Abstract
Objective
A prospective, randomized controlled trial was conducted to evaluate the efficacy of nerve-sparing radical hysterectomy (NSRH) in preserving bladder function and its oncologic safety in the treatment of cervical cancer.
Methods
From March 2003 to November 2005, 92 patients with cervical cancer stage IA2 to IIA were randomly assigned for surgical treatment with conventional radical hysterectomy (CRH) or NSRH, and 86 patients finally included in the analysis. Adequacy of nerve sparing, radicality, bladder function, and oncologic safety were assessed by quantifying the nerve fibers in the paracervix, measuring the extent of paracervix and harvested lymph nodes (LNs), urodynamic study (UDS) with International Prostate Symptom Score (IPSS), and 10-year disease-free survival (DFS), respectively.
Results
There were no differences in clinicopathologic characteristics between two groups. The median number of nerve fiber was 12 (range, 6 to 21) and 30 (range, 17 to 45) in the NSRH and CRH, respectively (p<0.001). The extent of resected paracervix and number of LNs were not different between the two groups. Volume of residual urine and bladder compliance were significantly deteriorated at 12 months after CRH. On the contrary, all parameters of UDS were recovered no later than 3 months after NSRH. Evaluation of the IPSS showed that the frequency of long-term urinary symptom was higher in CRH than in the NSRH group. The median duration before the postvoid residual urine volume became less than 50 mL was 11 days (range, 7 to 26 days) in NSRH group and was 18 days (range, 10 to 85 days) in CRH group (p<0.001). No significant difference was observed in the 10-year DFS between two groups.
Conclusion
NSRH appears to be effective in preserving bladder function without sacrificing oncologic safety.
Keywords: Disease-Free Survival; Hysterectomy; Urinary Bladder, Neurogenic; Uterine Cervical Neoplasms
INTRODUCTION
Radical hysterectomy (RH) is one of the most common surgeries for gynecologic malignancies, especially for early-stage cervical cancer [1]. The quality of life (QoL) is a very important issue because most of the patients can live without disease for long time after the treatment. Although conventional radical hysterectomy (CRH) is an effective approach for the management of early-stage cervical carcinoma and it has shown 5-year survival rates of more than 90%, it has been demonstrated that this procedure frequently causes pelvic organ dysfunction, especially bladder dysfunction up to 85% of cervical cancer survivors [2]. These complications are believed to be the result of surgical trauma to the sympathetic and parasympathetic branches of the pelvic autonomic nervous system [2,3,4,5].
Although these autonomic nerves of the pelvic organs and their origins are well described in anatomic textbooks, these structures are rarely visualized and preserved in operating rooms by surgical oncologists until the publications by several pioneer surgeons during the last two decades [6,7,8,9]. They proposed that preserving the pelvic autonomic nerves with the nerve-sparing surgical techniques may reduce the incidence of long-term complications following CRH, without reducing the radicality of the operation. However, a conclusion on this subject could not be made because only a few small randomized trials without a long-term follow-up have been reported [10,11,12].
We have developed and performed nerve-sparing radical hysterectomy (NSRH) based on the experiences with Professor M. Höckel and Professor A. Schneider in Germany in 2001 (JWR), and the published articles describing the surgical methods of NSRH in detail [6,7,13,14].
After the pilot trial for this new surgical procedure over a 1 year, we designed a prospective randomized controlled trial (RCT) to assess the efficacy of NSRH in prevention of bladder dysfunction and its oncologic safety compared to that of CRH. Here, we present the results with a long-term follow-up.
MATERIALS AND METHODS
1. Study subjects
This study was conducted prospectively in patients with cervical cancer the International Federation of Gynecology and Obstetrics (FIGO) stage IB1-IIA. Exclusion criteria included neuroendocrine histology, pathologically proven distant metastasis, history of psychiatric disease, preoperative urinary dysfunction, and another coexisting malignancy. Patients with an adequate follow-up duration of more than one year after the surgery were included in the analysis.
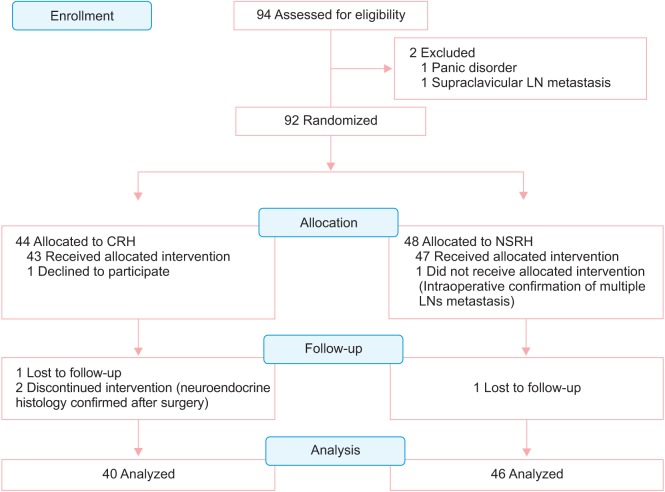
Between March 2003 and November 2005, 94 consecutive patients with cervical cancer FIGO stage IB1-IIA were enrolled and 92 patients were randomly assigned to surgical treatment with CRH or NSRH after excluding panic disorder (n=1) and pathologically confirmed supraclavicular lymph node (LN) metastasis (n=1). After random assignment, one patient declined to get included in the CRH group, and one patient with intraoperatively confirmed multiple metastatic LNs was converted to chemoradiation followed by pelvic and para-aortic LND in NSRH group. Two patients in the CRH group who had confirmed neuroendocrine histology in the surgical specimen were excluded from the study, and treated by systemic chemotherapy. One patient in each group was lost to follow-up within one year after the surgery. Eighty-six patients (40 in the CRH group and 46 in the NSRH group) were included in the final analysis (Fig. 1). This prospective study was approved by the Institutional Review Board of the National Cancer Center of Korea.
Fig. 1. Flow diagram of the patients enrolled in this study. CRH, conventional radical hysterectomy; LN, lymph node; NSRH, nerve-sparing radical hysterectomy.
2. Surgical procedure
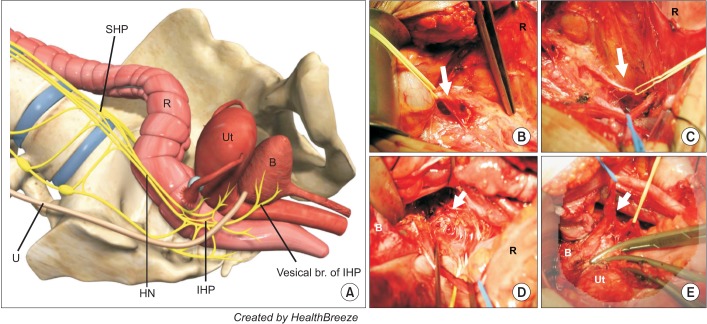
All operations were performed by either or both surgeons (JWR and SYP) who were skilled in CRH and already had experience with NSRH for one year before this study in the pilot trial. Laparotomy through hypogastric midline incision and left circumcision of the umbilicus was performed for the procedure. A schematic three-dimensional (3D)-illustration of the nervous system of the pelvis and key steps in the surgical procedure are presented in Fig. 2. The key for the nerve-sparing during RH included four steps. The first step was to identify the superior hypogastric plexus (SHP) at the aortic bifurcation and mobilize it from the sacral promontary, which would be the starting point of the nerve-sparing procedure (Fig. 2B). The second step was, after entering the retroperitoneal pelvic space and completion of pelvic LND, the hypogastric nerves (HN) originating from the SHP and the upper part of the inferior hypogastric plexus (IHP) were exposed along the lateral border of the mesorectum (Fig. 2C). The third step was for the IHP (Fig. 2D). The vascular part of the paracervix was ligated at the level where uterine vessels branch from the internal iliac vessels. After incision of the rectouterine peritoneal fold, separation of the anterior mesorectum from the proximal vagina and lateral mobilization of the IHP, which was HN fused with the pelvic splanchnic nerves from S2 to S4, were performed before transaction of the uterosacral ligament. After an anterior incision between the bladder and the cervix, the medial aspect of the distal ureter was exposed by separation of the uterine vessels, lymphatics, and a few small LNs from the bladder mesentery. For complete removal of the paracervical tissues, liposuction was performed with Hercules aspirator (Wells Johnson Co., Tucson, AZ, USA) below the vascular part of the paracervix.
Fig. 2. Three-dimensional (3D) illustration and key steps in nerve-sparing radical hysterectomy. (A) Schematic 3D-illustration of the nervous system of the pelvis which should be preserved during nerve-sparing radical hysterectomy. (B) Separation and preservation of the superior hypogastric plexus on the sacral promontory (arrow, SHP). (C) Isolation and tracing of the hypogastric nerve on the lateral border of the rectum (arrow, HN). (D) Identification and preservation of the inferior hypogastric plexus composed of the hypogastric nerve and pelvic splanchnic nerve below the vascular part of the paracervix (arrow, IHP). (E) Vesical branch of the inferior hypogastric plexus during dissection of the vesicouterine ligament (arrow, vesical branch of IHP). B, bladder; HN, hypogastric nerve; IHP, inferior hypogastric plexus; R, rectum; SHP, superior hypogastric plexus; U, ureter; Ut, uterus.
The last part of nerve-sparing was for the bladder branch of the IHP (Fig. 2E). The vesicovaginal venous connection and anterior condensed ligamentous portion crossing the ureters were ligated and transected, and then the vagina at a level 2 to 3 cm distal to the tumor was clamped while saving the posterior part of the vesicouterine ligament which contained the bladder branch of the IHP.
After the insertion of two Jackson-Pratt closed suction drains, suprapubic cystostomy was performed. Bladder emptying with suprapubic catheterization was performed for one week, and then self-voiding was attempted after clamping of the suprapubic catheter. Residual urine (RU) volume was recorded by declamping the catheter immediately after the self-voiding. The suprapubic catheter was removed when the RU measured less than 50 mL at least two times in a low. The duration of bladder catheterization after the surgery was recorded and compared.
For the quantification of nerve fibers retained in the resected paracervix, longitudinal paracervical tissues were marked at 2 cm lateral to the isthmus of the resected uterus at the operating theater (Supplementary Fig. 1). Microscopic section of full length of the labeled paracervix was stained with a general nerve marker, S-100 protein, in order to quantify the nerve fibers. Nerve fibers larger than 100 µm on both sides were counted by the pathologist (SL) without any clinical information and surgical protocol.
Postoperative external radiotherapy (RT) was employed when the final pathologic report revealed LN metastasis or histologically confirmed parametrial invasion, and intracavitary RT was added when the vaginal resection margin was involved by tumor.
3. Evaluation of urinary function
Urodynamic studies (UDSs) were carried out before the operation and at 1, 3, and 12 months after the operation. UDS were carried out using the Duet MultiP (Medtronic Inc., Minneapolis, MN, USA) and air-charged urethral and abdominal sensors. All procedures were performed in a sitting erect position on a toilet seat with room-temperature sterile water. The filling rate was 30 mL/min unless this provoked urinary urgency. Abdominal leak point pressures were measured at 200 cm3, with the urethral catheter in place, unless otherwise specified. The abdominal pressure transducer was placed rectally. Provocative maneuvers, including water stimulation and cough, were used in an effort to provoke detrusor overactivity. Urethral pressure profile was performed using a mechanical puller at a rate of 1 mm/sec. Both static and dynamic profiles were performed at cystometric capacity. Recorded urodynamic parameters in addition to the urodynamic tracings were from the uroflowmetry (voided volume, postvoid RU, maximal flow rate, voiding time), cystometrogram (first sensation, first desire to void, capacity, filling rate, detrusor overactivity, urodynamic stress incontinence, abdominal leak point pressure at 200 cm3), and urethral pressure profile. One urologist (JSC) reviewed each case without any clinical information.
Subjective bladder dysfunction was evaluated with a standard questionnaire of the Korean version of International Prostate Symptom Score (IPSS). The scoring system for voiding function described above was based on a 0 to 5 scale, as follows; 0, not at all; 1, less than one time in five; 2, less than half the time; 3, about half the time; 4, more than half the time; and 5, almost always. Questionnaires were analyzed and divided into emptying, frequency, intermittency, urgency, weak stream, straining, and nocturia. Total IPSS score was calculated by adding the score of each item. It can be expected that the greater is the increase in the IPSS, the lesser is the urinary function.
4. Evaluation of oncologic safety
All enrolled patients were followed up every 3 months for the first 2 years after the surgery and every 6 months thereafter with a physical gynecological examination, vaginal cytology, chest X-ray, tumor markers (squamous cell carcinoma antigen and carcinoembryonic antigen), and other imaging modality including computed tomography (CT), magnetic resonance imaging, positron emission tomography (PET), and PET/CT if indicated.
Disease-free survival (DFS) and overall survival (OS) were calculated as time, in months, from the date of the primary surgery to the time of confirmed recurrence of cervical cancer and death, respectively. DFS and OS were compared between the two groups by survival analysis with a long-term follow-up.
5. Statistical analysis
Continuous variables were assessed for normal distribution (Kolmogorov-Smirnov test) and expressed as appropriate (mean with SD or median with range). Categorical variables were evaluated with the use of the Fisher exact test. For paired data, such as postoperative changes in UDS or IPSS score compared with preoperative baseline, Wilcoxon singed rank test was used for analysis. A p<0.05 was considered statistically significant. DFS and OS were evaluated by Kaplan-Meier analysis. IBM SPSS ver. 20.0 (IBM Co., Armonk, NY, USA) was used for all statistical analyses.
RESULTS
1. Clinicopathologic characteristics and surgical outcomes
The detailed clinical and pathologic characteristics of the enrolled patients and the surgical outcomes in both groups are detailed in Table 1. The general characteristics of the patients, including age, BMI, FIGO stage, histologic distribution, tumor size, operating time, estimated blood loss, adjuvant RT, and LN metastasis were not different in the two groups. With respect to the evaluation of radicality of NSRH, surgical outcomes such as the width and length of the resected paracervix, length of safety margin of the resected vagina, and the number of harvested LNs were also similar between the two groups. Average count of resected nerve bundles stained with S-100 in the removed paracervix was significantly lower in the NSRH (12; range, 6 to 21) compared to CRH (30; range, 17 to 45; p<0.001).
Table 1. Clinicopathologic characteristics and surgical outcomes.
| Characteristic | CRH (n=40) | NSRH (n=46) | p-value |
|---|---|---|---|
| Age (yr) | 49.5±9.1 | 46.7±9.4 | NS* |
| BMI (kg/m2) | 25.4±3.2 | 24.3± 2.2 | NS* |
| FIGO stage | NS† | ||
| IB1 | 31 (77.5) | 34 (74.0) | |
| IB2 | 3 (7.5) | 6 (13.0) | |
| IIA | 6 (15.0) | 6 (13.0) | |
| Tumor size (cm) | 2.5±1.1 | 2.1±1.3 | NS* |
| Histologic type | NS† | ||
| Squamous cell carcinoma | 33 (82.5) | 35 (76.0) | |
| Adenocarcinoma | 6 (15.0) | 11 (23.9) | |
| Adenosquamous carcinoma | 1 (2.5) | 0 | |
| Operation time (min) | 278 (244-321) | 297 (256-368) | NS‡ |
| Estimated blood loss (mL) | 520.8±239.8 | 478.9±206.5 | NS* |
| Radicality | |||
| Paracervical length, right (cm) | 4.7±1.4 | 4.2±0.9 | NS* |
| Paracervical width, right (cm) | 3.6±0.8 | 3.7±1.0 | NS* |
| Paracervical length, left (cm) | 4.8±1.4 | 4.2±1.0 | NS* |
| Paracervical width, left (cm) | 3.3±0.8 | 3.6±0.9 | NS* |
| Vaginal length (cm) | 3.0±0.8 | 3.0±0.6 | NS* |
| No. of harvested pelvic LN | 25.8±7.8 | 26.9±8.1 | NS* |
| No. of harvested para-aortic LN | 5.9±4.7 | 6.2±4.8 | NS* |
| LN involvement | 2 (5.0) | 4 (8.7) | NS† |
| No. of dissected nerve fibers | 30 (17-45) | 12 (6-21) | <0.001‡ |
| Postoperative complication | 3 (7.5) | 2 (4.3) | NS† |
| Incisional hernia | 1 | 1 | |
| Infected lymphocele | 2 | 1 | |
| No. of cases of CIC | 3 (7.5) | 0 | <0.001† |
| Days for RU <50 mL | 18 (10-85) | 11 (7-26) | <0.001‡ |
| Postoperative radiotherapy | 15 (37.5) | 14 (31.1) | NS† |
| Follow-up duration (mo) | 101 (13-137) | 111 (13-139) | NS* |
| Recurrence | 2 (5.0) | 3 (6.5) | NS† |
| 10-Year DFS (%) | 94.9 | 92.4 | NS§ |
Values are presented as mean±SD, number (%), or median (range).
BMI, body mass index; CIC, clean intermittent catheterization; CRH, conventional radical hysterectomy; DFS, disease-free survival; FIGO, International Federation of Gynecology and Obstetrics; LN, lymph node; NS, not significant; NSRH, nerve-sparing radical hysterectomy; RU, residual urine.
*Student t-test. †Fisher exact test. ‡Mann-Whitney test. §Kaplan-Meier survival analysis.
2. Evaluation of urinary function
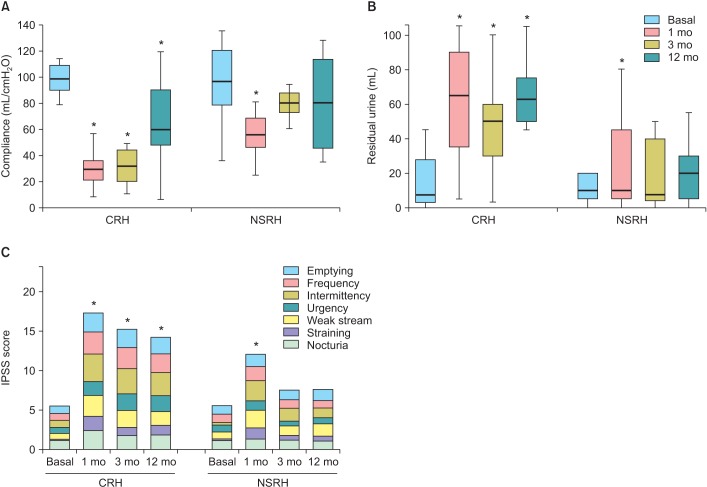
The median duration before the postvoid RU volume became less than 50 mL was 11 days (range, 7 to 26 days) among the patients in the NSRH group and was 18 days (range, 10 to 85 days) among the patients in the CRH group (p<0.001). No significant difference in the preoperative data of UDS was found between the two groups (p>0.05). Postoperative changes in UDS compared with preoperative data are shown in Table 2. At postoperative 1 month, almost all parameters of UDS were significantly changed in the CRH group, and several parameters including maximal flow rate, voided volume, RU, compliance, and maximal urethral pressure were also changed in the NSRH group. All changed parameters of USD in the NSRH group were recovered at postoperative 3 months examination, while changes in many parameters of USD in the CRH group were maintained 3 months later. One year after the operation, changes of bladder compliance and RU were still persistent in the CRH group (Fig. 3). For the evaluation of subjective urinary symptoms, postoperative IPSS scores were compared with preoperative IPSS scores (Table 3).
Table 2. Postoperative changes in the parameters of urodynamic study compared to preoperative basal values.
| Variable | Conventional radical hysterectomy | Nerve-sparing radical hysterectomy | ||||||
|---|---|---|---|---|---|---|---|---|
| Basal | 1 mo | 3 mo | 12 mo | Basal | 1 mo | 3 mo | 12 mo | |
| MFR (mL/sec) | 18.5 (8.9-63.9) | 10.5 (4,4-21,1)* | 16.5 (5.6-40.8) | 16.0 (8.3-25.2) | 18.5 (9.3-39.3) | 14.5 (5.0-49.5)* | 15.8 (6.7-35.2) | 15.5 (9.0-46.5) |
| AFR (mL/sec) | 8.7 (2.5-47.0) | 4.7 (1.0-11.3)* | 6.9 (3.4-46.6) | 6.1 (2.2-12.8) | 8,1 (2.2-65.0) | 6.4 (3.10-71.0) | 6.6 (2.6-56.0) | 7.2 (3.2-21.0) |
| VV (mL) | 368.5 (115.0-677.0) | 259.5 (56.0-604.0)* | 330.0 (85.0-564.0) | 380.0 (230.0-566.0) | 356.5 (142.0-779.0) | 308.5 (32.0-606.0)* | 407.5 (97.0-813.0) | 350.0 (120.0-566.0) |
| MDP (cmH2O) | 61.0 (23.0-181.0) | 54.5 (0-199.0)* | 53.5 (17.0-90.0) | 60.5 (1.0-143.0) | 44.0 (20.0-113.0) | 45.0 (16.0-106.0) | 43.0 (18.0-126.0) | 55.0 (22.0-144.0) |
| RU (mL) | 16.5 (0-80.0) | 70.0 (0-181.0)* | 51.5 (0-220.0)* | 51.0 (0-120.0)* | 10.0 (0-100.0) | 20.0 (0-100.0)* | 18.0 (0-120.0) | 20.0 (0-75.0) |
| Compliance (mL/cmH2O) | 93.8 (34.6-159.6) | 29.1 (3.5-82.4)* | 30.3 (4.5-95.6)* | 61.9 (6.5-194.3)* | 83.0 (32.1-169.9) | 52.5 (21.6-125.3)* | 80.4 (34.0-138.0) | 59.7 (4.9-294.3) |
| FVS (mL) | 209.5 (98.0-414.0) | 207.5 (90.0-343.0) | 242.0 (44.0-508.0) | 235.5 (109.0-312.0) | 193.5 (90.0-430.0) | 185.0 (129.0-461.0) | 212.0 (51.0-448.0) | 248.0 (80.0-389.0) |
| Urgency (mL) | 411.0 (190.0-659.0) | 371.9 (210.0-550.0) | 356.8 (97.0-630.0)* | 369.0 (302.0-450.0) | 375.5 (214.0-606.0) | 348.5 (230.0-584.0) | 400.0 (240.0-600.0) | 370.0 (176.0-550.0) |
| Capacity (mL) | 443.0 (206.0-674.0) | 395.3 (220.0-550.0)* | 376.1 (99.0-630.0) | 401.0 (330.0-462.0) | 415.0 (273.0-608.0) | 355.0 (240.0-586.0) | 429.0 (269.0-612.0) | 410.0 (181.0-550.0) |
| MUP (cmH2O) | 88.0 (36.0-158.0) | 73.5 (38.0-123.0)* | 76.5 (37.0-193.0)* | 76.5 (11.0-109.0)* | 97.0 (44.0-183.0) | 85.0 (43.0-151.0)* | 79.0 (19.0-143.0) | 96.0 (19.0-132.0) |
| MCP (cmH2O) | 88.0 (36.0-159.0) | 74.1 (34.0-122.0)* | 78.0 (37.0-194.0)* | 77.0 (12.0-111.0) | 95.5 (45.0-148.0) | 85.0 (43.0-148.0) | 84.0 (20.0-143.0) | 97.0 (19.0-116.0) |
| FUL (mm) | 92.0 (35.0-197.0) | 86.5 (36.0-218.0) | 89.5 (23.0-193.0) | 80.0 (27.0-117.0) | 85.0 (34.0-250.0) | 79.0 (27.0-214.0) | 76.5 (25.5-232.0) | 97.0 (56.0-132.0) |
Values are presented as median (range).
AFR, average flow rate; FUL, functional urethral length; FVS, first voiding sense; MCP, maximal closure pressure; MDP, maximal detrusor pressure; MFR, maximal flow rate; MUP, maximal urethral pressure; RU, residual urine; VV, voided volume.
*p<0.05, compared with preoperative basal data by Wilcoxon signed rank test.
Fig. 3. (A) Bladder compliance and (B) volume of residual urine were evaluated by urodynamic study preoperatively, and at 1, 3, and 12 months after conventional radical hysterectomy (CRH) or nervesparing radical hysterectomy (NSRH). (C) Subjective urinary symptoms were evaluated with the International Prostate Symptom Score (IPSS). Postoperative results were compared with preoperative basal values by Wilcoxon signed rank test. *p<0.05.
Table 3. Postoperative changes of International Prostate Symptom Score.
| Variable | Conventional radical hysterectomy | Nerve-sparing radical hysterectomy | ||||||
|---|---|---|---|---|---|---|---|---|
| Basal | 1 mo | 3 mo | 12 mo | Basal | 1 mo | 3 mo | 12 mo | |
| Emptying | 1 (0-5) | 2 (0-5)* | 3 (0-5)* | 2 (0-5)* | 1 (0-5) | 2 (0-5) | 1 (0-4) | 1 (0-5) |
| Frequency | 1 (0-5) | 3 (0-5)* | 3 (0-5)* | 2 (0-5)* | 1 (0-3) | 2 (0-5)* | 1 (0-3) | 1 (0-4) |
| Intermittency | 0 (0-5) | 4 (0-5)* | 3 (0-5)* | 3 (0-5)* | 0 (0-1) | 2 (1-5)* | 1 (0-4)* | 1 (0-5)* |
| Urgency | 0 (0-5) | 1 (0-5)* | 2 (0-5)* | 2 (0-5)* | 1 (0-5) | 1 (0-5) | 1 (0-2) | 0 (0-5) |
| Weak stream | 0 (0-5) | 3 (0-5)* | 2 (0-5)* | 1 (0-5)* | 1 (0-4) | 2 (0-5)* | 1 (0-4) | 1 (0-5) |
| Straining | 0 (0-1) | 2 (0-5)* | 1 (0-5)* | 1 (0-5)* | 0 (0-1) | 1 (0-5)* | 1 (0-1)* | 0 (0-5) |
| Nocturia | 1 (0-3) | 2 (1-4)* | 2 (0-3)* | 2 (0-3)* | 1 (0-3) | 1 (0-5) | 1 (0-3) | 1 (0-3) |
| Total | 3 (0-28) | 20 (3-28)* | 17 (3-26)* | 14 (3-33)* | 3 (0-20) | 11 (3-33)* | 9 (1-16) | 6 (0-24) |
Values are presented as median (range).
*p<0.05 compared with preoperative basal data by Wilcoxon signed rank test.
There were changes in every item for urinary symptoms, emptying, frequency, intermittency, urgency, weak stream, straining, and nocturia, after CRH and these changes were persistent for more than a year. On the contrary, there were no changes in all urinary symptoms except for intermittency in the NSRH group after a year, although four items for frequency, intermittency, weak stream, and straining indicated deterioration immediately after the operation.
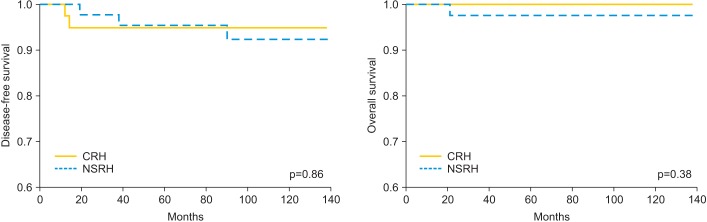
3. Evaluation of oncologic safety
The median duration of follow-up was 101 months (range, 13 to 137 months) in the CRH group and 111 months (range, 13 to 139 months) in the NSRH group. Ten-year DFS of the patients in the CRH and NSRH groups was 94.9% and 92.4%, respectively (Fig. 4). During the follow-up, two patients in the CRH group and three patients in the NSRH group developed recurrence. Three out of the five patients developed recurrence within 2 years, and one patient was diagnosed with pulmonary metastasis at 7-year follow-up. Four out of the five patients had systemic metastatic diseases, and only one patient was diagnosed para-aortic LN metastasis and was treated by laparoscopic resection followed by RT. One patient in the NSRH group was died with systemic metastatic lesions at 21 months after the initial diagnosis. The clinicopathologic features of the recurred cases are summarized in Supplementary Table 1. The 10-year DFS and OS were not different between the two groups.
Fig. 4. (A) Disease-free survival and (B) overall survival in patients with cervical cancer treated by conventional radical hysterectomy (CRH) or nerve-sparing radical hysterectomy (NSRH).
DISCUSSION
This was an RCT with the greatest number of cases enrolled and the longest duration of follow-up for the evaluation of efficacy and oncologic safety of NSRH till date. This means that the results of this prospective study strongly support the efficacy of NSRH in preventing urinary dysfunction without sacrifice of oncologic safety.
Ideal surgical management of cervical cancer should reduce early and late morbidity without compromising oncological disease control. Although CRH has been confirmed to be a standard treatment modality resulting in reduced risk of pelvic recurrence for FIGO stage IB1-IIA cervical cancer, it has been criticized for its high rate of postoperative pelvic organ dysfunction, especially urinary dysfunction. According to the literatures, urinary dysfunction (sensory loss, storing and voiding dysfunctions, urinary incontinence, and detrusor instability) is the most common long-term complication following CRH. The incidence has been reported to occur in 70% to 85% of reported studies [2,15,16]. Nowadays, postoperative QoL has become a more important issue, considering that more than 90% of the patients with cervical cancer could survive for a long time [2]. Deterioration of QoL after the surgery is believed to be the result of nerve injury during the procedure. In general, sympathetic branches of the hypogastric nerve and the vesical branch of the pelvic plexus stimulate the urethral sphincter and inhibit the detrusor muscle of the bladder, while parasympathetic branches of the pelvic splanchnic nerve and the vesical branch of the pelvic plexus relax the urethral sphincter and stimulate the detrusor muscle of the bladder. In order to maintain bladder function, those nerve networks should be preserved intact as much as possible unless these attempts sacrifice the therapeutic role of surgery. Although various attempts have been made to prevent pelvic organ dysfunction via autonomic nerve preservation, most of these studies provide either subjective or objective UDS data for a relatively short-time after the surgery [17,18,19,20].
It has been reported that RH is also associated with significant urodynamic changes and that these alterations may persist for at least 1 year following surgery [15,21,22]. Immediately after the operation, many factors including postoperative inflammation, local edema, temporary electrical injury, and decreased blood supply may influence the voiding function irrespective of nerve injury. Also, the bladder function after RH could be improved by 12 months after the operation [11,23,24]. Therefore, reliable data should be obtained for a long-time period of at least 1 year. The strong point of this study is in assessing the efficacy of NSRH in preserving voiding function. Both objective and subjective evaluations of voiding function using both UDS and IPSS were performed preoperative and at 1, 3, and 12 months after the surgery. In our study, increased RU volume and decreased compliance were maintained over a one year after the CRH. These results were compatible with those in the previous reports [15,21]. Differences in subjective urinary symptoms by questionnaire-based IPSS were more significant than that on UDS. Subjective voiding dysfunction seems to be strengthened because all parameters should be coordinated to maintain normal urination and even a malfunctioning detail could affect the general sense of normal voiding. The results from this study support the claim that NSRH is very effective method for increasing the QoL of cervical cancer survivors.
In terms of postoperative chronic morbidity, many literatures including this study have provided evidence of favorable outcomes for urinary function after NSRH compared with CRH [10,11,25], and a recent meta-analysis also showed that NSRH is associated with less bladder dysfunction and fewer complications [26]. Nevertheless, NSRH has not yet become popular among gynecologic surgeons. The most important barrier to the widespread use of this concept is the lack of sufficient survival data comparing the oncologic outcomes of NSRH with CRH. Although a lot of studies have already reported the results of NSRH, they had various limitations in ensuring the oncologic safety. Most of the studies were retrospective analysis without control or non-randomized historical comparison, and they mainly focused on the comparison of urinary dysfunctions between CRH and NSRH without longterm survival results.
For relevant survival analysis, well-designed RCTs with sufficient number of cases and adequate duration of follow-up are the basic prerequisites for drawing a conclusion. Till date, only three small-scale RCTs have reported the clinical data of NSRH [10,11,12], and two of them only focused on the efficacy of NSRH in reducing the postoperative morbidity without survival results [11,12], and the other study reported only the 2-year DFS rate for a small number of patients [10]. A recently published systematic review of oncological outcomes of NSRH concluded that the evidence addressing the oncologic safety of NSRH over that of CRH is neither adequate nor statistically relevant [27]. The authors emphasized that properly designed, prospective randomized noninferiority trial with more than five hundred cases in each arm is needed to assess the equality of survival [27].
Although the number of enrolled patients in this study were not enough to assess the noninferior oncologic outcome of NSRH compared to that of CRH, long-term follow-up duration of over 10-year period compensated for this limitation to some extent, and this study provided the evidence for the safety of NSRH. Late recurrence after 5 years occurs occasionally in patients with cervical cancer, although more than two-thirds of recurrences develop within 2 years after diagnosis. Therefore, 10-year DFS has been reported to show the total outcome of treatment for cervical cancer [28,29]. In fact, one out of the five recurred cases in this study was diagnosed with recurrence at the 7-year follow-up.
In conclusion, the results of this study provided evidence that NSRH should be regarded as a very effective modality to improve the QoL of cervical cancer survivors without sacrificing oncologic safety. A well-designed, large-scale prospective noninferiority trial should be conducted in near future to ensure the safety of NSRH.
ACKNOWLEDGMENTS
I (JWR) would like to thank Professor Dr. M. Höckel (Leipzig, Germany) and Professor Dr. A. Schneider (Berlin, Germany) for their excellent guidance and hospitality during my training in Germany. Artistic 3D-illustration of nervous system of pelvis was provided by HealthBreeze (Seoul, Korea). This work was supported by a grant from National Cancer Center of Korea (NCC 0310040).
Footnotes
CONFLICT OF INTEREST: No potential conflict of interest relevant to this article was reported.
SUPPLEMENTARY MATERIALS
(A) Longitudinal section of the paracervical tissue at 2 cm apart from the isthmus was fixed for nerve staining. (B) Immunohistochemical staining with S-100 protein for quantification of nerve fibers after conventional radical hysterectomy, and (C) nerve-sparing radical hysterectomy (×40).
Supplementary Table 1. Summary of clinicopathologic characteristics of recurred cases.
| Case no. | Group | Age (yr) | Pathology | FIGO stage | Site of recurrence | Duration from surgery (mo) | Treatment modality for recurrence | Current status |
|---|---|---|---|---|---|---|---|---|
| 1 | CRH | 43 | Adenocarcinoma | IB1 | PALN | 13 | Laparoscopic operation→RT | NED |
| 2 | NSRH | 45 | Adenocarcinoma | IB1 | Lung | 90 | Chemotherapy | NED |
| 3 | CRH | 51 | SCCA | IB1 | Lung | 15 | Resection→chemotherapy | NED |
| 4 | NSRH | 47 | SCCA | IIA | Lung, liver | 19 | Chemotherapy | DOD |
| 5 | NSRH | 47 | Adenocarcinoma | IB2 | Pelvis | 38 | Pelvic exenteration→RT | Alive with disease |
| Lung | 47 | Resection→chemotherapy |
CRH, conventional radical hysterectomy; DOD, death of disease; FIGO, International Federation of Gynecology and Obstetrics; NED, no evidence of disease; NSRH, nerve-sparing radical hysterectomy; PALN, para-aortic lymph node; RT, radiotherapy; SCCA, squamous cell carcinoma.
References
- 1.Donato DM. Surgical management of stage IB-IIA cervical carcinoma. Semin Surg Oncol. 1999;16:232–235. doi: 10.1002/(sici)1098-2388(199904/05)16:3<232::aid-ssu7>3.0.co;2-y. [DOI] [PubMed] [Google Scholar]
- 2.Zullo MA, Manci N, Angioli R, Muzii L, Panici PB. Vesical dysfunctions after radical hysterectomy for cervical cancer: a critical review. Crit Rev Oncol Hematol. 2003;48:287–293. doi: 10.1016/s1040-8428(03)00125-2. [DOI] [PubMed] [Google Scholar]
- 3.Ercoli A, Delmas V, Gadonneix P, Fanfani F, Villet R, Paparella P, et al. Classical and nerve-sparing radical hysterectomy: an evaluation of the risk of injury to the autonomous pelvic nerves. Surg Radiol Anat. 2003;25:200–206. doi: 10.1007/s00276-003-0137-7. [DOI] [PubMed] [Google Scholar]
- 4.Maas CP, Trimbos JB, DeRuiter MC, van de Velde CJ, Kenter GG. Nerve sparing radical hysterectomy: latest developments and historical perspective. Crit Rev Oncol Hematol. 2003;48:271–279. doi: 10.1016/s1040-8428(03)00122-7. [DOI] [PubMed] [Google Scholar]
- 5.Landoni F, Maneo A, Cormio G, Perego P, Milani R, Caruso O, et al. Class II versus class III radical hysterectomy in stage IB-IIA cervical cancer: a prospective randomized study. Gynecol Oncol. 2001;80:3–12. doi: 10.1006/gyno.2000.6010. [DOI] [PubMed] [Google Scholar]
- 6.Hockel M, Konerding MA, Heussel CP. Liposuction-assisted nerve-sparing extended radical hysterectomy: oncologic rationale, surgical anatomy, and feasibility study. Am J Obstet Gynecol. 1998;178:971–976. doi: 10.1016/s0002-9378(98)70533-2. [DOI] [PubMed] [Google Scholar]
- 7.Possover M, Stober S, Plaul K, Schneider A. Identification and preservation of the motoric innervation of the bladder in radical hysterectomy type III. Gynecol Oncol. 2000;79:154–157. doi: 10.1006/gyno.2000.5919. [DOI] [PubMed] [Google Scholar]
- 8.Trimbos JB, Maas CP, Deruiter MC, Peters AA, Kenter GG. A nerve-sparing radical hysterectomy: guidelines and feasibility in Western patients. Int J Gynecol Cancer. 2001;11:180–186. doi: 10.1046/j.1525-1438.2001.01023.x. [DOI] [PubMed] [Google Scholar]
- 9.Yabuki Y, Asamoto A, Hoshiba T, Nishimoto H, Nishikawa Y, Nakajima T. Radical hysterectomy: an anatomic evaluation of parametrial dissection. Gynecol Oncol. 2000;77:155–163. doi: 10.1006/gyno.1999.5723. [DOI] [PubMed] [Google Scholar]
- 10.Chen C, Li W, Li F, Liu P, Zhou J, Lu L, et al. Classical and nerve-sparing radical hysterectomy: an evaluation of the nerve trauma in cardinal ligament. Gynecol Oncol. 2012;125:245–251. doi: 10.1016/j.ygyno.2011.12.448. [DOI] [PubMed] [Google Scholar]
- 11.Wu J, Liu X, Hua K, Hu C, Chen X, Lu X. Effect of nerve-sparing radical hysterectomy on bladder function recovery and quality of life in patients with cervical carcinoma. Int J Gynecol Cancer. 2010;20:905–909. doi: 10.1111/IGC.0b013e3181df99c0. [DOI] [PubMed] [Google Scholar]
- 12.Chen L, Zhang WN, Zhang SM, Yang ZH, Zhang P. Effect of laparoscopic nerve-sparing radical hysterectomy on bladder function, intestinal function recovery and quality of sexual life in patients with cervical carcinoma. Asian Pac J Cancer Prev. 2014;15:10971–10975. doi: 10.7314/apjcp.2014.15.24.10971. [DOI] [PubMed] [Google Scholar]
- 13.Hockel M, Horn LC, Hentschel B, Hockel S, Naumann G. Total mesometrial resection: high resolution nerve-sparing radical hysterectomy based on developmentally defined surgical anatomy. Int J Gynecol Cancer. 2003;13:791–803. doi: 10.1111/j.1525-1438.2003.13608.x. [DOI] [PubMed] [Google Scholar]
- 14.Possover M. Technical modification of the nerve-sparing laparoscopy-assisted vaginal radical hysterectomy type 3 for better reproducibility of this procedure. Gynecol Oncol. 2003;90:245–247. doi: 10.1016/s0090-8258(03)00255-5. [DOI] [PubMed] [Google Scholar]
- 15.Scotti RJ, Bergman A, Bhatia NN, Ostergard DR. Urodynamic changes in urethrovesical function after radical hysterectomy. Obstet Gynecol. 1986;68:111–120. [PubMed] [Google Scholar]
- 16.Fishman IJ, Shabsigh R, Kaplan AL. Lower urinary tract dysfunction after radical hysterectomy for carcinoma of cervix. Urology. 1986;28:462–468. doi: 10.1016/0090-4295(86)90144-5. [DOI] [PubMed] [Google Scholar]
- 17.Raspagliesi F, Ditto A, Fontanelli R, Solima E, Hanozet F, Zanaboni F, et al. Nerve-sparing radical hysterectomy: a surgical technique for preserving the autonomic hypogastric nerve. Gynecol Oncol. 2004;93:307–314. doi: 10.1016/j.ygyno.2004.01.048. [DOI] [PubMed] [Google Scholar]
- 18.Fujii S, Takakura K, Matsumura N, Higuchi T, Yura S, Mandai M, et al. Anatomic identification and functional outcomes of the nerve sparing Okabayashi radical hysterectomy. Gynecol Oncol. 2007;107:4–13. doi: 10.1016/j.ygyno.2007.08.076. [DOI] [PubMed] [Google Scholar]
- 19.Charoenkwan K, Srisomboon J, Suprasert P, Tantipalakorn C, Kietpeerakool C. Nerve-sparing class III radical hysterectomy: a modified technique to spare the pelvic autonomic nerves without compromising radicality. Int J Gynecol Cancer. 2006;16:1705–1712. doi: 10.1111/j.1525-1438.2006.00649.x. [DOI] [PubMed] [Google Scholar]
- 20.Katahira A, Niikura H, Kaiho Y, Nakagawa H, Kurokawa K, Arai Y, et al. Intraoperative electrical stimulation of the pelvic splanchnic nerves during nerve-sparing radical hysterectomy. Gynecol Oncol. 2005;98:462–466. doi: 10.1016/j.ygyno.2005.05.004. [DOI] [PubMed] [Google Scholar]
- 21.Lin LY, Wu JH, Yang CW, Sheu BC, Lin HH. Impact of radical hysterectomy for cervical cancer on urodynamic findings. Int Urogynecol J Pelvic Floor Dysfunct. 2004;15:418–421. doi: 10.1007/s00192-004-1187-z. [DOI] [PubMed] [Google Scholar]
- 22.Kanao H, Fujiwara K, Ebisawa K, Hada T, Ota Y, Andou M. Various types of total laparoscopic nerve-sparing radical hysterectomies and their effects on bladder function. J Gynecol Oncol. 2014;25:198–205. doi: 10.3802/jgo.2014.25.3.198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ralph G, Tamussino K, Lichtenegger W. Urological complications after radical abdominal hysterectomy for cervical cancer. Baillieres Clin Obstet Gynaecol. 1988;2:943–952. doi: 10.1016/s0950-3552(98)80021-7. [DOI] [PubMed] [Google Scholar]
- 24.Todo Y, Kuwabara M, Watari H, Ebina Y, Takeda M, Kudo M, et al. Urodynamic study on postsurgical bladder function in cervical cancer treated with systematic nerve-sparing radical hysterectomy. Int J Gynecol Cancer. 2006;16:369–375. doi: 10.1111/j.1525-1438.2006.00345.x. [DOI] [PubMed] [Google Scholar]
- 25.Plotti F, Zullo MA, Montera R, Angioli R, Pierluigi BP. Bladder function after laparoscopic nerve-sparing radical hysterectomy. Gynecol Oncol. 2011;120:315. doi: 10.1016/j.ygyno.2010.10.027. [DOI] [PubMed] [Google Scholar]
- 26.Long Y, Yao DS, Pan XW, Ou TY. Clinical efficacy and safety of nerve-sparing radical hysterectomy for cervical cancer: a systematic review and meta-analysis. PLoS One. 2014;9:e94116. doi: 10.1371/journal.pone.0094116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Basaran D, Dusek L, Majek O, Cibula D. Oncological outcomes of nerve-sparing radical hysterectomy for cervical cancer: a systematic review. Ann Surg Oncol. 2015 Jan 23; doi: 10.1245/s10434-015-4377-7. http://dx.doi.org/10.1245/s10434-015-4377-7. [DOI] [PubMed] [Google Scholar]
- 28.Yeung AR, Amdur RJ, Morris CG, Morgan LS, Mendenhall WM. Long-term outcome after radiotherapy for FIGO stage IIIB and IVA carcinoma of the cervix. Int J Radiat Oncol Biol Phys. 2007;67:1445–1450. doi: 10.1016/j.ijrobp.2006.11.013. [DOI] [PubMed] [Google Scholar]
- 29.Liu J, Liu J, Li J, Chen Y, Guan X, Wu X, et al. Tumor-stroma ratio is an independent predictor for survival in early cervical carcinoma. Gynecol Oncol. 2014;132:81–86. doi: 10.1016/j.ygyno.2013.11.003. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(A) Longitudinal section of the paracervical tissue at 2 cm apart from the isthmus was fixed for nerve staining. (B) Immunohistochemical staining with S-100 protein for quantification of nerve fibers after conventional radical hysterectomy, and (C) nerve-sparing radical hysterectomy (×40).
Supplementary Table 1. Summary of clinicopathologic characteristics of recurred cases.
| Case no. | Group | Age (yr) | Pathology | FIGO stage | Site of recurrence | Duration from surgery (mo) | Treatment modality for recurrence | Current status |
|---|---|---|---|---|---|---|---|---|
| 1 | CRH | 43 | Adenocarcinoma | IB1 | PALN | 13 | Laparoscopic operation→RT | NED |
| 2 | NSRH | 45 | Adenocarcinoma | IB1 | Lung | 90 | Chemotherapy | NED |
| 3 | CRH | 51 | SCCA | IB1 | Lung | 15 | Resection→chemotherapy | NED |
| 4 | NSRH | 47 | SCCA | IIA | Lung, liver | 19 | Chemotherapy | DOD |
| 5 | NSRH | 47 | Adenocarcinoma | IB2 | Pelvis | 38 | Pelvic exenteration→RT | Alive with disease |
| Lung | 47 | Resection→chemotherapy |
CRH, conventional radical hysterectomy; DOD, death of disease; FIGO, International Federation of Gynecology and Obstetrics; NED, no evidence of disease; NSRH, nerve-sparing radical hysterectomy; PALN, para-aortic lymph node; RT, radiotherapy; SCCA, squamous cell carcinoma.