Abstract
Antipsychotic drugs are thought to produce secondary negative symptoms, which can also exacerbate primary negative symptoms. In the present study, we examined whether motivational deficits in particular were related to antipsychotic treatment in patients with schizophrenia in a dose-dependent manner. Five hundred and twenty individuals with schizophrenia who were receiving antipsychotic monotherapy for at least 6 months and followed prospectively were included in the present study. Participants were receiving one of five antipsychotic medications (olanzapine, perphenazine, quetiapine, risperidone, or ziprasidone), and analyses were conducted for patients receiving each drug separately. Analysis of covariance models were constructed to examine the effect of antipsychotic dose on level of motivational impairment, controlling for selected demographic and clinical variables (eg, positive symptoms). Level of motivation, or deficits therein, were evaluated using a derived measure from the Quality of Life Scale, and in addition with scores derived from the Positive and Negative Syndrome Scale. Antipsychotic dose was not related to the level of amotivation for any of the medications examined. Moreover, severity of sedation was not significantly related to the degree of amotivation. One hundred and twenty-one individuals were identified as antipsychotic-free at baseline, and after 6 months of antipsychotic treatment, no change in motivation was found. Chronic treatment with antipsychotics does not necessarily impede or enhance goal-directed motivation in patients with schizophrenia. It is possible that the negative impact of antipsychotics in this regard is overstated; conversely, the present results also indicate that we must look beyond antipsychotics in our efforts to improve motivation.
INTRODUCTION
Negative symptoms are a prevalent and prominent feature of schizophrenia (Bobes et al, 2010). These include many broad signs and symptoms including blunted affect, alogia, and avolition/amotivation. Amotivation refers specifically to the inability to initiate and sustain goal-directed activity relating to a diminished sense of drive. The use of this term herein does not connote a complete absence of motivation, but rather we imply a degree of motivational deficit. What would later be defined as negative symptoms were described decades before the introduction of antipsychotic medications (Kraepelin, 1919; Bleuler, 1950), clearly establishing primary negative symptoms as distinguishable from secondary medication effects. Further to this point, negative symptoms are evident in first-episode, antipsychotic-naïve individuals (Peralta et al, 2000), as well as individuals in the putative prodrome before the onset of frank psychosis (Piskulic et al, 2012).
Antipsychotic drugs have been identified as a causative factor in secondary (ie, iatrogenic) negative symptoms, which may also aggravate primary (ie, idiopathic) negative symptoms related to the underlying illness (Carpenter et al, 1988; Schooler, 1994; Kelley et al, 1999). In terms of mechanism of action, antipsychotics block dopamine (D2) receptors (Farde et al, 1988), and it is this reduction in dopaminergic transmission that has been linked to the dampened ability of organisms to attribute incentive salience and drive in a multitude of pre-clinical studies (Salamone and Correa, 2012). Whereas there is evidence that a single administration of an antipsychotic leads to some degree of motivation impairment (Artaloytia et al, 2006; Saeedi et al, 2006; Mas et al, 2013), although not consistently (Park et al, 2012), evidence linking chronic treatment to these deficits does not exist. Higher dopamine D2 receptor blockade has been linked to worse subjective experiences (ie, greater dysphoria) in patients chronically treated with antipsychotics (de Haan et al, 2003; Mizrahi et al, 2007), but subjective experience and dysphoria do not speak to motivation deficits per se. Seemingly paradoxically, negative symptoms have also been found to improve following antipsychotic treatment (Tollefson and Sanger, 1997; Leucht et al, 2009), even in non-psychotic individuals (McGlashan et al, 2006), and withdrawal of antipsychotic medication has been linked to worsening of negative symptom burden in patients with schizophrenia (Breier et al, 1987; Miller et al, 1994; Harvey et al, 1996; Weickert et al, 2003).
Several studies have examined whether higher doses of antipsychotics are related to more severe negative symptoms (broadly defined) and have failed to confirm such an association (Prosser et al, 1987; Tugg et al, 1997; Peralta et al, 2000); moreover, the average dose of antipsychotic received during acute exacerbation is not related to the degree of change in negative symptoms (Peralta et al, 2000). Other studies have failed to link higher antipsychotic occupancy of the dopamine D2 receptor with more severe negative symptoms, or with reduction in these symptoms (de Haan et al, 2003). More recent clinical studies examining patients chronically treated with antipsychotics have reported that patients receiving higher dosages of antipsychotic medication are not more impaired in their willingness to expend effort in pursuit of goals (Gold et al, 2013; Fervaha et al, 2013b; Hartmann et al, 2014; Wolf et al, 2014); moreover, at least a subpopulation of chronically treated patients do not differ from untreated healthy controls (Gold et al, 2013; Hartmann et al, 2014). In line with this, one pre-clinical investigation has demonstrated that goal pursuit following chronic haloperidol treatment is no different than following vehicle treatment (Bedard et al, 2011). These findings taken together suggest that chronic treatment with antipsychotic medication may not necessarily worsen the amotivational state associated with schizophrenia.
In the present study, we examine the effect of antipsychotics on motivational deficits in particular, rather than negative symptoms more broadly, as these symptoms have emerged as a discrete aspect of negative symptoms as supported by a host of factor analytic studies (Blanchard and Cohen, 2006), are differentially related to outcome variables (Sayers et al, 1996), and may therefore have different underlying mechanisms than other negative symptoms such as reduced emotional expression. Specifically, the present study examines whether motivational deficits were related to antipsychotics in a dose-dependent manner using a large sample of individuals maintained on selected antipsychotics. We further examined whether motivational deficits would worsen in antipsychotic-free individuals subsequently started on, and chronically treated with, a single antipsychotic medication. On the basis of the available clinical evidence, we hypothesized that antipsychotic dose would not be related to the degree of amotivation.
MATERIALS AND METHODS
Study Design
Data were collected as part of the Clinical Antipsychotic Trial of Intervention Effectiveness (CATIE) schizophrenia study; for which the details of the study design and primary results are reported elsewhere (Stroup et al, 2003; Lieberman et al, 2005). The CATIE project conducted between January 2001 and December 2004 at 57 sites in the United States was designed to examine the effectiveness of atypical and a single typical antipsychotic medication for the treatment of chronic schizophrenia.
Participants were eligible to participate in the CATIE study if they were between the ages of 18 and 65 years and had a diagnosis of schizophrenia confirmed using the Structured Clinical Interview for DSM-IV Axis I Disorders (First, 1997). Participants were excluded from the study if they had a diagnosis of schizoaffective disorder, mental retardation, or other cognitive disorders; had a documented history of treatment refractory illness; or had a serious and unstable medical condition. Eligible participants were initially randomized to olanzapine (7.5–30 mg per day), perphenazine (8–32 mg per day), quetiapine (200–800 mg per day), risperidone (1.5–6.0 mg per day), or ziprasidone (40–160 mg per day) under double-blind conditions and were followed for up to 18 months or until treatment was discontinued for any reason (Stroup et al, 2003). Patients could receive between one and four capsules of study medication, corresponding to the minimum and maximum amounts noted above.
The study was approved by the institutional ethics review board at each site, and written informed consent was obtained from the patients or their legal guardians. All participants demonstrated adequate decision-making capacity in regard to participating in the CATIE study as determined by the MacArthur Competence Assessment Tool (Appelbaum and Grisso, 2001).
Participants
Individuals who received the same antipsychotic medication for at least 6 months were included in the present analysis. Only individuals judged to have been actually receiving the medication were included in the present analysis (ie, rated as taking their medication ‘always' or between 75–100% of the time). Medication adherence was evaluated on a single global item based on all available information including pill count and information from patients (Stroup et al, 2003).
In addition, participants who reported not receiving any antipsychotic medication for at least the preceding 2 weeks were included in a separate analysis examining longitudinal change in level of motivation following 6 months of antipsychotic treatment. Notably, these participants were not medication-naive, but had received antipsychotic treatment in the past.
Measures
Motivation was evaluated using three items from the intrapsychic foundations subscale of the Heinrichs-Carpenter Quality of Life Scale (Heinrichs et al, 1984): curiosity, goal-directed motivation, and sense of purpose (Nakagami et al, 2008). The Quality of Life Scale is a rater-administered semi-structured interview instrument, and this derived measure of motivation is thought to index general motivation (ie, the ability or willingness to engage in goal-directed activities, not linked to any specific task or incentive scheme), and deficits therein. Though there is no gold standard instrument for the assessment of motivation in people with schizophrenia, this measure has been used in numerous empirical studies (Nakagami et al, 2008; Gard et al, 2009; Nakagami et al, 2010; Yamada et al, 2010; Saperstein et al, 2011; Vohs et al, 2013; Choi et al, 2013). We evaluated the reliability of this motivation measure in a subsample of individuals in the present study who did not evince a prospective change in antipsychotic dosage over 6 months. This measure demonstrated high longitudinal consistency (intraclass coefficient=0.82). Importantly, this measure has been found to be sensitive to change over time (Nakagami et al, 2010; Choi et al, 2013). In terms of construct validity, this measure has been shown to have significant overlap with other measures of amotivation (Saperstein et al, 2011), but conversely has not been linked with severity of positive symptoms (Vohs et al, 2013), or depressive symptoms (Nakagami et al, 2010). These latter findings of discriminant validity are echoed here; motivation was only weakly associated with severity of positive symptoms (r=−0.24, P<0.001) and depression as measured with the Calgary Depression Scale for Schizophrenia (r=−0.17, P<0.001) (Addington et al, 1992). In the present sample, a higher level of motivation was significantly associated with lower negative symptom burden (r=−0.46, P<0.001); however, this translates to approximately 21% overlap between the two measures, suggesting that the motivation measure is not redundant with more broad negative symptom assessment and therefore may be evaluating a somewhat distinct construct. Higher scores on this measure reflect a greater level of motivation.
The Positive and Negative Syndrome Scale (PANSS) was used to evaluate severity of psychopathology (Kay et al, 1987). The PANSS is a clinician-rated instrument that includes 30 items: 7 evaluating positive symptoms (eg, hallucinations), 7 evaluating negative symptoms (eg, blunted affect), and 16 assessing general psychopathology (eg, anxiety). Higher scores on this scale reflect greater symptom severity.
A secondary measure of amotivation was also employed. Specifically, a social amotivation score was derived by summing the following items from the PANSS: emotional withdrawal, passive apathetic withdrawal, and active social avoidance (Fervaha et al, 2014). These items have been shown to form a separate subfactor within the PANSS negative symptoms factor (Liemburg et al, 2013; Fervaha et al, 2014), and represent items that demonstrate the highest convergence with more detailed amotivation measures (Faerden et al, 2008). This measure was moderately related to the motivation measure derived from the Quality of Life Scale (r=−0.44, P<0.001). Notably, the Quality of Life Scale motivation measure demonstrated a significantly higher degree of overlap with the social amotivation score, compared with a diminished expression score also derived from the PANSS (r=−0.36, P<0.001; Steiger's test: z=2.19, P=0.01) (Fervaha et al, 2014). This PANSS-derived social amotivation score also demonstrated good test-retest reliability (intraclass coefficient=0.78). Higher scores on this social amotivation measure reflect greater motivational deficits.
Extrapyramidal symptoms were evaluated using an abbreviated version of the Simpson-Angus Scale (Simpson and Angus, 1970; Tracy et al, 1997). This instrument includes six items which are rated based on clinical examination, where higher scores denoting more severe extrapyramidal side effects. The specific items include: gait, arm dropping, shoulder shaking, elbow rigidity, wrist rigidity, and tremor.
Sedation (ie, sleepiness) and akinesia were evaluated using a single item which was rated on a 0 to 3 scale, where higher scores reflected greater severity. For these items, clinicians were instructed to not rate symptoms related to schizophrenia that, for example, are included in the PANSS.
Statistical Analyses
The effect of antipsychotic dose on motivation scores was examined using analysis of covariance models, adjusting for age, sex, and severity of positive symptoms. Separate models were constructed for each antipsychotic medication. Notably, although we include severity of positive symptoms as a covariate as an index of general clinical severity, the results remain unchanged if instead of this variable, severity of negative symptoms, or severity of overall symptoms are included in the models.
Collapsing across drugs and doses, another model was constructed to examine whether individuals differed on their level of motivation based on the medication they were receiving, and further whether there was differential change in motivation as a function of specific antipsychotic received. This latter analysis was conducted using a repeated-measures analysis of covariance model, adjusting for age, sex, and changes in positive symptoms.
Longitudinal change in the level of motivation was also examined in individuals who were antipsychotic-free at baseline. This was done by computing a repeated-measures analysis of variance model which did not include any covariates.
The relationships between the level of amotivation and severity of side effects such as sedation and akinesia were quantified using Spearman rank-order correlation coefficients. Statistical significance was set at P<0.05 (two-tailed) and analyses were carried out using SPSS version 20 (IBM Corporation, Armonk, NY).
RESULTS
Patient Characteristics
Sociodemographic and clinical characteristics of the study sample are presented in Table 1. Five hundred and twenty individuals who received that same antipsychotic medication for 6 months and had available data on motivation were included in the present study.
Table 1. Demographic and Clinical Characteristics for Study Sample.
| Variable | Mean (SD) or % | Range |
|---|---|---|
| Age (years) | 42.0 (11.3) | 18–66 |
| Sex (males) | 74.6 | — |
| Race | ||
| White | 63.0 | — |
| Black | 32.6 | — |
| Other | 4.4 | — |
| Employment status (unemployed) | 83.7 | — |
| Patient's education (years) | 12.1 (2.3) | 3–21 |
| Illness duration (years since first prescribed antipsychotic medication) | 15.1 (11.5) | 0–56 |
| Motivation score | 7.9 (4.2) | 0–18 |
| Social amotivation score | 9.2 (3.4) | 3–18 |
| Symptoms at 6 months | ||
| PANSS (total score) | 64.4 (16.6) | 30–122 |
| PANSS—positive subscale score | 14.6 (5.0) | 7–35 |
| PANSS—negative subscale score | 17.9 (5.9) | 7–37 |
| PANSS—general psychopathology subscale score | 31.9 (8.7) | 16–63 |
| Motivation score | 8.6 (4.2) | 0–18 |
| Social amotivation score | 8.3 (3.2) | 3–18 |
Abbreviations: PANSS: Positive and Negative Syndrome Scale.
Medication Type and Amotivation
The severity of motivational impairment for individuals receiving each medication for 6 months is reported in Table 2. No main effect of antipsychotic medication type on the level of motivation was observed (F1,506=0.62, P=0.43). Furthermore, there was no indication that the level of motivation differentially changed based on the specific antipsychotic medication received (drug-by-time interaction; F1,506=0.46, P=0.69), suggesting that specific antipsychotic drugs do not undermine, or promote, motivation to a differential degree.
Table 2. Severity of Amotivation Stratified by Antipsychotic Medication.
| Antipsychotic medication | Motivation at 6 months Mean (SD) | Social amotivation at 6 months Mean (SD) |
|---|---|---|
| Olanzapine (N=155)a | 8.3 (4.0) | 8.2 (3.3) |
| Dose 1 (7.5 mg; N=16) | 9.8 (5.5) | 7.0 (3.1) |
| Dose 2 (15 mg; N=49) | 9.1 (3.6) | 8.2 (3.5) |
| Dose 3 (22.5 mg; N=45) | 7.2 (4.0) | 7.9 (3.3) |
| Dose 4 (30 mg; N=44) | 7.8 (3.7) | 8.8 (3.0) |
| Perphenazine (N=88) | 8.5 (4.4) | 8.0 (3.5) |
| Dose 1 (8 mg; N=9) | 8.4 (3.6) | 6.9 (2.7) |
| Dose 2 (16 mg; N=29) | 9.9 (4.1) | 7.6 (3.2) |
| Dose 3 (24 mg; N=22) | 7.7 (4.2) | 8.9 (4.3) |
| Dose 4 (32 mg; N=28) | 7.8 (5.0) | 8.0 (3.3) |
| Quetiapine (N=100) | 9.0 (4.3) | 8.1 (2.8) |
| Dose 1 (200 mg; N=5) | 12.6 (1.9) | 8.0 (2.9) |
| Dose 2 (400 mg; N=31) | 8.9 (4.7) | 8.2 (2.9) |
| Dose 3 (600 mg; N=24) | 9.8 (4.1) | 7.0 (2.7) |
| Dose 4 (800 mg; N=40) | 8.1 (4.1) | 8.8 (2.7) |
| Risperidone (N=117)b | 8.6 (4.1) | 8.3 (2.9) |
| Dose 1 (1.5 mg; N=7) | 11.9 (2.1) | 6.0 (2.2) |
| Dose 2 (3 mg; N=43) | 9.3 (4.3) | 8.1 (2.9) |
| Dose 3 (4.5 mg; N=30) | 8.0 (3.7) | 8.5 (2.8) |
| Dose 4 (6 mg; N=34) | 7.7 (4.2) | 9.0 (3.0) |
| Ziprasidone (N=60) | 8.8 (4.6) | 8.1 (3.5) |
| Dose 1 (40 mg; N=2) | 8.5 (2.1) | 5.5 (2.1) |
| Dose 2 (80 mg; N=19) | 9.2 (5.4) | 8.1 (3.6) |
| Dose 3 (120 mg; N=16) | 9.6 (5.1) | 7.6 (4.0) |
| Dose 4 (160 mg; N=23) | 7.9 (3.6) | 8.7 (3.2) |
Dose information was missing for one participant.
Dose information was missing for three participants.
Side Effects and Amotivation
Clinical ratings of severity of sedation were not associated with the degree of motivational deficit (r=−0.02, P=0.63). Ratings of akinesia were, however, weakly, though statistically significantly, related to level of motivational deficit (r=−0.10, P=0.02); however, prospective changes in motivation were not related to changes in akinesia ratings (r=−0.07, P=0.16). Severity of extrapyramidal symptoms were also weakly, but statistically significantly, associated with severity of amotivation (r=−0.15, P=0.001); however, like the relationship with akinesia, prospective changes in extrapyramidal symptoms were not linked to changes in motivation (r=0.02, P=0.72).
Antipsychotic Dose and Amotivation
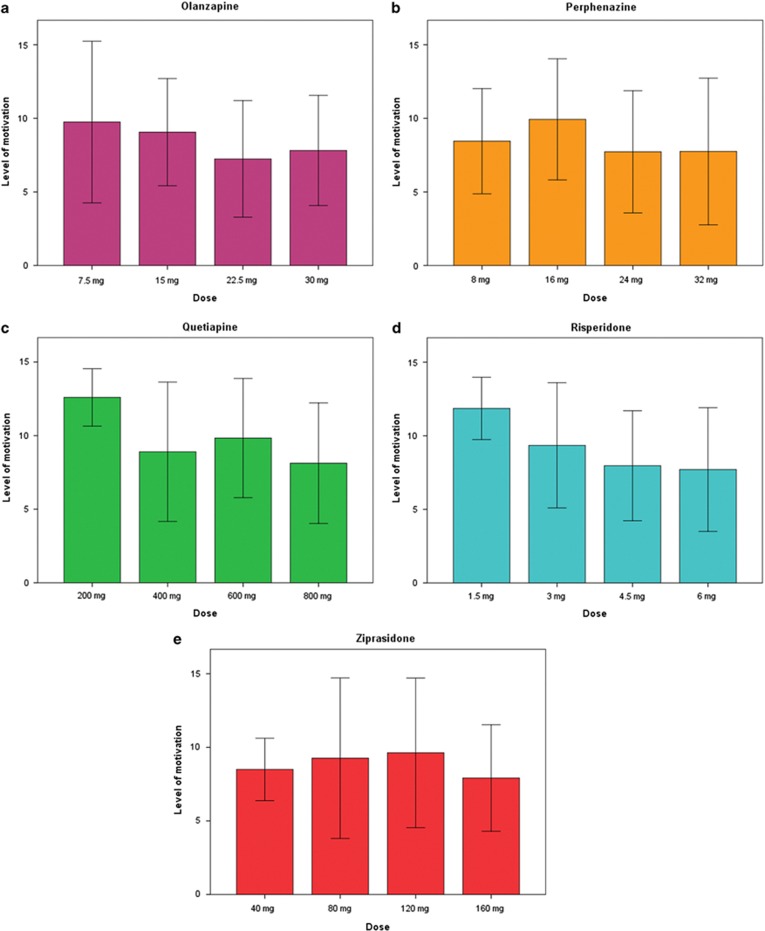
For each antipsychotic drug evaluated, dose did not emerge as a significant factor affecting level of motivation after 6 months of treatment (olanzapine: F3,147=1.62, P=0.19; perphenazine: F3,81=1.15, P=0.34; quetiapine: F3,93=1.80, P=0.15; risperidone: F3,106=1.25, P=0.30; ziprasidone: F3,53=0.27, P=0.85; Figure 1). This analysis was repeated excluding individuals receiving the lowest dose, as the number of individuals in this group was relatively small (Table 2), and still dose of antipsychotic was not a significant predictor of level of motivation (all P's>0.05). Adding sedation, akinesia, or extrapyramidal symptoms to the model as a covariate did not alter the results (all P's>0.05). Thus, antipsychotic dose was not a significant determinant of amotivation.
Figure 1.
Level of motivation stratified by dose for each antipsychotic drug: (a) olanzapine, (b) perphenazine, (c) quetiapine, (d) risperidone, and (e) ziprasidone. Higher score on this measure denote greater motivation, or less deficits therein. Error bars denote standard deviations.
Furthermore, prospective changes in the level of motivation from 6 to 12 months were not related to changes in antipsychotic dose for any antipsychotic medication (all P's>0.05), even after adjusting for longitudinal changes in positive symptoms (all P's>0.05). These results remained even when restricting the analyses to include only individuals who received a dose change (N=102; all P's>0.05).
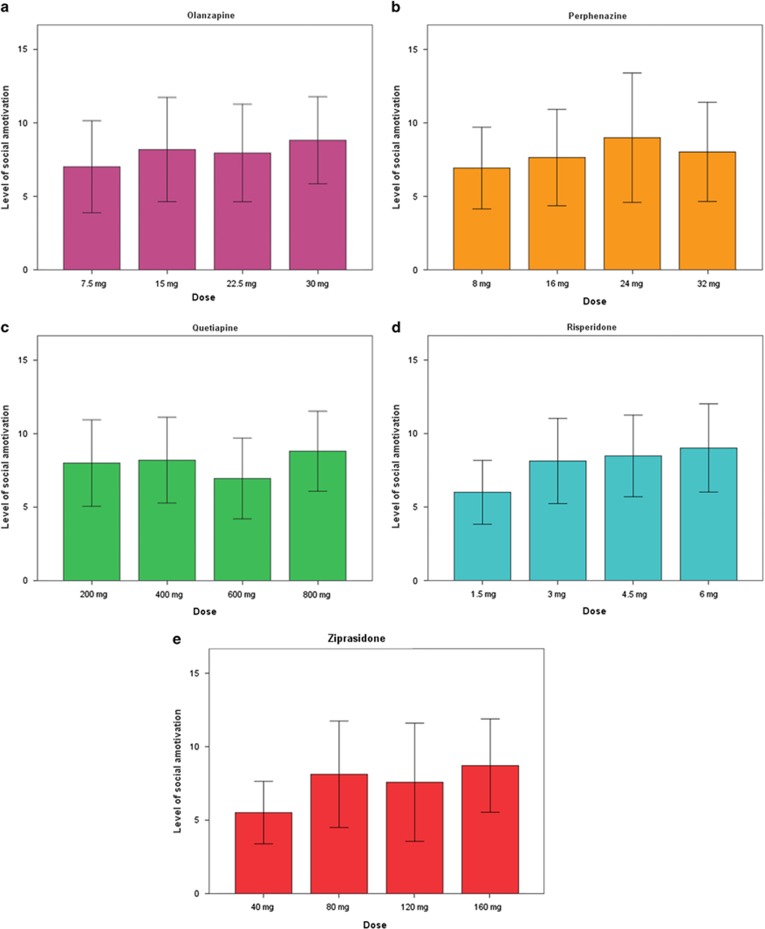
Next, we repeated the above analysis examining the effect of antipsychotic dose on amotivation, but utilized a measure of social amotivation derived from the PANSS. The results of this analysis were consistent with those found with the other motivation measure, namely, dose did not emerge as a significant factor affecting level of social amotivation after 6 months of treatment (olanzapine: F3,147=0.11, P=0.95; perphenazine: F3,81=0.82, P=0.49; quetiapine: F3,93=1.32, P=0.27; risperidone: F3,106=1.24, P=0.30; ziprasidone: F3,53=0.51, P=0.68; Figure 2). This remained so even after excluding the relatively small number of individuals receiving the lowest dose (all P's>0.05).
Figure 2.
Level of social amotivation stratified by dose for each antipsychotic drug: (a) olanzapine, (b) perphenazine, (c) quetiapine, (d) risperidone, and (e) ziprasidone. Higher score on this measure denote greater severity of motivational deficits. Error bars denote standard deviations.
Initiating Antipsychotic Treatment
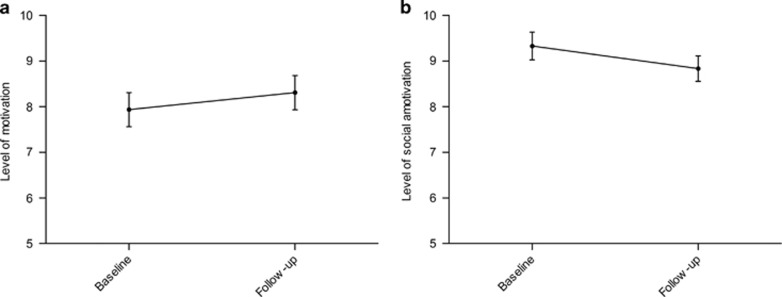
At baseline, 121 individuals reported not receiving any antipsychotic medication and had both baseline and follow-up motivation data. We examined whether there was any change in the level of motivation after these individuals received antipsychotic medication for 6 months. Going from an antipsychotic-free state to longer-term (ie, non-acute) treatment with antipsychotics did not result in a significant change in the degree of observed motivational deficits (F1,120=1.02, P=0.31; Figure 3a). In fact, there was a nominal increase in motivation, rather than decrease (score at baseline=7.4, SD=4.1; score at follow-up=8.3, SD=4.1). This remained the case for each individual antipsychotic examined; 6 months of treatment with olanzapine, perphenazine, quetiapine, risperidone, or ziprasidone did not significantly change level of motivation (all P's>0.05).
Figure 3.
Change in the level of motivation from an antipsychotic-free state (baseline), and after 6 months of antipsychotic treatment (follow-up). (a) Level of motiation as measured by the Quality of Life Scale is plotted, where higher scores denote greater motivation. (b) Level of social amotiation as measured by the Positive and Negative Syndrome Scale is plotted, where higher scores denote greater amotivation, or less motivation. Error bars reflect standard error of the mean.
Adding age, sex, and prospective change in positive symptoms into a repeated measures analysis of variance model did not alter the findings; there was no change in the level of motivation after 6 months of antipsychotic treatment (F1,115=0.12, P=0.73). This remained true for each antipsychotic medication examined (all P's>0.05).
We also examined changes in social amotivation after these antipsychotic-free individuals received medication for 6 months. The results here too were consistent with those found with the other motivation measure; receipt of antipsychotics did not result in a significant change in the severity of social motivation deficits (F1,118=3.80, P=0.054; Figure 3b). Though a trend for change was observed for social amotivation, the direction of change denotes improvement in motivation rather than worsening (score at baseline=9.3, SD=3.3; score at follow-up=8.8, SD=3.1). Adding age, sex, and prospective change in positive symptoms into a repeated measures analysis of variance model did not alter these findings; there was no change in social amotivation scores after 6 months of antipsychotic treatment (F1,115=0.03, P=0.86). This remained true for each antipsychotic medication examined (all P's>0.05).
DISCUSSION
The present study examined whether higher antipsychotic doses, given chronically, were linked to greater deficits in motivated behavior. We failed to find such a relationship. Though previous studies have linked antipsychotics with sedation (Lieberman et al, 2005), this too was not related to the degree of amotivation in this investigation. Finally, chronic treatment with antipsychotics did not prospectively diminish motivation compared with baseline in individuals who were antipsychotic-free. The present findings therefore argue against the notion that antipsychotic drugs cause or worsen amotivation in patients with schizophrenia.
Though some previous work has linked antipsychotics to aberrant reward-system functioning (Juckel et al, 2006), more recent findings suggest that these medications may actually improve functioning within this circuit (Lahti et al, 2009; Nielsen et al, 2012). This seems at odds with previous studies demonstrating that acute (ie, single) doses of antipsychotics negatively affect motivation and reward processing (Artaloytia et al, 2006; Saeedi et al, 2006). The present study only examined relatively chronic effects of antipsychotics (ie, differences in motivation after 6 months of treatment), and therefore cannot speak to the relatively acute effects of antipsychotics and potential differences in findings therein. Nonetheless, the present study does demonstrate a lack of effect of chronic antipsychotic treatment on motivation. This raises the question as to why there is discrepancy in effects of acute and chronic dosing. We speculate that several factors might be involved. First, individuals may habituate to the sedative effects of these medications, a process which could involve compensatory (neurobiological) changes. Second, it is possible that antipsychotics bias the type of goals that treated individuals pursue, and that although motivated behavior in general is not altered, underlying processing of reward attributes is altered causing a shift in goals being pursued. This should be directly tested in future work.
The mechanism(s) that might underlie our findings of chronic treatment with antipsychotics not undermining motivation remain to be elucidated. As the majority of pre-clinical studies examining the effects of antipsychotics on motivated behavior have employed acute dosing paradigms, parallels to the present study, and indeed real-world practice, cannot be drawn. We can nonetheless speculate as to some potential candidate mechanisms. One such mechanism involves habituation or the development of tolerance to antipsychotic medications. There is in fact several pre-clinical studies that have documented tolerance-like effects after chronic exposure to antipsychotics (Samaha et al, 2007), whereas other studies have documented that the acute and chronic effects of antipsychotics are distinct both behaviorally and neurobiologically (Amato et al, 2011). These effects have been linked to both increased number of dopamine D2 receptors (Samaha et al, 2007), as well as increased sensitivity of the receptors (Bedard et al, 2011). Increased dopamine D2 receptor expression outside the context of antipsychotics has in fact been linked with increases in goal-directed behavior (Trifilieff et al, 2013). Clinically, the number of dopamine D2 receptors has been suggested to be slightly increased in medicated patients with schizophrenia, a finding that is not observed in antipsychotic-naive individuals (Howes et al, 2012). It should be underscored that these findings have not been linked to motivated behavior per se, and as such future pre-clinical work should first examine whether chronic, rather than acute, antipsychotic exposure is linked with motivational deficits, and second determine potential neurobiological mechanisms underlying this plasticity.
Motivation is a multi-faceted construct encompassing multiple underlying and overlapping, yet distinct, processes (Barch and Dowd, 2010; Fervaha et al, 2013a). The two measures used in the present investigation evaluate subjective reports of drive and behavioral output as it relates to the pursuit of goals, including social interactions in the case of the PANSS social amotivation measure. These measures, however, do not disentangle the precise processes that ultimately manifest as goal-directed behavior or ‘motivation.' In fact, across-studies clinical ratings of amotivation have been found to be related to a number of reward processes including, for example, effort cost computations (Fervaha et al, 2013b; Gold et al, 2013; Hartmann et al, 2014; Wolf et al, 2014), and reinforcement learning (Waltz et al, 2011; Vogel et al, 2013). It is important to move beyond examining effects of various variables, in our case, the effect of antipsychotic medication, on ‘motivation' more broadly defined toward examining these effects on underlying subprocesses, ideally evaluating multiple reward-related components concurrently. Though several recent studies have examined specific reward processes, few, to our knowledge, have examined multiple processes within the same subjects. It would be valuable to know whether chronic antipsychotic treatment differentially affects certain approach-related behaviors while sparing others; pre-clinical studies are well positioned to answer such questions.
The present results do not refute the existence of antipsychotic-induced adverse effects such as akinetic extrapryamidal symptoms, which have long been linked to treatment with these mediations (Rifkin, 1975). However, the present results suggest that such akinesia is only weakly linked with motivation, at least as evaluated in the present study (ie, the initiation and pursuit of goals). Akinesia is also present in antipsychotic-naive patients with schizophrenia and in these individuals linked with higher negative symptom burden (Peralta et al, 2000). This relationship, observed before initiation of antipsychotics, suggests that akinesia itself is not solely an iatrogenic feature of the illness, and may obfuscate attempts to identify drug-induced side effects, especially secondary negative symptoms.
A strength of the present investigation is its examination of dose across multiple antipsychotic drug types, including conventional as well as atypical, but doing so individually rather than collapsing across medications and using a crude conversion (eg, chlorpromazine equivalents). At the same time, the present study has several limitations that should be mentioned. First, our first set of analyses was restricted to the dose of antipsychotic received, rather than plasma or brain levels. Future studies would be well positioned to replicate and extend the findings presented herein to examine more proximal effects of antipsychotic drugs, using, for example, positron emission tomography. Second, medication dosing was not assigned randomly, but rather determined based on real-world clinical decisions, a limitation shared by naturalistic investigations and empirical studies employing fixed, flexible dosing. Third, as motivation was not assessed directly following initiation of antipsychotic medication (ie, within a few days), we were not able to directly contrast acute and more chronic treatment with these drugs; nonetheless, our results hold for the latter. Fourth, the analysis examining the effect of initiating antipsychotics was carried out in a drug-free, but previously treated, population rather than in antipsychotic-naïve individuals. Fifth, the measure of motivation employed involved both patient self-report and clinician judgment, rather than objective assessment. Given the importance of motivational deficits, especially in terms of functioning (Fervaha et al, 2014), it is imperative that future studies determine the effect of chronically administered antipsychotic medication on objective behavioral assessments of goal-directed motivation (eg, effort-based decision making), ideally employing longitudinal designs. Last, our analysis included only five medications. Although these spanned both typical and atypical agents, it remains possible that specific antipsychotics not examined here have an effect on motivation. Related to this point, the present study did not include very high doses, but rather included doses reflective of current practice.
It has long been held that antipsychotic medications can produce secondary negative symptoms (Carpenter et al, 1988; Schooler, 1994; Kelley et al, 1999), which in turn can exacerbate primary negative symptoms. Amotivation is considered an important feature of these symptoms; however, the present study did not find evidence that these medications when given over a longer period of time diminish motivation. Moreover, we failed to find a dose-dependent relationship between antipsychotics and amotivation. Our findings raise the possibility that individuals may habituate to, at least some of the side effects of these medications, and that these medications do not necessarily undermine goal-directed motivation. It should be noted that we found no evidence that a larger amount of antipsychotic received was associated with greater amotivation; but by the same token, we also did not find evidence that higher doses of antipsychotic promote motivation, suggesting that novel treatments targeting different mechanisms are needed for these impairments.
FUNDING AND DISCLOSURE
Mr Fervaha and Dr Fletcher have no competing interests to disclose. Dr Takeuchi has received manuscript fees from Dainippon Sumitomo Pharma. Dr Lee has received consultant fees from Roche. Dr Foussias has been involved in research sponsored by Medicure Inc., and Neurocrine Bioscience; served on advisory boards for Roche; and has received speaker fees from Roche, Lundbeck, and Novartis. Dr Agid has received research support from Pfizer Inc. and Janssen-Ortho; consultant fees from Janssen-Ortho, Eli Lilly Inc. US, Eli Lilly Canada, Sepreacor, Sunovion and Lundbeck; and speaker's fees from Janssen-Ortho, Eli Lilly Inc. US, Eli Lilly Canada, Novartis, Sepracor and Sunovion. Dr Remington has received research support from the Schizophrenia Society of Ontario, CIHR, Research Hospital Fund—Canada Foundation for Innovation, Canadian Diabetes Association, Novartis Canada, Medicure Inc., and Neurocrine Bioscience; as a co-investigator he has received research support from the Canadian Psychiatric Research Foundation and Pfizer Inc.; consultant fees from Laboratorios Farmacéuticos ROVI, Synchroneuron, Novartis, and Roche; and speaker's fees from Novartis.
Acknowledgments
Data used in the preparation of this article were obtained from the limited access datasets (Version 1) distributed from the NIH-supported ‘Clinical Antipsychotic Trials of Intervention Effectiveness in Schizophrenia' (CATIE-Sz). This is a multisite, clinical trial of persons with schizophrenia comparing the effectiveness of randomly assigned medication treatment. The study was supported by NIMH Contract #N01MH90001 to the University of North Carolina at Chapel Hill. The ClinicalTrials.gov identifier is NCT00014001. This manuscript reflects the views of the authors and may not reflect the opinions or views of the CATIE-Sz Study Investigators or the NIH.
References
- Addington D, Addington J, Maticka-Tyndale E, Joyce J. Reliability and validity of a depression rating scale for schizophrenics. Schizophr Res. 1992;6:201–208. doi: 10.1016/0920-9964(92)90003-n. [DOI] [PubMed] [Google Scholar]
- Amato D, Natesan S, Yavich L, Kapur S, Muller CP. Dynamic regulation of dopamine and serotonin responses to salient stimuli during chronic haloperidol treatment. Int J Neuropsychopharmacol. 2011;14:1327–1339. doi: 10.1017/S1461145711000010. [DOI] [PubMed] [Google Scholar]
- Appelbaum PS, Grisso T. MacArthur competence assessment tool for clinical research (MacCAT-CR) Professional Resource Press: Sarasota, FL; 2001. [Google Scholar]
- Artaloytia JF, Arango C, Lahti A, Sanz J, Pascual A, Cubero P, et al. Negative signs and symptoms secondary to antipsychotics: a double-blind, randomized trial of a single dose of placebo, haloperidol, and risperidone in healthy volunteers. Am J Psychiatry. 2006;163:488–493. doi: 10.1176/appi.ajp.163.3.488. [DOI] [PubMed] [Google Scholar]
- Barch DM, Dowd EC. Goal representations and motivational drive in schizophrenia: the role of prefrontal-striatal interactions. Schizophr Bull. 2010;36:919–934. doi: 10.1093/schbul/sbq068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bedard AM, Maheux J, Levesque D, Samaha AN. Continuous, but not intermittent, antipsychotic drug delivery intensifies the pursuit of reward cues. Neuropsychopharmacology. 2011;36:1248–1259. doi: 10.1038/npp.2011.10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blanchard JJ, Cohen AS. The structure of negative symptoms within schizophrenia: implications for assessment. Schizophr Bull. 2006;32:238–245. doi: 10.1093/schbul/sbj013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bleuler E. Dementia Praecox or the group of schizophrenias. International Universities Press: New York; 1950. [Google Scholar]
- Bobes J, Arango C, Garcia-Garcia M, Rejas J. Prevalence of negative symptoms in outpatients with schizophrenia spectrum disorders treated with antipsychotics in routine clinical practice: findings from the CLAMORS study. J Clin Psychiatry. 2010;71:280–286. doi: 10.4088/JCP.08m04250yel. [DOI] [PubMed] [Google Scholar]
- Breier A, Wolkowitz OM, Doran AR, Roy A, Boronow J, Hommer DW, et al. Neuroleptic responsivity of negative and positive symptoms in schizophrenia. Am J Psychiatry. 1987;144:1549–1555. doi: 10.1176/ajp.144.12.1549. [DOI] [PubMed] [Google Scholar]
- Carpenter WT, Jr, Heinrichs DW, Wagman AM. Deficit and nondeficit forms of schizophrenia: the concept. Am J Psychiatry. 1988;145:578–583. doi: 10.1176/ajp.145.5.578. [DOI] [PubMed] [Google Scholar]
- Choi KH, Fiszdon JM, Bell MD. Beyond cognition: a longitudinal investigation of the role of motivation during a vocational rehabilitation program. J Nerv Ment Dis. 2013;201:173–178. doi: 10.1097/NMD.0b013e3182848bd4. [DOI] [PubMed] [Google Scholar]
- de Haan L, van Bruggen M, Lavalaye J, Booij J, Dingemans PM, Linszen D. Subjective experience and D2 receptor occupancy in patients with recent-onset schizophrenia treated with low-dose olanzapine or haloperidol: a randomized, double-blind study. Am J Psychiatry. 2003;160:303–309. doi: 10.1176/appi.ajp.160.2.303. [DOI] [PubMed] [Google Scholar]
- Faerden A, Nesvag R, Barrett EA, Agartz I, Finset A, Friis S, et al. Assessing apathy: the use of the Apathy Evaluation Scale in first episode psychosis. Eur Psychiatry. 2008;23:33–39. doi: 10.1016/j.eurpsy.2007.09.002. [DOI] [PubMed] [Google Scholar]
- Farde L, Wiesel FA, Halldin C, Sedvall G. Central D2-dopamine receptor occupancy in schizophrenic patients treated with antipsychotic drugs. Arch Gen Psychiatry. 1988;45:71–76. doi: 10.1001/archpsyc.1988.01800250087012. [DOI] [PubMed] [Google Scholar]
- Fervaha G, Foussias G, Agid O, Remington G. Motivational and neurocognitive deficits are central to the prediction of longitudinal functional outcome in schizophrenia. Acta Psychiatr Scand. 2014;130:290–299. doi: 10.1111/acps.12289. [DOI] [PubMed] [Google Scholar]
- Fervaha G, Foussias G, Agid O, Remington G. Neural substrates of effort computation in schizophrenia. Neurosci Biobehav Rev. 2013;37:2649–2665. doi: 10.1016/j.neubiorev.2013.09.001. [DOI] [PubMed] [Google Scholar]
- Fervaha G, Graff-Guerrero A, Zakzanis KK, Foussias G, Agid O, Remington G. Incentive motivation deficits in schizophrenia reflect effort computation impairments during cost-benefit decision-making. J Psychiatr Res. 2013;47:1590–1596. doi: 10.1016/j.jpsychires.2013.08.003. [DOI] [PubMed] [Google Scholar]
- First MB. User's guide for the Structured clinical interview for DSM-IV axis I disorders SCID-I: clinician version. Amer Psychiatric Pub Inc: Washington, DC; 1997. [Google Scholar]
- Gard DE, Fisher M, Garrett C, Genevsky A, Vinogradov S. Motivation and its relationship to neurocognition, social cognition, and functional outcome in schizophrenia. Schizophr Res. 2009;115:74–81. doi: 10.1016/j.schres.2009.08.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gold JM, Strauss GP, Waltz JA, Robinson BM, Brown JK, Frank MJ. Negative symptoms of schizophrenia are associated with abnormal effort-cost computations. Biol Psychiatry. 2013;74:130–136. doi: 10.1016/j.biopsych.2012.12.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hartmann MN, Hager OM, Reimann AV, Chumbley JR, Kirschner M, Seifritz E, et al. 22 July2014Apathy but not diminished expression in schizophrenia is associated with discounting of monetary rewards by physical effort Schizophr Bull; e-pub ahead of print.. [DOI] [PMC free article] [PubMed]
- Harvey PD, Davidson M, White L, Keefe RS, Hirschowitz J, Mohs RC, et al. Empirical evaluation of the factorial structure of clinical symptoms in schizophrenia: effects of typical neuroleptics on the brief psychiatric rating scale. Biol Psychiatry. 1996;40:755–760. doi: 10.1016/0006-3223(95)00486-6. [DOI] [PubMed] [Google Scholar]
- Heinrichs DW, Hanlon TE, Carpenter WT., Jr The Quality of Life Scale: an instrument for rating the schizophrenic deficit syndrome. Schizophr Bull. 1984;10:388–398. doi: 10.1093/schbul/10.3.388. [DOI] [PubMed] [Google Scholar]
- Howes OD, Kambeitz J, Kim E, Stahl D, Slifstein M, Abi-Dargham A, et al. The nature of dopamine dysfunction in schizophrenia and what this means for treatment: meta-analysis of imaging studies. Arch Gen Psychiatry. 2012;69:776–786. doi: 10.1001/archgenpsychiatry.2012.169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Juckel G, Schlagenhauf F, Koslowski M, Filonov D, Wustenberg T, Villringer A, et al. Dysfunction of ventral striatal reward prediction in schizophrenic patients treated with typical, not atypical, neuroleptics. Psychopharmacology (Berl) 2006;187:222–228. doi: 10.1007/s00213-006-0405-4. [DOI] [PubMed] [Google Scholar]
- Kay SR, Fiszbein A, Opler LA. The positive and negative syndrome scale (PANSS) for schizophrenia. Schizophr Bull. 1987;13:261–276. doi: 10.1093/schbul/13.2.261. [DOI] [PubMed] [Google Scholar]
- Kelley ME, van Kammen DP, Allen DN. Empirical validation of primary negative symptoms: independence from effects of medication and psychosis. Am J Psychiatry. 1999;156:406–411. doi: 10.1176/ajp.156.3.406. [DOI] [PubMed] [Google Scholar]
- Kraepelin E. Dementia Praecox and Paraphrenia. Livingstone: Edinburgh, UK; 1919. [Google Scholar]
- Lahti AC, Weiler MA, Holcomb HH, Tamminga CA, Cropsey KL. Modulation of limbic circuitry predicts treatment response to antipsychotic medication: a functional imaging study in schizophrenia. Neuropsychopharmacology. 2009;34:2675–2690. doi: 10.1038/npp.2009.94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leucht S, Arbter D, Engel RR, Kissling W, Davis JM. How effective are second-generation antipsychotic drugs? A meta-analysis of placebo-controlled trials. Mol Psychiatry. 2009;14:429–447. doi: 10.1038/sj.mp.4002136. [DOI] [PubMed] [Google Scholar]
- Lieberman JA, Stroup TS, McEvoy JP, Swartz MS, Rosenheck RA, Perkins DO, et al. Effectiveness of antipsychotic drugs in patients with chronic schizophrenia. N Engl J Med. 2005;353:1209–1223. doi: 10.1056/NEJMoa051688. [DOI] [PubMed] [Google Scholar]
- Liemburg E, Castelein S, Stewart R, van der Gaag M, Aleman A, Knegtering H. Two subdomains of negative symptoms in psychotic disorders: established and confirmed in two large cohorts. J Psychiatr Res. 2013;47:718–725. doi: 10.1016/j.jpsychires.2013.01.024. [DOI] [PubMed] [Google Scholar]
- Mas S, Gasso P, Fernandez de Bobadilla R, Arnaiz JA, Bernardo M, Lafuente A. Secondary nonmotor negative symptoms in healthy volunteers after single doses of haloperidol and risperidone: a double-blind, crossover, placebo-controlled trial. Hum Psychopharmacol. 2013;28:586–593. doi: 10.1002/hup.2350. [DOI] [PubMed] [Google Scholar]
- McGlashan TH, Zipursky RB, Perkins D, Addington J, Miller T, Woods SW, et al. Randomized, double-blind trial of olanzapine versus placebo in patients prodromally symptomatic for psychosis. Am J Psychiatry. 2006;163:790–799. doi: 10.1176/ajp.2006.163.5.790. [DOI] [PubMed] [Google Scholar]
- Miller DD, Flaum M, Arndt S, Fleming F, Andreasen NC. Effect of antipsychotic withdrawal on negative symptoms in schizophrenia. Neuropsychopharmacology. 1994;11:11–20. doi: 10.1038/npp.1994.31. [DOI] [PubMed] [Google Scholar]
- Mizrahi R, Rusjan P, Agid O, Graff A, Mamo DC, Zipursky RB, et al. Adverse subjective experience with antipsychotics and its relationship to striatal and extrastriatal D2 receptors: a PET study in schizophrenia. Am J Psychiatry. 2007;164:630–637. doi: 10.1176/ajp.2007.164.4.630. [DOI] [PubMed] [Google Scholar]
- Nakagami E, Hoe M, Brekke JS. The prospective relationships among intrinsic motivation, neurocognition, and psychosocial functioning in schizophrenia. Schizophr Bull. 2010;36:935–948. doi: 10.1093/schbul/sbq043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nakagami E, Xie B, Hoe M, Brekke JS. Intrinsic motivation, neurocognition and psychosocial functioning in schizophrenia: testing mediator and moderator effects. Schizophr Res. 2008;105:95–104. doi: 10.1016/j.schres.2008.06.015. [DOI] [PubMed] [Google Scholar]
- Nielsen MO, Rostrup E, Wulff S, Bak N, Broberg BV, Lublin H, et al. Improvement of Brain Reward Abnormalities by Antipsychotic Monotherapy in Schizophrenia. Arch Gen Psychiatry. 2012;69:1195–1204. doi: 10.1001/archgenpsychiatry.2012.847. [DOI] [PubMed] [Google Scholar]
- Park CH, Park TW, Yang JC, Lee KH, Huang GB, Tong Z, et al. No negative symptoms in healthy volunteers after single doses of amisulpride, aripiprazole, and haloperidol: a double-blind placebo-controlled trial. Int Clin Psychopharmacol. 2012;27:114–120. doi: 10.1097/YIC.0b013e3283502773. [DOI] [PubMed] [Google Scholar]
- Peralta V, Cuesta MJ, Martinez-Larrea A, Serrano JF. Differentiating primary from secondary negative symptoms in schizophrenia: a study of neuroleptic-naive patients before and after treatment. Am J Psychiatry. 2000;157:1461–1466. doi: 10.1176/appi.ajp.157.9.1461. [DOI] [PubMed] [Google Scholar]
- Piskulic D, Addington J, Cadenhead KS, Cannon TD, Cornblatt BA, Heinssen R, et al. Negative symptoms in individuals at clinical high risk of psychosis. Psychiatry Res. 2012;196:220–224. doi: 10.1016/j.psychres.2012.02.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prosser ES, Csernansky JG, Kaplan J, Thiemann S, Becker TJ, Hollister LE. Depression, parkinsonian symptoms, and negative symptoms in schizophrenics treated with neuroleptics. J Nerv Ment Dis. 1987;175:100–105. doi: 10.1097/00005053-198702000-00006. [DOI] [PubMed] [Google Scholar]
- Rifkin A. Akinesia: a poorly recognized drug-induced extrapyramidal behavioral disorder. Arch Gen Psychiatry. 1975;32:672–674. [Google Scholar]
- Saeedi H, Remington G, Christensen BK. Impact of haloperidol, a dopamine D2 antagonist, on cognition and mood. Schizophr Res. 2006;85:222–231. doi: 10.1016/j.schres.2006.03.033. [DOI] [PubMed] [Google Scholar]
- Salamone JD, Correa M. The mysterious motivational functions of mesolimbic dopamine. Neuron. 2012;76:470–485. doi: 10.1016/j.neuron.2012.10.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Samaha AN, Seeman P, Stewart J, Rajabi H, Kapur S. ‘Breakthrough' dopamine supersensitivity during ongoing antipsychotic treatment leads to treatment failure over time. J Neurosci. 2007;27:2979–2986. doi: 10.1523/JNEUROSCI.5416-06.2007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saperstein AM, Fiszdon JM, Bell MD. Intrinsic motivation as a predictor of work outcome after vocational rehabilitation in schizophrenia. J Nerv Ment Dis. 2011;199:672–677. doi: 10.1097/NMD.0b013e318229d0eb. [DOI] [PubMed] [Google Scholar]
- Sayers SL, Curran PJ, Mueser KT. Factor structure and construct validity of the Scale for the Assessment of Negative Symptoms. Psychol Assess. 1996;8:269. [Google Scholar]
- Schooler NR. Deficit symptoms in schizophrenia: negative symptoms versus neuroleptic-induced deficits. Acta Psychiatr Scand Suppl. 1994;380:21–26. doi: 10.1111/j.1600-0447.1994.tb05827.x. [DOI] [PubMed] [Google Scholar]
- Simpson GM, Angus JW. A rating scale for extrapyramidal side effects. Acta Psychiatr Scand. 1970;212:11–19. doi: 10.1111/j.1600-0447.1970.tb02066.x. [DOI] [PubMed] [Google Scholar]
- Stroup TS, McEvoy JP, Swartz MS, Byerly MJ, Glick ID, Canive JM, et al. The National Institute of Mental Health Clinical Antipsychotic Trials of Intervention Effectiveness (CATIE) project: schizophrenia trial design and protocol development. Schizophr Bull. 2003;29:15–31. doi: 10.1093/oxfordjournals.schbul.a006986. [DOI] [PubMed] [Google Scholar]
- Tollefson GD, Sanger TM. Negative symptoms: a path analytic approach to a double-blind, placebo- and haloperidol-controlled clinical trial with olanzapine. Am J Psychiatry. 1997;154:466–474. doi: 10.1176/ajp.154.4.466. [DOI] [PubMed] [Google Scholar]
- Tracy K, Adler LA, Rotrosen J, Edson R, Lavori P. Interrater reliability issues in multicenter trials, Part I: Theoretical concepts and operational procedures used in Department of Veterans Affairs Cooperative Study #394. Psychopharmacol Bull. 1997;33:53–57. [PubMed] [Google Scholar]
- Trifilieff P, Feng B, Urizar E, Winiger V, Ward RD, Taylor KM, et al. Increasing dopamine D2 receptor expression in the adult nucleus accumbens enhances motivation. Mol Psychiatry. 2013;18:1025–1033. doi: 10.1038/mp.2013.57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tugg LA, Desai D, Prendergast P, Remington G, Reed K, Zipursky RB. Relationship between negative symptoms in chronic schizophrenia and neuroleptic dose, plasma levels and side effects. Schizophr Res. 1997;25:71–78. doi: 10.1016/s0920-9964(97)00009-1. [DOI] [PubMed] [Google Scholar]
- Vogel SJ, Strauss GP, Allen DN. Using negative feedback to guide behavior: impairments on the first 4 cards of the Wisconsin Card Sorting Test predict negative symptoms of schizophrenia. Schizophr Res. 2013;151:97–101. doi: 10.1016/j.schres.2013.07.052. [DOI] [PubMed] [Google Scholar]
- Vohs JL, Lysaker PH, Nabors L. Associations of personality with intrinsic motivation in schizophrenia. Psychiatry Res. 2013;208:78–80. doi: 10.1016/j.psychres.2013.03.008. [DOI] [PubMed] [Google Scholar]
- Waltz JA, Frank MJ, Wiecki TV, Gold JM. Altered probabilistic learning and response biases in schizophrenia: behavioral evidence and neurocomputational modeling. Neuropsychology. 2011;25:86–97. doi: 10.1037/a0020882. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weickert TW, Goldberg TE, Marenco S, Bigelow LB, Egan MF, Weinberger DR. Comparison of cognitive performances during a placebo period and an atypical antipsychotic treatment period in schizophrenia: critical examination of confounds. Neuropsychopharmacology. 2003;28:1491–1500. doi: 10.1038/sj.npp.1300216. [DOI] [PubMed] [Google Scholar]
- Wolf DH, Satterthwaite TD, Kantrowitz JJ, Katchmar N, Vandekar L, Elliott MA, et al. Amotivation in schizophrenia: integrated assessment with behavioral, clinical, and imaging measures. Schizophr Bull. 2014;40:1328–1337. doi: 10.1093/schbul/sbu026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yamada AM, Lee KK, Dinh TQ, Barrio C, Brekke JS. Intrinsic motivation as a mediator of relationships between symptoms and functioning among individuals with schizophrenia spectrum disorders in a diverse urban community. J Nerv Ment Dis. 2010;198:28–34. doi: 10.1097/NMD.0b013e3181c8aa71. [DOI] [PMC free article] [PubMed] [Google Scholar]