Abstract
Context:
Hypoxemia is a common and potentially lethal complication of acute respiratory infection in children under-five, particularly among those with severe disease.
Aims:
The aim of this study was to determine the prevalence of hypoxemia in under-five Sudanese children with pneumonia.
Settings and Design:
A cross-sectional study conducted in a pediatrics hospital in a developing country.
Subjects and Methods:
Data were collected using structured questionnaire and oxygen saturation was measured using a pulse oximeter. Hypoxemia was defined as arterial blood oxygen saturation <90%.
Results:
Of 150 studied patients, 86 (57.3%) were males and 46 (32%) were in the age group 2 to ≤12 months. Of the total number, 42.7% had hypoxemia (with pulse oximeter oxygen saturation <90%), out of them 36 (56.25%) were in the age group <2 months. Of the hypoxic patients, 30 (46.88%) had severe pneumonia, and 7 (10.94) had very severe pneumonia (P < 0.001).
Conclusions:
The prevalence of hypoxemia was 42.7% among the studied population. There was a significant association between the hypoxemia and small age group and very severe pneumonia. In limited resource settings pulse oximeter can be used to correctly identify hypoxemia in under-five children particularly among those diagnosed clinically as very severe pneumonia.
Keywords: Children, hypoxemia, pneumonia, pulse oximeter, Sudan
Introduction
Pneumonia is one of the most common global childhood illnesses, and it is the most common cause of childhood mortality. It has been identified as the major “forgotten killer of children” by the United Nations Children's Fund and the World Health Organization (WHO).[1] Pneumonia is the leading cause of the infection-attributable mortality in under-5-year-old children. Recent global estimates indicate that there are 10 million deaths annually of this age group and that 99% of these deaths occur in developing countries, with 70% caused by infections.[1] Many of these deaths are potentially preventable if appropriate clinical and laboratory tools are in place to facilitate early detection of the pneumonia, identification of the pathogen involved, and institution of appropriate therapy or, even better, implementation of appropriate vaccination schedules.[2]
The incidence of acute respiratory infection (ARI) in children under-five is estimated to be 0.22 episodes per child-year in developing countries, translated into 151 million new episodes each year.[3] Of all community pneumonia cases, 7–13% is severe enough to be life-threatening and requires hospitalization.[3] In Sudan, the estimated numbers of pneumonia episodes in 2004 was 2 million.[4]
Pneumonia is responsible for about 21% of all deaths in children aged <5 years, and it is estimated that of every 1000 children born alive, 12–20 will die from pneumonia before their fifth birthday.[5] WHO developed a case management strategy in the 1980s aiming to reduce deaths from pneumonia. This was a cornerstone of the ARI program and was later incorporated into the Integrated Management of Childhood Illness (IMCI) guidelines, which include primary care and hospital-based case management.[1] One of the most important basis for the case management strategy was that: Hypoxemia is common and potentially associated with increased risk of death.[6,7]
Hypoxemia is a common and potentially lethal complication of ARI in under-five children, particularly among those with severe disease and those living at high altitude.[7,8,9] Hypoxemia prevalence among childhood pneumonia cases varies widely between geographic regions and at different altitudes, as well as with pneumonia severity.[10] 13.3% of WHO-defined pneumonia cases globally are hypoxemic.[11] In lower-lying African countries, prevalence ranges from 3% to 10%, whereas in Asia at higher altitudes prevalence ranges from 9% to 39%. Hypoxemia at baseline also is a common cause of treatment failure in hospitalized children with pneumonia.[12] Early detection of hypoxemia, and oxygen therapy improves the outcome of children with ARI. In developing countries, facilities for measuring arterial oxygen saturation are not available in most settings, which make it difficult for health providers to detect hypoxemia in children with ARI. Most health providers rely on symptoms and signs to identify hypoxemia and start oxygen therapy.[13] In the setting of limited resource hospitals, the presence of a pulse oximeter might help a lot in early detection of hypoxemia.
In Sudan, there is no published data about the prevalence of hypoxemia.
The aim of this study is, therefore, to determine the prevalence of hypoxemia in under-five children with pneumonia in an emergency pediatrics hospital using a pulse oximeter.
Subjects and Methods
An observational, cross-sectional, hospital-based study was conducted in Mohamed Alamin Hamid Hospital for children. It is one of the major pediatrics hospitals in Omdurman city at an elevation of 390 m. It is a 350 beds pediatrics hospital. The frequency of patients seen per 24 h is 300–350. About 30–40 are admitted to the ARI unit per day, 10–12 of them for 24 h.
The populations of this study were children aged from 2 months up to 5 years who presented to the ARI emergency unit with an acute history of cough and rapid respiration or difficulty in breathing. Children with asthma were excluded. Patients were selected using simple random sampling technique.
Data were collected using structured questionnaire. Variables included were gender, and age. In addition to findings of the history which was obtained from the mother about the presence of various symptoms: Cough, fever, and difficulty in breathing, rapid breathing, diarrhea, irritability, convulsions, feeding pattern, and inability to drink/feed.
The clinical examination was done by one of the investigators. Children with pneumonia were then classified according to the WHO guidelines of acute lower respiratory tract infections (ALRIs)[14] into mild, severe, and very severe. Children aged 2–60 months who presented with chest in-drawing and/or fast breathing were classified as having severe pneumonia; children with fast breathing and had one or more of the danger signs (convulsions, sleepy/difficult to awake, unable to breastfeed/drink, stridor, flaring of alae nasi, chest in-drawing, and fever) were classified as having very severe pneumonia.
Oxygen saturation was measured by a registered nurse using a digital pulse oximeter (Geratherm® oxy control, Germany) attached to the finger or toe. Recordings were taken after stabilization of the pulse oximetry reading for 1-min while the child was breathing room air. Hypoxemia was defined as arterial blood oxygen saturation, SpO2, below 90%.
Informed consent was obtained from the guardians of all the study participants. The study was performed in line with the declaration of Helsinki. Ethical approval was obtained from the institutional ethical committee.
The data were analyzed using software program SPSS version 19.0 (IBM SPSS Statistics). Chi-square tests (χ2) were used to compare means between the groups, and statistical significance was defined as P < 0.05.
Results
A total of 150 children with pneumonia were enrolled in this study. Of them, 86 (57.3%) were males. The children were categorized into two age groups: 2 to ≤12 months and >12–60 months. There were 48 (32%) in the first group [Figure 1].
Figure 1.
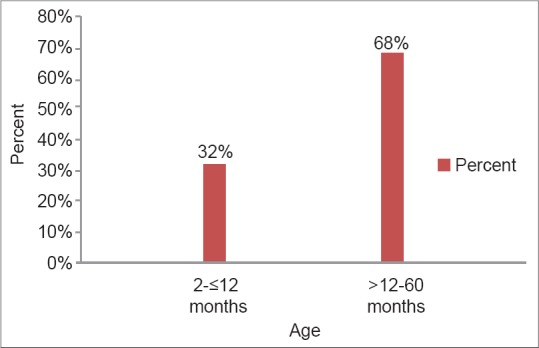
Distribution of the study group according to age
The children studied were classified according to the severity of the condition. Of the children studied 7 (4.6%) presented with very severe pneumonia, 70 (46.7%) with severe pneumonia, and 73 (48.7%) with pneumonia [Figure 2].
Figure 2.
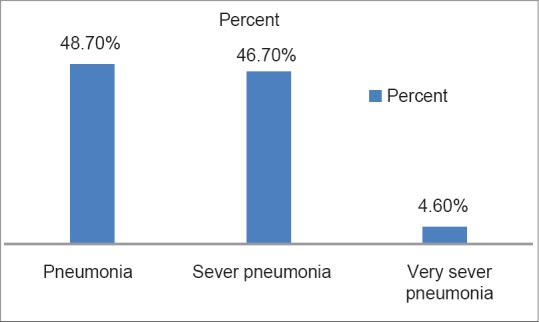
Classification of pneumonia according to the Integrated Management of Childhood Illness among the studied children
Of 150 studied children, 42.7% of patients had hypoxemia (with pulse oximeter oxygen saturation < 90%), 36 (56.25%) were in the age group <2 months. Of the hypoxic patients, 30 (46.88%) have severe pneumonia and 7 (10.94) have very severe pneumonia.
Using inferential statistics hypoxemia was found to be more in the small age group (P < 0.001) [Figure 3]. Hypoxemia also increased in male sex but not of statistical significance (P = 0.72). Hypoxemia significantly increased in patients diagnosed as very severe disease (P < 0.001) [Figure 4]. Presence of hypoxemia was significantly associated with the presence of danger signs collectively (P < 0.01).
Figure 3.
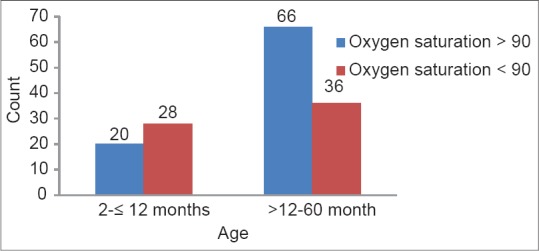
Relation between oxygen saturation and age of the studied children
Figure 4.
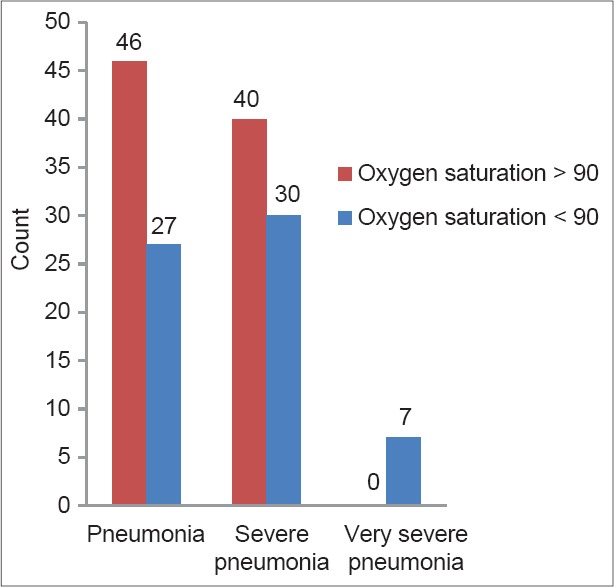
Relationship between oxygen saturation and classification of pneumonia among the studied population
Discussion
This study revealed that 42.7% of patients who were hospitalized and radiologically confirmed to have pneumonia had hypoxemia. These results were comparable to what Lozano reported following his systematic review of the published literature to determine the prevalence of hypoxemia in under-five children suffering from acute lower respiratory infections from out-patient clinics, emergency departments, and hospital wards in 23 health facilities from 10 countries.[7] Seventeen published studies were found, that included 4021 under-five children with ARI, and reported that out-patient children with a clinical diagnosis of upper ARI had a low risk of hypoxemia (pooled estimate of 6–9%).[7] The prevalence increased to 31% and to 43% in patients in emergency departments and in cases with clinical pneumonia, respectively, and it was even higher among hospitalized children (47%) and in those with radiographically confirmed pneumonia (72%).[7]
In other studies done in India hypoxemia prevalence was found to be in a range between 23.8%, and 25.7% of the study groups, but those studies were conducted in the out-patient departments, which included all children with ARI and radiological confirmation of pneumonia.[9,15] Other studies revealed a prevalence range between 9.3% and 37.5%.[11,16]
This study revealed that hypoxemia was found to be more in the small age group (P < 0.001). This is in accordance with the results of Basnet et al. who found that the number of infants with respiratory illness (P = 0.03) and hypoxemia (Odds ratio = 2.21, 95% confidence interval 1.03, 4.76) was significantly higher.[17] Furthermore, De Graaff et al. reported that the incidence of the intraoperative hypoxemia increased with younger age with the highest incidence in neonates.[18]
In the current study, hypoxemia was significantly increased in very severe pneumonia. This was found to be in consistent with many other studies done to predict hypoxemia in children with pneumonia. Zhang, et al., showed that clinical severity correlates with case-fatality rate, while, nonsevere pneumonia is far more common than severe pneumonia, most deaths occur in children with severe pneumonia.[19]
The presence of danger signs (convulsions, sleepy/difficult to awake, unable to breastfeed/drink, stridor, flaring of alae nasi, chest in-drawing, and fever), collectively was found to be significantly associated with hypoxemia in this study. This was in concordance with study done by Rao, et al., where chest wall retraction, which is a sign of severe pneumonia, was observed to be the most sensitive indicator of hypoxemia (sensitivity = 90%).[9] In the same study nasal flaring (sensitivity = 84%) was also detected as an important indicator. Inability to feed which is a danger sign according to IMCI and indicator of very severe pneumonia was also considered high indicator of hypoxemia in their patients with pneumonia (sensitivity = 81%).[9] However, it is contradicted by Lodha et al. and Dyke et al. who concluded that clinical symptoms and sings alone or in combination do not have sufficient sensitivity and specificity to predict hypoxemia in children with ALRI.[15,20] Misdiagnosis of the presence or absence of hypoxemia using clinical signs alone is common.[16] A systematic review and meta-analysis of prospective diagnostic studies that evaluated the accuracy of individual or combined clinical symptoms and signs in predicting hypoxemia among children aged <5 years with ARI, revealed that cyanosis, inability to feed, head nodding, respiratory rate >70/min and unresponsiveness/impaired arousability had high specificity but low sensitivity.[19] About 20% of hypoxemic children would be missed, and 17–50% of children given supplemental oxygen would not need it in high sensitivity models based on clinical signs.[8]
When used correctly, pulse oximetry can provide reliable monitoring with little or no distress to the patient, and is the accepted standard for detecting hypoxemia in developing countries. Pulse oximetry can correctly identify 20–30% more children with hypoxemias than using clinical signs alone.[21] Pulse oximetry can ensure the most efficient use of oxygen therapy, which is especially important in resource-limited settings. As not all patients with signs associated with hypoxemia will have hypoxemia, the use of oximetry can also reduce unnecessary oxygen use.[8,21,22,23,24]
The limitations of this study include that it did not study the sensitivity and specificity of pulse oximeter by measuring oxygen saturation using blood gas analyzer, which was not available in this hospital. This should also be compared with sensitivity, and specificity of clinical signs alone.
Conclusions
The prevalence of hypoxemia was 42.7% among the studied population. There was a significant correlation between the hypoxemia and small age group, very severe pneumonia and presence of danger signs in children with pneumonia (P < 0.001). In limited resource settings, recording oxygen saturation by the pulse oximeter is highly recommended in all patients with pneumonia, to avoid potentially fatal complications.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
References
- 1.Wardlaw T, Johansson EW, Hodge M. UNICEF's Division of Communication. New York: WHO Press; 2006. Pneumonia: The Forgotten Killer of Children. [Google Scholar]
- 2.Pitcher D, Chalker VJ, Sheppard C, George RC, Harrison TG. Real-time detection of Mycoplasma pneumoniae in respiratory samples with an internal processing control. J Med Microbiol. 2006;55:149–55. doi: 10.1099/jmm.0.46281-0. [DOI] [PubMed] [Google Scholar]
- 3.Rudan I, Boschi-Pinto C, Biloglav Z, Mulholland K, Campbell H. Epidemiology and etiology of childhood pneumonia. Bull World Health Organ. 2008;86:408–16. doi: 10.2471/BLT.07.048769. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Mafubelu D, Mason L. Child and Adolescent Health and Development Progress Report 2009: Highlights, Printed. France: WHO Press; 2010. [Google Scholar]
- 5.Williams BG, Gouws E, Boschi-Pinto C, Bryce J, Dye C. Estimates of world-wide distribution of child deaths from acute respiratory infections. Lancet Infect Dis. 2002;2:25–32. doi: 10.1016/s1473-3099(01)00170-0. [DOI] [PubMed] [Google Scholar]
- 6.Duke T, Mgone J, Frank D. Hypoxaemia in children with severe pneumonia in Papua New Guinea. Int J Tuberc Lung Dis. 2001;5:511–9. [PubMed] [Google Scholar]
- 7.Lozano JM. Epidemiology of hypoxaemia in children with acute lower respiratory infection. Int J Tuberc Lung Dis. 2001;5:496–504. [PubMed] [Google Scholar]
- 8.Duke T, Blaschke AJ, Sialis S, Bonkowsky JL. Hypoxaemia in acute respiratory and non-respiratory illnesses in neonates and children in a developing country. Arch Dis Child. 2002;86:108–12. doi: 10.1136/adc.86.2.108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Rao YK, Midha T, Kumar P, Tripathi VN, Rai OP. Clinical predictors of hypoxemia in Indian children with acute respiratory tract infection presenting to pediatric emergency department. World J Pediatr. 2012;8:247–51. doi: 10.1007/s12519-012-0365-1. [DOI] [PubMed] [Google Scholar]
- 10.Junge S, Palmer A, Greenwood BM, Kim Mulholland E, Weber MW. The spectrum of hypoxaemia in children admitted to hospital in the Gambia, West Africa. Trop Med Int Health. 2006;11:367–72. doi: 10.1111/j.1365-3156.2006.01570.x. [DOI] [PubMed] [Google Scholar]
- 11.Subhi R, Adamson M, Campbell H, Weber M, Smith K, Duke T, et al. The prevalence of hypoxaemia among ill children in developing countries: A systematic review. Lancet Infect Dis. 2009;9:219–27. doi: 10.1016/S1473-3099(09)70071-4. [DOI] [PubMed] [Google Scholar]
- 12.Jain DL, Sarathi V, Jawalekar S. Predictors of treatment failure in hospitalized children [3-59 months] with severe and very severe pneumonia. Indian Pediatr. 2013;50:787–9. doi: 10.1007/s13312-013-0220-z. [DOI] [PubMed] [Google Scholar]
- 13.Singhi S, Deep A, Kaur H. Prevalence and predictors of hypoxemia in acute respiratory infections presenting to pediatric emergency department. Indian J Crit Care Med. 2003;7:118–23. [Google Scholar]
- 14.Acute Respiratory Infections in Children: Case Management in Small Hospitals in Developing Countries. Geneva: WHO/ARI/90.5; 1990. World Health Organization Programme for the Control of Acute Respiratory Infections. [Google Scholar]
- 15.Lodha R, Bhadauria PS, Kuttikat AV, Puranik M, Gupta S, Pandey RM, et al. Can clinical symptoms or signs accurately predict hypoxemia in children with acute lower respiratory tract infections? Indian Pediatr. 2004;41:129–35. [PubMed] [Google Scholar]
- 16.Duke T, Graham SM, Cherian MN, Ginsburg AS, English M, Howie S, et al. Oxygen is an essential medicine: A call for international action. Int J Tuberc Lung Dis. 2010;14:1362–8. [PMC free article] [PubMed] [Google Scholar]
- 17.Basnet S, Adhikari RK, Gurung CK. Hypoxemia in children with pneumonia and its clinical predictors. Indian J Pediatr. 2006;73:777–81. doi: 10.1007/BF02790384. [DOI] [PubMed] [Google Scholar]
- 18.De Graaff JC, Bijker JB, Kappen TH, van Wolfswinkel L, Zuithoff NP, Kalkman CJ. Incidence of intraoperative hypoxemia in children in relation to age. Anesth Analg. 2013;117:169–75. doi: 10.1213/ANE.0b013e31829332b5. [DOI] [PubMed] [Google Scholar]
- 19.Zhang L, Mendoza-Sassi R, Santos JC, Lau J. Accuracy of symptoms and signs in predicting hypoxaemia among young children with acute respiratory infection: A meta-analysis. Int J Tuberc Lung Dis. 2011;15:317–25. [PubMed] [Google Scholar]
- 20.Dyke T, Lewis D, Heegaard W, Manary M, Flew S, Rudeen K. Predicting hypoxia in children with acute lower respiratory infection: A study in the highlands of Papua New Guinea. J Trop Pediatr. 1995;41:196–201. doi: 10.1093/tropej/41.4.196. [DOI] [PubMed] [Google Scholar]
- 21.Graham SM, English M, Hazir T, Enarson P, Duke T. Challenges to improving case management of childhood pneumonia at health facilities in resource-limited settings. Bull World Health Organ. 2008;86:349–55. doi: 10.2471/BLT.07.048512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Lee WW, Mayberry K, Crapo R, Jensen RL. The accuracy of pulse oximetry in the emergency department. Am J Emerg Med. 2000;18:427–31. doi: 10.1053/ajem.2000.7330. [DOI] [PubMed] [Google Scholar]
- 23.Weber MW, Mulholland EK. Pulse oximetry in developing countries. Lancet. 1998;351:1589. doi: 10.1016/s0140-6736(05)61160-9. [DOI] [PubMed] [Google Scholar]
- 24.Duke T, Subhi R, Peel D, Frey B. Pulse oximetry: Technology to reduce child mortality in developing countries. Ann Trop Paediatr. 2009;29:165–75. doi: 10.1179/027249309X12467994190011. [DOI] [PubMed] [Google Scholar]


