Abstract
Lymphatic contractile dysfunction is central to a number of pathologies that affect millions of people worldwide. Due to its critical role in the process of inflammation, a dysfunctional lymphatic system also compromises the immune response, further exacerbating a number of inflammation related diseases. Despite the critical physiological functions accomplished by the transport of lymph, a complete understanding of the contractile machinery of the lymphatic system lags far behind that of the blood vasculature. However, there has been a surge of recent research focusing on different mechanisms that underlie both physiological and pathophysiological aspects of lymphatic contractile function. This review summarizes those emerging paradigms that shed some novel insights into the contractile physiology of the lymphatics in normal as well as different disease states. In addition, this review emphasizes the recent progress made in our understanding of various contractile parameters and regulatory elements that contribute to the normal functioning of the lymphatics.
Keywords: Lymphatic Muscle, Lymphatic Valve, Lymph Flow, Lymphatic Contraction, Nitric Oxide, Inflammation
Introduction to lymphatic contractile function
The lymphatic system is critically involved in the movement of fluid from interstitial spaces in tissue parenchyma and accomplishes its normal functions through the controlled movement of lymph [1]. Through its interconnected network of initial lymphatics, collecting lymphatic vessels and lymph nodes, the lymphatic system moves fluid and its other contents (macromolecules, lipids/chylomicra, immune cells) from the interstitium against an uphill pressure gradient and eventually empties them into the great veins [2]. Lymph transport is thus a critical part of processes involved with body fluid regulation, macromolecular homeostasis, lipid absorption, and immune function.
The initial lymphatics, or lymphatic capillaries, are the primary sites of interstitial fluid exchange and the rate of lymph formation is the principal passive force that influences lymph flow in every lymphatic bed. Initial lymphatics are composed of a layer of endothelial cells and completely lack muscle cells. Another important characteristic is that the endothelial cells are physically tethered to the surrounding tissue structure through anchoring filaments [2-5]. Capillary lymphatic endothelial cells (LECs) are linked to each other by discontinuous, buttonlike intercellular junctions that differ from those found in the rest of the lymphatic network. The presence of these junctions likely make lymphatic capillaries highly permeable to interstitial fluid and solutes, allowing the entry of macromolecules such as lipids and even permitting trafficking of immune cells. These oak leaf-shaped LECs have a unique microarchitecture, as overlapping flaps of adjacent cells form primary valve structures [6, 7]. This primary valve system is required to prevent fluid escape from the initial lymphatics back into the interstitial space. These unique structural characteristics, coupled with the changing physical conditions in active tissues, allow lymph to be formed when interstitial pressure is higher than the pressure in the lumen of the initial lymphatic [8-10].
Initial lymphatics converge to form collecting lymphatic vessels, which are similar to blood vessels in having a basement membrane and continuous endothelial junctions. Collecting lymphatics contain anatomically distinct, bicuspid luminal valves spaced at intervals of 1 to several millimeters. These vessels are also covered by one or more muscle layers that control the transport of lymph by contraction and relaxation of the vessel wall, even in the face of adverse pressure gradients. The functional unit of the collecting lymphatic system is called a lymphangion—the segment between two adjacent secondary valves—and these are arranged in series to propel lymph forward [11-14]. Forward lymph movement is determined by a combination of two factors: the active, intrinsic contraction/relaxation cycle of the lymphangion, and passive, external compressive forces. External forces include contractions of skeletal muscles, respiratory movements, variations in central venous pressure, pulsations of nearby arteries and gravitational forces [2, 15], all of which can easily collapse or alter the diameter of the thin-wall, low-pressure collecting vessels. During an active collecting lymphatic pump cycle, the primary valves in the initial lymphatics are thought to be open to permit fluid flow into the lymphatic lumen, while the secondary valves inside the collecting lymphatics remain closed to prevent intraluminal fluid backflow. During external compression, fluid is transported proximally toward the contractile lymphatics and nodes, at which time the primary valves close to prevent escape of fluid back into the interstitium while the secondary valves are open [16].
The intrinsic lymphatic pump acts similar to the heart in its generation of a pressure head to drive flow. The pumping activity of collecting lymphatics can be investigated using analogies to the cardiac pump, with alternating periods of diastolic filling and systolic ejection (see reviews [1, 2, 14, 17]). For the transport of lymph, the intrinsic pump depends on the contractile machinery in its muscle layer present in larger collecting vessels that transport lymph against an adverse pressure gradient [2]. Previous studies from our lab have shown that the lymphatic muscle is uniquely composed of both smooth and striated muscle components and recent studies elucidating their contractile behavior have unequivocally established that this is a new class of muscle that is distinct from smooth and cardiac muscle types [18-21]. Like vascular smooth muscle, the contractile activity of lymphatic muscle exhibits basal, myogenic tone and myogenic responses to pressure changes [18], as well as being modulated by various neuromodulatory, vasoactive and mechanical factors [22-29]. However, unlike most blood vascular smooth muscle, lymphatic muscle exhibits rapid, phasic contractile activity that drives the intrinsic lymphatic pumping in addition to the slower, tonic form of contractions also characteristic of blood vascular muscle. The uniqueness of lymphatic contractile function can be directly attributed to the unique ultrastructure of lymphatic muscle, which contains both striated and smooth muscle components [20]. Our studies have demonstrated that differences in both contractile function and contractile protein composition exist between blood vessels and lymphatics as well as among lymphatics from different body regions [15, 20]. The uniqueness of lymphatic muscle is further highlighted by the presence of L-type or ‘long-lasting’, Ca2+ channels (characteristic of smooth muscle cells) and T-type ‘transient’ Ca2+ channels (implicated as a possible pacemaker component in both cardiac and lymphatic tissues) [30].
The extra-lymphatic forces that passively influence lymph transport differentially affect lymph flow depending on the anatomical location of the lymphatic vessel. Most notably, fluctuations in central venous pressure, respiratory movements and gravitational forces vary across different regions of the body. Gashev et al., have shown that lymphatic vessels effectively adapt their contractile force to the particular hydrodynamic conditions (transmural pressures and intraluminal flows) and local demands placed on them by the tissue fluid dynamics that exist in different regions of the lymphatic system [15, 31]. Thus, peripheral lymphatics, including mesenteric and femoral vessels, which have comparatively high outflow resistance, act as relatively strong pumping vessels; in contrast, cervical lymphatics and thoracic duct, which are closer to the final outflow of the lymphatic tree, exhibit attenuated pumping activities with significantly reduced frequency, contraction amplitude, ejection fraction and fractional pump flow [15, 20, 32]. Thus, it is evident that the lymphatic function is under the constant influence of various hydrodynamic factors as pressure/stretch, active and passive lymph pumps, intrinsic and extrinsic flow/shear stress, modulating its unique contractile machinery to elicit both phasic and tonic contractions that are key to its role both as conduit and pump.
Stretch-mediated regulation of lymphatic contraction
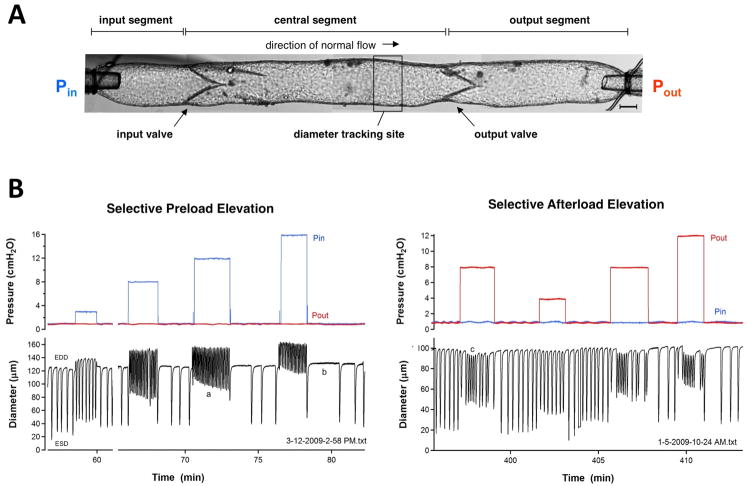
Lymphatic pumping has been shown to be very sensitive to changes in transmural pressure. Stretch-dependent modulation of lymphatic contractility is one of the primary determinants of the adaptation of collecting lymphatics to changes in fluid load [15, 24, 25, 32, 33]. This characteristic also determines the potential capacity of these vessels to adapt to increased loads during edemagenic and/or gravitational stress. Figure 1 shows an isolated rat mesenteric lymphangion and illustrates the original recordings of several fundamental contractile properties of lymphatic muscle. Preload, which is determined by the stretch of the lymphatic wall during the diastolic filling phase of the contractile cycle, is a significant determinant of lymphatic pump function; multiple studies have shown that lymphatic vessels are exquisitely sensitive to different changes in filling pressure and accordingly modulate pump output in a manner similar to the heart [25, 34-37]. As shown in the left panel of Figure 1B, increases in preload result in increased contraction frequency over a relatively wide pressure range (0-15 cmH2O). A change in pressure as little as 0.5 cmH2O can lead to a 2-fold change in contraction frequency [34]. Phasic contraction strength also increases with increasing preload, but beyond a certain point the contractile machinery begins to fail and contraction amplitude falls [1, 2, 25, 38]. This inherent limitation may contribute to contractile dysfunction of collecting vessels observed in chronic lymphedema, where there is a chronic elevation of fluid output pressure and the collecting vessels appear to be near-maximally distended [39, 40].
Figure 1. Original recordings from rat isolated mesenteric lymphangions illustrating several fundamental contractile properties of lymphatic muscle.
A) Nomenclature used throughout to describe the components of an individual lymphangion. Pin and Pout are the pressures set by the input and output cannulating pipettes, respectively. The typical diameter tracking site is just upstream from the output valve. The shadow at the upper left is a servo-nulling micropipette used to puncture the wall and measure pressure in the central segment, which is the lymphangion proper (trace not shown). Calibration bar is 80 μm. B) Examples of the responses of two different rat mesenteric lymphatics to preload elevation at constant afterload (left panel) or afterload elevation at constant preload (right panel). EDD is end diastolic diameter and ESD is end systolic diameter; contraction amplitude is the difference between the two. When preload is elevated by raising input pressure, frequency increases, EDD increases and contraction amplitude is reduced. However, a progressive, secondary recovery in contraction amplitude occurs over the time course of 1-2 minutes (a), due to a decrease in ESD, reflecting an increase in contractility. When Pin is stepped rapidly from a high to low value, a rate-sensitive inhibition of contraction frequency occurs (b); note that the interval between the end of the step and the next contraction increases with the magnitude of the Pin step. When afterload is elevated by selectively raising output pressure (right panel), frequency increases and EDD decreases (c), in part due to a myogenic mechanism (see text).
Lymphatic muscle has been shown to undergo an intrinsic increase in contractility when subjected to an elevated afterload [34]. When output pressure is increased in a step-wise manner, the isolated lymphangion responds with a constriction, i.e., a time-dependent decline in end-diastolic diameter; simultaneously there is an initial increase, then time-dependent decrease in end systolic diameter, reflecting a change in contractility (Figure 1B, right panel). Simultaneous measurement of intraluminal pressure enabled analysis of the pressure-volume (P-V) relationship analogous to that of the heart. Elevated afterload evoked a leftward shift in the end-systolic P-V relationship and a significant increase in dP/dt, consistent with an increase in contractility, or positive inotropy, in the strict sense in which those terms are used in the cardiac literature. This increase in contractility is sustained for several minutes after afterload is returned to its original level [34]. The effect of afterload also depends on the preload. Scallan et al tested the responses of single, isolated lymphangions to selective changes in preload and the effects of changing preload on the response to an imposed afterload [37]. Lymphangions subjected to increased output pressures that exceeded their ejection limit could strengthen contraction as a compensatory mechanism. Depending on its regional location or due to postural changes, a lymphatic vessel might experience a preload change with or without a parallel change in afterload. This is important, as adaptation to an increased preload is necessary for maintaining a sufficient output flow [37].
Von der Weid et al., [41] show a tight correlation between the resting membrane potential (Vm) and stretch-induced increases in contraction frequency. At low levels of isometric tension, action potentials occur more regularly than in un-stretched vessels. The frequency of the action potentials is augmented with increases in preload, as is the force generated during each contraction [41]. The resting Vm values recorded in the wire-myograph-mounted vessels are markedly more depolarized than those recorded in un-stretched vessels still embedded in the mesentery. The authors propose that vasoactive substances released by the lymphatic endothelium contribute to modulation of the contractile activity of the lymphatic muscle, as well as to its resting Vm. This rhythmic contractile activity (i.e. lymphatic pumping) increases in rate with an increase in luminal pressure and relies on activation of voltage-dependent Ca2+ channels (VDCCs). The stretch-induced increase in force of lymphatic vessel contractions is significantly attenuated by both L-type and T-type VDCC blockers. It is proposed that activation of T-type VDCCs depolarizes Vm, regulating the frequency of lymphatic contractions via opening of L-type VDCCs, which allow Ca2+ entry to determine the strength of contractions [30]. This entire mechanism can be modified by external stimuli. In line with the vasodilatory/relaxing actions typically observed in other smooth muscles, nitric oxide (NO) and prostanoids, such as prostaglandin E2 and prostacyclin, cause the lymphatic muscle to hyperpolarize and the pumping frequency to slow [42].
Valve function and lymphatic contraction
Normally the net pressure gradient from the lymphatic capillaries to the venous compartment does not favor the passive flow of lymph centrally. As mentioned previously, the movement of lymph along the lymphatic network relies on forces that are generated both extrinsically and intrinsically to the lymphatic system [2, 14]. The secondary valves play key roles in the action of both forces to: 1) minimize lymph backflow when the pressure gradients are not conducive to central lymph flow; and 2) reduce the gravitational influence on lymph pressure by breaking up the hydrostatic column of lymph. In a standing gravitational column, the valves allow the sequential buildup of intraluminal pressure through successive lymphangions to help overcome opposing pressure gradients, as long as the diastolic pressure in any given lymphangion does not exceed its optimal preload [43]. Dysfunctional or malformed lymphatic valves serve to exacerbate fluid accumulation in interstitium and are closely associated with lymphatic malfunction in certain genetic conditions [44, 45].
A series of recent studies have provided new insights into the contractile and valve properties of collecting lymphatic vessels [34, 37, 46, 47]. Although there is some evidence for the possible role of specialized lymphatic muscle cells in the closure of secondary valves in some (bovine) lymphatics [1, 48], it is thought that most secondary lymphatic valves behave similar to cardiac valves, closing passively when output (downstream) pressure is elevated [49]. Unlike cardiac valves, lymphatic vessel distension profoundly affects the ability of the lymphatic valves to open and close [46]. When a vessel has only a low degree of distention (i.e. operates at a low baseline pressure), the adverse pressure gradient required for valve closure is only a fraction of a cmH2O; however, the pressure gradient required for closing increases ∼20-fold, to a several cmH2O, when the vessel nears maximal distention. This relationship would obviously become an important determinant of valve efficiency in edema states where intraluminal pressures and diastolic diameters are chronically elevated. The anatomical basis of this phenomenon is unknown but is likely related to stiffening of collagen and other ECM fibers in the valve leaflets as the vessel distends [46]. Because of the higher adverse pressure gradient required for closing at a near-maximal vessel diameter, active force generation by lymphatic muscle cells can indirectly affect valve gating. Both intrinsic (myogenic) and agonist-induced tone can thereby make it easier for valves to close when the vessel is pumping against an elevated afterload [46].
In addition to basal tone, collecting lymphatic vessels undergo a relatively powerful constriction when exposed to an adverse pressure gradient. To investigate the response of collecting lymphatics to elevated downstream pressure, Scallan et al. used vessels containing one valve (a partial lymphangion) or two valves (complete lymphangion) that were isolated from the rat mesentery and tied to two glass cannulae capable of independent pressure control. Downstream pressure was selectively raised to various levels, either stepwise or ramp-wise, while holding upstream pressure constant [47]. With increased output pressure, contractile activity of the downstream, post-valve vessel segment increased. Interestingly, the pre-valve segment constricted in response to the increased output pressure even though the output valve prevented backward transmission of pressure (as evident in Figure 1B, right panel). This constriction was composed of two components: a pressure-dependent, myogenic component and a frequency-dependent component [18, 47, 50]. The myogenic component derived from the fact that when output pressure is elevated, mean diastolic pressure in the segment between the valves increased as the vessel continued spontaneous contractions—and that rise in pressure stimulated a slight myogenic constriction. The frequency component derived from the fact that the rise in output pressure stimulated the output segment (downstream from the output valve) to contract at a higher frequency, which paced the entire lymphangion, presumably via electrical transmission through gap junctions across the valve region. Whether this signal traveled via the muscle layer or the endothelium or both was not determined [47, 51]. The higher frequency resulted in less time for filling in diastole (negative lusitropy) and therefore a time-averaged lowering of diastolic diameter. The combination of these two mechanisms resulted in a substantial constriction that preserved the ability of valves to close at relatively low adverse pressure gradients. It is thus evident from these findings that the lymphatic myogenic constriction has significant mechanistic similarity to the arteriolar myogenic constriction. Further, it is clear that the lymphatic constriction in response to elevated afterload protects the lymphatic vasculature from an elevation in pressure both by modulating the contractile strength of the pump and by preserving normal valve gating of individual collecting lymphatics, the absence of which would contribute to edema.
NO-mediated regulatory mechanisms of lymphatic vessel function
The role of NO in modulating lymphatic contractile function and lymph flow has been intensively studied [32, 52-56]. Under normal conditions, there are multiple sources of NO that could influence collecting lymphatic vessel contraction [54, 57-59]: 1) production from eNOS in LECs, due either to shear-stress or pharmacological stimulation; 2) production from iNOS in immune cells or lymphatic muscle cells; 3) production from nNOS in the parenchyma or perivascular lymphatic nerves. In some tissues there is also a possibility of countercurrent exchange of NO from adjacent arteries or veins. The role of iNOS will be discussed in a subsequent section on inflammation. The role of nNOS in regulation of lymphatic contraction is an unexplored topic. The following section will focus on NO production from eNOS in lymphatic endothelium.
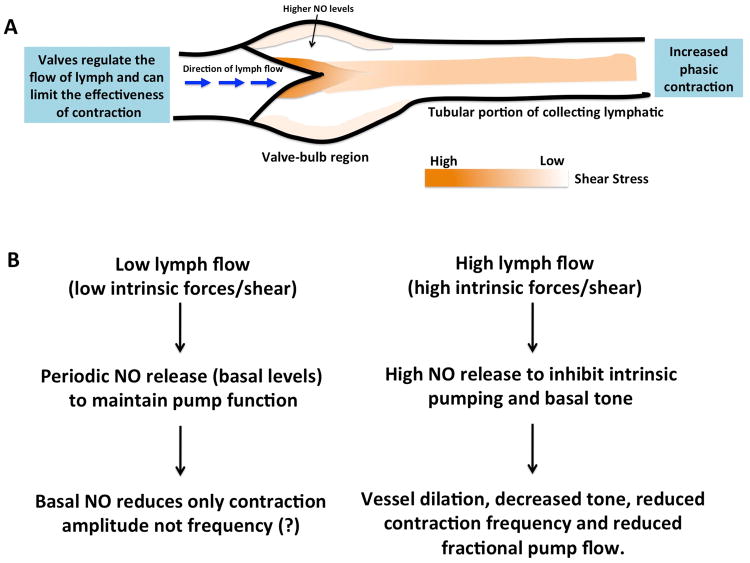
As in the blood vasculature, NO can be produced from eNOS in the lymphatic endothelial cell layer in response to shear stress or flow. Activation of the NO/cyclic GMP (cGMP) pathway causes blood vascular smooth muscle cell relaxation through multiple cGMP-dependent protein kinases (PKG) [60-65]. Gasheva et al., have shown that the cGMP/PKG inhibitor eliminated the intrinsic flow-dependent/NO-dependent relaxation of lymphatic vessel and that its high sensitivity to flow/shear is dependent upon the cGMP/PKG regulatory pathway [66]. As shown schematically in Figure 2A, the intrinsic, spontaneous pumping activity of the collecting lymphatics produces pulsatile changes in both flow and shear stress [67] during the contraction cycle that can potentially generate NO. Bohlen et al find that within 1-3s after the initiation of lymphatic contraction a transient rise in NO levels occurs near the vessel wall [68]. Both the valvular and tubular sections of the lymphatics increase their generation of NO during each phasic contraction (with the concomitant rise in flow/shear stress) and the NO generated is cumulative as contraction frequency increases. Measurements of NO with microelectrodes reveal that the highest concentration of NO occurs in the valve-bulb region with lower concentrations in the tubular portions of rat mesenteric lymphatics [68, 69]. Immunohistochemical analysis confirms a higher expression of eNOS in the bulb compared to tubular regions, possibly due to the increased density of endothelial cells in the leaflets. It is therefore likely that the high-shear force of lymph flowing through the open valve leaflets contributes to elevated NO levels near the valve. The ability of NO to modulate an ongoing contraction is thought to be predominantly a localized event that is coordinated along the lymphatic vessel primarily by the flow of lymph to regionally increase shear forces and any vasoactive NO-dependent mediators in the lymph or tissue [70]. Valves appear to generate most of the NO in the bulb region, which in turn relaxes the contractile components of the bulb; the valves not only govern the physical movement of lymph along the lymphatic vessel but also have a regulatory role in influencing the pumping rate and force of contraction of the overall lymphatic structure through the effects of NO.
Figure 2. Schematic representation of NO mediated regulation of lymphatic contractility.
A. A section of a collecting vessel lymphangion showing increased NO production from the endothelial cells of a lymphatic vessel during phasic contractions and high shear stress. Increased levels of NO are noted near the valve and tubular regions of the lymphatic, with highest concentrations in the valve bulb region. The increased NO affects the contractile machinery near the valve region that in turn plays an important role in regulating the flow of lymph and force of the contraction. The arrows indicate the direction of lymph flow. The shaded regions depict the difference in the levels of shear stress across the lymphangion, with the darker regions corresponding to high while lighter regions correspond to lower shear stress. B. During low levels of lymph inflow in the collecting lymphatics (low extrinsic flows), the intrinsic pump is hypothesized to dominate with periodic NO release due to the phasic flow/shear patterns of the lymph pump to maintain efficient lymph transport. It is a disputed hypothesis that basal NO may reduce only contraction amplitude and not frequency. When the levels of lymph formation and inflow to the collecting lymphatics are significantly increased by agonists (high extrinsic flows), the influences of extrinsic forces dominate, leading to an increased NO production that in turn inhibits the intrinsic pumping and basal tone of the lymphatic vessels to optimize the conduit function of the vessel.
In addition to phasic production of NO in association with the lymphatic contraction cycle, sustained forward flow through the lymphangion can result in NO production from the lymphatic endothelium [32, 57]. This condition is predicted to occur in the intestinal lymphatic system after an absorptive load, which may temporarily create a downhill pressure gradient through the collecting vessels. Isolated, pressurized lymphatic vessels have been widely used to assess the effects of imposed (forward) flow on lymphatic contractile properties. The advantage of these methods is that the effect of flow can potentially be assessed with minimal change in intraluminal pressure (recall that a 0.5 cmH2O change in pressure can lead to a 2-fold change in contraction frequency), which would otherwise confound interpretation of any change in contractile parameters. Forward flow is imposed by simultaneously raising the pressure in the input cannulating pipette while lowering the output pressure by an equal amount, using cannulating pipettes with balanced resistances [71]. In mesenteric lymphatics as well as lymphatics from other regions in the rat, increases in the axial pressure gradient result in concomitant reductions in spontaneous contraction frequency and amplitude [15, 32]. These effects on contractile parameters are graded with the degree of imposed flow, and the reduction in both frequency and amplitude result in an even greater reduction in calculated fractional pump flow (FPF), which is the product of frequency and amplitude. Suppression of NO synthase (NOS) with Nω-nitro-L-arginine methyl ester (L-NAME) or L-NG-monomethyl Arginine (L-NMMA) increases the frequency of contraction under basal conditions (i.e. phasic flows associated with phasic contractions) and blocks the fall in contraction frequency, amplitude and FPF associated with imposed flow [32, 57, 72].
In rat thoracic duct, the NO production associated with phasic contractions does not appear to concomitantly lower both contraction frequency and amplitude [57]. During the systolic phase of a contraction, NO production near the valve area [68] acts on the muscle layer, lowering contraction frequency and tone, which together allow for increased filling of the lymphangion [57]. The increased filling can produce a larger contraction amplitude through the preload mechanism previously described, and this is analogous to positive lusitropy in cardiac muscle. In the rat thoracic duct, any inhibitory effect of NO on contraction amplitude is apparently more than compensated by positive lusitropy so that the calculated FPF can be maintained constant or even increased slightly. Whether this same effect (increased contraction amplitude in response to phasic flow) is a general principle that applies to collecting lymphatics in other regions is a topic of debate. As depicted in Figure 2B, it is a widely held opinion that the relatively high concentrations of NO evoked by agonists [53, 56, 73-75] or by continuous unidirectional flow inhibit both contraction frequency and amplitude [32, 56], whereas lower (basal) levels of NO are thought to decrease frequency but increase contraction strength / amplitude [57-59, 68, 70, 76]; however, the latter observation has only been made in rat thoracic duct under conditions where significant pressure changes were unlikely to occur [57].
Two recent studies in mice are relevant to this topic. Liao et al [59] measured reduced lymphatic contraction strength and increased lymphatic diameter of popliteal lymphatic vessels, studied in situ, in both eNOS−/− mice and in WT mice after the latter were subjected to sustained NOS inhibition (3 days of L-NMMA infusion). In contrast to observations after temporary NO inhibition in isolated lymphatic vessels from rats [15, 32, 68], both groups of NO-deficient mouse popliteal lymphatics exhibited larger lymphatic diameters compared with control animals. However, calculated lymph output in popliteal vessels from eNOS−/− and WT mice ± L-NMMA treatment were not significantly different, suggesting that increases in lymphatic diameter and contraction frequency may have resulted from systemic compensation for the reduced strength of contraction in order to maintain fluid balance. In contrast, Scallan & Davis [74] studied isolated popliteal lymphatic vessels from eNOS−/− mice and WT mice during acute NO inhibition, and found that in both cases NO deficiency resulted in increases in contraction strength and modest increases in frequency. Basal NO production depressed contraction amplitude but not frequency, with higher concentrations of NO then inhibiting both amplitude and frequency. The authors proposed that NO production, whether basal or stimulated, depresses murine collecting lymphatic contractile activity, although this conclusion may only apply to lymphatics that are peripherally located. If this pattern holds for other types of collecting lymphatics, then a possible role for basal NO in collecting lymphatics might be to set contractile amplitude at a level that can be increased or decreased to modulate lymph flow [74]. To address the discrepancy in the disparate results from in situ and in vitro mouse popliteal lymphatics, Scallan et al proposed that the elevated frequency, decreased contraction amplitude and increased diameter in response to eNOS ablation in situ [59], might be explained by an increased diastolic lymphatic pressure / preload that leads to an increase in end-diastolic diameter and frequency while reducing contraction amplitude in proportion to the pressure change [34, 37, 74].
It is apparent from the discussion above that in vivo and ex vivo methods can lead to disparate conclusions about the effects of shear-stress-mediated NO production on lymphatic contraction. The ex vivo study of isolated lymphatic vessels allows for control of pressure and/or flow, but alters the normal environment of the vessel, e.g. by interrupting axial and radial tethering forces and removing sources/sinks for NO production/action. The extent to which those factors contribute to lymphatic function, relative to the intrinsic sensitivity of the lymphatic wall to pressure and shear stress, is a complicated issue that will require both in vivo and ex vivo methods in tandem to fully understand.
Modulation of myosin light chain 20 (MLC20) as a determinant of lymphatic contractile strength
MLC20 phosphorylation plays a central role in smooth muscle contraction. The regulatory mechanisms of MLC20 phosphorylation by myosin light chain kinase (MLCK) and myosin light chain phosphatase (MLCP) pathways have been well documented in several smooth muscle cell types [77-80]. Studies from our group have shown that regulation and changes in levels of MLC20 are critical determinants of tonic lymphatic contraction [19, 21, 84, 85].
The molecular mechanisms regulating tonic and phasic contractions of lymphatic muscle are basically unknown. Wang et al have shown that tonic contraction strength and phasic contraction amplitude of the lymphatics can be differentially regulated; an increase in transmural pressure decreases MLC20 phosphorylation and tonic contraction, while phasic contraction frequency and amplitude are increased. The MLCK inhibitor, ML-7, did not alter phasic contraction amplitude of mesenteric lymphatics, but decreased tone, indicating an MLCK-dependent mechanism for tonic contraction and the existence of other pathways for the regulation of phasic contractions [21]. Nepiyushchikh et al performed the first study to directly quantify levels of MLC-P and MLC-2P in pressurized rat thoracic duct and cervical lymphatics using urea glycerol gel electrophoresis [85]. Thoracic ducts exhibited a significant decrease in tone in response to elevated pressure that correlated with a decrease in MLC-2P, whereas, in cervical lymphatics, a trend towards decreasing tone was observed under the same conditions, along with a small but significant decrease in MLC-2P [85].
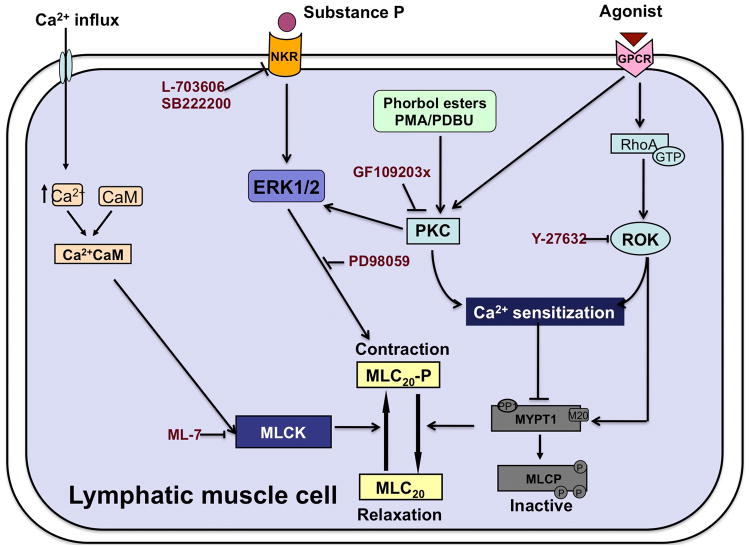
Two important signaling pathways involved in modulating the Ca2+ sensitivity of the smooth muscle contractile apparatus and affect MLC20 in response to agonist stimulation are Rho-associated kinase (ROCK) and protein kinase C (PKC) [80, 86]. We have recently shown that activation of PKC signaling with phorbol ester such as Phorbol 12,13-dibutyrate (PDBu) induces strong contractions and increases the Ca2+ sensitivity of the contractile apparatus in lymphatic muscle. The initial rapid increase in tension development was associated with MLC20 phosphorylation, although sustained contraction in permeabilized lymphatic vessels was not associated with changes in MLC20. [19]. Dissociation of contractile force and MLC20 phosphorylation after the sustained activation of PKC may be due to enhanced cooperativity between phosphorylated and unphosphorylated cross-bridges, i.e., the sustained contraction and slowed rate of relaxation may reflect attachment and force production by strongly bound, unphosphorylated myosin cross-bridges [19]. It has been shown that RhoA/ROCK-mediated Ca2+-sensitizing mechanism directly affects mesenteric lymphatic tone and application of the ROCK inhibitor Y-27632 causes a loss of tone in isolated rat iliac collecting lymphatic vessels and in the rat thoracic duct [87-89]. Further, Kurtz et al. have shown that ROCK1 and ROCK2 increase Ca2+ sensitivity, leading to enhanced tone in isolated collecting lymphatic vessels [90]. As clearly demonstrated by our previous findings, changes in lymphatic tone directly correlates to changes in MLC20 phosphorylation. As summarized in Figure 3, it is clearly evident that a complex molecular mechanism exists in lymphatic muscle that mediates the regulation of phosphorylation of MLC20 and subsequent determination of the contractile response.
Figure 3. Schematic representation of regulation of MLC20 pathways in lymphatic muscle cells.
Regulation of lymphatic muscle contraction occurs primarily through phosphorylation of the 20-kDa regulatory myosin light chain (MLC20), which is regulated by the relative activities of MLC kinase (MLCK) and MLC phosphatase (MLCP). Increased levels of cytosolic Ca2+ presumably initiate lymphatic muscle contraction by binding to the universal intracellular Ca2+ receptor protein, calmodulin (CaM). This complex activates the catalytic subunit of myosin light-chain kinase (MLCK). In turn, MLCK phosphorylates MLC20, leading to contraction. MLC20 phosphorylation is reversed by MLC phosphatase (MLCP) that results in muscle relaxation. Phosphorylation of the MLCP subunit MYPT1 inactivates it, leading to sustained muscle contraction. Two important signaling pathways involved in modulating the Ca2+ sensitivity of the smooth muscle contractile apparatus in response to agonist stimulation are Rho-associated kinase (ROCK) and protein kinase C (PKC). Agonist stimulation activates the G-protein coupled receptors that activate the small GTPase RhoA and its downstream effector Rho-kinase (ROCK). This pathway, as well as phorbol esters, also activates PKC. Both ROCK and PKC may potentially increase MLC20 phosphorylation by activation of MLCP and subsequent inhibition of its activity. Application of ROCK inhibitor Y-27632 results in a loss of tonic contraction. On the other hand, PKC may also directly activate ERK1/2 to initiate MLC20 phosphorylation. The PKC inhibitor GF109203x has been shown to abrogate this PKC-mediated ERK activation in lymphatic muscle. In a parallel pathway, Substance P (SP) binding to neurokinin receptors NK1R and/or NK3R activates ERK1/2. Activation of p-ERK increases MLC20 phosphorylation, which is diminished upon inhibition of ERK1/2 with PD-98059. SP-mediated downstream signaling is blocked by the neurokinin receptor inhibitor NK1R (L703606) and/or NK3R (SB222200). Inhibition of MLCK activity by ML-7 decreases levels of phosphorylated forms of MLC20, and leads to a subsequent decrease in tonic contraction.
Regulation of lymphatic contractile function during inflammation
As the lymphatics are critically involved in the immune response and act as conduits of immune cells, they are central to a number of inflammation-related pathologies [17, 91-93]. The contradiction between the expansion of the lymphatic network and the reduction of lymphatic drainage in some models of inflammation may be explained by the dysregulation of collecting lymphatic vessel function. Inflammation generally enhances the flow of lymph [94] and enhances interstitial fluid volume due to enhanced microvascular permeability [24]. As discussed above, this volume load induces a stretch on the lymphatic vessel wall, which would generally tend to enhance contractile frequency and/or strength. The paradoxical reduction of lymphatic drainage is most likely explained by the production of the various neuromediators associated with immune and inflammatory responses, such as substance P (SP), calcitonin gene related peptide (CGRP), neuropeptide Y, vasoactive intestinal polypeptide (VIP) and prostaglandins; all have been reported to strongly affect lymphatic vessel contractile function (reviewed in [17, 95]).
SP, a proinflammatory neuropeptide, significantly induces tonic contraction in mesenteric lymphatics that is attenuated by inhibition of MLC20 phosphorylation [21, 85, 96]. In addition, SP is able to activate both contractile and inflammatory pathways in lymphatic muscle cells primarily by mediating the phosphorylation of MLC20 as well as activation of the proinflammatory p38/ERK pathways [97]. Inhibition of ERK1/2 decreased levels of p-MLC20 after SP activation, in a PKC dependent manner (Figure 3). SP is known to mediate its effects through the neurokinin receptors. We found that in rat mesenteric lymphatic muscle cells NK1R and NK3R are expressed and both are necessary for SP-mediated signaling (Figure 3). We hypothesize that different concentrations of SP found during inflammatory conditions could activate both contractile and inflammatory pathways, which exhibit crosstalk with each other, and that a graded release of SP under such conditions would maintain a fine balance between modulation of contractile function and progression of inflammation [97].
As mentioned previously, nitric oxide (NO) is produced by LECs in response to shear stress and various agonists and is an important modulator of lymphatic contractile function [32, 57, 70, 72, 98]. However, NO is also produced by immune cells surrounding collecting lymphatic vessels and in adjacent spaces of the interstitium [59]. However, studies addressing the effects of these immune cells on lymphatic contractility are limited. Liao et al [59] have shown that under inflammatory conditions, inducible NOS (iNOS)-expressing CD11b+Gr-1+ cells attenuate lymphatic contraction in mouse popliteal lymphatics in situ. During inflammation, excessive amounts of NO produced by iNOS in infiltrated bone marrow-derived cells (BMDCs) overwhelm the spatial and temporal NO gradients produced by eNOS (see discussion above), thus inhibiting contraction. Furthermore, iNOS-derived NO may cause chronic relaxation of perilymphatic SMCs, increasing vessel diameter, reducing inotropy, and thus reducing contraction strength [59]. Ablation of NO in eNOS-/- animals caused a reduction in contractility, whereas paradoxically, under inflammatory conditions, removing NO produced by iNOS in BMDCs increased contraction strength. This lends credence to the hypothesis that the temporal and spatial gradients of NO, in addition to the total amount produced, are critical to its ultimate function [99, 100]. The suppression of NOS, while lymph vessels are activated, disrupts the contraction/relaxation cycle in favor of excessive contraction. The resultant NO generation by the activated lymph vessel is essential to diastolic filling and, thereby, the maintenance of elevated lymph pump flow [101]. A computational flow and mass transfer model using physiologic geometries obtained from confocal images of a rat mesenteric lymphatic vessel recently offered some interesting insights in the possible characteristics of NO transport in the lymphatic flow regime. Simulations revealed areas of flow stagnation adjacent to the valve leaflets, suggesting the high concentrations observed experimentally in that region are due to minimal convection. Additionally it was shown that high NO concentrations adjacent to the valve leaflets are most likely due to flow-mediated processes rather than differential production by shear-sensitive LECs [102]. These data suggest that lymphatic contractility, flow of lymph and inflammatory mechanisms are closely tied together in determining a specific contractile response.
Changes in the surrounding immune cell population also modulate the availability of key cytokines and chemokines critical to maintenance of normal lymphatic function. For example, dietary endotoxins such as LPS modulate the recruitment of immune cells such as neutrophils, monocytes and macrophages associated with mesenteric lymphatic vessels or in adjacent regions and are associated with significant impairment of lymphatic contractile function and pump flow ([103] unpublished data). Further, Chatterjee et al., [104] have shown that mesenteric lymphatic vessels have a population of mast cells that are closely associated with but outside of the lymphatic vessel wall. A higher degree of preactivated mast cells was found associated with the aged lymphatic vessels and could attribute to the development of aging-associated impairment of function of mesenteric lymphatic vessels by promoting an aging-associated chronic inflammatory environment in the mesenteric lymphatic bed [104]. These mast cells (or other closely associated immune cells) could release a host of agents able to potentially alter the electrophysiological activities of the lymphatic vessel. Interestingly, Chatterjee et al., detected expression of the histamine-producing enzyme HDC, not only in mast cells but also in the walls of lymphatic vessels [104, 105]. Histamine itself was detected in lymphatic endothelium as well as within lymphatic vessels, where it was found to be more concentrated in the lymphatic valve regions [106]. In contrast to the extensive literature on endothelial-dependent dilators other than NO in the regulation of tone in the blood vasculature, there are only sparse literature reports indicating the potential existence of such mechanisms regulating lymphatic contractility and tone in a shear-dependent manner. Low doses of externally added histamine increase frequency and amplitude of lymphatic contractions while higher doses of externally added histamine relax lymphatic vessels [107, 108]. Such findings appear to be highly supportive of the idea that NO and histamine produce relaxation of lymphatic muscle through the same molecular targets [74, 106]. Mediators like histamine could in turn affect other local inflammatory mediators that modulate lymphatic contractility [106, 109].
In collecting lymphatics, alterations in lymphatic function associated with edema and inflammation are well known, but the integrity of the lymphatic endothelial barrier during inflammation is not. It has been shown recently that endothelial permeability was increased following treatment with pro-inflammatory cytokines (TNF-α, IL-6, IL-1β, IFN-γ and LPS) [110]. This effect depended on the production of NO and was associated with changes in levels of p-MLC20. Changes in lymphatic permeability are associated with large changes in fluid preload that have been shown to significantly affect contractile function. In mouse models of lymphedema, as well as clinical lymphedema specimens, lymphatic stasis results in a CD4 T-cell inflammation and T-helper 2 (Th2) differentiation. Avraham et al., show that CD4 inflammation is a critical regulator of tissue fibrosis and lymphatic dysfunction in lymphedema and that inhibition of Th2 differentiation markedly improves lymphatic function independent of lymphangiogenic cytokine expression [111]. Further, an acute administration of LPS-induced inflammation results in cessation of propulsive flow in mesenteric lymphatics. Similar effects are also observed by various cytokines induced in the lymphatics by LPS, such as IL-6, TNF-α, and IL-1β that have been shown to decrease systemic lymphatic propulsion [112]. Taken together, these studies directly indicate that inflammatory changes in the surrounding microenvironment significantly affect the lymphatic contractile behavior and subsequent flow of lymph.
Pathologies with underlying lymphatic contractile dysfunction
Metabolic syndrome, obesity and atherosclerosis
Recently, we have shown that metabolic syndrome (MetSyn), which is characterized by chronic subclinical inflammation, induces a remodeling of collecting lymphatics, thereby effectively reducing their potential load capabilities and impairing the intrinsic contractility required for proper lymph flow [113]. Architectural remodeling of the blood microvasculature has long been associated with various chronic inflammatory conditions [91, 114, 115]. Recently, much attention has been directed at lymphatic capillary and collecting vessel function during acute inflammation as these play critical roles in the resolution of edema within the inflamed region [116, 117]. Lymphatics from MetSyn rats had significant negative chronotropy at all pressures, effectively reducing the intrinsic flow-generating capacity of these vessels by ∼50%. Prenodal lymphatic collecting vessels in MetSyn rats were significantly smaller in diameter than their control counterparts under pressurized conditions. Mesenteric lymphatics from MetSyn rats exhibited a two-fold reduction in their total force production and their myofilaments were significantly less sensitive to Ca2+ compared with control myofilaments [113]. We propose that the lymphatics form a critical bridge between MetSyn-induced physiological changes in the mesenteric bed, the surrounding adipose and inflammatory response [84, 113]. Our data also showed elevated levels of the lipid metabolism regulator genes, PPARα and SREBP1c, along with the inflammatory cytokine TNFα, in MetSyn animals, corroborating the onset of an inflammatory phenotype. Both smooth and skeletal muscle weakness have been demonstrated in muscle tissue from insulin-resistant models where circulating cytokines are thought to play a critical role [118]. Through aberrant chylomicron production, MetSyn alters the mechanical characteristics of lymph via changes in viscosity and osmolarity, creating a permissive state for an increased inflammatory profile of the postprandial mesenteric lymph.
Therefore we speculate that the inflammatory conditions and mechanical stresses in MetSyn contribute to the remodeling of the mesenteric lymphatics and the reduction of vessel diameter. Consistent with these studies, Blum et al. have shown that adipose tissue expansion in mice fed a high fat diet leads to functional impairment of collecting lymphatics [119]. Lymphatic impairment in obese mice is substantially aggravated by lymphatic injury and lymphedema, leading to increased fat deposition, fibrosis and chronic inflammatory reactions [120]. Obesity has also been shown to significantly remodel lymph node architecture and impair dendritic cell migration to the node [121].
Lymphatic vessels have also emerged as active players in reverse cholesterol transport. In apoE or LDL receptor knockout mice, which develop hypercholesterolemia, skin lymphatic vessels exhibit structural defects that severely compromise their function. These observations suggest that the accumulation of cholesterol in arteries and skin from hyper-cholesterolemic mice result from poor lymphatic drainage [122]. Restoration of lymphatic drainage in these mice significantly improves cholesterol clearance. Conversely, obstruction of lymphatic vessels in wild-type mice significantly impairs this function [122, 123].
Lymphedema
Insufficient lymphatic function causes interstitial accumulation of fluid, leading to chronic swelling of the limbs, or lymphedema. In addition to swelling, the protein-rich interstitial fluid induces an inflammatory reaction, leading to fibrosis and accumulation of adipose and connective tissue. This will consequently cause impaired immune responses and wound healing, which will increase the susceptibility of the patient to secondary infections [124, 125]. Sustained swelling due to fluid accumulation leads to lymphatic hyperplasia and up-regulation of vascular endothelial growth factor, VEGF-C, which may exacerbate the edema because the hyperplastic vessels are poorly functional [126]. Zampell et al. have demonstrated that the loss of TLR function results in worsening of the lymphedema, decreases interstitial fluid flow, increases fat deposition, inhibits macrophage infiltration and increases tissue fibrosis [127]. Lymphatic fluid stasis has been shown to further aggravate the inflammatory response by activation of endogenous danger signals that activate deleterious inflammatory reactions [128]. Indeed, patients with lymphedema are prone to developing chronic bacterial, fungal, and viral infection in the stagnant lymph of the edematous limb. This is possibly due to an inefficient clearance of the pathogen via the lymph in addition to impaired adaptive immunity [129]. The same mechanisms also contribute to diseases such as filariasis, which is the leading cause of secondary lymphedema worldwide. Filarial lymphedema is associated with characteristic alterations of the lymphatic system, including the dilation of lymphatics with extensive collateral formation, loss of functional valves, and retrograde lymph flow (reviewed in [130]).
Inflammatory Bowel Disease
The lymphatic system plays a significant role in the onset and progression of inflammatory bowel disease (IBD) [131]. Patients suffering from IBD are characterized by interstitial edema and dilated intestinal initial lymphatics or lacteals [132-134]. Edema serves to aggravate the condition as poor drainage leads to impaired transport of immune cells and other inflammatory agents and in turn promotes infection and delays the immune response [134]. In a 2,4,6-Trinitrobenzenesulfonic acid (TNBS) model of guinea pig ileitis, the ability of mesenteric lymphatics to undergo phasic contractions was strongly impaired and the vessels were significantly dilated [135]. The inhibition of spontaneous contractions was markedly reversed in vivo and in vitro upon application of indomethacin or a combination of COX-1 and COX-2 selective inhibitors. These findings suggest a role for prostanoids in inflammation-induced lymphatic contractile dysfunction [134].
Lymphatic vessel function in aging
Aging-associated diminution in lymphatic vessel function and lymph flow has been demonstrated by a number of recent studies [136, 137]. In thoracic duct segments from older rats, lower lymphatic tone together with decreased lymphatic contraction amplitude may be considered an indicator of age-related weakening of muscle cells and their diminished ability to generate enough force to maintain the level of tone and contractile force appropriate to the lymphatic preload [138, 139]. The ability of the aged thoracic duct to adapt its pumping to different levels of extrinsic lymph flow is also severely altered. In fact the eNOS-mediated imposed flow-dependent regulatory mechanism was completely depleted in 24-month-old thoracic duct segments [137]. Aging-associated weakening of the lymphatic pump has also been observed in mesenteric lymphatic vessels and it is proposed that aging remarkably weakens mesenteric lymphatic vessel contractility, which would predispose this lymphatic network to lower total lymph flows under resting conditions and limit its ability to respond to edemagenic challenges in the elderly [138, 139]. Aging has also been shown to significantly affect the muscle investiture of collecting lymphatics [140]. Evaluation of muscle cell density in mesenteric lymphatics in reference to the position of lymphatic valve in different zones of the lymphangion within various age groups, showed that zones located immediately upstream of lymphatic valves possess the lowest density of lymphatic muscle cells. Most of the high muscle cell density zones were found downstream to the lymphatic valve, and this was not affected by aging. However, the pre-valve and valve zones showed significant aging-associated decreases in muscle cell density. Changes in the distribution of these cells may thus have an important functional impact on the biomechanics of the lymphatic valve gating and/or the electrical coupling between lymphangions, such that aged lymphatic vessels may have limited adaptive reserves [140].
Conclusions and future challenges
It is thus clearly evident that a number of factors regulate the contractile functions of lymphatic vessels and determine their physiological impact. These factors may be components of the surrounding microenvironment or induced within the endothelial or muscle layer of the lymphatic vessel wall in response to a pathological condition or inflammatory stimuli. The last decade has seen major strides in delineating different aspects of lymphatic contractile dysfunction in normal and pathological conditions. Although we now have a significant understanding of the different characteristics of basic contractile parameters, much remains to be explored to clearly define the molecular mechanisms that underlie the lymphatic dysfunction associated with inflammatory pathologies. A large number of studies have addressed the role of lymphatics in development, endothelial inflammation, transport of immune cells, and the subsequent effects of cytokines and the surrounding microenvironment in mediating the progression and resolution of inflammation and growth of new lymphatic vessels. Most of those studies have focused on the initial lymphatics that serve as the entry point of interstitial fluid. However, only a few groups worldwide are focused on delineating the contractile physiology of the collecting lymphatics that is central to the function of the entire system. Further research in this area is critical as insufficient lymphatic drainage or fluid stasis is the key underlying feature of several debilitating diseases. A better understanding of the signaling pathways and regulatory mechanisms can yield better therapeutic intervention strategies for mitigating the effects of incomplete lymphatic drainage by improving lymphatic contraction and lymph flow. In spite of a surge of recent research in this area, the precise molecular mechanisms that regulate tonic and phasic contractions of the lymphatics are still not clearly defined. Recent studies also underscore the role of nitric oxide and various other inflammatory mediators in the vicinity of the lymphatics in regulating the nature and strength of lymphatic contractility. However, it is not clear the extent to which inflammatory mediators directly influence lymphatic contractile function and how lymphatic contraction and lymph flow may in turn influence the immune response. A sequential dissection of these various mechanisms is necessary for targeting lymphatic dysfunction.
Acknowledgments
This work was supported by NIH R01 DK99221 to MM and NIH R01HL-120867 to MJD.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Zawieja DC. Contractile physiology of lymphatics. Lymphat Res Biol. 2009;7:87–96. doi: 10.1089/lrb.2009.0007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Gashev AA, Zawieja DC. Hydrodynamic regulation of lymphatic transport and the impact of aging. Pathophysiology : the official journal of the International Society for Pathophysiology / ISP. 2010;17:277–87. doi: 10.1016/j.pathophys.2009.09.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Collin H. The ultrastructure of conjunctival lymphatic anchoring filaments. Exp Eye Res. 1969;8:102–5. doi: 10.1016/s0014-4835(69)80019-9. [DOI] [PubMed] [Google Scholar]
- 4.Leak L, Burke J. Ultrastructural studies on the lymphatic anchoring filaments. J Cell Biol. 1968;36:129–49. [PMC free article] [PubMed] [Google Scholar]
- 5.Leak LV. The structure of lymphatic capillaries in lymph formation. Fed Proc. 1976;35:1863–71. [PubMed] [Google Scholar]
- 6.Baluk P, Fuxe J, Hashizume H, Romano T, Lashnits E, Butz S, et al. Functionally specialized junctions between endothelial cells of lymphatic vessels. J Exp Med. 2007;204:2349–62. doi: 10.1084/jem.20062596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Oliver G, Alitalo K. The lymphatic vasculature: recent progress and paradigms. Annual review of cell and developmental biology. 2005;21:457–83. doi: 10.1146/annurev.cellbio.21.012704.132338. [DOI] [PubMed] [Google Scholar]
- 8.Lynch PM, Delano FA, Schmid-Schonbein GW. The primary valves in the initial lymphatics during inflammation. Lymphat Res Biol. 2007;5:3–10. doi: 10.1089/lrb.2007.5102. [DOI] [PubMed] [Google Scholar]
- 9.Trzewik J, Mallipattu SK, Artmann GM, Delano FA, Schmid-Schonbein GW. Evidence for a second valve system in lymphatics: endothelial microvalves. FASEB J. 2001;15:1711–7. doi: 10.1096/fj.01-0067com. [DOI] [PubMed] [Google Scholar]
- 10.Mendoza E, Schmid-Schonbein GW. A model for mechanics of primary lymphatic valves. Journal of biomechanical engineering. 2003;125:407–14. doi: 10.1115/1.1568128. [DOI] [PubMed] [Google Scholar]
- 11.Mislin H. Structural and functional relations of the mesenteric lymph vessels. New Trends in Basic Lymphology. Experientia; Proceedings of a Symposium held at Charleroi (Belgium); July 11-13, 1966; 1966. pp. 87–96. [Google Scholar]
- 12.Mislin H. Active contractility of the lymphangion and coordination of lymphangion chains. Experientia. 1976;32:820–2. doi: 10.1007/BF02003701. [DOI] [PubMed] [Google Scholar]
- 13.Muthuchamy M, Zawieja D. Molecular regulation of lymphatic contractility. Ann N Y Acad Sci. 2008;1131:89–99. doi: 10.1196/annals.1413.008. [DOI] [PubMed] [Google Scholar]
- 14.Zawieja D. Lymphatic biology and the microcirculation: past, present and future. Microcirculation. 2005;12:141–50. doi: 10.1080/10739680590900003. [DOI] [PubMed] [Google Scholar]
- 15.Gashev AA, Davis MJ, Delp MD, Zawieja DC. Regional variations of contractile activity in isolated rat lymphatics. Microcirculation. 2004;11:477–92. doi: 10.1080/10739680490476033. [DOI] [PubMed] [Google Scholar]
- 16.Schmid-Schonbein GW. The second valve system in lymphatics. Lymphat Res Biol. 2003;1:25–9. doi: 10.1089/15396850360495664. discussion 9-31. [DOI] [PubMed] [Google Scholar]
- 17.von der Weid PY, Muthuchamy M. Regulatory mechanisms in lymphatic vessel contraction under normal and inflammatory conditions. Pathophysiology. 2010;17:263–76. doi: 10.1016/j.pathophys.2009.10.005. [DOI] [PubMed] [Google Scholar]
- 18.Davis MJ, Davis AM, Ku CW, Gashev AA. Myogenic constriction and dilation of isolated lymphatic vessels. Am J Physiol Heart Circ Physiol. 2009;296:H293–302. doi: 10.1152/ajpheart.01040.2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Dougherty PJ, Nepiyushchikh ZV, Chakraborty S, Wang W, Davis MJ, Zawieja DC, et al. PKC activation increases Ca(2)(+) sensitivity of permeabilized lymphatic muscle via myosin light chain 20 phosphorylation-dependent and -independent mechanisms. Am J Physiol Heart Circ Physiol. 2014;306:H674–83. doi: 10.1152/ajpheart.00732.2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Muthuchamy M, Gashev A, Boswell N, Dawson N, Zawieja D. Molecular and functional analyses of the contractile apparatus in lymphatic muscle. Faseb J. 2003;17:920–2. doi: 10.1096/fj.02-0626fje. [DOI] [PubMed] [Google Scholar]
- 21.Wang W, Nepiyushchikh Z, Zawieja DC, Chakraborty S, Zawieja SD, Gashev AA, et al. Inhibition of myosin light chain phosphorylation decreases rat mesenteric lymphatic contractile activity. American journal of physiology Heart and circulatory physiology. 2009;297:H726–34. doi: 10.1152/ajpheart.00312.2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Amerini S, Ziche M, Greiner ST, Zawieja DC. Effects of substance P on mesenteric lymphatic contractility in the rat. Lymphat Res Biol. 2004;2:2–10. doi: 10.1089/1539685041690409. [DOI] [PubMed] [Google Scholar]
- 23.Benoit JN. Effects of alpha-adrenergic stimuli on mesenteric collecting lymphatics in the rate. American Journal of Physiology. 1997;273:R331–6. doi: 10.1152/ajpregu.1997.273.1.R331. [DOI] [PubMed] [Google Scholar]
- 24.Benoit JN, Zawieja DC, Goodman AH, Granger HJ. Characterization of intact mesenteric lymphatic pump and its responsiveness to acute edemagenic stress. American Journal of Physiology. 1989;257:H2059–69. doi: 10.1152/ajpheart.1989.257.6.H2059. [DOI] [PubMed] [Google Scholar]
- 25.McHale NG, Roddie IC. The effect of transmural pressure on pumping activity in isolated bovine lymphatic vessels. The Journal of Physiology. 1976;261:255–69. doi: 10.1113/jphysiol.1976.sp011557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ohhashi T, Azuma T, Sakaguchi M. Transmembrane potentials in bovine lymphatic smooth muscle. Proc Soc Exp Biol Med. 1978;159:350–2. doi: 10.3181/00379727-159-40346. [DOI] [PubMed] [Google Scholar]
- 27.Shirasawa Y, Benoit JN. Stretch-induced calcium sensitization of rat lymphatic smooth muscle. Am J Physiol Heart Circ Physiol. 2003;285:H2573–7. doi: 10.1152/ajpheart.00002.2003. [DOI] [PubMed] [Google Scholar]
- 28.Zhang RZ, Gashev AA, Zawieja DC, Davis MJ. Length-tension relationships of small arteries, veins, and lymphatics from the rat mesenteric microcirculation. Am J Physiol Heart Circ Physiol. 2007;292:H1943–52. doi: 10.1152/ajpheart.01000.2005. [DOI] [PubMed] [Google Scholar]
- 29.Zhao J, van Helden DF. ET-1-associated vasomotion and vasospasm in lymphatic vessels of the guinea-pig mesentery. Br J Pharmacol. 2003;140:1399–413. doi: 10.1038/sj.bjp.0705573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Lee S, Roizes S, von der Weid PY. Distinct roles of L- and T-type voltage-dependent Ca2+ channels in regulation of lymphatic vessel contractile activity. J Physiol. 2014 doi: 10.1113/jphysiol.2014.280347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Gashev AA, Zhang RZ, Muthuchamy M, Zawieja DC, Davis MJ. Regional heterogeneity of length-tension relationships in rat lymph vessels. Lymphat Res Biol. 2012;10:14–9. doi: 10.1089/lrb.2011.0013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Gashev AA, Davis MJ, Zawieja DC. Inhibition of the active lymph pump by flow in rat mesenteric lymphatics and thoracic duct. J Physiol. 2002;540:1023–37. doi: 10.1113/jphysiol.2001.016642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Ohhashi T, Azuma T, Sakaguchi M. Active and passive mechanical characteristics of bovine mesenteric lymphatics. American Journal of Physiology. 1980;239:H88–95. doi: 10.1152/ajpheart.1980.239.1.H88. [DOI] [PubMed] [Google Scholar]
- 34.Davis MJ, Scallan JP, Wolpers JH, Muthuchamy M, Gashev AA, Zawieja DC. Intrinsic increase in lymphangion muscle contractility in response to elevated afterload. Am J Physiol Heart Circ Physiol. 2012;303:H795–808. doi: 10.1152/ajpheart.01097.2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Eisenhoffer J, Kagal A, Klein T, Johnston MG. Importance of valves and lymphangion contractions in determining pressure gradients in isolated lymphatics exposed to elevations in outflow pressure. Microvasc Res. 1995;49:97–110. doi: 10.1006/mvre.1995.1008. [DOI] [PubMed] [Google Scholar]
- 36.Elias RM, Wandolo G, Ranadive NS, Eisenhoffer J, Johnston MG. Lymphatic pumping in response to changes in transmural pressure is modulated by erythrolysate/hemoglobin. Circ Res. 1990;67:1097–106. doi: 10.1161/01.res.67.5.1097. [DOI] [PubMed] [Google Scholar]
- 37.Scallan JP, Wolpers JH, Muthuchamy M, Zawieja DC, Gashev AA, Davis MJ. Independent and interactive effects of preload and afterload on the pump function of the isolated lymphangion. Am J Physiol Heart Circ Physiol. 2012;303:H809–24. doi: 10.1152/ajpheart.01098.2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Hargens AR, Zweifach BW. Contractile stimuli in collecting lymph vessels. American Journal of Physiology. 1977;233:H57–65. doi: 10.1152/ajpheart.1977.233.1.H57. [DOI] [PubMed] [Google Scholar]
- 39.Olszewski WL. Contractility patterns of normal and pathologically changed human lymphatics. Ann N Y Acad Sci. 2002;979:52–63. doi: 10.1111/j.1749-6632.2002.tb04867.x. discussion 76-9. [DOI] [PubMed] [Google Scholar]
- 40.Olszewski WL, Kruszewski S, Sokolowski J, Zgliczynski L, Nielubowicz J. Observations of movements of lymph vessels in patients with lymphoedema of the limbs. Polski Tygodnik Lekarski. 1968;23:1345–47. Polish. [PubMed] [Google Scholar]
- 41.von der Weid PY, Lee S, Imtiaz MS, Zawieja DC, Davis MJ. Electrophysiological properties of rat mesenteric lymphatic vessels and their regulation by stretch. Lymphat Res Biol. 2014;12:66–75. doi: 10.1089/lrb.2013.0045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Rehal S, Blanckaert P, Roizes S, von der Weid PY. Characterization of biosynthesis and modes of action of prostaglandin E2 and prostacyclin in guinea pig mesenteric lymphatic vessels. Br J Pharmacol. 2009;158:1961–70. doi: 10.1111/j.1476-5381.2009.00493.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Eisenhoffer J, Elias RM, Johnston MG. Effect of outflow pressure on lymphatic pumping in vitro. Am J Physiol. 1993;265:R97–102. doi: 10.1152/ajpregu.1993.265.1.R97. [DOI] [PubMed] [Google Scholar]
- 44.Brice G, Mansour S, Bell R, Collin JR, Child AH, Brady AF, et al. Analysis of the phenotypic abnormalities in lymphoedema-distichiasis syndrome in 74 patients with FOXC2 mutations or linkage to 16q24. Journal of medical genetics. 2002;39:478–83. doi: 10.1136/jmg.39.7.478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Petrova TV, Karpanen T, Norrmen C, Mellor R, Tamakoshi T, Finegold D, et al. Defective valves and abnormal mural cell recruitment underlie lymphatic vascular failure in lymphedema distichiasis. Nat Med. 2004;10:974–81. doi: 10.1038/nm1094. [DOI] [PubMed] [Google Scholar]
- 46.Davis MJ, Rahbar E, Gashev AA, Zawieja DC, Moore JE., Jr Determinants of valve gating in collecting lymphatic vessels from rat mesentery. Am J Physiol Heart Circ Physiol. 2011;301:H48–60. doi: 10.1152/ajpheart.00133.2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Scallan JP, Wolpers JH, Davis MJ. Constriction of isolated collecting lymphatic vessels in response to acute increases in downstream pressure. J Physiol. 2013;591:443–59. doi: 10.1113/jphysiol.2012.237909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Petrenko VM. Conceptions on the structural organization of the active lymph flow between the neighboring lymphangions. Morfologiia. 2007;132:87–92. [PubMed] [Google Scholar]
- 49.Schmid-Schonbein GW. Microlymphatics and Lymph Flow. Physiological reviews. 1990;70:987–1028. doi: 10.1152/physrev.1990.70.4.987. [DOI] [PubMed] [Google Scholar]
- 50.Mizuno R, Dornyei G, Koller A, Kaley G. Myogenic responses of isolated lymphatics: modulation by endothelium. Microcirculation. 1997;4:413–20. doi: 10.3109/10739689709146805. [DOI] [PubMed] [Google Scholar]
- 51.von der Weid PY. Lymphatic myogenic constriction - how lymphatic vessels pump lymph uphill. J Physiol. 2013;591:391–2. doi: 10.1113/jphysiol.2012.247080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Elias RM, Johnston MG. Modulation of lymphatic pumping by lymph-borne factors after endotoxin administration in sheep. Journal of applied physiology. 1990;68:199–208. doi: 10.1152/jappl.1990.68.1.199. [DOI] [PubMed] [Google Scholar]
- 53.Ferguson MK, DeFilippi VJ. Nitric oxide and endothelium-dependent relaxation in tracheobronchial lymph vessels. Microvascular Research. 1994;47:308–17. doi: 10.1006/mvre.1994.1024. [DOI] [PubMed] [Google Scholar]
- 54.Shirasawa Y, Ikomi F, Ohhashi T. Physiological roles of endogenous nitric oxide in lymphatic pump activity of rat mesentery in vivo. American Journal of Physiology. 2000;278:G551–6. doi: 10.1152/ajpgi.2000.278.4.G551. [DOI] [PubMed] [Google Scholar]
- 55.von der Weid PY, Crowe MJ, Van Helden DF. Endothelium-dependent modulation of pacemaking in lymphatic vessels of the guinea-pig mesentery. The Journal of Physiology. 1996;493:563–75. doi: 10.1113/jphysiol.1996.sp021404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Yokoyama S, Ohhashi T. Effects of acetylcholine on spontaneous contractions in isolated bovine mesenteric lymphatics. American Journal of Physiology. 1993;264:H1460–4. doi: 10.1152/ajpheart.1993.264.5.H1460. [DOI] [PubMed] [Google Scholar]
- 57.Gasheva OY, Zawieja DC, Gashev AA. Contraction-Initiated NO-Dependent Lymphatic Relaxation: A Self-Regulatory Mechanism in Rat Thoracic Duct. J Physiol. 2006 doi: 10.1113/jphysiol.2006.115212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Hagendoorn J, Padera TP, Kashiwagi S, Isaka N, Noda F, Lin MI, et al. Endothelial Nitric Oxide Synthase Regulates Microlymphatic Flow via Collecting Lymphatics. Circ Res. 2004 doi: 10.1161/01.RES.0000135549.72828.24. 01.RES.0000135549.72828.24. [DOI] [PubMed] [Google Scholar]
- 59.Liao S, Cheng G, Conner DA, Huang Y, Kucherlapati RS, Munn LL, et al. Impaired lymphatic contraction associated with immunosuppression. Proc Natl Acad Sci U S A. 2011;108:18784–9. doi: 10.1073/pnas.1116152108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Murad F, Forstermann U, Nakane M, Schmidt H, Pollock J, Sheng H, et al. The nitric oxide-cyclic GMP signal transduction pathway in vascular smooth muscle preparations and other tissues. Japanese journal of pharmacology. 1992;58(Suppl 2):150P–7P. [PubMed] [Google Scholar]
- 61.Walter U. Physiological role of cGMP and cGMP-dependent protein kinase in the cardiovascular system. Reviews of physiology, biochemistry and pharmacology. 1989;113:41–88. doi: 10.1007/BFb0032675. [DOI] [PubMed] [Google Scholar]
- 62.Warner TD, Mitchell JA, Sheng H, Murad F. Effects of cyclic GMP on smooth muscle relaxation. Advances in pharmacology. 1994;26:171–94. doi: 10.1016/s1054-3589(08)60054-x. [DOI] [PubMed] [Google Scholar]
- 63.Aratow M, MD, Hargens AR, PhD, Meyer JU, PhD, Arnaud SB., MD Postural Responses of Head and Foot Cutaneous Microvascular Flow and Their Sensitivity to Bed Rest. Aviation, Space, and Environmental Medicine. 1991;62:246–51. [PubMed] [Google Scholar]
- 64.Ohhashi T, Yokoyama S. Nitric oxide and the lymphatic system. Japanese Journal of Physiology. 1994;44:327–42. doi: 10.2170/jjphysiol.44.327. [DOI] [PubMed] [Google Scholar]
- 65.von der Weid PY, Zhao J, Van Helden DF. Nitric oxide decreases pacemaker activity in lymphatic vessels of guinea pig mesentery. Am J Physiol Heart Circ Physiol. 2001;280:H2707–16. doi: 10.1152/ajpheart.2001.280.6.H2707. [DOI] [PubMed] [Google Scholar]
- 66.Gasheva OY, Gashev AA, Zawieja DC. Cyclic guanosine monophosphate and the dependent protein kinase regulate lymphatic contractility in rat thoracic duct. J Physiol. 2013;591:4549–65. doi: 10.1113/jphysiol.2013.258681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Dixon JB, Greiner ST, Gashev AA, Cote GL, Moore JE, Zawieja DC. Lymph flow, shear stress, and lymphocyte velocity in rat mesenteric prenodal lymphatics. Microcirculation. 2006;13:597–610. doi: 10.1080/10739680600893909. [DOI] [PubMed] [Google Scholar]
- 68.Bohlen HG, Wang W, Gashev A, Gasheva O, Zawieja D. Phasic contractions of rat mesenteric lymphatics increase basal and phasic nitric oxide generation in vivo. Am J Physiol Heart Circ Physiol. 2009;297:H1319–28. doi: 10.1152/ajpheart.00039.2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Bohlen HG, Zhou X, Unthank JL, Miller SJ, Bills R. Transfer of nitric oxide by blood from upstream to downstream resistance vessels causes microvascular dilation. Am J Physiol Heart Circ Physiol. 2009;297:H1337–46. doi: 10.1152/ajpheart.00171.2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Bohlen HG, Gasheva OY, Zawieja DC. Nitric oxide formation by lymphatic bulb and valves is a major regulatory component of lymphatic pumping. Am J Physiol Heart Circ Physiol. 2011;301:H1897–906. doi: 10.1152/ajpheart.00260.2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Kuo L, Davis MJ, Chilian WM. Endothelium-dependent, flow-induced dilation of isolated coronary arterioles. American Journal of Physiology. 1990;259:H1063–70. doi: 10.1152/ajpheart.1990.259.4.H1063. [DOI] [PubMed] [Google Scholar]
- 72.Tsunemoto H, Ikomi F, Ohhashi T. Flow-mediated release of nitric oxide from lymphatic endothelial cells of pressurized canine thoracic duct. Jpn J Physiol. 2003;53:157–63. doi: 10.2170/jjphysiol.53.157. [DOI] [PubMed] [Google Scholar]
- 73.Leak LV, C JL, Griffin CP, Richardson K. Nitric oxide production by lymphatic endothelial cells in vitro. Biochemical & Biophysical Research Communications. 217:96–105. doi: 10.1006/bbrc.1995.2750. [DOI] [PubMed] [Google Scholar]
- 74.Scallan JP, Davis MJ. Genetic removal of basal nitric oxide enhances contractile activity in isolated murine collecting lymphatic vessels. J Physiol. 2013;591:2139–56. doi: 10.1113/jphysiol.2012.250662. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.von der Weid PY, Zhao J, Van Helden DF. Nitric oxide decreases pacemaker activity in lymphatic vessels of guinea pig mesentery. American Journal of Physiology. 2001;280:H2707–16. doi: 10.1152/ajpheart.2001.280.6.H2707. [DOI] [PubMed] [Google Scholar]
- 76.Kesler CT, Liao S, Munn LL, Padera TP. Lymphatic vessels in health and disease. Wiley interdisciplinary reviews Systems biology and medicine. 2013;5:111–24. doi: 10.1002/wsbm.1201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Cole WC, Welsh DG. Role of myosin light chain kinase and myosin light chain phosphatase in the resistance arterial myogenic response to intravascular pressure. Arch Biochem Biophys. 2011;510:160–73. doi: 10.1016/j.abb.2011.02.024. [DOI] [PubMed] [Google Scholar]
- 78.Hirano K. Current topics in the regulatory mechanism underlying the Ca2+ sensitization of the contractile apparatus in vascular smooth muscle. Journal of pharmacological sciences. 2007;104:109–15. doi: 10.1254/jphs.cp0070027. [DOI] [PubMed] [Google Scholar]
- 79.Kim HR, Appel S, Vetterkind S, Gangopadhyay SS, Morgan KG. Smooth muscle signalling pathways in health and disease. J Cell Mol Med. 2008;12:2165–80. doi: 10.1111/j.1582-4934.2008.00552.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Somlyo AP, Somlyo AV. Ca2+ sensitivity of smooth muscle and nonmuscle myosin II: modulated by G proteins, kinases, and myosin phosphatase. Physiological reviews. 2003;83:1325–58. doi: 10.1152/physrev.00023.2003. [DOI] [PubMed] [Google Scholar]
- 81.Ihara E, Moffat L, Ostrander J, Walsh MP, MacDonald JA. Characterization of protein kinase pathways responsible for Ca2+ sensitization in rat ileal longitudinal smooth muscle. Am J Physiol Gastrointest Liver Physiol. 2007;293:G699–710. doi: 10.1152/ajpgi.00214.2007. [DOI] [PubMed] [Google Scholar]
- 82.Komatsu S, Hosoya H. Phosphorylation by MAPKAP kinase 2 activates Mg(2+)-ATPase activity of myosin II. Biochem Biophys Res Commun. 1996;223:741–5. doi: 10.1006/bbrc.1996.0966. [DOI] [PubMed] [Google Scholar]
- 83.Niiro N, Ikebe M. Zipper-interacting Protein Kinase Induces Ca2+-free Smooth Muscle Contraction via Myosin Light Chain Phosphorylation. J Biol Chem. 2001;276:29567–74. doi: 10.1074/jbc.M102753200. [DOI] [PubMed] [Google Scholar]
- 84.Chakraborty S, Zawieja S, Wang W, Zawieja DC, Muthuchamy M. Lymphatic system: a vital link between metabolic syndrome and inflammation. Ann N Y Acad Sci. 2010;1207(Suppl 1):E94–102. doi: 10.1111/j.1749-6632.2010.05752.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Nepiyushchikh ZV, Chakraborty S, Wang W, Davis MJ, Zawieja DC, Muthuchamy M. Differential effects of myosin light chain kinase inhibition on contractility, force development and myosin light chain 20 phosphorylation of rat cervical and thoracic duct lymphatics. The Journal of physiology. 2011;589:5415–29. doi: 10.1113/jphysiol.2011.218446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Somlyo AP, Somlyo AV. Signal transduction and regulation in smooth muscle. Nature. 1994;372:231–6. doi: 10.1038/372231a0. [DOI] [PubMed] [Google Scholar]
- 87.Hosaka K, Mizuno R, Ohhashi T. Rho-Rho kinase pathway is involved in the regulation of myogenic tone and pump activity in isolated lymph vessels. Am J Physiol Heart Circ Physiol. 2003;284:H2015–25. doi: 10.1152/ajpheart.00763.2002. [DOI] [PubMed] [Google Scholar]
- 88.Si YH, Niu CY, Zhao ZG, Zhang LM, Zhang YP. Role of RhoA in regulating the pump function of isolated lymphatics from hemorrhagic shock rats. Shock. 2013;40:49–58. doi: 10.1097/SHK.0b013e31829635cf. [DOI] [PubMed] [Google Scholar]
- 89.Souza-Smith FM, Molina PE, Breslin JW. Reduced RhoA activity mediates acute alcohol intoxication-induced inhibition of lymphatic myogenic constriction despite increased cytosolic [Ca(2+)] Microcirculation. 2013;20:377–84. doi: 10.1111/micc.12032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Kurtz KH, Souza-Smith FM, Moor AN, Breslin JW. Rho kinase enhances contractions of rat mesenteric collecting lymphatics. PLoS One. 2014;9:e94082. doi: 10.1371/journal.pone.0094082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Huggenberger R, Siddiqui SS, Brander D, Ullmann S, Zimmermann K, Antsiferova M, et al. An important role of lymphatic vessel activation in limiting acute inflammation. Blood. 2011;117:4667–78. doi: 10.1182/blood-2010-10-316356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Ji RC. Lymphatic endothelial cells, inflammatory lymphangiogenesis, and prospective players. Current medicinal chemistry. 2007;14:2359–68. doi: 10.2174/092986707781745541. [DOI] [PubMed] [Google Scholar]
- 93.Randolph GJ, Angeli V, Swartz MA. Dendritic-cell trafficking to lymph nodes through lymphatic vessels. Nature reviews Immunology. 2005;5:617–28. doi: 10.1038/nri1670. [DOI] [PubMed] [Google Scholar]
- 94.Benoit JN, Zawieja DC. Effects of f-Met-Leu-Phe-induced inflammation on intestinal lymph flow and lymphatic pump behavior. American Journal of Physiology. 1992;262:G199–202. doi: 10.1152/ajpgi.1992.262.2.G199. [DOI] [PubMed] [Google Scholar]
- 95.Von Der Weid PY, Rehal S. Lymphatic pump function in the inflamed gut. Ann N Y Acad Sci. 2010;1207(Suppl 1):E69–74. doi: 10.1111/j.1749-6632.2010.05715.x. [DOI] [PubMed] [Google Scholar]
- 96.Davis MJ, Lane MM, Davis AM, Durtschi D, Zawieja DC, Muthuchamy M, et al. Modulation of lymphatic muscle contractility by the neuropeptide substance P. Am J Physiol Heart Circ Physiol. 2008;295:H587–97. doi: 10.1152/ajpheart.01029.2007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Chakraborty S, Nepiyushchikh Z, Davis MJ, Zawieja DC, Muthuchamy M. Substance P activates both contractile and inflammatory pathways in lymphatics through the neurokinin receptors NK1R and NK3R. Microcirculation. 2011;18:24–35. doi: 10.1111/j.1549-8719.2010.00064.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Mizuno R, Koller A, Kaley G. Regulation of the vasomotor activity of lymph microvessels by nitric oxide and prostaglandins. American Journal of Physiology. 1998;274:R790–6. doi: 10.1152/ajpregu.1998.274.3.R790. [DOI] [PubMed] [Google Scholar]
- 99.Fukumura D, Kashiwagi S, Jain RK. The role of nitric oxide in tumour progression. Nature reviews Cancer. 2006;6:521–34. doi: 10.1038/nrc1910. [DOI] [PubMed] [Google Scholar]
- 100.Kashiwagi S, Tsukada K, Xu L, Miyazaki J, Kozin SV, Tyrrell JA, et al. Perivascular nitric oxide gradients normalize tumor vasculature. Nat Med. 2008;14:255–7. doi: 10.1038/nm1730. [DOI] [PubMed] [Google Scholar]
- 101.Bohlen HG. Rapid and slow nitric oxide responses during conducted vasodilation in the in vivo intestine and brain cortex microvasculatures. Microcirculation. 2011;18:623–34. doi: 10.1111/j.1549-8719.2011.00127.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Wilson JT, Wang W, Hellerstedt AH, Zawieja DC, Moore JE. Confocal image-based computational modeling of nitric oxide transport in a rat mesenteric lymphatic vessel. Journal of biomechanical engineering. 2013;135:51005. doi: 10.1115/1.4023986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Chakraborty S, W W, Zawieja DC, Muthuchamy M. LPS mediated decreases in immune cells recruitment on or near lymphatics impairs lymphatic contractility. The FASEB Journal. 2013 [Google Scholar]
- 104.Chatterjee V, Gashev AA. Aging-associated shifts in functional status of mast cells located by adult and aged mesenteric lymphatic vessels. Am J Physiol Heart Circ Physiol. 2012;303:H693–702. doi: 10.1152/ajpheart.00378.2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Chatterjee V, Gashev AA. Mast cell-directed recruitment of MHC class II positive cells and eosinophils towards mesenteric lymphatic vessels in adulthood and elderly. Lymphat Res Biol. 2014;12:37–47. doi: 10.1089/lrb.2013.0031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Nizamutdinova IT, Maejima D, Nagai T, Bridenbaugh E, Thangaswamy S, Chatterjee V, et al. Involvement of histamine in endothelium-dependent relaxation of mesenteric lymphatic vessels. Microcirculation. 2014;21:640–8. doi: 10.1111/micc.12143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Kurtz KM, S-S F, Breslin JW. Involvement of NO/sGC, but not ROCK, in histamine-induced collecting lymphatic relaxation. The FASEB Journal. 2013 [Google Scholar]
- 108.Petunov SG, Egorova AA, Orlov RS, Nikitina ER. Effect of histamine on spontaneous contractions of mesenteric lymphatic vessels and lymph nodes of white rats: endothelium-dependent responses. Doklady biological sciences : proceedings of the Academy of Sciences of the USSR, Biological sciences sections / translated from Russian. 2010;432:176–80. doi: 10.1134/S0012496610030038. [DOI] [PubMed] [Google Scholar]
- 109.von der Weid PY, Muthuchamy M. Regulatory mechanisms in lymphatic vessel contraction under normal and inflammatory conditions. Pathophysiology. 2009 doi: 10.1016/j.pathophys.2009.10.005. [DOI] [PubMed] [Google Scholar]
- 110.Cromer WE, Zawieja SD, Tharakan B, Childs EW, Newell MK, Zawieja DC. The effects of inflammatory cytokines on lymphatic endothelial barrier function. Angiogenesis. 2014;17:395–406. doi: 10.1007/s10456-013-9393-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Avraham T, Zampell JC, Yan A, Elhadad S, Weitman ES, Rockson SG, et al. Th2 differentiation is necessary for soft tissue fibrosis and lymphatic dysfunction resulting from lymphedema. FASEB J. 2013;27:1114–26. doi: 10.1096/fj.12-222695. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Aldrich MB, Sevick-Muraca EM. Cytokines are systemic effectors of lymphatic function in acute inflammation. Cytokine. 2013;64:362–9. doi: 10.1016/j.cyto.2013.05.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Zawieja SD, Wang W, Wu X, Nepiyushchikh ZV, Zawieja DC, Muthuchamy M. Impairments in the intrinsic contractility of mesenteric collecting lymphatics in a rat model of metabolic syndrome. American journal of physiology Heart and circulatory physiology. 2012;302:H643–53. doi: 10.1152/ajpheart.00606.2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Cromer WE, Mathis JM, Granger DN, Chaitanya GV, Alexander JS. Role of the endothelium in inflammatory bowel diseases. World J Gastroenterol. 2011;17:578–93. doi: 10.3748/wjg.v17.i5.578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Ezaki T, Baluk P, Thurston G, La Barbara A, Woo C, McDonald DM. Time course of endothelial cell proliferation and microvascular remodeling in chronic inflammation. Am J Pathol. 2001;158:2043–55. doi: 10.1016/S0002-9440(10)64676-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Baluk P, Yao LC, Feng J, Romano T, Jung SS, Schreiter JL, et al. TNF-alpha drives remodeling of blood vessels and lymphatics in sustained airway inflammation in mice. J Clin Invest. 2009;119:2954–64. doi: 10.1172/JCI37626. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Zgraggen S, Ochsenbein AM, Detmar M. An important role of blood and lymphatic vessels in inflammation and allergy. Journal of allergy. 2013;2013:672381. doi: 10.1155/2013/672381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Natali A, Toschi E, Baldeweg S, Ciociaro D, Favilla S, Sacca L, et al. Clustering of insulin resistance with vascular dysfunction and low-grade inflammation in type 2 diabetes. Diabetes. 2006;55:1133–40. doi: 10.2337/diabetes.55.04.06.db05-1076. [DOI] [PubMed] [Google Scholar]
- 119.Blum KS, Karaman S, Proulx ST, Ochsenbein AM, Luciani P, Leroux JC, et al. Chronic high-fat diet impairs collecting lymphatic vessel function in mice. PLoS One. 2014;9:e94713. doi: 10.1371/journal.pone.0094713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Savetsky IL, Torrisi JS, Cuzzone DA, Ghanta S, Albano NJ, Gardenier JC, et al. Obesity increases inflammation and impairs lymphatic function in a mouse model of lymphedema. Am J Physiol Heart Circ Physiol. 2014;307:H165–72. doi: 10.1152/ajpheart.00244.2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Weitman ES, Aschen SZ, Farias-Eisner G, Albano N, Cuzzone DA, Ghanta S, et al. Obesity impairs lymphatic fluid transport and dendritic cell migration to lymph nodes. PLoS One. 2013;8:e70703. doi: 10.1371/journal.pone.0070703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Lim HY, Rutkowski JM, Helft J, Reddy ST, Swartz MA, Randolph GJ, et al. Hypercholesterolemic mice exhibit lymphatic vessel dysfunction and degeneration. Am J Pathol. 2009;175:1328–37. doi: 10.2353/ajpath.2009.080963. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Martel C, Li W, Fulp B, Platt AM, Gautier EL, Westerterp M, et al. Lymphatic vasculature mediates macrophage reverse cholesterol transport in mice. J Clin Invest. 2013;123:1571–9. doi: 10.1172/JCI63685. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Karpanen T, Alitalo K. Molecular biology and pathology of lymphangiogenesis. Annual review of pathology. 2008;3:367–97. doi: 10.1146/annurev.pathmechdis.3.121806.151515. [DOI] [PubMed] [Google Scholar]
- 125.Rockson SG. Lymphedema. Am J Med. 2001;110:288–95. doi: 10.1016/s0002-9343(00)00727-0. [DOI] [PubMed] [Google Scholar]
- 126.Rutkowski JM, Moya M, Johannes J, Goldman J, Swartz MA. Secondary lymphedema in the mouse tail: Lymphatic hyperplasia, VEGF-C upregulation, and the protective role of MMP-9. Microvasc Res. 2006;72:161–71. doi: 10.1016/j.mvr.2006.05.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Zampell JC, Elhadad S, Avraham T, Weitman E, Aschen S, Yan A, et al. Toll-like receptor deficiency worsens inflammation and lymphedema after lymphatic injury. Am J Physiol Cell Physiol. 2012;302:C709–19. doi: 10.1152/ajpcell.00284.2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Zampell JC, Yan A, Avraham T, Andrade V, Malliaris S, Aschen S, et al. Temporal and spatial patterns of endogenous danger signal expression after wound healing and in response to lymphedema. Am J Physiol Cell Physiol. 2011;300:C1107–21. doi: 10.1152/ajpcell.00378.2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Angeli V, Llodra J, Rong JX, Satoh K, Ishii S, Shimizu T, et al. Dyslipidemia associated with atherosclerotic disease systemically alters dendritic cell mobilization. Immunity. 2004;21:561–74. doi: 10.1016/j.immuni.2004.09.003. [DOI] [PubMed] [Google Scholar]
- 130.Chakraborty S, Gurusamy M, Zawieja DC, Muthuchamy M. Lymphatic filariasis: perspectives on lymphatic remodeling and contractile dysfunction in filarial disease pathogenesis. Microcirculation. 2013;20:349–64. doi: 10.1111/micc.12031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Van Kruiningen HJ, Colombel JF. The forgotten role of lymphangitis in Crohn's disease. Gut. 2008;57:1–4. doi: 10.1136/gut.2007.123166. [DOI] [PubMed] [Google Scholar]
- 132.Kovi J, Duong HD, Hoang CT. Ultrastructure of Intestinal Lymphatics in Crohn's Disease. Am J Clin Pathol. 1981;76:385–94. doi: 10.1093/ajcp/76.4.385. [DOI] [PubMed] [Google Scholar]
- 133.Robb-Smith AH. A bird's-eye view of Crohn's disease. Proceedings of the Royal Society of Medicine. 1971;64:157–61. [PMC free article] [PubMed] [Google Scholar]
- 134.von der Weid PY, Rainey KJ. Review article: lymphatic system and associated adipose tissue in the development of inflammatory bowel disease. Alimentary pharmacology & therapeutics. 2010;32:697–711. doi: 10.1111/j.1365-2036.2010.04407.x. [DOI] [PubMed] [Google Scholar]
- 135.Wu TF, Carati CJ, Macnaughton WK, von der Weid PY. Contractile activity of lymphatic vessels is altered in the TNBS model of guinea pig ileitis. Am J Physiol Gastrointest Liver Physiol. 2006;291:G566–74. doi: 10.1152/ajpgi.00058.2006. [DOI] [PubMed] [Google Scholar]
- 136.Akl TJ, Nagai T, Cote GL, Gashev AA. Mesenteric lymph flow in adult and aged rats. Am J Physiol Heart Circ Physiol. 2011;301:H1828–40. doi: 10.1152/ajpheart.00538.2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Gasheva OY, Knippa K, Nepiushchikh ZV, Muthuchamy M, Gashev AA. Age-related alterations of active pumping mechanisms in rat thoracic duct. Microcirculation. 2007;14:827–39. doi: 10.1080/10739680701444065. [DOI] [PubMed] [Google Scholar]
- 138.Gashev AA, Chatterjee V. Aged lymphatic contractility: recent answers and new questions. Lymphat Res Biol. 2013;11:2–13. doi: 10.1089/lrb.2013.0003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Nagai T, Bridenbaugh EA, Gashev AA. Aging-associated alterations in contractility of rat mesenteric lymphatic vessels. Microcirculation. 2011;18:463–73. doi: 10.1111/j.1549-8719.2011.00107.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Bridenbaugh EA, Nizamutdinova IT, Jupiter D, Nagai T, Thangaswamy S, Chatterjee V, et al. Lymphatic muscle cells in rat mesenteric lymphatic vessels of various ages. Lymphat Res Biol. 2013;11:35–42. doi: 10.1089/lrb.2012.0025. [DOI] [PMC free article] [PubMed] [Google Scholar]