Abstract
Background
HIV research in Vietnam has focused primarily on its large heroin injector population. Data on men who have sex with men [MSM], particularly the large and growing population of men who exchange sex for money or other material rewards, male sex workers [MSWs], is very limited.
Methods
Data derive from a cross-sectional study of MSW, age 16-35, recruited using community sampling methods in three cities in 2010-2011, including Hanoi, Ho Chi Minh City [HCMC], and Nha Trang City (n=710). Assessments included demographic characteristics, substance use, sexual risk, and use of health services. A series of “event” questions were used to assess the influence of alcohol and drugs on sexual risk.
Results
Both tobacco and alcohol are initiated at a young age and most participants currently use both substances overall across all three cities. While alcohol and tobacco use precede the initiation of sex work, stimulant and opiate use are initiated following the initiation of sex work. There was substantial overlap between substance use and sexual risk, and this overlap was strongest in sexual events involving male and female elective partners rather than sex work clients.
Conclusion
Although rates of HIV infection in this group are low, this may be an artifact of the young age of the sample. High rates of drug use, including alcohol, tobacco and illicit drugs, coupled with high rates of ulcerative STIs such as HPV, suggest the potential for rapid amplification of STI/HIV risk among MSW and their complex sex partnering networks.
Keywords: Male Sex Work, Vietnam, Onset of Drug, Sexual Risk
Introduction
Vietnam reported its first case of HIV infection in 1990. HIV has spread rapidly since that time, with nearly 200,000 individuals currently living with HIV infection and 14,000 new infections each year (Ministry of Health, 2011). The early HIV epidemic was primarily associated with the post-war shift from opium smoking to high risk heroin injection practices among injection drug users (IDUs). Although injection risk continues to contribute new infections, sexually-mediated transmission accounts for an increasing number of new infections in recent years, particularly among women (Go et al., 2011, Quan et al., 2010, Thanh et al., 2009, Clatts et al., 2007).
More recently, Vietnam has seen a rapid transformation of its local drug markets and this is further reshaping the HIV epidemic in a number of important ways. Once primarily dominated by heroin, a wide variety of synthetic drugs (amphetamine type substances - ATS, Ecstasy, ketamine, etc.) have appeared in local drug markets, and are particularly popular among younger age cohorts. While most of these synthetic substances are not injected, and hence do not confer the same risks for injection-mediated HIV transmission, there is nevertheless substantive concern regarding the potential for these substances to contribute to sexual risk. Indeed, STI/HIV rates have increased sharply concomitant with rapid increases in the availability and use of synthetic drugs, particularly in younger age cohorts (Vu et al., 2012, Clatts et al., 2010).
Largely ignored in the first decade of the HIV epidemic in Vietnam, men who have sex with men (MSM) were added to sentinel HIV surveillance activities in 2007 and rates of infection in this diverse group have sharply increased since that time. For example, surveillance reports show that the prevalence of HIV among MSM in Hanoi is currently estimated to be 19.8% (an increase from 11.0% in 2006; Ministry of Health, 2010, 2011). Similar increases were observed among MSM in Ho Chi Minh City (HCMC), currently estimated at 14.3% (an increase from 6.2% in 2006) and there is general agreement that sharp increases in the use of synthetic drugs (notably ATS) have contributed to sexual transmission among MSM (Vu et al., 2012).
Although there has been increased research attention to HIV risk among MSM in Vietnam in recent years, a general dearth of epidemiological information about particularly vulnerable subgroups within the overall MSM population remains. Research on the large, complex, and apparently growing population of male sex workers (MSWs) in Vietnam is particularly lacking. A number of studies of MSWs elsewhere in S.E. Asia, particularly Thailand (Chemnasiri, et al., 2010; Toledo, et al., 2010; Guadamuz, et al., 2010; Guadamuz, et al., 2011), have shown alarming levels of behavioral risk in this group as well as high rates of STI/HIV. Similarly, previous studies of young IDUs in Vietnam have noted the high rates of both drug and sexual risk among MSWs within the young IDU population (Clatts et al., 2007). However, there has been only one published study of MSW themselves in Vietnam (Mimiaga et al., 2013). Moreover, although several studies of the general MSM population in Vietnam have suggested that alcohol and drug use (particularly ATS) may contribute to sexual risk (Vu et al., 2012), most of the available data is correlational and the actual impact of drug and alcohol use on sexual risk in various subpopulations of MSM remains unclear.
In an effort to enhance our understanding of drug and sexual risk among MSWs in Vietnam, in 2007, a multi-city epidemiological study was undertaken in three cities, including Hanoi, Ho Chi Minh City, and Nha Trang City. Based upon data from this study, this paper describes substance use among MSWs, including prevalence of alcohol and a wide array of illicit substances. Additionally, we provide a preliminary epidemiological trajectory of the onset and initiation of drug and sexual risk. Finally, given MSWs’ substantial partnering complexity, we use sexual event data to examine the role of drugs and alcohol in understanding sexual risk across different types of sexual partners.
Methods
Sample Construction
MSWs were recruited using a combination of locally-tailored “targeted” and “time-by-location” community sampling methods. (Waters and Biernacki, 1989; Clatts et al., 1995). Survey activities began in Hanoi in March 2010, and were subsequently initiated in Ho Chi Minh City in January 2011 and in Nha Trang in July 2011. In each city, data collection was preceded by formative ethnographic research (including observation, mapping, and informal interviews) to identify and map local settings and social groups in which male sex workers were present and could be recruited for research, including bus stations, public parks, tea stalls, internet cafes, massage parlors, drug “copping” sites, and similar types of public or semi-public settings. While no claim to formal representativeness is made, the ethnographic data served as the basis for development of a targeted sampling plan which was oriented to maximizing theoretical variability in the sample, including age, migration status, sexual identification, drug involvement, and settings for client-recruitment.
Selection of subjects was facilitated through the use of a brief, field-based, conversationally-oriented intercept interview which included questions about male sex work but masked screening criteria, thus limiting potential for self-selection among non-male sex workers in the venues. Potentially eligible subjects were referred to a private research office where formal screening, written informed consent, behavioral survey interviews, and biological testing activities were conducted. Although the assessment measure included questions about a broad range of both monetary and non-material rewards in exchange for sex, eligibility was restricted to males between the age of 16 and 35 who self-reported having exchanged sex for some form of material remuneration (including money, drugs, food, clothing, or some other kind of material benefit) within 90 days prior to study recruitment.
Written informed consent procedures included a formal assessment of capacity for consent. Subjects were paid the equivalent of US$10 in local Vietnamese currency (“đồng”) in compensation for their time. All study procedures and instruments were reviewed and approved by institutional review boards in both the US (the University of Puerto Rico) and Vietnam (Hanoi Medical University).
Measures
The survey interview included five general domains: 1) Demographic Characteristics (including age, birth place, education, employment, sexual self-concept, etc.); 2) Alcohol, Tobacco, and Illicit Substance Use (including age at first use, current use, age at first injection, current injection, for a broad range of illicit and/or illegal substances); 3) Sexual History and Current Practices (including age at onset of first sex with different types of partners, current sexual practices and partner characteristics, and practices and partner types at last sexual exchange); 4) Mental Health Indicators (including the Beck Anxiety Inventory to assess anxiety symptoms and the 20-item version of the CES-D to assess symptoms of depression); 5) Knowledge of HIV transmission risk; and 6) Use of health services (including STI/HIV testing in the last year). Following completion of the survey interview, subjects met with a staff physician who conducted pre-test counseling procedures (in accordance with applicable laws and standards for STI/HIV screening in both the US and Vietnam). Specimens were screened for Syphilis, Gonorrhea, Chlamydia, Human Papilloma virus (HPV), Hepatitis-B (HBV), Hepatitis-C (HCV), and HIV-1.
Data Analysis
Descriptive statistics were used to initially describe the prevalence of recent and lifetime use of tobacco, alcohol, and a broad array of illicit substances, including injection. Repeated analysis of variance (ANOVA) tests were used to determine the differences in the age of onset of drug use (alcohol, tobacco, cannabis and opiates and/or stimulants) and to construct a preliminary trajectory of onset of behavioral risks. Finally, using event level data from the last sexual encounter with each partner type [female, elective male, male client], prevalence of substance use before and during the last sexual encounter was described and the associations between substance use and sexual risk, such as UAI [unprotected anal intercourse], were examined using chi-square tests. SPSS (version 20.0) was used for all analyses.
Results
Sample Characteristics
The final sample included a total of 710 men, all but one of whom were born in Vietnam (see Table 1). Mean age is 22 (SD 3.9, median 21, range 16-35). Education levels vary, with 19.7% currently in school. Among those who were not in school at the time of the interview, only a third (38%) had completed a full 12 years of secondary education. More than half (53%) are migrants, defined for the purposes of this analysis as having moved to the city in which they were interviewed within the past five years, had no parents living in the interview city, and were not born and raised in the interview city. Migrants primarily came from rural areas of Vietnam.
Table 1.
Demographic Characteristics of Sample of Male Sex Workers
| Male Sex Workers | ||
|---|---|---|
| (N=710) | % | |
| Age | ||
|
| ||
| < 21 | 282 | 39.7% |
| >= 21 | 428 | 60.3% |
|
| ||
| Highest Grade | ||
|
| ||
| < HS | 401 | 56.5% |
| >= HS | 309 | 43.5% |
|
| ||
| Currently in School | ||
|
| ||
| Yes | 140 | 30.8% |
| No | 314 | 69.2% |
|
| ||
| Income | ||
|
| ||
| < 3.5 million VND | 320 | 45.1% |
| >= 3.5 million VND | 390 | 54.9% |
|
| ||
| Marital Status | ||
|
| ||
| Single/Separated/Divorced | 17 | 2.4% |
| Married/Cohabitated | 693 | 97.6% |
|
| ||
| Birthplace | ||
|
| ||
| Outside 3 Cities | 414 | 58.3% |
| Hanoi | 60 | 8.5% |
| HCM | 125 | 17.6% |
| Nha Trang | 111 | 15.6% |
|
| ||
| Family Lives | ||
|
| ||
| Outside 3 Cities | 385 | 54.2% |
| Hanoi | 65 | 9.2% |
| HCM | 119 | 16.8% |
| Nha Trang | 141 | 19.9% |
|
| ||
| Migration | ||
|
| ||
| Outside 3 Cities | 379 | 53.4% |
| Hanoi | 76 | 10.7% |
| HCM | 145 | 20.4% |
| Nha Trang | 110 | 15.5% |
|
| ||
| No Stable Housing last 30 Days | ||
|
| ||
| Yes | 80 | 11.3% |
| No | 630 | 88.7% |
|
| ||
| How Long Lived at Current Residence | ||
|
| ||
| < 6 Months | 232 | 32.7% |
| 6 Mo – 2 Yrs | 115 | 16.2% |
| 2 Yrs – 5 Yrs | 113 | 15.9% |
| >= 5 Yrs | 65 | 9.2% |
| Since Birth | 185 | 26.1% |
|
| ||
| Sexual Identity | ||
|
| ||
| Man | 441 | 62.2% |
| Woman | 44 | 6.2% |
| Transgender | 44 | 6.2% |
| Other | 56 | 7.9% |
| Not sure | 124 | 17.5% |
|
| ||
| Sexual Preferences | ||
|
| ||
| Exclusively Men | 166 | 23.4% |
| Both Men and Women | 326 | 46.1% |
| Exclusively Women | 216 | 30.5% |
Since male sex work in Vietnam is often seasonal or episodic (i.e., non-continuous), it is difficult to specify duration of exposure to sex work. On average, however, the interval between first sex work and the time of the interview was 2.4 years, indicating that the sample includes young men who are relatively “new” to sex work.
Median monthly income is relatively high by general Vietnam standards, 3,600,000 VND (approximately US $173 at the time of the study), more than half (53%) of which is derived from sex work. Only a minority (23%) describe themselves as exclusively attracted to men and only 37% of those who are exclusively or primarily attracted to men self-identify as “Gay.”
Significant differences in sample characteristics are observed between cities: MSWs in Hanoi are significantly more likely to have completed high school (X2(2)= 27.7, p<.001), to be married (X2(2)= 7.2, p=.03), and to have lived at their current residence for less than six months (X2(2)= 29.2, p<.001). MSWs in Nha Trang are significantly less likely to be homeless than men from either of the other two cities (X2(2)= 19.8, p<.001). Although sexual self-concept and sexual attraction vary across cities, overall the majority of the sample self-identify as heterosexual (62%) and only a minority describe having a primary or exclusive attraction to sex with men (37%).
Lifetime Exposure and Current Use of Alcohol, Tobacco, and Drugs
Lifetime exposure to alcohol is common in the sample, as well as exposure to a wide variety of substances that are illicit and/or illegal in Vietnam (see Table 2). However, rates of current drug use (last 30 days) are substantially lower.
Table 2.
Lifetime and Current (Last 30 Days) Use of Alcohol, Tobacco, and Drugs among MSWs in Vietnam
| Drugs | Lifetime Prevalence % |
Current Prevalence % |
|---|---|---|
| Alcohol | 98.0% | 83.9% |
| Tobacco | 79.7% | 72.7% |
| Cannabis | 28.0% | 10.0% |
| Opiates and/or Simulants | 46.0% | 24.9% |
| Amphetamine/Methamphetamine | 32.7% | 16.9% |
| MDMA | 37.2% | 12.3% |
| Heroin (Non-Injection) | 7.5% | 2.8% |
| Heroin (Injection) | 7.5% | 4.1% |
| Ketamine | 10.3% | 3.0% |
| Opium | 8.0% | 2.0% |
| Cocaine | 1.1% | 0.3% |
| Diazepam | 0.6% | 0.1% |
| Avg Drug Use | 3.1 | 2.1 |
| Avg Current Age | 22.18 | 22.18 |
| N | 710 | 710 |
Almost all (98%) have used alcohol in their lifetime and a similarly high proportion (84%) are current alcohol users. 80% have used tobacco in their lifetime and 73% are current users. Roughly one quarter (28%) have used cannabis in their lifetime and 10% are current users. Almost half (46%) have used one or more types of opiates and/or stimulants in their lifetime (including heroin, opium, ATS, Ecstasy, ketamine, cocaine, and/or Diazepam). 8% had ever injected heroin.
MSWs in Hanoi and Nha Trang are significantly more likely than those in HCMC to be currently using heroin or opium (X2(2)= 10.8, p=.004), although the prevalence was less than 11% in all cities. Men in HCMC (32%) are significantly more likely than those in Nha Trang (8%) or Hanoi (4%) to currently use ATS (X2(2)= 89.2, p<.001). HCMC MSWs are also more likely to have used one or more opiates and/or stimulants within the last 30 days (X2(2)= 31.5, p<.001).
Trajectory of Onset of Behavioral Risks
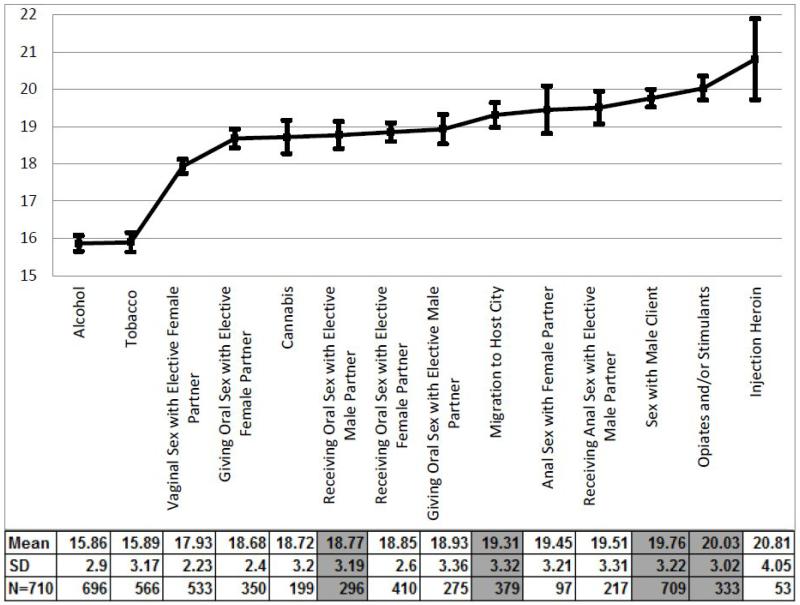
Age of onset for sexual practices and drug use were examined to determine temporal patterns in the acquisition of behavioral risks. As shown in Figure 1, alcohol and tobacco were the first drugs used, on average by the age of 16 (SD 2.90). On average, first penetrative sex with a female partner occurred prior to age 18 (SD 2.23), followed by oral sex (with both male and female partners) prior to age 19 (SD 2.40). Initial use of cannabis also occurred prior to age 19 (SD 3.20). Migration, first heroin and/or cocaine use, and first male sex work, began prior to age 20, followed by initiation of other illicit drugs, including first heroin injection prior to age 21.
Figure 1.
Trajectory of Onset of Behavioral Risk with the Affiliated 95% CI
Using a repeated measures ANOVA, bolded cells show that the average age of first sex with men, migration to the host city, first sex with clients and first use of opiates and/or stimulants statistically differ (p < 0.001).
83.3% (110/132) of the time points show that first sex with men precedes first use of opiates and/or stimulants, 78.2% (147/188) show that migration precedes first use of opiates and/or stimulants and 69.7% (232/333) show that first sex with clients precedes first use of opiates and/or stimulants.
Substance Use and Sexual Risk
We examined alcohol and drug use in recent sexual encounters with different types of sexual partners. Five different sexual events were assessed: vaginal and anal sex with elective female partners, anal sex with elective male partners, and anal sex with both Vietnamese and foreign male sex work clients. Differences in alcohol and drug use are seen between event types, with the highest rates of use found in anal intercourse with elective (non-client) partners (53% for alcohol [X2(4)= 45.7, p=<.001] and 17% for drugs [X2(4)= 22.9, p=<.001]) and vaginal intercourse (46% alcohol [X2(4)= 45.7, p=<.001], 10% drugs [X2(4)= 22.9, p=<.001]) with female partners. These results can be seen in Table 3.
Table 3.
Substance Use and Penetrative Sex at the Last Sexual Encounter by Partner Type
| Elective Female Partner | Elective Male Partner |
Male Client Partner | |||||
|---|---|---|---|---|---|---|---|
| Vaginal Sex (n = 389) |
Anal Sex (n = 58) |
Anal Sex (n = 195) |
Vietnamese (n = 701) |
Foreign (n = 165) |
X2 (df) | p | |
| Participant | |||||||
| Alcohol | 179 (46%) | 31 (53%) | 74 (38%) | 250A (36%) | 30A (18%) | 45.7 (4) | <.001 |
| Before/During Sex* | |||||||
| Drug Before/During Sex* |
38 (10%) | 10 (17%) | 8 (4%) | 40 (6%) | 5 (3%) | 22.9 (4) | <.001 |
| Partner | |||||||
| Alcohol | 94 (24%) | 16 (28%) | 74 (38%) | 261A (37%) | 32A (19%) | 35.7 (4) | <.001 |
| Before/During Sex* | |||||||
| Drug Before/During Sex* | 20 (5%) | 9 (16%) | 6 (3%) | 31 (4%) | 6 (4%) | 16.7 (4) | .002 |
There is a statistically significant difference at the 5% alpha level in the prevalence of substance use between the different types of sexual partners [elective female, elective male and male clients].
There is a significant difference at the 0.5% alpha level in substance use between Vietnamese male clients and foreign male clients.
MSWs that used alcohol at the last penetrative sex are three times more likely to have engaged in receptive unprotected anal intercourse (UAI) with elective male partners (24/53, 45%) than those that did not use alcohol (10/46, 22%) (X2 = 6.1, p = 0.01). Although there was a similar trend of increased risk for UAI for the partner’s use of alcohol use, this did not reach statistical significance (see Table 4).
Table 4.
Substance Use and Receptive UAI at the Last Sexual Encounter by Partner Type
| OR (95% CI) | Elective Male Partner Receptive UAI (n = 195) |
X2 (df) | p | Male Client Partner Receptive UAI |
p** | |
|---|---|---|---|---|---|---|
| Vietnamese (n = 701) |
Foreign (n = 165) |
|||||
| Participant | ||||||
| Alcohol | 3.0* (1.2 – 7.2) | 6.1 (1) | 0.01 | ----- | 0.5 (0.1 – 2.6) | 0.41 |
| Before/During Receptive UAI |
||||||
| Partner | ||||||
| Alcohol | 1.5 (0.7 – 3.6) | 1.0 (1) | 0.32 | ----- | 0.3 (0.1 – 1.7) | 0.20 |
| Before/During Receptive UAI |
||||||
Participants that use alcohol at last penetrative sex are three times more likely to engage in receptive UAI with elective male partners (24/53, 45%) than participants that do not use alcohol (10/46, 22%).
P-value is calculated from the Fisher’s exact test
--- OR undefined because of an observed zero cell count.
Discussion/Conclusion
Data from this study shows high rates of lifetime and current substance use among MSWs in Vietnam. Of particular interest in terms of a young adult population and for planning interventions is the question of trajectories and temporal patterns of risk acquisition. Generally consistent with those of young adults within the larger population in Vietnam, use of alcohol and tobacco are initiated at a relatively young age. Sexual activity often begins with female partners, with onset of oral sex with male partners occurring somewhat later. Migration (when applicable) precedes initiation of anal sex with any partner type. Similarly, both oral and receptive anal sex with male partners typically precedes onset of male sex work, and both precede initiation of the use of opiates and/or stimulant drugs. Notably, while rates of lifetime exposure to a broad range of opiates and/or stimulant drugs were observed among MSW, current use of these substances was significantly lower. Moreover, drug use was only predictive of UAI among elective male partners. We note, however, that low rates of UAI may be an artifact of the young age of the sample and the fact that overall, the group was relatively new to sex work.
With this complexity in mind, the data support a number of observations about the interaction between substance use and sexual risk among MSW in Vietnam. First, as noted above, the sample evidences high rates of tobacco use, typically consumed in the form of a cigarette or sometimes in a traditional pipe. While rates of smoking tobacco among young men in Vietnam is generally high, in this sample smoking is coupled with high rates of oral STIs, particularly high rates of oral gonorrhea (Vu et al., 2013) as well as high rates of Human Papilloma Virus (HPV) infection (Clatts et al., 2014). This is of concern because, particularly when combined with smoking, high rates of HPV infection are generally associated with increased risk of oral, penile, and anal cancer (Phanuphak et al., 2013). This highlights the urgent need to develop models for effectively engaging these groups in early interventions (particularly targeted health services with which to engage and retain MSWs in HPV vaccination programs and related preventative health services).
Second, and consistent with prevailing patterns of consumption among young men in Vietnam, the sample also evidences high rates of alcohol use (98% for lifetime and 84% for current use). A substantial body of literature has documented an association between alcohol use and sexual risk among MSM, much of it following a “cognitive lapse” model in which alcohol is said to contribute to impaired decision- making and/or decreased protective inhibitions (and hence to increased sexual risk-taking) (e.g., Stall et al., 2001). Others have argued that the causal interaction between alcohol and sexual risk is more complex and that in some contexts alcohol (and other types of substances) may be used instrumentally for the purposes of having unrestricted sex and/or in relation to sex with particular types of sexual partners (Clatts et al. 1989; Bolton et al. 1992). The data in this study suggest a similarly complex interaction: alcohol use at last sexual encounter was associated with increased risk for UAI among elective partners but it was not predictive of UAI among client partners.
This is not to say that the potential consequences of high rates of alcohol use in this sample are benign. While alcohol may not confer increased risk for UAI with client partners, it may nevertheless contribute to health risks in more subtle ways. For example, MSWs in this sample evidenced high rates of oral STIs, most notably pharyngeal gonorrhea (24.1%; Vu et al., 2013). High rates of oral STIs in this group are consistent with the general preference among MSWs for oral rather than anal sex in client partner exchanges. Anecdotally, MSWs describe the general practice of retaining ejaculate in their mouth until after the sex act has been completed, rather than swallowing it. However, it is well established in the available clinical literature that alcohol has the effect of reducing saliva and related protective enzymes in the mouth, and generally contributes to increased dryness in the mouth (Riedel et al., 2005). Thus, independent of whatever impact it may have on intention and cognitive decision- making, alcohol use before and during sex may create an environment in the mouth and throat that facilitates transmission of oral STIs. Particularly in the context of a population that has high numbers of sex partners (including partnering groups with high background levels of STIs, this may explain why high rates of oral STIs were observed among MSWs.
Third, and consistent with general trends in the SE Asia region, which show high rates of ATS among multiple types of vulnerable youth populations (Koe et al., 2010; Clatts et al., 2014), this sample evidences high rates of lifetime ATS exposure. A third had used ATS in their lifetime. However, only about half of those who had ever used ATS are current users (17%). Similarly, about a third (37%) had used MDMA in their lifetime, but only 12% are current users. Similar to patterns of lifetime exposure to heroin coupled with low rates of current use, the data indicate that MSWs are at high risk for exposure to a wide variety of substances and that risk for exposure to a given substance increases with age, but that exposure does not inevitably lead to habitual use or dependence (at least as this can be inferred from the large numbers of MSW who have been exposed to these substances but are not currently using them). Given high rates of exposure to drugs among MSWs, additional research is needed to understand what factors confer increased risk for habituated use and chronic dependency, particularly onset of injection risk. However, such research should include substantive attention to the fact that substantial levels of resiliency appear to be present in this group. Understanding factors that confer a protective influence against risk for habituation or dependency may offer critical lessons for policy and significantly inform strategies for both prevention and treatment.
The data indicate that multiple types of risks are temporally clustered within relatively close proximity to each other, with initiation of “hard” drug use (albeit among a minority of subjects) following (rather than preceding) initiation of sex work. This suggests that high rates of lifetime exposure to drugs in this group may be better understood as an adaptation to stressors associated with MSW (including migration, the vagaries of wage labor and exposure to urban environments in which those substances are more readily available), but that an underlying/pre-existing drug dependence is not a significant causal factor in why some young men initiate male sex work (Clatts, et al., 2005). Accordingly, policies that focus on the eradication of sex work on the assumption that doing so will contribute to a decrease in drug use or HIV risk may have very little positive impact, and on the contrary may only serve to further alienate MSWs from critical prevention and treatment services. Alternatively, interventions that enhance the availability of sustainable employment opportunities, particularly among vulnerable migrant populations, may have a greater impact on reducing both drug and sexual risk as well as associated harms.
There are a number of limitations to be considered in interpreting these findings. First, the data are cross-sectional and group average (mean) was used as the basis for analysis of the initiation data. Second, the types of drug and sexual behaviors described here are highly stigmatized in Vietnam and many are subject to significant legal sanction, and this may contribute to self-report biases. Similarly, data are based on self-reported age at first occurrence, with potential errors in recall. This may be particularly problematic in the context of behaviors that occurred in close temporal proximity. Finally, we acknowledge that the data are primarily quantitative. Yet we know that male sex work environments differ substantially, both within Vietnam as well as between Vietnam and neighboring countries in SE Asia. MSW is prevalent throughout this region and may contribute significantly to sustaining the regions’ HIV epidemic. Additional qualitative research in these settings, particularly comparative work, may help to illuminate behavioral risk trajectories and to better identify critical opportunities for targeted interventions for MSWs.
Highlights.
710 male sex workers were recruited from Hanoi, Ho Chi Minh City and Nha Trang using community sampling methods.
Alcohol and tobacco are initiated at a young age.
Most participants use both substances.
Alcohol and tobacco use precede the initiation of sex work.
Hard drug use is initiated following the initiation of sex work.
Acknowledgement
First and foremost, we would like to thank the many young men who participated in the study. This research was supported by Grant DA022170 (Diffusion of HIV-1 among Drug Using Men in SE Asia) from the U.S. National Institute on Drug Abuse, U.S. National Institutes of Health. Data collection was led by our research team at Hanoi Medical University. Additionally, we would like to thank the Hanoi Provincial AIDS Center, Ho Chi Minh City’s Office of Committee for AIDS Prevention and Control, and Khanh Hoa’s Center for Health Education and Communication. Professor Nguyen Tran Hien, M.D., Ph.D., provided valuable guidance and support in planning and implementation of the study.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Bolton R, Vincke J, Mak R, Dennehy E. Alcohol and risky sex: in search of an elusive connection. Med Anthropol. 1992;14:323–63. doi: 10.1080/01459740.1992.9966077. [DOI] [PubMed] [Google Scholar]
- Chemnasiri T, Netwong T, Visarutratana S. Inconsistent condom use among young men who have sex with men, male sex workers, and transgenders in Thailand. AIDS Education and Prevention. 2010;22:100–109. doi: 10.1521/aeap.2010.22.2.100. [DOI] [PubMed] [Google Scholar]
- Clatts MC, Davis WR, Atillasoy A. Hitting a Moving Target: The Use of Ethnographic Methods in the Evaluation of AIDS Outreach Programs for Homeless Youth in NYC. Qualitative Methods in Drug Abuse and HIV Research: NIDA Res. Monograph. 1995;157:117–135. [PubMed] [Google Scholar]
- Clatts MC, Goldsamt LA, Yi H, Gwadz MV. Homelessness and drug abuse among young men who have sex with men in New York city: A preliminary epidemiological trajectory. Journal of Adolescence. 2005;28:201–214. doi: 10.1016/j.adolescence.2005.02.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clatts MC, Giang LM, Goldsamt LA, Cólon-López V. Nonmedical use of promethazine hydrochloride among heroin injectors in Vietnam: unrecognized risks and unintended consequences. Subst Use Misuse. 2010;45:515–527. doi: 10.3109/10826080903452520. [DOI] [PubMed] [Google Scholar]
- Clatts MC, Giang LM, Goldsamt LA, Colon-Lopez V. Accelerated transition to injection among male heroin initiates in Hanoi, Vietnam: Implications for early harm reduction interventions. J. of Community Health. 2011;34:258–67. doi: 10.1007/s10900-011-9400-8. [DOI] [PubMed] [Google Scholar]
- Clatts MC, Giang LM, Goldsamt LA, Yi H. Male sex work and HIV risk among young heroin users in Hanoi, Vietnam. Sexual Health. 2007;4:261–267. doi: 10.1071/sh07018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clatts MC, Giang LM, Goldsamt LA, Yu G, Miller M. Sexual Practices, Partner Concurrency and Prevalence of STIs and HIV Among Male Sex Workers in Three Cities in Vietnam. Sexual Health. doi: 10.1071/SH14101. Submitted in 2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clatts MC, Mutchler KM. AIDS and the dangerous other: Metaphors of sex and deviance in the representation of disease. Med Anthropol. 1989;10:105–14. doi: 10.1080/01459740.1989.9965956. [DOI] [PubMed] [Google Scholar]
- Colby D. HIV Knowledge and Risk Factors Among Men Who Have Sex with Men in Ho Chi Minh City, Vietnam. JAIDS. 2003;32:80–85. doi: 10.1097/00126334-200301010-00012. [DOI] [PubMed] [Google Scholar]
- Colby D, Minh TT, Toan TT. Down on the farm: homosexual behavior, HIV risk and HIV prevalence in rural communities in Khanh Hoa province, Vietnam. Sex Transm Infect. 2008;84:439–443. doi: 10.1136/sti.2008.031294. [DOI] [PubMed] [Google Scholar]
- Giang LM, Clatts MC, Goldsamt LA, Yu G. High Rates of Oral STIs Among Male Sex Workers in Vietnam. Sex Transm Infect. 2014;90:528. doi: 10.1136/sextrans-2013-051423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Go VF, Frangakis C, Van Nam L, Sripaipan T, Bergenstrom A, Li F, Latkin C, Celentano DD, Quan VM. Characteristics of High-Risk HIV-Positive IDUs in Vietnam: Implications for Future Interventions. Substance Use Misuse. 2011;46:381–389. doi: 10.3109/10826084.2010.505147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guadamuz TE, Kunawararak P, Beyrer C, Pumpaisanchai J, Wei C, Celentano DD. HIV prevalence, sexual and behavioral correlates among Shan, Hill tribe, and Thai male sex workers in Northern Thailand. AIDS Care. 2010;22:597–605. doi: 10.1080/09540120903280935. [DOI] [PubMed] [Google Scholar]
- Guadamuz TE, Wimonsate W, Varangrat A, Phanuphak P, Jommaroeng R, Mock PA, Tappero JW, van Griensven F. Correlates of forced sex among populations of men who have sex with men in Thailand. Arch Sex Behav. 2011;40:259–266. doi: 10.1007/s10508-009-9557-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koe S. Asia Internet MSM Sex Survey (AIMSS): Self-reported HIV prevalence, HIV testing history & risk behavior among MSM in 17 countries in Southeast & East Asia: Comparing results from two large scale, multi-language online surveys in 2009 & 2010. 2010 Retrieved 23rd July 2010 from http://www.fridae.asia/tc/newsfeatures/2010/07/23/10164.asia-internet-msm-sex-survey-2010-preliminary-report.
- Mimiaga MJ, Reisner SL, Closson EF, Perry N, Perkovich B, Nguyen T, Trang NNN, Lan HX, Thien DD, Mayer KH, Colby D. Self-perceived HIV risk and the use of risk reduction strategies among men who engage in transactional sex with other men in Ho Chi Minh City, Vietnam. AIDS Care. 2013;25:1039–1044. doi: 10.1080/09540121.2012.748873. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ministry of Health of Vietnam . Vietnam HIV/AIDS Estimates and Projections, 2007-2012. National Institute of Hygiene and Epidemiology and Family Health International; Hanoi, Vietnam: 2010. [Google Scholar]
- Ministry of Health of Vietnam . Results from the HIV/STI Integrated Biological and Behavioral Surveillance (IBBS) in Vietnam IBBS Round II, 2009. National Institute of Hygiene and Epidemiology and Family Health International; Hanoi, Vietnam: 2011. [Google Scholar]
- Ministry of Health of Vietnam . Vietnam AIDS Response Progress Report: HIV/AIDS Estimates and Projection 2012. Hanoi, Viet Nam: 2011. [Google Scholar]
- Phanuphak N, Teeratakulpisarn N, Pankam T, Kerr SJ, Barisri J, Deesua A, Rodmamrung P, Hongchookiat P, Chomchey N, Phanuphak P, Sohn AH. Anal Human Papillomavirus Infection Among Thai Men Who Have Sex With Men With and Without HIV Infection: Prevalence, Incidence, and Persistence. JAIDS. 2013;63:472–479. doi: 10.1097/QAI.0b013e3182918a5a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Quan VM, Minh NL, Ha TV, Ngoc NP, Vu PT, Celentano DD, Mo TT, Go VF. Mortality and HIV transmission among male Vietnamese injection drug users. Addiction. 2011;106:583–589. doi: 10.1111/j.1360-0443.2010.03175.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Riedel F, Goessler UR, Hormann K. Alcohol-Related Diseases of the Mouth and Throat. Digestive Diseases. 2005;23:195–203. doi: 10.1159/000090166. [DOI] [PubMed] [Google Scholar]
- Stall R, Paul JP, Greenwood G, Pollack LM, Bein E, Crosby GM, Mills TC, Binson D, Coates TJ, Catania JA. Alcohol use, drug use and alcohol-related problems among men who have sex with men: the Urban Men’s Health Study. Addiction. 2001;96:1589–601. doi: 10.1046/j.1360-0443.2001.961115896.x. [DOI] [PubMed] [Google Scholar]
- Thanh DC, Hien NT, Tuan NA, Thang BD, Long NT, Fylkesnes K. HIV Risk Behaviors and Determinants Among People Living with HIV/AIDS in Vietnam. AIDS Behavior. 2009;13:1151–1159. doi: 10.1007/s10461-008-9451-8. [DOI] [PubMed] [Google Scholar]
- Toledo CA, Varangrat A, Wimolsate W, et al. Examining HIV infection among male sex workers in Bangkok, Thailand: a comparison of participants recruited at entertainment and street venues. AIDS Education and Prevention. 2010;22:299–311. doi: 10.1521/aeap.2010.22.4.299. [DOI] [PubMed] [Google Scholar]
- Vietnam Administration of HIV/AIDS Control (VAAC) Sentinel Surveillance Survey 2011. 2011 [Google Scholar]
- Vu BN, Mulvey KP, Baldwin S, Nguyen ST. HIV risk among drug-using men who have sex with men, men selling sex, and transgender individuals in Vietnam. Culture Health Sex. 2012;14:167–180. doi: 10.1080/13691058.2011.630756. [DOI] [PubMed] [Google Scholar]
- Vu VD, Giang LM, Nguyen SM, Clatts MC, Goldsamt LA. High Prevalence of Gonorrhoea and HPV Among Male Sex Workers in Three Cities of Vietnam: Challenges in Addressing HIV Epidemic Among MSM Populations. Sex Transm Infect. 2013;89:A1–A428. [Google Scholar]
- Waters JK, Biernacki P. Targeted sampling: Options for the study of hidden populations. Soc Probl. 1989;36:416–430. [Google Scholar]