Abstract
Background
Suicide is a public health concern, but little is known about the patterns of healthcare visits made before a suicide attempt, and whether those patterns differ by race/ethnicity.
Objectives
To examine racial/ethnic variation in the types of healthcare visits made before a suicide attempt, when those visits occur, and whether mental health or substance use diagnoses were documented.
Research Design
Retrospective, longitudinal study, 2009–2011.
Participants
22,387 individuals who attempted suicide and were enrolled in the health plan across 10 health systems in the Mental Health Research Network.
Measures
Cumulative percentage of different types of healthcare visits made in the 52-weeks before a suicide attempt, by self-reported racial/ethnicity and diagnosis. Data were from the Virtual Data Warehouse at each site.
Results
Over 38% of individuals made any healthcare visit within the week before their suicide attempt and ~95% within the preceding year; these percentages varied across racial/ethnic groups (p<0.001). White individuals had the highest percentage of visits (>41%) within 1-week of suicide attempt. Asian Americans were the least likely to make visits within 52 weeks. Hawaiian/Pacific Islanders had proportionally the most inpatient and emergency visits before an attempt, but were least likely to have a recorded mental health or substance use diagnosis. Overall, visits were most common in primary care and outpatient general medical settings.
Conclusions
This study provides temporal evidence of racial/ethnic differences in healthcare visits made prior to suicide attempt. Healthcare systems can use this information to help focus the design and implementation of their suicide prevention initiatives.
Keywords: Suicide, Suicide Attempt, Health Services, Healthcare, Race/ethnicity
INTRODUCTION
In the United States (US), more than one million people attempt suicide each year.(1) The adult rate of completed suicides has increased by 30% over the last decade.(2–4) As such, suicide was recently prioritized through the publication of a National Strategy for Suicide Prevention.(5)
The report concludes that one of the best places to prevent suicide is within healthcare. Research on where and when to target interventions was identified as a primary objective of the prioritized research agenda.(6, 7) Evidence suggests that over 80% of individuals make healthcare contacts before suicide.(8) Although rates of suicidal behavior vary across racial/ethnic groups,(9–12) there are limited data on when and where different groups use services prior to a suicide attempt. Population based surveys have shown that non-White groups are less likely to receive specialty mental health care in the same year as their attempt.(13–15) However, these studies do not provide temporal data on the types and timing of care received prior to an attempt. New information is essential as healthcare systems determine how to focus suicide prevention activities.
This study uses data on US healthcare users to examine racial/ethnic differences in the types and timing of healthcare visits made prior to suicide attempt. This study assesses whether racial/ethnic variation exists in 1) receipt of various types of services, 2) the timing of visits in relation to a suicide attempt, and 3) the documentation of mental health or substance use diagnoses during visits.
METHODS
This nationwide study was conducted across 10 large healthcare systems – all Mental Health Research Network (MHRN) members.(8, 16–19) These systems include varying organizational structures, including health maintenance organizations, mixed-model systems, and internal medical groups serving patients with different insurance plans. All MHRN sites are part of the HMO Research Network (HMORN).(20)
Participating sites (by US state) include: Group Health Cooperative (Washington), Harvard Pilgrim Health Care (Massachusetts, New Hampshire, Maine), HealthPartners (Minnesota, Wisconsin), Henry Ford Health System (Michigan), and Scott & White Healthcare (Texas) as well as five Kaiser Permanente systems (Colorado, Georgia, Hawaii, Northern California, and Oregon/Northwest). These sites provide services for approximately 8 million members per year. Population characteristics of these systems are available online (http://www.hmoresearchnetwork.org/en/). The institutional review boards at each site approved this study.
Data were extracted from the HMORN Virtual Data Warehouse (VDW).(20–22) The VDW is a federated data structure consisting of electronic medical record and insurance claims data organized using the same variables and definitions at each site. VDW programs were developed and tested at one site and then distributed to all participating sites. Aggregated data from each site were quality checked locally and then returned to the initiating site.
VARIABLES
Data were captured on suicide attempts occurring between January 1, 2009 and December 31, 2011 using a three-method algorithm derived from International Classification of Diseases, 9th revision (ICD-9) codes.(23) The methods were: 1) codes E950-E959, 2) code V62.84 accompanied by same day code 870–899 or 960–989, and 3) code 881, 960–989, or 994.7 accompanied by same day code 290.8–290.9, 293.83, 295–299, 300.4, 301, 301.13, 301.20–301.22, 309.0–309.9, 311, or 780.1. While method 1 is most often used, previous research has shown that e-codes are commonly missing from healthcare databases.(16, 24) Thus, methods 2 and 3 were also applied and have been validated previously.(24, 25) As individuals could have multiple attempts, each attempt was considered a separate event in the analyses.
Data on healthcare visits in the year before a suicide attempt were extracted. ICD-9 codes were used to identify visits by diagnosis, including mental health (293–302.9 or 306.0–316), substance use (291–292.9 or 303.0–305.9), and ‘other.’ All visits were categorized into subtypes (outpatient specialty, inpatient, primary care, and emergency). For suicide attempts occurring during 2009, data were captured for the preceding 12-months dating back into 2008.
Approximately 78% (n=17,428) of all those with a suicide attempt had a self-reported race/ethnicity recorded at a healthcare encounter. Racial/ethnic categories included Alaskan Native/Native American, Asian, Black, Hispanic, Hawaiian/Pacific Islander, and White. Patients who self-reported as Hispanic were categorized as such regardless of race. Individuals without a race/ethnicity (n=4,927) and those with more than one race/ethnicity (n=32) were excluded.
DATA ANALYSIS
This study used a retrospective longitudinal design. The frequency of suicide attempts was stratified by race/ethnicity. All health plan members enrolled during the year prior to attempt were included. Descriptive analyses examined the cumulative percentage of individuals making 1) any visit and 2) any visit with a mental health diagnosis within 1, 4, and 52 weeks prior to the attempt. Chi-square tests were used for racial/ethnic group comparisons. Visits were stratified by subtype, diagnosis, and racial/ethnic group. Stratified cumulative utilization curves examined the proportion of individuals who made visits within weekly increments prior to attempt.
RESULTS
There were 22,387 suicide attempts captured. The majority of individuals in this study were White (n=12,119; 54.1%), compared to an estimated 62% nationally.(1) Approximately 65% were female, 30% less than 20 years old, 33% between ages 20–39, 30% between ages 40–64, and 6% age 65 or older. Over 38% made any visit within the week before their attempt, nearly 64% within 4-weeks, and almost 95% within one year. One-quarter made a visit with a mental health diagnosis within one week, 43.9% within 4-weeks, and 73.3% within 52-weeks of their attempt.
As shown in Table 1, the percentage who made any visit or any visit with a mental health diagnosis varied by race/ethnicity (p<0.001). Over 41% of White individuals made any visit within one week compared to less than 35% for other groups. Nearly 27% of White individuals made a mental health visit versus less than 20% of Asian, Hawaiian/Pacific Islander, and Black individuals in this period. Within 4 weeks, all visits and mental health visits remained most common for White individuals (67.3% and 47.4%, respectively) and least common among Asian individuals (52.8% and 31.9%, respectively). Within 52-weeks, more than 90% made any visit. Alaskan Native/Native American (81.5%) and White individuals (79.5%) made mental health visits 10–25% more often than other groups.
Table 1.
Cumulative percentage of individuals who made healthcare visits prior to suicide attempt.
| 1-Week | All (N=22,387) |
Am. Ind. / Al. Nat. (N=200) |
Asian (N=1,015) |
Black (N=1,543) |
Hispanic (N=2,322) |
Hawaii / Pac. Is. (N=229) |
White (N=12,119) |
Chi- Square |
p-value |
|---|---|---|---|---|---|---|---|---|---|
| N, enrolled | 21977 | 196 | 997 | 1474 | 2272 | 224 | 11900 | ||
| Any Visit | 38.3% | 34.0% | 31.9% | 33.7% | 35.2% | 29.7% | 41.1% | 83.8 | <0.001 |
| Any MH Visit | 24.6% | 23.0% | 19.2% | 19.3% | 21.9% | 13.5% | 26.7% | 89.2 | <0.001 |
| 4-Weeks | |||||||||
| N, enrolled | 21773 | 197 | 989 | 1468 | 2256 | 222 | 11820 | ||
| Any Visit | 63.7% | 65.0% | 52.8% | 59.9% | 58.6% | 54.1% | 67.3% | 157.4 | <0.001 |
| Any MH Visit | 43.9% | 46.0% | 31.9% | 37.0% | 38.8% | 33.6% | 47.4% | 178.0 | <0.001 |
| 52-Weeks | |||||||||
| N, enrolled | 18367 | 158 | 866 | 1301 | 1995 | 194 | 10294 | ||
| Any Visit | 94.6% | 95.0% | 91.9% | 94.0% | 94.3% | 94.8% | 96.5% | 63.7 | <0.001 |
| Any MH Visit | 73.3% | 81.5% | 54.7% | 64.2% | 66.4% | 59.8% | 79.5% | 484.6 | <0.001 |
Al. Nat. denotes Alaska Native; Nat. Am., Native American; Pac. Is., Pacific Islander; Any MH Visit, any visit with a mental health diagnosis
Numbers in parentheses equal the total number of individuals with a suicide attempt in each category
Cumulative percentages were calculated by dividing the total number of individuals who made a visit at any time during the specified period prior to suicide attempt within each category by the total number of individuals in that category who attempted suicide.
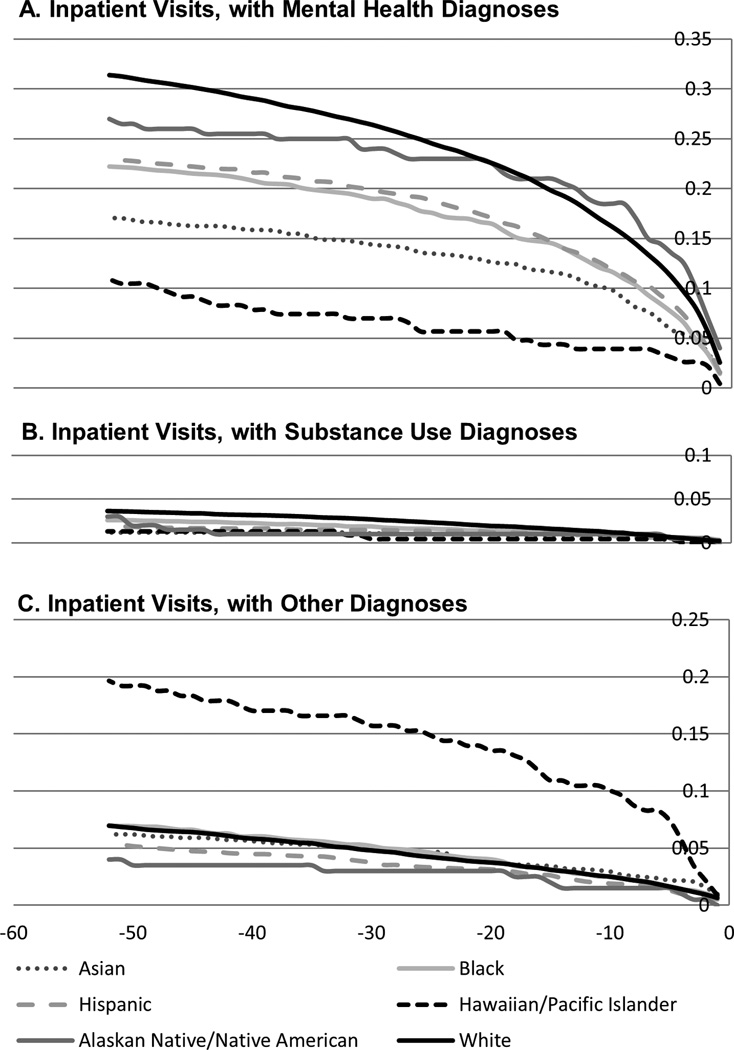
Over 31% of White individuals and 27% of Alaskan Native/Native Americans had an inpatient stay with a mental health diagnosis within 52 weeks of a suicide attempt, compared to less than 11% of Hawaiian/Pacific Islanders (Figure 1). In contrast, Hawaiian/Pacific Islanders were most likely to have an inpatient stay without a mental health or substance use diagnosis (19.7%).
Figure 1. Cumulative proportion of individuals who had inpatient hospital stays prior to suicide attempt.
Aggregated data on inpatient hospital stays across 10 Mental Health Research Network affiliated health systems serving 13 US states are presented in 52 weekly increments prior to each suicide attempt. Data are from individuals who attempted suicide from 2009 thru 2011 and are stratified by racial/ethnicity and diagnosis recorded at the visit (mental health, substance use, other).
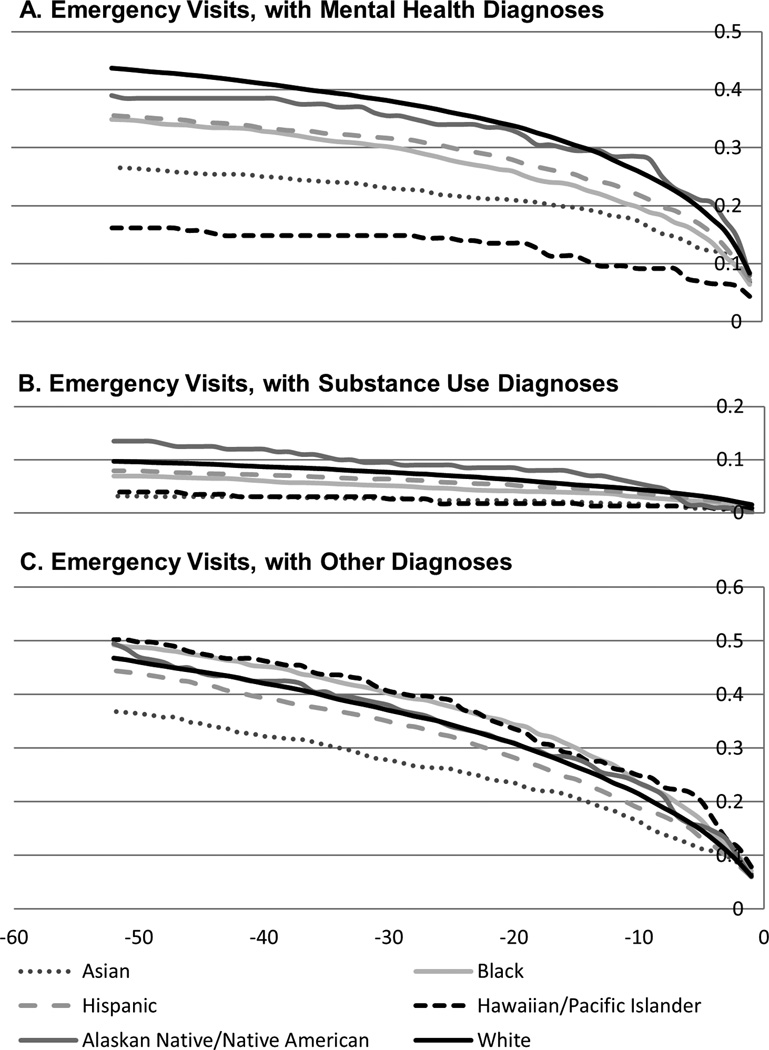
Emergency department visits with mental health and substance use diagnoses were most common among Alaskan Native/Native American (39.0% and 13.9%, respectively) and White (43.7% and 9.7%, respectively) individuals (Figure 2). The proportion of Asian individuals with the same visits was much lower (26.6% and 3.1%, respectively). Emergency visits by Asian individuals without psychiatric diagnoses (36.8%) were also least common.
Figure 2. Cumulative proportion of individuals who made emergency department visits prior to suicide attempt.
Aggregated data on emergency department visits across 10 Mental Health Research Network affiliated health systems serving 13 US states are presented in 52 weekly increments prior to each suicide attempt. Data are from individuals who attempted suicide from 2009 thru 2011 and are stratified by racial/ethnicity and diagnosis recorded at the visit (mental health, substance use, other).
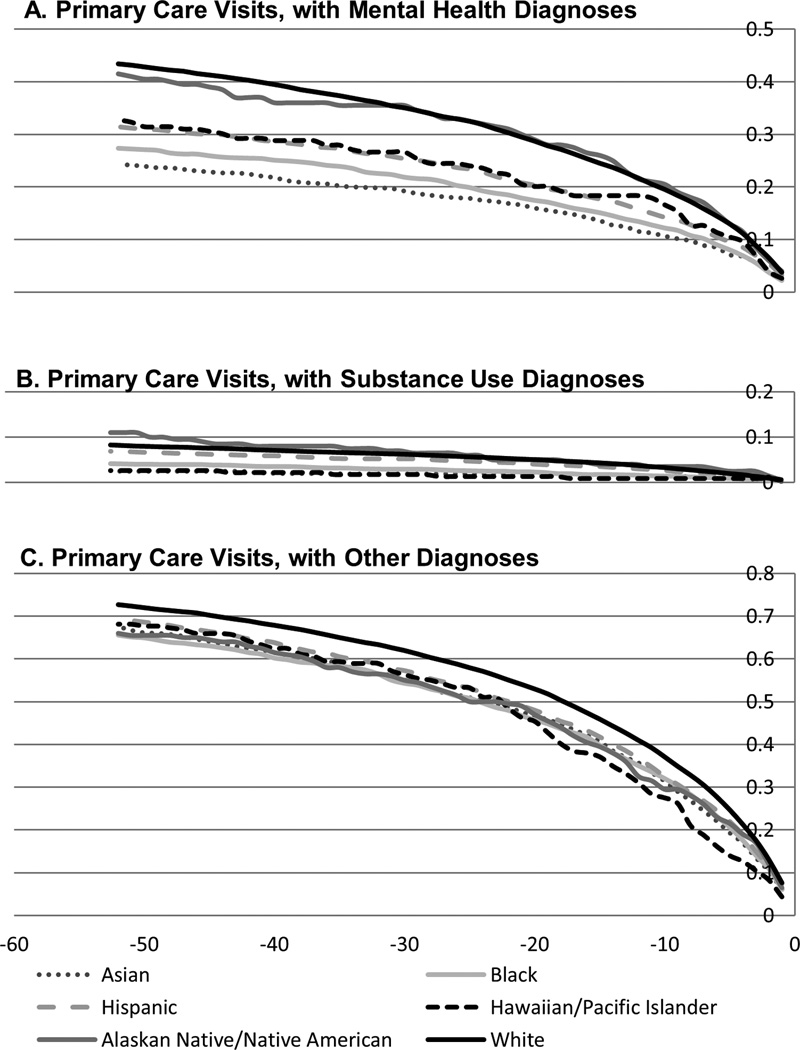
Primary care visits with mental health and other diagnoses were most common among White individuals (43.4% and 72.7%, respectively; Figure 3). Visits with substance use diagnoses were most common among Alaskan Native/Native Americans (11%). The proportion of individuals who made primary care visits with substance use and mental health diagnoses was lowest among Hawaiian/Pacific Islanders (2.6%) and Asian individuals (24.3%), respectively.
Figure 3. Cumulative proportion of individuals who made primary care visits prior to suicide attempt.
Aggregated data on primary care visits across 10 Mental Health Research Network affiliated health systems serving 13 US states are presented in 52 weekly increments prior to each suicide attempt. Data are from individuals who attempted suicide from 2009 thru 2011 and are stratified by racial/ethnicity and diagnosis recorded at the visit (mental health, substance use, other).
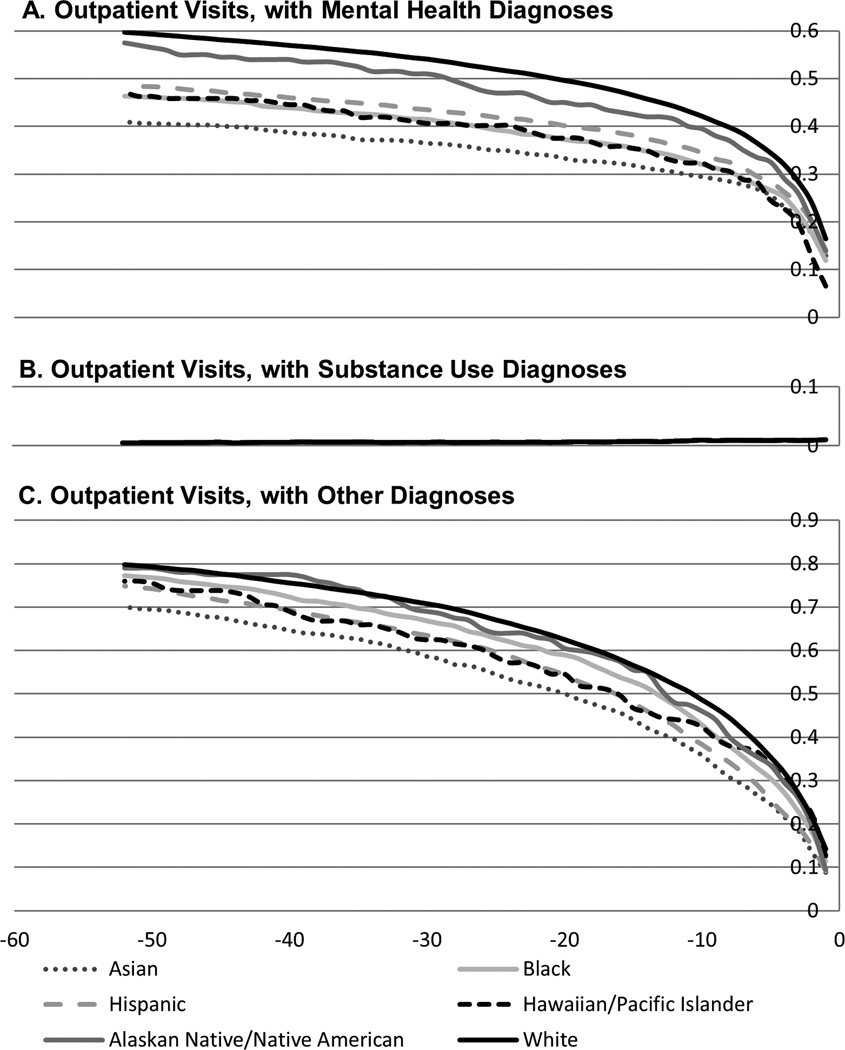
The proportion of individuals who made an outpatient mental health specialty visit ranged from nearly 60% of White individuals to 40% for Asian individuals (Figure 4). Asian individuals also made the lowest percentage of outpatient specialty visits without a mental health or substance use diagnosis (70%).
Figure 4. Cumulative proportion of individuals who made outpatient specialty visits prior to suicide attempt.
Aggregated data on outpatient specialty visits across 10 Mental Health Research Network affiliated health systems serving 13 US states are presented in 52 weekly increments prior to each suicide attempt. Data are from individuals who attempted suicide from 2009 thru 2011 and are stratified by racial/ethnicity and diagnosis recorded at the visit (mental health, substance use, other).
DISCUSSION
This is the largest US study providing temporal evidence of racial/ethnic differences in the types and timing of healthcare encounters made before a suicide attempt. Most individuals made a visit in the year prior to an attempt. These estimates are slightly higher than those from population surveys of healthcare use in the same year as an attempt.(15) This is likely because individuals in this study had insurance, and same-year visits measured on surveys could occur after an attempt.
Even though >90% of individuals made visits within 52 weeks of a suicide attempt, White individuals tended to make visits closer to the date of their attempt. This finding supports evidence that White individuals are more likely to access and engage in healthcare throughout the year.(26, 27) There may be a great opportunity to prevent suicide right before it happens within this population, especially since White individuals have high suicide rates.(3) While there is still an opportunity to intervene with individuals of other race/ethnicities during healthcare visits, the lower proportion of visits suggests that it is important to also find other opportunities for prevention.
Variation in access to health insurance has been hypothesized as one reason for racial/ethnic disparities in access to care.(28) However, since all individuals in this study had insurance, it suggests that other factors played a role. Studies have identified poor doctor-patient communication as an important factor in racial/ethnic disparities in healthcare use, but racial bias, patient preference, perceived discrimination, and cultural variation in stigma about mental illness may also be influential.(29–32) Improving these factors and outreach efforts may improve healthcare use among racial/ethnic minorities.
The most common types of visits occurred in outpatient specialty and primary care settings without mental health diagnoses. This is consistent with prior findings and is not surprising given that most individuals ordinarily use these services.(8) However, most suicide prevention efforts have been focused in emergency and behavioral health settings, and recent guidelines from the US Preventive Services Task Force do not recommend suicide screening in primary care.(33–35) This study supports the promotion of suicide prevention within general outpatient settings, where most people visit before suicide attempt.
Asian individuals were among the least likely to make various types of healthcare visits before suicide attempt. English language proficiency, provider stereotyping, and perceived discrimination are major barriers to healthcare use among Asian Americans.(36–38) These factors are important to consider when designing suicide interventions.
Mental health and substance use diagnoses were less common than ‘other’ diagnoses. White and Alaskan Native/Native American individuals were most likely to have mental health and substance use diagnoses. This is consistent with other research demonstrating high rates of suicide, mental health conditions, and substance use among these populations.(3, 39, 40) Hawaiian/Pacific Islanders made proportionally the fewest inpatient and emergency visits with a mental health diagnosis, but were the most likely to make those types of visits with ‘other’ diagnoses. This underscores possible cultural variation in the way this group deals with mental illness.
Overall, there are two factors that may explain these findings. First, mental health may be differentially underdiagnosed among minorities. This issue is most apparent among Hawaiian/Pacific Islanders. Suicide prevention should include improved culturally competent mental illness detection and treatment tailored to this group. Second, there may be other important unknown factors associated with suicide. This issue is a major objective for future research.(6) Future research may also investigate racial/ethnic variation in patterns of medications, procedures, and numbers of visits made before suicide attempt.
LIMITATIONS
There are potential limitations. First, it is likely that not all suicide attempts were captured, since some individuals do not receive healthcare after attempts. Second, mental health may have been assessed during visits, but a diagnosis was not recorded. Third, as all participants had insurance, these findings may not represent those who are uninsured. Fourth, the inpatient data did not delineate between psychiatric and general hospital stays, as focus was placed on whether a provider recorded a mental health diagnosis. Future research may differentiate between inpatient visits. Fifth, the data for this study included aggregated counts from sites; thus stratified and adjusted person-level analyses were not conducted. Future research may consider additional investigation along these lines. Finally, data were not presented on socioeconomic status, age, and sex. Preliminary analysis showed little variation in healthcare use by income (data not shown). It is unlikely that socioeconomic differences alone accounted for the observed differences.
CONCLUSIONS
This study provides evidence of racial/ethnic differences in the types and timing of healthcare visits made prior to suicide attempt. These data underscore the need for more efficient and effective tools for identifying patients at risk in routine outpatient care. Our findings also highlight the importance of considering sociocultural differences when attempting to assess risk and prevent suicide.
ACKNOWLEDGEMENT
This project was supported by Award Number U19MH092201 from the National Institute of Mental Health. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institute of Mental Health or the National Institutes of Health. Drs. Ahmedani and Stewart had full access to all of the data and take responsibility for the integrity of the data and accuracy of the data analysis. All authors have contributed to and have approved the final submitted manuscript. The authors would like to thank all members of the HMO and Mental Health Research Networks, whose contributions to building the Virtual Data Warehouse and to the integrity of the data have made this study possible.
Footnotes
CONFLICT OF INTEREST
The authors report no conflicts of interest for this project.
Contributor Information
Brian K. Ahmedani, Email: bahmeda1@hfhs.org.
Christine Stewart, Email: stewart.c@ghc.org.
Gregory E. Simon, Email: simon.g@ghc.org.
Frances Lynch, Email: Frances.Lynch@kpchr.org.
Christine Y. Lu, Email: christine_lu@harvardpilgrim.org.
Beth E. Waitzfelder, Email: Beth.E.Waitzfelder@nsmtp.kp.org.
Leif I. Solberg, Email: Leif.I.Solberg@HealthPartners.Com.
Ashli A. Owen-Smith, Email: Ashli.A.Owen-Smith@kp.org.
Arne Beck, Email: Arne.Beck@kp.org.
Laurel A. Copeland, Email: lcopeland@sw.org.
Enid M. Hunkeler, Email: Enid.Hunkeler@kp.org.
Rebecca C. Rossom, Email: rebecca.c.rossom@healthpartners.com.
L. Keoki Williams, Email: KWILLIA5@hfhs.org.
REFERENCES
- 1.Crosby AE, Han B, Ortega LA, et al. Suicidal thoughts and behaviors among adults aged >/=18 years--United States, 2008–2009. MMWR Surveill Summ. 2011;60:1–22. [PubMed] [Google Scholar]
- 2.Heron M. Deaths: leading causes for 2010. National vital statistics reports : from the Centers for Disease Control and Prevention, National Center for Health Statistics, National Vital Statistics System. 2013;62:1–96. [PubMed] [Google Scholar]
- 3.Crosby AE, Ortega L, Stevens MR. Suicides - United States, 1999–2007. MMWR Surveill Summ. 2011;60(Suppl):56–59. [PubMed] [Google Scholar]
- 4.Holinger PC, Klemen EH. Violent deaths in the United States, 1900–1975. Relationships between suicide, homicide and accidental deaths. Soc Sci Med. 1982;16:1929–1938. doi: 10.1016/0277-9536(82)90392-6. [DOI] [PubMed] [Google Scholar]
- 5.US Department of Health and Human Services; Office of the Surgeon General and National Action Alliance for Suicide Prevention. National Strategy for Suicide Prevention: Goals and Objectives for Action. Washington, D.C.: 2012. [PubMed] [Google Scholar]
- 6.National Action Alliance for Suicide Prevention, Research Prioritization Task Force. A Prioritized Research Agenda for Suicide Prevention: An Action Plan to Save Lives. Rockville, MD: 2014. [Google Scholar]
- 7.Ahmedani BK, Vannoy S. National pathways for suicide prevention and health services research. Am J Prev Med. 2014;47:S222–S228. doi: 10.1016/j.amepre.2014.05.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ahmedani BK, Simon GE, Stewart C, et al. Health care contacts in the year before suicide death. J Gen Intern Med. 2014;29:870–877. doi: 10.1007/s11606-014-2767-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Joe S, Baser RE, Breeden G, et al. Prevalence of and risk factors for lifetime suicide attempts among blacks in the United States. JAMA. 2006;296:2112–2123. doi: 10.1001/jama.296.17.2112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lorenzo-Luaces L, Phillips JA. Racial and ethnic differences in risk factors associated with suicidal behavior among young adults in the USA. Ethn Health. 2014;19:458–477. doi: 10.1080/13557858.2013.846299. [DOI] [PubMed] [Google Scholar]
- 11.Baca-Garcia E, Perez-Rodriguez MM, Keyes KM, et al. Suicidal ideation and suicide attempts among Hispanic subgroups in the United States: 1991–1992 and 2001–2002. J Psychiatr Res. 2011;45:512–518. doi: 10.1016/j.jpsychires.2010.09.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Baca-Garcia E, Perez-Rodriguez MM, Keyes KM, et al. Suicidal ideation and suicide attempts in the United States: 1991–1992 and 2001–2002. Mol Psychiatry. 2010;15:250–259. doi: 10.1038/mp.2008.98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Freedenthal S. Racial disparities in mental health service use by adolescents who thought about or attempted suicide. Suicide Life Threat Behav. 2007;37:22–34. doi: 10.1521/suli.2007.37.1.22. [DOI] [PubMed] [Google Scholar]
- 14.Ahmedani BK, Perron BE, Ilgen MA, et al. Suicide thoughts and attempts and psychiatric treatment utilization: Informing prevention strategies. Psychiatr Serv. 2012;63:186–189. doi: 10.1176/appi.ps.201100159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Nock MK, Green JG, Hwang I, et al. Prevalence, correlates, and treatment of lifetime suicidal behavior among adolescents: results from the National Comorbidity Survey Replication Adolescent Supplement. JAMA Psychiatry. 2013;70:300–310. doi: 10.1001/2013.jamapsychiatry.55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lu CY, Stewart C, Ahmed AT, et al. How complete are E-codes in commercial plan claims databases? Pharmacoepidemiol Drug Saf. 2014;23:218–220. doi: 10.1002/pds.3551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Penfold RB, Stewart C, Hunkeler EM, et al. Use of antipsychotic medications in pediatric populations: what do the data say? Curr Psychiatry Rep. 2013;15:426. doi: 10.1007/s11920-013-0426-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Simon GE, Stewart C, Beck A, et al. National Prevalence of Receipt of Antidepressant Prescriptions by Persons Without a Psychiatric Diagnosis. Psychiatr Serv. 2014;65:944–946. doi: 10.1176/appi.ps.201300371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lu CY, Zhang F, Lakoma MD, et al. Changes in antidepressant use by young people and suicidal behavior after FDA warnings and media coverage: quasi-experimental study. BMJ. 2014;348:g3596. doi: 10.1136/bmj.g3596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ross TR, Ng D, Brown JS, et al. The HMO Research Network Virtual Data Warehouse: A Public Data Model to Support Collaboration. eGEMS. 2014;2:2. doi: 10.13063/2327-9214.1049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hornbrook MC, Hart G, Ellis JL, et al. Building a virtual cancer research organization. J Natl Cancer Inst Monogr. 2005:12–25. doi: 10.1093/jncimonographs/lgi033. [DOI] [PubMed] [Google Scholar]
- 22.Go AS, Magid DJ, Wells B, et al. The Cardiovascular Research Network: a new paradigm for cardiovascular quality and outcomes research. Circ Cardiovasc Qual Outcomes. 2008;1:138–147. doi: 10.1161/CIRCOUTCOMES.108.801654. [DOI] [PubMed] [Google Scholar]
- 23.International Classification of Diseases, Ninth Revision, Clinical Modification. Atlanta, GA: CDC; 2010. National Center for Health Statistics, Centers for Disease Control and Prevention. [Google Scholar]
- 24.Patrick AR, Miller M, Barber CW, et al. Identification of hospitalizations for intentional self-harm when E-codes are incompletely recorded. Pharmacoepidemiol Drug Saf. 2010;19:1263–1275. doi: 10.1002/pds.2037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Simon GE, Rutter CM, Peterson D, et al. Does response on the PHQ-9 Depression Questionnaire predict subsequent suicide attempt or suicide death? Psychiatr Serv. 2013;64:1195–1202. doi: 10.1176/appi.ps.201200587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Waidmann TA, Rajan S. Race and ethnic disparities in health care access and utilization: an examination of state variation. Med Care Res Rev. 2000;57(Suppl 1):55–84. doi: 10.1177/1077558700057001S04. [DOI] [PubMed] [Google Scholar]
- 27.Smedley BD, Stith AY, Nelson AR. Unequal Treatment: Confronting Racial and Ethnic Disparities in Health Care. Washington (DC): National Academies Press; 2003. [PubMed] [Google Scholar]
- 28.Lillie-Blanton M, Hoffman C. The role of health insurance coverage in reducing racial/ethnic disparities in health care. Health Aff (Millwood) 2005;24:398–408. doi: 10.1377/hlthaff.24.2.398. [DOI] [PubMed] [Google Scholar]
- 29.Ashton CM, Haidet P, Paterniti DA, et al. Racial and ethnic disparities in the use of health services: bias, preferences, or poor communication? J Gen Intern Med. 2003;18:146–152. doi: 10.1046/j.1525-1497.2003.20532.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Hausmann LR, Jeong K, Bost JE, et al. Perceived discrimination in health care and health status in a racially diverse sample. Med Care. 2008;46:905–914. doi: 10.1097/MLR.0b013e3181792562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Benjamins MR. Race/ethnic discrimination and preventive service utilization in a sample of whites, blacks, Mexicans, and Puerto Ricans. Med Care. 2012;50:870–876. doi: 10.1097/MLR.0b013e31825a8c63. [DOI] [PubMed] [Google Scholar]
- 32.Byrne MM, O'Malley KJ, Suarez-Almazor ME. Ethnic differences in health preferences: analysis using willingness-to-pay. J Rheumatol. 2004;31:1811–1818. [PubMed] [Google Scholar]
- 33.Boudreaux ED, Miller I, Goldstein AB, et al. The Emergency Department Safety Assessment and Follow-up Evaluation (ED-SAFE): method and design considerations. Contemp Clin Trials. 2013;36:14–24. doi: 10.1016/j.cct.2013.05.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Mann JJ, Apter A, Bertolote J, et al. Suicide prevention strategies: a systematic review. JAMA. 2005;294:2064–2074. doi: 10.1001/jama.294.16.2064. [DOI] [PubMed] [Google Scholar]
- 35.O'Connor E, Gaynes BN, Burda BU, et al. Screening for and Treatment of Suicide Risk Relevant to Primary Care: A Systematic Review for the U.S. Preventive Services Task Force. Ann Intern Med. 2013;158(10):741–754. doi: 10.7326/0003-4819-158-10-201305210-00642. [DOI] [PubMed] [Google Scholar]
- 36.Spencer MS, Chen J, Gee GC, et al. Discrimination and mental health-related service use in a national study of Asian Americans. Am J Public Health. 2010;100:2410–2417. doi: 10.2105/AJPH.2009.176321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Ye J, Mack D, Fry-Johnson Y, et al. Health care access and utilization among US-born and foreign-born Asian Americans. J Immigr Minor Health. 2012;14:731–737. doi: 10.1007/s10903-011-9543-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Juckett G, Nguyen C, Shahbodaghi SD. Caring for Asian immigrants: tips on culture that can enhance patient care. J Fam Pract. 2014;63:E1–E9. [PubMed] [Google Scholar]
- 39.Duran B, Sanders M, Skipper B, et al. Prevalence and correlates of mental disorders among Native American women in primary care. Am J Public Health. 2004;94:71–77. doi: 10.2105/ajph.94.1.71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Beals J, Novins DK, Whitesell NR, et al. Prevalence of mental disorders and utilization of mental health services in two American Indian reservation populations: mental health disparities in a national context. Am J Psychiatry. 2005;162:1723–1732. doi: 10.1176/appi.ajp.162.9.1723. [DOI] [PubMed] [Google Scholar]