Abstract
Objective:
To improve the clearance of lower caliceal stones (LCSs) after shock wave lithotripsy (SWL) using a combination of intra-operative forced diuresis and inversion therapy.
Materials and Methods:
One hundred and fifty-seven consecutive patients with symptomatic, single LCSs of 5–20 mm size were prospectively randomized into two groups. The first (study group, SG) underwent SWL at the time of the maximum diuresis with the patient in the Trendelenburg position with an angle of 30 degree, while the second group (control group, CG) underwent standard SWL. After the last SWL session, patients were followed-up regularly using plain abdominal X-ray and renal ultrasound. The primary endpoint of the study was the stone-free rate (SFR) at 12 weeks.
Results:
A total of 141 patients completed the study treatment protocol and follow-up: 69 patients in SG and 72 patients in CG. Both groups were comparable in baseline data. SG showed significantly higher SFR at all follow-up time points. At week 12, 78.3% of SG were rendered stone free, whereas only 61.1% were stone free in CG (P = 0.030). Also, there was a significantly higher SFR for larger stones (>10 mm) and stones with higher attenuation value (>500 Hounsfield units) in SG than CG. Mild non-significant complications were reported in both groups.
Conclusion:
SWL with intraoperative forced diuresis and inversion seems to be an effective measure with minimal extra cost to improve LCS clearance post-SWL.
Keywords: Extracorporeal shockwave lithotripsy, inversion therapy, outcome, renal stone, stone free
INTRODUCTION
Shock wave lithotripsy (SWL) is the preferred treatment modality for most renal stones ≤ 2 cm in maximum length. In addition, SWL has high patient and practitioners’ acceptance owing to its convenience and non-invasiveness.[1] In spite of its safety, the high rate of residual fragments (RFs) of the lower caliceal stones (LCSs) after SWL has been the cause of concern.[2,3] It has been shown that these RFs can grow and may act as a nidus for further stone formation.[4,5,6,7,8] There is no standard auxiliary procedure to facilitate the clearance of LCS fragments after SWL. As a result, alternative invasive treatment modalities with a high clearance rate, such as percutaneous nephrolithotripsy (PCNL) or ureterorenoscopy (URS), are used instead of SWL for LCSs.[6,8,9]
As the gravity-dependent position of the lower calyces is the main factor inhibiting stone clearance after SWL for LCS, adjuvant procedures such as intraoperative inversion, urinary diuresis and mechanical percussion are used to facilitate stone clearance.[9,10,11,12,13]
The aim of the current study was to evaluate the combination of two adjuvant procedures, namely intraoperative forced diuresis and inversion, as a method for enhancing clearance of LCS fragments after SWL.
MATERIALS AND METHODS
Patients’ selection and assessment
After institutional ethics board approval, this randomized controlled study was conducted between August 2010 and January 2014. Patients ≥ 18 years old with symptomatic, single LCS of 5–20 mm maximum diameter who agreed to participate in the study and provided an informed written consent were included. All patients underwent (a) detailed history, (b) clinical examination, (c) laboratory investigations including routine urinalysis, complete blood cell count, serum creatinine, liver function tests, fasting blood glucose, serum electrolytes and coagulation profile, (d) renal ultrasonography, (e) plain abdominal X-ray for kidneys, ureter and urinary bladder (KUB) and (f) non-contrast computed tomography (NCCT) supplemented by contrast study if indicated. The stone size was determined by the largest dimensions of the stone on NCCT. The stone to skin distance (SSD) and stone attenuation value were also determined on NCCT as described elsewhere.[14]
Patients with morbid obesity, musclo-skeletal disorder that impede positioning, severe cardio-vascular or neurological diseases, previous failed SWL, urinary tract infection, elevated serum creatinine, uncontrolled coagulation disorders, abnormal renal anatomy (as horseshoe kidney, duplex kidney or bifid pelvis), severe hydronephrosis, obstructed calyx or urinary tract obstruction at any level in the ipsilateral renal unit and those with medical problems that contradicted overhydration, forced diuresis or inversion therapy, as well as patients requiring a pre-treatment auxiliary procedures such as JJ ureteral stent insertion or percutaneous nephrostomy drainage were excluded from the study.
Randomization
Patients who met the inclusion criteria were randomly assigned to two treatment groups. To distribute patients efficiently between groups, stratified-blocked randomization was performed using computer random tables in a 1:1 ratio. Patients were assigned to one of the two groups across two pre-determined stone size groupings at a cutoff 10 mm.
Study procedure
The first group (study group, SG) underwent SWL with the patient in the Trendelenburg position with an angle of 30 degree combined with intravenous hydration with 1000 mL normal saline solution and 20 mg furosemide that were started 30 min before and continued through the procedure; hence, SWL was performed during the diuresis phase. The second group (control group, CG) had standard SWL.
An electromagnetic shockwave generator was used and all patients were treated with the same machine (Dornier lithotripter SII, Dornier MedTech, Wessling, Germany). All patients were treated on an outpatient basis without anesthesia. Only intravenous sedoanalgesia (Meperidine Hydrochloride 1 mg/kg, to a maximum dose of 100 mg) was given 10 min before starting the SWL session. With the patients in a supine position, stone localization was performed using ultrasound and/or fluoroscopy guidance with exposure when needed. The shock wave frequency was 60–90/min and number of shocks per session was 3500 or until the stone was completely fragmented. At the end of the procedure, patients were discharged home on antibiotic and analgesic and encouraged to drink plenty of fluids during the post-SWL period. The patients were followed-up and re-SWL was carried out for a maximum of three sessions depending on the response.
Follow-up and outcome measurements
Patients were evaluated 4, 8, 12 and 24 weeks after the last SWL session by medical history taking, physical examination, urinalysis, serum creatinine, X-ray KUB and renal ultrasonography. At the follow-up week 4, patients with no signs of stone fragmentation were discharged from the treatment regimen and shifted to another treatment modality. At the end of follow-up, patients with large residual fragment (RF) (≥4 mm) were advised to continue SWL for up to two sessions while patients with small RF (<4 mm) that are expected to pass spontaneously without further treatment were scheduled for regular follow-up. The primary endpoint was the SFR at follow-up week 12. Stone-free status was defined as no visible stone or RF < 4 mm on ultrasonography and X-ray KUB. Number of SWL sessions, total number of shock waves, time to stone clearance and adverse events were also evaluated and compared in both groups.
Statistical analysis
Statistical analysis was performed using the commercially available Statistical Package for Social Science (SPSS, Chicago, IL, USA) with full analysis set principle (intent-to-treat set, who completed at least one post-SWL follow-up visit). The Fisher exact test was used to compare categorical variables while the Student t-test and ANOVA test were used to compare continuous variables. The Mann–Whitney U and Kruskal–Wallis tests were used for skewed data. The Pearson correlation test was used to determine the correlation between stone size and stone attenuation value and the number of shock waves required. A critical two-sided P < 0.05 was considered statistically significant. Sample size was calculated to detect a 30% difference in SFRs between the groups,[15,16] with a power of 80% and a 2-sided alfa of 5%. Therefore, 60 patients were calculated for each group, bringing the total sample size to 132, after adding 10% for expecting drop-out and loss to follow-up.
RESULTS
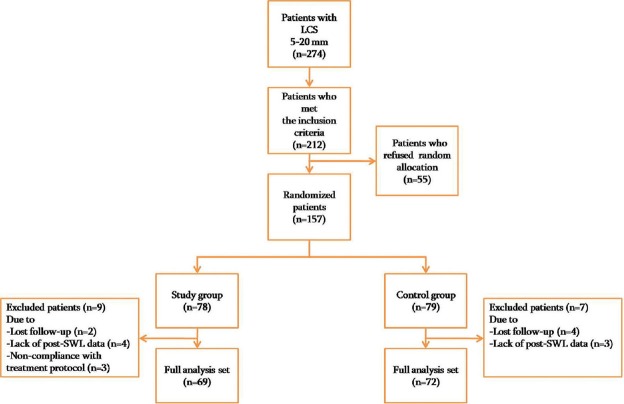
Of 274 patients with LCS, 212 met the inclusion criteria, of whom 55 refused random allocation. The remaining 157 were randomly divided into the study group (SG, 78 patients) and control group (CG, 79 patients). Nine patients from SG and seven patients from CG were excluded from analysis as they did not complete data at any post-SWL follow-up visit. Therefore, we were left with 69 patients in SG and 72 patients in CG [Figure 1].
Figure 1.
Study flow
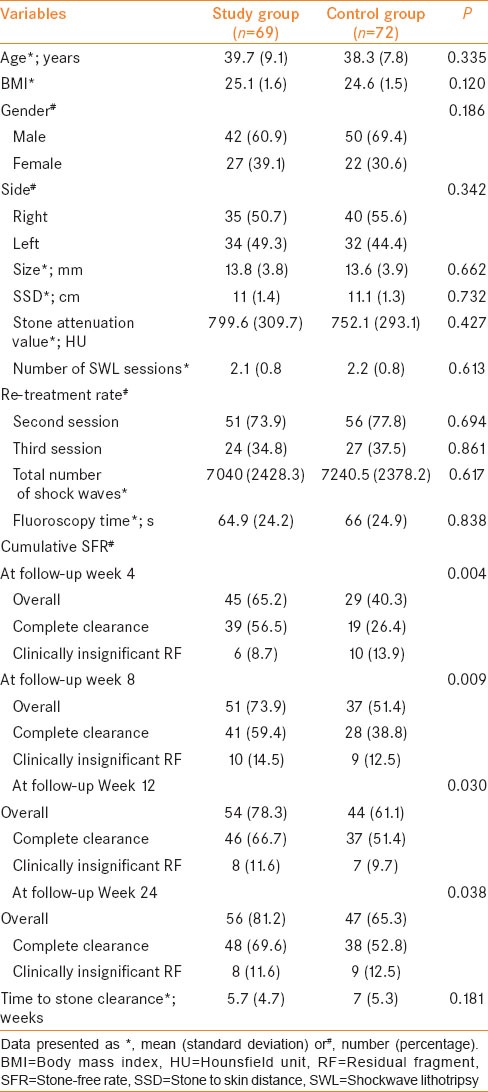
Both groups were comparable in terms of their demographic data and stone characteristics. A total of 21 patients (14.9%), nine (13%) in SG and 12 (16.6%) in CG, showed no sign of stone fragmentation at the follow-up week 4 and were shifted to other treatment modalities. The SFRs increased with time in both groups and were significantly higher in SG from the first follow-up visit till the end of the study. At follow-up week 12, the SFR was 78.3% in SG and 61.1% in CG (P = 0.030). At follow-up week 24, the SFRs increased to 81.2% in SG and 65.3% in CG (P = 0.038). No significant difference was observed between both groups regarding time to stone clearance (P = 0.181). The baseline data and treatment characteristics of the studied patients are summarized in Table 1.
Table 1.
Baseline and treatment characteristics, stone-free rate and time to stone clearance of the study and control groups
In both groups, the stone size and total number of SWL sessions and shock waves required until complete stone fragmentation correlated significantly (r = 0.672 and 0.601; P < 0.001). Also, the attenuation value and total number of SWL sessions and shock waves required until complete stone fragmentation correlated significantly (r = 0.776 and 0.771; P < 0.001).
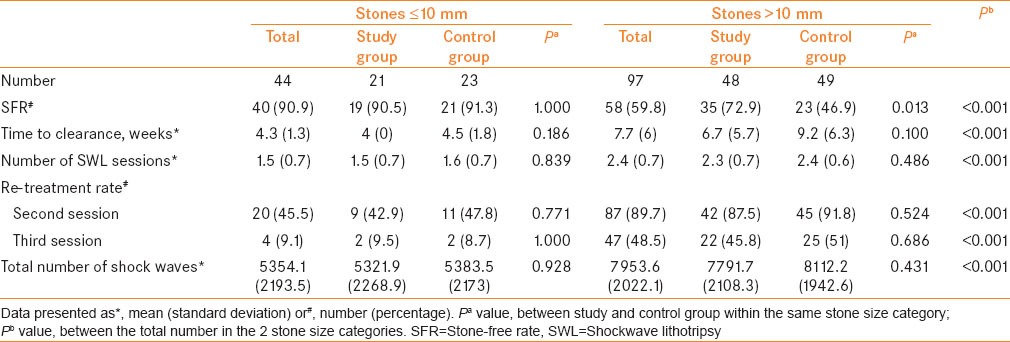
Stratified by size, the patients in SG with larger stones (>10 mm) were found to have significantly higher SFR at the end of the study (P = 0.013). Within both groups, stones ≤ 10 mm had significantly higher SFR, shorter time to stone clearance, lower re-treatment rate and fewer number of SWL sessions and shock waves than larger stones (P < 0.001) [Table 2].
Table 2.
Post-SWL lower caliceal stone clearance, time to stone clearance, number of SWL sessions and shockwaves required, stratified by stone size, in the study and control groups
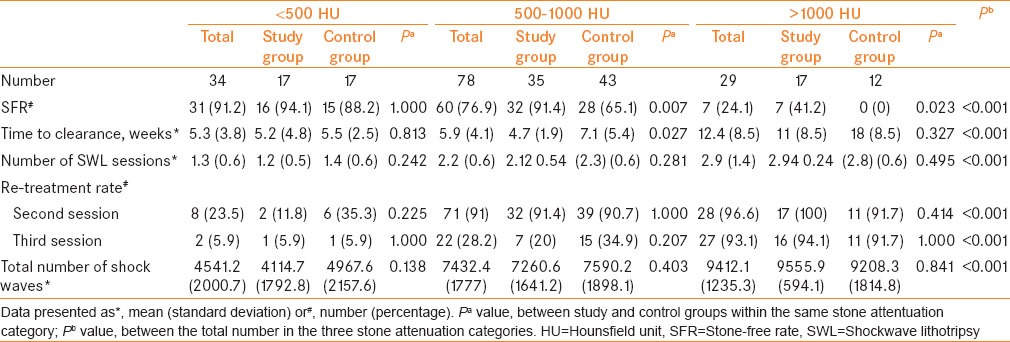
Based on attenuation value, the stones were categorized into ≤ 500 Hounsfield unit (HU), 500–1000 HU and >1000 HU. We found that stones with a higher attenuation value (>500 HU) had significantly higher SFR in SG than CG. Within both groups, stones with lower attenuation values had significantly higher SFR, shorter time to stone clearance, lower re-treatment rate and a fewer number of SWL sessions and shock waves (P < 0.001) [Table 3]. Post hoc test and all pairwise multiple comparisons were found to be significant (P < 0.001), except for time to stone clearance where no significant difference between stones with an attenuation value ≤500 and that for stones with an attenuation value 500–1000 (P = 0.585).
Table 3.
Post-SWL lower caliceal stone clearance, time to stone clearance, number of SWL sessions and shockwaves required, stratified by stone attenuation value, in the study and control groups
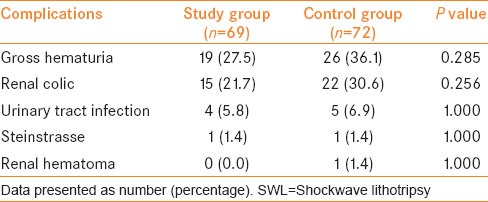
There were no significant differences between the study and control group in terms of post-SWL adverse events [Table 4]. All reported complications were mild and managed conservatively.
Table 4.
Post-SWL complications in the study and control groups
DISCUSSION
The combination of diuresis and inversion is an effective option in improving stone clearance of LCS after SWL. However, considerable clinical controversy still exists concerning the management of LCS due to concerns related to stone clearance rather than stone fragmentation. Secondary therapeutic procedures are usually necessary even after optimal SWL for LCS.[10,17]
Although PCNL is effective independent of stone size with an approximately 90% SFR, it is an invasive procedure that needs hospitalization and anesthesia as well as the associated morbidity such as bleeding, perforation of the collecting system, urosepsis and colon perforation, in addition to the troublesome nephrostomy tube inserted at the end of the procedure.[2,18] As a result, many authors have advocated adjuvant procedures to enhance clearance of lower caliceal fragments after SWL, such as inversion, diuresis, mechanical percussion and repetition of SWL.[9,13,19,20]
In this study, we prospectively evaluated the combined effect of both intra-operative forced diuresis and inversion in improving the clearance of fragmented LCS and overall SFR. The rationale for overcoming the effect of gravity by inversion with fragment flushing by forced diuresis during SWL was to increase the SFR in patients with LCS while avoiding the morbidity of more invasive procedures.
Fagment elimination is poorest from the lower pole calices due to their dependent position.[20,21] Computed tomography and magnetic resonance studies have demonstrated an oblique axis of the lower calyces with 20–30 degree tilt.[22,23] To overcome the gravity effect on the lower pole fragments, patients must be positioned head down for 30 degree or more. Sixty degree inversion therapy was tried; however, this was found to be uncomfortable.[13] Therefore, the 30 degree inversion position was adopted in the current cohort for being easier and comfortable for the patients. The inversion, diuresis and mechanical percussion was found to be 13-times more likely to render a patient stone free than observation alone.[13] Also, using boosted (stir–up) SWL significantly promotes the liberation of residual stone material.[20]
In the present study, when we combined two adjuvant measures, 78.3% of SFR was achieved after 12 weeks, which was significantly higher than in patients who were treated by standard SWL with only 61.1% SFR (P = 0.030). This was consistent with that reported by Leong et al.,[10] with an overall SFR of 76% and Albanis et al.,[12] with an overall SFR of 83%. The SFR improved with time as 81.2% being stone free at the follow-up week 24. This trend was also observed by Leong et al.[10] in their prospective study with 1-year follow-up.
The re-treatment rate, fluoroscopy time and mean number of SWL sessions and shockwaves needed for stone fragmentation in the current cohort were comparable between both groups. The re-treatment rate in the SG (73.9%) was lower than that previously reported by Leong et al.[10] using the same technique (90%), and constant with the average number of sessions used by Kupeli et al.[24] for the treatment of LCS, where 79.4% of their patients needed more than one session. The fluoroscopy time is dependent on the operator experience with significant differences between urologists.[25] The overall fluoroscopy time in the current study (65.5 s) was lower than the previously reported fluoroscopy average time of 156 and 147 s.[24,25,26] This is due to the limited use of fluoroscopy as we based mainly on ultrasound for stone localization. The fluoroscopy time is much less than that needed for PCNL, which averaged 25 min in LCS.[27]
Some authors have proposed that the lower caliceal anatomy as infundibulo-pelvic angle and infundibular length and width have an impact on the stone-free status after SWL.[8,23,24,28] However, more recent prospective studies have failed to find any significant effect of the differences in the intra-renal anatomy of lower calyx on stone clearance after SWL.[16,29,30] The lower caliceal infundibular diameter significantly differs during different phases of intravenous urography, where the post-voiding film showed the smallest width and early compression films showed the greatest width.[31] Therefore, it is realistic that the measurements of static images do not fully represent the dynamic system of lower pole drainage. As the role of evaluating lower pole anatomy has currently much controversy, the lower caliceal anatomy was not considerably evaluated in the current study. In a recent study, it was found that stone size rather than caliceal anatomy could predict treatment outcome post SWL.[16]
Stone size has a great impact on SFR after SWL for LCS. In the current study, a SFR of 90.9% was detected for stones smaller than 10 mm, which was higher than that reported by Leong et al.,[10] where only 79% of the patients with the same stone size were stone free. On the other hand, for the stones larger than 10 mm, the SFR was 59.8% in our SG, which was much higher than 23% SFR in the study of Albala et al.[16] but comparable to Lingeman et al.'s[2] meta-analysis and Leong et al.'s[10] study, where 56% and 69% of the patients with the same stone size (10–20 mm) rendered stone free.
Several studies have identified lower stone attenuation values as a predictor of SWL success.[14,32,33,34] Our results agree with these findings. We found that the SFR for stones ≤500 HU was 91.2% compared with 88.2% for stones 500–1000 HU and 24.1% for stones >1000 HU. This is related to stone fragmentation as the stone attenuation value is a good predictor for stone fragility and dispersal of stone material is important for diuresis to flush them out during SWL.
When we compared the SFR in both groups regarding the stone size and stone attenuation value, we found that there was a significantly higher SFR for larger stones (>10 mm) and stones with higher attenuation value (>500 HU) in patients treated with simultaneous inversion/diuresis than those treated with standard SWL. In clinical practice, this indicates the higher benefit of adjuvant procedures even if it is applied to larger and harder stones.
There were no significant differences between both groups regarding SWL-related complications. All reported complications were mild and comparable to that previously reported.[13,20,35,36]
Despite being a prospective study, this cohort has its shortcomings. The main limitation is using two measures simultaneously to facilitate stone clearance; therefore, it is unclear which measure had greater contribution. However, as these measures are simple and non-invasive, it can be combined together without harm to achieve the ultimate goal of stone clearance. Also, our patients were followed by X-ray KUB and renal ultrasonography, which may have limited the ability to detect residual fragments. Further three-arm studies and follow-up of patients with low radiation NCCT may be warranted to document a greater depth of precise information about the beneficial effect of the two adjuvant procedures separately.
CONCLUSION
SWL with forced diuresis and inversion seems to be an effective minimally invasive option to improve the clearance of LCS fragments. This therapy might be a valuable alternative to the more invasive treatment modalities such as PCNL or URS for lower caliceal stones less than 20 mm.
ACKNOWLEDGMENTS
The authors are grateful to Maria Christa G. Bernardo, Glenalyn Z. Goyena, Maxshane Grace R. Mariano and Sophiamol Joseph for technical assistance and reporting data.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Tiselius HG, Ackermann D, Alken P, Buck C, Conort P, Gallucci M. Guidelines on urolithiasis. Eur Urol. 2001;40:362–71. doi: 10.1159/000049803. [DOI] [PubMed] [Google Scholar]
- 2.Lingeman JE, Siegel YI, Steele B, Nyhuis AW, Woods JR. Management of lower pole nephrolithiasis: A critical analysis. J Urol. 1994;151:663–7. doi: 10.1016/s0022-5347(17)35042-5. [DOI] [PubMed] [Google Scholar]
- 3.Graff J, Diederichs W, Schulze H. Long-term followup in 1,003 extracorporeal shock wave lithotripsy patients. J Urol. 1988;140:479–83. doi: 10.1016/s0022-5347(17)41696-x. [DOI] [PubMed] [Google Scholar]
- 4.Beck EM, Riehle RA., Jr The fate of residual fragments after extracorporeal shock wave lithotripsy monotherapy of infection stones. J Urol. 1991;145:6–9. doi: 10.1016/s0022-5347(17)38230-7. discussion -10. [DOI] [PubMed] [Google Scholar]
- 5.Buchholz NP, Meier-Padel S, Rutishauser G. Minor residual fragments after extracorporeal shockwave lithotripsy: Spontaneous clearance or risk factor for recurrent stone formation? J Endourol. 1997;11:227–32. doi: 10.1089/end.1997.11.227. [DOI] [PubMed] [Google Scholar]
- 6.Carr LK, D’A Honey J, Jewett MA, Ibanez D, Ryan M, Bombardier C. New stone formation: A comparison of extracorporeal shock wave lithotripsy and percutaneous nephrolithotomy. J Urol. 1996;155:1565–7. doi: 10.1016/s0022-5347(01)66127-5. [DOI] [PubMed] [Google Scholar]
- 7.Talati J. In: The management of lithiasis: The rationale development of technology. Boston: Kluwer Academic Publishers; 1997. The residual calcular fragments: a risk factor for recurrent stone disease; pp. 269–73. [Google Scholar]
- 8.Elbahnasy AM, Clayman RV, Shalhav AL, Hoenig DM, Chandhoke P, Lingeman JE, et al. Lower-pole caliceal stone clearance after shockwave lithotripsy, percutaneous nephrolithotomy, and flexible ureteroscopy: Impact of radiographic spatial anatomy. J Endourol. 1998;12:113–9. doi: 10.1089/end.1998.12.113. [DOI] [PubMed] [Google Scholar]
- 9.Netto NR, Jr, Claro JF, Lemos GC, Cortado PL. Renal calculi in lower pole calices: What is the best method of treatment? J Urol. 1991;146:721–3. doi: 10.1016/s0022-5347(17)37905-3. [DOI] [PubMed] [Google Scholar]
- 10.Leong WS, Liong ML, Liong YV, Wu DB, Lee SW. Does simultaneous inversion during extracorporeal shock wave lithotripsy improve stone clearance: A long-term, prospective, single-blind, randomized controlled study. Urology. 2014;83:40–4. doi: 10.1016/j.urology.2013.08.004. [DOI] [PubMed] [Google Scholar]
- 11.Chiong E, Hwee ST, Kay LM, Liang S, Kamaraj R, Esuvaranathan K. Randomized controlled study of mechanical percussion, diuresis, and inversion therapy to assist passage of lower pole renal calculi after shock wave lithotripsy. Urology. 2005;65:1070–4. doi: 10.1016/j.urology.2004.12.045. [DOI] [PubMed] [Google Scholar]
- 12.Albanis S, Ather HM, Papatsoris AG, Masood J, Staios D, Sheikh T, et al. Inversion, hydration and diuresis during extracorporeal shock wave lithotripsy: Does it improve the stone-free rate for lower pole stone clearance? Urol Int. 2009;83:211–6. doi: 10.1159/000230026. [DOI] [PubMed] [Google Scholar]
- 13.Pace KT, Tariq N, Dyer SJ, Weir MJ, D’A Honey RJ. Mechanical percussion, inversion and diuresis for residual lower pole fragments after shock wave lithotripsy: A prospective, single blind, randomized controlled trial. J Urol. 2001;166:2065–71. [PubMed] [Google Scholar]
- 14.Tanaka M, Yokota E, Toyonaga Y, Shimizu F, Ishii Y, Fujime M, et al. Stone attenuation value and cross-sectional area on computed tomography predict the success of shock wave lithotripsy. Korean J Urol. 2013;54:454–9. doi: 10.4111/kju.2013.54.7.454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.D’a Honey RJ, Luymes J, Weir M, Kodama R, Tariq N. Mechanical percussion inversion can result in relocation of lower pole stone fragments after shock wave lithotripsy. Urology. 2000;55:204–6. doi: 10.1016/s0090-4295(99)00527-0. [DOI] [PubMed] [Google Scholar]
- 16.Albala DM, Assimos DG, Clayman RV, Denstedt JD, Grasso M, Gutierrez-Aceves J, et al. Lower pole I: A prospective randomized trial of extracorporeal shock wave lithotripsy and percutaneous nephrostolithotomy for lower pole nephrolithiasis-initial results. J Urol. 2001;166:2072–80. doi: 10.1016/s0022-5347(05)65508-5. [DOI] [PubMed] [Google Scholar]
- 17.Nagele U, Knoll T, Schilling D, Michel MS, Stenzl A. Lower pole calyceal stones. Urologe A. 2008;47:875–84. doi: 10.1007/s00120-008-1780-8. [DOI] [PubMed] [Google Scholar]
- 18.Lingeman JE, Coury TA, Newman DM, Kahnoski RJ, Mertz JH, Mosbaugh PG, et al. Comparison of results and morbidity of percutaneous nephrostolithotomy and extracorporeal shock wave lithotripsy. J Urol. 1987;138:485–90. doi: 10.1016/s0022-5347(17)43236-8. [DOI] [PubMed] [Google Scholar]
- 19.Kaye KW. Renal anatomy for endourologic stone removal. J Urol. 1983;130:647–8. doi: 10.1016/s0022-5347(17)51384-1. [DOI] [PubMed] [Google Scholar]
- 20.Krings F, Tuerk C, Steinkogler I, Marberger M. Extracorporeal shock wave lithotripsy retreatment (“stir-up”) promotes discharge of persistent caliceal stone fragments after primary extracorporeal shock wave lithotripsy. J Urol. 1992;148:1040–1. doi: 10.1016/s0022-5347(17)36810-6. [DOI] [PubMed] [Google Scholar]
- 21.Newman D, Scott J, Lingeman J. Two year follow up of patients treated with ESWL. J Endourol. 1988;2:163–71. [Google Scholar]
- 22.Robert M, Maubon A, Roux JO, Rouanet JP, Navratil H. Direct percutaneous approach to the upper pole of the kidney: MRI anatomy with assessment of the visceral risk. J Endourol. 1999;13:17–20. doi: 10.1089/end.1999.13.17. [DOI] [PubMed] [Google Scholar]
- 23.Hopper KD, Yakes WF. The posterior intercostal approach for percutaneous renal procedures: Risk of puncturing the lung, spleen, and liver as determined by CT. AJR Am J Roentgenol. 1990;154:115–7. doi: 10.2214/ajr.154.1.2104692. [DOI] [PubMed] [Google Scholar]
- 24.Kupeli B, Biri H, Sinik Z, Karaca K, Tuncayengin A, Karaoglan U, et al. Extracorporeal shock wave lithotripsy for lower caliceal calculi. Eur Urol. 1998;34:203–6. doi: 10.1159/000019713. [DOI] [PubMed] [Google Scholar]
- 25.Logarakis NF, Jewett MA, Luymes J, Honey RJ. Variation in clinical outcome following shock wave lithotripsy. J Urol. 2000;163:721–5. [PubMed] [Google Scholar]
- 26.Carter HB, Naslund EB, Riehle RA., Jr Variables influencing radiation exposure during extracorporeal shock wave lithotripsy. Review of 298 treatments. Urology. 1987;30:546–50. doi: 10.1016/0090-4295(87)90433-x. [DOI] [PubMed] [Google Scholar]
- 27.Bush WH, Jones D, Brannen GE. Radiation dose to personnel during percutaneous renal calculus removal. AJR Am J Roentgenol. 1985;145:1261–4. doi: 10.2214/ajr.145.6.1261. [DOI] [PubMed] [Google Scholar]
- 28.Parr NJ, Ritchie AW, Smith G, Moussa SA, Tolley DA. Does further extracorporeal lithotripsy promote clearance of small residual fragments? Br J Urol. 1991;68:565–7. doi: 10.1111/j.1464-410x.1991.tb15415.x. [DOI] [PubMed] [Google Scholar]
- 29.Sorensen CM, Chandhoke PS. Is lower pole caliceal anatomy predictive of extracorporeal shock wave lithotripsy success for primary lower pole kidney stones? J Urol. 2002;168:2377–82. doi: 10.1016/S0022-5347(05)64149-3. [DOI] [PubMed] [Google Scholar]
- 30.Madbouly K, Sheir KZ, Elsobky E. Impact of lower pole renal anatomy on stone clearance after shock wave lithotripsy: fact or fiction? J Urol. 2001;165:1415–8. [PubMed] [Google Scholar]
- 31.Pace KT, Weir MJ, Harju M, Tariq N, D’A Honey RJ. Individual patient variation and inter-rater reliability of lower calyceal infundibular width on routine intravenous pyelography. BJU Int. 2003;92:607–9. doi: 10.1046/j.1464-410x.2003.04452.x. [DOI] [PubMed] [Google Scholar]
- 32.Pareek G, Hedican SP, Lee FT, Jr, Nakada SY. Shock wave lithotripsy success determined by skin-to-stone distance on computed tomography. Urology. 2005;66:941–4. doi: 10.1016/j.urology.2005.05.011. [DOI] [PubMed] [Google Scholar]
- 33.Perks AE, Gotto G, Teichman JM. Shock wave lithotripsy correlates with stone density on preoperative computerized tomography. J Urol. 2007;178:912–5. doi: 10.1016/j.juro.2007.05.043. [DOI] [PubMed] [Google Scholar]
- 34.Kacker R, Zhao L, Macejko A, Thaxton CS, Stern J, Liu JJ, et al. Radiographic parameters on noncontrast computerized tomography predictive of shock wave lithotripsy success. J Urol. 2008;179:1866–71. doi: 10.1016/j.juro.2008.01.038. [DOI] [PubMed] [Google Scholar]
- 35.Delius M, Enders G, Xuan ZR, Liebich HG, Brendel W. Biological effects of shock waves: Kidney damage by shock waves in dogs--dose dependence. Ultrasound Med Biol. 1988;14:117–22. doi: 10.1016/0301-5629(88)90178-0. [DOI] [PubMed] [Google Scholar]
- 36.Fuchs G. Effects of extracorporeally induced high energy shockwaves on the rabbit kidney and ureter: A morphologic and functional study. J Endourol. 1988;2:341. [Google Scholar]