Abstract
Gentian violet (GV) has a long and varied history as a medicinal agent. Historically used as an anti-bacterial and anti-fungal, recent reports have shown its utility as an anti-typranosomal, anti-viral and anti-angiogenic agent. The objective of this paper is to summarize evidence regarding the efficacy, and safety of GV use in dermatology. Recent discoveries have found novel targets of GV, namely NADPH oxidase in mammalian cells and thioredoxin reductase 2 in bacterial, fungal, and parasitic cells. These discoveries have expanded the use of GV in the 21st century. Given that GV is well tolerated, effective and inexpensive, its use in dermatology is predicted to increase.
Keywords: Gentian Violet, crystal violet, triphenylmethane dye, triphenylmethane dye
Introduction
Gentian violet ((GV) hexamethyl pararosaniline, also known as crystal violet, methyl violet) is a triphenylmethane dye with anti-bacterial, anti-fungal, anti-helminithic, anti-trypanosomal, anti-angiogenic and anti-tumor properties. GV has a lengthy history and has been used successfully as monotherapy and an adjunct to treatment in a variety of diseases.
Synthesis of GV was attributed French chemist Charles Lauth in 1861 under the name of ‘Violet de Paris’1 and was popularized by George Grubler, a German pharmacist in 1880.2 Grubler marketed his dye only to biologists and it was not used in textiles.3 In 1884 Hans Gram noted the irreversible fixation of GV by Gram positive bacteria, which became the basis of the Gram stain for categorizing bacteria.4 GV was first introduced as an antiseptic by Stilling in 1891, which he marketed as pyoctanin. Stilling made boisterous claims about pyoctanin’s therapeutic use and advocated it for wounds, ulcers and infections of the eye. One physician from Vienna reported injections of pyoctanin successfully treating two cases of sarcoma6, predating GVs use in the treatment of malignant melanoma and as an inhibitor of angiogenesis by over 120 years. However, pyoctanin did not come into favor and its curative allegations were disputed.7 For the next two decades, further experimentation with GV in human subjects was abandoned.
In 1912, Churchman noted the bacteriostatic action of GV against Gram-positive microorganisms both in vitro and in animal studies.8 Based upon results from Churchman, in 1925 Hinton used GV intravenously in 12 patients with severe sepsis from Gram positive organisms, of which seven patients improved.9 In 1928, a case of staphylococcal meningitis was also cured by intrathecal injections of GV.10 Throughout the first half of the 20th century, GV was widely adopted for use in a variety of diseases including trench mouth11, thrush12, impetigo13, burns14, pinworm15, cutaneous16 and systemic fungal infections17. Claims of GVs efficacy during this time period are difficult to ascertain, given that the composition of GV dyes varied and the authors did not always describe the solutions used in their publications. Following discovery and mass production of sulfa drugs and penicillin in the 1940’s, GV fell out of favor with physicians and scientific research became focused on the discovery of novel classes of antibiotics.
With the emergence of antibiotic resistance there has been a recent resurgence into the GV therapy for anti-sepsis, as well as for a variety of other uses. Recent studies of its mechanisms of activity have expanded its potential uses in dermatology. GV is readily available, inexpensive ($0.16 USD/mL for a 2% solution)18, easy to use and has minimal side effects. The purpose of this article is to review uses of GV in dermatology as well as to discuss potential applications and areas of future research.
Definition of Gentian Violet
Today, GV USP is defined as hexamethylrosaniline, a completely symmetric molecule in which every amino group contains 2 methyl groups.19 Given that GV is a trimer of dimethylaniline, which is resonance stabilized to yield a highly colored compound, there are six methyl groups. However, in the past, there was considerable variability of the composition of GV, with compounds containing less than the maximum 6 methyl groups possible. Early preparations of GV were called methyl violet, and had mixtures of hexamethylrosaniline (GV, Methyl violet 10B, crystal violet) and pentamethylrosaniline (Methyl violet 2B).
Antibacterial activity
GV was revisited as an anti-microbial for dermatological disease by Bakker et al in 1992.20 The authors were investigating writing a formulary for dermatological preparations to be used in developing countries. Thus they required a drug that was inexpensive, simple to prepare, chemically stable, active in low concentrations, with a broad spectrum and minimal resistance as well as minimal toxicity. The authors applied gentian violet and a related triphenylmethane dye, brilliant green, to 5 bacterial species (Streptococcus A & B, Proteus, Pseudomonas aeruginosa and Staphylococcus aureus) as well as Candida albicans in vitro. The study showed that GV was very effective, with a low critical concentration, against Candida and Streptococcus and Staphylococcus species, and moderately effective against the Gram negative bacteria. GV was found to be more potent and effective against a greater number of bacteria than its related compound, brilliant green. The investigators also found that increasing the pH lead to greater activity of GV against S. aureus.
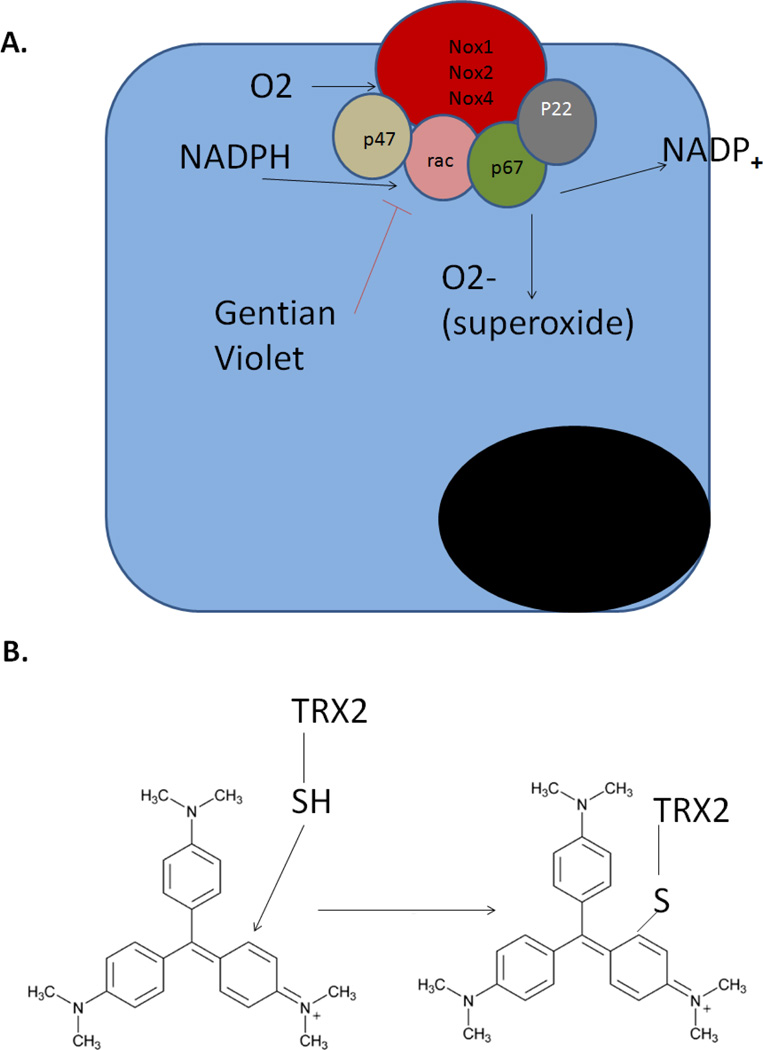
The exact mechanism of action of GV is unknown.21 Multiple hypothesis exist for an explanation of its anti-microbial effects4,22: an alteration in redox potential by the dye23, inhibition of reduced nicotinamide adenine dinucleotides phosphate (NADPH) oxidases24, free radical formation25,26, formation of an un-ionized complex of bacteria with the dye27, inhibition of protein synthesis28,29, inhibition of glutamine synthesis29, uncoupling of oxidative phosphorylation31 or inhibition of formation of the bacterial cell wall32. Recently, our group discovered that the closely related dye brilliant green formed covalent adducts with thioredoxin reductase 2, a protein conserved from bacteria to humans, with an essential function for cellular activity (Figure 1).33 Notably, gentian violet is highly effective against Gram positive bacteria, which also form adducts with gentian violet, due to its ability to penetrate the bacterial cell wall and covalently bond to proteins. GV is far less effective against Gram negative bacteria and Mycobacterium, presumably due to its inability to penetrate the lipids surrounding the cell wall. This is the basis of the Gram stain, which is still in clinical use for over a century.
Figure 1. Dual mechanisms of action of Gentian violet.
In mammalian cells (A), GV blocks the activity of NADPH oxidases 1,2, and 4 to inhibit the conversion of molecular oxygen to superoxide. Decreased superoxide results in decreased oxidation of IkB, leading to NFkB inhibition and anti-inflammatory activity. In bacterial, fungal, and parasitic cells (B), GV forms a covalent adduct with thioredoxin reductase 2 (TRX2), leading to malfunction of TRX2 and subsequent cell death.
Clinical studies of the efficacy of GV in skin infections are mostly limited to case reports and case series with a small number of patients. Brockrow et al. investigated the use of GV in impetiginized eczema both in vitro and in vivo.34 The researchers divided 38 consecutive patients with acute eczema colonized with S. aureus into three treatment groups: 0.3% GV, topical diflucortolone, and a 10% tar solution. Of the three treatments, GV was the only treatment to show anti-staphylococcus activity in vitro. Additionally, GV was found to significantly reduce S. aureus density in lesional and unaffected skin and also significantly reduced the clinical severity of eczema after 4 days. No adverse events were reported by the authors. In a 2010 study, the senior author (JA) also reported a case of severe eczema superinfected with group A Streptococcus, unresponsive to conventional therapy, successfully treated with oral doxycycline and daily applications of a 1% solution of GV.35 The results of these studies are concordant with the recent evidence that treatment of impetiginized eczema reduces eczema severity.36
GV has also been used for many years in preventing bacterial colonization of the umbilical stump following childbirth.37,38
Treatment of Methicillin Resistant Staphylococcus aureus
Multiple studies have proven GVs efficacy against methicillin resistant Staphylococcus aureus (MRSA).39 Taguchi et al. first documented GVs effectiveness against MRSA in vivo.40 Similar to the observations by Bakker et al. with methicillin sensitive staphylococcus aureas20, GV was found to have a very low minimum inhibitory concentration against MRSA. Clinically, multiple studies have shown GVs use against MRSA in the setting of ulcers. A randomized controlled trial performed by Toba et al. showed that GV, when compared to standard treatment of MRSA infected ulcers with iodine, was more effective in killing MRSA.41 After 14 weeks of treatment with GV, the pressure ulcers decreased to 45% of the area at the start of treatment and no adverse events occurred during the study period. Saji et al. showed that by using an ointment containing 0.1% gentian violet to 12 cases of patients with MRSA infected decubitis ulcers, MRSA was eliminated completely from the infected areas of the skin within 4 weeks.42 A subsequent report by the same group showed that among 18 patients with MRSA infected ulcers, the average time to eradication of MRSA was 10.8 days (+/− 2.7).43 In both studies, there were not any appreciable side effects among the patients treated with GV. Recently, among 28 cases of MRSA pyodermas treated with GV, Okano et al. found that the mean time for eradication was 9.1 +/− 6.0 days.44 Concurrent with findings from previously mentioned studies, GV had a low minimum inhibitory concentration for MRSA and no appreciable side effects were reported.
Outside the field of dermatology, GV has been successfully to treat MRSA in otitis media45, mediastinitis46, prosthetic vascular bypass graft infection47, as well as nasal carriage of MRSA44. In the face of increasing incidence and emerging resistance to standard therapies, GV has emerged as a potential treatment option for MRSA infections.
Treatment of Gram negative organisms
While early studies of GV found it to be less effective against Gram negative organisms8, separate studies by Bakker20 and Fung48 have found that GV inhibited growth of Pseudomonas, an extremely virulent Gram negative rod, in vitro. Recently a report by Wang et al.49 showed that GV disrupts Pseudomonas biofilms in vitro. Biofilms are an organized community of microorganisms encased in an extracellular matrix that is adherent to a surface and are a significant a source of resistance to host defense as well as resistance to anitbiotics.50 Additionally, invasive devices such as endotracheal tubes, central venous catheters, and urinary catheters coated with gendine, a mixture of gentian violet and chlorhexidine, have been shown to reduce bacterial adherence and prolong antimicrobial durability against the Gram negative organisms Pseudomonas, E. Coli and Klebsiella both in vitro and in vivo.51,52 These findings build upon previous research by Bhatnagar, who showed that GV’s antibacterial effects on silastic implants.53
Antimycotic activity
Churchman first showed the antimyoctic effects of GV against multiple species of Candida in his initial 1912 experiments.8 In 1927, intravenous GV was reported to have treated a systemic Blastomyces infection.17 Currently, multiple studies have proven the efficacy of GV against Candida in the setting of catheter infections.51,52,54 GV was shown to not only have direct fungicidal action, but also disrupt the adherence of Candida to catheters. Silver alloy coated urinary catheters are currently the most common catheter used in the United States, but only reduce the relative risk of UTI by 32%.55 GV coated catheters were found to be significantly superior to silver alloy urinary catheters in reducing colony counts of seven different microorganisms as well as reducing E. Coli burden in the bladder and urine in an in vivo rabbit model.51
GV has also been used extensively for oral candidasis (thrush). Painting the mouth of an infant with oral thrush with GV has for more than 90 years been a safe and effective treatment.12,56,57 More recently, GV has been used to treat oral candidasis in human immunodeficiency virus (HIV) infected individuals, especially in developing countries58,59 where treatment with fluconazole is impractical due to availability, cost of treatment and the development of resistance.60,61 In a randomized trial comparing GV to nystatin and ketoconazole amongst patients with HIV and oral candidasis, after 14 days, 11/26 (42%) patients treated with GV had complete resolution of their disease, compared with 10/23 (43%) patients treated with ketoconazole and only (2/23 (9%) patients treated with nystatin.58
GV has shown excellent anti-candidal efficacy in vitro, with significantly greater antimycotic activity against 91 candidal strains than other topical alternatives to fluconazole such as chlorhexidine and povidone iodine in one study62, and a markedly lower minimal inhibitory concentration when compared to povidone iodine against 102 yeast isolates in a second study.63 GV has also been found to inhibit biofilms of Candida isolates taken from HIV infected patients in vitro.64
Currently we also use gentian violet for onychomycosis, with application of 1–2% GV to pared nails 3× weekly for one month, and have noted significant improvement (unpublished data). Further studies are needed to establish mycological clearance.
In the previously mentioned studies, topical application of GV for oral candidasis was well tolerated by all of the patients, with staining of the teeth and infrequent local irritation being the only reported concerns.58,59 There have been reports toxicity of gentian violet in the treatment of oral candidiasis, including oral mucosal irritation65,66 and necrosis67, difficulty with breast feeding68 and obstructive laryngotracheitis69.
Recently our group demonstrated that tinea versicolor retains topical GV and that GV can be applied as a bedside test to determine the presence of fungal colonization since other hypopigmentary disorders do not accentuate with GV. We have named this phenonmenon in vivo Gram staining.70
Additional antimicrobial effects
In addition to having antibacterial and antimycotic properties, GV is also effective against a broad spectrum of infectious agents. GV has been used since the 1950’s as a blood additive for prevention of the transmission of Chagas’ disease (caused by protozoan parasite T. cruzi) in Latin America where the disease is endemic.71–73 GV has been postulated to form a radical by abstracting an electron from NADPH or NADH that is cytotoxic to the Chagas trypanosome.74
Hundreds of thousands of patients have received blood transfusions containing GV, without side effects and without any reported cases of transmissible Chagas disease.73,75 A recent study found that GV was effective against the protozoa Leishmania, the causative agent of cutaneous leshmaniasis, both in vitro and in vivo in a mouse model.76 Gentian violet has also been used historically to treat the parasitic nematodes Strongyloides77,78 and Enterobium (pinworm)15,79,80.
Two studies have shown GV to have antiviral activity. A case report published by the author (JA) reported complete resolution of biopsy proven oral hairy leukoplakia (caused by the Epstein-Barr virus) in an HIV infected patient following 3 treatments with GV.81 A 2009 study demonstrated the anti-viral properties of GV in vitro against the Nipah and Hendra viruses.82
Anti-angiogenesis and anti-tumor activity
Recent investigational use of GV has shown that it is efficacious as both an anti-angiogenic and anti-tumor agent. Angiogenesis is the generation of new microvessels sprouting from the preexisting vasculature, and has been implicated in the development of a number of dermatological conditions, including hemangiomas, psoriasis, atopic dermatitis, lupus, tumor growth and metastasis.83 As such, angiogenesis is a pivotal target for development of pharmacological treatments for a variety of conditions. Angiopoietins are Tie2 receptor ligands that play key roles in angiogenesis. Angiopoietin-2 (ang-2) in particular is a mediator of pathologic vascular permeability, while angiopoietin-1 mediates vascular stability. Ang-2 is stored in endothelial cells and expressed in growing blood vessels. It promotes angiogenesis and tumor growth by destabilizing blood vessels84 and is also involved in promotion of vascular leak in the inflammatory response, allowing cellular elements to translocate across the vascular wall.85 Because of its role in mediating inflammatory and tumor angiogenesis, ang-2 is a particular target of antiangiogenic strategies, because blockade of ang-2 results in a decrease of both vascular permeability and angiogenesis. This process has been termed vascular normalization.86–90 Inhibition of Ang2 may promote vessel stability and reduce angiogenesis as well as promote antibiotic delivery to sites of infection by reducing third spacing.39 Finally, NADPH oxidase blockade may impinge on additional inflammatory pathways. Ultraviolet radiation induces NADPH oxidase activates the NLRP3 inflammosome. The NLRP3 inflammosome then leads to the production of caspase-1, which increases mature IL-1b, and thus stimulates inflammation.91
GV downregulates the production of ang-2 by blocking NADPH oxidase, which is a master regulator of angiogenesis, and regulates both ang-2 and vascular endothelial growth factor.92 In a previous study, we found GV to be effective in reducing intratumor levels of ang-2 expression in a murine model of hemangioma as well as reducing tumor size by 95.7% compared to controls.24 A recent study was performed with topical eosin solution, a triphneylmethlamine dye structurally similar to GV, in treatment of 18 cases of ulcerated infantile hemangioma. Complete ulcer healing occurred in 16 patients after 4 weeks of therapy and decreased ang-2 expression was found in hemangioma cells in vitro following treatment with eosin.93 Topical administration of angiogenesis inhibitors allows targeted therapy and avoids systemic drug absorption and adverse effects such as vessel regression in healthy tissues and rebound angiogenesis following discontinuation of therapy.86,88,94 Further studies are needed to explore the potential benefits of GV as an inhibitor of angiogenesis in dermatological disease. Recently, topical rapamycin has been shown to be effective in inhibiting reperfusion of regeneration and revascularization of photocoagulated blood vessels in humans and animal models of port wine stain birthmarks.95,96
Finally, our group has created triphenylmethane analogs of GV for systemic anticancer therapies. One of our derivatives, imipramine blue, was synthesized from the tricyclic antidepressant imipramine and is considerably more lipophilic than GV. Imipramine blue crosses the blood brain barrier, especially when administered in a liposomal vehicle. Remarkably, imipramine blue prevents the invasive behavior of glioblastoma in rats, and when combined with liposomal doxorubicin, results in long term remission from glioblastoma.97,98 We anticipate that imipramine blue will be useful in the treatment of tumors that use superoxide for signaling, a phenotype known as the reactive oxygen driven tumor.99 Of interest, GV is effective in murine models of mesothelioma.100
Recently, there has been an extensive investigation into angiogenesis inhibitors for the treatment of advanced melanoma, most notably in the clinical trials of Axitinib101 and Bevacizumab102. Further investigations into the clinical benefit of angiogenesis inhibitors in melanoma are needed. We have reported a case of cutaneous melanoma metastasis successfully treated with no recurrence at 6 months with combination of imiquimod and GV.103 It is hypothesized that GV, in addition to directly inhibiting angiogenesis, may potentiate an immune response broader than that of imiquimod alone. A potential mechanism is that melanoma may express immunosuppressive molecules such as B7H1, CD200, indoleamine 2,3-dioxygenase and interleukin-10 which kill cytotoxic T cells and promote the development of regulatory T-cells and myeloid dendritic cells.104–108 We have preliminary data that brilliant green downregulates B7-H1 in a variety of tumor cells (Arbiser and Parsa, unpublished data). Addition of NADPH blockade by gentian violet may enhance the response to interferons by blocking the development of regulatory T-cells and myeloid dendritic cells. Based on these findings, we also routinely use the combination of GV and imiquimod on plantar warts. In the case of plantar warts, we pare the lesions, apply 2% GV, and then instruct the patient to apply GV prior to imiquimod to the warts daily.
Dermatitis and other uses in dermatology
GV has been used successfully for treatment of dermatitis, especially in the setting of radiation. However in a recent survey of 45 external beam radiotherapy institutions in the United Kingdom, GV was only used in 2/45 departments (4%) for moist desquamation, while 33/45 institutions were treating with hydrogels (73%).109 The institutional preference to use hydrogel over GV may stem from the results of two studies, which showed patients prefer hydrogel to GV due to the skin discoloration and drying effect of GV and that GV was less effective than hydrogel in wound healing.110,111 However, these studies are limited by their extremely small sample studies, and further research in this area is needed, especially given the anti-microbial properties of GV compared to hydrogel and the high risk of infection in patients with radiation dermatitis.
There have also been published case reports of GV treating the skin lesions of transgrediens pachyonychia congenita112 and hypereosinophillic syndrome.113 A recent study showing that topical administration of GV may be effective in treating purigo nodularis and atopic dermatitis, and further study is needed.114 We have found that atopic dermatitis expresses high levels of ang-2, accounting for the vascular permeability and erythema observed in atopic dermatitis.35 In addition, since atopic dermatitis is usually colonized with Gram positive organisms, especially MRSA, treatment with GV has the dual benefit of decreasing bacterial colonization as well as reducing proinflammatory ang-2. Finally, it has been demonstrated that crystal violet selectively photo-oxidizes cysteine to cysteic acid over the complete pH range. While this quality has not been fully utilized, it could potentially be used in the future to determine the oxidation state of free sulhydryls in cells and tissue specimens115. The published dermatologic clinical studies of gentian violet are summarized in Table 1.
Table 1.
Clinical studies of cutaneous disorders treated with gentian violet (GV)
| Reference (author, year) | Disorder | Type of study, intervention, number of patients |
Results |
|---|---|---|---|
| Brockrow et al.33, 1999 | Staphylococcus Aureus colonized atopic eczema | Open label trial, comparison between topical 0.3% aqueous gentian violet to diflucortolone-21-valerate and tar solution, n=31 | significant reduction in eczema severity and reduction of S. aureus density after four days |
| Stoff et al.34, 2010 | Group A Streptococcus colonized atopic eczema | Case report, GV 1% solution applied to affected areas twice daily and doxycycline 100 mg bid, n=1 | Complete resolution at two week follow up |
| Toba et al.,40 1997 | Pressure sores infected with MRSA | Randomized controlled trial, GV plus dibutyryl cAMP vs. povidone-iodine plus sugar, n=19 | At 14 weeks mean area of pressure sores decreased by 45%, 93% of culture dishes showed no S. aureus |
| Saij et al.42, 1993 | MRSA infected decubitis ulcers | Open label trial, 0.1% GV applied to ulcers following 2–24 weeks of failed eradication with antibiotic therapy, n=18 | Complete eradication of MRSA in average of 10.5 +/− 2.5 days |
| Okano et al.43, 2000 | MRSA infected pyodermas | Open label trial, 0.5% GV applied qd, n=28 | Complete eradication of MRSA in average of 9.1 +/− 6 days |
| Nyst et al.57, 1992 | oropharyngeal and esophageal candidiasis in AIDS | Randomized unblinded, 0.5% GV aqueous solution vs. ketoconazole vs. nystatin, n=141 | Resolution of oropharyngeal lesions in 42%, improvement in 39%. Resolution of esophageal lesions in 9%, improvement in 32% |
| Wright et al.58, 2009 | Oropharyngeal cadidiasis in AIDS | Randomized controlled trial, 0.5% GV aqueous solution vs. lemon grass vs. lemon juice, n=90 | Resolution of oropharyngeal lesions in 52% |
| Bhandarkar et al.79, 2008 | Oral hairy leukoplakia in AIDS | Case report, 2% GV, n=1 | Complete clinical resolution after three treatments |
| Lapidoth et al.85, 2009 | Ulcerated infantile hemangiomas | Open label trial, Eosin 2% solution tidor qd under dressing, n=18 | Complete ulcer healing in 88% afterfour weeks |
| Arbiser et al.88, 2012 | Cutaneous melanoma metastasis | Case report, 1% GV plus imiquimod follow cryotherapy, n=1 | No recurrence at 6 months follow up |
| Harris et al.97, 2012 | Transgrediens pachyonychia congenita | Case report, 2% GV, n=2 | Substantial clinical improvement |
Toxicity
Since it has been shown that GV can interact with the DNA of cells116, some controversy exists on its safety and oncogenic potential. In vivo studies have shown that GV acts as a mitotic poison as well as a clastogen.117,118 Studies in mice that have been fed extremely large doses of GV showed an increased in hepatocellular carcinoma119,120 and in a large trial conducted by the food and drug administration of the United States (FDA), GV fed to rats were shown to have an increase in thyroid cancer after two years.121 This latter finding is likely due to GVs inhibition of thyroid peroxidase, given the recent finding that GV is a NADPH oxidase inhibitor24, GV likely also inhibits thyroid peroxidase, a structurally similar molecule causing hypothyroidism and feedback stimulation of thyroid-stimulating hormone from the pituitary gland, causing the replication of thyroid cells.122
We believe that GV is extremely safe and without major contraindications for use. Despite more than a century of use, no cases of cancer have been definitively linked to GV. Toxicity of GV in humans is limited to case reports,65–69,123–126 trials involving the use of GV have shown no or very mild adverse effects33,39,40,57,58 and the FDA allows the sale of gentian violet over the counter.
Summary
Gentian violet is an inexpensive drug with a long history of topical use, as well as systemic use, especially in the prevention of Chagas disease through sterilization of blood transfusions in endemic areas of South America. Given that it is stable at room temperature for years, it has become a staple of dermatologic treatment in underdeveloped countries. However, several factors, including the development of antibiotic resistance, use of catheters and indwelling devices, suggest that GV should be used more extensively in the developed world as well. The clinical usefulness of GV appears to be linked to two distinct mechanisms of action (Figure 1). In mammalian cells, GV inhibits the NADPH oxidase complex, including Nox1,2, and 4, leading to downregulation of superoxide production (Fig 1a). In bacteria, fungi and parasites, gentian violet may form a covalent adduct with thioredoxin 2 (Trx2) (Fig 1B). The discovery that GV inhibits NADPH oxidase demonstrates that GV has an effect on the host as well as infectious organisms, and this can be used to augment anti-angiogenesis and tumor immunity in the 21st century.
Gentian Violet has an extensive history as an anti-bacterial and anti-fungal agent
New discoveries have expanded upon its historical uses use, as well as new anti-parasitic, anti-angiogenic and anti-tumor therapies. GV is well tolerated, and inexpensive with a wide spectrum of applications
Acknowledgments
Dr. Maley and Arbiser performed the research, analyzed the data and wrote the paper.
Dr. Arbiser was supported by the grant RO1 AR47901and P30 AR42687 Emory Skin Disease Research Core Center Grant from the National Institutes of Health, a Veterans Administration Hospital Merit Award, as well as funds from the Margolis Foundation, Rabinowitch-Davis Foundation for Melanoma Research and the Betty Minsk Foundation for Melanoma Research.
Abbreviations
- GV
Gentian Violet
- MRSA
Methicillin-resistant Staphylococcus aureus
- HIV
Human Immunodeficiency Virus
- ang-2
Angiopoietin-2
- NADPH
nicotinamide adenine dinucleotide phosphate
- FDA
Food and Drug Administration
Footnotes
Conflicts of Interest
Drs. Maley and Arbiser have no conflicts of interest to report.
References
- 1.Lauth C. On the new aniline dye, Violet de paris. Laboratory. 1867;1:138–139. [Google Scholar]
- 2.Titford M. George Grubler and Karl Hollborn: two founders of the biological stain industry. J Histotechnol. 1993;16:155–158. doi: 10.1179/his.1993.16.2.155. [DOI] [PubMed] [Google Scholar]
- 3.Conn HJ. An investigation of American gentian violets: Report of Committee on Bacteriological Technic. J. Bacteriol. 1922;7:529–536. doi: 10.1128/jb.7.1.127-148.1922. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Balabanova M, Popova L, Tchipeva R. Dyes in Dermatology, Clin Dermatol. 2003;21:2–6. doi: 10.1016/s0738-081x(02)00330-9. [DOI] [PubMed] [Google Scholar]
- 5.Stilling J. The anline dyes and antispetics. Lancet. 1891;137:872–873. [Google Scholar]
- 6.Vienna Lancet. 1891;137:344. [Google Scholar]
- 7.Alumni and Faculty of Medicine of the University of Pennsylvania. Pyoctanin. Vol. 3. The University Medical Magazine; 1890. pp. 38–39. [Google Scholar]
- 8.Churchman JW. The selective bactericidal action of gentian violet. J Exp Med. 1912;16:221–247. doi: 10.1084/jem.16.2.221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hinton D. Results of the intravenous use of gentian violet in chases of extreme septicaemia. Ann Surg. 1925;81:687–692. doi: 10.1097/00000658-192503010-00015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lamb, Frank H. Report of a Case of Staphylococcus Meningitis Treated with Intraventricular Injections of Gentian Violet. Arch. Pediat. 1928;45:306. [Google Scholar]
- 11.Albray R. Vincent's infection of the mouth. Laryngoscope. 1928;4:250–263. [Google Scholar]
- 12.Faber, Harold K, Dickey LB. The treatment of thrush with gentian violet. JAMA. 1925;85:900–901. [Google Scholar]
- 13.Peterkin GAG, Jones EC. Impetigo in the Services. British Medical Journal. 1943;318 [Google Scholar]
- 14.Aldrich RH. The role of infection in burns: the theory and treatment with special reference to gentian violet. New England Journal of Medicine. 1933;208:299–309. [Google Scholar]
- 15.Bumbalo TS, Gustina FJ. The treatment of pinworm infection (enterobiasis) with gentian violet suspension. J Pediatr. 1955;47:311–314. doi: 10.1016/s0022-3476(55)80005-4. [DOI] [PubMed] [Google Scholar]
- 16.Farley DL. The use of gentian violet as a restrainer in the isolation of the pathogenic molds. Arch Derm Syphilol. 1920;2:459–465. [Google Scholar]
- 17.Sanderson ES, Smith DC. The effect of gentian viole ton the organism of blastomycotic infection. Arch Derm Syphilol. 1927;16:153–155. [Google Scholar]
- 18.Gentian violet. [Accessed April 07];2013 Amazon.com. Available from: http://www.amazon.com/GENTIAN-VIOLET-SOL-HUM-Size/dp/B000GCQ05G/ref=sr_1_1?ie=UTF8&qid=1365358396&sr=8-1&keywords=gentian+violet+2%25. [Google Scholar]
- 19.U.S. Pharmacopeial Convention: Gentian Violet USP.org. [Accessed September 04];2013 Available from: http://www.usp.org/pdf/EN/referenceStandards/certificates/1290002-G0E112.pdf. [Google Scholar]
- 20.Bakker P, Van Doorne H, Gooskens V, Wieringa NF. Activity of gentian violet and brilliant green against some microorganisms associated with skin infections. Int J Dermatol. 1992;31:210–213. doi: 10.1111/j.1365-4362.1992.tb03939.x. [DOI] [PubMed] [Google Scholar]
- 21.Burkhart CN, Katz KA. Chapter 222. Other Topical Medications. In: Goldsmith LA, Katz SI, Gilchrest BA, Paller AS, Leffell DJ, Dallas NA, editors. Fitzpatrick's Dermatology in General Medicine. 8th ed. New York: McGraw-Hill; 2012. [Google Scholar]
- 22.Docampo, Roberto, Silvia NJ, Moreno The metabolism and mode of action of gentian violet. Drug metabolism reviews. 1990;22:161–178. doi: 10.3109/03602539009041083. [DOI] [PubMed] [Google Scholar]
- 23.Ingraham MA. The bacteriostatic action of gentian violet and dependence on the oxidation-reduction potential. Journal of Bacteriology. 1933;26:573. doi: 10.1128/jb.26.6.573-598.1933. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Perry BN, Govindarajan B, Bhandarkar SS, et al. Pharmacologic blockade of angiopoietin-2 is efficacious against model hemangiomas in mice. J Invest Dermatol. 2006;126:2316–2322. doi: 10.1038/sj.jid.5700413. [DOI] [PubMed] [Google Scholar]
- 25.Levin D, Lovely T, Klekowski E. Light-enhanced genetic toxicity of crystal violet. Mutation research. 1982;103:283. doi: 10.1016/0165-7992(82)90055-0. [DOI] [PubMed] [Google Scholar]
- 26.Harrelson W, Mason R. Microsomal reduction of gentian violet. Evidence for cytochrome P-450-catalyzed free radical formation. Molecular pharmacology. 1982;22:239–242. [PubMed] [Google Scholar]
- 27.Stearn EW, Stearn AE. The mechanical behavior of dyes, especially gentian violet, in bacteriological media. Journal of Bacteriology. 1923;8:567–572. doi: 10.1128/jb.8.6.567-572.1923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Gustafsson P, Nordström K, Normark S. Outer penetration barrier of Escherichia coli K-12: kinetics of the uptake of gentian violet by wild type and envelope mutants. Journal of bacteriology. 1973;116:893–900. doi: 10.1128/jb.116.2.893-900.1973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Hoffmann ME, Jang J, Moreno SN, Docampo R. Inhibition of protein synthesis and amino acid transport by crystal violet in Trypanosoma cruzi. J Eukaryot Microbiol. 1995;42:293–297. doi: 10.1111/j.1550-7408.1995.tb01583.x. [DOI] [PubMed] [Google Scholar]
- 30.Fry BA. Basic triphenylmethane dyes and the inhibition of glutamine synthesis by Staphylococcus aureus. Journal of general microbiology. 1957;16:341–349. doi: 10.1099/00221287-16-2-341. [DOI] [PubMed] [Google Scholar]
- 31.Moreno SN, Gadelha FR, Docampo R. Crystal violet as an uncoupler of oxidative phosphorylation in rat liver mitochondria. Journal of Biological Chemistry. 1988;263:12493–12499. [PubMed] [Google Scholar]
- 32.Park JT. Uridinediphosphate derivatives in Staphylococcus aureus treated with crystal violet or various antibiotics. Federation Proc. 1954;13:271. [Google Scholar]
- 33.Zhang X, Zheng Y, Fried LE, et al. Disruption of the mitochondrial thioredoxin system as a cell death mechanism of cationic triphenylmethanes. Free Radic Biol Med. 2011;50:811–820. doi: 10.1016/j.freeradbiomed.2010.12.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Brockow K, Grabenhorst P, Abeck D, et al. Effect of gentian violet, corticosteroid and tar preparations in Staphylococcus aureus colonized atopic eczema. Dermatology. 1999;199:231–236. doi: 10.1159/000018253. [DOI] [PubMed] [Google Scholar]
- 35.Stoff B, MacKelfresh J, Fried L, Cohen C, Arbiser JL. A nonsteroidal alternative to impetiginized eczema in the emergency room. J Am Acad Dermatol. 2010;63:537–539. doi: 10.1016/j.jaad.2009.05.027. [DOI] [PubMed] [Google Scholar]
- 36.Huang JT, Abrams M, Tlougan B, Rademaker A, Paller AS. Treatment of Staphylococcus aureus colonization in atopic dermatitis decreases disease severity. Pediatrics. 2009;123:e808–e814. doi: 10.1542/peds.2008-2217. [DOI] [PubMed] [Google Scholar]
- 37.Zupan J, Garner P, Omari A. Topical umbilical cord care at birth. Cochrane Database Syst Rev. 2004;3(3):15. doi: 10.1002/14651858.CD001057.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Wald ER, Snyder MJ, Gutberlet RL. Group B beta-hemolytic streptococcal colonization. Acquisition, persistence, and effect of umbilical cord treatment with triple dye. Am J Dis Child. 1977;131:178–180. doi: 10.1001/archpedi.1977.02120150060011. [DOI] [PubMed] [Google Scholar]
- 39.Berrios RL, Arbiser JL. Effectiveness of gentian violet and similar products commonly used to treat pyodermas. Dermatol Clin. 2011;29:69–73. doi: 10.1016/j.det.2010.08.009. [DOI] [PubMed] [Google Scholar]
- 40.Taguchi S, Saji M, Sakisaka M, et al. Studies of selective bactericidal effects of various dye preparations on MRSA. Chemotherapy. 1993;41:935–940. [Google Scholar]
- 41.Toba K, Sudoh N, Nagano K, et al. Randomized prospective trial of gentian violet with dibutyryl cAMP and povidone-iodine with sugar as treatment for pressure sores infected with methicillin-resistant Staphylococcus aureus in elderly patients. Nippon Ronen Igakkai Zasshi. 1997;34:577–582. doi: 10.3143/geriatrics.34.577. [DOI] [PubMed] [Google Scholar]
- 42.Saji M. Effect of gentiana violet against methicillin-resistant Staphylococcus aureus (MRSA) Kansenshōgaku zasshi:The Journal of the Japanese Association for Infectious Diseases. 1992;66:914. doi: 10.11150/kansenshogakuzasshi1970.66.914. [DOI] [PubMed] [Google Scholar]
- 43.Saji M, Taguchi S, Hayama N, Ohzono E, Kobayashi Y, Uchiyama K, Kanekawa T, Ohkuni H. Effect of gentian violet on the elimination of methicillin-resistant Staphylococcus aureus (MRSA) existing in the decubitus region. Nihon Ronen Igakkai Zasshi. 1993;30:795–801. doi: 10.3143/geriatrics.30.795. [DOI] [PubMed] [Google Scholar]
- 44.Okano, Masaki, et al. Topical gentian violet for cutaneous infection and nasal carriage with MRSA. International journal of dermatology. 2000;39:942–944. doi: 10.1046/j.1365-4362.2000.00128.x. [DOI] [PubMed] [Google Scholar]
- 45.Kayama C, Goto Y, Shimoya S, et al. Effects of gentian violet on refractory discharging ears infected with methicillin-resistant Staphylococcus aureus. J Otolaryngol. 2006;35:384–386. doi: 10.2310/7070.2006.0076. [DOI] [PubMed] [Google Scholar]
- 46.Kato T, Takagi H, Matsuno Y, Imaizumi M, Umemoto T. High-pressure irrigation and gentian-violet application for mediastinitis following replacement of ascending aorta and aortic valve. Heart Vessels. 2006;21:392–394. doi: 10.1007/s00380-006-0921-5. [DOI] [PubMed] [Google Scholar]
- 47.Igari K, Jibiki M, Kudo T, Sugano N, Inoue Y. Drainage surgery followed by postoperative irrigation with gentian violet for prosthetic graft infection caused by methicillin-resistant Staphylococcus aureus. Eur J Vasc Endovasc Surg. 2011;41:278–280. doi: 10.1016/j.ejvs.2010.10.010. [DOI] [PubMed] [Google Scholar]
- 48.Fung DYC, Miller RD. Effect of dyes on bacterial growth. Appl Microbiol. 1973;25:793–799. doi: 10.1128/am.25.5.793-799.1973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Wang EW, Agostini G, Olomu O, Runco D, Jung JY, Chole RA. Gentian violet and ferric ammonium citrate disrupt Pseudomonas aeruginosa biofilms. Laryngoscope. 2008;118:2050–2056. doi: 10.1097/MLG.0b013e3181826e24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Stewart PS, Costerton JW. Antibiotic resistance of bacteria in biofilms. Lancet. 2001;358:135–138. doi: 10.1016/s0140-6736(01)05321-1. [DOI] [PubMed] [Google Scholar]
- 51.Hachem R, Reitzel R, Borne A, et al. Novel antiseptic urinary catheters for prevention of urinary tract infections: correlation of in vivo and in vitro test results. Antimicrob Agents Chemother. 2009;53:5145–5149. doi: 10.1128/AAC.00718-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Chaiban G, Hanna H, Dvorak T, Raad I. A rapid method of impregnating endotracheal tubes and urinary catheters with gendine: a novel antiseptic agent. J Antimicrob Chemother. 2005;55:51–56. doi: 10.1093/jac/dkh499. [DOI] [PubMed] [Google Scholar]
- 53.Bhatnagar V, Sundaram KR. Studies on antibacterial properties of gentian violet impregnated silastic. Indian J Med Res. 1993;97:206–208. [PubMed] [Google Scholar]
- 54.Camacho DP, Gasparetto A, Svidzinski TI. The effect of chlorhexidine and gentian violet on the adherence of Candida spp. to urinary catheters. Mycopathologia. 2007;163:261–266. doi: 10.1007/s11046-007-9007-x. [DOI] [PubMed] [Google Scholar]
- 55.Karchmer TB, Giannetta ET, Muto CA, Strain BA, Farr BM. A randomized crossover study of silver-coated urinary catheters in hospitalized patients. Arch. Intern. Med. 2000;160:3294–3298. doi: 10.1001/archinte.160.21.3294. [DOI] [PubMed] [Google Scholar]
- 56.Heller MM, Fullerton-Stone H, Murase JE. Caring for new mothers: diagnosis, management and treatment of nipple dermatitis in breastfeeding mothers. Int J Dermatol. 2012;51:1149–1161. doi: 10.1111/j.1365-4632.2011.05445.x. [DOI] [PubMed] [Google Scholar]
- 57.Wilson-Clay B. More on thrush and the use of gentian violet. J Hum Lact. 1991;7:58. doi: 10.1177/089033449100700209. [DOI] [PubMed] [Google Scholar]
- 58.Nyst MJ, Perriens JH, Kimputu L, Lumbila M, Nelson AM, Piot P. Gentian violet, ketoconazole and nystatin in oropharyngeal and esophageal candidiasis in Zairian AIDS patients. Ann Soc Belg Med Trop. 1992;72:45–52. [PubMed] [Google Scholar]
- 59.Wright SC, Maree JE, Sibanyoni M. Treatment of oral thrush in HIV/AIDS patients with lemon juice and lemon grass (Cymbopogon citratus) and gentian violet. Phytomedicine. 2009;16:118–124. doi: 10.1016/j.phymed.2008.07.015. [DOI] [PubMed] [Google Scholar]
- 60.Pienaar ED, Young T, Holmes H. Interventions for the prevention and management of oropharyngeal candidiasis associated with HIV infection in adults and children. Cochrane Database Syst Rev. 2010;10:CD003940. doi: 10.1002/14651858.CD003940.pub2. [DOI] [PubMed] [Google Scholar]
- 61.Mulu A, Kassu A, Anagaw B, et al. Frequent detection of 'azole' resistant Candida species among late presenting AIDS patients in northwest Ethiopia. BMC Infect Dis. 2013;12:82. doi: 10.1186/1471-2334-13-82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Traboulsi RS, Mukherjee PK, Ghannoum MA. In vitro activity of inexpensive topical alternatives against Candida spp. isolated from the oral cavity of HIV-infected patients. Int J Antimicrob Agents. 2008;31:272–276. doi: 10.1016/j.ijantimicag.2007.11.008. [DOI] [PubMed] [Google Scholar]
- 63.Kondo S, Tabe Y, Yamada T, Misawa S, Oguri T, Ohsaka A, Miida T. Comparison of antifungal activities of gentian violet and povidone-iodine against clinical isolates of Candida species and other yeasts: a framework to establish topical disinfectant activities. Mycopathologia. 2012;173:21–25. doi: 10.1007/s11046-011-9458-y. [DOI] [PubMed] [Google Scholar]
- 64.Traboulsi RS, Mukherjee PK, Chandra J, Salata RA, Jurevic R, Ghannoum MA. Gentian violet exhibits activity against biofilms formed by oral Candida isolates obtained from HIV-infected patients. Antimicrob Agents Chemother. 2011;55:3043–3045. doi: 10.1128/AAC.01601-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Slotkowski EL, Redondo D. Mucosal irritation following the use of gentian violet. Am J Dis Child. 1966;112:40–42. doi: 10.1001/archpedi.1966.02090100076007. [DOI] [PubMed] [Google Scholar]
- 66.Verbov J. Oral irritation with gentian violet. Br Med J. 1976;11:639. doi: 10.1136/bmj.2.6036.639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.John RW. Necrosis of oral mucosa after local application of crystal violet. Br Med J. 1968;1:157–158. doi: 10.1136/bmj.1.5585.157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Utter AR. Gentian violet treatment for thrush: can its use cause breastfeeding problems? J Hum Lact. 1990;6:178–180. doi: 10.1177/089033449000600417. [DOI] [PubMed] [Google Scholar]
- 69.Baca D, Drexler C, Cullen E. Obstructive Laryngotracheitis Secondary to Gentian Violet Exposure. Clin Pediatr. 2001;40:233–235. doi: 10.1177/000992280104000411. [DOI] [PubMed] [Google Scholar]
- 70.Spence-Shishido A, Carr C, Bonner MY, Arbiser JL. In Vivo Gram Staining of Tinea Versicolor. JAMA Dermatol. 2013 May;15:1–2. doi: 10.1001/jamadermatol.2013.2699. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Nussenzweig V, Sonntag R, Biancalana A, et al. Effect of triphenylmethane dyes on Trypanosoma cruzi in vitro; use of gentian violet in prevention of transmission of Chagas disease by blood transfusion. Hospital (Rio J) 1953;44:731–744. [PubMed] [Google Scholar]
- 72.Ramirez LE, Lages-Silva E, Pianetti GM, Rabelo RM, Bordin JO, Moraes-Souza H. Prevention of transfusion-associated Chagas' disease by sterilization of Trypanosoma cruzi-infected blood with gentian violet, ascorbic acid, and light. Transfusion. 1995;35:226–230. doi: 10.1046/j.1537-2995.1995.35395184279.x. [DOI] [PubMed] [Google Scholar]
- 73.Docampo R, Moreno SN, Gadelha FR, de Souza W, Cruz FS. Prevention of Chagas' disease resulting from blood transfusion by treatment of blood: toxicity and mode of action of gentian violet. Biomed Environ Sci. 1988;1:406–413. [PubMed] [Google Scholar]
- 74.Docampo R, Moreno SN, Muniz RP, Cruz FS, Mason RP. Light-enhanced free radical formation and trypanocidal action of gentian violet (crystal violet) Science. 1983;220:1292–1295. doi: 10.1126/science.6304876. [DOI] [PubMed] [Google Scholar]
- 75.Wendel, Silvano Transfusion transmitted Chagas disease: Is it really under control? Acta Tropica. 2010;115:28–34. doi: 10.1016/j.actatropica.2009.12.006. [DOI] [PubMed] [Google Scholar]
- 76.de Souza Pietra RCC, Rodrigues LF, Teixeira E, et al. Triphenylmethane Derivatives Have High In Vitro and In Vivo Activity against the Main Causative Agents of Cutaneous Leishmaniasis. PloS one. 2013;8:e51864. doi: 10.1371/journal.pone.0051864. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Kyle LH, McKay DG, Sparling HJ. Strongyloidiasis. Ann Intern Med. 1948;29:1014–1042. doi: 10.7326/0003-4819-29-6-1014. [DOI] [PubMed] [Google Scholar]
- 78.Browne DC, Contacos PG, Welch GE, McHardy G. Treatment of Strongyloides stercoralis infection with intravenous gentian violet. The American Journal of Tropical Medicine and Hygiene. 1957;6:1066–1067. doi: 10.4269/ajtmh.1957.6.1066. [DOI] [PubMed] [Google Scholar]
- 79.Jung RC, Beaver PC. Treatment of enterobiasis (pinworm infestation) with diphenan, egression and gentian violet. Pediatrics. 1953;11:611–616. [PubMed] [Google Scholar]
- 80.Askue WE. A comparison of egressin and gentian violet in the treatment of enterobiasis (pinworm infestation) J Pediatr. 1953;42:332–338. doi: 10.1016/s0022-3476(53)80189-7. [DOI] [PubMed] [Google Scholar]
- 81.Bhandarkar SS, MacKelfresh J, Fried L, Arbiser JL. Targeted therapy of oral hairy leukoplakia with gentian violet. J Am Acad Dermatol. 2008;58:711–712. doi: 10.1016/j.jaad.2007.11.017. [DOI] [PubMed] [Google Scholar]
- 82.Aljofan M, Sganga ML, Lo MK, et al. Antiviral activity of gliotoxin, gentian violet and brilliant green against Nipah and Hendra virus in vitro. Virol J. 2009;4:187. doi: 10.1186/1743-422X-6-187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Fried LE, Arbiser JL. Application of angiogenesis to clinical dermatology. Adv Dermatol. 2008;24:89–103. doi: 10.1016/j.yadr.2008.09.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Hashizume H, Falcón BL, Kuroda T, et al. Complementary actions of inhibitors of angiopoietin-2 and VEGF on tumor angiogenesis and growth. Cancer Res. 2010;70:2213–2223. doi: 10.1158/0008-5472.CAN-09-1977. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Fiedler U, Augustin HG. Angiopoietins: a link between angiogenesis and inflammation. Trends Immunol. 2006;27:552e8. doi: 10.1016/j.it.2006.10.004. [DOI] [PubMed] [Google Scholar]
- 86.Cao Y, Arbiser J, D'Amato RJ, et al. Forty-year journey of angiogenesis translational research. Sci Transl Med. 2011;3:114rv3. doi: 10.1126/scitranslmed.3003149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Cao Y. Antiangiogenic cancer therapy: why do mouse and human patients respond in a different way to the same drug? Int J Dev Biol. 2011;55:557–562. doi: 10.1387/ijdb.103236yc. [DOI] [PubMed] [Google Scholar]
- 88.Cao Y, Langer R. Optimizing the delivery of cancer drugs that block angiogenesis. Sci Transl Med. 2010;2(15):15ps3. doi: 10.1126/scitranslmed.3000399. [DOI] [PubMed] [Google Scholar]
- 89.Huang Y, Goel S, Duda DG, Fukumura D, Jain RK. Vascular normalization as an emerging strategy to enhance cancer immunotherapy. Cancer Res. 2013;73:2943–2948. doi: 10.1158/0008-5472.CAN-12-4354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Cao Y. Angiogenesis: What can it offer for future medicine? Exp Cell Res. 2010;316:1304–1308. doi: 10.1016/j.yexcr.2010.02.031. [DOI] [PubMed] [Google Scholar]
- 91.Hiramoto K, Kobayashi H, Yamate Y, Ishii M, Sato EF. Intercellular pathway through hyaluronic acid in UVB-induced inflammation. Exp Dermatol. 2012;21:911–914. doi: 10.1111/exd.12032. [DOI] [PubMed] [Google Scholar]
- 92.Arbiser JL, Petros J, Klafter R, Govindajaran B, McLaughlin ER, Brown LF, et al. Reactive oxygen generated by Nox1 triggers the angiogenic switch. Proc Natl Acad Sci USA. 2002;99:715–720. doi: 10.1073/pnas.022630199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Lapidoth M, Ben-Amitai D, Bhandarkar S, et al. Efficacy of topical application of eosin for ulcerated hemangiomas. J Am Acad Dermatol. 2009;60:350e1. doi: 10.1016/j.jaad.2008.10.034. [DOI] [PubMed] [Google Scholar]
- 94.Kamba T, Tam BY, Hashizume H, et al. VEGF-dependent plasticity of fenestrated capillaries in the normal adult microvasculature. Am J Physiol Heart Circ Physiol. 2006;290:H560–H576. doi: 10.1152/ajpheart.00133.2005. [DOI] [PubMed] [Google Scholar]
- 95.Jia W, Sun V, Tran N, et al. Longterm blood vessel removal with combined laser and topical rapamycin antiangio genic therapy: implicationsfor effective port wine stain treatment. Lasers Surg Med. 2010;42:105–112. doi: 10.1002/lsm.20890. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Tan W, Jia W, et al. Topical rapamycin suppresses the angiogenesis pathways induced by pulsed dye laser: molecular mechanisms of inhibition of regeneration and revascularization of photocoagulated cutaneous blood vessels. Lasers Surg Med. 2012;44:796–804. doi: 10.1002/lsm.22101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Munson JM, Fried L, Rowson SA, et al. Anti-invasive adjuvant therapy with imipramine blue enhances chemotherapeutic efficacy against glioma. Sci Transl Med. 2012;4:127ra36. doi: 10.1126/scitranslmed.3003016. [DOI] [PubMed] [Google Scholar]
- 98.Munson J, Bonner M, Fried L, Hofmekler J, Arbiser J, Bellamkonda R. Finding new small molecule anti-invasive compounds for glioma treatment. Cell Cycle. 2013 Jun 21;12(14) doi: 10.4161/cc.25334. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Bonner MY, Arbiser JL. Targeting NADPH oxidases for the treatment of cancer and inflammation. Cell Mol Life Sci. 2012;69:2435–2442. doi: 10.1007/s00018-012-1017-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Newick K, Cunniff B, Preston K, et al. Peroxiredoxin 3 is a redox-dependent target of thiostrepton in malignant mesothelioma cells. PLoS One. 2012;7:e39404. doi: 10.1371/journal.pone.0039404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Fruehauf J, Lutzky J, McDermott D, et al. Multicenter, phase II study of axitinib, a selective second-generation inhibitor of vascular endothelial growth factor receptors 1, 2, and 3, in patients with metastatic melanoma. Clin Cancer Res. 2011;117:7462–7469. doi: 10.1158/1078-0432.CCR-11-0534. [DOI] [PubMed] [Google Scholar]
- 102.Perez DG, Suman VJ, Fitch TR, et al. Phase 2 trial of carboplatin, weekly paclitaxel, and biweekly bevacizumab in patients with unresectable stage IV melanoma: a North Central Cancer Treatment Group study, N047A. Cancer. 2009;115:119–127. doi: 10.1002/cncr.23987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Arbiser JL, Bips M, Seidler A, Bonner MY, Kovach C. Combination therapy of imiquimod and gentian violet for cutaneous melanoma metastases. J Am Acad Dermatol. 2012;67:e81–e83. doi: 10.1016/j.jaad.2011.10.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Cao Y, Zhang L, Ritprajak P, Tsushima F, Youngnak-Piboonratanakit P, Kamimura Y, et al. Immunoregulatory molecule B7-H1 (CD274) contributes to skin carcinogenesis. Cancer research. 2011;71:4737–4741. doi: 10.1158/0008-5472.CAN-11-0527. [DOI] [PubMed] [Google Scholar]
- 105.Talebian F, Liu JQ, Liu Z, Khattabi M, He Y, Ganju R, Bai XF. Melanoma cell expression of CD200 inhibits tumor formation and lung metastasis via inhibition of myeloid cell functions. PloS one. 2012;7:e31442. doi: 10.1371/journal.pone.0031442. (2012) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Munn DH, Mellor AL. Indoleamine 2, 3-dioxygenase and tumor-induced tolerance. Journal of Clinical Investigation. 2007;117:1147–1154. doi: 10.1172/JCI31178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.McCarter M, Clarke J, Richter D, Wilson C. Melanoma skews dendritic cells to facilitate a T helper 2 profile. Surgery. 2005;138:321–328. doi: 10.1016/j.surg.2005.06.011. [DOI] [PubMed] [Google Scholar]
- 108.Eiselein MW. Suppression of immune surveillance in melanoma. Medical hypotheses. 2001;56:648–652. doi: 10.1054/mehy.2000.1211. [DOI] [PubMed] [Google Scholar]
- 109.Harris, Rachel, et al. Radiotherapy skin care: A survey of practice in the UK. Radiography. 2012;18:21–27. [Google Scholar]
- 110.Mak SS, Molassiotis A, Wan WM, Lee IY, Chan ES. The effects of hydrocolloid dressing and gentian violet on radiation-induced moist desquamation wound healing. Cancer Nurs. 2000;23:220–229. doi: 10.1097/00002820-200006000-00010. [DOI] [PubMed] [Google Scholar]
- 111.Gollins S, Gaffney C, Slade S, et al. RCT on gentian violet versus a hydrogel dressing for radiotherapy-induced moist skin desquamation. J Wound Care. 2008;17:268–270. 272, 274–265. doi: 10.12968/jowc.2008.17.6.29589. [DOI] [PubMed] [Google Scholar]
- 112.Harris K, Hull PR, Hansen CD, et al. Transgrediens pachyonychia congenita (PC): case series of a nonclassical PC presentation. Br J Dermatol. 2012;166:124–128. doi: 10.1111/j.1365-2133.2011.10537.x. [DOI] [PubMed] [Google Scholar]
- 113.Leiferman, Kristin M, Gerald J, Gleich Hypereosinophilic syndrome: case presentation and update. Journal of allergy and clinical immunology. 2004;113:50–58. doi: 10.1016/j.jaci.2003.10.051. [DOI] [PubMed] [Google Scholar]
- 114.Fukushi S, Ito Y, Kimura Y, Aiba S. The inhibitory effects of gentian violet on STAT6 signaling shed light on its classic yet modern therapeutic use for prurigo nodularis. Journal of Dermatological Science. 2013;69:e33–e33. [Google Scholar]
- 115.Pearse AGE. Histochemistry - Theoretical and Applied. 4th Ed. Volume 2. Churchill-Livingstone, Edinburgh – New York: Analytical Technology; 1985. [Google Scholar]
- 116.Rosenkranz HS, Carr HS. Possible hazard in use of gentian violet. Br Med J. 1971;183(5776):702–703. doi: 10.1136/bmj.3.5776.702-d. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Au W, Pathak S, Collie CJ, Hsu TC. Cytogenetic toxicity of gentian violet and crystal violet on mammalian cells in vitro. Mutat Res. 1978;58:269–276. doi: 10.1016/0165-1218(78)90019-8. [DOI] [PubMed] [Google Scholar]
- 118.Au W, Butler MA, Bloom SE, Matney TS. Further study of the genetic toxicity of gentian violet. Mutat Res. 1979;66:103–112. doi: 10.1016/0165-1218(79)90054-5. [DOI] [PubMed] [Google Scholar]
- 119.Culp SJ, Mellick PW, Trotter RW, Greenlees KJ, Kodell RL, Beland FA. Carcinogenicity of malachite green chloride and leucomalachite green in B6C3F1 mice and F344 rats. Food Chem Toxicol. 2006;44:1204–1212. doi: 10.1016/j.fct.2006.01.016. [DOI] [PubMed] [Google Scholar]
- 120.Littlefield NA, Blackwell BN, Hewitt CC, Gaylor DW. Chronic toxicity and carcinogenicity studies of gentian violet in mice. Fundam Appl Toxicol. 1985;5:902–912. doi: 10.1016/0272-0590(85)90172-1. [DOI] [PubMed] [Google Scholar]
- 121.Littlefield NA, Gaylor DW, Blackwell BN, Allen RR. Chronic toxicity/carcinogenicity studies of gentian violet in Fischer 344 rats: two-generation exposure. Food Chem Toxicol. 1989;27:239–247. doi: 10.1016/0278-6915(89)90162-2. [DOI] [PubMed] [Google Scholar]
- 122.Arbiser JL. Gentian violet is safe. J Am Acad Dermatol. 2009;61:359. doi: 10.1016/j.jaad.2009.03.029. [DOI] [PubMed] [Google Scholar]
- 123.Piatt JP, Bergeson PS. Gentian violet toxicity. Clin Pediatr (Phila) 1992;31:756–757. doi: 10.1177/000992289203101212. [DOI] [PubMed] [Google Scholar]
- 124.Horsfield P, Logan FA, Newey JA. Letter: Oral irritation with gentian violet. Br Med J. 1976;28:529. doi: 10.1136/bmj.2.6034.528-e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Walsh C, Walsh A. Haemorrhagic cystitis due to gentian violet. Br Med J (Clin Res Ed) 1986;293:732. doi: 10.1136/bmj.293.6549.732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Kim SJ, Koh DH, Park JS, Ahn HS, Choi JB, Kim YS. Hemorrhagic cystitis due to intravesical instillation of gentian violet completely recovered with conservative therapy. Yonsei Med J. 2003;44:163–165. doi: 10.3349/ymj.2003.44.1.163. [DOI] [PubMed] [Google Scholar]