Abstract
Background
Recent advances in external fixation technique and pin design have sought to minimize complications such as pin site infection and premature removal of the external fixator. Although newer forms of internal fixation have gained popularity, external fixation may still have a role in managing pediatric femoral shaft fractures.
Questions/purposes
We sought to assess the time to healing, limb alignment, and complications observed in a cohort of pediatric patients with closed femoral shaft fractures who were treated with external fixation.
Methods
Over a 15-year period, one surgeon treated 289 pediatric patients with femur fractures, 31 (11%) of whom received an external fixator. The general indications for use of an external fixator during the period in question included length-unstable fractures, metadiaphyseal location, refracture, and pathologic fracture. Six patients (19%) had inadequate followup data and four patients (13%) were treated with a combination of flexible intramedullary nails and external fixation, leaving 21 patients for analysis. Mean age at injury was 10 years (range, 6–15 years) and followup averaged 22 months (range, 5–45 months) after removal of the fixator. Radiographs were examined for alignment and limb length discrepancy. Complications were recorded from a chart review.
Results
Mean time in the fixator was 17 weeks (range, 9–24 weeks). One patient sustained a refracture and one patient with an isolated femur fracture had a leg length discrepancy > 2 cm. There were no pin site infections requiring intravenous antibiotics or additional surgery. One patient with Blount disease and previous tibial osteotomy developed transient peroneal nerve palsy.
Conclusions
Despite improvements in pin design and predictable fracture healing, complications such as refracture and leg length discrepancy after external fixation of pediatric femoral shaft fractures can occur. However, external fixation remains a viable alternative for certain fractures such as length-unstable fractures, metadiaphyseal location, pathologic fractures, and refractures.
Level of Evidence
Level IV, therapeutic study. See Guidelines for Authors for a complete description of levels of evidence.
Introduction
Femoral shaft fractures account for approximately 2% of all pediatric fractures with an annual incidence of 16 to 19 per 100,000 [11, 13]. There is a bimodal distribution with peaks at age 2 to 3 years and during adolescence. Treatment is typically based on the patient’s age and the fracture pattern with treatment options including spica casting, flexible and rigid intramedullary nailing, submuscular plating, and external fixation [2, 16]. Over time, operative treatment of pediatric femoral shaft fractures has gained popularity over nonoperative treatment because it shortens hospitalizations and allows earlier mobilization [27].
External fixation was one of the earliest forms of operative treatment for such fractures. Although it has traditionally been used for indications such as open fractures, concomitant soft tissue injuries, and unstable or polytrauma patients, some authors also advocated external fixation for managing isolated closed pediatric femoral fractures [1, 3, 4, 14, 26]. With the advent of other forms of fixation, the use of external fixation has become less popular [11]. The recent American Academy of Orthopaedic Surgeons clinical practice guideline for treating pediatric diaphyseal femur fractures does not even mention external fixation as a treatment option [15].
Compared with various internal fixation devices, the potential advantages of external fixation include minimal invasiveness, lower blood loss, and shorter operating time [2]. The disadvantages typically cited for external fixation include concerns for refracture, pin site infection, and malunion [4, 14, 18]. However, these complications have variable incidence and functional implications in the literature [4, 9, 14, 18, 24].
Although newer methods of internal fixation have grown in popularity, we believe that external fixation may still have a role in the management of certain pediatric femoral shaft fractures. We therefore sought to assess time to healing, limb alignment, and complications in a cohort of pediatric patients with closed femoral shaft fractures who were treated with contemporary external fixation techniques.
Materials and Methods
Institutional review board approval was obtained for this retrospective case series. The surgical database of a single pediatric orthopaedic surgeon (SS) at a Level I trauma center was searched. All patients between the ages of 6 months and 18 years who underwent external fixation for a femur fracture from 1997 to 2012 were identified. Patients were included for analysis provided they had adequate radiographs and clinical notes at a minimum followup of 3 months after the external fixator was removed. Patients were excluded from the study if the preoperative radiographs or at least one set of postoperative radiographs of the involved femur were not available. The treatment modality used was chosen at the discretion of the surgeon based on several factors, including patient age, patient size, fracture location, and fracture pattern. In general, our indications for use of external fixation included length-unstable fracture (12), metadiaphyseal location (seven), pathologic fracture (two), and refracture after treatment with intramedullary flexible nails (two). Two hundred eighty-nine children with pediatric femur fractures were treated by the senior author (SS) over the 15-year study period, of whom 31 (11%) were treated with external fixation. Six patients (19%) were excluded as a result of inadequate radiographs or length of followup. In addition, four patients underwent fixator-augmented intramedullary nailing and were also excluded from analysis. The minimum followup of the remaining 21 patients was 5 months (mean, 22 months; range, 5–45 months) after removal of the fixator.
Medical records and radiographs were reviewed by a senior orthopaedic surgery resident (HK). Demographic data, mechanism of injury, medical history, and associated injuries were identified (Table 1). Initial radiographs were reviewed to assess fracture location and pattern and measurements taken for fracture angulation, displacement, and shortening (Table 2) [23, 25]. Fracture location was divided into proximal metadiaphyseal (at or proximal to the lesser trochanter); proximal, middle, or distal third shaft; and distal metadiaphyseal (distal to the metaphyseal flare). Fracture pattern was categorized as transverse, oblique, spiral, or comminuted. The presence of any underlying pathologic lesion was documented. Fracture angulation was measured as the angle between fracture fragments in both the coronal (varus/valgus) and sagittal (flexion/extension) planes. Displacement (in millimeters) was measured as the amount of translation between the fracture fragments noted on the AP and lateral views. Shortening (in millimeters) was measured as the maximum amount of overlap between the fragments in either the AP or lateral view.
Table 1.
Demographic data of 21 children with closed femoral shaft fractures treated with external fixation
| Demographic | Mean (range) |
|---|---|
| Age (years) | 10 (6–15) |
| Sex | |
| Male | 19 |
| Female | 2 |
| Body mass index (kg/m2) | 21 (13–44) |
| Mechanism of injury | |
| Motor vehicle accident | 11 |
| Low-energy fall | 6 |
| High-energy fall | 4 |
| Underlying disorders | |
| Osteogenesis imperfecta | 1 |
| Prior ipsilateral lower extremity fracture or osteotomy | 6 |
Table 2.
Details of preoperative fracture characteristics based on radiographs
| Preoperative fracture characteristic | Mean (range) |
|---|---|
| Fracture location | |
| Proximal metadiaphyseal | 3 |
| Proximal shaft | 8 |
| Midshaft | 4 |
| Distal shaft | 2 |
| Distal metadiaphyseal | 4 |
| Fracture pattern | |
| Transverse | 4 |
| Oblique | 5 |
| Spiral | 2 |
| Comminuted | 10 |
| Initial angulation (degrees) | |
| AP | 17 (4–40) |
| Lateral | 16 (2–35) |
| Initial displacement (mm) | |
| AP | 12 (0–27) |
| Lateral | 14 (0–34) |
| Initial shortening (mm) | 20 (0–71) |
Surgical Technique
The surgical technique for external fixation of pediatric femur fractures has been previously reported [20, 21]. Patients were positioned supine on a radiolucent table with the entire leg and lower abdomen included in the sterile field. Reference pins were placed perpendicular to the proximal and distal axes of the femur. The width of the underlying bone determined the diameter of the half pin (no greater than one-third the diameter of the underlying bone), and hydroxyapatite-coated pins were preferred, if available. Two or three pins each were placed into the proximal and distal fragments. To avoid thermal necrosis of the underlying bone, hand insertion of predrilled half pins was used. Pin clamps, arches, or rings were then applied and the fracture was reduced under fluoroscopic control. The proximal and distal pin clusters were connected using longitudinal connectors (bars, threaded rods, or struts). To confirm the overall alignment of the limb, an electrocautery cord was used to assess the mechanical axis of the entire limb (center of the femoral head to the center of the tibial plafond) [22].
Aftercare
If able, patients were mobilized partial weightbearing with assistive devices and advanced to unrestricted full weightbearing 3 to 5 weeks postoperatively. Outpatient physical therapy was not routinely prescribed. Daily pin care with half-strength hydrogen peroxide was recommended. A prescription for a 1-week course of oral antibiotics (usually a first-generation cephalosporin) was provided to the caretakers with instructions to start the antibiotics if there was increasing erythema or purulent drainage around the pin site(s).
When early radiological healing was noted, the external fixator was often dynamized by loosening the longitudinal connection between the proximal and distal pin clusters. Generally, the patient was scheduled for removal of the external fixator once at least three cortices were radiographically healed on two orthogonal radiographs of the fracture site. In ambulatory children, fracture healing was also assessed clinically by the patient’s ability to fully bear weight without pain or assistive devices.
Removal of the External Fixator
Removal of the external fixator was performed in the operating room under general anesthesia. This provided an opportunity to assess healing of the fracture under fluoroscopy, débride the pin tracts with undermining of the puckered skin edges, and apply a cast or prefabricated brace across the fracture site. The type of postremoval immobilization depended on the patient’s age, fracture pattern and location, underlying bone quality, and ability to comply with weightbearing instructions.
Operative notes and radiographs were reviewed for the type of external fixator (monolateral, circular, hybrid) and the number of rings, arches, and half pins used. Followup radiographs were examined for fracture healing, including the number of cortices healed at the time of fixator removal. Postremoval immobilization was also recorded. At 1, 3, 6, and 12 months postremoval and most recent followup, radiographs were again examined for alignment of the femur, including residual angulation at the fracture site. If a full-length standing radiograph of both lower extremities was available, radiographic limb length discrepancy, mechanical axis deviation, and mechanical lateral distal femoral angle were also measured [23]. Patients who had concomitant lower extremity fractures or previous osteotomies were excluded from the analysis of limb length discrepancy and alignment. Fracture nonunion was defined as lack of progressive callus formation at least 6 months after injury.
Outpatient records were reviewed for complications (such as refracture, infection, leg length discrepancy, or angular deformity), postremoval ROM, clinical leg length discrepancy, and functional status. It was also noted if any additional treatment or unplanned surgery was required.
Statistical Analysis
Descriptive statistical measures such as mean and range were calculated for various demographic, clinical, and radiologic outcome parameters using Microsoft ExcelTM (Redmond, WA, USA). The prevalence of complications was calculated as a percentage of the number of fractures (and patients).
Results
Healing and Radiographic Alignment
Mean time in the external fixator was 17 weeks (range, 9–24 weeks). Only one patient had less than three cortices healed at the time of fixator removal. Minimum length of followup after fixator removal was 5 months (mean, 22 months; range, 5–45 months). Radiographic analysis demonstrated that there were no nonunions and that one patient had residual apex anterior angulation > 10° (15°) without functional deficits (Table 3).
Table 3.
Details of treatment and final radiographic measurements
| Details of treatment and final radiographic measurements | Mean (range) |
|---|---|
| Type of external fixator | |
| Hybrid | 14 |
| Circular | 1 |
| Monolateral | 6 |
| Time in external fixator (weeks) | 17 (9–24) |
| Postoperative immobilization | |
| Hip-knee-ankle-foot orthosis | 5 |
| Abduction brace | 7 |
| Long leg cast | 7 |
| Knee immobilizer | 1 |
| Hip spica cast | 1 |
| Length of followup (months) | 22 (5–45) |
| Final fracture angulation (degrees) | |
| AP | 2 (0–5) |
| Lateral | 6 (2–15) |
| Final lateral distal femoral angle (degrees) | 87 (83–93) |
| Final leg length discrepancy (mm) | 7 (0–22) |
Complications
Complications in this cohort included one refracture (5%) (Table 4). This patient was initially treated for 18 weeks in a monolateral fixator (Fig. 1) and then refractured after a low-energy fall. He underwent open reduction and submuscular plating and the fracture healed uneventfully. One patient with an isolated femur fracture had a radiographic leg length discrepancy > 2 cm (ipsilateral shortening of 2.2 cm) with no functional deficits or additional treatment. A second patient was initially treated in a spica cast overseas and then presented to our institution 6 weeks later with 36 mm of shortening in the cast. He underwent hybrid external fixation with 34-mm residual shortening and eventually required contralateral distal femoral epiphysiodesis. The leg length discrepancy in this patient was not included as a complication because he had presented late and the shortening was present at the time of external fixation.
Table 4.
Details of complications after external fixation in 21 patients
| Complication (number of patients) | Treatment | Outcome |
|---|---|---|
| Refracture (1) | ORIF (plating) | Healed without complication |
| Radiographic leg length discrepancy > 2 cm (1) | Observation | No functional deficits |
| Ankle and great toe extensor weakness (1) | Revision of external fixator | Residual weakness, no functional deficits |
| Fracture angulation > 10°, apex anterior (1) | Observation | No functional deficits |
ORIF = open reduction and internal fixation.
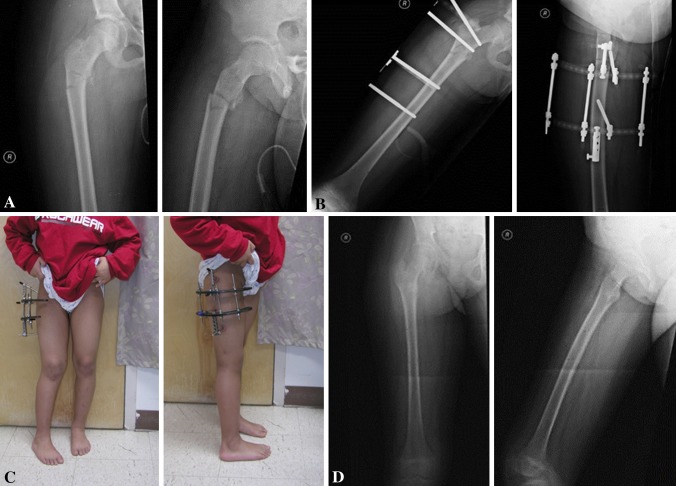
Fig. 1A–F.
A 13-year-old boy sustained a comminuted midshaft femur fracture (A), which was treated with a monolateral external fixator. After 18 weeks, three cortices were healed radiographically (B) and the external fixator was removed. The patient had a low-energy fall 3 days after removal of the fixator and application of a long leg cast, sustaining a refracture through the original fracture site (C). The refracture was treated with open reduction and submuscular plating (D). The latest radiographs 2 years after submuscular plating demonstrate complete fracture healing (E). At latest followup, the patient had full knee ROM and no leg length discrepancy or angulation (F).
One patient had a postoperative nerve injury without a clear explanation. This obese adolescent patient had a history of Blount disease and prior ipsilateral proximal tibial osteotomy. Postoperatively, he was unable to dorsiflex his ankle or extend his great toe, and the fixator was revised. At latest followup 12 months postoperatively, the patient had regained normal ankle dorsiflexion strength but had persistent asymptomatic weakness of the extensor hallucis longus.
Although pin site drainage was common, it usually responded to local pin care and a short course of oral antibiotics. No patients required intravenous antibiotics or early removal of the external fixator as a result of loosening.
Discussion
There are several fixation options for treating femoral shaft fractures in children and adolescents. With internal fixation devices such as submuscular plates and intramedullary nails gaining popularity, external fixation is often not even mentioned as a treatment option as is the case in the recent American Academy of Orthopaedic Surgeons clinical practice guideline for treating pediatric diaphyseal femur fractures [15]. Given the recent advances in half pin designs and availability of various types of external fixators, we thought that external fixation might still have a role in the management of pediatric femoral shaft fractures. We therefore sought to assess the time to healing, limb alignment, and complications in a cohort of pediatric patients with closed femoral shaft fractures who were managed with contemporary techniques of external fixation. Based on a retrospective review of 21 pediatric femoral shaft fractures treated with external fixation for various indications, predictable healing was achieved without any major pin-related issues and with acceptable alignment. However, complications such as refracture and leg length discrepancy still were observed.
There are several limitations in our study. First, this is a retrospective case series with a modest sample size. Nevertheless, all patients were treated by a single surgeon with a relatively consistent surgical technique and postoperative protocol. Second, some patients had relatively short followup, so late fractures and complications may have been missed. However, many of our patients did have followup of several years. Six patients (19%) had insufficient followup and were not included in this study; it is possible that these patients were not doing as well as those who had complete followup, and this should be considered. Third, we did not have a control group. Although a case-control study design would have been more robust, we were unable to match patients based on multiple variables including patient age and fracture pattern. Nevertheless, we did draw on the existing literature to make comparisons. The use of external fixation versus other modalities was at the discretion of the surgeon and was influenced by patient characteristics, fracture pattern, and location. Although this can be considered a selection bias, it may actually be more representative of the decision-making process used to guide treatment in clinical practice. Lastly, different types of external fixators were chosen at the surgeon’s discretion. Because we planned to determine the role for external fixation as a whole in managing pediatric femoral shaft fractures, this heterogeneity may in fact be clinically relevant as well.
Given the high proportion of patients whose fractures healed, we believe that the indications we used here, including length-unstable fracture patterns, metadiaphyseal location (Fig. 2), and refracture after flexible nailing, were appropriate. External fixation may also be useful for certain pathologic fractures (Fig. 3). In pediatric patients, pathologic fractures are often related to benign lesions such as bone cysts and nonossifying fibromas [6]. These lesions are often metadiaphyseal and may be more difficult to stabilize with flexible nails or plating. However, external fixation allows fracture stabilization through percutaneous means while sparing the physis. The high proportion of patients whose fractures healed in this study was consistent with other studies on external fixation [3, 4, 7, 9, 10, 14, 18] and is comparable to that of studies using internal fixation techniques [2].
Fig. 2A–D.
A 9-year-old girl sustained a proximal metadiaphyseal fracture (A), which is a challenging location for fixation with flexible nailing or plating. A hybrid external fixator using two arches was applied, as seen in these radiographs (B) and clinical photographs (C). There was uneventful healing of the fracture after removal of the external fixator (D).
Fig. 3A–C.
This 14-year-old boy was tackled while playing football. Radiographs and CT scan demonstrate fracture through a distal metadiaphyseal benign-appearing lesion (A). Closed reduction was performed and a circular external fixator applied (B). At 10 months followup, the fracture had healed (C).
Our 5% frequency of residual angular deformity (one of the 21 patients) is on the lower end of the reported risk of 3% to 19% [3, 4, 7, 9, 10, 14, 18]. Interestingly, our case had apex anterior angulation with near normal frontal plane alignment. Because sagittal plane deformities are in the plane of knee motion, these may not be as clinically significant as similar magnitude deformities in the frontal plane. It is likely that not enough attention was given to ensuring accurate reduction in the sagittal plane intraoperatively, especially with the overlying external fixator. One patient (5%) with an isolated femur fracture had radiographic shortening. Previous investigators have reported a limb length discrepancy (usually defined as > 1.5–2 cm) of 0% to 14% [3, 9, 14, 18]. Another patient was initially treated overseas with a hip spica cast and presented to us 6 weeks postinjury with substantial shortening. This amount of leg length discrepancy may have been prevented with a more anatomic reduction and stabilization using an internal or external device rather than a spica cast at the time of his original injury.
Previous studies have reported on the complications of external fixation for pediatric femoral shaft fractures (Table 5). The most common complications include malunion, delayed union, refracture, and pin tract infection [2–4, 7, 9, 14, 18, 24]. However, advances in external fixation technique and pin design have aimed to minimize these complications, including hydroxyapatite-coated half pins, avoiding thermal necrosis by using sharp drill bits and inserting predrilled half pins without using power, selecting the appropriate sized half pins based on the diameter of the underlying bone, early use of oral antibiotics for pin site drainage, and possibly dynamization of the frame [5, 8, 10, 19, 21]. In our study there was one refracture through the fracture site (5%) and none through the pin tracts. This patient had a middiaphyseal comminuted fracture that was treated with a monolateral external fixator. Our refracture rate is toward the lower end of the range cited in the literature (1%–22%) [3, 4, 14, 18, 24]. Skaggs et al. [24] reported that fractures with three to four cortices healed radiographically at the time of fixator removal had a significantly lower refracture rate than those with less than three cortices healed (4% versus 33%). In our series, all but one patient had at least three cortices healed at the time of fixator removal. Recently, the use of submuscular bridge plating has gained popularity for the treatment of length-unstable and very proximal or distal femur fractures [17]. However, Heyworth et al. [12] recently reported an increased likelihood of developing distal femoral valgus deformity after submuscular plating of distal femoral shaft fractures. Both our refracture and residual angular deformity occurred in patients with comminuted middiaphyseal fractures. Although this has not been thoroughly studied, perhaps submuscular plating or a statically locked intramedullary nail may be more appropriate for length-unstable middiaphyseal fractures and external fixation more suited for fractures closer to the physis. Although pin site inflammation and drainage are quite common (up to 100% in some studies), no patients in this study required intravenous antibiotics or additional surgery [3, 4, 9, 14, 18, 24]. This may be the result of our use of hydroxyapatite-coated half pins, a compression bandage around pins, and the use of oral antibiotics to address superficial pin tract infections.
Table 5.
Prior studies reporting outcome, including complications after external of pediatric femoral shaft fractures
| Study | Number of patients | Delayed or nonunion | Refracture | Deep pin tract infection | Leg length discrepancy (> 2 cm) | Malunion or angulation (> 10°) | |||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Aronson and Tursky [3] | 44 | 0/44 | 0% | 0/44 | 0% | 5/44 | 11% | 5/44 | 11% | 8/44 | 18% |
| Blasier et al. [4] | 139 | 0/139 | 0% | 2/139 | 1.4% | 7/139 | 5% | N/A | N/A | 4/139 | 3% |
| de Sanctis et al. [7] | 82 | 0/82 | 0% | N/A | N/A | 0/82 | 0% | N/A | N/A | 6/82 | 7% |
| Gregory et al. [9] | 27 | 0/27 | 0% | 4/27 | 15% | 1/27 | 4% | 2/27 | 7% | 5/27 | 19% |
| Hedin and Larsson [10] | 98 | 0/98 | 0% | 2/98 | 2% | 0/98 | 0% | 0/98 | 0% | 5/98 | 5% |
| Kapukaya et al. [14] | 57 | 0/57 | 0% | 1/57 | 2% | 0/57 | 0% | 0/57 | 0% | N/A | N/A |
| Miner and Carroll [18] | 37 | 1/37 | 3% | 8/37 | 22% | 2/33 | 6% | 5/37 | 14% | 4/21 | 19% |
| Skaggs et al. [24] | 66 | N/A | N/A | 8/66 | 12% | 9/66 | 14% | N/A | N/A | N/A | N/A |
N/A = data not available.
Despite its limitations, this study draws out useful tips and concepts that may help to further elucidate the indications for external fixation of pediatric femur fractures. Using current techniques, external fixation remains a viable option in managing pediatric femoral shaft fractures that are length-unstable, metadiaphyseal in location, refractures after elastic nailing, and pathologic fractures with benign metaphyseal lesions. In our experience, children and their caretakers have been able to tolerate the external fixator well. Given its wider availability and lower cost, external fixation may also be a viable treatment option for managing certain pediatric femoral shaft fractures in resource-challenged and austere settings. With additional modifications in surgical technique and postoperative protocol, there is a potential for further improvement in clinical outcome in closed femoral shaft fractures in children and adolescents.
Footnotes
One of the authors (SS) is the guest editor for the Limb Lengthening and Reconstruction Society (LLRS) Proceedings for CORR®. Although the selected papers were graded by a panel of judges (who were selected by the LLRS Board of Directors), his being a coauthor for this article could be perceived as a potential conflict of interest.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research editors and board members are on file with the publication and can be viewed on request.
Each author certifies that his or her institution approved the human protocol for this investigation, that all investigations were conducted in conformity with ethical principles of research, and that informed consent for participation in the study was obtained.
References
- 1.Alonso JE, Horowitz M. Use of the AO/ASIF external fixator in children. J Pediatr Orthop. 1987;7:594–600. doi: 10.1097/01241398-198709000-00018. [DOI] [PubMed] [Google Scholar]
- 2.Anglen JO, Choi L. Treatment options in pediatric femoral shaft fractures. J Orthop Trauma. 2005;19:724–733. doi: 10.1097/01.bot.0000192294.47047.99. [DOI] [PubMed] [Google Scholar]
- 3.Aronson J, Tursky EA. External fixation of femur fractures in children. J Pediatr Orthop. 1992;12:157–163. doi: 10.1097/01241398-199203000-00003. [DOI] [PubMed] [Google Scholar]
- 4.Blasier RD, Aronson J, Tursky EA. External fixation of pediatric femur fractures. J Pediatr Orthop. 1997;17:342–346. [PubMed] [Google Scholar]
- 5.De Bastiani G, Aldegheri R. Renzi Brivio L. The treatment of fractures with a dynamic axial fixator. J Bone Joint Surg Br. 1984;66:538–545. doi: 10.1302/0301-620X.66B4.6746689. [DOI] [PubMed] [Google Scholar]
- 6.De Mattos CBR, Binitie O, Dormans JP. Pathological fractures in children. Bone Joint Res. 2012;1:272–280. doi: 10.1302/2046-3758.110.2000120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.de Sanctis N, Gambardella A, Pempinello C, Mallano P. Della Corte S. The use of external fixators in femur fractures in children. J Pediatr Orthop. 1996;16:613–620. doi: 10.1097/01241398-199609000-00013. [DOI] [PubMed] [Google Scholar]
- 8.Domb BG, Sponseller PD, Ain M, Miller NH. Comparison of dynamic versus static external fixation for pediatric femur fractures. J Pediatr Orthop. 2002;22:428–430. [PubMed] [Google Scholar]
- 9.Gregory P, Pevny T, Teague D. Early complications with external fixation of pediatric femoral shaft fractures. J Orthop Trauma. 1996;10:191–198. doi: 10.1097/00005131-199604000-00007. [DOI] [PubMed] [Google Scholar]
- 10.Hedin H, Larsson S. Technique and considerations when using external fixation as a standard treatment of femoral fractures in children. Injury. 2004;35:1255–1263. doi: 10.1016/j.injury.2003.07.006. [DOI] [PubMed] [Google Scholar]
- 11.Heideken J, Svensson T, Blomqvist P, Haglund-Akerlind Y, Janarv PM. Incidence and trends in femur shaft fractures in Swedish children between 1987 and 2005. J Pediatr Orthop. 2011;31:512–519. doi: 10.1097/BPO.0b013e31821f9027. [DOI] [PubMed] [Google Scholar]
- 12.Heyworth BE, Hedequist DJ, Nasreddine AY, Stamoulis C, Hresko MT, Yen YM. Distal femoral valgus deformity following plate fixation of pediatric femoral shaft fractures. J Bone Joint Surg Am. 2013;95 526–533. [DOI] [PubMed]
- 13.Hinton RY, Lincoln A, Crockett MM, Sponseller P, Smith G. Fractures of the femoral shaft in children. Incidence, mechanisms, and sociodemographic risk factors. J Bone Joint Surg Am. 1999;81:500–509. doi: 10.2106/00004623-199904000-00007. [DOI] [PubMed] [Google Scholar]
- 14.Kapukaya A, Subasi M, Necmioglu S, Arslan H, Kesemenli C, Yildirim K. Treatment of closed femoral diaphyseal fractures with external fixators in children. Arch Orthop Trauma Surg. 1998;117:387–389. doi: 10.1007/s004020050273. [DOI] [PubMed] [Google Scholar]
- 15.Kocher MS, Sink EL, Blasier RD, Luhmann SJ, Mehlman CT, Scher DM, Matheney CT, Sanders JO, Watters WC, Goldberg MJ, Keith MW, Haralson RH, Turkelson CM, Wies JL, Sluka P, McGowan R. American Academy of Orthopaedic Surgeons Clinical Practice Guideline on Treatment of Pediatric Diaphyseal Femur Fracture. J Bone Joint Surg Am. 2010;92:1790–1792. doi: 10.2106/JBJS.J.00137. [DOI] [PubMed] [Google Scholar]
- 16.Kuremsky MA, Frick SL. Advances in the surgical management of pediatric femoral shaft fractures. Curr Opin Pediatr. 2007;19:51–57. doi: 10.1097/MOP.0b013e3280123142. [DOI] [PubMed] [Google Scholar]
- 17.Li Y, Hedequist DJ. Submuscular plating of pediatric femur fracture. J Am Acad Orthop Surg. 2012;20:596–603. doi: 10.5435/JAAOS-20-09-596. [DOI] [PubMed] [Google Scholar]
- 18.Miner T, Carroll KL. Outcomes of external fixation of pediatric femoral shaft fractures. J Pediatr Orthop. 2000;20:405–410. [PubMed] [Google Scholar]
- 19.Moroni A, Vannini F, Mosca M, Giannini S. State of the art review: techniques to avoid pin loosening and infection in external fixation. J Orthop Trauma. 2002;16:189–195. doi: 10.1097/00005131-200203000-00009. [DOI] [PubMed] [Google Scholar]
- 20.Sabharwal S. Role of Ilizarov external fixator in the management of proximal/distal metadiaphyseal pediatric femur fractures. J Orthop Trauma. 2005;19:563–569. doi: 10.1097/01.bot.0000174706.03357.26. [DOI] [PubMed] [Google Scholar]
- 21.Sabharwal S, Kishan S, Behrens F. Principles of external fixation of the femur. Am J Orthop. 2005;34:218–223. [PubMed] [Google Scholar]
- 22.Sabharwal S, Zhao C. Assessment of lower limb alignment: supine fluoroscopy compared with a standing full-length radiograph. J Bone Joint Surg Am. 2008;90:43–51. doi: 10.2106/JBJS.F.01514. [DOI] [PubMed] [Google Scholar]
- 23.Sabharwal S, Zhao C, Edgar M. Lower limb alignment in children: reference values based on a full-length standing radiograph. J Pediatr Orthop. 2008;28:740–746. doi: 10.1097/BPO.0b013e318186eb79. [DOI] [PubMed] [Google Scholar]
- 24.Skaggs DL, Leet AI, Money MD, Shaw BA, Hale JM, Tolo VT. Secondary fractures associated with external fixation in pediatric femur fractures. J Pediatr Orthop. 1999;19:582–586. [PubMed] [Google Scholar]
- 25.Slongo T, Audigé L, AO Pediatric Classification Group (2007). AO Pediatric Comprehensive Classification of Long-Bone Fractures (PCCF). Davos, Switzerland: AO Foundation; 2010.
- 26.Tolo VT. External skeletal fixation in children’s fractures. J Pediatr Orthop. 1983;3:435–442. doi: 10.1097/01241398-198309000-00004. [DOI] [PubMed] [Google Scholar]
- 27.Wright JG, Wang EE, Owen JL, Stephens D, Graham HK, Hanlon M, Nattrass GR, Reynolds RA, Coyte P. Treatments for paediatric femoral fractures: a randomised trial. Lancet. 2005;365:1153–1158. doi: 10.1016/S0140-6736(05)71878-X. [DOI] [PubMed] [Google Scholar]