Abstract
Objective
To evaluate the ability of out-of-hospital physiologic measures to predict serious injury for field triage purposes among older adults and potentially reduce the under-triage of seriously injured elders to non-trauma hospitals.
Methods
This was a retrospective cohort study involving injured adults 55 years and older transported by 94 emergency medical services (EMS) agencies to 122 hospitals (trauma and non-trauma) in 7 regions of the western United States from January 1, 2006 to December 31, 2008. We evaluated initial out-of-hospital Glasgow Coma Scale (GCS) score, systolic blood pressure (SBP), respiratory rate, heart rate, shock index (SBP ÷ heart rate), out-of-hospital procedures, mechanism of injury, and patient demographics. The primary outcome was “serious injury,” defined as Injury Severity Score (ISS) ≥ 16, as a measure of trauma center need. We used multivariable regression models, fractional polynomials and binary recursive partitioning to evaluate appropriate physiologic cut-points and the value of different physiologic triage criteria.
Results
A total of 44,890 injured older adults were evaluated and transported by EMS, of whom 2,328 (5.2%) had ISS ≥ 16. Nonlinear associations existed between all physiologic measures and ISS ≥ 16 (unadjusted and adjusted p ≤ 0.001 for all,), except for heart rate (adjusted p = 0.48). Revised physiologic triage criteria included GCS score ≤ 14; respiratory rate < 10 or > 24 breaths per minute or assisted ventilation; and SBP < 110 or > 200 mmHg. Compared to current triage practices, the revised criteria would increase triage sensitivity from 78.6 to 86.3% (difference 7.7%, 95% CI 6.1–9.6%), reduce specificity from 75.5 to 60.7% (difference 14.8%, 95% CI 14.3–15.3%), and increase the proportion of patients without serious injuries transported to major trauma centers by 60%.
Conclusions
Existing out-of-hospital physiologic triage criteria could be revised to better identify seriously injured older adults at the expense of increasing over-triage to major trauma centers.
Keywords: EMS, trauma, triage
Background
Undertriage of seriously injured older adults to non-trauma centers is a major problem in trauma systems.1–6 This mismatch of patient need and hospital resources suggests that older adults most in need of major trauma care are not consistently receiving this care. Previous research demonstrates that undertriage steadily rises in patients over 60 years to a high of 58% among patients over 90 years of age.6 Possible reasons for this disparity include low-velocity mechanisms resulting in serious injury (e.g., ground-level falls)7,8; subtle presentations of serious injury; lack of elder-specific training for field providers5; medical fragility; medications that increase the risk of serious injury (e.g., anticoagulants); patient choice of non-trauma hospitals for transport9; and insensitive triage criteria. Revision of the physiologic field triage criteria has been suggested as one method to potentially reduce undertriage among older adults.
Early identification of seriously injured patients is important in matching hospital resources to patient need and maximizing survival and functional outcome following an injury event.10 Older adults with serious injuries are often complicated to manage, requiring higher levels of care, specialized resources, and unique clinical expertise. Understanding differences in the early physiologic response to injury among older adults may provide the basis for integrating such age-specific physiologic criteria into national field triage guidelines11 to reduce undertriage, allow more timely use of interventions, and improve outcomes in this patient population.
The purpose of this study was to evaluate the ability of out-of-hospital physiologic measures to predict serious injury (and therefore need for care in a major trauma center) among adults ≥ 55 years of age, including the relative value of different physiologic measures, potential changes to the current physiologic triage criteria, and comparison to current triage practices.
Methods
Study Design
This was a multisite retrospective cohort study. Sixteen institutional review boards at 7 sites approved this protocol and waived the requirement for informed consent.
Study Setting
The study included injured older adults who were evaluated and transported by 94 EMS agencies to 122 hospitals (including 15 level I, 8 level II, 3 level III, 4 level IV, 1 level V, and 91 community/private/federal hospitals) in 7 regions across the western United States from January 1, 2006 through December 31, 2008. The 7 regions included Portland, OR/Vancouver, WA (4 counties); King County, WA; Sacramento, CA (2 counties); San Francisco, CA; Santa Clara, CA (2 counties); Denver County, CO; and Salt Lake City, UT (4 counties). Each region consisted of a prespecified geographic “footprint” corresponding to EMS agency service areas (a central metropolitan region and surrounding areas).
Selection of Participants
The study sample included all injured adults ≥ 55 years for whom the 9-1-1 EMS system was activated and the patient was transported to an acute care hospital (trauma and non-trauma centers) within the 7 predefined geographic regions. Specifying the sample in this manner provided an out-of-hospital injury cohort of patients with both minor and serious injuries that approximates the group of older adults to whom field triage guidelines are routinely applied. The 55-year age cut-point identifies patients with the greatest rates of undertriage,1–6 the highest trauma-related mortality,12–14 and the age used in current national triage guidelines,11,15 and allowed for several levels of age strata to examine physiologic responses to injury in this study. We restricted the sample to patients who matched to a hospital record and excluded interhospital transfers without an initial EMS presentation, non-transported patients, and deaths in the field.
Measurements
The primary predictor variables of interest were initial out-of-hospital physiologic measures: Glasgow Coma Scale (GCS) score, systolic blood pressure (SBP) in mmHg, respiratory rate in breaths per minute, need for assisted ventilation (bag–valve–mask ventilation, intubation, supraglottic airway, or cricothyrotomy), heart rate in beats per minute, and shock index (heart rate ÷ SBP). We also collected field triage status (a dichotomous measure termed “field trauma activation” in this study) and all individual triage criteria used by field providers in these regions.16 Because missing values for individual triage criteria are common in EMS charts, we increased the capture of triage status and minimized misclassification bias by triangulating data sources (EMS charts, matched trauma registry records, and matched EMS phone records from base hospitals). All other patients were considered triage-negative (nontrauma activations).
We collected several additional out-of-hospital variables, including patient demographics (age and sex), intravenous line placement, mechanism of injury (15 categories), and hospital type. We categorized acute care hospitals as major trauma centers (level I and II trauma hospitals) versus non-trauma hospitals.
Outcome
The primary outcome measure was “serious injury,” defined as an Injury Severity Score (ISS) ≥ 16, representing a marker of requiring care in a major trauma center.10,17 To obtain the ISS, we used probabilistic linkage (LinkSolv v8.2, Strategic Matching, Morrisonville, NY) to match EMS records to hospital records from trauma registries, emergency department databases, and state discharge databases. Linkage methodology has been used to match EMS data to hospital records in previous studies,18 validated for matching ambulance records to trauma registry data,19 and rigorously evaluated in this database.20 Because ISS is not included in administrative data sources, we used a mapping function (ICDPIC.ado Stata module) to generate ISS from ICD-9-CM diagnosis codes.21 Previous studies have validated the process of mapping administrative diagnosis codes to generate anatomic injury scores22,23 and we have validated ICDPIC-generated ISS values against manually abstracted ISS values in this database.24 We defined “undertriage” as the proportion of patients with ISS ≥ 16 who were triage-negative and “overtriage” as the proportion of patients with ISS < 16 who were triage-positive.
Data Analysis
We used descriptive statistics to characterize the cohort and a variety of analytic approaches to investigate out-of-hospital physiologic measures as predictors of serious injury. We began with multivariable logistic regression models to investigate the association between each physiologic measure and ISS ≥ 16, both unadjusted and adjusted for other out-of-hospital covariates (mechanism of injury, assisted ventilation, intravenous line placement, age, sex, and site). Assisted ventilation was omitted from models assessing respiratory rate, so as not to obscure findings among patients with low respiratory rates. We used the Hosmer-Lemeshow goodness of fit test to assess fit for all models.
To test nonlinear associations between each physiologic measure and ISS ≥ 16 in the models, we used fractional polynomials.25–27 Fractional polynomials provide a method for assessing nonlinear associations by transforming continuous variables into higher-order terms (44 different first- and second-order variables) that can be compared using a standardized algorithm, both unadjusted and adjusted for other covariates.25 After selection of the best-fit version of each physiologic measure, we tested for effect modification (interaction) between age (as a continuous variable) and each physiologic measure.28 We considered effect modification present for interaction terms with p < 0.05. For physiologic measures with effect modification by age, we constructed additional multivariable models stratified by age group (55–64 years, 65–74 years, 75–84 years and ≥85 years) to assess the best-fit fractional polynomial for each physiologic measure within each age strata. We visually evaluated all results by plotting the predicted probability of ISS ≥ 16 against standard values for each physiologic measure.
Finally, we used CART analysis (v. 8.0, Salford Systems, San Diego, CA) to assess the relative importance of each physiologic measure in field triage and further explore the most appropriate physiologic cut-points for older adults. CART is a nonparametric method of binary recursive partitioning well suited for development of clinical decision rules29 and provides a measure of “variable importance” (a score from 0 to 100) based on the number of times the covariate is used as a primary or surrogate decision node “splitter” in the tree-building process. We selected misclassification costs to generate decision trees with high sensitivity (i.e., ≥95%). CART uses the “cost-complexity” method for pruning decision trees, which prunes away terminal nodes (lower branches) if the additional accuracy gained by the branch is minimal in comparison to tree complexity. To reduce the potential for overfitting of the dataset, we randomly sampled 60% of patients for the CART analysis, with the remaining 40% used as a validation sample to generate estimates for proposed changes to the triage decision scheme. We also used cross-validation methods to further reduce over-fitting the dataset. To fully evaluate the importance of physiologic measures in the triage process, we ran three CART analyses with different combinations of variables: (1) only primary physiologic measures (GCS, SBP, respiratory rate, assisted ventilation, heart rate, shock index); (2) primary physiologic measures and current physiologic triage criteria (as used by EMS providers); and (3) primary physiologic measures and all current triage criteria. We also repeated these CART analyses using patients ≥ 65 years of age to assess potential changes in variable importance with an older patient group. We coupled information from the fractional polynomial models and the CART analysis to generate new physiologic triage criteria for older adults, including estimates for triage sensitivity, triage specificity, absolute number of patients over- and undertriaged, and receiver operating characteristic (ROC) values using the validation sample.
We used SAS (v. 9.2, SAS Institute, Cary, NC) for database management and descriptive statistics and Stata (v.12, StataCorp, College Station, TX) to assess and compare fractional polynomials.
Results
There were 44,890 injured older adults transported by participating EMS agencies during the study period with a matched hospital record available. Of these patients, 2,328 (5.2%) had ISS ≥ 16 and 1,189 (2.7%) died during their hospital stay. A total of 12,273 (27.3%) met field trauma activation triage criteria. Of the 2,328 older adults with serious injuries, 1,857 (79.8%) met field triage criteria and 1,509 (65.4%) received care in level I or II trauma centers. Characteristics of the sample are listed in Table 1.
Table 1.
Characteristics of injured older patients transported by EMS in 7 regions
| Overall | Seriously injured (ISS ≥ 16) | Non-seriously injured (ISS < 16) | |
|---|---|---|---|
| n | 44,890 | 2,328 | 42,562 |
| Demographics | |||
| Median age in years (IQR) | 77 (64–85) | 71 (61–82) | 77 (64–85) |
| 55–64 years | 11, 592 (25.8%) | 821 (35.3%) | 10, 771 (25.3%) |
| 65–74 years | 8, 448 (18.8%) | 496 (21.3%) | 7, 952 (18.7%) |
| 75–84 years | 12, 588 (28.0%) | 585 (25.1%) | 12, 003 (28.2%) |
| ≥85 years | 12, 262 (27.3%) | 426 (18.3%) | 11, 836 (27.8%) |
| Female (%) | 28, 245 (63.4%) | 1, 100 (47.6%) | 27, 145 (64.2%) |
| Out-of-hospital physiology and procedures | |||
| Median SBP in mmHg (IQR) | 142 (128–161) | 140 (120–161) | 142 (128–161) |
| Median GCS (IQR) | 15 (15–15) | 15 (13–15) | 15 (15–15) |
| Median respiratory rate in breaths per minute (IQR) | 18 (16–20) | 18 (16–20) | 18 (16–20) |
| Median heart rate in beats per minute (IQR) | 83 (72–94) | 84 (72–96) | 83 (72–94) |
| Triage criteria – any | 12, 273 (27.3%) | 1, 857 (79.8%) | 10, 416 (24.5%) |
| SBP < 90 mmHg | 725 (1.7%) | 95 (4.8%) | 630 (1.6%) |
| GCS ≤ 13 | 1, 920 (5.3%) | 453 (26.2%) | 1, 467 (4.3%) |
| Respiratory rate <10 or >29 | 732 (1.8%) | 147 (7.5%) | 585 (1.5%) |
| Any assisted ventilation | 355 (0.8%) | 184 (8.1%) | 171 (0.4%) |
| Intubation attempt | 258 (0.6%) | 152 (6.7%) | 106 (0.3%) |
| Mechanism of injury | |||
| Gunshot wound | 57 (0.2%) | 21 (1.3%) | 36 (0.1%) |
| Stabbing | 139 (0.4%) | 10 (0.6%) | 129 (0.4%) |
| Assault | 420 (1.3%) | 32 (1.9%) | 388 (1.3%) |
| Fall | 22, 429 (71.4%) | 896 (53.7%) | 21, 533 (72.4%) |
| Motor vehicle crash | 5, 169 (16.5%) | 495 (29.6%) | 4, 674 (15.7%) |
| Pedestrian vs. auto | 595 (1.9%) | 109 (6.5%) | 486 (1.6%) |
| Bicycle | 221 (0.7%) | 27 (1.6%) | 194 (0.7%) |
| Other | 2, 395 (7.6%) | 80 (4.8%) | 2, 315 (7.8%) |
| Hospital measures | |||
| Initial transport to level I/II | 14, 072 (31.4%) | 1, 509 (65.4%) | 12, 563 (29.6%) |
| Median Injury Severity Score (IQR) | 1 (1–8) | 20 (17–26) | 1 (1–5) |
| ISS ≥16 | 2, 328 (5.2%) | 2, 328 (100%) | 0 (0%) |
| Non-orthopedic surgery | 1, 992 (4.4%) | 570 (24.5%) | 1, 422 (3.3%) |
| Orthopedic surgery | 11, 281 (25.1%) | 468 (20.1%) | 10, 813 (25.4%) |
| Median length of stay in days (IQR) | 2 (0–5) | 5 (2–11) | 2 (0–5) |
| In-hospital mortality | 1, 189 (2.7%) | 359 (15.4%) | 830 (2.0%) |
Descriptive statistics are calculated based on observed values, so the denominator may change slightly for certain variables due to missing data.
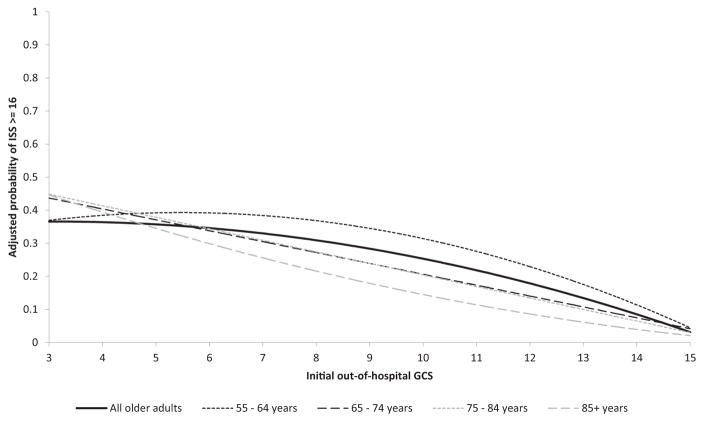
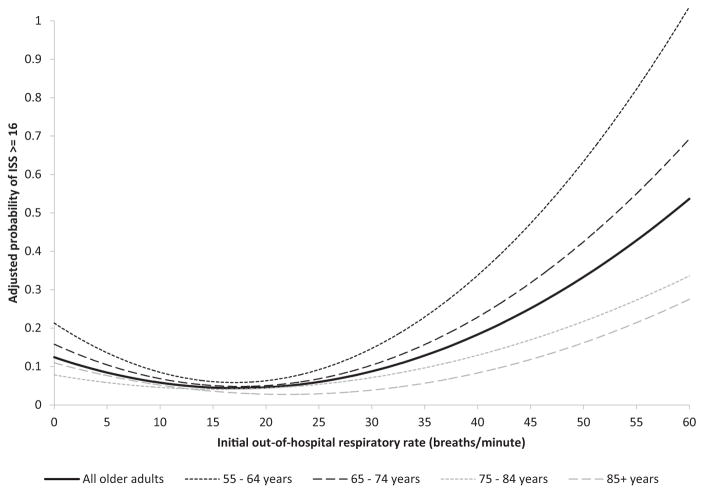
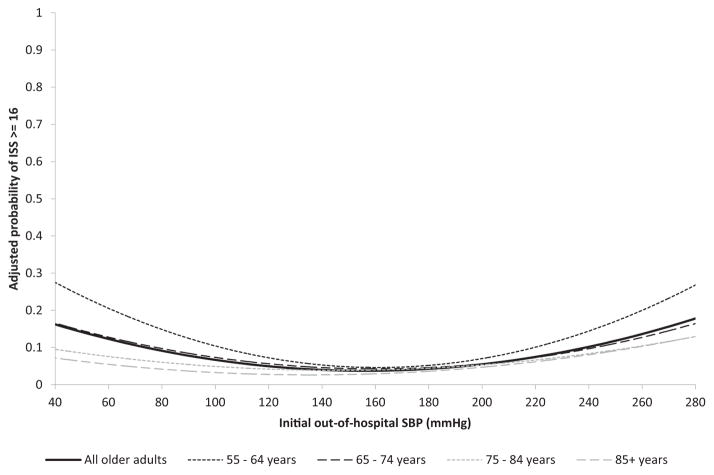
All 5 field physiologic measures (GCS score, SBP, respiratory rate, heart rate, and shock index) had significant nonlinear associations with ISS ≥ 16 in unadjusted models (p < 0.001). In multivariable models adjusted for out-of-hospital covariates, 4 of the physiologic measures (GCS score, SBP, respiratory rate, and shock index) retained their nonlinear association with serious injury (p ≤ 0.001). Heart rate was not associated with ISS ≥ 16 in adjusted models (p = 0.48) and was excluded from further analysis. Each of the 4 remaining physiologic measures demonstrated effect modification by age (interaction: physiologic measure × age) in adjusted models (p < 0.05 for all). Analyses stratified by age group (55–64 years, n = 11,592; 65–74 years, n = 8,448; 75–84 years, n = 12,588; and ≥85 years, n = 12,262) demonstrated slightly different best-fit fractional polynomials for each physiologic measure within each age strata. Figures 1–4 illustrate the adjusted predicted probability of ISS ≥ 16 using best-fit fractional polynomials for GCS, respiratory rate, SBP, and shock index, overall and within age strata. Adding covariates to multivariable models compared to unadjusted models had little effect on the best-fit fractional polynomial for each physiologic measure.
Figure 1.
Adjusted probability of serious injury by initial out-of-hospital Glasgow Coma Scale (GCS) score among injured older adults transported by EMS (n = 44,890).
Figure 4.
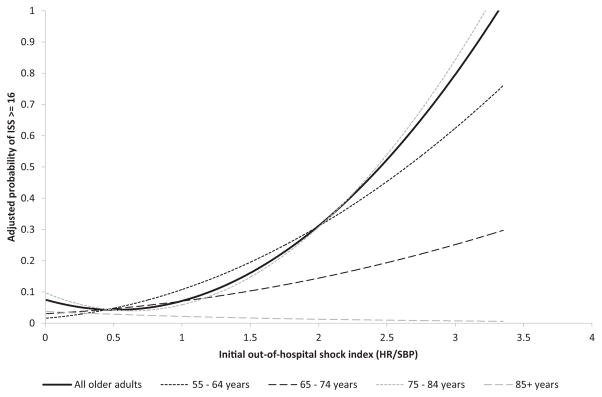
Adjusted probability of serious injury by initial out-of-hospital shock index among injured older adults transported by EMS (n = 44,890).
In Figure 1, we demonstrate the association between GCS score and serious injury. The steepest portion of the curve appears at higher GCS scores (9–15). There were only slight differences in plotted GCS curves predicting serious injury across age groups. In Figure 2, we show the J-shaped association between out-of-hospital respiratory rate and serious injury, which appeared greatest among patients 55–64 years of age. There was less change in predicted probability (flattening of the curve) among older age groups. Figure 3 illustrates the U-shaped association between SBP and serious injury. As with respiratory rate, patients 55–64 years had the most pronounced changes in serious injury with low and high SBP values; the SBP curve flattened with increasing age. Shock index (Figure 4) demonstrated an increased probability of serious injury among patients with values greater than 1, although there was little relationship between shock index and serious injury among the oldest patients.
Figure 2.
Adjusted probability of serious injury by initial out-of-hospital respiratory rate among injured older adults transported by EMS (n = 44,890).
Figure 3.
Adjusted probability of serious injury by initial out-of-hospital systolic blood pressure (SBP) among injured older adults transported by EMS (n = 44,890).
GCS score ranked highest in importance in the CART analysis, whether compared to only physiologic measures, current physiologic triage criteria, or all triage criteria (Table 2). Respiratory rate was second in variable importance among physiologic measures, though it was surpassed by the age triage criterion (>55 years of age) when compared against all triage criteria. Hemodynamic measures (SBP, shock index, and heart rate) ranked low in variable importance, with no clear benefit of shock index over SBP in identifying older adults with serious injuries. When restricted to adults 65 years of age and older, the findings were qualitatively similar, except that the age triage criterion surpassed GCS score for greatest importance and respiratory rate dropped in relative value.
Table 2.
Variable importance of out-of-hospital physiologic measures in identifying seriously injured patients in a derivation sample (n = 27,086)
| Tree 1
|
Tree 2
|
Tree 3
|
|||
|---|---|---|---|---|---|
| Physiologic measures (7 variables) | Var impta | Physiologic measures and current physiologic triage criteria (11 variables) | Var impta | Physiologic measures and all triage criteria (36 variablesb) | Var impta |
| GCS | 100 | GCS | 100 | GCS | 100 |
| Respiratory rate | 28.4 | Respiratory rate | 28.3 | Criterion – age > 55 years | 64.2 |
| SBP | 16.1 | Criterion – GCS ≤ 13 | 19.7 | Respiratory rate | 28.1 |
| Shock index | 10.9 | SBP | 18.7 | Criterion – GCS ≤ 13 | 19.7 |
| Assisted ventilation | 7.1 | Shock index | 16.5 | Shock index | 18.1 |
| Intubation | 6.7 | Heart rate | 10.9 | Criterion – EMS provider judgment | 16.4 |
| Heart rate | 6.4 | Criterion – SBP | 5.7 | SBP | 16.4 |
| Criterion – airway | 4.2 | Criterion – fall | 13.6 | ||
| Intubation | 0 | Heart rate | 12.7 | ||
| Assisted ventilation | 0 | Criterion – pedestrian vs. auto | 10.1 | ||
| Criterion – respiratory rate <10 or >29 | 0 | Criterion – respiratory rate <10 or >29 | 6.0 | ||
| Criterion – motor cycle crash | 5.3 | ||||
| Assisted ventilation | 2.8 | ||||
| Criterion – MVC with passenger space intrusion | 2.6 | ||||
| Intubation | 2.5 | ||||
| Criterion – environment | 2.0 | ||||
| Criterion – comorbidities | 1.6 | ||||
| ROC values for CART trees | |||||
|
| |||||
| 0.68 | 0.70 | 0.73 | |||
Estimates for variable importance (var impt) were calculated using classification and regression tree analysis to develop high-sensitivity (≥95%) decision trees. GCS, Glasgow Coma Scale score; SBP, systolic blood pressure; Criterion, field triage criteria, as determined on-scene by EMS personnel; MVC, motor vehicle crash; ROC, receiver operating characteristic.
19 of 36 predictors were not used in decision tree development and therefore given a variable importance score of zero. These predictors are omitted from the table for clarity, but include criterion – paralysis, criterion – SBP < 90, criterion – MVC with rollover, criterion – intoxication, criterion – airway, criterion – flail chest, criterion – MVC with death of occupant, criterion - penetrating torso injury, criterion – CPR, criterion – amputation, criterion – burn, criterion - steering wheel deformity, criterion - skull fracture, criterion – pelvic fracture, criterion – high speed MVC, criterion – long bone fractures, criterion – mangled extremity, criterion –MVC with ejection, and criterion – MVC with extrication.
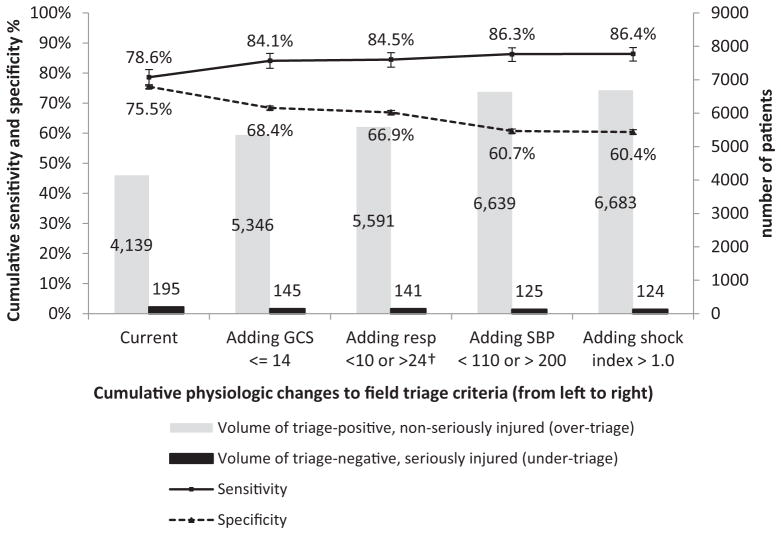
Figure 5 illustrates estimates for the cumulative impact of revised physiologic triage criteria for older adults, compared to current triage practices. We derived the revised physiologic triage criteria and rank-order list from both the fractional polynomial models (physiologic cut-points) and the CART analysis (physiologic cut-points and relative importance of physiologic measures). The revised criteria were defined as follows: GCS score ≤ 14; respiratory rate < 10 or > 24 breaths per minute or need for assisted ventilation; SBP < 110 or > 200 mmHg; and shock index > 1.0. The modified GCS score criterion produced the largest single increase in triage sensitivity, with a similar percentage decrease in specificity. Adding revised criteria for respiratory status, SBP, and shock index resulted in smaller gains in sensitivity. When simulating implementation of the new GCS, respiratory and SBP criteria, there was a cumulative increase in triage sensitivity from 78.6 to 86.3% (absolute difference 7.7%, 95% CI 6.1–9.6%) and decrease in the number of undertriaged patients in our sample from 195 to 125. These triage modifications reduced the specificity of the triage guidelines from 75.5 to 60.7% (absolute difference 14.8%, 95% CI 14.3–15.3%), increasing the number of patients without serious injuries targeted for transport to major trauma centers by 60% (from 4,139 to 6,639 in our sample).
Figure 5.
Estimates for cumulative changes in field triage sensitivity, specificity, under- and overtriage based on modification to the physiologic triage criteria for older adults using a validation sample (n = 17,804). The receiver operating characteristic values for each triage strategy are as follows: 0.77 (current triage criteria); 0.76 (adding GCS ≤ 14); 0.76 (adding assisted ventilation or respiratory rate < 10 or > 24 breaths/minute); 0.73 (adding SBP < 110 or > 200 mmHg); and 0.73 (adding shock index > 1.0). The respiratory criterion includes the need for assisted ventilation (bag–valve–mask ventilation or intubation) and respiratory rate < 10 or > 24 breaths/minute.
Discussion
In this study, we demonstrate that the physiologic criteria used in current national field triage guidelines are not ideal for identifying older adults with serious injury. Using multiple analytic methods to explore the predictive value of out-of-hospital physiologic measures, we illustrate the potential impact of modest revisions to the physiologic triage criteria in older adults. The suggested revisions would likely improve, but not eliminate undertriage among older adults, while increasing the overtriage of patients without serious injuries to major trauma centers.
Older adults with serious injuries are commonly missed by current field triage processes3–6 and cared for in non-trauma hospitals.1,2 While explanations for undertriage are multifactorial, we focused on potential changes to the physiologic triage criteria to reduce undertriage. The 2011 revisions to the field triage guidelines draw attention to unique physiologic aspects of identifying older adults with serious injuries (e.g., systolic blood pressure < 110 mmHg in patients over 65 years of age),11 though out-of-hospital studies to support such cut-points are sparse. Previous studies on this topic are limited by the use of hospital-based physiologic data, single-center trauma registries, exclusion of certain types of patients (e.g., penetrating injury, traumatic brain injury), and use of mortality as the primary outcome.30–33 Each of these factors introduces bias and reduces the ability to extrapolate findings to the out-of-hospital setting. We undertook the current study to help fill this void and better inform the next revision of the national field triage guidelines.
The physiologic measure most predictive of serious injury was GCS score. We demonstrate that changing the GCS triage criterion from ≤13 (current value) to ≤14 would reduce undertriage with a similar increase in overtriage. The potential benefit of such a change among other age groups has been previously evaluated.34 While the GCS score is criticized as overly complicated, having poor interrater reliability, and confounded by intoxicants,35 it remains the most widely used out-of-hospital marker of mental status and brain function for injured patients in the United States. There is practical benefit in maximizing the value of familiar physiologic measures before attempting to integrate new metrics that require additional training and resources at the field level. Using GCS ≤ 14 would also simplify the GCS criterion to a dichotomous value of “normal” mentation (GCS = 15) versus “abnormal” (GCS ≤ 14) mentation. With all its imperfections, this potential modification to the GCS score cut-point may provide the single greatest improvement in triage sensitivity for older adults.
Respiratory status (including the need for assisted ventilation) was the next most important out-of-hospital physiologic triage criterion. Including need for assisted ventilation reflects actual field triage practices where EMS providers may not have time to count a specific respiratory rate in high-acuity patients36 and is consistent with the 2011 triage guidelines.11 Although our results show respiratory status to be a strong predictor of serious injury, the reduction in undertriage with the proposed change was small, suggesting that many patients with abnormal respiratory status are already identified by an abnormal GCS score.
Hemodynamic measures (SBP, heart rate, and shock index) were relatively poor predictors of serious injury among older adults, with changes to these measures offering little reduction in undertriage. While the cut-points we identified in SBP were similar to those proposed in other studies,31,33 the yield of such triage revisions appeared small. The lack of predictive value of SBP and heart rate among injured older adults has been previously demonstrated.30 Although combining out-of-hospital heart rate with SBP (shock index) has been suggested to predict hospital resource use and mortality,37 we did not find similar results among older adults. Also, the age-stratified analysis of SBP suggested that predictive value decreases as patient age increases, possibly due to blunted hemodynamic responses to injury and increased use of certain medications (e.g., beta blockers). These findings suggest that age-specific revisions to hemodynamic measures are unlikely to have substantive impact on the accuracy of field triage among older adults.
It is important to consider the potential implications of modifying the physiologic triage criteria, including overtriage and changes in EMS transport patterns to different hospitals. We have previously demonstrated that triage sensitivity and specificity are inversely related and do not change in linear fashion.34 While small increases in overtriage may be tolerated, large shifts in EMS transport patterns may have substantial consequences, including reduced trauma system efficiency, increased costs, less patient autonomy, and disruption in continuity of care. Age-specific physiologic criteria would also increase the complexity of applying the triage algorithm by EMS personnel in the time-constrained out-of-hospital environment. However, recognizing differences in the physiologic response to injury between age groups is an important educational aspect for training EMS personnel. “Inadequate training in managing injured elderly patients” has been cited by EMS personnel as the largest contributor to undertriage of older adults.5
We used a retrospective cohort study design for this project, which is subject to potential unmeasured confounding and bias. We also restricted the primary sample to patients who matched to a hospital record, which may have skewed the sample toward a higher-acuity population. Also, our estimates for changes in triage sensitivity and specificity with the revised physiologic criteria assume universal application of the criteria and that all patients meeting such criteria would be transported to major trauma centers. Selective application of the criteria or variation in transport destination for field trauma activations would reduce our estimates for sensitivity and trauma center volume.
We defined serious injury as ISS ≥ 16,10, 17 although this definition may miss some high-risk older adults with lower ISS values who require major trauma care. There is no universally accepted definition of trauma center need for older adults. We were also unable to account for pre-injury physiologic status, baseline mentation, comorbidities and intoxicants, all of which may affect the predictive value of certain physiologic measures. Finally, our results require validation in prospective studies.
In summary, revising the out-of-hospital physiologic triage criteria (e.g., GCS score ≤ 14) for older adults may better identify patients with serious injuries. Such changes may reduce, though not eliminate, under-triage among older adults at the expense of increases in overtriage and the volume of non-seriously injured patients targeted for transport to major trauma centers.
Acknowledgments
This project was supported by the Robert Wood Johnson Foundation Physician Faculty Scholars Program; the Oregon Clinical and Translational Research Institute (grant #UL1 RR024140); UC Davis Clinical and Translational Science Center (grant #UL1 RR024146); Stanford Center for Clinical and Translational Education and Research (grant #1UL1 RR025744); University of Utah Center for Clinical and Translational Science (grant #UL1-RR025764 and C06-RR11234); and UCSF Clinical and Translational Science Institute (grant #UL1 RR024131). All Clinical and Translational Science Awards are from the National Center for Research Resources, a component of the National Institutes of Health (NIH), and NIH Roadmap for Medical Research.
We want to acknowledge and thank all the participating EMS agencies, EMS medical directors, trauma registrars, and state offices that supported and helped provide data for this project.
Footnotes
An abstract of these results was presented at the 2013 Society for Academic Emergency Medicine Annual in Atlanta, GA, May 17, 2013.
The authors report no conflicts of interest. The authors alone are responsible for the content and writing of the paper.
References
- 1.Hsia RY, Wang E, Torres H, et al. Disparities in trauma center access despite increasing utilization: data from California, 1999 to 2006. J Trauma. 2010;68:217–24. doi: 10.1097/TA.0b013e3181a0e66d. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Vassar MJ, Holcroft JJ, Knudson MM, et al. Fractures in access to and assessment of trauma systems. J Am Coll Surg. 2003;197:717–25. doi: 10.1016/S1072-7515(03)00749-X. [DOI] [PubMed] [Google Scholar]
- 3.Scheetz LJ. Effectiveness of prehospital trauma triage guidelines for the identification of major trauma in elderly motor vehicle crash victims. J Emerg Nurs. 2003;29:109–15. doi: 10.1067/men.2003.59. [DOI] [PubMed] [Google Scholar]
- 4.Newgard CD, Zive D, Holmes JF, et al. A multi-site assessment of the ACSCOT field triage decision scheme for identifying seriously injured children and adults. J Am Coll Surg. 2011;213:709–21. doi: 10.1016/j.jamcollsurg.2011.09.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Chang DC, Bass RR, Cornwell EE, et al. Undertriage of elderly trauma patients to state-designated trauma centers. Arch Surg. 2008;143:776–81. doi: 10.1001/archsurg.143.8.776. [DOI] [PubMed] [Google Scholar]
- 6.Nakamura Y, Daya M, Bulger EM, et al. Evaluating age in the field triage of injured persons. Ann Emerg Med. 2012;60:335–45. doi: 10.1016/j.annemergmed.2012.04.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Chisholm KM, Harruff RC. Elderly deaths due to ground-level falls. Am J Forensic Med Pathol. 2010;31:350–4. doi: 10.1097/PAF.0b013e3181f69c87. [DOI] [PubMed] [Google Scholar]
- 8.Spaniolas K, Cheng JD, Gestring ML, et al. Ground level falls are associated with significant mortality in elderly patients. J Trauma. 2010;69:821–5. doi: 10.1097/TA.0b013e3181efc6c6. [DOI] [PubMed] [Google Scholar]
- 9.Newgard CD, Mann NC, Hsia RY, Bulger EM, Ma OJ, Staudenmayer K, Haukoos JS, Sahni R, Kuppermann N. Patient Choice in the Selection of Hospitals by 9-1-1 Emergency Medical Services Providers in Trauma Systems. Acad Emerg Med. 2013;20:911–9. doi: 10.1111/acem.12213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.MacKenzie EJ, Rivara FP, Jurkovich GJ, et al. A national evaluation of the effect of trauma-center care on mortality. NEJM. 2006;354:366–78. doi: 10.1056/NEJMsa052049. [DOI] [PubMed] [Google Scholar]
- 11.Sasser SM, Hunt RC, Faul M, et al. Guidelines for field triage of injured patients: recommendations of the National Expert Panel on Field Triage, 2011. MMWR. 2012;61:1–20. [PubMed] [Google Scholar]
- 12.Finelli F, Jonsson J, Champion H, et al. A case control study for major trauma in geriatric patients. J Trauma. 1989;29:541–8. doi: 10.1097/00005373-198905000-00001. [DOI] [PubMed] [Google Scholar]
- 13.Demetriades D, Sava J, Alo K, et al. Old age as a criterion for trauma team activation. J Trauma. 2001;51:754–7. doi: 10.1097/00005373-200110000-00022. [DOI] [PubMed] [Google Scholar]
- 14.Caterino J, Valasek T, Werman H. Identification of an age cutoff for increased mortality in patients with elderly trauma. Am J Emerg Med. 2010;28:151–8. doi: 10.1016/j.ajem.2008.10.027. [DOI] [PubMed] [Google Scholar]
- 15.Resources for the Optimal Care of the Injured Patient. Chicago, IL: American College of Surgeons; 2006. [Google Scholar]
- 16.Barnett AS, Wang NE, Sahni R, et al. Variability in prehospital use and uptake of the national field triage decision scheme. Prehosp Emerg Care. 2013;17:135–48. doi: 10.3109/10903127.2012.749966. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Mullins RJ, Veum-Stone J, Helfand M, et al. Outcome of hospitalized injured patients after institution of a trauma system in an urban area. JAMA. 1994;271:1919–24. doi: 10.1001/jama.1994.03510480043032. [DOI] [PubMed] [Google Scholar]
- 18.Dean JM, Vernon DD, Cook L, et al. Probabilistic linkage of computerized ambulance and inpatient hospital discharge records: a potential tool for evaluation of emergency medical services. Ann Emerg Med. 2001;37:616–26. doi: 10.1067/mem.2001.115214. [DOI] [PubMed] [Google Scholar]
- 19.Newgard CD. Validation of probabilistic linkage to match de-identified ambulance records to a state trauma registry. Acad Emerg Med. 2006;13:69–75. doi: 10.1197/j.aem.2005.07.029. [DOI] [PubMed] [Google Scholar]
- 20.Newgard CD, Malveau S, Staudenmayer K, et al. Evaluating the use of existing data sources, probabilistic linkage and multiple imputation to build population-based injury databases across phases of trauma care. Acad Emerg Med. 2012;19:469–80. doi: 10.1111/j.1553-2712.2012.01324.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Clark DE, Osler TM, Hahn DR. ICDPIC: Stata Module to Provide Methods for Translating International Classification of Diseases (Ninth Revision) Diagnosis Codes into Standard Injury Categories and/or Scores. Boston: Boston College, Department of Economics; 2009. [Google Scholar]
- 22.MacKenzie EJ, Steinwachs DM, Shankar BS, et al. An ICD-9CM to AIS conversion table: development and application. Proc AAAM. 1986;30:135–51. [Google Scholar]
- 23.MacKenzie EJ, Steinwachs DM, Shankar B. Classifying trauma severity based on hospital discharge diagnoses: validation of an ICD-9CM to AIS-85 conversion table. Med Care. 1989;27:412–22. doi: 10.1097/00005650-198904000-00008. [DOI] [PubMed] [Google Scholar]
- 24.Fleischman R, Mann NC, Wang NE, et al. Validating the use Of ICD9 codes to generate Injury Severity Score: the ICD-PIC mapping procedure. [Abstract] Acad Emerg Med. 2012;19 (suppl):S314. [Google Scholar]
- 25.Royston P, Altman DG. Regression using fractional polynomials of continuous covariates: parsimonious parametric modeling. Appl Statist. 1994;43:429–67. [Google Scholar]
- 26.Royston P, Sauerbrei W. Stability of multivariable fractional polynomial models with selection of variables and transformations: a bootstrap investigation. Statist Med. 2003;22:639–59. doi: 10.1002/sim.1310. [DOI] [PubMed] [Google Scholar]
- 27.Sauerbrei W, Meier-Hirmer C, Benner A, et al. Multivariable regression model building by using fractional polynomials: description of SAS, STATA and R programs. Comput Stat Data Anal. 2006;50:3464–85. [Google Scholar]
- 28.Royston P, Sauerbrei W. A new approach to modeling interactions between treatment and continuous covariates in clinical trials by using fractional polynomials. Statist Med. 2004;23:2509–25. doi: 10.1002/sim.1815. [DOI] [PubMed] [Google Scholar]
- 29.Breiman L, Freidman JH, Olshen RA, et al. Classification and Regression Trees. New York: Chapman & Hall; 1984. [Google Scholar]
- 30.Lehmann R, Beekley A, Casey L, et al. The impact of advanced age on trauma triage decisions and outcomes: a statewide analysis. Am J of Surg. 2009;197:571–5. doi: 10.1016/j.amjsurg.2008.12.037. [DOI] [PubMed] [Google Scholar]
- 31.Zarzaur BL, Croce MA, Magnotti LJ, et al. Identifying life-threatening shock in the older injured patient: an analysis of the National Trauma Data Bank. J Trauma. 2010;68:1134–8. doi: 10.1097/TA.0b013e3181d87488. [DOI] [PubMed] [Google Scholar]
- 32.Martin JT, Alkhoury F, O’Connor JA, et al. ‘Normal’ vital signs belie occult hypoperfusion in geriatric trauma patients. Am Surgeon. 2010;76:65–9. [PubMed] [Google Scholar]
- 33.Heffernan DS, Thakkar RK, Monaghan SF, et al. Normal presenting vital signs are unreliable in geriatric blunt trauma victims. J Trauma. 2010;69:813–20. doi: 10.1097/TA.0b013e3181f41af8. [DOI] [PubMed] [Google Scholar]
- 34.Newgard CD, Hsia RY, Mann NC, et al. The trade-offs in field trauma triage: a multi-region assessment of accuracy metrics and volume shifts associated with different triage strategies. J Trauma Acute Care Surg. 2013;74:1298–306. doi: 10.1097/TA.0b013e31828b7848. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Green SM. Cheerio, Laddie! Bidding farewell to the Glasgow Coma Scale. Ann Emerg Med. 2011;58:427–30. doi: 10.1016/j.annemergmed.2011.06.009. [DOI] [PubMed] [Google Scholar]
- 36.Newgard CD, Nelson MJ, Kampp M, et al. Out-of-hospital decision-making and factors influencing the regional distribution of injured patients in a trauma system. J Trauma. 2011;70:1345–53. doi: 10.1097/TA.0b013e3182191a1b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.McNab A, Burns B, Bhullar I, et al. A prehospital shock index for trauma correlates with measures of hospital resource use and mortality. Surgery. 2012;152:473–6. doi: 10.1016/j.surg.2012.07.010. [DOI] [PubMed] [Google Scholar]