Abstract
Purpose
The association between excess calcium intake and cardiovascular mortality has already been reported. In the present study, we investigated the relation between dietary calcium intake and Framingham Risk Score (FRS) according to serum 25-hydroxyvitamin D [25(OH)D] status.
Materials and Methods
A total of 7809 subjects (3452 males and 4357 female) aged over 40 years were selected for this cross-sectional study from data obtained from the Korea National Health and Nutrition Examination Survey (2008-2011). Daily dietary calcium intake was categorized into <300, 300-600, 600-900, 900-1200, and >1200 mg/day and serum 25(OH)D concentration classified into <50, 50-75, >75 mmol/L. The FRS was compared by the daily dietary calcium intake categories according to 25(OH)D concentration after adjustment with relevant variables in both genders.
Results
Higher FRS was observed in males with both <300 mg and >1200 mg of dietary calcium intake and females with <300 mg of dietary calcium intake without adjustment. The significantly higher FRS remained in the <300 mg and >1200 mg of dietary calcium intake groups in both genders after adjustments for relevant variables. FRS was significantly higher in the group with >1200 mg of dietary calcium intake and serum 25(OH)D <50 nmol/L, which was the male only vitamin D deficient group.
Conclusion
Very low (<300 mg/day) and excess (>1200 mg/day) dietary calcium intake were related with higher FRS in both genders. In particular, higher FRS was observed in the excess (>1200 mg/day) dietary calcium intake male group under vitamin D deficiency (<50 nmol/L).
Keywords: 25-hydroxyvitamin D, calcium, coronary disease
INTRODUCTION
A large number of studies have shown a potential relationship between serum calcium concentration and cardiovascular disease.1,2,3,4,5,6,7 In 1996, Reunanen, et al.8 found an increased risk of premature death in men (<50 years) with increasing serum calcium concentration. Calcium supply is usually assessed through evaluation of dietary calcium or supplementary intake. Dietary calcium intake has been emphasized because of its proposed benefit for bone health and calcium supplementation has become widely used. A recent study9 reported that more than 50% of older men and almost 70% of older women in the United States were taking supplemental calcium. However, its non-skeletal effects, including effects on cardiovascular health, are not established and remain largely unknown and controversial.10,11
A Swedish population-based investigation of men with relatively high intakes of dietary calcium showed a reduction in all-cause mortality when taking more than the recommended daily amount.12 Previous observational and interventional studies suggested a calcium benefit against cardiovascular diseases.13,14,15 However, the most recent study from the National Institute of Health-AARP Diet and Health Study showed that high intake of supplemental calcium is related to an increased risk of cardiovascular disease in men but not in women.8 In addition, there is no previous report that accounts for dietary calcium intake according to serum 25-hydroxyvitamin D [25(OH)D] concentration on cardiovascular diseases and various health condition.
Framingham Risk Score (FRS) is generally considered as a tool to assess future cardiovascular risk.16 Dietary calcium intake and serum 25(OH)D concentration in Korean are low compared to other western countries such as the United States17,18 and it is highly possible that FRS can be differently associated with the dietary calcium intake according to the serum 25(OH)D concentration. Therefore, the aim of this study was to evaluate the relation of daily calcium intake with FRS according to serum 25(OH)D concentration in Korean males and females, aged over 40 years of age, using the Korea National Health and Nutrition Examination Survey (KNHANES, 2008-2011), which showed a relatively low dietary calcium intake and serum 25(OH)D concentration condition compared to the United States.
MATERIALS AND METHODS
Subjects
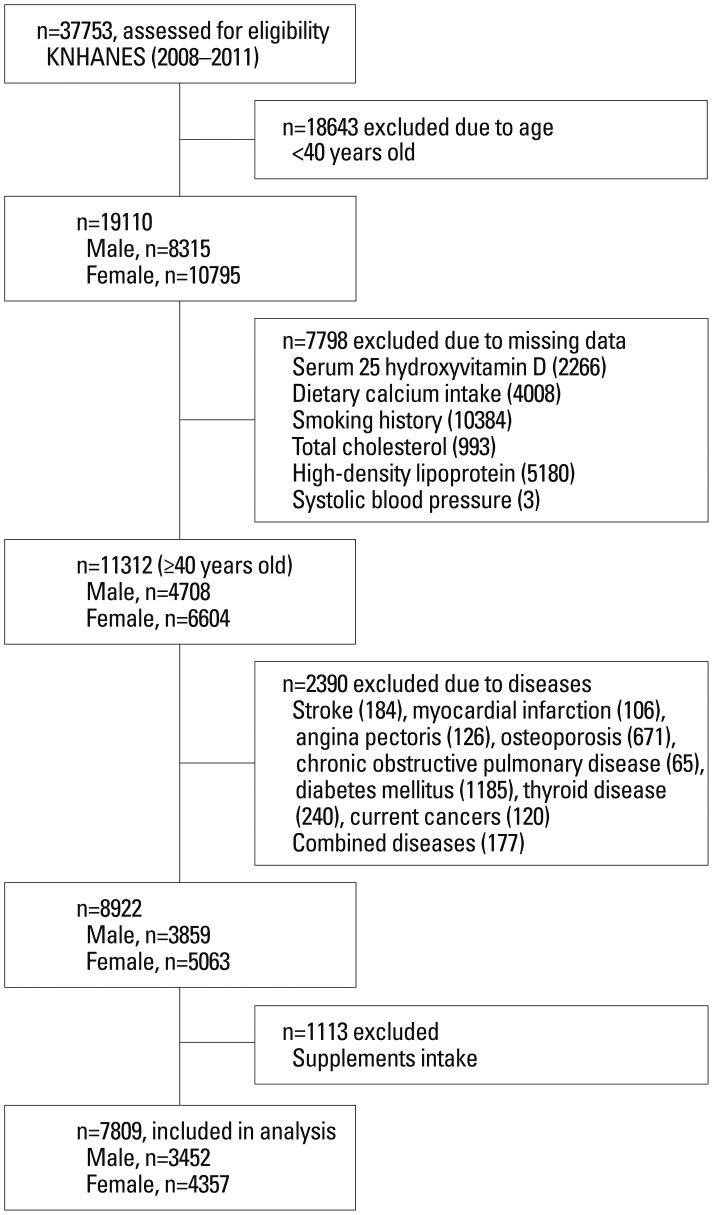
Conducted periodically by the Korea Centers for Disease Control and Prevention since 1998, KNHANES provides comprehensive information on health status, health behavior, nutritional status, and socio-demographics in national districts in Korea. Data from the fourth (IV-2 and IV-3, 2008, 2009) and fifth (V-1 and V-2, 2010, 2011) KNHANES data, containing dietary calcium intake and calculated FRSs were used in this cross-sectional analysis. From an initial total of 37753 males and females, 19110 subjects (8315 males and 10795 females) were evaluated. Of 19110 subjects evaluated, 7798 subjects were excluded for missing data and 2390 subjects were excluded for chronic diseases. An additional 1113 subjects were excluded for any vitamin and mineral supplement use, in particular calcium supplementation. A total of 7809 participants (3452 men and 4357 women) were used in this analysis as shown in Fig. 1. All participants provided written informed consent before the survey.
Fig. 1. Flow diagram of subject inclusion and exclusion in the Korea National Health and Nutrition Examination Surveys. This figure shows the selection of study subjects in the KNHANES 2008-2011. KNHANES, Korea National Health and Nutrition Examination Survey.
Biochemistry, dietary and supplement assessment
Blood samples were collected year-round following an 8-hour fasting period. They were immediately processed, refrigerated, and transported in cold storage to the central testing institute (NeoDin Medical Institute, Seoul, Korea) where they were then analyzed within 24 hours. Serum 25(OH)D concentration was measured with a radioimmunoassay kit (DiaSorin Inc., Stillwater, MN, USA) using a r-counter (1470 Wizard; PerkinElmer, Turku, Finland). The inter-assay coefficients of variation (CV) were 2.8-6.2% for 2008-2009 samples and 1.9-6.1% for 2010-2011 samples. To minimize analytical variation, serum 25(OH)D was measured in the same institute every other week throughout the analysis period.
Nutrient intakes, including total calorie and calcium intakes, were assessed with a 24-hour dietary recall questionnaire administered by a trained dietician. The results were calculated using the Food Composition Table developed by the National Rural Resources Development Institute (7th revision).19 Physical examinations were performed by a trained examiner following a standardized procedure. Body weight and height were measured to the nearest 0.1 kg and 0.1 cm, respectively, in light indoor clothing without shoes. Age of menarche was determined using a health questionnaire administered by a trained examiner.
Lifestyle questionnaires
Physical activity was assessed by a questionnaire and categorized as "yes" or "no"; "yes" meaning >30 minutes of moderate physical activity three or more times in the last week in which the subject was tired compared to ordinary levels. Current smokers were defined as those who were currently smoking and had smoked more than five packs of cigarettes during their life-time. Ex-smokers were persons who had smoked in the past but had quit and nonsmokers had no history of smoking. Regular alcohol drinkers were those who drank alcohol more than once a month and nondrinkers were all others. Occupations were classified into two groups; indoor and outdoor workers. Indoor workers included managers, professionals and related workers, clerical office workers, service workers, and sales workers. Unemployed subjects were classified as indoor workers considering their limited outdoor activities. Outdoor workers included skilled agricultural, forestry, and fishery workers.
Statistical analysis
A complex sample analysis was used for weighting all KNHANES data values following the guidance of statistics from the Korea Centers for Disease Control and Prevention. Initially, we calculated the FRSs by gender. The males and females were stratified into five groups by calcium intake; <300, 300-600, 600-900, 900-1200, >1200 mg/day. Serum 25(OH)D concentration was further used to classify subjects in each gender group into three categories; <50, 50-75, and >75 nmol/L. Framingham risk equations20 were used to predict the risk of developing total coronary disease events (angina, myocardial infarction, or coronary heart disease death) over the next 10 years. General characteristics such as age, body mass index (BMI), total calorie intake, serum 25(OH)D concentration, systolic blood pressure, diastolic blood pressure, serum glucose concentration and serum lipid profiles (total cholesterol, high density lipoprotein, and triglyceride) were presented by dietary calcium intake groups using ANOVA test in males and females after data weighting. FRS was compared by ANCOVA test after adjustments for age, BMI, jobs, education, smoking status, alcohol intake, moderate physical activity, serum 25(OH)D and total calorie intake in men. Menopause, oral contraceptives, and hormone replacement therapy were also adjusted for with women. Finally, we compared FRS according to daily dietary calcium intake and serum 25(OH)D category by ANCOVA test after adjustments for age, BMI, jobs, education, smoking status, alcohol intake, moderate physical activity, serum 25(OH)D and total calories intake and season in men. For wemen, menopause, oral contraceptives and hormone replacement therapy were also adjusted. All p-values were P for trend to assess the significance of all analysis and p<0.05 was considered significant. Data were analyzed using SPSS 19.0 (SPSS Inc., Chicago, IL, USA).
RESULTS
Mean dietary calcium intake in adult males and females was 552.4 mg/day and 440.8 mg/day, respectively. Mean FRS in males and females was 11.3 points and 11.4 points. General characteristics of males and females by calcium intake are presented in Table 1. Mean age, BMI, energy intake, and FRS showed significant difference by calcium intake groups in both genders. In addition, FRS was higher in both low (<300 mg/day) and excess (>1200 mg/day) dietary calcium intake groups than other groups in both genders, showing a J-shaped pattern.
Table 1. General Characteristics of Study Subjects by Dietary Calcium Intake Groups.
| Variables | Dietary calcium intake (mg/day) | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Male (n=3452) | Female (n=4357) | |||||||||||
| <300 | 300-600 | 600-900 | 900-1200 | >1200 | p value | <300 | 300-600 | 600-900 | 900-1200 | >1200 | p value | |
| Subjects (n) | 714 | 1574 | 751 | 255 | 158 | 1618 | 1807 | 617 | 205 | 110 | ||
| Age (yrs) | 57.4 (0.6) | 52.7 (0.3) | 51.8 (0.3) | 51.8 (0.7) | 52.7 (0.9) | <0.001 | 57.3 (0.4) | 53.1 (0.3) | 51.8 (0.4) | 52.2 (0.7) | 53.5 (1.1) | <0.001 |
| BMI (kg/m2) | 23.5 (0.2) | 24.1 (0.1) | 24.2 (0.1) | 24.2 (0.2) | 24.8 (0.3) | 0.001 | 24.0 (0.1) | 24.0 (0.1) | 23.5 (0.1) | 23.8 (0.2) | 23.3 (0.4) | 0.051 |
| Energy (kcal/day) | 1644.7 (26.6) | 2173.2 (22.3) | 2597.0 (33.9) | 2815.1 (62.7) | 3127.1 (90.5) | <0.001 | 1278.9 (12.8) | 1676.7 (15.5) | 1954.5 (32.9) | 2144.0 (57.0) | 2369.6 (79.8) | <0.001 |
| 25(OH)D (nmol/L) | 50.7 (1.0) | 52.0 (0.7) | 51.2 (0.8) | 52.3 (1.2) | 52.6 (2.0) | 0.660 | 42.6 (0.6) | 43.4 (0.6) | 43.4 (0.8) | 43.1 (1.4) | 49.0 (2.1) | 0.070 |
| HTN (n) (%) | 188 (22.5) | 375 (45.1) | 174 (20.8) | 54 (6.5) | 43 (5.1) | 0.385 | 475 (44.6) | 426 (40.1) | 108 (10.2) | 38 (3.5) | 17 (1.6) | <0.001 |
| SBP (mm Hg) | 123.0 (0.9) | 121.6 (0.6) | 119.7 (0.6) | 120.3 (1.3) | 121.7 (1.3) | 0.026 | 122.1 (0.6) | 118.9 (0.5) | 115.2 (0.8) | 118.8 (1.3) | 118.4 (2.0) | <0.001 |
| DBP (mm Hg) | 78.4 (0.6) | 79.6 (0.4) | 79.1 (0.5) | 78.4 (0.8) | 79.3 (0.8) | 0.296 | 76.0 (0.3) | 75.6 (0.3) | 74.0 (0.5) | 76.0 (0.8) | 75.1 (1.2) | 0.009 |
| Glucose (mmol/L) | 5.49 (0.06) | 5.49 (0.03) | 5.49 (0.05) | 5.49 (0.06) | 5.87 (0.27) | 0.734 | 5.35 (0.03) | 5.28 (0.02) | 5.20 (0.04) | 5.17 (0.05) | 5.23 (0.07) | 0.002 |
| Insulin (uIU/mL) | 9.8 (0.3) | 9.5 (0.2) | 9.8 (0.3) | 9.7 (0.4) | 10.2 (0.6) | 0.725 | 10.2 (0.2) | 10.1 (0.1) | 10.0 (0.5) | 9.8 (0.3) | 9.0 (0.5) | 0.301 |
| TC (mmol/L) | 4.91 (0.04) | 5.01 (0.03) | 4.96 (0.04) | 5.07 (0.08) | 5.13 (0.14) | 0.164 | 5.06 (0.03) | 5.05 (0.02) | 5.01 (0.05) | 5.01 (0.07) | 5.23 (0.10) | 0.346 |
| HDL (mmol/L) | 1.25 (0.01) | 1.29 (0.01) | 1.27 (0.01) | 1.28 (0.03) | 1.23 (0.03) | 0.083 | 1.38 (0.01) | 1.40 (0.01) | 1.43 (0.02) | 1.41 (0.02) | 1.49 (0.03) | 0.002 |
| TG (mmol/L) | 1.86 (0.06) | 1.88 (0.05) | 1.89 (0.08) | 1.84 (0.10) | 2.43 (0.33) | 0.567 | 1.45 (0.03) | 1.38 (0.03) | 1.18 (0.03) | 1.35 (0.06) | 1.24 (0.09) | <0.001 |
| FRS (points)/10-yr risk (%) | 11.5 (0.2)/10 | 10.5 (0.1)/8 | 10.2 (0.2)/6 | 9.9 (0.3)/6 | 11.1 (0.3)/8 | <0.001 | 12.0 (0.2)/1 | 10.0 (0.2)/1 | 9.1 (0.2)/1 | 9.6 (0.4)/1 | 10.0 (0.6)/1 | <0.001 |
BMI, body mass index; HTN, hypertension; SBP, systolic blood pressure; DBP, diastolic blood pressure; TC, total cholesterol; HDL, high density lipoprotein; TG, triglyceride; FRS, Framingham Risk Score; Energy, total calorie intake; Calcium, daily intake; serum 25(OH)D, serum 25-hydroxyvitamin D concentration.
Data represent mean (standard error).
p values represent P for trends by ANOVA test without adjustment.
After adjustments for relevant variables [for both genders: age, BMI, jobs, education, smoking status, alcohol intake, moderate physical activity, serum 25(OH)D, total calorie intake; for women only: menopause, oral contraceptives and hormone replacement therapy], FRS values were significantly different in the five dietary calcium intake groups in both genders. A J-shaped pattern was also observed (Table 2).
Table 2. Difference of Framingham Risk Score by Calcium Intake Groups.
| Calcium intake (mg/day) | ||||||
|---|---|---|---|---|---|---|
| <300 | 300-600 | 600-900 | 900-1200 | >1200 | P for trend | |
| Male | 11.1 (0.2)/714 | 10.5 (0.1)/1574 | 10.4 (0.2)/751 | 10.2 (0.3)/255 | 11.1 (0.3)/158 | <0.001 |
| Female | 10.3 (0.1)/1618 | 9.4 (0.1)/1807 | 9.2 (0.2)/617 | 9.4 (0.3)/204 | 10.7 (0.5)/110 | <0.001 |
BMI, body mass index; 25(OH)D, 25-hydroxyvitamin D.
All values represent Framingham Risk Score (SE)/subject numbers. P for trend was obtained by ANCOVA test after adjustments for age, BMI, jobs, education, smoking status, alcohol intake, moderate physical activity, serum 25(OH)D and total calories intakes for both genders. Menopause, oral contraceptives and hormone replacement therapy were also adjusted for with women.
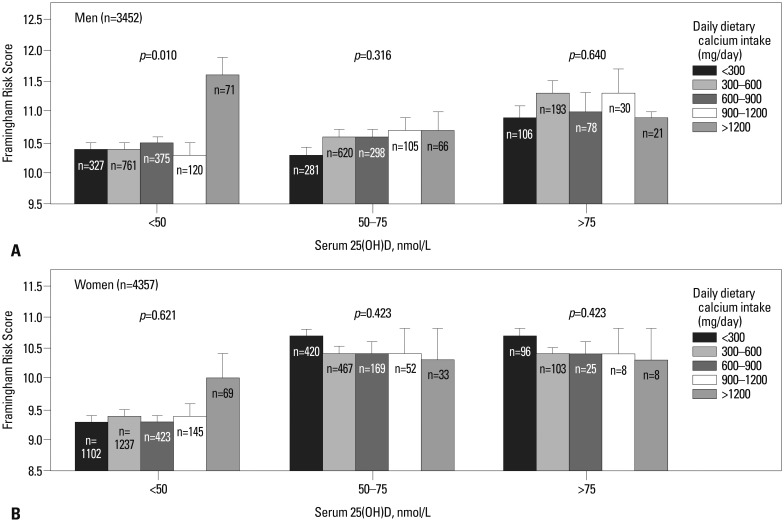
To evaluate the difference in FRS within the dietary calcium intake groups according to serum 25(OH)D concentrations, we compared FRS after adjustment of season in addition to the relevant variables listed above. FRS was significan-tly higher in the group with >1200 mg/day of dietary calcium intake as well as in the male serum 25(OH)D <50 nmol/L (p=0.010) group. A similar pattern was observed in females, however, there was no statistical significance (Fig. 2).
Fig. 2. Framingham Risk Score according to the dietary calcium intake and serum 25(OH)D. p-values were obtained by ANCOVA test after adjustments for age, BMI, jobs, education, smoking status, alcohol intake, moderate physical activity, serum 25(OH)D, total calories intakes and season for both genders (A: men, B: women). Menopause, oral contraceptives and hormone replacement therapy were also adjusted for with women. BMI, body mass index; 25(OH)D, 25-hydroxyvitamin D.
DISCUSSION
This cross-sectional study showed that both low (<300 mg) or excess (>1200 mg) daily calcium intake was associated with higher FRS. In particular, FRS can be elevated in a vitamin D deficient Korean adult male with excess (>1200 mg) dietary calcium intake.
In the Framingham Study,21 calcium intake was not associated with increased coronary artery calcification and the authors suggested that their result did not support the hypothesis that high calcium intake could increase coronary artery calcification, which is an important measure of the progression of atherosclerosis. Van der Vijver, et al.22 showed that dietary calcium was not related to CVD deaths in Dutch civil servants and other studies23,24 also found no association of calcium intake and CVD death. On the other hand, however, high intake of calcium was found to relate to all-cause and cardiovascular mortality,25 and Xiao, et al.7 showed that high intake of supplemental calcium is associated with the risk of CVD death in men but not in women.
Non-skeletal effects of calcium remain uncertain and especially cardiovascular effects are controversial. Dietary calcium regulates blood pressure and modulates peripheral vascular resistance via calcitrophic hormones26 and intracellular calcium can not only accelerate vascular calcification but also increase mortality in patients with renal failure.27 Slinin, et al.28 showed that high plasma calcium was associated with cardiovascular events after adjusting for plasma 25(OH)D, parathyroid hormone and phosphorus. The possible mechanisms, however, are not clear.
Serum 25(OH)D is associated with calcium metabolism and cardiovascular diseases as well as bone metabolism via osteocalcin in the osteoblast and bone-forming cell. Several hypotheses which could explain association between cardiovascular diseases and 25(OH)D have been proposed. One hypothesis is that vitamin D receptors affect the expression of matrix metalloproteinase and tissue inhibitors of metalloproteinases.29 Vitamin D also suppresses foam cell formation by reducing acetylated or oxidized LDL.30 Low serum 25(OH)D levels are associated with cardiovascular diseases and all-cause mortality.31,32 Thus, we assessed the relation of calcium intake and FRS according to serum 25(OH)D concentration.
FRS has been a tool to assess future CVD risk. However, we did not assess 10 year-risk by percentage because 1 point of FRS in the high risk group is more weighted than in the low risk group. In addition, dietary calcium intake and serum 25(OH)D concentration may be influenced or different by some components of FRS (by gender, age, smoking, and blood pressure). Therefore, evaluation of the difference of FRS according to the calcium intake and serum 25(OH)D is reasonable.
In our study, excess dietary calcium intake (>1200 mg/day) was associated with higher FRS. Specifically, in the adult male serum 25(OH)D deficiency group, significant difference in FRS was observed even after adjustment for season. We are not certain why this J-shaped pattern for the FRS is associated with dietary calcium intake. In the present study, however, we found that moderate dietary calcium intake was associated with relatively low FRS after relevant variables were adjusted for, including total calories intake, and that, men who had high dietary calcium intake with vitamin D deficient status had high FRS. Therefore, it is highly likely that high dietary calcium intake under low vitamin D status can be associated with harmful effects on the cardiovascular system. This can partially explain why excconcentration was measured witess dietary calcium intake can influence the calcium homeostasis with respect to cardiovascular health.
Dietary calcium is essential for bones,33 however, if serum vitamin D concentration is too low, absorbed dietary calcium can adversely affect cardiovascular risk. Vitamin D plays a role in absorbing dietary or supplemental calcium and maintaining optimal bone health.34 In cases of vitamin D deficiency, calcium cannot be absorbed well and the absorbed calcium does not accumulate in bone. Vitamin D also plays a role in producing osteocalcin in the osteoblast,35 the bone-forming cell, and reduced osteocalcin results in failed calcium deposition in bone. Consequently, calcium remains in the blood and can move around blood vessels to adversely affect the cardiovascular system. Meanwhile, the test group with sufficient vitamin D levels did not show a favorable result on FRS in our study. In addition, there was no statistical significance in FRS for adult females. This result may be due to the fact that dietary calcium intake (552.4 mg/day vs. 440.8 mg/day) and serum 25(OH)D concentration (53.1 nmol/L vs. 44.2 nmol/L) were higher in men than those in women.
There are some unavoidable limitations in our study. First, this is a cross-sectional design, not a prospective one. Second, FRS is a simple tool to assess future cardiovascular risk, therefore, it has limitations when correlating cross-sectional results with future FRS. Third, it is different to explain why excess dietary calcium intake shows significance only in adult males, but not in adult females. Fourth, KNHANES does not contain individual medication history including thiazide diuretics or the presence of hyperparathyroidism to influence serum calcium homeostasis. However, our investigation differs from previous study, because of using FRSs to assess cardiovascular disease risk according to dietary calcium intake and serum 25(OH)D concentration. To our best knowledge, this is the first study to assess the cardiovascular risk using dietary calcium intake combined with serum 25(OH)D concentration.
In conclusion, this study suggests that excess (>1200 mg/day) as well as very low (<300 mg/day) dietary calcium intake are related to higher FRS in both genders. In particular, higher FRS was observed in the vitamin D deficient (<50 nmol/L) Korean adult male group with excess (>1200 mg/of day) dietary calcium intake. Further study is needed to evaluate the mechanism involved and effects of dietary calcium intake on cardiovascular risk with various vitamin D levels.
Footnotes
The authors have no financial conflicts of interest.
References
- 1.Grandi NC, Brenner H, Hahmann H, Wüsten B, März W, Rothenbacher D, et al. Calcium, phosphate and the risk of cardiovascular events and all-cause mortality in a population with stable coronary heart disease. Heart. 2012;98:926–933. doi: 10.1136/heartjnl-2011-300806. [DOI] [PubMed] [Google Scholar]
- 2.Leifsson BG, Ahrén B. Serum calcium and survival in a large health screening program. J Clin Endocrinol Metab. 1996;81:2149–2153. doi: 10.1210/jcem.81.6.8964843. [DOI] [PubMed] [Google Scholar]
- 3.Lundgren E, Lind L, Palmér M, Jakobsson S, Ljunghall S, Rastad J. Increased cardiovascular mortality and normalized serum calcium in patients with mild hypercalcemia followed up for 25 years. Surgery. 2001;130:978–985. doi: 10.1067/msy.2001.118377. [DOI] [PubMed] [Google Scholar]
- 4.Marco MP, Craver L, Betriu A, Belart M, Fibla J, Fernández E. Higher impact of mineral metabolism on cardiovascular mortality in a European hemodialysis population. Kidney Int Suppl. 2003:S111–S114. doi: 10.1046/j.1523-1755.63.s85.26.x. [DOI] [PubMed] [Google Scholar]
- 5.Ogard CG, Petersen J, Jørgensen T, Almdal T, Vestergaard H. Serum ionised calcium and cardiovascular disease in 45-years old men and women followed for 18 years. Eur J Epidemiol. 2006;21:123–127. doi: 10.1007/s10654-005-5438-1. [DOI] [PubMed] [Google Scholar]
- 6.Palmer SC, Hayen A, Macaskill P, Pellegrini F, Craig JC, Elder GJ, et al. Serum levels of phosphorus, parathyroid hormone, and calcium and risks of death and cardiovascular disease in individuals with chronic kidney disease: a systematic review and meta-analysis. JAMA. 2011;305:1119–1127. doi: 10.1001/jama.2011.308. [DOI] [PubMed] [Google Scholar]
- 7.Xiao Q, Murphy RA, Houston DK, Harris TB, Chow WH, Park Y. Dietary and supplemental calcium intake and cardiovascular disease mortality: the National Institutes of Health-AARP diet and health study. JAMA Intern Med. 2013;173:639–646. doi: 10.1001/jamainternmed.2013.3283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Reunanen A, Knekt P, Marniemi J, Mäki J, Maatela J, Aromaa A. Serum calcium, magnesium, copper and zinc and risk of cardiovascular death. Eur J Clin Nutr. 1996;50:431–437. [PubMed] [Google Scholar]
- 9.Bailey RL, Dodd KW, Goldman JA, Gahche JJ, Dwyer JT, Moshfegh AJ, et al. Estimation of total usual calcium and vitamin D intakes in the United States. J Nutr. 2010;140:817–822. doi: 10.3945/jn.109.118539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hennekens CH, Barice EJ. Calcium supplements and risk of myocardial infarction: a hypothesis formulated but not yet adequately tested. Am J Med. 2011;124:1097–1098. doi: 10.1016/j.amjmed.2011.05.001. [DOI] [PubMed] [Google Scholar]
- 11.Reid IR, Bolland MJ, Grey A. Calcium supplements and risk of myocardial infarction: an hypothesis twice tested. Am J Med. 2012;125:e15. doi: 10.1016/j.amjmed.2011.09.006. [DOI] [PubMed] [Google Scholar]
- 12.Kaluza J, Orsini N, Levitan EB, Brzozowska A, Roszkowski W, Wolk A. Dietary calcium and magnesium intake and mortality: a prospective study of men. Am J Epidemiol. 2010;171:801–807. doi: 10.1093/aje/kwp467. [DOI] [PubMed] [Google Scholar]
- 13.Bucher HC, Cook RJ, Guyatt GH, Lang JD, Cook DJ, Hatala R, et al. Effects of dietary calcium supplementation on blood pressure. A meta-analysis of randomized controlled trials. JAMA. 1996;275:1016–1022. doi: 10.1001/jama.1996.03530370054031. [DOI] [PubMed] [Google Scholar]
- 14.Cappuccio FP, Elliott P, Allender PS, Pryer J, Follman DA, Cutler JA. Epidemiologic association between dietary calcium intake and blood pressure: a meta-analysis of published data. Am J Epidemiol. 1995;142:935–945. doi: 10.1093/oxfordjournals.aje.a117741. [DOI] [PubMed] [Google Scholar]
- 15.Reid IR, Mason B, Horne A, Ames R, Clearwater J, Bava U, et al. Effects of calcium supplementation on serum lipid concentrations in normal older women: a randomized controlled trial. Am J Med. 2002;112:343–347. doi: 10.1016/s0002-9343(01)01138-x. [DOI] [PubMed] [Google Scholar]
- 16.Zhu B, Haruyama Y, Muto T, Yamasaki A, Tarumi F. Evaluation of a community intervention program in Japan using Framingham risk score and estimated 10-year coronary heart disease risk as outcome variables: a non-randomized controlled trial. BMC Public Health. 2013;13:219. doi: 10.1186/1471-2458-13-219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Joo NS, Dawson-Hughes B, Kim YS, Oh K, Yeum KJ. Impact of calcium and vitamin D insufficiencies on serum parathyroid hormone and bone mineral density: analysis of the fourth and fifth Korea National Health and Nutrition Examination Survey (KNHANES IV-3, 2009 and KNHANES V-1, 2010) J Bone Miner Res. 2013;28:764–770. doi: 10.1002/jbmr.1790. [DOI] [PubMed] [Google Scholar]
- 18.Joo NS, Dawson-Hughes B, Yeum KJ. 25-Hydroxyvitamin D, calcium intake, and bone mineral content in adolescents and young adults: analysis of the fourth and fifth Korea National Health and Nutrition Examination Survey (KNHANES IV-2, 3, 2008-2009 and V-1, 2010) J Clin Endocrinol Metab. 2013;98:3627–3636. doi: 10.1210/jc.2013-1480. [DOI] [PubMed] [Google Scholar]
- 19.Food composition table. 7th ed. Suwon, Korea: National Rural Resource Development Institute; 2006. [Google Scholar]
- 20.Wilson PW, D'Agostino RB, Levy D, Belanger AM, Silbershatz H, Kannel WB. Prediction of coronary heart disease using risk factor categories. Circulation. 1998;97:1837–1847. doi: 10.1161/01.cir.97.18.1837. [DOI] [PubMed] [Google Scholar]
- 21.Samelson EJ, Booth SL, Fox CS, Tucker KL, Wang TJ, Hoffmann U, et al. Calcium intake is not associated with increased coronary artery calcification: the Framingham Study. Am J Clin Nutr. 2012;96:1274–1280. doi: 10.3945/ajcn.112.044230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Van der Vijver LP, van der Waal MA, Weterings KG, Dekker JM, Schouten EG, Kok FJ. Calcium intake and 28-year cardiovascular and coronary heart disease mortality in Dutch civil servants. Int J Epidemiol. 1992;21:36–39. doi: 10.1093/ije/21.1.36. [DOI] [PubMed] [Google Scholar]
- 23.Ascherio A, Rimm EB, Hernán MA, Giovannucci EL, Kawachi I, Stampfer MJ, et al. Intake of potassium, magnesium, calcium, and fiber and risk of stroke among US men. Circulation. 1998;98:1198–1204. doi: 10.1161/01.cir.98.12.1198. [DOI] [PubMed] [Google Scholar]
- 24.Umesawa M, Iso H, Date C, Yamamoto A, Toyoshima H, Watanabe Y, et al. Dietary intake of calcium in relation to mortality from cardiovascular disease: the JACC Study. Stroke. 2006;37:20–26. doi: 10.1161/01.STR.0000195155.21143.38. [DOI] [PubMed] [Google Scholar]
- 25.Michaëlsson K, Melhus H, Warensjö Lemming E, Wolk A, Byberg L. Long term calcium intake and rates of all cause and cardiovascular mortality: community based prospective longitudinal cohort study. BMJ. 2013;346:f228. doi: 10.1136/bmj.f228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Zemel MB. Regulation of adiposity and obesity risk by dietary calcium: mechanisms and implications. J Am Coll Nutr. 2002;21:146S–151S. doi: 10.1080/07315724.2002.10719212. [DOI] [PubMed] [Google Scholar]
- 27.Goodman WG, Goldin J, Kuizon BD, Yoon C, Gales B, Sider D, et al. Coronary-artery calcification in young adults with end-stage renal disease who are undergoing dialysis. N Engl J Med. 2000;342:1478–1483. doi: 10.1056/NEJM200005183422003. [DOI] [PubMed] [Google Scholar]
- 28.Slinin Y, Blackwell T, Ishani A, Cummings SR, Ensrud KE. Serum calcium, phosphorus and cardiovascular events in post-menopausal women. Int J Cardiol. 2011;149:335–340. doi: 10.1016/j.ijcard.2010.02.013. [DOI] [PubMed] [Google Scholar]
- 29.Weber KT, Weglicki WB, Simpson RU. Macro- and micronutrient dyshomeostasis in the adverse structural remodelling of myocardium. Cardiovasc Res. 2009;81:500–508. doi: 10.1093/cvr/cvn261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Wang J, Luben R, Khaw KT, Bingham S, Wareham NJ, Forouhi NG. Dietary energy density predicts the risk of incident type 2 diabetes: the European Prospective Investigation of Cancer (EPIC)-Norfolk Study. Diabetes Care. 2008;31:2120–2125. doi: 10.2337/dc08-1085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Melamed ML, Michos ED, Post W, Astor B. 25-hydroxyvitamin D levels and the risk of mortality in the general population. Arch Intern Med. 2008;168:1629–1637. doi: 10.1001/archinte.168.15.1629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Dobnig H, Pilz S, Scharnagl H, Renner W, Seelhorst U, Wellnitz B, et al. Independent association of low serum 25-hydroxyvitamin d and 1,25-dihydroxyvitamin d levels with all-cause and cardiovascular mortality. Arch Intern Med. 2008;168:1340–1349. doi: 10.1001/archinte.168.12.1340. [DOI] [PubMed] [Google Scholar]
- 33.Lambert HL, Eastell R, Karnik K, Russell JM, Barker ME. Calcium supplementation and bone mineral accretion in adolescent girls: an 18-mo randomized controlled trial with 2-y follow-up. Am J Clin Nutr. 2008;87:455–462. doi: 10.1093/ajcn/87.2.455. [DOI] [PubMed] [Google Scholar]
- 34.Heaney RP, Dowell MS, Hale CA, Bendich A. Calcium absorption varies within the reference range for serum 25-hydroxyvitamin D. J Am Coll Nutr. 2003;22:142–146. doi: 10.1080/07315724.2003.10719287. [DOI] [PubMed] [Google Scholar]
- 35.Patti A, Gennari L, Merlotti D, Dotta F, Nuti R. Endocrine actions of osteocalcin. Int J Endocrinol. 2013;2013:846480. doi: 10.1155/2013/846480. [DOI] [PMC free article] [PubMed] [Google Scholar]