Abstract
Introduction
Tracheal varices are a rare condition but they can be an important source of massive or recurrent haemoptysis. Usually they are related to increased pressure in the pulmonary veins. Mediastinal goiter is often associated to compressive effects on the surrounding structures, including mediastinal vessels with potential superior vena cava syndrome.
Case report
We describe a case, not previously reported in literature, of mediastinal goiter with hemoptysis as first clinical manifestation. Bleeding was attributed to a superior vena cava syndrome associated to a tracheal fragile mucosa with an easily bleeding intramural nodule which was diagnosed as tracheal varices after total thyroidectomy. The nodule in fact disappeared together with the venous hypertensive signs after venous decompression of the mediastinum.
Conclusions
Compressive symptoms including tracheal varices, related to mediastinal goiter, can be treated surgically by total thyroidectomy via cervicotomy and when required with associated median sternotomy.
Keywords: Mediastinal goiter, Tracheal varices, Vena cava syndrome, Hemoptysis, Thyroidectomy
Introduction
Tracheal varices (TV) are a rare condition, but they can be an important source of massive or recurrent haemoptysis. They are described at endoscopy as easily bleeding singular or multiple tracheal nodes (1). Possible causes are increased pressure in the pulmonary veins due to mitral valve stenosis, venous occlusive disease, consequences after pediatric cardiac surgery (1). Mediastinal goiter (MG) is one of the possible cause of mediastinal compression with superior vena cava syndrome (SVCS) (2) and consequent reduced flow from tracheal veins. We report a case of SVCS due to the presence of a large MG in which symptomatic TV were observed but correctly diagnosed only after total thyroidectomy. In our knowledge this is the first report in literature.
Case report
A male patient, 58 years old, with history of high blood pressure and tabagism, was admitted in our institution for severe recurrent hemoptysis. Physical examination showed distention of superficial neck and thoracic veins and eyelids edema. No neck mass was detected. Thoracic and abdominal clinical examination resulted normal. All laboratory tests resulted within the normal ranges.
Chest x-ray showed a mediastinal mass and a left tracheal deviation but did not show any pulmonary lesion. Therefore the patient underwent neck and thorax CT which showed diffusely enlarged thyroid gland with extension below the substernal notch to the tracheal bifurcation.
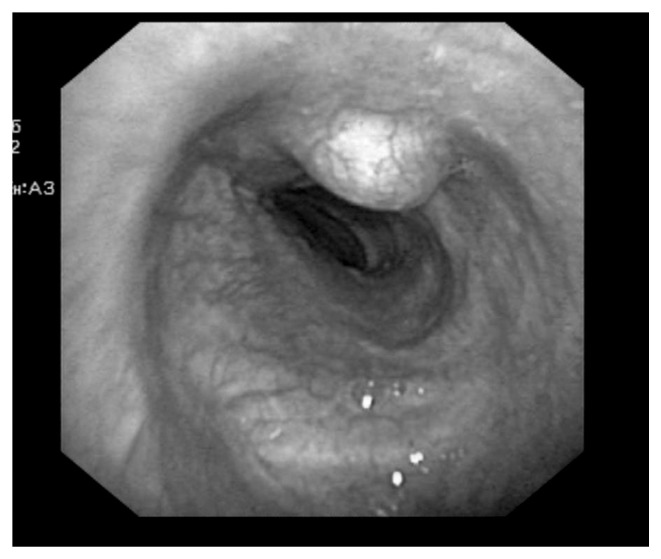
Enlargement of the gland was asymmetrical, with prevalence of the right lobe, presenting two large nodules respectively 80x45 and 85x68 mm large. The mediastinal portion of the goiter reached the right bronchus determining a severe tracheal compression with deviation to the left side. Venous collateral circulation and a polypoid lesion of the pars membranacea of the trachea were observed. We decided to perform a fiberoptic bronchoscopy which showed congested and easily bleeding cervical tracheal mucosa with a purple polypoid formation of the pars membranacea (Figure 1). The biopsy on the polypoid lesion caused a severe bleeding which was very demanding to control. Histological examination excluded the presence of cancer cells.
Fig. 1.
Endoscopic image of the cervical trachea presenting congested and easily bleeding mucosa with a purple polyp-shaped mass of the pars membranacea.
Since clinical signs of SVCS associated to clear radiological and endoscopic evidence of tracheal venous hypertension, we hypothesized to deal with TV due to the large MG with compressive effect. Since absolute indication to perform a thyroidectomy we gave primary surgical indication proposing an eventual subsequent endoscopic biopsy by rigid bronchoscopy, after the removal of the mediastinal mass, in order to check if there was a specific correlation between MG and TV. The patient decided to accept the procedure and underwent total thyroidectomy via cervicotomy and combined sternotomy. The postoperative course was uneventful and the patient was discharged in postoperative day 5 after a flexible bronchoscopy which showed the disappearance of the venous collateral circles and also of the polypoid tracheal lesion. Histology demonstrated diffuse struma with papillary carcinoma (pT3). After surgery the patient was referred to radioiodine treatment. At one year follow-up he presented no signs of cancer progression and a complete remission of the indirect signs of venous hypertension of the neck and of the thoracic wall, without recurrence of hemoptysis. At one year control, brochoscopy showed a normal picture of the tracheal mucosa without any signs of recurrent TV.
Discussion
Intrathoracic thyroid masses account for 5.8% of all mediastinal masses (3). The definition of MG generally refers to a struma with a location for at least 50% of its volume in substernal position (4). For embryologic reasons, MG are mostly located in the anterior and middle mediastinum, and rarely in the posterior mediastinum. Up to 40% of MG are asymptomatic and they are diagnosed incidentally (5). When clinically manifest, MG is usually associated to compressive symptoms which mainly determine effects on surrounding structures, especially on the trachea with consequent dislocation producing choking, dyspnoea and sleeping apnea or on the oesophagus with dysphagia. Less frequently are observed compressive effects on cervical and mediastinal neurovascular structures with rare cases of SVCS due to venous compression and thrombosis and even of Horner’s syndrome for chronic compression on the sympathetic chain (5–7). Total thyroidectomy with en bloc removal of the intrathoracic portion of the thyroid, is the treatment of choice. Usually a cervical approach is appropriate in most of the cases being the mediastinal portion easily externalized by traction and digital manoeuvres. In selected cases a partial or complete median sternotomy or a thoracotomy are required to achieve radical excision without haemorrhagic complications (8).
SVCS is characterized by facial congestion, venous distension of the chest wall, arm swelling, and facial plethora which may worsen in the supine position. The primary causes of this syndrome are mediastinal malignancies especially mediastinal lymphadenopaty. Nevertheless many benign causes of SVCS such as mediastinal fibrosis, venous thrombosis and tuberculous mediastinitis are described (9). As reported for the first time by Steenerson et al. in 1978, MG can be either considered a potential cause of SVCS (10–13). In MG compressive symptoms are always associated to venous collateral circulation as described by some authors, reporting clinically evident SVCS due to MG, whose clinical presentation were recurrent episodes of hematemesis (7, 14–16). In these patients esophagogastroduodenoscopy usually shows upper esophageal varices. This scenario of “portal pseudo-hypertension” (15) is related to the large MG extending below the carina which causes compression of the right innominate vein generating multiple dilated collaterals, including esophageal superior plexus, which drains into the innominate veins through the inferior thyroid veins. Whereas “portal pseudo-hypertension” presenting with hematemesis is seldom described in literature associated to MG in the clinical picture of SVCS, in our knowledge there are no reports of TV in the same setting. TV are uncommon but an important source of massive or recurrent hemoptysis. They are a rare cause of benign mural nodules in the trachea together with amiloydosis, sarcoidosis, inflammatory pseudotumor and rheumatoid nodules (1). The evidence of extensive tracheal collateral vessels should raise suspicion. The principal cause of tracheal varices is pulmonary venous hypertension usually due to mitral valve stenosis, to venous occlusive disease and to the postoperative consequences of cardiac surgery (1). The rationale for considering our observation related to the association of TV to MG with SVCS is founded on the evidence that after removal of the mediastinal mass, the improved venous hypertension immediately determined the complete regression of the tracheal nodule and of the mucosal congestion as they were related to venous decompression.
The anatomical and physiological bases are that the blood supply to the cervical trachea is different from that of the thoracic portion. In fact in the former, arteries originate from the inferior thyroid arteries whereas veins drain into the inferior thyroid venous plexus which itself drains into the innominate vein and the superior vena cava.
Large MG therefore, may generate a compression on innominate vein with difficult venous drainage upstream which may cause tracheal veins plexus distention. This can be clinically evident at brochoscopy and be confused with small mural nodules as in our observation. The use of CT which is normally adopted in the preoperative study of MG (8), although without iodine contrast, is useful to eventually detect anomalous circulation around the trachea and the presence of intramural nodules which are not otherwise defined without a vascular phase study. The adoption of bronchoscopy and esophagogastroduodenoscopy in a SVCS can detect the presence of both suspicious tracheal and esophageal varices. A biopsy in this event can be associated to the risk of severe bleeding as in our experience and must be avoided if TV are suspected by endotracheal nodules in presence of large MG and SVCS.
The treatment of TV is therefore consequent to that of MG, being total thyroidectomy, via a cervical approach alone or in selected patients associated to a partial or total sternotomy, the standard of treatment (2, 8).
Conclusions
Although rare TV are potentially associated to MG in a clinical condition of SVCS due to mediastinal compression. Hemoptysis can be present together with specific CT and broncoscopic signs. The only treatment is related to mediastinal decompression which is obtained by total thyroidectomy.
Footnotes
Conflict of interest
The Authors declare that there is no conflict of interest and there are no financial sponsors for this research.
References
- 1.Grillo HC. Tumorlike lesions of trachea. Hamilton: BC Decker Inc; 2004. Surgery of trachea and bronchi; pp. 98–102. [Google Scholar]
- 2.Polistena A, Monacelli M, Lucchini R, Triola R, Conti C, Avenia S, Rondelli F, Bugiantella W, Barillaro I, Sanguinetti A, Avenia N. Surgical management of mediastinal goiter in the elderly. Int J Surg. 2014;12:S148–S152. doi: 10.1016/j.ijsu.2014.08.360. [DOI] [PubMed] [Google Scholar]
- 3.Migliore M, Costanzo M, Cannizzaro MA. Cervico-mediastinal goiter: is telescopic exploration of the mediastinum (videomedia-stinoscopy) useful? Interact Cardiovasc Thorac Surg. 2010;10:439–40. doi: 10.1510/icvts.2009.217638. [DOI] [PubMed] [Google Scholar]
- 4.Rugiu MG, Piemonte M. Surgical approach to retrosternal goitre: do we still need sternotomy? Acta Otorhinolaryngol Ital. 2009;29:331–8. [PMC free article] [PubMed] [Google Scholar]
- 5.Shen WT, Kepebew E, Duh QY, Clark OH. Predictors of airway complications after thyroidectomy for substernal goiter. Arch Surg. 2004;139:656–60. doi: 10.1001/archsurg.139.6.656. [DOI] [PubMed] [Google Scholar]
- 6.Rosato L, De Toma G, Bellantone R, Avenia N, Cavallaro G, Dobrinja C, Chiofalo MG, De Crea C, De Palma M, Gasparri G, Gurrado A, Lombardi C, Miccoli P, Mullineris B, Nasi PG, Pelizzo MR, Pezzullo L, Perigli G, Testini M. Diagnostic, therapeutic and health-care management protocols in thyroid surgery: 3rd consensus conference of the Italian association of endocrine surgery units (U.E.C. CLUB) Minerva Chir. 2012;67:365–79. [PubMed] [Google Scholar]
- 7.Anders HJ. Compression syndromes caused by substernal goitres. Postgrad Med J. 1998;74(872):327–9. doi: 10.1136/pgmj.74.872.327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Polistena A, Monacelli M, Lucchini R, Triola R, Conti C, Avenia S, Micol Sole Patrizi, Barillaro I, Boccolini A, Sanguinetti A, Avenia N. Mediastinal goiter: twenty-eight years experience of a referral centre for endocrine surgery on 1721 patients. Minerva Chir. 2014;69(2 Suppl 1):7–13. [Google Scholar]
- 9.Herscovici R, Szyper-Kravitz M, Altman A, Eshet Y, Nevo M, Agmon-Levin N, Shoenfeld Y. Superior vena cava syndrome - changing etiology in the third millennium. Lupus. 2012;21(1):93–6. doi: 10.1177/0961203311412412. [DOI] [PubMed] [Google Scholar]
- 10.Steenerson RL, Barton RT. Mediastinal goiter and superior vena cava syndrome. Laryngoscope. 1978;88(10):1688–90. doi: 10.1288/00005537-197810000-00016. [DOI] [PubMed] [Google Scholar]
- 11.Marcelino M, Nobre E, Conceição J, Lopes L, Vilar H, de Castro JJ. Superior vena cava syndrome and substernal goiter. Thyroid. 2010;20(2):235–6. doi: 10.1089/thy.2009.0188. [DOI] [PubMed] [Google Scholar]
- 12.Ulreich S, Lowman RM, Stern H. Intrathoracic goitre: a cause of the superior vena cava syndrome. Clin Radiol. 1977;28(6):663–5. doi: 10.1016/s0009-9260(77)80053-6. [DOI] [PubMed] [Google Scholar]
- 13.Siderys H, Rowe GA. Superior vena cava syndrome caused by intrathoracic goiter. Am Surg. 1970;36(7):446–50. [PubMed] [Google Scholar]
- 14.Bedard EL, Deslauriers J. Bleeding “downhill” varices: a rare complication of intrathoracic goiter. Ann Thorac Surg. 2006;81:358–60. doi: 10.1016/j.athoracsur.2004.08.020. [DOI] [PubMed] [Google Scholar]
- 15.Machado AS, Caldeiro JM, Fonseca L, Azevedo F, Lobo LA, Gomes T, Almeida J, Silva AO, de Freitas F. Portal pseudo-hypertension. Acta Med Port. 2006;19(1):93–8. [PubMed] [Google Scholar]
- 16.Kelly TR, Mayors DJ, Boutsicaris PS. “Downhill” varices; a cause of upper gastrointestinal hemorrhage. Am Surg. 1982;48(1):35–8. [PubMed] [Google Scholar]