Abstract
Context/objective
Traumatic spinal cord injuries (T-SCI) have a devastating impact and place a significant financial burden on the healthcare system. The incidence of T-SCI ranges from 10.4 to 83 cases per million and varies with age, sex, or geographical region. This study describes the epidemiology and demographic characteristics of patients treated for T-SCI in our region over 11 years.
Design
Retrospective cohort study.
Setting
Single Level-I trauma center in Québec, Canada.
Participants
Patients who sustained T-SCI between 1 April 2000 and 31 March 2011.
Interventions
None.
Outcome measures
Data concerning T-SCI patients was retrieved from the Québec Trauma Registry. Information on age, sex, trauma, level of injury, type and severity of neurological deficit (ASIA scale), and treatment was extracted. Annual, age-standardized rates of T-SCI were calculated and trends over time were examined.
Results
Eight hundred and thirty-one patients with T-SCI were identified. The incidence of T-SCI did not change over time but there was a 13-year increase in age between 2002 and 2010. More than 60% of patients aged 55 years or more were injured following a fall and 80% became tetraplegic. These patients were more likely to have central cord syndrome (CCS) and incomplete neurological injury, compared to younger patients. The incidence of CCS increased from 25 to 37% over 11 years.
Conclusions
The T-SCI population is aging and is more frequently sustaining injuries associated with CCS, incomplete neurological deficits and tetraplegia.
Keywords: Central cord syndrome, Epidemiology, Spinal cord injury, Tetraplegia, Trauma
Background
Traumatic spinal cord injuries (T-SCI) are relatively rare but second only to traumatic brain injury for burden of injury and years lived with disability.1 T-SCI typically affects young males and can have a devastating physical and psychological impact. T-SCI leads to decreased quality of life, social participation, and productivity as well as significant financial burden. Costs of T-SCI to society were estimated in 2006 at 9.7 billion United States Dollars (USD) per year in the USA. Individuals with tetraplegia cost three times more (874 000 USD) than individuals with incomplete motor function (246 000 USD)2 and continue to incur costs of 28 000 USD per year beyond the acute injury phase.3 In Canada, attributable costs in the first year after T-SCI were estimated at 122 900 Canadian Dollars (CAD) (in 2002; 78 262 USD) for a complete lesion and 43 400 CAD (27 637 USD) for an incomplete lesion,4 with a mean acute hospitalization cost of more than 24 000 CAD in Québec (15 283 USD).5 In the 5 years following injury, annual costs were 6400 CAD (4075 USD) and 3800 CAD (2420 USD) for complete and incomplete lesions, respectively, as compared to yearly healthcare costs for the general population ranging between 1000 and 1300 CAD (637–828 USD).4
The worldwide estimated incidence of T-SCI varies from 10.4 to 83 cases per million,6 variability being due to regional differences in motor vehicle use and legislation, developing vs. developed countries,7 and trends over time. Developed nations (Iceland,8 France,9 USA,10 South Korea,11 Netherlands, Ireland, Portugal, Australia12) have reported that the average age of T-SCI is increasing, as well as the rate of T-SCI due to simple falls. The mortality rate for individuals with T-SCI in developed nations is half the rate in developing nations.5,13 This increasing survivability and increasing age of individuals with T-SCI will pose significant financial burdens to healthcare systems.14
The aging of the T-SCI population also impacts the type of neurological injury. Central cord syndrome (CCS) is an incomplete neurological injury that occurs following hyperextension of the cervical spine with a small spinal canal, secondary to other conditions such as spondylosis and cervical stenosis. Affected individuals are typically older and have no overt spinal instability but present a spectrum of neurological injury ranging from mild hand numbness to tetraplegia. The upper limbs are more affected than the lower limbs and hand function impairment is a significant long-term disability.15,16 Although cost estimates have not addressed CCS specifically, incomplete cervical SCI has been shown to be the most costly of all types of T-SCI (4.78 million USD for incomplete cervical SCI (most) vs. 0.16 million USD for complete lumbar SCI (least)).3 Due to the aging population and the relatively low-velocity injuries that lead to CCS, we believe that CCS is an important and increasing subset of T-SCI. In addition, the prognosis of CCS is generally good and differs from that of incomplete T-SCI overall (when adjusted for age). CCS is therefore presented and analyzed separately from T-SCI overall in this study.15,16
The Canadian age-adjusted incidence of T-SCI is higher for individuals older than 64 years (51.4 cases per million) than for individuals aged between 15 and 64 years (42.4 cases per million),17 and is variable regionally (24.0–50.9 cases per million in Ontario,13,18 52.5 cases per million in Alberta,19 and 35.7 cases per million in British Columbia).20 Specifically, Lenehan et al.20 have reported two peaks in the T-SCI incidence in British Columbia, the second one being observed in individuals aged 55 years or older. The incidence of CCS in these populations was however not specifically studied.
The purpose of this study was to describe the epidemiology and demographic characteristics of individuals with T-SCI in the province of Québec, Canada. Due to the previously discussed worldwide and Canadian trends of increasing age, increasing incidence of CCS, decreasing velocity of trauma, and decreasing mortality, we hypothesized that Québec would show similar trends and focused on these comparisons. We also hypothesized that CCS would occur more often in older individuals due to low-velocity trauma and that this was partially responsible for the aging of the T-SCI population overall. To address these hypotheses, 11 consecutive years (1 April 2000 to 31 March 2011) of registry data were used. To address more specifically the demographic and clinical differences of individuals with T-SCI with respect to age, two age groups were compared: <55-years-old and ≥55-years-old. Examining trends in T-SCI over time may aid the development of treatment or prevention programs for this challenging population.
Methods
All individuals with acute T-SCI admitted to our hospital between 1 April 2000 and 31 March 2011 were included in this retrospective study. Please note for clarity purposes that when referring to year 2000, we are including data collected between 1 April 2000 and 31 March 2001, and so on until year 2010, which refers to data between 1 April 2010 and 31 March 2011. Our level-1 trauma center is one of two Centers of Expertise for Spinal Cord Injuries (CEBMOQ) in Québec21 and serves as the tertiary referral center for T-SCI in western Québec (60% of Québec's population) and as the single referral center for all ventilation-assisted T-SCI in Québec.
Individuals with T-SCI were identified using the prospective Québec Trauma Registry (QTR), which includes all patients treated for a traumatic injury in Québec. This administrative database managed by the Québec Health Ministry provides information on individuals who are treated in a healthcare facility following any trauma causing associated injuries. It contains data on the traumatic event, facilities and emergencies that provided care, hospital stay, medical examination, interventions, complications and injuries caused by the traumatic event, and does not involve any follow-up after discharge. All individuals who sustain a trauma with injuries and that died prior to or during hospitalization, or that were admitted and treated in a designated trauma center in the province or Québec are automatically included in the QTR. Data are collected on all patients who were admitted following trauma by medical archivists on a daily basis, and stored in the local computer system. Thus, individuals with T-SCI who were admitted to our facility were identified using the local portion of the QTR.
Cases were identified using the International Classification of Diseases, Ninth Revision codes 806.X (SCI with vertebral fracture) and 952.X (SCI without evidence of spinal bone injury) as well as the International Classification of Diseases, Tenth Revision codes S14.X, S24.X, and S34.X. Individuals were included in the study if they sustained a T-SCI involving the bony levels between C1 and L2. Injuries below L2 were excluded to avoid neurological syndromes distal to the spinal cord. Data from the QTR were supplemented by manual chart review and institutional review board approval was obtained.
The information obtained from our local portion of the QTR included age, sex, etiology of trauma (sporting accident, fall, motor vehicle accident (MVA), violent event, other), level of injury (cervical, thoracic, lumbar), diagnosis (associated spinal fracture or not), occurrence of CCS, severity of neurological deficit pre-operatively (ASIA Impairment Scale or AIS grade: A, B, C, or D), and Injury Severity Score (ISS). Annual, age-standardized incidence of T-SCI was calculated for western Québec using its total population for years 2000–2010.
Statistical analysis was performed using Statistica V7.1 software (Statsoft; Tulsa, OK, USA). T-SCI individuals were separated in two age groups (young: <55-years-old; old: ≥55-years-old) that were based on the second peak in T-SCI occurrence for individuals aged 55 years or older found by Lenehan et al.20 Annual incidence was calculated using the absolute number of individuals with a T-SCI per year divided by the population of the area served by our facility, which represents ∼60% of the total population of the province of Québec. Age-standardized incidence used the population of the western portion of Québec for each age group (<55-years-old; ≥55-years-old). Mortality rate was computed using the number of individuals who died after their T-SCI, either prior to being transferred to our facility, or during hospitalization, divided by the total number of individuals with acute T-SCI. Descriptive statistics were reported using means and standard deviations for continuous data, and ratios or proportions for categorical data. Demographic trends and relationships over the 2000–2010 period were tested using the χ2 test and the Spearman's rank-order correlation test. The strength of association between age groups, sex, etiology of trauma, ASIA grade, diagnosis, the presence or absence of CCS, and mortality rate were also tested using the χ2 and Spearman's rank-order correlation tests. Variations in continuous data (age, ISS) across time were analyzed using one-way analysis of variances and Student's t-tests were used when those variables were dichotomized with respect to study periods, age groups, or occurrence of a CCS diagnosis. Associations and differences were considered significant when P < 0.05.
Results
Demographics and annual incidence
Eight hundred and thirty-one patients with T-SCI were identified. The demographics and details regarding the T-SCI of this sample are presented in Table 1.
Table 1 .
Demography and clinical characteristics of T-SCI in Québec, Canada from 2000 to 2010
| Year | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Overall | 2000 | 2001 | 2002 | 2003 | 2004 | 2005 | 2006 | 2007 | 2008 | 2009 | 2010 | |
| Number of T-SCI cases | 831 | 46 | 54 | 61 | 53 | 100 | 101 | 79 | 93 | 81 | 80 | 83 |
| Incidence (cases per million) | ||||||||||||
| Global population | 16.9 | 10.6 | 12.4 | 13.9 | 12.0 | 22.5 | 22.6 | 17.6 | 20.5 | 17.7 | 17.3 | 17.8 |
| < 55 y.o. | 16.1 | 9.8 | 13.0 | 16.1 | 13.0 | 20.8 | 21.7 | 17.9 | 19.8 | 14.7 | 16.8 | 13.3 |
| ≥ 55 y.o. | 18.9 | 12.4 | 10.9 | 8.2 | 9.6 | 26.7 | 24.7 | 16.6 | 22.3 | 24.7 | 18.5 | 27.8 |
| Age | ||||||||||||
| Mean (SD) | 46.2 (19.2) | 47.8 (17.9) | 42.1 (18.9) | 39.1 (15.9) | 41.0 (16.0) | 45.7 (18.5) | 46.5 (20.6) | 45.8 (19.9) | 46.7 (19.4) | 50.1 (19.4) | 46.4 (20.0) | 52.1 (19.0) |
| Sex | ||||||||||||
| Male (%) | 79.8 | 80.4 | 77.8 | 82.0 | 75.5 | 82.0 | 83.2 | 79.7 | 80.6 | 72.8 | 81.3 | 79.5 |
| ISS | ||||||||||||
| Mean (SD) | 24.2 (11.3) | 27.8 (13.0) | 24.9 (12.9) | 24.4 (12.7) | 23.3 (11.2) | 23.8 (11.1) | 22.7 (9.7) | 23.0 (9.9) | 26.1 (12.3) | 24.6 (10.6) | 22.0 (7.7) | 25.6 (13.1) |
| Etiology of trauma | ||||||||||||
| Sports (%) | 11.6 | 2.2 | 5.6 | 9.8 | 18.9 | 13.0 | 13.9 | 15.2 | 14.0 | 12.3 | 8.8 | 8.4 |
| Fall (%) | 35.0 | 41.3 | 29.6 | 34.4 | 32.1 | 34.0 | 31.7 | 32.9 | 26.9 | 38.3 | 38.8 | 47.0 |
| MVA (%) | 41.5 | 41.3 | 46.3 | 44.3 | 37.7 | 38.0 | 42.6 | 39.2 | 49.5 | 37.0 | 42.5 | 38.6 |
| Violence (%) | 4.8 | 6.5 | 7.4 | 3.3 | 7.5 | 4.0 | 5.9 | 1.3 | 7.5 | 1.2 | 6.3 | 3.6 |
| Other (%) | 7.1 | 8.7 | 11.1 | 8.2 | 3.8 | 11.0 | 5.9 | 11.4 | 2.2 | 11.1 | 3.8 | 2.4 |
| Injury level | ||||||||||||
| Cervical (%) | 63.4 | 56.5 | 63.0 | 57.4 | 56.6 | 65.0 | 71.3 | 64.6 | 54.8 | 66.7 | 65.0 | 68.7 |
| Thoracic (%) | 26.5 | 30.4 | 25.9 | 32.8 | 30.2 | 26.0 | 14.9 | 30.4 | 33.3 | 25.9 | 22.5 | 25.3 |
| Lumbar (%) | 10.1 | 13.0 | 11.1 | 9.8 | 13.2 | 9.0 | 13.9 | 5.1 | 11.8 | 7.4 | 12.5 | 6.0 |
| ASIA grade | ||||||||||||
| A (%) | 33.1 | 45.7 | 37.0 | 37.7 | 35.9 | 37.0 | 23.8 | 31.7 | 43.0 | 25.9 | 20.0 | 34.9 |
| B (%) | 13.0 | 15.2 | 16.7 | 11.5 | 9.4 | 11.0 | 12.9 | 13.9 | 11.8 | 18.5 | 12.5 | 10.8 |
| C (%) | 18.3 | 10.9 | 22.2 | 14.8 | 20.8 | 22.0 | 20.8 | 17.7 | 12.9 | 18.5 | 21.3 | 16.9 |
| D (%) | 35.3 | 23.9 | 22.2 | 36.1 | 34.0 | 30.0 | 42.6 | 36.7 | 32.3 | 37.0 | 46.3 | 37.4 |
| Paraplegia or tetraplegia | ||||||||||||
| Tetraplegia (%) | 63.9 | 58.7 | 61.1 | 55.7 | 56.6 | 64.0 | 73.3 | 65.8 | 55.9 | 66.7 | 66.3 | 69.9 |
| Diagnosis | ||||||||||||
| Occurrence of CCS (%) | 29.1 | 26.1 | 24.1 | 24.6 | 22.6 | 22.0 | 35.7 | 29.1 | 24.7 | 30.9 | 37.5 | 37.4 |
| Mortality rate | ||||||||||||
| Deceased patients (%) | 6.1 | 13.0 | 7.4 | 8.2 | 1.9 | 4.0 | 9.9 | 3.8 | 4.3 | 4.9 | 6.3 | 6.0 |
T-SCI, traumatic spinal cord injury; y.o., years old; SD, standard deviation; MVA, motor vehicle accident.
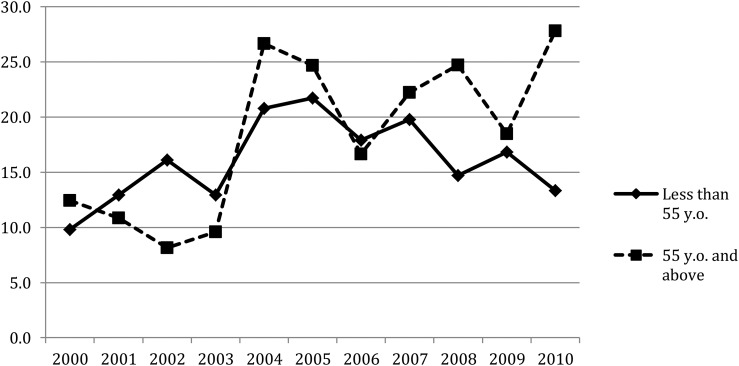
The absolute number of T-SCI cases ranged between 46 and 101, for an annual average of 76 cases. The population of western Québec increased from 4.3 to 4.6 million between 2000 and 201020 and represents ∼60% of the total population of Québec. This resulted in an annual incidence of T-SCI ranging from 10.6 cases per million in 2000 (95% confidence interval (CI): 7.5–13.7) to 22.6 cases per million in 2005 (95% CI: 18.2–27.0). The age-standardized annual incidence of T-SCI remained constant between 2000 and 2010. In individuals aged <55-years-old, the incidence of T-SCI ranged from 9.8 cases per million in 2000 (95% CI: 6.3–13.3) to 21.7 cases per million in 2005 (95% CI: 16.6–26.9); in individuals aged ≥55-years-old, it varied between 8.2 cases per million in 2002 (95% CI: 3.1–13.2) and 27.8 cases per million in 2010 (95% CI: 19.2–36.4) (Table 1). The incidence of T-SCI for individuals aged ≥55-years-old was less than their younger counterparts before 2004 but beyond 2004 this trend reversed and people aged ≥55-years-old became the population most frequently affected by T-SCI, with the exception of year 2006, where the incidences in both groups were fairly similar (<55-years-old: 17.9 cases per million; ≥55-years-old: 16.7 cases per million) (Fig. 1).
Figure 1 .
Annual incidence of T-SCI referred to our Center in Québec, Canada. Figure showing the variation over time of the incidence (in cases per million population) of T-SCI in Québec, Canada from 2000 to 2010. Two groups are represented: individuals aged <55-years-old (diamonds) and individuals ≥55-years-old (squares) with the older group becoming more frequently affected by T-SCI over time.
The mean age of individuals with T-SCI is also increasing in time (F(10,820) = 2,89; P = 0.001). In 2002, the average age was 39.1 ± 15.9 years old and increased to 52.1 ± 19.0 years old in 2010. More than half of the entire study population was aged ≥55-years-old and a breakdown of the 11-year period in two intervals where the cut-off corresponds to the year where the incidence of T-SCI in individuals aged ≥55-years-old becomes greater than in individuals <55-years-old (i.e. 2000–2003 vs. 2004–2010), also confirmed that the T-SCI population in Québec is aging (2000–2003: 43.3 ± 17.8 years old; 2004–2010: 48.0 ± 19.8 years old; t(829) = −3.43; P < 10−3).
T-SCI occurred more frequently in males than females (χ2(1,831) = 161.2; P < 10−3), and the ratio ranged between 2.7:1 and 4.6:1 (men:women) over the 11-year period. Along the same lines, no differences were seen in the sex-standardized incidence rate. The proportion of men sustaining a T-SCI was always much higher than the proportion of women; this discrepancy between sexes did not change over time.
Etiology of trauma
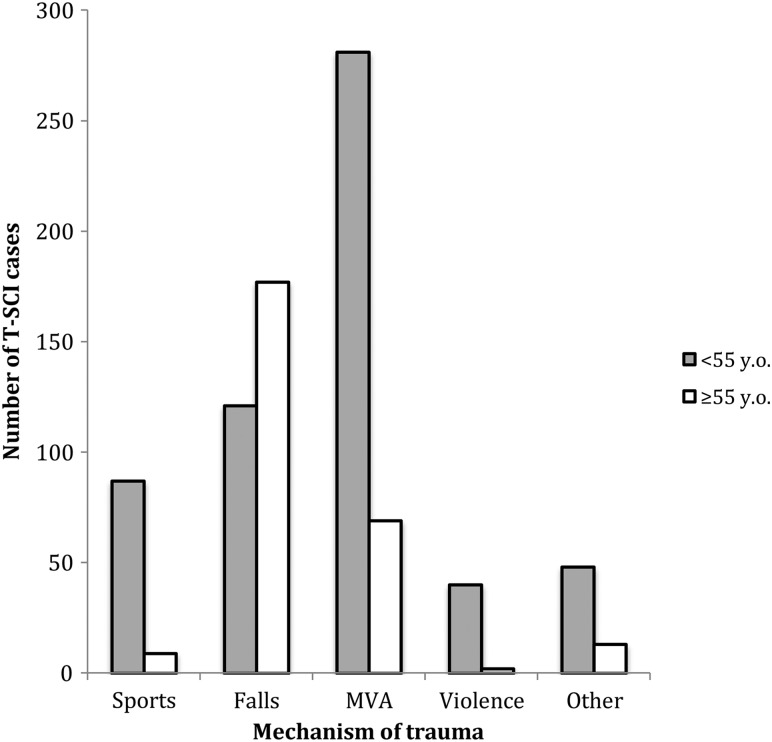
We identified four major causes of T-SCI: sports, falls (from standing height, stairs, etc.), MVA, and violent events (suicide attempts, assaults, etc.). A fifth category, “other causes”, included all cases not easily classified (falling objects, crush injuries, electrocution, etc.). Accidental falls and MVA were responsible for over 75% of cases of T-SCI and there were no significant differences in trauma etiology over time (2000–2010; χ2(40,831) = 48.25; P = 0.17). The age of T-SCI individuals was significantly correlated with trauma etiology (χ2(4,831) = 168.91; P < 10−3), with 80% of all MVA, 90.6% of sporting accidents, and 95.0% of violent events occurring in younger individuals (<55-years-old). In contrast, 60.5% of T-SCI due to accidental falls occurred in older individuals (≥55-years-old). Sex did not affect the etiology of T-SCI (Fig. 2).
Figure 2 .
Etiology of T-SCI according to age group. Figure demonstrating the varying etiology of T-SCI according to age (<55-years-old = gray, ≥55-years-old = white). MVA, motor vehicle accident.
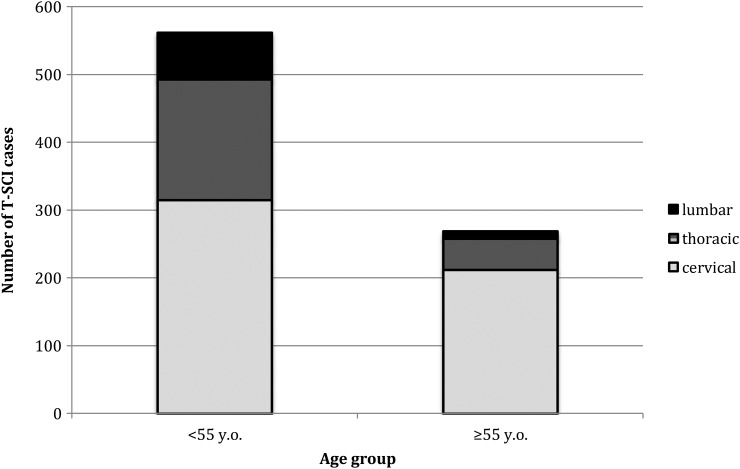
Level of injury
At the cervical level (C1–C7), 63.4% of injuries were observed. Thoracic and lumbar injuries accounted for 26.5 and 10.1% of all T-SCI, respectively. The level of T-SCI remained constant across the 2000–2010 period except for a trend towards more cervical trauma at the decade's end. The level of T-SCI was significantly related to age (χ2(2, 831) = 59.97; P < 10−3; Fig. 3), but not to sex. Individuals aged ≥55-years-old sustained cervical T-SCI more often than individuals <55-years-old (78.8 and 56.1% for patients ≥55-years-old and <55-years-old, respectively). Thoracic and lumbar T-SCI were proportionally greater in individuals aged <55-years-old (79.5% of thoracic injuries; 85.7% of lumbar injuries) than in individuals ≥55-years-old (20.5% of thoracic and 14.3% of lumbar injuries). Consistent with the level of injury, paraplegia and tetraplegia were also related to age (χ2(1,831) = 46.51; P < 10−3). Individuals <55-years-old were more frequently paraplegic whereas individuals aged ≥55-years-old were more frequently tetraplegic (79.6%). In addition, many tetraplegic individuals were diagnosed with CCS, which is expected to be more frequent in the older population.
Figure 3 .
Level of SCI (cervical, thoracic, or lumbar) as a function of age. Figure illustrating the proportion of cervical (gray), thoracic (horizontal bars), and lumbar (black) levels of SCI according to age. On the left is the younger population (<55 years) and on the right is the older population (≥55 years), showing an increased proportion of cervical-level injuries with increasing age.
Diagnosis and incidence of CCS
Individuals with a diagnosis of CCS were separated out from the T-SCI population and trends over time were analyzed. Spearman's correlation test revealed a statistically significant increase in the proportion of individuals with T-SCI diagnosed with CCS over time. This proportion increased from 25.0% in 2000 to 37.4% in 2010 (rs = 0.09; P = 0.006). When the analysis is performed over the time periods of 2000–2003 and 2004–2010, there is a clear and significant increase in CCS in the last portion of the decade (23% in 2000–2003 and 32% in 2004–2010; χ2(1,831) = 7.95; P < 10−2).
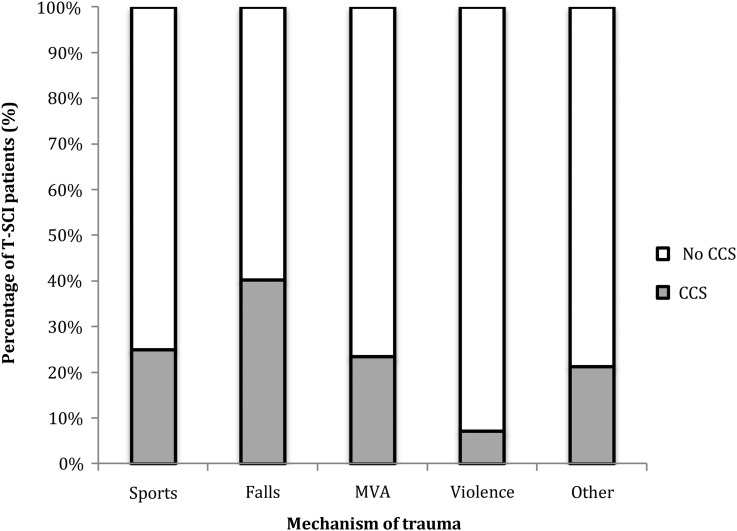
There also exists a relationship between the occurrence of CCS and the age of individuals with T-SCI (χ2(1,831) = 86.12; P < 10−3). Fifty percent of individuals aged ≥55-years-old had CCS, compared to only 19% of individuals younger than 55-years-old. In addition, individuals with CCS were on average 15.7 years older than other individuals with T-SCI (57.2 ± 18.2 years old vs. 41.5 ± 17.7 years old; t(829) = − 11.3; P < 10−3). The occurrence of CCS diagnosis was related to sex, where females were diagnosed with CCS in 33% of the cases as compared to 21% of males with a T-SCI (χ2(1, 831) = 8.68; P < 10−2). Nearly half (49.8%) of individuals with CCS were injured following a simple fall, whereas falls were responsible of 29% of other T-SCI not associated with a CCS. This difference was statistically significant (χ2(4, 831) = 36.00; P < 10−3; Fig. 4).
Figure 4 .
Percentage of individuals with T-SCI who sustain CCS: a breakdown by etiology of trauma. The percentage of individuals with CCS (in gray) is expressed as part of the whole T-SCI (in white) population and divided according to etiology of trauma. The proportion of individuals with CCS clearly varies according to trauma etiology and simple falls incur the highest risk of CCS.
Severity of neurological deficit
The severity of neurological deficits after T-SCI, as described by the AIS grade, changed slightly but significantly between 2000 and 2010 (Table 1). The proportion of incomplete injuries (AIS B, C, D) increased as of 2005, while the proportion of complete injuries (AIS A) decreased (χ2(1, 831) = 4.31; P = 0.04). AIS grade was associated with age, where individuals aged ≥55-years-old suffered significantly more incomplete injuries than their younger counterparts (81.0 vs. 59.9% for ≥55-years-old and <55-years-old, respectively; χ2(1, 831) = 38.53; P < 10−3) regardless of time period. The less severe incomplete injuries (AIS C, D) were also significantly more frequent in older individuals (≥55 years: 69.5%; <55 years: 46.2%; χ2(3, 831) = 57.64; P < 10−3). Women sustained a greater proportion of incomplete T-SCI than men (females: 76.5%; males: 65.3%; χ2(1, 831) = 6.83; P < 10−2).
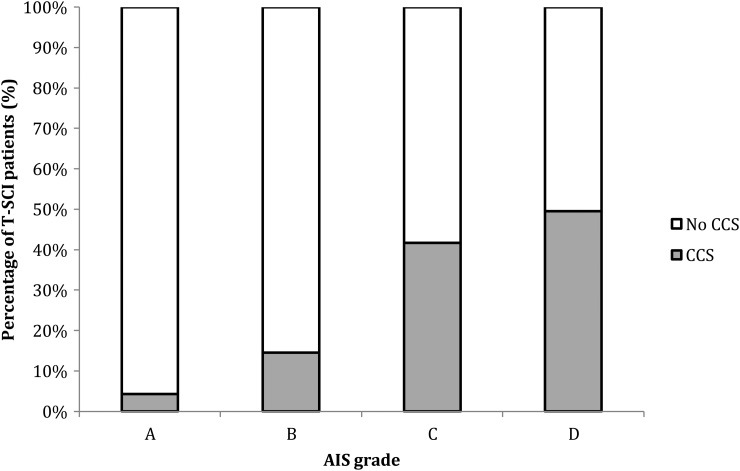
The severity of neurological deficits was inversely related to the occurrence of CCS (χ2(3, 831) = 167.71; P < 10−3). Only 5.0% of T-SCI individuals diagnosed with CCS had complete neurological injuries (AIS A), whereas 61.6% of individuals with CCS were graded as mild neurological impairment (AIS D) at their initial evaluation. If this is compared to individuals who did not receive a diagnosis of CCS, 44.9% presented with complete (AIS A) neurological injuries and only 24.6% presented with mild deficits (AIS D) (Fig. 5).
Figure 5 .
Severity of neurological deficit in individuals with T-SCI who sustain CCS: a breakdown by ASIA grade. The percentage of individuals with CCS (in gray) is expressed as part of the whole T-SCI (in white) population and divided according to severity of neurological deficit. Four grades of neurological deficit according to the ASIA (American Spine Injury Association) scale are shown: A – complete neurological deficit; B–D – incomplete neurological deficits in decreasing severity.
Injury severity score
The average ISS in the T-SCI population remained stable over time (22.0 ± 7.7 in 2009 to 27.8 ± 13.0 in 2000). Individuals aged <55-years-old had significantly greater ISS (25.9 ± 12.3) than individuals aged ≥55-years-old (20.9 ± 7.7; t(829) = 6.04; P < 10−3), suggesting that the latter sustained T-SCI following less significant trauma. In addition, individuals with CCS had significantly lower ISS (19.1 ± 8.0) than individuals without CCS (26.4 ± 11.8; t(829) = 8.80; P < 10−3). This is consistent with both the older age of individuals with CCS and the increased incidence of CCS following falls.
Mortality rate
The mortality rate did not vary significantly over time, with the absolute number of deaths following T-SCI ranging between 1 (in 2003) and 10 (in 2005). However, mortality rate was significantly related to age. Individuals <55-years-old had a lower rate (2.5%) than individuals aged ≥55-years-old (13.8%; χ2(1, 831) = 40.71; P < 10−3). Mortality was not related to the occurrence of CCS.
Discussion
In this study, we have described the demographics and evolving patterns of T-SCI in the western region of Québec, Canada using a cohort of 831 patients over an 11-year period. The incidence varied between 10.6 and 22.6 per million per year and this falls within the range reported worldwide (10.4–83 per million per year),5 though it is slightly less than the Canadian average (23.1–51.4 cases per million per year).17–20 Although our referral base for T-SCI in western Québec represents only 60% of the entire population of Québec21 (100% of ventilator-assisted T-SCI), we assume that this is representative of the whole population of Québec. Indeed, a previous report comparing the demographics of individuals with T-SCI in our institution with the other specialized SCI center in Québec showed similar trends in age, sex, etiology of trauma, and neurological lesions.22 Although our healthcare facility is the tertiary referral center for T-SCI, some individuals are still treated in other institutions. Data obtained through the main rehabilitation center where T-SCI patients are transferred upon discharge showed that the number of individuals not managed at our trauma center following their spine injury ranged from 15 to 38 per year, between 2005 and 2010. When including those patients in the calculation of incidences for years 2005–2010, incidences increase by approximately five cases per million per year, which is more comparable to the Canadian values. Another factor that could explain the lower incidences in the current study is that patients with T-SCI who died prior to hospital admission and patients with cauda equina syndrome were excluded.
Not surprisingly, T-SCI was more common in males in our study with a ratio between 2.7 and 4.6:1(male:female). This was consistent with ratios reported internationally (2–6.7:1)5,6,8,9,11 and nationally (2.5–4.4:1)17–20 and did not change over time.
Of particular interest is the evolution in the demographics of patients with T-SCI over time, as well as the increasing proportion of T-SCI injuries associated with a CCS diagnosis. The median age in our study was 44.8 years and this is greater than the 35-year median age reported in Lenehan's (1995–2004; British Columbia, Canada)20 and Dryden's (1997–2000; Alberta, Canada)19 studies. This increase in age may reflect the later period of our study (2000–2011 vs. 1995–2004) and the continuing aging of the T-SCI population. In Québec, individuals with T-SCI were 13 years older (on average) in 2010 as compared to 2002, which is consistent with Couris’ study (2003–2006; Ontario, Canada). This study was later than Lenehan's and Dryden's studies and reported a stable and somewhat older mean age of 50.5–52.5 years.18 Unfortunately, median age was not reported in Couris’ study, which may limit meaningful comparisons.
Previous studies have suggested that the rate of T-SCI due to falls is increasing over time.9,10 This was not the case in our study, nor in previous Canadian studies, as MVA remains the leading cause of T-SCI when individuals of all ages are considered.17–20 MVA and falls are consistently the top two causes of T-SCI6,11,13 and this was demonstrated in our, and other Canadian, studies.17–20 Although the incidence of T-SCI resulting from MVA did not change over time, the incidence of severe injury of any type resulting from MVA has declined from 2000 to 2010.23 It is likely that improved security measures (newer vehicles) and reinforcement of road safety laws (decreased rate of severe injuries overall) may have contributed to the parallel decline in the severity of T-SCI. In May 2000, the SAAQ (Québec Automobile Association) noted that 41% of all road accident mortality was due to motorcycle use and that the victims were mostly new drivers. They instituted a series of policies limiting access to motorcycle driving permits. In addition, in 2000 they launched a collaborative 5-year road safety plan with the goal of reducing mortality and severe injury by 15%. This was a continuation and improvement upon their 1995–2000 4-facet plan (addressed Human, Vehicle, Road Environment, and Socioeconomic Environment issues) that reduced mortality by 18% and severe injury by 16%.24,25
Mortality due to road injury has been progressively declining in Québec since the 1980s. However, for reasons that are unclear, severe and minor injuries due to road accidents increased from 2000 to 2005 (minor peak in 2007) but have been decreasing since.26 This may help explain the peak in T-SCI seen in 2005 in our study in both younger and older populations (Fig. 1) with a gradual decline afterwards. T-SCI in the younger population of our study continues to decline steadily after 2005 but increases in the older population. We believe this is due to the overall aging of the T-SCI population and injuries due to simple falls, which would not be addressed by road safety legislature.
T-SCI due to falls were significantly more frequent in older individuals (≥ 55 years) in our, and in other Canadian, studies.17–20 With the increasing age of individuals with T-SCI, it is likely that falls will become a more important cause of T-SCI in the future. The population of Québec is aging overall,27 which helps to explain the increase in T-SCI in older individuals. The population is expected to continue to age and we believe that individuals with T-SCI will continue to age in parallel. It is therefore important to assess fall risk in individuals that are 55-years-old and older.
As reported above, the proportion of older individuals suffering T-SCI is increasing over time, as well as the proportion of individuals suffering CCS. Older individuals are suffering a greater percentage of cervical injuries (78.8%) than their younger counterparts (56.1%) and there is a trend of increasing cervical injury incidence over time. Correspondingly, older individuals are more frequently tetraplegic (79.6%) and have a higher incidence of CCS (50.0% ≥55 years vs. 19.0% <55 years). Consistent with the large percentage of cervical injuries in the older portion of T-SCI population, the incidence of CCS has also increased significantly (23.0% in 2000–2004; 32.0% in 2005–2010). This rate of CCS is less than what was found by Pickett et al.17 in Ontario (35%) and was not reported in the other three Canadian studies.
Along the same lines, the incidence of incomplete neurological injury also increased over time, while the incidence of complete injury correspondingly decreased. Older individuals suffered more incomplete neurological deficits than younger individuals (≥55 years: 81.0%; <55 years: 59.9%), which is consistent with the lower severity of trauma sustained by this population, as measured by the ISS (≥55 years: 20.9 ± 7.7; <55 years: 25.9 ± 12.3). Sixty-one percent of individuals with CCS were graded as AIS D at the time of their primary evaluation but this may underestimate the impact of upper extremity deficits, in particular manual dexterity. The AIS was not designed to evaluate fine motor function and CCS is acknowledged as separate “clinical syndrome” from the standard AIS B–D incomplete SCI. These results are also limited by the broad and often debated definition of CCS.14,15 In our study, we restricted the definition of CCS to the “classic” hyperextension injury with pre-existing spondylotic pathology (reduced spinal canal diameter) and typical neurological findings. Considering that CCS mainly affects individuals older than 55 years, a proper neurological assessment to rule out subtle signs/symptoms of myelopathy from cervical spondylosis may also be relevant when evaluating these individuals for fall risk.
Finally, the mortality rate found in this study was stable over time and comparable to the rest of Canada (Alberta: 7.7%,19 British Columbia: 3.1%,20 and Ontario: 8–11.6%17,18). As reported by Lenehan et al.20 and Pickett et al.,17 mortality was significantly related to age (<55 years: 2.5%; ≥55 years; 13.8%). This is likely due to a higher incidence of comorbidities, complications, and lower reserve in the older population. In addition, it is possible that in the presence of a severe neurological deficit, older individuals are less likely to accept active treatment such as sustained mechanical ventilation, particularly in the face of multiple or severe complications.
One limitation of this study is the lack of cost analysis. Although incomplete cervical T-SCI has been shown to be the most costly of the T-SCI subtypes,3 this previous cost analysis cannot be directly applied to the CCS subtype. In addition, while the database is prospective, the analyses were performed retrospectively and this may contribute to bias or statistical error. Finally, the use of 55 years as the cut-off for “older” vs. “younger” populations was based on previous studies on T-SCI and was chosen to facilitate comparisons between studies. The true definition of “old” is likely the result of a combination of physiological factors (including incidence of spinal stenosis) and may be higher or lower than 55 years.
Conclusion
This study presented the demographics and epidemiology of T-SCI in Québec from 2000 to 2010. The incidence of T-SCI (10.6–22.6 per million per year) is comparable to previously published data. T-SCI occurs more often in males with a ratio of 2.7–4.6:1 over the 11-year period.
People with T-SCI in Québec are getting older. These older individuals (≥55 years) are most frequently sustaining their injury following simple falls and are at increased risk of cervical injury (78.8%) and tetraplegia (79.6%). Fully half of individuals aged 55 years or more are diagnosed with CCS and over 61% of individuals with CCS have mild neurological deficits (AIS D). However, functional hand impairment may be experienced by 23–57% of individuals.14 Understanding the evolving epidemiology of T-SCI can be helpful for healthcare resource planning and preventative strategies.
Disclaimer statements
Contributors All authors have contributed to the analysis and writing of the manuscript. CT – study design, data collection, data analysis, data interpretation, literature search, and writing of the article. JM – study design, data collection, data interpretation, literature search, writing, and critical revision of the article. SP – study design and critical revision of the article. J-MM-T – study design, literature search, and critical revision of the article.
Conflicts of interest None.
Ethics approval The study presented has received ethical approval by the institutional ethics committee of the Hôpital Sacré-Coeur de Montréal.
Funding This study has been supported by the Fonds de recherche du Québec-Santé; Fonds de recherche et d'éducation en orthopédie de l'Université de Montréal.
References
- 1.Polinder S, Meerding WJ, Mulder S, Petridou E, van Beeck E, EUROCOST Reference Group. Assessing the burden of injury in six European countries. Bull World Health Organ 2007;85(1):27–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Garcia-Altes A, Perez K, Novoa A, Suelves JM, Bernabeu M, Vidal J, et al. . Spinal cord injury and traumatic brain injury: a cost-of-illness study. Neuroepidemiology 2012;39(2):103–8. [DOI] [PubMed] [Google Scholar]
- 3.French DD, Campbell RR, Sabharwal S, Nelson AL, Palacios PA, Gavin-Dreschnack D. Health care costs for patients with chronic spinal cord injury in the Veterans Health Administration. J Spinal Cord Med 2007;30(5):477–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Dryden DM, Saunders LD, Jacobs P, Schopflocher DP, Rowe BH, May LA, et al. . Direct health care costs after traumatic spinal cord injury. J Trauma 2005;59(2):441–7. [DOI] [PubMed] [Google Scholar]
- 5.Mac-Thiong JM, Feldman DE, Thompson C, Bourassa-Moreau E, Parent S. Does timing of surgery affect hospitalisation costs and length of stay for acute care following a traumatic spinal cord injury? J Neurotrauma 2012;29(81):2816–22. [DOI] [PubMed] [Google Scholar]
- 6.Wyndaele M, Wyndaele JJ. Incidence, prevalence and epidemiology of spinal cord injury: what learns a worldwide literature survey? Spinal Cord 2006;44(9):523–9. [DOI] [PubMed] [Google Scholar]
- 7.Chiu W-T, Lin H-C, Lam C, Chu SF, Chiang YH, Tsai SH. Review: epidemiology of traumatic spinal cord injury: comparisons between developed and developing countries. Asia Pac J Public Health 2010;22(1):9–18. [DOI] [PubMed] [Google Scholar]
- 8.Knutsdottir S, Thorisdottir H, Sigvaldason K, Jonsson H Jr, Bjornsson A, Ingvarsson P. Epidemiology of traumatic spinal cord injuries in Iceland from 1975 to 2009. Spinal Cord 2012;50(2):123–6. [DOI] [PubMed] [Google Scholar]
- 9.Lieutaud T, Ndiaye A, Laumon B, Chiron M. Spinal cord injuries sustained in road crashes are not on the decrease in France: a study based on epidemiological trends. J Neurotrauma 2012;29(3):479–87. [DOI] [PubMed] [Google Scholar]
- 10.DeVivo MJ. Epidemiology of traumatic spinal cord injury: trends and future implications. Spinal Cord 2012;50(5):365–72. [DOI] [PubMed] [Google Scholar]
- 11.Shin JC, Kim DH, Yu SJ, Yang HE, Yoon SY. Epidemiologic change of patients with spinal cord injury. Ann Rehabil Med 2013;37(1):50–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Van den Berg MEL, Castellote JM, Mahillo-Fernandez I, de Pedro-Cuesta J. Incidence of spinal cord injury worldwide: a systematic review. Neuroepidemiology 2010;34(3):184–92. [DOI] [PubMed] [Google Scholar]
- 13.Cripps RA, Lee BB, Wing P, Weerts E, Mackay J, Brown D. A global map for traumatic spinal cord epidemiology: towards a living data repository for injury prevention. Spinal Cord 2011;49(4):493–501. [DOI] [PubMed] [Google Scholar]
- 14.Ning GZ, Yu TQ, Feng SQ, Zhou XH, Ban DX, Liu Y, et al. . Epidemiology of traumatic spinal cord injury in Tianjin, China. Spinal Cord 2011;49(3):386–90. [DOI] [PubMed] [Google Scholar]
- 15.Nowak DD, Lee JK, Gelb DE, Poelstra KA, Ludwig SC. Central cord syndrome. J Am Acad Orthop Surg 2009;17(12):756–65. [DOI] [PubMed] [Google Scholar]
- 16.Harrop JS, Sharan A, Ratliff J. Central cord injury: pathophysiology, management, and outcomes. Spine J. 2006;6(6 Suppl):198S–206S. [DOI] [PubMed] [Google Scholar]
- 17.Pickett GE, Campos-Benitez M, Keller JL, Duggal N. Epidemiology of traumatic spinal cord injury in Canada. Spine 2006;31(7):799–805. [DOI] [PubMed] [Google Scholar]
- 18.Couris CM, Guilcher SJ, Munce SE, Fung K, Craven BC, Verrier M, et al. . Characteristics of adults with incident traumatic spinal cord injury in Ontario, Canada. Spinal Cord 2010;48(1):39–44. [DOI] [PubMed] [Google Scholar]
- 19.Dryden DM, Saunders LD, Rowe BH, May LA, Yiannakoulias A, Svenson LW, et al. . The epidemiology of traumatic spinal cord injury in Alberta, Canada. Can J Neurol Sci 2003;30(2):113–21. [DOI] [PubMed] [Google Scholar]
- 20.Lenehan B, Street J, Kwon BK, Noonan V, Zhang H, Fisher CG, et al. . The epidemiology of traumatic spinal cord injury in British Columbia, Canada. Spine 2012;37(4):321–9. [DOI] [PubMed] [Google Scholar]
- 21.Governement of Canada. Statistics Canada. Retrieved July 15, 2012 [cited 2011 Feb 4]. Availale from: http://www.statcan.gc.ca.
- 22.Noreau L, Lavoie A, Fougeyrollas P, Gravel D, LeSage N. Evaluation des services médicaux et de réadaptation fournis aux personnes qui ont subi une blessure médullaire. FQRSC=Fonds de Recherche Societe et Culture, Quebec. Retrieved March 15, 2013 [cited 2004 Feb]. Available from: http://www.fqrsc.gouv.qc.ca/upload/editeur/actionConcerte/blessemed0304.pdf.
- 23.Government of Canada. Canadian Motor Vehicle Traffic Collision Statistics: 2010. Transport Canada. Retrieved June 30, 2013 [cited 2012 Oct 24] Available from: http://www.tc.gc.ca/eng/roadsafety/tp-1317.htm#2.
- 24.Bouchard J, Boulet J, Dussault C, Fournier L, Marmette M, Michaud J, et al. . Politique de Securite dans les transports 2001–2005 – Volet Routier: Les Faits Saillants – in French. Bibliotheque Nationale du Quebec – Depot Legal 2001; ISBN 2-550-37504-1. Available from: http://www.saaq.gouv.qc.ca/rdsr/sites/files/42001002.
- 25.Simard R. Evaluation du Plan Quinquennal 1995–2000 de Prevention Routiere – in French. Societe de l'Assurance Automobile du Quebec; 2003. Available from: http://www.saaq.gouv.qc.ca/rdsr/sites/files/32003005.pdf.
- 26.Donnees et Statistiques 2011 Societe de l'Assurance Automobile du Quebec – in French. Bibliotheque et Archives Nationales du Quebec – Depot Legal 2012; ISBN 978-2-550-65631-9 (printed) or ISBN 978-2-550-65632-6 (pdf). Available from: http://www.saaq.gouv.qc.ca/rdsr/sites/files/22011010.pdf.
- 27.Institut National de Santé Publique du Québec. Vieillissement de la population, état fonctionnel des personnes âgées et besoins futurs en soins de longue durée au Québec. Retrieved April 09, 2014 [2010 Mar]. Available from: http://www.inspq.qc.ca/pdf/publications/1082_VieillissementPop.pdf.