Abstract
Background:
Recent combat operations have involved large numbers of personnel. Long-term health effects of military deployment remain largely unknown.
Objectives:
To examine patterns and trends in long-term disability among combat veterans and to relate disability to aspects of wartime experience.
Participants:
A total of 60,228 Australian military personnel deployed between 1962 and 1975 during the Vietnam War, and 82,877 military personnel who were not deployed overseas.
Outcome Measures:
Accepted physician-assessed disability claims were evaluated over follow-up periods up to 50 years after deployment, and compared with age-matched controls. Multivariable analysis was used to examine differences by service branch, rank, age, and deployment duration.
Results:
The steepest rise in disability incidence was observed among Vietnam veterans starting in the 1990s, around 20–30 years after deployment for most veterans. After 1994, when Statements of Principles were introduced to guide evaluation of disability claims, the hazard ratio for disability incidence was 1.53 (95% confidence interval, 1.32–1.77) compared with the prior period. By January 2011, after an average follow-up of 42.5 years, 69.7% (95% confidence interval, 69.4%–70.1%) of veterans had at least 1 war-related disability. Many veterans had multiple disabilities, with leading causes being eye and ear disorders (48.0%), mental health conditions (47.9%), and musculoskeletal disorders (18.4%). For specific categories of disability, relative risks for accepted claims among veterans compared with controls were highest for mental health disorders, at 22.9 (21.9–24.0) and lowest for injuries, at 1.5 (1.4–1.6) with a relative risk for any disability of 3.7 (3.7–3.8). Veterans with service of >1 year were 2.5 (2.2–2.7) times more likely to have a mental health disability than those who served <100 days, and 2.3 (2.1–2.5) times more likely to have other disabilities.
Conclusions:
Long-term effects of deployment into military conflicts are substantial, and likelihood of war-related disability is associated with service history. If similar patterns follow from more recent conflicts, significant additional resources will be needed to prevent and treat long-term health conditions among veterans.
Key Words: veterans health, disability, Vietnam war, mental health
A large number of service personnel have been deployed in peacekeeping or combat roles in recent years, prompting renewed interest in how military deployment impacts physical and mental health. Armed conflicts are increasingly recognized as having long-term detrimental consequences for the health of combatants even after they return to civilian life.1 The treatment of, and compensation for, these war-related disabilities will likely require major ongoing commitments of resources by many governments.2 A recent study estimated that future health and pension costs for the US Government from its involvement in the Iraq and Afghanistan wars may exceed $800 billion, representing the single largest accrued liability from these conflicts.3
To date, empirical studies documenting the impact of recent conflicts have focused on combat injury,4 immediate effects of deployment on spouses and children of military personnel,5,6 and aspects of health following return from deployment using durations of follow-up ranging from a few months7 to a few years.8 Thus far, only short-term impacts of recent and ongoing conflicts are known. To understand the potential longer-term health impact of combat deployment, it is useful to examine patterns and trends observed among veterans from earlier conflicts. For example, health studies of service personnel from the Vietnam War have typically been based on surveys9–11 and have primarily highlighted the high prevalence of mental health conditions such as posttraumatic stress disorder (PTSD). However, these studies face a number of methodological challenges, including difficulties of tracking service personnel after they return to civilian life, low participation rates, and problems of recall and survivorship bias.12 Studies from the first Gulf War have similar limitations.13 High-quality empirical data are lacking on the burden of illness and disability over remaining lifetimes.
Therefore, in this study, we aimed to assess the incidence of physical and mental health disorders among a large cohort of Australian veterans who served during the Vietnam War and compare these outcomes to those among former military personnel who did not serve in that conflict. We used long-term follow-up information from accepted physician-assessed administrative claims for disabilities up to 50 years after deployment, with data linkage to war service records. The aims of this study are: (i) to examine time trends in the incidence of disability among combat veterans; (ii) to compare outcomes across different types of disability, and between Vietnam veterans and veterans who were not deployed in combat; and (iii) to evaluate how the frequency and nature of disability relates to aspects of wartime experience, including rank, age at deployment, and duration of service.
METHODS
Study Population
The study population consisted of all 60,228 military personnel who served in the Australian Army, Navy, and Air Force in Vietnam, or in the waters adjacent to Vietnam during the conflict between May 1962 and April 1975. The study subjects were identified from the Nominal Roll of Vietnam Veterans in Australia,14 which was constructed from records contained at the Australian War Memorial, the Department of Defence, and the National Archives of Australia. The Nominal Roll records sex, date of birth, rank, service branch, dates of deployments, and date of death during service for each service member. A control group was defined as 82,877 military personnel who had at least 3 years of peacetime service in the Australian Defence Force between 1972 and 1994, but who had no evidence of deployment overseas. The age structure of the peacetime defence forces was obtained from the Department of Veterans’ Affairs (DVA) estimates.12
Policy Background
Australian Vietnam veterans and some military personnel with peacetime service have access to a national system of compensation for disabilities that are related to their military service.15 Claims for compensation must be made in relation to a particular conflict or period of service (including peacetime service). When making a claim, the veteran can provide a physician’s diagnosis of the condition and the time of onset,16 and the claim is then determined by the DVA, which may require further medical examinations and collection of additional information on medical history. Since 1994 the process for evaluating claims has been governed by a set of Statements of Principles,17 which define—for each of a range of health conditions—the specific factors that must exist to connect each condition to the circumstances of a person’s relevant military service.
In Australia, there was considerable controversy during the 1980s on the long-term health impacts of veteran exposure to the defoliant commonly known as “Agent Orange,” which culminated in a commission of inquiry. Although this commission did not find a link between Agent Orange and veterans’ health, it did conclude that Vietnam veterans were at a greater risk for a range of disorders and disease. It recommended a more liberal interpretation of the legal framework governing war-related disability to make it easier for veterans to claim.18 Subsequently a more structured framework was adopted to assess the evidence to have a disability accepted, which resulted in more expedient processing of claims.17 Under the Veterans’ Entitlements Act 1986, an accepted war-related disability provides the veteran with access to a range of health care benefits, a disability pension and other allowances if the disability results in a specified level of incapacity.16
Data Sources
Information on disability status for both the Vietnam veterans and the control group were obtained from an administrative database on accepted disability claims, prospectively maintained by the Australian DVA. DVA disability records contain the primary diagnosis associated with each claim, the date the claim was accepted, and the conflict or period of service relevant to the claim. Primary diagnoses are coded according to various revisions of the International Classification of Diseases (ICD). For this study, we grouped disabilities into categories, each corresponding to 1 or 2 ICD-10 chapters: (1) infectious diseases (ICD chapter I); (2) cancers (chapter II); (3) mental and behavioral disorders (chapter V); (4) diseases of the eye and ear (chapters VII and VIII); (5) circulatory diseases (chapter IX); (6) respiratory diseases (chapter X); (7) digestive diseases (chapter XI); (8) skin diseases (chapter XII); (9) musculoskeletal diseases (chapter XIII); (10) injuries (chapters XIX and XX); and (11) all other diseases.
Among the Vietnam veterans cohort we used probabilistic record linkage methods19 to link DVA disability claims to service history records from the Nominal Roll. Record linkage was undertaken using ChoiceMaker software.20 Matching was based on full name, date of birth, and sex. Linkage was attained when records reached a predefined cutoff regarding the probability of a match, followed by a manual clerical review. Using these methods, the records of 51,528 Vietnam veterans from the Nominal Roll could be uniquely matched with DVA administrative disability records, and a further 1534 records were identified that included disabilities relating to service in Vietnam, but among military personnel who could not be unambiguously linked to a unique service member on the Nominal Roll. As of January 20, 2011 there were 163,810 separate ICD-coded DVA disability records on 40,471 of the 51,528 uniquely matched veterans, and 5168 disabilities from the additional 1534 veterans who were not uniquely matched. A further 22,521 disability records identified the cause of disability only in a free-text field, without reporting an ICD code. These records were reviewed by 2 independent coders, who each assigned an ICD-10 chapter. Records with coding discrepancies were reexamined to determine a final classification.
The same procedure was followed to identify disabilities among the control group. A total of 17,095 former military personnel had records that indicated disabilities due to peacetime service and no evidence of overseas service.
Statistical Analysis
Time Trends in Accepted Disability Claims Among Vietnam Veterans
The primary outcome measure in this cohort study was an accepted claim for a Vietnam War-related disability. In the initial analysis, the number of veterans with disabilities (comprising both the 51,528 uniquely matched veterans plus the 1534 unmatched veterans with evidence of Vietnam War-related disability) was expressed as a proportion of the total Vietnam veteran cohort (N=60,228). To examine changes in the rates of accepted disability claims over time, a Cox proportional hazards model with time-varying covariates was used.21 The model was specified to allow for changes in rates occurring between periods marked by the following events: (i) conclusion of the Australian involvement in Vietnam War in January 1973; (ii) release of the Royal Commission Report on effects of Agent Orange in 1985; and (iii) introduction of the Statements of Principles governing assessment of disability claims in relation to military service in 1994. The Cox proportional hazard model was also used to test for differences in disability rates across categories of duration of service in Vietnam.
Comparison of Disability Among Vietnam Veterans and Control Group
We compared age-standardized cumulative incidence of disability claims by the end of follow-up between the Vietnam veteran group and the control group, and computed relative risks in the 2 groups for different specific types of disability, as well as relative risks by age cohort for the broad categories of mental and nonmental health disabilities.
Evaluation of Predictors of Disability Based on Characteristics of Service
Within the Vietnam veteran cohort, we used multivariable logistic regression to estimate associations between cumulative disability by the end of follow-up and individual-level characteristics, including age, sex, calendar year of first deployment divided into 2 periods to enable trends to be observed, rank, service branch, and duration of service in Vietnam. Focusing in particular on the association between disability claims and duration of service, we stratified by service branch and estimated odds ratios for duration, categorized as <100, 100–199, 200–364, and ≥365 days, controlling for age, sex, calendar year of first deployment, and rank, respectively. A P-value of <0.05 was deemed to be significant in all analyses. Statistical analyses were undertaken with STATA (version 12.1/MP).
RESULTS
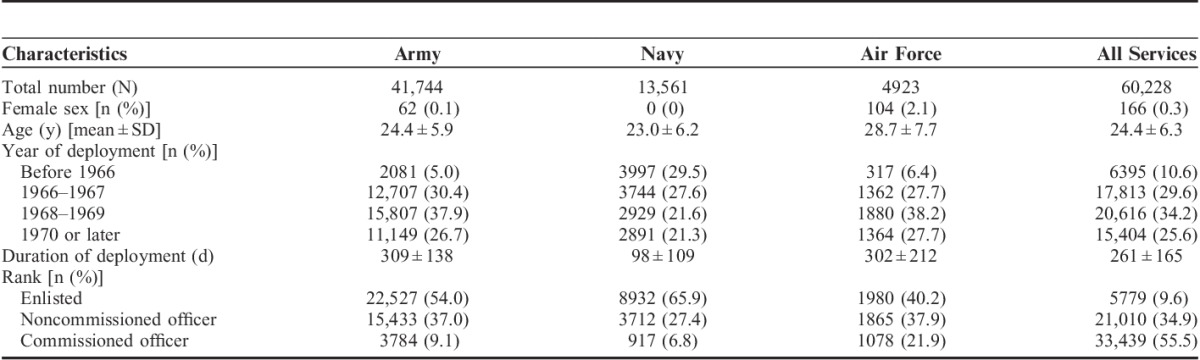
Characteristics of the Vietnam veteran study cohort are reported in Table 1. Only a small proportion were female (0.3%), and the average age at time of first deployment to Vietnam was 24.4±6.3 years.
TABLE 1.
Demographic and Military Characteristics of the Study Population
Time Trends in Accepted Disability Claims
Figure 1A shows the cumulative incidence of accepted disability claims (ie, the proportion of the full cohort acquiring at least 1 accepted disability claim) over calendar time, for all personnel who served in Vietnam. By the end of Australia’s involvement in the Vietnam War in 1973, around 10% of veterans had at least 1 accepted disability claim. Over the period between 1973 and 1985, when the report on findings regarding Agent Orange was released, the rate of accepted claims was around 40% lower than the rate during the war. Over the period between 1985 and 1994, there was a nonstatistically significant (P=0.056) increase in the rate of claims. Following the introduction, in 1994, of the Statements of Principles for assessing disability claims, the rate of accepted claims increased significantly (hazard ratio=1.53; 95% confidence interval, 1.32–1.77). By January 2011, after an average follow-up of 42.5 years after deployment, 69.7% of the Vietnam Veteran’s cohort (95% confidence interval, 69.4%–70.1%) had at least 1 disability claim.
FIGURE 1.
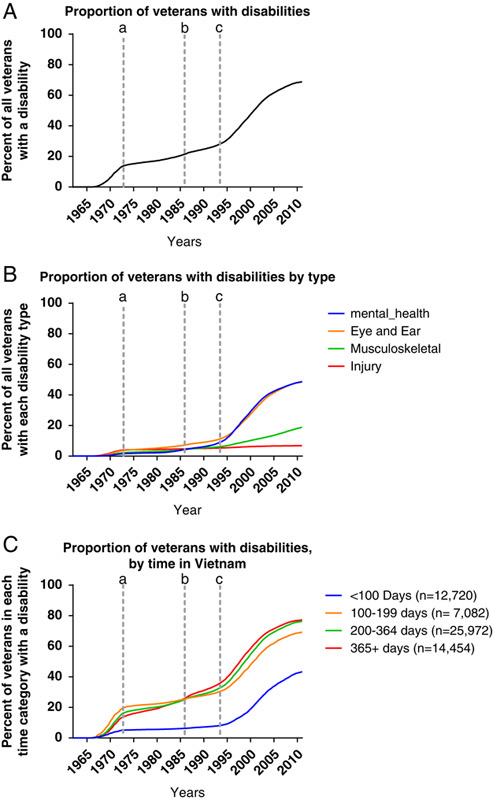
Proportion of all Vietnam veteran cohort with accepted disability claims, for any type of disability (A); for 4 specific types of disability (B); stratified by the duration of service in Vietnam (C). Vertical lines mark (a) the end of Australian involvement in Vietnam; (b) the release of the report of the Agent Orange Commission; and (c) the introduction of Statements of Principles governing assessment of disability claims.
Figure 1B presents analogous time-series analyses specific to certain major categories of disability, including the 3 leading causes of disability and—for comparison—injuries. Following the general pattern shown in Figure 1A, the steepest rise in the incidence of accepted disability claims for the leading causes of disability occurred after the year 1994, which for most veterans was around 20–30 years following their wartime deployment. For example, 46% of mental health claims, 36% of eye and ear, and 25% of musculoskeletal disability claims were awarded during the 1990s. In contrast, injury claims tended to occur earlier, and only 17% were awarded during 1990–2000.
Figure 1C stratifies the cumulative incidence by the duration of service in Vietnam. The high initial rates among those with shorter durations of service are most likely a result of a disability-related condition prompting evacuation from Vietnam. From the end of Australia’s involvement in the Vietnam War, the disability rates are significantly higher for those with longer service durations which results in a crossing of the lines tracing cumulative disability by duration. Comparing the longest duration category (365+ d) with the shortest (<100 d) using a Cox regression model, the hazard ratio of disability claims was >7 times higher, indicating persistently higher relative rates of incident disability claims among veterans with longer periods of service.
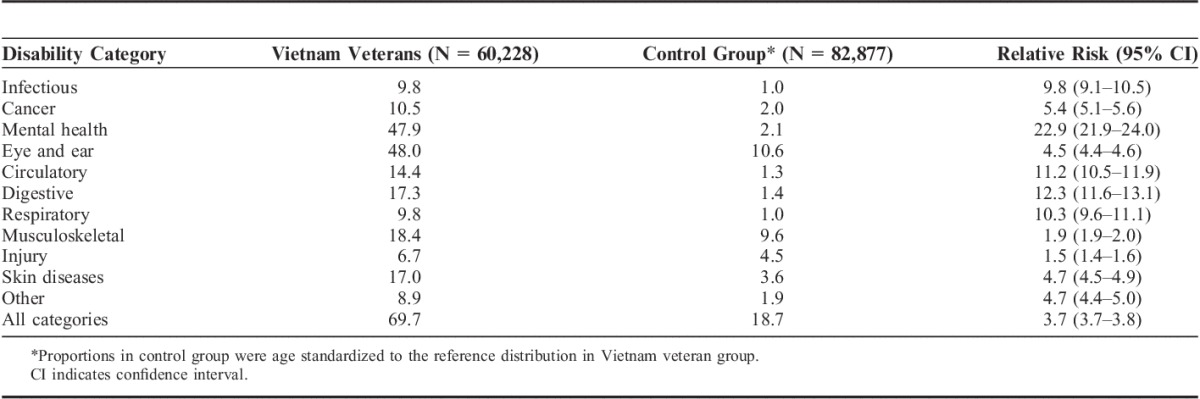
Outcomes by Type of Disability, in Vietnam Veterans Versus Controls
Table 2 shows the proportion of service personnel with accepted disability claims by the end of follow-up, in the Vietnam veteran group and the control group of military personnel not serving in Vietnam, with results for the latter age standardized to the reference distribution in the Vietnam group. In the Vietnam veteran group, the most common reasons for disability were eye and ear disorders and mental health conditions (each around 48%) and musculoskeletal and connective tissue disorders (18%). In the control group, the probability of accepted disability claims was significantly lower in every category, with the overall probability of any claim being 20%, implying a relative risk for the Vietnam veteran group of 3.7 (3.7–3.8). Leading causes of disability in the control group were eye and ear disorders (11%), musculoskeletal and connective tissue disorders (10%), and injury (5%). For specific categories of disability, relative risks for accepted claims among veterans compared with controls were highest for mental health disorders, at 22.9 (21.9–24.0), and lowest for injuries, at 1.5 (1.4–1.6).
TABLE 2.
Proportion of Former Australian Defence Force Members with Accepted Disability Claims, in Vietnam Veterans Group and Control Group, by Disability Category
Disability and Characteristics of Service
Multivariable analyses of predictors of accepted disability claims among the Vietnam veterans group are reported in Table 3. Age at first deployment was variably associated with the type of disability; for eye and ear problems the highest rate was among those aged 20–24 years at the time of first deployment, whereas for musculoskeletal disabilities, probabilities were highest among those aged 25–29 years. In contrast, the odds of having a mental health–related disability declined with increasing age at first deployment. The small proportion of women serving during the Vietnam War had much lower probabilities of claims for all types of disability. Year of deployment was another significant predictor of disability, with those involved before 1966 around 50% more likely to have disability than those involved after 1970. We found that noncommissioned officers had similar rates of disability as enlisted personnel, except for musculoskeletal diseases for which rates were higher for noncommissioned officers.
TABLE 3.
Multivariable Logistic Regression Results for Any Accepted Disability Claim, and for 3 Most Common Categories of Disability, N=60,228*
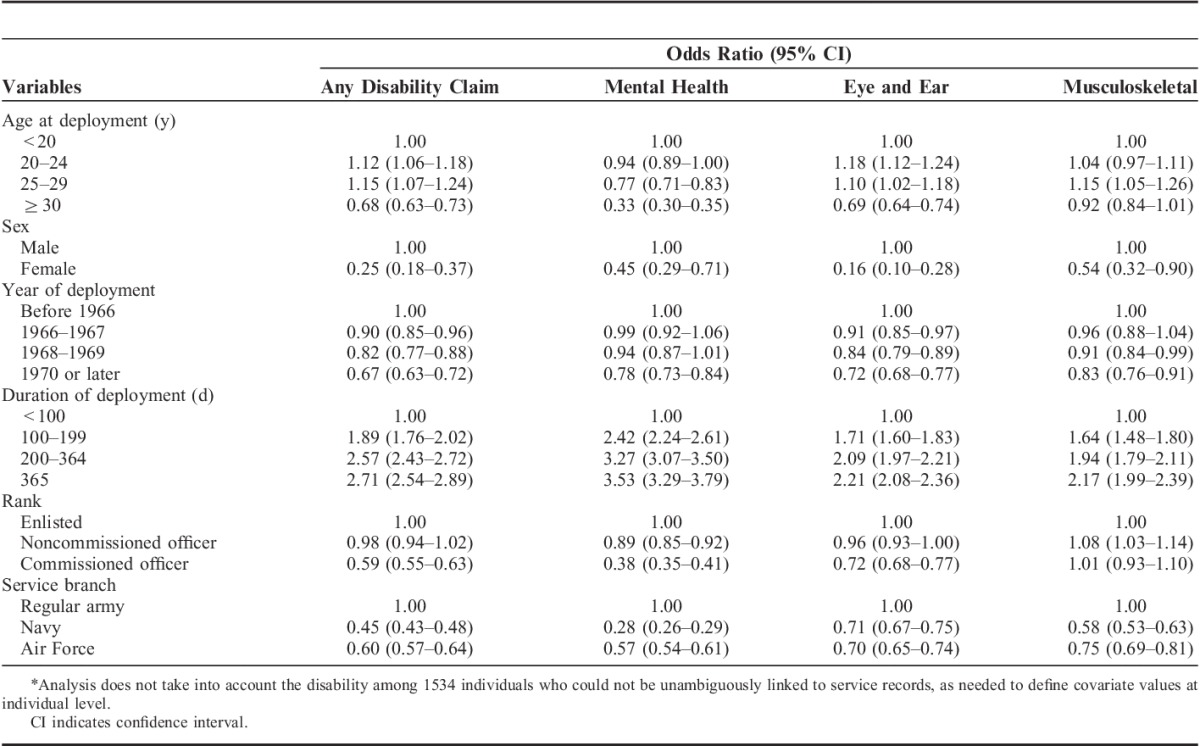
Across all categories, the likelihood of an accepted disability claim increased monotonically with longer periods of service in Vietnam (Fig. 2). Compared with army personnel serving <100 days in Vietnam, those with army service of at least 1 year in Vietnam were 2.5 (2.2–2.7) times more likely to have a mental health disability and 2.3 (2.1–2.5) times more likely to have any other form of disability. Comparison to nonarmy personnel, who on average faced lower intensity of combat exposure, indicates the same general pattern of association between duration of deployment and disability, however, lower overall likelihoods of accepted disability claims.
FIGURE 2.
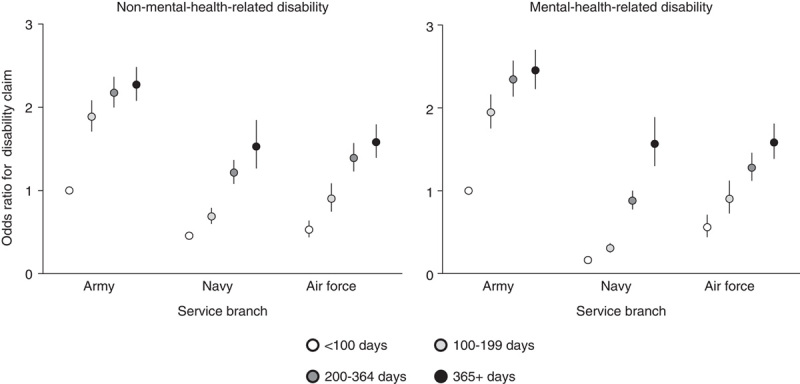
Association between accepted disability claims and duration of deployment in Vietnam, according to service branch. Results based on multivariable logistic regression (N=51,528), adjusting for age at deployment, sex, year of deployment, and rank. Bars indicate 95% confidence intervals. Reference category is Army, <100 days.
DISCUSSION
In the largest study to date of a cohort of veterans who served during the Vietnam War, we found that more than two thirds of military personnel have experienced at least 1 disability attributed to their wartime service, and more than half have experienced ≥2 types of disability. Most accepted disability claims did not occur during deployment or in the period immediately following repatriation, but 20–30 years later. The most frequent causes of accepted disability claims were eye and ear disorders, mental health conditions, and musculoskeletal disorders. The prevalence of many disabilities was significantly associated with aspects of wartime experience such as duration of deployment. In every category of disability, claims were significantly higher in the Vietnam veteran group than in an age-matched group of military personnel who did not serve overseas. For mental health conditions the risk was almost 23 times higher in the Vietnam group, with a relative risk >37 in the age cohort born between 1935 and 1939.
Like other modern conflicts, the Vietnam War was characterized by very high rates of survival, of around 97%–98% for wounded Australian soldiers who were able to reach a military field hospital.22 However, wounds from high-velocity small arms or antipersonnel mines often resulted in severe injuries that would have proved fatal in previous conflicts. Battlefield injuries affected <5% of the total service personnel who served in Vietnam (including both personnel who were exposed to active combat and those who played support roles),11 and our study shows that just over 10% of veterans had any disability claim accepted by the end of Australia’s involvement in the war.
An important finding of this study is the delayed nature of accepted disability claims among veterans from the Vietnam War, as the majority of claims occurred decades after war service. A steep rise in disability claims, particularly for mental health and eye/ear conditions, is observed after 1994, which was the year of adoption of a set of Statements of Principles governing the assessment of disability claims in connection to military service. Whether these findings represent effects of war that take decades to manifest, or more typical age-related illnesses, or the effects of the policy changes regarding assessment of war-related disability in the 1980s and 1990s, are unclear. Examples of specific shifts in the boundaries under which claims could be made include the definition of PTSD as a disease23 and the acceptance of smoking-related illness as a potentially war-related disability.24 Importantly, all Australian Vietnam veterans are assessed under the same framework and so are equally impacted by any policy changes. Differences in the patterns of disability claims over time across strata of veterans with different durations of exposure to war signal that at least part of the delay in disability claims relates to delays in the onset of disability that is sufficiently severe to warrant medical intervention meeting the threshold for a disability claim.
Most recent reports on the health effects of combat1 have focused on PTSD and other mental health problems. An important insight from our work is that military service in an armed conflict impacts not only on mental health, but also on many aspects of physical health including eye and ear, musculoskeletal, skin, and digestive diseases, many of which are not identified as war-related disabilities until years after conflict ends. The studies of recent conflicts have primarily focused on short-term effects because of limited time for follow-up. For example, a recent study reported on causes for medical evacuation from Operation Iraqi Freedom or Operation Enduring Freedom and assessed determinants of return to duty after evacuation.4 One exception was a previous Australian study that compared the prevalence of self-reported chronic physical and mental health conditions among Vietnam veterans with a matched cohort from the general population, and found that prevalence was higher in veterans for 47 of 67 conditions examined.11 This study was based on a self-report survey, and had a relatively limited sample of 450 Vietnam veterans. A key element of our present study has been the linking of war service history with postwar medical records including physician-diagnosed disease over long periods of time. We were able to identify only 1 other study using this type of approach, which analyzed the long-term health of veterans of the US Civil War.25
In analyzing a broad set of disability causes, one important finding was that the dose-response relationship observed previously between duration of service and mental health outcomes like PTSD also appears to apply to nonmental health conditions. Considering the 3 leading causes of disability (mental health, eye and ear, and musculoskeletal conditions) in all cases, odds ratios for disability were >2.0 for veterans with at least a year of combat duty compared with those with <100 days. In general, we found that the association between duration of deployment and disability was strong for various types of causes, and across all service branches, even after controlling for a wide range of factors including rank and year of service. Further, the higher rate of disability claims among those with service of longer durations persisted for >2 decades after Australia’s withdrawal from Vietnam.
There are limitations to this study. Firstly, we have no information on the behavior and circumstances of veterans after their return from Vietnam. For example, studies have reported that smoking is related to claims of war-related disability in Australia, although less so in the United States.24,26 Information on health risk behaviors during and after the conflict as well as downstream information such as employment history would be useful for further understanding factors that lead to higher rates of disability in later life, particularly as there are complex relationships between the disability compensation system and disability claims behavior.27,28
Although the veterans not deployed overseas provided a useful control group, in the Vietnam veterans several factors should be noted. Studies of military personnel can be confounded by factors such as “healthy warrior” effects, which arise if those who are healthier are more likely to be deployed.12 Unfortunately, we have very little information that would enable us to account for these differences and the degree to which these factors could impact on long-term disability claims. Another potential confounding difference is that Vietnam veterans included a significant number of conscripts, whereas the nondeployed controls were entirely volunteers. Further, while both Vietnam veterans and those who have only peacetime service were able to make disability claims, those with overseas service have a lower evidentiary requirement to prove claims. In practice it not clear to what extent this contributes to high levels of disability among the Vietnam group. A recent review conducted for DVA indicates that around half of claims for psychiatric conditions by those with peacetime-only service were rejected.15 Even if all of these claims had been accepted they would not explain the differences we have observed.
If veterans from more recent conflicts follow a pattern similar to those from Vietnam, we should expect that the new disability claims are likely to continue for long periods of time after repatriation. The dominance of long lags between deployments in zones of conflict and the acceptance of disability has important implications for planning, as significant resources will be required to meet future health and disability costs, both for recent wars as well as for the future ones. The findings of our study are likely to be of immediate relevance to the 956,000 veterans from 41 nations who were deployed in the first Persian Gulf War between 1990 and 1991.29 There have been ongoing concerns about the impact of this war on a wide range of health conditions.30–34 A recent report by the Institute of Medicine suggested that there was sufficient evidence for deployment to have a causal link with PTSD and evidence of associations for a range of other conditions.13 Given that 20 years have now elapsed since the first Gulf War, these veterans are entering the postdeployment period during which the veterans in our study had a dramatic rise in disability claims.
Our study reinforces the value of very long-term follow-up studies of veterans such as the The Millennium Cohort Study35 that follow veterans who have been deployed to zones of conflict over long periods of time. This could be complemented by studies to evaluate potential interventions to prevent or treat the causes of these disability claims occurring later in life. Investing in this research is likely to yield dividends, as many developed countries now have an increasing number of military personnel who have combat exposure and so are vulnerable to future war-related disability.
Footnotes
The study was approved by the Department of Veterans Affairs Human Research Ethics Committee.
Supported by The Australian Department of Veterans’ Affairs (DVA) provided funding and administrative data for the study. Under the terms of funding, the Commonwealth of Australia retains copyright on this work. The design, analysis and interpretation of the results were undertaken solely by the investigators. DVA approved the manuscript for publication after providing comments that clarified terminology and technical aspects of the study. However, the views expressed do not necessarily represent the views of the Minister for Veterans’ Affairs or the Department of Veterans’ Affairs. The Commonwealth does not give any warranty nor accept liability in relation to the contents of this work.
Presented at the Australian Military Medicine Association conference in October 2012.
The authors declare no conflict of interest.
REFERENCES
- 1.Levy BS, Sidel VW. Health effects of combat: a life-course perspective. Annu Rev Public Health. 2009;30:123–136. [DOI] [PubMed] [Google Scholar]
- 2.Crum-Cianflone NF.Hendricks AJ. The millennium cohort study: answering long-term health concerns of US Military Service members by integrating longitudinal survey data with military health system records, chapter 5. Military Health Care: From Pre-Deployment to Post-Separation. 2013New York, NY: 55–77. [Google Scholar]
- 3.Bilmes LJ. The Financial Legacy of Iraq and Afghanistan: How Wartime Spending Decisions Will Constrain Future National Security Budgets. HKS Faculty Research Working Paper Series RWP13-006, March 2013.
- 4.Cohen SP, Brown C, Kurihara C, et al. Diagnoses and factors associated with medical evacuation and return to duty for service members participating in Operation Iraqi Freedom or Operation Enduring Freedom: a prospective cohort study. Lancet. 2010;375:301–309. [DOI] [PubMed] [Google Scholar]
- 5.Mansfield AJ, Kaufman JS, Marshall SW, et al. Deployment and the use of mental health services among US Army wives. N Engl J Med. 2010;362:101–109. [DOI] [PubMed] [Google Scholar]
- 6.Mansfield AJ, Kaufman JS, Engel CC, et al. Deployment and mental health diagnoses among children of US Army personnel. Arch Pediatr Adolesc Med. 2011;165:999–1005. [DOI] [PubMed] [Google Scholar]
- 7.Milliken CS, Auchterlonie JL, Hoge CW. Longitudinal assessment of mental health problems among active and reserve component soldiers returning from the Iraq war. JAMA. 2007;298:2141–2148. [DOI] [PubMed] [Google Scholar]
- 8.Hotopf M, Hull L, Fear NT, et al. The health of UK military personnel who deployed to the 2003 Iraq war: a cohort study. Lancet. 2006;367:1731–1741. [DOI] [PubMed] [Google Scholar]
- 9.Eisen SA, Griffith KH, Xian H, et al. Lifetime and 12-month prevalence of psychiatric disorders in 8,169 male Vietnam War era veterans. Mil Med. 2004;169:896–902. [DOI] [PubMed] [Google Scholar]
- 10.Dohrenwend BP, Turner JB, Turse NA, et al. The psychological risks of Vietnam for US veterans: a revisit with new data and methods. Science. 2006;313:979–982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.O’Toole BI, Catts SV, Outram S, et al. The physical and mental health of Australian Vietnam veterans 3 decades after the war and its relation to military service, combat, and post-traumatic stress disorder. Am J Epidemiol. 2009;170:318–330. [DOI] [PubMed] [Google Scholar]
- 12.Hotopf M, Wessely S. Can epidemiology clear the fog of war? Lessons from the 1990-91 Gulf War. Int J Epidemiol. 2005;34:791–800. [DOI] [PubMed] [Google Scholar]
- 13.Institute of Medicine. Gulf War and Health, Volume 8: Update of Health Effects of Serving in the Gulf War. 2010Washington, DC: The National Academies Press. [PubMed] [Google Scholar]
- 14.Department of Veterans’ Affairs. The Nominal Roll of Vietnam veterans. 1997Canberra: Department of Veterans’ Affairs. [Google Scholar]
- 15.Department of Veterans’ Affairs Review of Military Compensation Arrangements February 2011, Volume One, Department of Veterans’ Affairs. 2011. Available at: http://www.dva.gov.au/sites/default/files/files/consultation%20and%20grants/reviews/mrca/mrcareport/vol1-full18032011.pdf. Accessed February 23, 2015.
- 16.Department of Veterans’ Affairs. Making a Claim/Applying for an Increase in Disability Pension (DVA Factsheet DP18). Canberra: Department of Veterans’ Affairs]. Available at: http://factsheets.dva.gov.au/factsheets/documents/DP18HowtoclaimDisabilityPension.htm. Accessed October 22, 2012.
- 17.Ward JD, Donald KJ. Statements of Principles: evidence-based compensation for Australian Veterans and serving defence personnel. ADF Health. 2004;5:89–93. [Google Scholar]
- 18.Hall W. The logic of a controversy: the case of Agent Orange in Australia. Soc Sci Med. 1989;29:537–544. [DOI] [PubMed] [Google Scholar]
- 19.Papadouka V, Schaeffer P, Metroka A, et al. Integrating the New York citywide immunization registry and the childhood blood lead registry. J Public Health Manag Pract. 2004;suppl:S72–S80. [DOI] [PubMed] [Google Scholar]
- 20.Goldberg A, Borthwick A. The ChoiceMaker 2 Record Matching System. 2004New York: ChoiceMaker Technologies Inc.. [Google Scholar]
- 21.Cleves M, Gould W, Gutierrez RG, et al. An Introduction to Survival Analysis Using Stata. 2010:3rd edCollege Station, TX: STATA Press. [Google Scholar]
- 22.Knight RJ. Reception and resuscitation of casualties in South Vietnam. Experience at the First Australian Field Hospital. Lancet. 1972;2:29–31. [DOI] [PubMed] [Google Scholar]
- 23.McFarlane AC. PTSD in the medico-legal setting: current status and ongoing controversies. Psychiatry Psychol Law. 1995;2:25–35. [Google Scholar]
- 24.Offen N, Smith EA, Malone RE. “Willful misconduct”: how the US government prevented tobacco-disabled veterans from obtaining disability pensions. Am J Public Health. 2010;100:1166–1173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Pizarro J, Silver RC, Prause J. Physical and mental health costs of traumatic war experiences among Civil War veterans. Arch Gen Psychiatry. 2006;63:193–200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Topperwien B. Relaxed evidentiary rules veterans’ legislation: a comparative and empirical analysis. South Cross Univ Law Rev. 2003;7:259–307. [Google Scholar]
- 27.Angrist JD, Chen SH, Frandsen BR. Did Vietnam veterans get sicker in the 1990s? The complicated effects of military service on self-reported health. J Public Econ. 2010;94:824–837. [Google Scholar]
- 28.Siminski P. Employment effects of army service and veterans’ compensation: evidence from the Australian Vietnam-era conscription lotteries. Rev Econ Stat. 201287–97. [Google Scholar]
- 29.Hernandez LM, Durch JS, Blazer DG, et al. Gulf War Veterans: Measuring Health. 1999Washington, DC: National Academy Press. [PubMed] [Google Scholar]
- 30.Self-reported illness and health status among Gulf War veterans. A population-based study. The Iowa Persian Gulf Study Group. JAMA. 1997;277:238–245. [PubMed] [Google Scholar]
- 31.Gray GC, Gackstetter GD, Kang HK, et al. After more than 10 years of Gulf War veteran medical evaluations, what have we learned? Am J Prev Med. 2004;26:443–452. [DOI] [PubMed] [Google Scholar]
- 32.Eisen SA, Kang HK, Murphy FM, et al. Gulf War veterans’ health: medical evaluation of a US cohort. Ann Intern Med. 2005;142:881–890. [DOI] [PubMed] [Google Scholar]
- 33.Engel CC, Hyams KC, Scott K. Managing future Gulf War Syndromes: international lessons and new models of care. Philos Trans R Soc Lond B Biol Sci. 2006;361:707–720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Li B, Mahan CM, Kang HK, et al. Longitudinal health study of US 1991 Gulf War veterans: changes in health status at 10-year follow-up. Am J Epidemiol. 2011;174:761–768. [DOI] [PubMed] [Google Scholar]
- 35.Smith TC., I Millennium Cohort Study Team. The US Department of Defense Millennium Cohort Study: career span and beyond longitudinal follow-up. J Occup Environ Med. 2009;51:1193–1201. [DOI] [PubMed] [Google Scholar]


