Abstract
Background:
Scrub typhus is one of the differential diagnoses for fever with thrombocytopenia. ARDS associated with Scrub typhus has high morbidity and mortality.
Aims:
To evaluate clinical features, lab values, and outcome in patients with scrub typhus and comparison in patients with or without ARDS.
Methods:
A prospective observational study was conducted on 109 patients with febrile illness and thrombocytopenia during a period of 12 months. All 109 patients were tested with both Immune-chromatography test and Weil felix test. Patients having either Immune-chromatography test/Weil felix test positive have been included and considered as scrub typhus positive whereas negative for both Immune-chromatography and Weil felix test were excluded. Clinical features, lab parameters, and outcome were evaluated in all patients with scrub typhus. Statistical analysis used in this study was T-test.
Results:
Among 58 patients who were included (After exclusion of 51 patients among total of 109 patients) 34 patients had no ARDS and 24 patients had ARDS. The clinical feature like dyspnoea, cough, low blood pressure (MAP<65 mmHg), IVC collapsibility (by ultrasound) and laboratory parameters like decreased Hemoglobin, Hematocrit, Serum albumin, and increased serum creatinine, serum total bilirubin, SGOT, SGPT, LDH, CPK, and serum lactate were statistically significant (P < 0.0001) in scrub typhus patients group with ARDS. The higher titers of Weil-felix can be correlated with more severe form of disease according to our observation. All 34 Scrub typhus patients without ARDS recovered completely. Among 24 Scrub typhus patients with ARDS, 22 patients recovered, and 2 patients died.
Conclusion:
Scrub typhus is an important differential diagnosis in a patients having fever with thrombocytopenia. Scrub typhus associated with ARDS has high morbidity and mortality. Early diagnosis and treatment with doxycycline can prevent the occurrence of ARDS
Keywords: Acute respiratory distress syndrome, immunochromatography test, screening criteria, scrub typhus, thrombocytopenia, Weil-Felix test
Introduction
Scrub typhus is a mite borne acute infectious disease caused by Orientia tsutsugamushi.[1] The term scrub means the type of vegetation (Terrain between woods and clearings) that harbors the vector and typhus means “fever with stupor” or smoke in Greek. “Tsutsugamushi” means small and dangerous, and “mushi” means insect or mite. Humans are accidental hosts. It affects people of all age. Scrub typhus is endemic in so called “tsutsugamushi triangle” such as Japan, Taiwan, China, and South Korea on the north, India and Nepal on the west, and Australia and Indonesia in the south.[2]
A billion people are at risk, and nearly a million cases are reported every year.[3] O. tsutsugamushi is an obligate intracellular Gram-negative bacterium; it grows freely in the cytoplasm of infected cells since it lacks vacuolar membrane. It has 5 major serotypes - Boryon, Gilliam, Karp, Kato, and Kawazaki. Scrub typhus is one of the differential diagnosis for fever with thrombocytopenia or hemorrhagic fever.[4] Scrub typhus can manifest with either nonspecific febrile illness or constitutional symptoms (Fever, rash, myalgia, and headache) or with organ dysfunction such as kidney (acute kidney injury [AKI]), lungs (acute respiratory distress syndrome [ARDS]), heart (Myocarditis), liver (hepatitis) and central nervous system (Meningitis).[5]
The mortality of scrub typhus in untreated patients range from 0% to 30% and tends to vary with age and region of infection. The involvement of lungs has been described which range from bronchitis and interstitial pneumonitis to ARDS. ARDS is one of the serious complications of scrub typhus, which has high morbidity and mortality. The occurrence of ARDS is high in scrub typhus patients who were diagnosed late and received antibiotics late.[3,6]
This study may be useful in the early diagnosis of scrub typhus (using clinical features and initial lab values) so that the early initiation of specific antibiotic (Doxycycline) can prevent the occurrence or reduce the severity of ARDS.
Materials and Methods
After informed consent either from patient or patient attender (in case where patient is not able to give consent) and ethical clearance from the institutional ethical committee, a prospective observational study was conducted on 109 patients with febrile illness and thrombocytopenia during a period of 12 months between June 2012 and May 2013 in Acute medical care unit of a super specialty hospital. All 109 patients were tested with both immune-chromatography test (ICT) and Weil-Felix test (WFT). Patients having either ICT/WFT (of 1:80 titer and above) positive have been included and considered as scrub typhus positive whereas negative for both immune-chromatography and WFT were excluded from this observational study. 51 patients were excluded as they were negative for both ICT/WFT and remaining 58 patients were positive for either ICT/WFT.
Clinical features, lab parameters, and final outcome were evaluated in these patients. Area of residence (Andhra Pradesh),[7] detailed clinical examination, presence or absence of eschar, rash and lymphadenopathy were noted. Routine basic labs were sent for all patients. Tropical and other co-endemic diseases such typhoid, Dengue, Leptospirosis and Malaria tests were done in all patients. Additional tests such as ultrasonography of abdomen, Arterial blood gas analysis, chest X-ray, electrocardiogram, two-dimensional echocardiogram, cerebrospinal fluid study, electroencephalography, computed tomography/magnetic resonance imaging brain, blood, and sputum/bronchoalveolar lavage cultures, etc., were sent as indicated. WFT and ICT done for all cases. APACHE-II and sequential organ failure assessment (SOFA) were calculated for all these patients.
Diagnosis of ARDS was based on criteria for ARDS by Berlin definition.[8] (1) Onset within 1-week of a known clinical insult or new or worsening respiratory Symptoms, (2) Bilateral lung opacities - not fully explained by effusions, lobar/lung collapse, or Nodules, (3) Pulmonary edema not fully explained by cardiac failure or fluid overload need objective assessment (echocardiography) to exclude hydrostatic edema if no risk factor present, (4) PaO2 /FiO2 ≤ 300 mm Hg with positive end expiratory pressure or continuous positive airway pressure ≥5 cm H2 O). Doxycycline was administered for all patients with proved scrub typhus. Various complications associated with disease (AKI, hypotension, ARDS, hepatitis, meningitis) were managed accordingly.
Results
Among 58 patients proved to be having positive for scrub typhus, 24 patients had ARDS and 34 patients had no ARDS. The clinical features and lab values have been compared among these groups. Table 1 shows the clinical characteristics of scrub typhus patients. The incidence of AKI, acute hepatitis and delay in starting treatment with doxycycline were significant in ARDS scrub typhus group compared to non ARDS scrub typhus group.
Table 1.
The clinical characteristics of scrub typhus patients with or without ARDS

Table 2 shows PaO2 /FiO2 ratio, Intensive Care Unit (ICU) length of stay, and severity of infection. In our observational study among 24 patients with ARDS (mild ARDS: 8 patients, moderate ARDS: 16 patients, and severe ARDS: 2 patients) the lung injury score, intubation rate, ventilator days, ICU length of stay, APACHE and SOFA score were statistically significant as compared to non ARDS scrub typhus group.
Table 2.
PaO2/FiO2 ratio and LIS with mortality

The clinical features of scrub typhus patients at the time admission have been shown in Table 3. The most common clinical feature in both groups were fever, headache, nausea, vomiting, myalgia, generalized weakness, pain abdomen, chest pain, conjunctival congestion, hepato-splenomegaly, eschar and macula-papular rashes. The clinical feature such as dyspnea, cough, low blood pressure (mean arterial pressure <65 mmHg), and inferior vena cava collapsibility of >50% by ultrasound (hypovolemia) were statistically significant in scrub typhus patients with ARDS.
Table 3.
The clinical features of scrub typhus patients with or without ARDS

Table 4 shows the initial laboratory parameters of scrub typhus patients at the time admission. The laboratory parameters such as decreased hemoglobin, hematocrit, serum albumin, and increased serum creatinine, serum total bilirubin, serum glutamic oxaloacetic transaminase, serum glutamic pyruvic transaminase, lactate dehydrogenase (LDH), creatine phosphokinase (CPK), and serum lactate were statistically significant (P < 0.0001) in scrub typhus patients group with ARDS.
Table 4.
The laboratory parameters (at admission) of scrub typhus patients with or without ARDS

The correlation between WF and ICT of scrub typhus patients at the time admission have been shown in Table 5. In our observational study all patients were positive for scrub typhus by ICT but WF titers were insignificant (<1:80) in 7 of them.
Table 5.
WFT results among patients of immunochromatography proven scrub typhus with or without ARDS

Discussion
Scrub typhus is a mite borne acute infectious disease caused by O. tsutsugamushi. O. tsutsugamushi is an obligate intracellular Gram-negative bacterium. Mites are both the vectors and the reservoirs.[9] Humans are accidental hosts. It affects people of all ages. The mortality of scrub typhus in untreated patients range from 0% to 30% and tends to vary with age and region of infection. Generally seen in people whose occupational or recreational activities bring them into contact with ecotypes favorable with vector chiggers.[10]
Scrub typhus manifest as either nonspecific febrile illness or multi-organ dysfunction such as AKI, ARDS, myocarditis, hepatitis, and meningo-encephalitis. In our prospective observational study conducted over 12 months, 58 patients had scrub typhus. Table 1 shows the clinical characteristics of scrub typhus patients with or without ARDS. The involvement of lungs has been described which range from bronchitis and interstitial pneumonitis to ARDS.[11] Figure 1 shows chest X-ray of scrub patient with severe ARDS. The pathogenesis of ARDS in scrub typhus is not known, thought to be immunological response of the lung to previous O. tsutsugamushi infection without direct invasion of the organism and diffuse alveolar damage without evidence of vasculitis.[12] High incidence of ARDS (24 patients) has been observed in our study. When the patients presented with atypical symptoms, initially they were not diagnosed (delay in diagnosis) as scrub typhus at outside hospital or when the patient came to our hospital it was average 11.333 ± 0.570 days and 5.264 ± 0.431 days from the onset of signs and symptoms in scrub typhus patients with and without ARDS, respectively. Probably delay in treatment might have caused a high incidence of ARDS.
Figure 1.
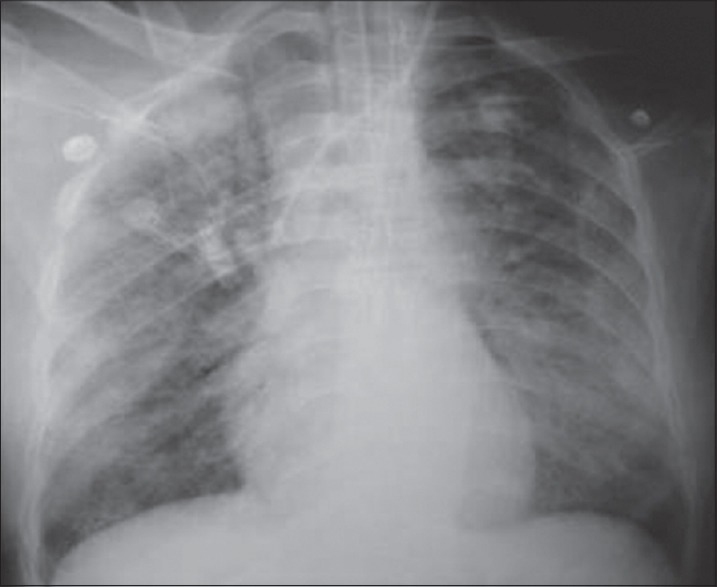
Chest X-ray showing acute respiratory distress syndrome in patient with scrub typhus
Table 2 shows PaO2 /FiO2 ratio, ICU length of stay and mortality. The majority of patients in ARDS group had moderate ARDS, the number of ventilator days and ICU mortality were high which was statistically significant (P < 0.05). Eschar is a vesicular lesion at the site of mite feeding is the first sign of disease and also pathognomonic of scrub typhus often found in the groin, axilla, genitalia, and neck. This is rarely seen in South East Asia and Indian subcontinent.[13,14,15] In our observational study, 6 out of 34 scrub patients without ARDS and 4 out of 24 scrub patients with ARDS had Eschar. Figure 2 shows the Eschar seen near right axilla in one of our patient coming from an endemic area.
Figure 2.

Eschar over anterior chest wall near axilla - on right side
Table 3 shows the clinical features of scrub typhus patients with or without ARDS. Fever, headache, conjunctival congestion, myalgia, generalized weakness, vomiting, and pain abdomen were the common clinical features. In ARDS group, the hypovolemia was more common which was statistically significant (P < 0.05). Table 4 shows the laboratory parameters (at admission) of scrub typhus patients with or without ARDS. Patients in ARDS group had more severe disease in the form of deranged liver parameters, increased serum creatinine, elevated LDH, CPK, and serum lactate.
Serology is the mainstay of diagnosing scrub typhus, immuno-florescence antibody test or indirect immuno-peroxidase assay is the gold standard.[16] Due to high-cost factor and nonavailability of above two tests we have done both ICT and WFT in all 109 patients. Based on either ICT/WFT positivity patients we considered as scrub typhus positive. 51 patients were excluded as they were negative for both ICT/WFT. Remaining 58 patients were positive for interstitial cystitis test whereas 7 patients who are positive for ICT had WF titer <1:80. This shows that the WFT, which is cheap and commonly used in resource limited countries,[17,18,19] has a sensitivity of 30% and specificity of 100% at titer breakpoint of 1:80 in detection of scrub typhus.[20] ICT has a sensitivity of 39.1% and specificity 99.5%.[21] WFT results among patients of immuno-chromatography proven scrub typhus with or without ARDS have been shown in Table 5. The patients in ARDS group had high WF titers (1:320). The higher titers of WF can be correlated with more severe form of the disease according to our observation.[22,23]
Doxycycline has been considered as a drug of choice for treatment of scrub typhus. The optimal duration of therapy is uncertain. Short courses of doxycycline or chloramphenicol are associated with an increased risk of relapse.[24] Treatment of scrub typhus was initiated with doxycycline in 56 patients and combination of doxycycline and azithromycin was used in 2 patients with ARDS and multiple organ dysfunction syndrome (MODS). All the 58 patients were treated for 10 days. Most of the patients responded to doxycycline therapy within 2-3 days except 2 patients who died due to severe MODS (four organ involvement) and they were referred fairly late to our hospital. Azithromycin has shown to have comparable efficacy when compared to doxycycline in a small trial.[25] Rifampicin can be used in combination with azithromycin or doxycycline in cases of poor response to doxycycline alone.[26] All 34 scrub typhus patients without ARDS recovered completely and discharged. Among 24 scrub typhus patients with ARDS, 22 patients recovered, and 2 patients died (Refractory septic sepsis with severe MODS).
Conclusion
Scrub typhus is an important differential diagnosis in patients having fever with thrombocytopenia. Scrub typhus with ARDS has high morbidity and mortality. Early diagnosis using ICT in a patient from the rural background with a history of fever, thrombocytopenia and multiorgan dysfunction and treatment with doxycycline in these patients can help to reduce mortality.
Acknowledgments
We gratefully acknowledge the Physicians, Pulmonologists, Microbiologists, respiratory technicians, nurses and management of the hospital for their valuable support.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
References
- 1.Tamura A, Ohashi N, Urakami H, Miyamura S. Classification of Rickettsia tsutsugamushi in a new genus, Orientia gen. nov. as Orientia tsutsugamushi comb. nov. Int J Syst Bacteriol. 1995;45:589–91. doi: 10.1099/00207713-45-3-589. [DOI] [PubMed] [Google Scholar]
- 2.Chogle AR. Diagnosis and treatment of scrub typhus - The Indian scenario. J Assoc Physicians India. 2010;58:11–2. [PubMed] [Google Scholar]
- 3.Watt G, Parola P. Scrub typhus and tropical rickettsioses. Curr Opin Infect Dis. 2003;16:429–36. doi: 10.1097/00001432-200310000-00009. [DOI] [PubMed] [Google Scholar]
- 4.Kothari VM, Karnad DR, Bichile LS. Tropical infections in the ICU. J Assoc Physicians India. 2006;54:291–8. [PubMed] [Google Scholar]
- 5.Mahajan SK. Scrub typhus. J Assoc Physicians India. 2005;53:954–8. [PubMed] [Google Scholar]
- 6.Wang CC, Liu SF, Liu JW, Chung YH, Su MC, Lin MC. Acute respiratory distress syndrome in scrub typhus. Am J Trop Med Hyg. 2007;76:1148–52. [PubMed] [Google Scholar]
- 7.Subbalaxmi MV, Murali Krishna M, Krishna Prasad A, Teja VD, Swaroopa K, Chandra N, et al. Outbreak of scrub typhus in Andhra Pradesh - Experience at a tertiary care hospital. J Assoc Physicians India. 2014;60:490–6. [PubMed] [Google Scholar]
- 8.ARDS Definition Task Force. Ranieri VM, Rubenfeld GD, Thompson BT, Ferguson ND, Caldwell E, et al. Acute respiratory distress syndrome: The Berlin definition. JAMA. 2012;307:2526–33. doi: 10.1001/jama.2012.5669. [DOI] [PubMed] [Google Scholar]
- 9.Lerdthusnee K, Khuntirat B, Leepitakrat W, Tanskul P, Monkanna T, Khlaimanee N, et al. Scrub typhus: Vector competence of Leptotrombidium chiangraiensis chiggers and transmission efficacy and isolation of Orientia tsutsugamushi. Ann N Y Acad Sci. 2003;990:25–35. doi: 10.1111/j.1749-6632.2003.tb07333.x. [DOI] [PubMed] [Google Scholar]
- 10.Walker JS, Chan CT, Manikumaran C, Elisberg BL. Attempts to infect and demonstrate transovarial transmission of R. tsutsugamushi in three species of Leptotrombidium mites. Ann N Y Acad Sci. 1975;266:80–90. doi: 10.1111/j.1749-6632.1975.tb35090.x. [DOI] [PubMed] [Google Scholar]
- 11.Chayakul P, Panich V, Silpapojakul K. Scrub typhus pneumonitis: An entity which is frequently missed. Q J Med. 1988;68:595–602. [PubMed] [Google Scholar]
- 12.Park JS, Jee YK, Lee KY, Kim KY, Myong NH, Seo PW. Acute respiratory distress syndrome associated with scrub typhus: Diffuse alveolar damage without pulmonary vasculitis. J Korean Med Sci. 2000;15:343–5. doi: 10.3346/jkms.2000.15.3.343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Varghese GM, Abraham OC, Mathai D, Thomas K, Aaron R, Kavitha ML, et al. Scrub typhus among hospitalised patients with febrile illness in South India: Magnitude and clinical predictors. J Infect. 2006;52:56–60. doi: 10.1016/j.jinf.2005.02.001. [DOI] [PubMed] [Google Scholar]
- 14.Vivekanandan M, Mani A, Priya YS, Singh AP, Jayakumar S, Purty S. Outbreak of scrub typhus in Pondicherry. J Assoc Physicians India. 2010;58:24–8. [PubMed] [Google Scholar]
- 15.Sharma A, Mahajan S, Gupta ML, Kanga A, Sharma V. Investigation of an outbreak of scrub typhus in the himalayan region of India. Jpn J Infect Dis. 2005;58:208–10. [PubMed] [Google Scholar]
- 16.Koh GC, Maude RJ, Paris DH, Newton PN, Blacksell SD. Diagnosis of scrub typhus. Am J Trop Med Hyg. 2010;82:368–70. doi: 10.4269/ajtmh.2010.09-0233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Mathai E, Lloyd G, Cherian T, Abraham OC, Cherian AM. Serological evidence for the continued presence of human rickettsioses in southern India. Ann Trop Med Parasitol. 2001;95:395–8. doi: 10.1080/00034980120065804. [DOI] [PubMed] [Google Scholar]
- 18.Kamarasu K, Malathi M, Rajagopal V, Subramani K, Jagadeeshramasamy D, Mathai E. Serological evidence for wide distribution of spotted fevers and typhus fever in Tamil Nadu. Indian J Med Res. 2007;126:128–30. [PubMed] [Google Scholar]
- 19.Mahajan SK, Rolain JM, Sankhyan N, Kaushal RK, Raoult D. Pediatric scrub typhus in Indian Himalayas. Indian J Pediatr. 2008;75:947–9. doi: 10.1007/s12098-008-0198-z. [DOI] [PubMed] [Google Scholar]
- 20.Mahajan SK, Kaushik M, Raina R. Relevance of Weil-Felix test in diagnosis of scrub typhus in India. J Asssoc Physicians India. 2006;54:619–21. [PubMed] [Google Scholar]
- 21.Blacksell SD, Jenjaroen K, Phetsouvanh R, Tanganuchitcharnchai A, Phouminh P, Phongmany S, et al. Accuracy of rapid IgM-based immunochromatographic and immunoblot assays for diagnosis of acute scrub typhus and murine typhus infections in Laos. Am J Trop Med Hyg. 2010;83:365–9. doi: 10.4269/ajtmh.2010.09-0534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Sonthayanon P, Chierakul W, Wuthiekanun V, Phimda K, Pukrittayakamee S, Day NP, et al. Association of high Orientia tsutsugamushi DNA loads with disease of greater severity in adults with scrub typhus. J Clin Microbiol. 2009;47:430–4. doi: 10.1128/JCM.01927-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kim DM, Kang DW, Kim JO, Chung JH, Kim HL, Park CY, et al. Acute renal failure due to acute tubular necrosis caused by direct invasion of Orientia tsutsugamushi. J Clin Microbiol. 2008;46:1548–50. doi: 10.1128/JCM.01040-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Sheehy TW, Hazlett D, Turk RE. Scrub typhus. A comparison of chloramphenicol and tetracycline in its treatment. Arch Intern Med. 1973;132:77–80. doi: 10.1001/archinte.132.1.77. [DOI] [PubMed] [Google Scholar]
- 25.Phimda K, Hoontrakul S, Suttinont C, Chareonwat S, Losuwanaluk K, Chueasuwanchai S, et al. Doxycycline versus azithromycin for treatment of leptospirosis and scrub typhus. Antimicrob Agents Chemother. 2007;51:3259–63. doi: 10.1128/AAC.00508-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Watt G, Chouriyagune C, Ruangweerayud R, Watcharapichat P, Phulsuksombati D, Jongsakul K, et al. Scrub typhus infections poorly responsive to antibiotics in northern Thailand. Lancet. 1996;348:86–9. doi: 10.1016/s0140-6736(96)02501-9. [DOI] [PubMed] [Google Scholar]


