Summary
The requirements for accurate documentation within the process of burn assessment have increased dramatically over the years. TBSA (total body surface area) and burn depth are commonly determined by visual inspection, especially in the emergency or acute care setting. However, inexperience often results in incorrect estimation of these factors. In 2001, BurnCase 3D was initiated in order to develop a tool for objective burn assessment and documentation on mobile devices (Apple iPhoneTM). The centerpiece is a 3D model representing the actual patient. At two international burn meetings, a survey containing three pictures of patients was conducted and this data was collected. A patient-specific 3D model adapted to the height and weight of the real patient was created and the digital picture was superimposed in the computer system. The burns were transferred to the model and the TBSA in % was calculated by the software BurnCase 3D. The preferred methods of the 80 respondents for burn extent estimation were: the Rule of Nines (38%), the Rule of Palm (37%) and the Lund-Browder chart (18%). Analysis showed very high deviations of TBSA within the participants, even among the group of experts. In comparison to a computer-aided method we found massive overestimation of up to 230%. The use of BurnCase 3D could have a true impact on the quality of treatment in burns. In the acute care setting for burn injuries, telemedicine has great potential to help guide decisions regarding triage and transfer based on TBSA, burn depth, patient age and injury mechanism.
Keywords: telemedicine, TBSA, burn injuries, BurnCase 3D, application
Abstract
Les exigences en matière de documentation précise dans le processus de l’évaluation des brûlures ont augmenté de façon spectaculaire au cours des années. La SCT (surface corporelle totale) et la profondeur de la brûlure sont généralement déterminées par inspection visuelle, en particulier dans le contexte d’urgence ou de soins aigus. Cependant, l’inexpérience se traduit souvent par une estimation incorrecte de ces facteurs. En 2001, BurnCase 3D a été lancé afin de développer un outil d’évaluation des brûlures objectif et de la documentation sur les appareils mobiles d’Apple (iPhone™). La pièce maîtresse est un modèle 3D représentant le patient réel. Sur deux réunions de brûlures internationales, une enquête contenant trois photos de patients a été réalisée. Ces données ont été collectées. Un modèle 3D spécifique au patient adapté à la taille et le poids du patient réel a été créé et l’image a été superposée dans le système informatique. Les brûlures ont été transférés dans le modèle et le % de la surface corporelle totale a été calculé par le logiciel BurnCase 3D. Les méthodes préférées des 80 répondants pour l’estimation de la taille de la brûlure étaient : la règle des neuf (38%), la règle des palm (37%) et les tables de Lund et Browder (18%). L’analyse montre des écarts très élevés de SCT dans les participants, même parmi le groupe d’experts. Par rapport à un procédé assisté par ordinateur, nous avons trouvé surestimation massive de jusqu’à 230%. L’utilisation de BurnCase 3D pourrait avoir un véritable impact sur la qualité du traitement des brûlures. Dans le cadre de soins de courte durée pour les brûlures, la télémédecine a un grand potentiel pour aider à guider les décisions concernant le triage et le transfert sur la base de la SCT et la profondeur de la brûlure, l’âge du patient et le mécanisme de blessure.
Introduction
Mobile phones are a rapidly expanding technology and facilitate the remote exchange of medical information in order to assist diagnosis and treatment. TBSA and burn depth are routinely (and most commonly) determined by visual inspection, especially in the emergency or acute care setting. However, inexperience often results in incorrect estimation, possibly leading to significant errors in fluid resuscitation and airway management, by either increasing the likelihood of occasional undertriage or, more frequently, resource-wasting overtriage. A single-center study comparing the initial assessment of TBSA in the emergency room with the final evaluation made in the burn center showed that the TBSA was overestimated by over 100% in 24 out of 134 patients.1 In addition to this, the problem of incorrect representation of the actual patient using charts, as well as the complexity of projection from three dimensions (3D) to two dimensions (2D) remains a possible source of error. Nichter et al.2 described an error rate of 29% using the “Rule of Nines” and Lund Browder Charts. Another bias is based on the Body Mass Index (BMI): in underweight, obese and infant patients in particular,3,4 the estimation errors by standard methods are significantly increased.5 BurnCase 3D has the potential to address some of the above mentioned issues. Remote telemedicine-assisted screening already leads to a reduction of airborne medical transports in the acute care as well as specialist consultation sector without compromising patient-safety, while concomitantly significantly reducing medical costs.6,7 By providing remote assessment of burn depth and extent, tele-video or digital “store-andforward” communication can improve initial triage and provide cost-effective, convenient follow-up care.8-11 The technological advancement of computing performance and capability of mobile handhelds, nowadays routinely including a variety of sensors and digital cameras, finally enabled the exploitation of modern graphics technology for efficient and user-friendly handling of three-dimensional surfaces. In order to improve existing estimation methods, the research project BurnCase 3D (RISC Software GmbH, Johannes Kepler University Linz, Hagenberg, Austria) was set up in 2001. It was initially designed for Windows based PCs.12 By virtually representing the actual three-dimensional human body structure and additionally integrating different body shapes resulting from factors like sex, age, weight, size and corpulence, the research project aims at tackling the difficulties of burn assessment. In this paper, we demonstrate the technical background and methodologies used for remotely transferring mobile data using popular smartphone devices and present some future implementations with a focus on the acute care setting. Furthermore, we investigate assessment accuracy among burn specialists and their accuracy versus a computer- based surface estimation and documentation method. The main objective was to evaluate the potential impact of wrong burn size evaluation.
Methods
To overcome the issues described above, it was essential to find a way to objectively define the burned surface area and link all collected relevant data to reduce the work load and support personnel in making decisions for further medical treatment, with balanced scientific claims and pragmatic feasibility. A development team consisting of computer scientists and medical scientists has been working on a software system called BurnCase 3D since 2001. During this research project, which has followed the principles of action research, many challenges of modern burn care have been taken into account by the developers. The cooperation of multiple hospitals in Europe and America enabled the development of a simple and intuitive user interface; allowing quick data input without the need for sophisticated training.
At two international burn meetings (“14th European Burns Association Congress of the EBA” and “28. Jahrestagung der deutschsprachigen Arbeitsgemeinschaft für Verbrennungsbehandlung, DAV”) in 2010 and 2011, a survey containing three pictures of patients with different burn wound patterns and sizes was conducted. In order to provide different levels of complexity, we selected one patient with plenty of small disseminated burn areas (2-yearold, male), one with a limited amount of extended regions (35-year-old, male) and one with a mixture of both (4- year-old, female). The patients are shown in Fig. 1.
Fig. 1. Pictures of patients with different wound patterns depicted on the questionnaire: Patient 1 (2 years-of-age, male, 12 kg, 87 cm), Patient 2 (35 years-of-age, male, 80 kg, 182 cm), Patient 3 (4 years-of-age, female, 16 kg, 102 cm).

Data was collected anonymously, voluntarily and without offering any financial incentives. The survey sheets were handed out randomly to conference participants.
The questionnaire consisted of the following parts:
Description to clarify the aim and process of the survey: “The task is to estimate the total surface area within the yellow line per patient. The line itself is part of the burn area; the estimation should be independent of its burn depth.”
Estimation of the total burned surface areas (TBSA) using three photographs. The images show three patients with outlined burn injuries. The estimations were asked to be given in percentages.
-
Method(s) used on a regular basis; the possible alternatives were:
Rule of Palm
Rule of Nines
Lund-Browder Chart
Others
-
Profession; possible alternatives were:
Resident
Specialist
Nursing staff
We provided graphical representations of the “Rule of Palm”, the “Rule of Nines” and a “Lund-Browder Chart” on the back of the survey sheet. The questionnaire was printed on A4 paper (210x297mm, 80g/A4) with a highquality colour laser printer.
Statistical analysis
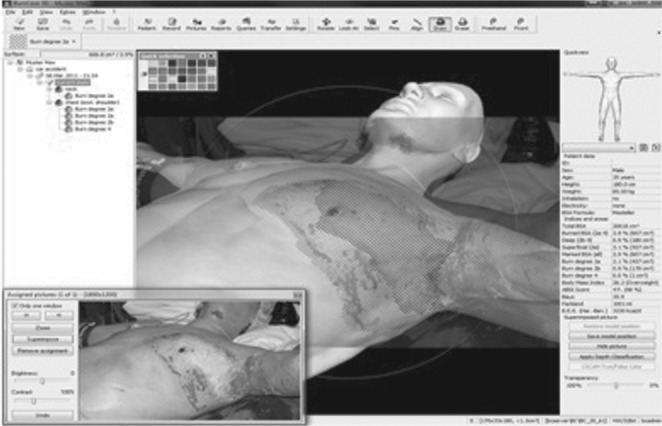
Collected data were manually and independently entered in respective Excel sheets (Microsoft Office, Excel, Version 2010, Richmond, MA, USA) by two persons, and descriptive statistical data were calculated. A patient-specific 3D model adapted to height and weight of the real patient according to Dirnberger et al.21 was created and the digital picture was superimposed in the computer system.
The burns were transferred to the model in three steps and the TBSA in % was calculated by the software BurnCase 3D (Fig. 2).21 For each patient the mean +/- standard deviation, the minimum estimated value (min.) and the maximum estimated value (max.) were calculated. The difference between the mean value and software result was used in order to demonstrate over- or underestimation.
Fig. 2. Burn wound data transfer from superimposed picture to 3D model with “BurnCase 3D”. To archive an optimal result, the model was overlapped with the picture in three separate steps. The first picture shows the patient only, the second picture shows the overlapping for transferring the burns on head. The third and fourth picture shows the overlapping positions for transferring chest and arm. On the most right picture, the virtual model with all burns transferred is shown.

Results
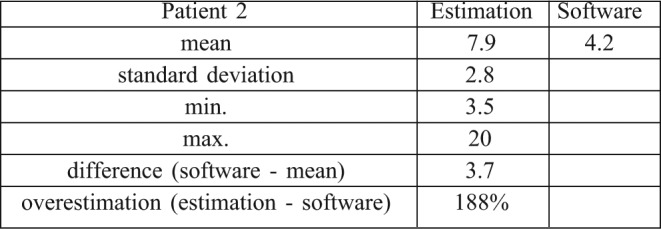
The total number of respondents was 80. The majority of respondents were specialists (32), followed by residents (27), and nursing staff (21). The preferred methods on a regular basis for burn extent estimation was headed by Rule of Nines (38.0%) closely followed by the Rule of Palm (37%) and the Lund-Browder chart (18.0%). Other techniques were mentioned in only 8.0%. The detailed results of each patient (Patient 1-3) are presented in Table I-III. To conclude, the analysis shows very high deviations of TBSA across the participants, even in the group of experts. In comparison to a computer-aided method we found massive overestimation of up to 230%.
Table I. Results of patient 1 (2 years-of-age, male, 12kg, 87cm).
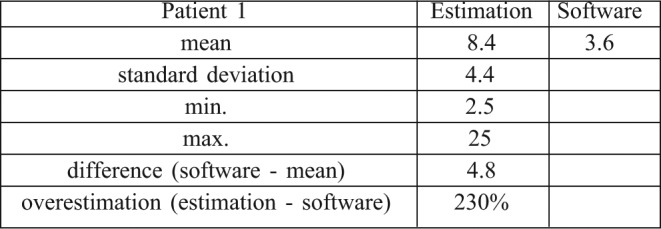
Table III. Results of patient 3 (4 years-of-age, female, 16kg, 102cm).
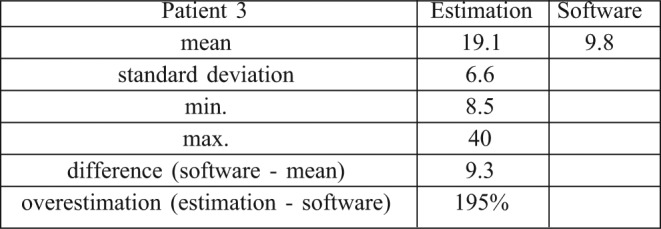
Table II. Results of patient 2 (35 years-of-age, male, 80kg, 182cm).
Technical description
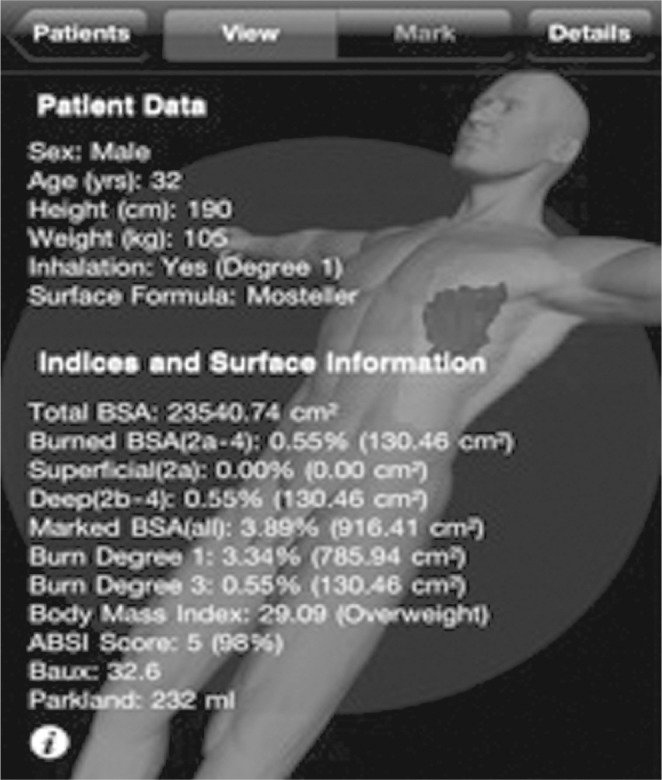
The latest software version 2.6 of BurnCase 3D can be installed on any Microsoft Windows PC. A mobile version is also available for the Apple iPhone.™ The system operates on a 3D virtual body representing the real patient. In simple terms, this model is built up as a three-dimensional mesh of over 90,000 connected triangles with each smaller than one square centimeter (cm2). By specifying age, sex, height and weight, and choosing an appropriate 3D standard model, the system generates an automatically adapted virtual body surface, which accurately fits the patient’s individual body shape. The standard model is precisely adapted to the patient’s height by scaling in longitudinal direction. Afterwards, a surface adaptation algorithm inflates the model until its TBSA exactly reaches the predicted value calculated by an established TBSA estimation formula. BurnCase 3D incorporates 12 of the most common TBSA estimation formulae in science.3,4 The adaptation algorithm also takes into account the growth behaviour of different body regions in order to reach a realistic body expansion. The research project BurnCase 3D has been ported to a mobile device to provide the possibility of a continuous documentation process throughout burn treatment. In the mobile version, by usage of the highly sensitive touchscreen, it is possible to mark the wounds and surgical procedures directly on the mobile device and take digital pictures of the wounds, e.g. during dressing changes. Therefore, the documentation needed by the physician is always provided. Data transfer from the mobile to the desktop version is also supported.
User interface
In the current desktop/mobile application, the burned surface area can be marked manually on a 3D body surface by touchscreen interaction, stylus or conventional mouse. The software then projects a two dimensional polygon onto the underlying three-dimensional body, and the marked area appears in a predefined colour and pattern, visualizing different degrees of burn or surgical procedures, dressings, medications or wound conditions. The covered surface area, the TBSA, and subsequently numerous medical scores (e.g. ASBI, Baux, Baxter-Parkland, etc.) are calculated simultaneously by the software and presented on the user interface immediately after drawing. By rotating and zooming the model all parts of the body can be visualized and documented (Figs. 3,4,5,6).
Fig. 3. Choosing an appropriate 3D standard model.
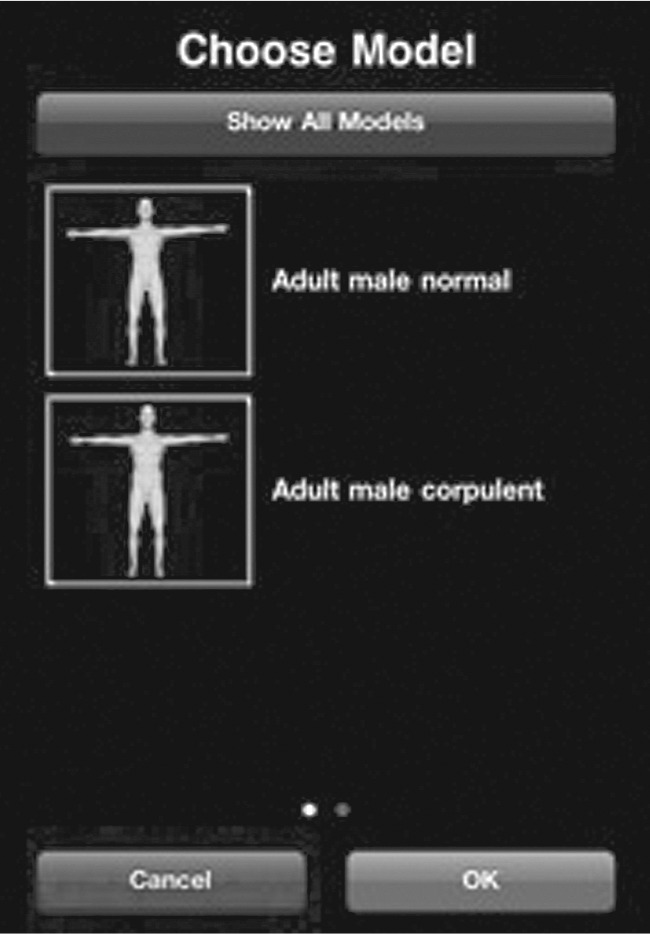
Fig. 4. The burned surface area can be marked manually on a 3D body surface by touchscreen interaction.
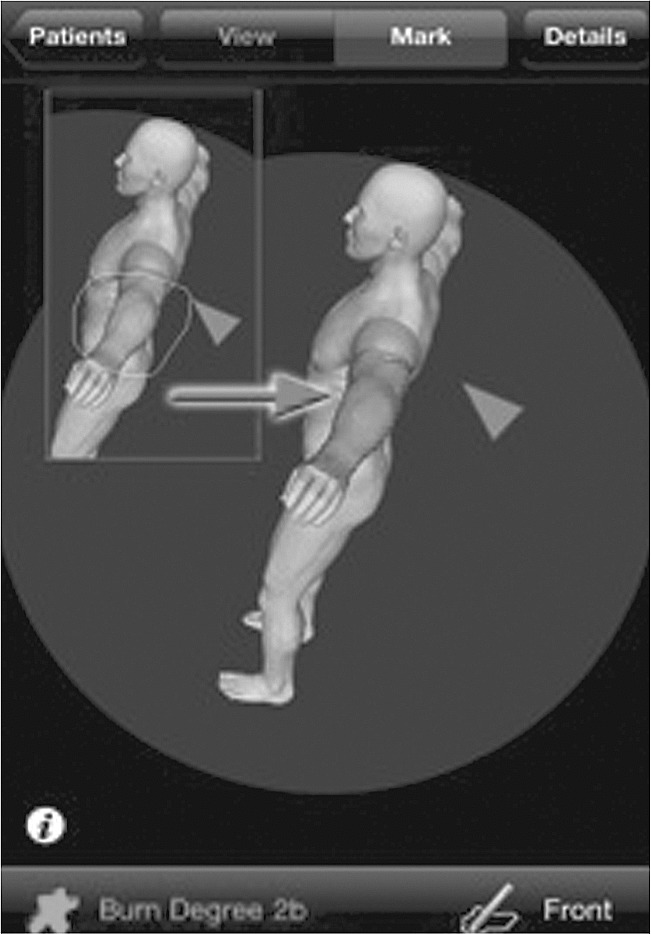
Fig. 5. BurnCase 3D incorporates the 12 most widely accepted TBSA estimation formulas in scientific.

Fig. 6. By specifying age, sex, height and weight and choosing an appropriate 3D standard model the system generates an automatically adapted virtual body surface, which accurately fits the patient’s individual body shape. Afterwards, a surface adaptation algorithm inflates the model until its TBSA exactly reaches the predicted value calculated by an established TBSA estimation formula.
In the near future, features mentioned in the PC version will be implemented on the mobile system.
Additional data fields for information will be available for documentation purposes, including, for example, cause of accident, past medical history, condition on admission, etc. In order to be able to supervise all changes to the stored data, the software keeps track of every data entry or deletion in a separate change log. The data collection is compatible to the United States’ National Trauma Registry (NTRACS).
An additional feature is the intuitive assignment of digital photographs to patients, dates, areas, burn conditions, procedures and notably 3D locations. Photos are then made searchable by these criteria. By integrating the processing of false-colour pictures generated by burn depth determination systems, burns can be automatically transferred to the 3D model. The system superimposes the digital image and aligns the model and the patient on the picture. A special algorithm automatically projects all false-coloured areas onto the model surface (Fig. 7).
Fig. 7. The integrated picture archive and alignment allow simple, fast, objective selection of TBSA-B and visual verification of acquired wound surfaces.
Discussion
Telemedicine is a rapidly growing technique in modern medicine, providing more efficiency and a better communication between clinicians.14 Telemedicine systems have proved useful in reducing unnecessary transfers in acute burn injuries15 and in reducing mortality, complications and costs in intensive care.16 Current mobile phone mainstream technology provides resolution superior to the earliest telemedicine programmes,17 and substantially better than the computer workstations of over only a decade ago.18 This may finally deliver on the promise of technology truly organised around the clinicians,19 especially if high quality interactive video mobile phones become ubiquitous, familiar, easily available and reliable. Furthermore, interactive dynamic systems are now available on many mobile phone and portable devices (e.g. SkypeTM, ooVooTM, FaceTimeTM and other mobile phone applications) as simple single touch applications.
Telemedicine evaluation for patients with major burns, helped speed provision of appropriate critical care and justify the expense and risks of air transport; patients with smaller burns were quickly identified for economical ground transport or given definitive local care at great cost savings, all without apparent increase in undertriage. Evaluation of burn injuries via telemedicine by experienced physicians is more precise, and correlates more closely with face to face assessment than do the estimates of on-the-spot providers/physicians, and is accurate enough to use in triage decision-making.20 For static applications, even mobile phones have surpassed the minimum requirements and provide sufficient information for burn assessment in case series,20,21 and Shokrollahi et al.20 demonstrate high correlation (r = 0.9) for minor burn assessment on the mobile phone compared to face-to-face. Wallace et al.13 do not document burn size estimation, although subgroup analysis shows a significantly improved accuracy of triage. Standard digital cameras have now surpassed this threshold, so that concerns over resolution missing subtle findings on computer screens are out-ofdate, 22-24 although this might prove relevant for the (small) size of mobile phone displays. For burn injuries in particular, a zoning image has been useful in the accuracy of diagnosis.25 One of the major determinants concerning burn severity is the risk factor of developing burn-related shock. Typically, adult patients are at risk of developing shock if they have burns greater than 15-20% of their body surface area (TBSA) and 10% in children. These patients require fluid resuscitation.
According to our data, some experts have estimated that our patients have burn sizes around 10% (Patient 1 and 3) and 15% (Patient 2) and that they will require “real” fluid resuscitation. This is the second most important aspect of exact burn size evaluation, because there is a direct relationship between fluid resuscitation and the burn size. We all know that too much volume will lead to more volume again. The highest overestimation was observed in the patient with the small scattered areas and the lowest overestimation in the patient with the single large area. Consequently, it seems that it is more difficult to estimate scattered surfaces than one big area; that is why we have to take special care when dealing with small and midsize burns, where we have found the biggest differences concerning minimal and maximal values, and also in comparison to the computer assisted burn size evaluation. Overresuscitation leads to dramatic fluid accumulation with oedema formation and complications such as abdominal compartment syndrome or cerebral oedema.
In comparison to the estimations done by experts, the software calculates significantly lower values. This shows a general overestimation and thereby a higher risk for overresuscitation could be shown compared to the computer analysis within all three patients. While it is absolutely right that these formulas are only first estimations and that we have to adapt our infusions according to the needs of the patients, the burns size factor is at least of the same importance, because it is a major factor in determining how we will start our fluid resuscitation protocol. We think that we have to determine burn size, one of the key factors in burn care, more precisely and in a more objective way.
By combining digital pictures with BurnCase 3D, the level of burn assessment and its accuracy can be improved. The use of a mobile device renders such a task more feasible by simply sketching the border of burn wounds on a picture on the mobile device. First results of the Burn- Case 3D project have been published by Dirnberger and Giretzlehner.26 BurnCase 3D is currently deployed in several burn units in Europe and the USA; since 2004 a continuously growing number of hospitals are using the system for their burn surface estimation and documentation and a free download version is available. Regular user feedback is necessary for continuous improvement of the system.
In the near future, further refinements will be implemented in the mobile version.12,26-28 Additional burn-related information, such as cause of burn, first aid, complications, previous illnesses, condition at admission, etc., as well as an intuitive model-picture-registration algorithm, which allows the physician to easily move the virtual body in the position of the patient on any digital picture, will be installed in the mobile system. Currently the research team is working on the implementation of the mobile version of BurnCase 3D for the GoogleTM operating system Android.TM
The ubiquitous availability of mobile smartphones among physcicians and allied health professionals enables using this hardware for the software application of a burn documentation system in the form of aplications. The benefits of using a mobile 3D computer-aided burn classification and documentation procedure over two-dimensional estimation charts are obvious. In first aid treatment, this software system may lower the risk of over- and underestimation of burn wounds by the less experienced. Secondly, a tremendous reduction of workload for documentation purposes for the physician is a major advantage, resulting in more time for patient treatment. A comprehensive three-dimensional track of the complete treatment history is created and stored in the database for every patient. It therefore fulfills the requirements of many countries to run complication statistics, and it offers a means to determine clinical complexity levels and to aid outcome prediction.28
Compared to the other various computer based systems for estimation of TBSA, BurnCase 3D provides an objective diagnostic method for burn injuries. Furthermore, BurnCase 3D is designed to provide data for clinical studies between different institutions and countries.29,30
Consequently, an improvement of the outcome of burn patients can be achieved. In order to reach this goal, it is necessary to deploy the system on a broad basis of burn units all over the world and to collect the experiences of these. It is clearly stated by the development team, that a lot of work has to be done in order to scientifically prove the correctness and accuracy of the surface estimation results. Particularly in infant and obese patients, the model library still has limitations. Perhaps in the future, the application BurnCase 3D may provide a triage service for emergency doctors to inform their hospitals about the physical status of patients. It is also worth mentionning that emergency units still use telemedicine with reasonable results for cardiac disease and monitoring heart patients.31,32
References
- 1.Hammond JS, Ward CG. Transfers from emergency room to burn center: Errors in burn size estimate. J Trauma. 1987;27:1161–5. doi: 10.1097/00005373-198710000-00011. [DOI] [PubMed] [Google Scholar]
- 2.Nichter LS, Bryant CA, Edlich RF. Efficacy of burned surface area estimates calculated from charts–the need for a computerbased model. J Trauma. 1985;25:477–81. doi: 10.1097/00005373-198506000-00001. [DOI] [PubMed] [Google Scholar]
- 3.Livingston EH, Lee S. Percentage of burned body surface area determination in obese and nonobese patients. J Surg Res. 2000;91:106–10. doi: 10.1006/jsre.2000.5909. [DOI] [PubMed] [Google Scholar]
- 4.Livingston EH, Lee S. Body surface area prediction in normalweight and obese patients. Am J Physiol Endocrinol Metab. 2001;281:586–91. doi: 10.1152/ajpendo.2001.281.3.E586. [DOI] [PubMed] [Google Scholar]
- 5.Verbraecken J, Van de HP, De BW, et al. Body surface area in normal-weight, overweight, and obese adults. A comparison study. Metabolism. 2006;55:515–24. doi: 10.1016/j.metabol.2005.11.004. [DOI] [PubMed] [Google Scholar]
- 6.Tsai SH, Kraus J, Wu HR, Chen WL, Chiang MF, Lu LH, Chang CE, Chiu WT. The effectiveness of video-telemedicine for screening of patients requesting emergency air medical transport (EAMT). J Trauma. 2007;62:504–11. doi: 10.1097/01.ta.0000219285.08974.45. [DOI] [PubMed] [Google Scholar]
- 7.Callahan CW, Malone F, Estroff D, Person DA. Effectiveness of an Internet-based store-and-forward telemedicine system for pediatric subspecialty consultation. Arch Pediatr Adolesc Med. 2005;159:389–93. doi: 10.1001/archpedi.159.4.389. [DOI] [PubMed] [Google Scholar]
- 8.Sagraves SG, Phade SV, Spain T, Bard MR, Goettler CE, Schenarts PJ, Toschlog EA, Newell MA, Claims BA, Peck MD, Rotondo MF. A collaborative systems approach to rural burn care. J Burn Care Res. 2007;28:111–4. doi: 10.1097/BCR.0B013E31802C893B. [DOI] [PubMed] [Google Scholar]
- 9.Smith AC, Youngberry K, Mill J, Kimble R, Wootton R. A review of three years experience using email and videoconferencing for the delivery of post-acute burns care to children in Queensland. Burns. 2004;30:248–52. doi: 10.1016/j.burns.2003.11.003. [DOI] [PubMed] [Google Scholar]
- 10.Redlick F, Roston B, Gomez M, Fish JS. An initial experience with telemedicine in follow-up burn care. J Burn Care Rehabil. 2002;23:110–5. doi: 10.1097/00004630-200203000-00007. [DOI] [PubMed] [Google Scholar]
- 11.Thomas C, Prasanna M. The role of a ‘satellite-service’ in the national organisation of burn care in the Sultanate of Oman. Burns. 2000;26:181–5. doi: 10.1016/s0305-4179(99)00115-1. [DOI] [PubMed] [Google Scholar]
- 12.Haller HL, Dirnberger J, Giretzlehner M, Rodemund C, Kamolz L. Understanding burns: Research project BurnCase 3D-overcome the limits of existing methods in burns documentation. Burns. 2009;35:311–7. doi: 10.1016/j.burns.2008.07.010. [DOI] [PubMed] [Google Scholar]
- 13.Wallace DL, Smith RW, Pickford MA. A cohort study of acute plastic surgery trauma and burn referrals using telemedicine. J Telemed Telecare. 2007;13:282–7. doi: 10.1258/135763307781644933. [DOI] [PubMed] [Google Scholar]
- 14.Ashworth DR, Liggins S. Digital photography in the management of maxillofacial trauma. Br J Oral Maxillofac Surg. 2004;42:275–6. doi: 10.1016/j.bjoms.2003.12.003. [DOI] [PubMed] [Google Scholar]
- 15.Hsieh CH, Jeng SF, Chen CY, et al. Teleconsultation with the mobile camera phone in remote evaluation of replantation potential. J Trauma. 2005;58:1208–12. doi: 10.1097/01.ta.0000175098.52974.fa. [DOI] [PubMed] [Google Scholar]
- 16.Barrett M, Larson A, Carville K, Ellis I. Challenges faced in implementation of a telehealth enabled chronic wound care system. Rural Remote Health. 2009;9:1154. [PubMed] [Google Scholar]
- 17.Murphy Jr RL, Fitzpatrick TB, Haynes HA, Bird KT, Sheridan TB. Accuracy of dermatologic diagnosis by television. Arch Dermatol. 1972;105:833–5. [PubMed] [Google Scholar]
- 18.Krupinski E, Gonzales M, Gonzales C, Weinstein RS. Evaluation of a digital camera for acquiring radiographic images for telemedicine applications. Telemed J E Health. 2000;6:297–302. doi: 10.1089/153056200750040156. [DOI] [PubMed] [Google Scholar]
- 19.Yellowlees PM. Successfully developing a telemedicine system. J Telemed Telecare. 2005;11:331–5. doi: 10.1258/135763305774472024. [DOI] [PubMed] [Google Scholar]
- 20.Shokrollahi K, Sayed M, Dickson W, Potokar T. Mobile phones for the assessment of burns: We have the technology. Emerg Med J. 2007;24:753–5. doi: 10.1136/emj.2007.046730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Knobloch K, Rennekampff HO, Vogt PM. Cell-phone based multimedia messaging service (MMS) and burn injuries. Burns. 2009;35:1191–3. doi: 10.1016/j.burns.2009.03.012. [DOI] [PubMed] [Google Scholar]
- 22.Scott Jr WW, Rosenbaum JE, Ackerman SJ, Reichle RL, Magid D, Weller JC, et al. Subtle orthopedic fractures: Teleradiology workstation versus film interpretation. Radiology. 1993;187:811–5. doi: 10.1148/radiology.187.3.8497636. [DOI] [PubMed] [Google Scholar]
- 23.Jacobs MJ, Edmondson MJ, Lowry JC. Accuracy of diagnosis of fractures by maxillofacial and accident and emergency doctors using plain radiography compared with a telemedicine system: A prospective study. Br J Oral Maxillofac Surg. 2002;40:156–62. doi: 10.1054/bjom.2001.0751. [DOI] [PubMed] [Google Scholar]
- 24.Loane MA, Gore HE, Corbett R, Steele K, Mathews C, Bloomer SE, et al. Effect of camera performance on diagnostic accuracy: Preliminary results from the Northern Ireland arms of the UK Multicentre Teledermatology Trial. J Telemed Telecare. 1997;3:83–8. doi: 10.1258/1357633971930913. [DOI] [PubMed] [Google Scholar]
- 25.Jones SM, Milroy C, Pickford MA, et al. Telemedicine in acute plastic surgical trauma and burns. Ann R Coll Surg Engl. 2004;86:239–42. doi: 10.1308/147870804344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Dirnberger J, Giretzlehner M, Ruhmer M, Haller H, Rodemund C. Modelling human burn injuries in a threedimensional virtual environment. Stud Health Technol Inform. 2003;94:52–8. [PubMed] [Google Scholar]
- 27.Dirnberger J, Giretzlehner M, Luckeneder T, Siegl D, Haller HL, Rodemund C. BurnCase 3D-realistic adaptation of 3-dimensional human body models. LNCS. 2004;3217:363–70. [Google Scholar]
- 28.Haller H. Data collection in burn injuries-rationale for BurnCase 3D. Osteo Trauma Care. 2007;15:34–41. [Google Scholar]
- 29.Neuwalder JM, Sampson C, Breuing KH, Orgill DP. A review of computer-aided body surface area determination: SAGE II and EPRI’s 3D Burn Vision. J Burn Care Rehabil. 2002;23:55–9. doi: 10.1097/00004630-200201000-00011. [DOI] [PubMed] [Google Scholar]
- 30.Buttemeyer R, Steen M, Henkel VD, Germann G. Establishing a baseline for organisation and outcome in burn care-basic data compiled by German burn centres, 1991–2000. Burns. 2004;30:115–20. doi: 10.1016/j.burns.2003.08.008. [DOI] [PubMed] [Google Scholar]
- 31.Brunetti ND, Dellegrottaglie G, Lopriore C, Di Giuseppe G, De Gennaro L, Lanzone S, Di Biase M. Prehospital telemedicine electrocardiogram triage for a regional public emergency medical service: Is it worth it? A preliminary cost analysis. Clin Cardiol. 2014 doi: 10.1002/clc.22234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Klack L, Ziefle M, Wilkowska W, Kluge J. Telemedical versus conventional heart patient monitoring: a survey study with German physicians. Int J Technol Assess Health Care. 2013;29:378–83. doi: 10.1017/S026646231300041X. [DOI] [PubMed] [Google Scholar]


