ziegelstein RC, Stewart DE, Abbey SE, Parakh K, Grace SL. Usefulness of persistent symptoms of depression to predict physical health status 12 months after an acute coronary syndrome. Am J Cardiol 2008; 101: 15– 9. [DOI] [PubMed] [Google Scholar]
- 36. Martens EJ, Smith OR, Winter J, Denollet J, Pedersen SS. Cardiac history, prior depression and personality predict course of depressive symptoms after myocardial infarction. Psychol Med 2008; 38: 257– 64. [DOI] [PubMed] [Google Scholar]
- 37. Spijkerman TA, van den Brink RH, Jansen JH, Crijns HJ, Ormel J. Who is at risk of post-MI depressive symptoms? J Psychosom Res 2005; 58: 425– 32. [DOI] [PubMed] [Google Scholar]
- 38. Freiheit EA, Hogan DB, Eliasziw M, Patten SB, Demchuk AM, Faris P, Anderson T, Galbraith D, Parboosingh JS, Ghali WA, Knudtson M, Maxwell CJ. A dynamic view of depressive symptoms and neurocognitive change among patients with coronary artery disease. Arch Gen Psychiatry 2012; 69: 244– 55. [DOI] [PubMed] [Google Scholar]
- 39. Strik JJ, Lousberg R, Cheriex EC, Honig A. One year cumulative incidence of depression following myocardial infarction and impact on cardiac outcome. J Psychosom Res 2004; 56: 59– 66. [DOI] [PubMed] [Google Scholar]
- 40. Giltay EJ, Geleijnse JM, Zitman FG, Hoekstra T, Schouten EG. Dispositional optimism and all-cause and cardiovascular mortality in a prospective cohort of elderly Dutch men and women. Arch Gen Psychiatry 2004; 61: 1126– 35. [DOI] [PubMed] [Google Scholar]
- 41. Meevissen Y, Peters ML, Alberts HJ. Become more optimistic by imagining a best possible self: effects of a two week intervention. J Behav Ther Exp Psychiatry 2011; 42: 371– 8. [DOI] [PubMed] [Google Scholar]


