Abstract
Background
Valproic acid (VPA) is a commonly prescribed drug for those affected by epilepsy and bipolar disorders. VPA has a well known teratogenic potential, causing a variety of birth defects including neural tube defects (NTDs) and other congenital malformations, when women are treated with this medication during pregnancy. Unfortunately, the mechanism by which VPA is teratogenic remains unknown, although a range of potential mechanisms including histone deacetylase inhibition and folate antagonism have been proposed. The latter is of considerable importance, as clinicians need to know if additional folate supplements can prevent VPA-induced defects.
Methods
We herein approach this question experimentally, using enzyme-linked immunosorbent assay assays and cell culture modeling, to demonstrate that VPA serves as a noncompetitive inhibitor of the high affinity folate receptors.
Results
Binding affinities experimentally determined through enzyme-linked immunosorbent assay assays indicate that VPA serves as a noncompetitive substrate that can lessen the ability of the three primary folate forms to bind to the high affinity folate receptors. Tests in HEK293T cells indicate that the membrane-bound folate receptors of VPA treated cells bind significantly lower amounts of folic acid than do untreated cells.
Conclusion
If these data translate to the overall transport and subsequent bioavailability of folates, noncompetitive inhibition of the folate receptors by VPA may serve to lower the bioavailable folates in VPA treated mothers. This represents a novel mechanism by which in utero VPA exposure could be disrupting developmental processes by noncompetitively binding to the folate receptors during embryogenesis, thus inducing the wide range of defects seen in babies born to VPA treated mothers.
Keywords: valproic acid, folate, vitamin transport, birth defects, teratogens
Introduction
The Centers for Disease Control and Prevention estimates that epilepsy currently affects 2.2 million Americans and 65 million people worldwide, while the National Institutes of Health estimates that bipolar disorder affects approximately 2.6% of the U.S. population, with the average onset of the disorder occurring at age 25, the middle of child-bearing years for women. Valproic acid (VPA) is one of the most commonly prescribed drugs to control epileptic seizures and regulate the mania associated with bipolar disorder. In late 2009, the Food and Drug Administration released a warning indicating that there is an increased risk for major birth defects, including craniofacial, neural, cardiac and cognitive defects, associated with VPA therapies applied during pregnancy. This official governmental warning occurred decades after the scientific literature demonstrated the increased prevalence of neural tube defects (NTDs) among babies born to mothers who were being treated with VPA (DiLiberti et al., 1984; Lammer et al., 1987; Committee on Genetics, 1999). Although these reports vary with regard to the potential mechanism by which VPA therapy increases the risk of having children affected by NTDs, scientists have long hypothesized that there exists a connection between VPA treatment and inadequate folate levels or metabolism (Elmazar and Nau, 1993).
The precise mechanism of action for VPA is still heavily debated in current literature, although evidence exists which suggests that VPA can increase levels of γ-aminobutyric acid in the brain, probably by inhibiting its catabolism (Crudup et al., 2011). It has also been suggested that VPA may directly inhibit voltage-gated sodium channels, or act as a histone deacetylase inhibitor by binding to the catalytic domain of those proteins (Rosenberg, 2007). When VPA is orally administered, the drug is readily absorbed upon entering the intestines, and freely passes into the blood stream (Ibarra et al., 2013). Many studies have indicated that women taking VPA during pregnancy have a 2- to 16-times greater chance of having a child with a congenital malformation (Smith and Whitehall, 2009; Hill et al., 2010; Jentink et al., 2010a). The most common malformations are cardiac and NTDs. No single mechanism of VPA teratogenicity has been established. Various hypotheses have been proposed, including the promotion of folate deficiency, metabolism of VPA by means of β-oxidation leading to coenzyme A sequestration, an increase in corporal oxidative stress levels, and the inhibition of histone deacetylases resulting in anti-angiogenic effects during development (Silva et al., 2008; Hsieh et al., 2012).
It has been well established that folate deficiency increases the risk for bearing children with NTDs, and that the supplementation of women during gestation with folic acid will decrease this risk for NTDs and other select congenital malformations (Smith et al., 2009). There have also been are many reports linking VPA teratogenicity to the possible changes it may cause in folate levels of a treated individual. It has been observed that VPA treatment in females (animal and human) leads to overall lower serum folate levels (Reynolds, 1973; Schwaninger et al. 1999). It has also been protective in animal models when co-administered with VPA, resulting in fewer congenital malformations (Padmanabhan and Shafiullah, 2003; Whitsel, 2002). The protective effects of folic acid in human pregnancies that are exposed to VPA have not been established in the literature, requiring future studies with higher statistical power and exploring a range of folates compounds have been proposed (Jentink et al., 2010b). In this brief report, we explore the hypothesis that VPA may directly interact with the high affinity folate receptors, therefore, explaining the connection between VPA treatment, associated lowered serum folate levels, and some of the teratogenic effects of VPA treatment. The binding affinities for three common folates (folic acid, s-folinic acid, and 5-methyltetrahydrofolate) to the three high affinity folate receptors (folate receptor α [FRα], folate receptor β [FRβ], and bovine folate binding protein [bFBP]) with and without VPA presence are explored herein.
Materials and Methods
To determine the different binding affinities of the folates to the receptors, an enzyme-linked immunosorbent assay (ELISA) assay was performed. The assay technique used in these studies was similar to methodologies previously reported (Cabrera et al., 2008). In short, proteins (either FRα, FRβ, or bFBP) were printed mechanically onto 96-well polystyrene ELISA plates (Immulon, Thermo Fisher Scientific Inc.) in 1.0-μl volumes with a concentration of 25 ng/μl. Plates were incubated at room temperature in the dark for 3 hr. Three washes with Tris buffered saline pH 8.0 and 0.05% Tween-20 were performed in each well to remove any excess protein.
A competitive standard curve was constructed using serial dilutions of known concentrations of folic acid (Sigma, St. Louis, MO), 5-S-formyltetrahydrofolate, [6s]-5-methyltetrahydrofolate (Metafolin; Merck Eprova AG, Schaffhausen, Switzerland), on the one hand, and an invariable concentration of folic acid horse radish peroxidase (FA-HRP) from Vitros Immunodiagnostics, Ortho-Clinical Diagnostics Inc., on the other. Plates were washed and incubated with standard curve reagents for 1 hr. Plates were washed again (Tween-20 followed by Tris buffered saline) and the interaction between the printed FRs, serial dilutions of each folate, and the FA-HRP conjugate was assayed using Super Signal ELISA Femto Maximum Sensitivity Substrate (Thermo Fisher Scientific Inc.). Photographs of the plates were taken using the Quansys Biosciences Q-Views™ Imager and Software. Pixel intensities detected were interpolated to the concentrations of each form of folate and plotted using Microsoft Excel. Medians of the pixel intensities were used. All variation coefficients were below 12%. The concentrations of substrates were then logarithmically transformed and plotted against pixel intensities. The numerical values (IC50) of the half-maximal binding of each receptor were calculated. The linear ranges of binding curves were fit to a linear regression function. The R2 value of these linear ranges were all greater than 0.975 (data not shown). The half-maximal pixel intensity was interpolated into the linear range to calculate the half maximal binding.
HEK293T cells were cultured in folate-free RPMI media (Gibco) with 10% FBS and 1% P/S for 2 weeks to upregulate surface folate receptor levels. Folate receptor alpha levels were confirmed to be upregulated by Western blot (Folate Receptor alpha antibody C17, Santa Cruz Biosci)(data not shown). HEK293T cells were exposed to various levels of VPA for 1 hr to determine a mortality curve and allow for a VPA concentration to be used which would not be fatal to the cells at this exposure level (Fig. 1). Confluent cells were washed three times with phosphate buffered saline, then once again with 0.15 M sodium chloride and 10 mm sodium acetate pH 3.5 (Leamon and Low, 1993). Cells were then incubated for 1 hr in serum-free RPMI with either 100 ng/ml FA and various concentrations of VPA, or only 100 ng/ml FA. After 1 hr, the cells were washed with phosphate buffered saline three times then incubated in folate stripping buffer for 1 min. This buffer was collected and used to quantify the FA bound to the surface receptors by means of the previously described ELISA assay. Cells were collected using RIPA buffer with protease inhibitors (Roche) and samples were normalized to total protein concentration. Pictures of cells before and after treatment were taken to verify that there were no gross morphological changes (data not shown).
FIGURE 1.
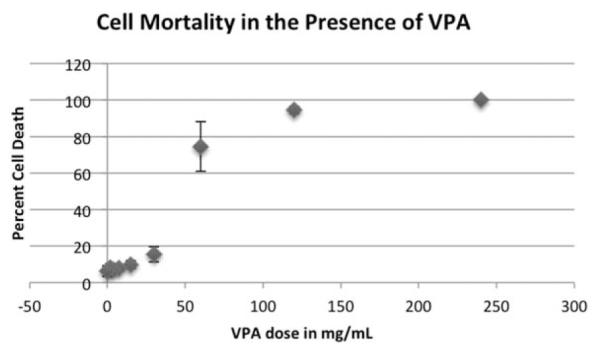
Mortality Rates of HEK 293T Cells with Differing VPA Exposures. HEK293T Cells were incubated in RPMI with different concentrations of VPA and folates. After 1 hr, cells were counted and stained with Trypan Blue to determine cell death. The starting concentration of 30 mg/ml VPA was chosen for the further experiments because this is when the majority of cells remained alive.
Results
EFFECTS OF VPA ON FOLATE BINDING CURVES OF THE HIGH AFFINITY FOLATE RECEPTORS
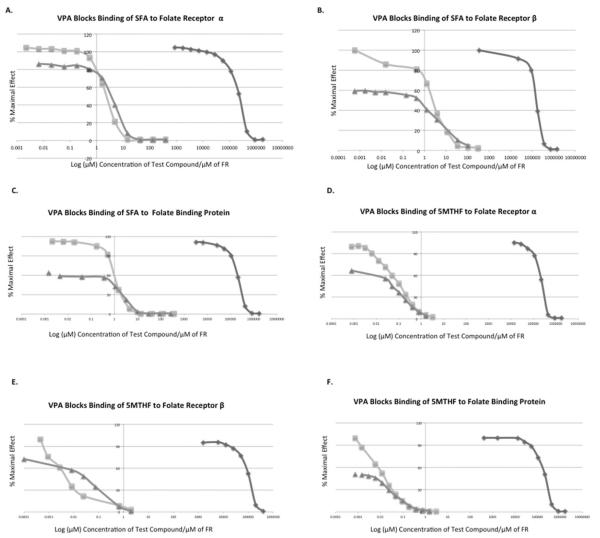
The binding curves shown in Figure 2 are from the output of a competitive binding ELISA between tagged and untagged folates. The HRP-tagged folate is used to quantify the amount of folate present by binding the open receptors when less folate substrate is present. The percent maximal effect represents the intensity of the HRP signal in relation to the maximal signal possible, or when no competing folates are present. The competitive binding ELISAs first performed were to determine the binding affinities of FA, 5-methyltetrahydrofolate, s-folinic acid, and VPA. The binding affinities of each of the folates ranged from 4 to 8 orders of magnitude higher, depending on the folate and the receptor, more so than that of VPA binding to the receptor. The IC50 value of VPA binding to each receptor was calculated: for FRα the IC50 was 40.58 mg/ml, for FRβ the IC50 was 34.74 mg/ml, and for bFBP the IC50 was 38.85 mg/ml. These values were then used for the assay presented in Figure 2, where VPA was constantly present at its appropriate IC50 value and the amount of folate was varied. Figure 2 demonstrates that the addition of VPA at the IC50 concentration shifts the binding curve for the test compound to a lower affinity. The curve where VPA is present never reaches the same maximal binding of folates as seen when VPA is not present. The noncompetitive nature of the antagonist VPA is also illustrated (Fig. 2), as the addition of VPA prevents the receptor from attaining saturation of signal.
FIGURE 2.
Binding of Folates to High Affinity Folate Receptors is Altered by VPA Presence. (A) to (C) illustrate the affinity of SFA (squares), VPA (diamonds), and SFA with VPA together at IC50 concentration (triangles) to the high affinity folate receptors. (D) to (F) illustrate the affinity of 5MTHF (squares), VPA (diamonds), and 5MTHF with VPA together at IC50 concentration (triangles) to the high affinity folate receptors.
EFFECTS OF VPA ON BINDING OF FOLIC ACID TO CELL SURFACE FOLATE RECEPTOR ALPHA
Supernatant collected from folate deprived cells that were exposed during a finite period of time with either folate or folate and VPA, was used to determine the amount of folates that would bind to the cell surface folate receptors. In Figure 3b, the cell surface receptors in HEK293T cells bind significantly less folate when exposed to VPA, as compared to control conditions. The numbers reported represent the results of a competitive binding assay for total folates, so folate concentration is inversely proportional to pixel intensity. A two-tailed t test showed a significance of p < 0.05 for the data sets indicating that the cells treated with VPA had a significantly lower amount of folates binding to their cell surface receptors. In addition, when the amounts of VPA are varied with a standard amount of folic acid, a dose response curve is seen such as that in Figure 3a. As previously described, with an increased amount of VPA, cells bind significantly less folate.
FIGURE 3.
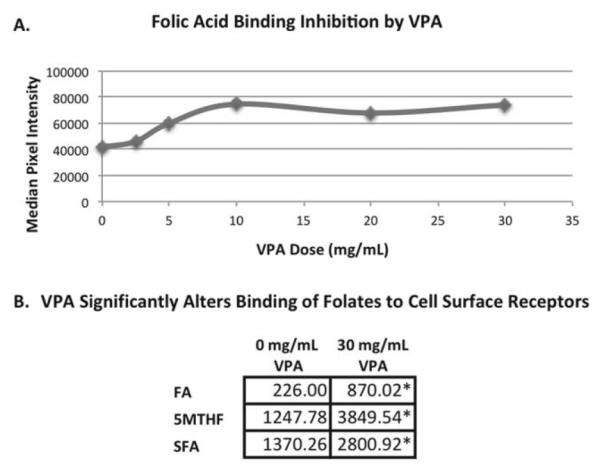
VPA Blocks Folate Binding to Cell Surface Receptors in HEK293T Cells. (A) The results of a competitive binding ELISA assay of a dose response curve relating the amount of folate able to bind to cell surface receptors of folate starved HEK 293T cells with various amounts of VPA present. Pixel intensity has an inverse relationship with the amount of folate present, thus showing that higher doses of VPA allow less folate binding to cell surface receptors. (B) The mean pixel intensity values from a folate assay for cells stripped of folates, then exposed to only folates or folates and VPA. Asterisks represent a significant departure from the cells that were not treated with VPA. A p < 0.05 from a two-tailed t test was considered significant. This is a competitive binding ELISA, therefore, lower pixel intensities directly reflect higher amounts of folates.
Discussion
The displacement curves of folate substrates versus VPA to the high-affinity folate receptors presented in this report demonstrate that VPA serves as an exogenous noncompetitive binding molecule to the high affinity folate receptors. This observation was subsequently validated in a cell culture system with epithelial cells that are known to express high levels of the folate receptor alpha. The mechanism of endocytosis of the high affinity folate receptors suggests that a surface-binding assay can be a reliable measure of the amount of experimental compounds that folate receptors can bind and transport in a cellular environment. It has been noted previously that the folate receptors rapidly deliver their folates after binding and return to the cell membrane free to bind again (Kamen and Smith, 2004; Yang et al., 2007). More recent studies indicate that the endocytosis of FRα occurs at a rather constant rate in each different tissue type and is independent of occupation of the receptor by a ligand (Bandera et al., 2014). This would indicate that folate receptors would be internalized at a standard rate and, therefore, deliver folates only when folates are available to bind to the receptor. Although direct kinetic transport data were not explored here, the binding curves presented are a representation of the possibility of folate transport that occurs when a folate receptor binds its substrate.
The addition of VPA to a closed system of substrate and receptor modified binding such that the maximal binding effect could never be achieved. The data described herein illustrate that VPA, acting alone, has a basal level of binding to the folate receptor, and therefore, serves to bind to either an allosteric site or directly to the folate receptor binding pocket. We suggest that upon oral dosing, VPA could bind to folate receptors as VPA is being absorbed in the epithelial cells of the intestine, a known region of folate receptor expression and function (Sega and Low, 2008). This binding by VPA is hypothesized to produce folate deficient conditions in the pregnant mother, reducing the transfer of folates to the developing embryo, which could potentially contribute to the range of congenital and developmental defects, such as NTDs, seen in embryos developing in a low folate environment. FRα is a developmentally relevant folate receptor and is readily expressed in the placenta (Solanky et al., 2010). Modifications to these high affinity folate receptors may even directly decrease the amount of folates, even folic acid, that are being passed through the placenta to the developing embryo. Folate deficient conditions, such as those that could result from VPA exposure, have been shown to increase the risk for selected congenital defects (Smithells et al., 1980).
This hypothesized folate deficient environment resulting from VPA exposure has been previously described (Alonso-Aperte and Varela-Moreiras, 2000; Whitsel et al., 2002; Padmanabhan and Shafiullah, 2003). Reports showing that concurrent doses of VPA and FA under experimental conditions operate to decrease damage to the developing embryo support the notion that VPA is a noncompetitive inhibitor (Umur et al., 2012). In fact, some physicians recommend the concurrent dosing of women of childbearing age who take VPA to also supplement with FA, in hopes to decrease their risk of having an NTD affected pregnancy (Ornoy, 2009). The Kd determined here for FA is orders of magnitude smaller than that of VPA, such that when the two compounds are administered in parallel, FA will bind more efficiently to the receptors and outcompete any other substrate available. Of interest, VPA is usually given to humans in divided dosages so that the patients maintain a stable concentration in their blood. The average circulating plasma concentration in a patient being treated with VPA is 40 to 100 μg/ml or 280 to 700 μmol/L VPA (Meek et al., 2004). Although the experiments presented here were preformed at superphysiologic concentrations of VPA, over time the effects of the VPA treatment may be seen through the reduction of total possible folates that may bind to their high affinity receptors. After a prolonged exposure to the folate receptors, these constant quantities of VPA may be able to bind to the folate receptors and block the binding and transport of some fraction of the FA provided to the patient in hopes of preventing NTDs and other birth defects. Recently, it has been demonstrated that FRα can function as a transcription factor (Boshnjaku et al., 2012). This report indicates that FRα will translocate into the nucleus and bind to cis-responsive elements on key developmental genes when exposed to folic acid. Although, a basal level of FRα was observed in the nucleus of cells, the addition of folic acid caused additional translocation of FRα to the nucleus (Boshnjaku et al., 2012). If VPA blocks even some of the binding of folic acid to FRα, this could change the signaling cascades started by the transcriptional control exerted by FRα, thereby causing developmental disregulation.
The data presented in this report provide a basis for a novel mechanism of VPA teratogenicity. The decreased levels of folates observed in VPA treated individuals may be a direct result of inhibition of the folate receptors by the small molecule valproic acid. If this inhibition is great enough, congenital malformations and NTDs manifest. Blocking the folate receptors from functioning to their normal capacity would be expected to increase risk for NTDs, as when these receptors are knocked out in mice, NTD phenotypes are observed (Blom et al., 2006). Further investigation will be conducted using folate transport knock-out mouse models. The existence of both the Proton Coupled Folate Receptor knock-out mouse and the Reduced Folate Carrier conditional mouse would allow for tissue specific studies (i.e., upper intestine) of folate transport in vivo by only folate receptor alpha. The study presented here will serve as the starting point of an investigation into the mechanism underlying some of the adverse effects associated with one of the most commonly prescribed drugs for epilepsy, a condition that accounts for 0.5% of all the peoples affected by disease globally.
Acknowledgment
This work was supported in part by NIH grants HD072251 and HD067244.
References
- Alonso-Aperte E, Varela-Moreiras G. Drugs-nutrient interactions: a potential problem during adolescence. Eur J Clin Nutr. 2000;54:S69–S74. [PubMed] [Google Scholar]
- Bandara NA, Hansen MJ, Low PS. Effect of receptor occupancy on folate receptor internalization. Mol Pharm. 2014;11:1007–1013. doi: 10.1021/mp400659t. [DOI] [PubMed] [Google Scholar]
- Blom HJ, Shaw GM, den Heijer M, Finnell RH. Neural tube defects and folate: case far from closed. Nat Rev Neurosci. 2006;7:724–731. doi: 10.1038/nrn1986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boshnjaku V, Shim KW, Tsurubuchi T, et al. Nuclear localization of folate receptor alpha: a new role as a transcription factor. Sci Rep. 2012;2:980. doi: 10.1038/srep00980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cabrera RM, Shaw GM, Ballard JL, et al. Autoantibodies to folate receptor during pregnancy and neural tube defect risk. J Reprod Immunol. 2008;79:85–92. doi: 10.1016/j.jri.2008.08.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Committee on Genetics Folic acid for the prevention of neural tube defects. Pediatrics. 1999;104:325–327. doi: 10.1542/peds.104.2.325. [DOI] [PubMed] [Google Scholar]
- Crudup JB, Hartley BI, Keel BR, et al. Recognizing and treating valproic acid toxicity: a case report. J Med Cases. 2011;5:185–187. [Google Scholar]
- DiLiberti JH, Farndon PA, Dennis NR, Curry CJ. The fetal valproate syndrome. Am J Med Genet. 1984;19:473–481. doi: 10.1002/ajmg.1320190308. [DOI] [PubMed] [Google Scholar]
- Elmazar MM, Nau H. Trimethoprim potentiates valproic acid-induced neural tube defects in mice. Reprod Toxicol. 1993;7:249–254. doi: 10.1016/0890-6238(93)90231-u. [DOI] [PubMed] [Google Scholar]
- Hill DS, Wlodarczyk BJ, Palacios AM, Finnell RH. Teratogenic effects of antiepileptic drugs. Expert Rev Neurother. 2010;10:943–959. doi: 10.1586/ern.10.57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hsieh CL, Wang HE, Tsai WJ, et al. Multiple point action mechanism of valproic acid-teratogenicity alleviated by folic acid, vitamin C, and N-acetylcysteine in chicken embryo model. Toxicology. 2012;291:32–42. doi: 10.1016/j.tox.2011.10.015. [DOI] [PubMed] [Google Scholar]
- Ibarra M, Vazquez M, Faqiolino P, Derendorf H. Sex related differences on valproic acid pharmacokinetics after oral single dose. J Pharmacokinet Pharmacodyn. 2013;40:479–486. doi: 10.1007/s10928-013-9323-3. [DOI] [PubMed] [Google Scholar]
- Jentink J, Loane MA, Dolk H, et al. Valproic acid mono-therapy in pregnancy and major congenital malformations. N Engl J Med. 2010a;362:2185–2193. doi: 10.1056/NEJMoa0907328. [DOI] [PubMed] [Google Scholar]
- Jentink J, Bakker MK, Nijenhuis CM, et al. Does folic acid use decrease the risk for spina bifida after in utero exposure to valproic acid? Pharmacoepidemiol Drug Saf. 2010b;19:803–807. doi: 10.1002/pds.1975. [DOI] [PubMed] [Google Scholar]
- Kamen B, Smith AK. A review of folate receptor alpha cycling and 5-methyltetrahydrofolate accumulation with an emphasis on cell models in vitro. Adv Drug Deliv Rev. 2004;56:1085–1097. doi: 10.1016/j.addr.2004.01.002. [DOI] [PubMed] [Google Scholar]
- Lammer EJ, Sever LE, Oakley GP. Teratogen update: valproic acid. Teratology. 1987;35:465–473. doi: 10.1002/tera.1420350319. [DOI] [PubMed] [Google Scholar]
- Leamon CP, Low PS. Membrane folate-binding proteins are responsible for folate-protein conjugate endocytosis into cultured cells. Biochem J. 1993;291:855–860. doi: 10.1042/bj2910855. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meek MF, Broekroelofs J, Yska JP, et al. Valproic acid intoxication: sense and non-sense of haemodialysis. Neth J Med. 2004;62:333–336. [PubMed] [Google Scholar]
- Ornoy A. Valproic acid in pregnancy: how much are we endangering the embryo and fetus? Reprod Toxicol. 2009;28:1–20. doi: 10.1016/j.reprotox.2009.02.014. [DOI] [PubMed] [Google Scholar]
- Padmanabhan R, Shafiullah MM. Amelioration of sodium valproate-induced neural tube defects in mouse fetuses by maternal folic acid supplementation during gestation. Congenit Anom (Kyoto) 2003;43:29–40. doi: 10.1111/j.1741-4520.2003.tb01024.x. [DOI] [PubMed] [Google Scholar]
- Reynolds EH. Anticonvulsants, folic acid, and epilepsy. Lancet. 1973;1:1376–1378. doi: 10.1016/s0140-6736(73)91690-5. [DOI] [PubMed] [Google Scholar]
- Rosenberg G. The mechanisms of action of valproate in neuropsychiatric disorders: can we see the forest for the trees? Cell Mol Life Sci. 2007;64:2090–2103. doi: 10.1007/s00018-007-7079-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schwaninger M, Ringleb P, Winter R, et al. Elevated plasma concentrations of homocysteine in antiepileptic drug treatment. Epilepsia. 1999;40:345–350. doi: 10.1111/j.1528-1157.1999.tb00716.x. [DOI] [PubMed] [Google Scholar]
- Sega EI, Low PS. Tumor detection using folate receptor-targeted imaging agents. Cancer Metastasis Rev. 2008;27:655–664. doi: 10.1007/s10555-008-9155-6. [DOI] [PubMed] [Google Scholar]
- Silva MF, Aires CC, Luis PB, et al. Valproic acid metabolism and its effects on mitochondrial fatty acid oxidation: a review. J Inherit Metab Dis. 2008;31:205–216. doi: 10.1007/s10545-008-0841-x. [DOI] [PubMed] [Google Scholar]
- Smith J, Whitehall J. Sodium valproate and the fetus: a case study and review of the literature. J Neonatal Nursing. 2009;28:363–367. doi: 10.1891/0730-0832.28.6.363. [DOI] [PubMed] [Google Scholar]
- Smithells RW, Sheppard S, Schorach CJ, et al. Possible prevention of neural-tube defects by periconceptional vitamin supplementation. Lancet. 1980;315:339–340. doi: 10.1016/s0140-6736(80)90886-7. [DOI] [PubMed] [Google Scholar]
- Solanky N, Requena Jimenez A, D’Souza SW, et al. Expression of folate transporters in human placenta and implications for homocysteine metabolism. Placenta. 2010;31:134–143. doi: 10.1016/j.placenta.2009.11.017. [DOI] [PubMed] [Google Scholar]
- Umur AS, Selcuki M, Bursali A, et al. Simultaneous folate intake may prevent adverse effect of valproic acid on neurulating nervous system. Childs Nerv Syst. 2012;28:729–737. doi: 10.1007/s00381-011-1673-9. [DOI] [PubMed] [Google Scholar]
- Whitsel A, Johnson CB, Forehand CJ. An in ovo chicken model to study the systemic and localized teratogenic effects of valproic acid. Teratology. 2002;66:153–63. doi: 10.1002/tera.10093. [DOI] [PubMed] [Google Scholar]
- Yang J, Chen H, Vlahov IR, et al. Characterization of the pH of folate receptor-containing endosomes and the rate of hydrolysis of internalized acid-labile folate-drug conjugates. J Pharmacol Exp Ther. 2007;321:462–468. doi: 10.1124/jpet.106.117648. [DOI] [PubMed] [Google Scholar]