Abstract
Background
Treatment of tibial nonunion with bone loss is extremely difficult. A variety of techniques have been described, but each has shortcomings, in particular prolonged external fixation time as well as serious complications such as nonunion and infection. Accordingly, we developed a technique that seeks to reduce these complications by using a circular external fixator in addition to an intramedullary nail to achieve union, limb lengthening, and stability of the regenerated segment.
Description of Technique
First, the pseudoarthrosis area is resected, and acute compression is continued until bone contact at the docking site was achieved. Then primary grafting is applied to the docking site using a graft harvested from the patient’s iliac bone, and the predrilled nail holes localized on the middle segment of the tibia are locked with a free-hand technique. Finally, lengthening is performed to overcome the leg-length discrepancy with an external fixator.
Methods
Between 2008 and 2011, this technique was used to treat five patients with tibial nonunion with bone loss. All patients were available for a minimum of a 14-month followup (mean, 30 months; range, 14–58 months). General indications for the procedure were age older than 16 years, tibial nonunion with bone loss, and the absence of any psychiatric disorder. We evaluated external fixation time, external fixation index (defined as the duration of external fixation in months divided by the total amount of bone transported and/or the amount of lengthening in centimeters), and time to union on plain radiographs, clinical results using the Paley bone and functional assessment scores, and postoperative complications from chart review.
Results
The external fixation time was 4 months (range, 3–5 months), and the average external fixation index was 0.4 months/cm. The mean time to bone union was 4.6 months (range, 3.5–5.5 months). All angles were determined to be in the normal range. No patients developed refracture or malalignment either on the docking site or the osteotomy site. Paley bone evaluation results were excellent in all five patients, and Paley functional results were excellent in four and good in one. We observed 10 pin-site infections as minor complications, and one patient was left with a residual equinus deformity of 5° as a major complication according to the Paley classification.
Conclusions
Our technique combining acute shortening and distraction osteogenesis had promising results for the treatment of tibial nonunion with bone loss in a small group of patients. However, future studies directly comparing available approaches to this difficult problem are required. Because this problem is uncommon, these studies will almost certainly require the cooperation of multiple large participating centers.
Level of Evidence
Level IV, therapeutic study. See Guidelines for Authors for a complete description of levels of evidence.
Introduction
The adverse effects of tibial nonunion on health-related quality of life are severe [3]. Several treatment methods have been described, including bone grafting with internal fixation, electrical stimulation, vascularized or nonvascularized transfer of fibula, the Papineau technique (a type of open bone grafting in which wounds are packed with cancellous bone with no attempt at soft tissue coverage), and débridement and resection of the bone followed by bone transport by Ilizarov [1, 2, 10, 11, 13, 21]. However, all of these techniques have high rates of nonunion, recurrence of infection, leg-length discrepancy, malalignment, refracture, and a prolonged treatment period [27].
We therefore describe a technique designed to reduce these complication rates that combined a circular external fixator with an intramedullary nail to achieve union, limb lengthening, and stability of the regenerated segment. Our technique involves gradual bone transport, which relies on compression and distraction. A similar technique was reported by Giebel [12] and popularized by Salis de Gauzag et al. [26]. The main differences between the current technique and those others are the acute shortening of the pseudoarthrosis site, and then gradual compression with a 2-mm/day period, and primary grafting of the docking site so that the risk of delayed union or nonunion is minimized.
In this study, five patients with tibial nonunion with bone loss were treated with this technique of acute shortening and distraction osteogenesis. We evaluated external fixation time, external fixation index (defined as the duration of external fixation in months divided by the total amount of bone transported and/or the amount of lengthening in centimeters), and time to union on plain radiographs, clinical results using the Paley bone and functional assessment scores, and postoperative complications from chart review.
Surgical Technique
The surgery was carried out on all five patients under general anesthesia without a tourniquet. The patient was placed supine on a radiolucent operating table, and 1 g first-generation cephalosporin was intravenously administered 30 minutes preoperatively. Custom-made Trigen nails (Smith & Nephew, Memphis, TN, USA) that were modified with additional locking holes according to nail thickness and length and a constructed Ilizarov frame (Tasarim Med; Topkapi, Istanbul, Turkey) were used; these were prepared from preoperative radiological measurements magnified by 100% (Fig. 1). For the surgery, a transverse incision was made in the nonunion site, and after débridement of the soft tissue, resection of the devitalized bone ends was performed until healthy-appearing bone with open intramedullary canals and bleeding surfaces (paprika sign) was reached (Fig. 2). If the fibula was intact, resection of the same length was performed at the same level so that the lengthening could be done. After closure of the subcutaneous tissue, a 2-cm vertical incision was made over the patellar ligament. A threaded Kirschner wire was inserted using a patellar ligament splitting approach to localize the entry point of the tibial nail under fluoroscopic control. After the confirmation of the entry point of the tibial nail, a guidewire was inserted through the medullary canal. The medullary canal was overreamed by 1.5 mm relative to the diameter of the intramedullary nail to be used to allow sliding of the nail for lengthening. Poller interference blocking screws were placed before nail insertion to reduce the larger diameter of the medullary canal at the metaphyseal level to prevent pendular movement of the nail. The length of the selected nail was longer to provide sufficient nail length on both sides of the regenerated bone at the completion of distraction. This necessitates the use of an intramedullary nail that is longer than the length of the tibia, so care was taken to allow the excess nail length to protrude into the suprapatellar region until distraction is completed, by which time the nail will glide gradually to its correct position. The distal holes of the nail were locked and proximal holes of the nail were locked on completion of the lengthening period in another session.
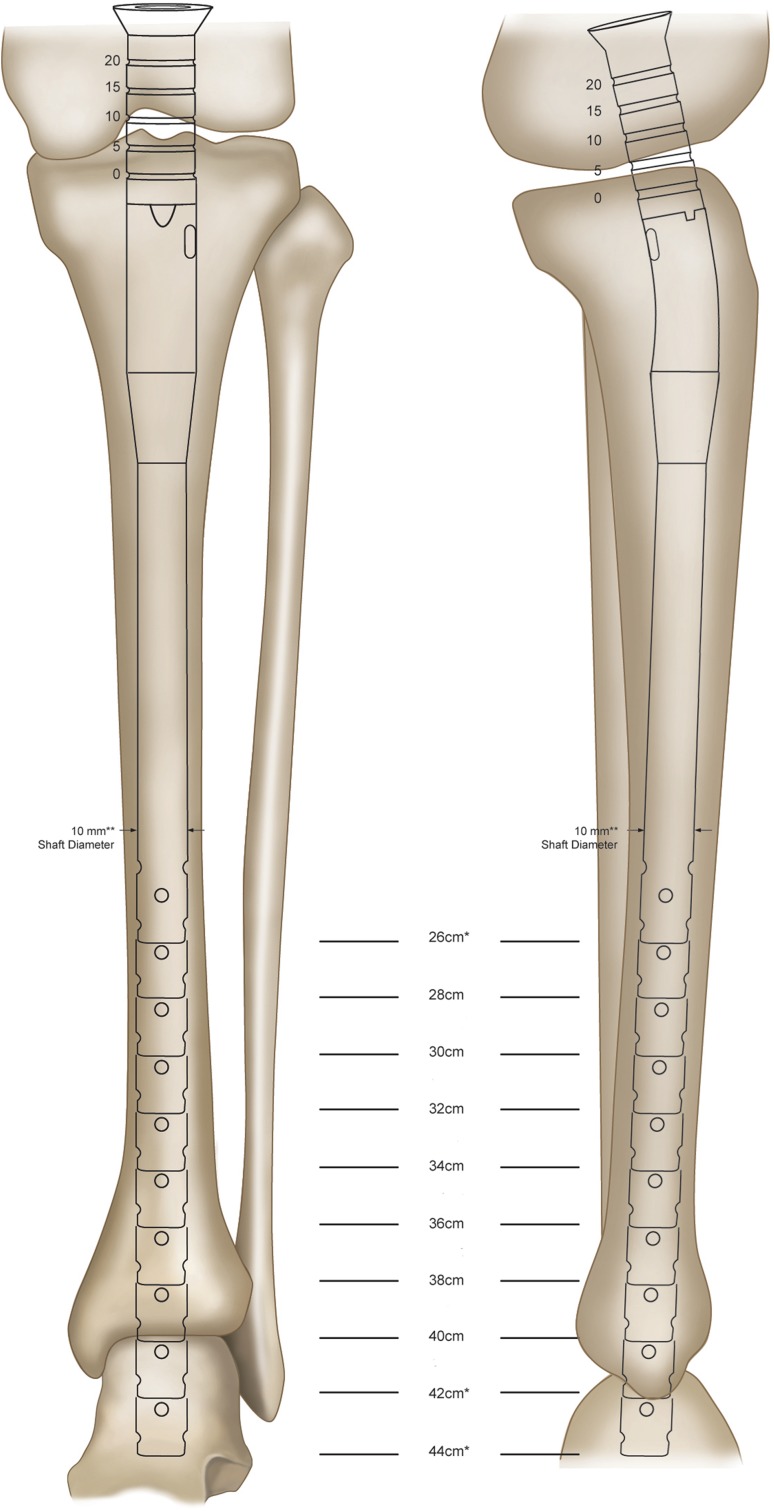
Fig. 1.
Drawing of an AP and lateral tibia view showing a template over a tibia to determine the length and width of the tibial nail and also the levels at which the extra locking holes should be predrilled.
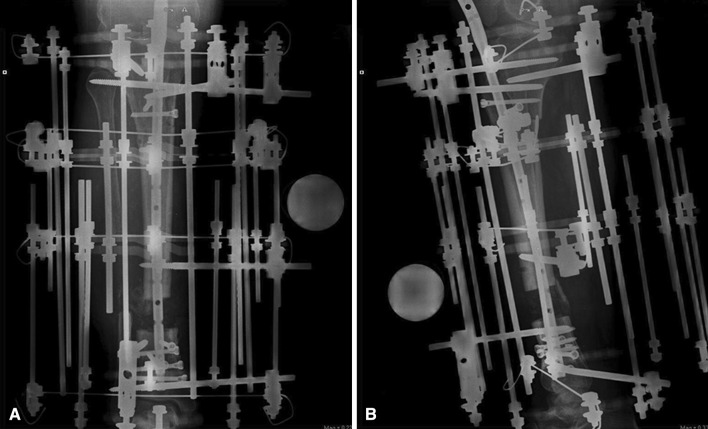
Fig. 2.
Treatment of a patient (Patient 5) with chronic osteomyelitis of the distal part of the tibia with transverse exposure is shown.
The second phase of the bifocal technique was the lengthening procedure. The preoperatively prepared four-ring circular external fixator was placed on the tibia, and each of the circular rings was held with one Kirschner wire and one half-pin, which was placed under fluoroscopy vertical to the tibial anatomic axis and parallel to the joint. Great care was taken to avoid contact of the Kirschner wires and Schanz screws with the intramedullary nail. At least 1 mm of free space should exist between the Schanz screws or Kirschner wires and the intramedullary nail to prevent medullary infection triggered by a pin-site infection [15]. To insert half-pins without contact with the nail, the cannulated drill-bit technique described by Paley et al. is used [20]. A Kirschner wire is inserted on the cortex of the tibia, perpendicular to the nail, at the level of the Schanz screw. The location of the wire is confirmed with an image intensifier. A hole is reamed over the Kirschner wire with a 4.8-mm cannulated drill bit. The half-pin is inserted, and the clearance between the nail and the Schanz screw is confirmed with fluoroscopy (Fig. 3). When alignment and configuration were confirmed to be appropriate under fluoroscopy, a 2-cm incision was made immediately distal to the tibial tuberosity on the proximal segment, and a percutaneous osteotomy was made with a Gigli saw (posterior cortex of the tibia) and bone osteotomes (anterior cortex of the tibia). A 5-cm acute shortening was performed while measuring the filling of the tibialis anterior and tibialis posterior muscles with a sterile Doppler instrument and monitoring capillary circulation (Fig. 4A–B). To prevent subsequent circulatory problems, compression of 2 mm/day was planned to complete the remaining shortening on the docking site. The distraction test was performed with a circular external fixator. Acute distraction of 2 mm was performed to confirm the completeness of the osteotomy under fluoroscopic control. The distraction was then recompressed. Daily compression was continued after full bone contact was achieved at the docking site, and compression was stopped if the patient started to experience pain.
Fig. 3.

Lateral image intensifier view depicting a clear space between the Schanz screws and the nail.
Fig. 4A–B.
A fixator is shown on a 57-year-old man (Patient 4) who had three unsuccessful operations resulting from an open tibial fracture. Resection bone length was 9.5 cm. Acute shortening of the tibia was up to 5 cm at the nonunion site. (A) AP radiographic image of the tibia at postoperative Day 1 showing acute shortening. (B) Lateral radiographic image of the tibia at postoperative Day 1 showing acute shortening.
Next, grafting was applied to the docking site using a graft harvested from the patient’s iliac bones under general anesthesia; the predrilled nail holes localized on the middle segment of the tibia were locked with a free-hand technique (Fig. 5A–C). Distraction for lengthening was initiated after the grafting at the docking side using a rate of 1 mm/day divided into four equal increments. Full weightbearing with two crutches was started immediately postoperatively. The patient was discharged with policlinic followups. Patients were asked not to do knee exercises until the nail reached the subchondral region of the tibia.
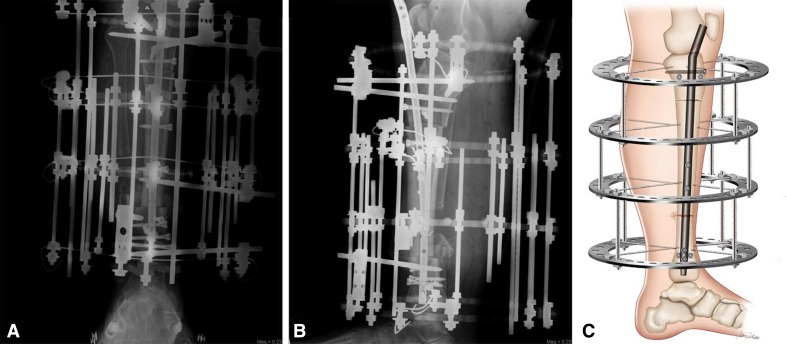
Fig. 5A–C.
Radiographic images and drawing of the tibia after autografting of the docking site and the predrilled nail holes localized on the middle segment of the tibia were locked with a free-hand technique. (A) Postoperative AP radiograph showing the intramedullary nail and the circular external fixator. The bone contact was achieved at the docking site, autogenous bone grafting of the docking site, and predrilled holes of the nail were locked with a free-hand technique. (B) Postoperative lateral radiograph showing the intramedullary nail and the circular external fixator, bone contact, primary autogenous grafting at the docking site, and predrilled holes of the nail were locked. (C) Drawing of the lateral tibia showing the bone contact and grafting at the docking site and locking of the predrilled holes of the nail.
A two-stage operation was carried out for one patient who had an infection together with pseudoarthrosis and bone loss (Cierny-Mader Type 4 [B]) [4]. In the first stage, the infected pseudoarthrotic area was resected; then a custom-made, antibiotic-impregnated, polymethylmethacrylate (a combination of 2.4 g teicoplanin and 40 g polymethylmethacrylate) intramedullary rod was placed in the pseudoarthrotic site and stabilization was achieved with a unilateral fixator. In the second stage, acute shortening and distraction were performed using the combined technique described. In the remaining four patients, all procedures were done during the same operation.
The patients were followed up at 2-week intervals during lengthening and 4-week intervals during consolidation. Lengthening was terminated when the desired bone length was achieved. The Ilizarov frame was removed, and the nail was locked proximally under general anesthesia. Isometric quadriceps and knee ROM exercises were then started (Fig. 6A–C). After removal of the external fixator, patients were encouraged to begin full weightbearing without a protective brace.
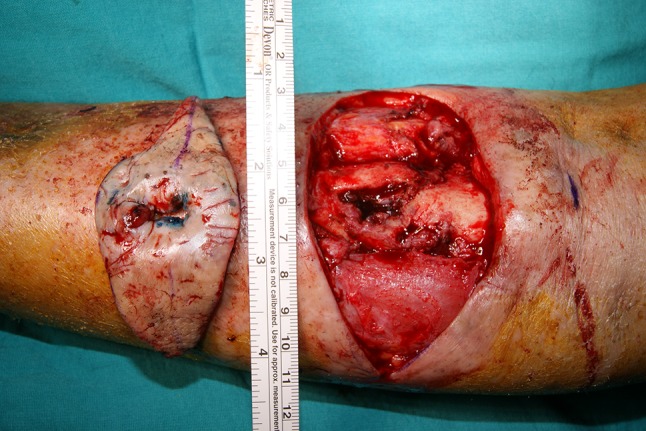
Fig. 6A–C.
Radiographic images and drawing of the tibia at 5 months followup showing removal of the circular external fixator; the proximal holes of the nail were locked with a free-hand technique. (A) AP radiograph showing the consolidated lengthening regenerate, the nail is locked proximally, and union at the docking site. (B) Lateral radiograph showing the consolidated lengthening regenerate, the nail is locked proximally, and union at the docking site. (C) Drawing of a lateral tibia image showing union at the docking site, the nail locked proximally, and the consolidated lengthening regenerate.
Patients and Methods
This study was approved by the local ethical committees of Dr Lutfi Kirdar Kartal Research and Training Hospital. Between 2008 and 2011, this technique was used to treat five patients with tibial atrophic nonunion with bone loss. All patients were available for a minimum of a 14-month followup period (mean, 30 months; range, 14–58 months). General indications for the procedure were age older than 16 years, tibial nonunion with bone loss, and no mental or psychiatric disorders. All patients were men, the average age of the patients at the time of the procedure was 38 years (range, 28–57 years), and the average bone loss was 8.6 cm (range, 6.5–10.5) (Table 1).
Table 1.
Demographics of the patients
| Patient number | Age (years) | Sex | Side | Previous surgeries |
|---|---|---|---|---|
| 1 | 28 | Male | Right | 1 |
| 2 | 34 | Male | Right | 1 |
| 3 | 31 | Male | Right | 2 |
| 4 | 57 | Male | Right | 3 |
| 5 | 41 | Male | Left | 3 |
The nonunions were the result of closed fractures in two patients and open fractures in three. The average number of previous surgeries was two (range, one to three). Preoperatively, plain AP and lateral radiographs and CT images were taken of all patients to evaluate the amount of resection of the dead or infected bone (Fig. 7A–C). Doppler ultrasonography was used to decide the vascular status of the involved limb. Atrophic bone resection was performed until good, bleeding bone ends were evident (paprika sign) [29] in the pseudoarthrosis regions of the four noninfected cases.
Fig. 7A–C.
Drawing and radiographs of a tibia are shown indicating the margins of resection as determined on AP and lateral radiographs. (A) Drawing of a lateral tibia showing the margins of resection (red dotted lines). (B) A 57-year-old man (Patient 4) who had tibial nonunion after three unsuccessful operations resulting from an open tibial fracture. AP radiograph of the right tibia showing a broken intramedullary nail and margin of the resection (black lines). (C) Lateral radiograph of the right tibia showing a broken intramedullary nail and margin of the resection (black lines).
We evaluated external fixation time, external fixation index (defined as the duration of external fixation in months divided by the total amount of bone transported and/or the amount of lengthening in centimeters), and time to union on plain radiographs, clinical results using the Paley bone and functional assessment scores, and postoperative complications from chart review. Conventional radiographs were taken every 2 weeks during the distraction phase and once a month during the consolidation phase. AP and lateral 14 × 17-inch radiographs of the tibia were used to determine bone union and consolidation. AP and lateral orthogonal radiographs were used to determine the medial proximal tibial angle, posterior proximal tibial angle, anterior distal tibial angle, and lateral distal tibial angle. All radiographic alignment measurements were completed by an independent orthopaedic surgeon (GB) who was not involved in the study. All radiological measurements and functional and bone assessment scores were determined at the final followup by the same reviewer. External fixator time was defined as the interval from the application of the fixator to removal of the fixator. External fixation index was defined as the duration of external fixation in months divided by the total amount of bone transported and/or the amount of lengthening in centimeters. Radiographic union was defined as the presence of callus in three of the four cortices as seen on AP and lateral radiographs.
The bone and functional results were evaluated by the classification of Paley et al. [19]. For bone results, four criteria were evaluated: union, infection, deformity, and leg-length discrepancy. An excellent bone result was one with union, no infection, deformity of less than 7°, and length discrepancy of less than 2.5 cm in the tibia. A good result was union plus any two of the others. A fair result was union plus one of the others. A poor result was nonunion or refracture or none of the others. The functional results were based on five criteria: significant limp, equinus rigidity of the ankle, soft tissue dystrophy (skin hypersensitivity, insensitivity of sole, or decubitus), pain, and inactivity (defined as unemployment because of the leg injury or inability to return to daily activities because of the leg injury). An excellent result was an active individual with none of the other four criteria; a good result was an active individual with one or two of the other four criteria; and a fair result was an active individual with three or four of the other criteria or an amputation. An inactive individual was considered a poor result regardless of the other criteria.
Complications were evaluated according to the Paley classification [17]. Minor complications were problems that did not require additional surgery, major complications were resolved with additional surgery, or where sequelae remained unresolved at the end of the treatment period.
Results
Radiographic Analysis
At latest followup, there was union in the pseudoarthrotic area in all five patients. The mean external fixation time was 4 months (range, 3–5 months) and the average external fixation index was 0.4 months/cm. The mean time to bone union was 4.6 months (range, 3.5–5.5 months) (Table 2). The average medial proximal tibial angle was 90° (range, 88°–95°), the average posterior proximal tibial angle was 78° (range, 77°–79°), the average lateral distal tibial angle was 85° (range, 78°–90°), and the average anterior distal tibial angle was 80° (range, 79°–81°). All angles were determined to be in the normal range (Table 3). No patients developed refracture or malalignment either on the docking site or the osteotomy site.
Table 2.
Outcome data on the study patients
| Patient number | Defect length (cm) | Acute shortening (cm; mean ± SD) and time (days) | Lengthening (cm) | EFT (months) |
|---|---|---|---|---|
| 1 | 6.5 | 5 ± 1.5 (7.5) | 7 | 3.2 |
| 2 | 9 | 5 ± 4 (20) | 10 | 4.2 |
| 3 | 7.5 | 5 ± 2.5 (12.5) | 8.5 | 3.5 |
| 4 | 9.5 | 5 ± 4.5 (22.5) | 10 | 3.8 |
| 5 | 10.5 | 5 ± 5.5 (27.5) | 10.5 | 4.5 |
| Patient number | EFI (months/cm) | Followup (months) | Docking site time (days) | Docking site time (months) | Docking site union (months) | Grafting |
|---|---|---|---|---|---|---|
| 1 | 0.5 | 58 | 10 | 0.3 | 3.5 | Yes |
| 2 | 0.4 | 34 | 25 | 0.8 | 4.5 | Yes |
| 3 | 0.4 | 24 | 18 | 0.6 | 4.3 | Yes |
| 4 | 0.4 | 19 | 25 | 0.8 | 5.5 | Yes |
| 5 | 0.4 | 14 | 28 | 0.9 | 5 | Yes |
EFT = external fixation time; EFI = external fixation index.
Table 3.
PPTA, MPTA, LDTA, and ADTA of the operated sides, Paley bone, and functional scores of the patients
| Patient number | Bone score | Functional score | Last followup PPTA (range, 77–84) | Last followup MPTA (range, 85–90) | Last followup LDTA (range, 86–92) | Last followup ADTA (range,78–82) |
|---|---|---|---|---|---|---|
| 1 | Excellent | Excellent | 78° | 88° | 86° | 79° |
| 2 | Excellent | Excellent | 78° | 90° | 85° | 80° |
| 3 | Excellent | Excellent | 79° | 89° | 85° | 81° |
| 4 | Excellent | Excellent | 77° | 95° | 78° | 80° |
| 5 | Excellent | Good | 79° | 88° | 90° | 80° |
PPTA = posterior proximal tibial angle; MPTA = medial proximal tibial angle; LDTA = lateral distal tibial angle; ADTA = anterior distal tibial angle.
Clinical Analysis: Paley Bone and Function Scores
The bone evaluation results were excellent in all five patients, and the functional results were excellent in four and good in one who were operated on as a result of the tibial nonunion associated with osteomyelitis.
Complications
We observed 10 pin-site infections, which were classified as minor complications. In three patients (Patients 1, 2, 3), the pin-site infections were evaluated as Dahl et al. [6] Stage 1 and were successfully treated with wet dressings. In another patient (Patient 4), Dahl Stage 2 infection developed at the tips of some of the external fixator pins and Schanz screws. One of the Schanz screws was removed, and the infection at the tip of the remaining pin was successfully treated with care and dressings. In this patient, because the tibialis anterior pulse was absent preoperatively, peripheral angiography was administered to confirm the absence of pulse. Angiography confirmed the damage of the tibialis anterior resulting from the previous surgeries. A 2 × 2-cm area of superficial skin necrosis developed in the postoperative wound site, and secondary healing was achieved with local débridement and close wound monitoring. Patient 5 (the one whose functional score was good rather than excellent) underwent a reoperation for chronic osteomyelitis. In this case, one of the Schanz screws holding the proximal ring was removed because of Stage 3 infection, and the infection around the other pin was treated with dressings. The Paley classification of this patient indicated limited ROM in the ankle and an equinus deformity. Although this improved with percutaneous achilloplasty and aggressive physiotherapy after fixator removal, the patient was left with a residual equinus deformity of 5°. This patient developed another complication during the second postoperative followup period; the proximal posterior tibial angle approached recurvatum in an unacceptable manner. The angle was reduced to 79° by adding a hinge to the proximal ring and including the supracondylar femur in the fixator system.
None of our patients developed any neurovascular deficits resulting from acute intraoperative compression or pin insertion. Similarly, no neurovascular deficits were observed during the lengthening period. No fat or pulmonary emboli were seen clinically, and there were no cases of intramedullary infection.
Discussion
Surgery for pseudoarthrosis and nonunion is problematic and difficult, and complications occur frequently. Dealing with bone loss and tibial nonunion is particularly challenging. Various treatment methods have been reported [16, 23, 24, 28], all of which aim to achieve tibial union, correct the deformity, cover soft tissue, align the limb, and compensate for orientation and leg-length discrepancy, thus achieving early mobilization and return to daily life for the patient. However, nonunion and infection still are frequently observed [24, 27]. We therefore developed a technique that seeks to reduce these complications by using a circular external fixator in addition to an intramedullary nail to achieve union, limb lengthening, and stability of the regenerated segment. We evaluated external fixation time, external fixation index (EFI), and time to union on plain radiographs, clinical results using Paley bone and functional assessment scores, and postoperative complications in a small group of patients who underwent this intervention.
This study is a small series, and, like any initial report, it has some important limitations. First, there could be a component of assessor bias because the surgeon is assessing his own results. Second, there was no comparison group to determine the success of the current study; future studies should do so.
Using an intramedullary nail with an Ilizarov external fixator is the main advantage; it has the potential to overcome the problems of shortening, plastic deformation, angular deformity, and fracture of the regenerated bone. Bone apposition on the docking site was achieved in a mean time of 21.2 days (range, 7.5–27.5 days). Compared with the classic external fixator, this combination technique has the potential to achieve reductions in the length of use of the external fixator, EFI, and the consolidation index. In a study by Cierny and Zorn [5], the EFI was calculated as 1.6 months/cm for a mean bone loss of 6.4 cm, Saleh and Rees [25] reported an EFI of 2.04 months/cm for a mean bone defect of 4.7 cm, Eralp et al. [10] reported EFI as 0.45 months/cm for a mean defect of 7 cm by using the combination of external fixator with intramedullary nail, Sala et al. [24] reported EFI as 2.0 ± 0.9 months/cm for a mean defect of 8.0 ± 2.6 cm using the Taylor Spatial Frame (Smith & Nephew, Memphis, TN, USA), and El-Rossay [9] reported EFI as 1.3 months/cm for a mean lengthening of 4.9 cm. In the present study, EFI was calculated as 0.4 months/cm, and mean bone loss was 8.6 cm (Table 4). However, to determine whether indeed these results are generalizable, comparative trials between our approach and other techniques are called for.
Table 4.
Details of bone transport studies
Results were evaluated using the Paley bone and functional assessment scores [19]. The bone evaluation results were excellent in all five patients, and the functional results were excellent in four and good in one patient who were operated on as a result of the tibial nonunion associated with osteomyelitis. All patients in the study group had returned to their preinjury jobs. Using a combination technique including an Ilizarov and a Taylor Spatial Frame, Sala et al. [24] reported 10 (83%) patients had excellent results, and two (17%) were good in terms of bony outcomes; functional results were excellent in six (50%), good in five (42%), and fair in one (8%). In that series, 12 patients were treated for postinfectious segmental tibial bone defects. Also using a Taylor Spatial Frame, Rozbruch et al. [22] found 24 (63%) excellent, 12 (32%) good, and two (5%) poor bone outcomes and 20 (53%) excellent, 14 (37%) good, two (5%) fair, and two (5%) poor patients with functional outcomes according to the Paley classification, but there were 11 persistent nonunions in their study group that were retreated. Using bifocal compression-distraction with an Ilizarov-type circular external fixator, Sen et al. [28] described the results of acute shortening and relengthening in the acute treatment of Grade III open tibial fractures with osteocutaneous loss in 24 patients. The bone results in their series were excellent in 21 (88%) and good in three (12%). The functional results were excellent in 19 (79%), good in four (17%), and fair in one (4%) patient. However, external fixation time was 7.1 months, EFI was 1.4 months/cm, and bone healing time was 7.5 months, which were longer than in the present study. Because they did not combine circular external fixator with intramedullary nailing, they did not use primary grafting of the docking site. However, to determine whether indeed these results are generalizable, comparative trials between our approach and other techniques are called for.
Early removal of the external fixator reduces the risk of pin-site infection and allows for earlier patient rehabilitation. In a study of 24 patients, Sen et al. [28] found a complication frequency of 2.08 per patient; other studies reported frequencies 2.2 complications per patient [25] and 2.5 complications per patient [7]. In this current study, our complication rate was 2.6 per patient, but most of the complications were minor and resolved without additional surgery. Patient 5, who underwent surgery for chronic osteomyelitis, was the only patient with a major complication, which resolved after additional surgery. Our combined technique has the potential to decrease the EFI and external fixation time by reducing problems originating from the circular external fixator [14, 18]. The use of intramedullary nailing together with an external fixator reduced the number of Schanz screws and Kirschner wires needed with the fixator. In this combined technique, a circular external fixator was preferred over a unilateral external fixator to avoid valgus malalignment deformity [14]. Angulations and translations were recorded as a bone transport complication. We did not observe any valgus deformity resulting from the Ilizarov external fixator. Only Patient 5 developed a posterior proximal tibial angle problem, which was resolved with an additional ring and a hinge system adapted to the proximal ring. Based on our results, we conclude that using an intramedullary nail with an external fixator will help minimize angulation and malalignment of the regenerated bone segment. The nail was extended from the proximal to the suprapatellar area during the acute shortening period. To preclude skin problems in the area of the proximal nail, physical therapy for the knee was not started until the nail reached the ideal location; none of the patients exhibited knee ROM loss, anterior knee pain, or skin wounds associated with the nail. Equinus deformity is a frequently encountered complication during bone transport and lengthening [9]. Eldridge and Bell [8] proposed that the foot must be included in the frame if the desired distraction is more than 10% of the total tibial length. In the current study, we had one case (Patient 5) with a major complication that was improved by percutaneous achilloplasty and aggressive physiotherapy.
Our technique combining acute shortening and distraction osteogenesis successfully treated tibial nonunion with bone loss in a small group of patients. This technique had favorable bone union time, external fixator time, EFI, and clinical results compared with reported parameters in studies of other approaches mentioned. However, future studies directly comparing available approaches to this difficult problem are required. Because this problem is uncommon, these studies will almost certainly require the cooperation of multiple large participating centers.
Acknowledgments
We thank Dr Guven Bulut for his radiographic measurements.
Footnotes
Each author certifies that he or she, or a member of his or her immediate family, has no funding or commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research ® editors and board members are on file with the publication and can be viewed on request.
Clinical Orthopaedics and Related Research ® neither advocates nor endorses the use of any treatment, drug, or device. Readers are encouraged to always seek additional information, including FDA-approval status, of any drug or device prior to clinical use.
Each author certifies that his or her institution approved the human protocol for this investigation, that all investigations were conducted in conformity with ethical principles of research, and that informed consent for participation in the study was obtained.
References
- 1.Aronson J. Current concepts review: limb lengthening, skeletal reconstruction bone transport with the Ilizarov method. J Bone Joint Surg Am. 1997;79:1243–1258. doi: 10.2106/00004623-199708000-00019. [DOI] [PubMed] [Google Scholar]
- 2.Atkins RM, Madhavan P, Sudhakar J, Whitwell D. Ipsilateral vascularized fibular transport for massive defects of the tibia. J Bone Joint Surg Br. 1999;81:1035–1040. doi: 10.1302/0301-620X.81B6.10001. [DOI] [PubMed] [Google Scholar]
- 3.Brinker MR, Hanus BD, Sen M, O’Connor DP. The devastating effects of tibial nonunion on health-related quality of life. J Bone Joint Surg Am. 2013;95:2170–2176. doi: 10.2106/JBJS.L.00803. [DOI] [PubMed] [Google Scholar]
- 4.Cierny G, 3rd, Mader JT, Penninck JJ. A clinical staging system for adult osteomyelitis. Clin Orthop Relat Res. 2003;414:7–24. doi: 10.1097/01.blo.0000088564.81746.62. [DOI] [PubMed] [Google Scholar]
- 5.Cierny G, 3rd, Zorn KE. Segmental tibial defects comparing conventional and Ilizarov methodology. Clin Orthop Relat Res. 1994;301:118–123. [PubMed] [Google Scholar]
- 6.Dahl MT, Gulli B, Berg T. Complications of limb lengthening. A learning curve. Clin Orthop Relat Res. 1994;301:10–18. [PubMed] [Google Scholar]
- 7.Dendrinos GK, Kontos S, Lyritis E. Use of the Ilizarov technique for treatment of non-union of the tibia associated with infection. J Bone Joint Surg Am. 1995;77:835–846. doi: 10.2106/00004623-199506000-00004. [DOI] [PubMed] [Google Scholar]
- 8.Eldridge JC, Bell DF. Problems with substantial limb lengthening. Orthop Clin North Am. 1991;22:625–631. [PubMed] [Google Scholar]
- 9.El-Rossay MA. Acute shortening and re-lengthening in the management of bone and soft-tissue loss in complicated fractures of the tibia. J Bone Joint Surg Br. 2007;89:80–88. doi: 10.1302/0301-620X.89B1.17595. [DOI] [PubMed] [Google Scholar]
- 10.Eralp L, Kocaoglu M, Rashid H. Reconstruction of segmental bone defects due to chronic osteomyelitis with use of an external fixator and an intramedullary nail. Surgical technique. J Bone Joint Surg Am. 2007;89:183–195. doi: 10.2106/JBJS.F.01579. [DOI] [PubMed] [Google Scholar]
- 11.Eralp L, Kocaoglu M, Yusof NM, Bulbul M. Distal tibial reconstruction with use of a circular external fixator and an intramedullary nail. The combined technique. J Bone Joint Surg Am. 2007;89:2218–2224. doi: 10.2106/JBJS.F.01579. [DOI] [PubMed] [Google Scholar]
- 12.Giebel G. Primary shortening in soft-tissue defects with subsequent callotasis in the tibia. Unfallchirurg. 1991;94:401–408. [Google Scholar]
- 13.Gordon L, Chiu EJ. Treatment of infected nonunions and segmental defects of the tibia with staged microvascular muscle transplantation and bone grafting. J Bone Joint Surg Am. 1988;70:377–386. [PubMed] [Google Scholar]
- 14.Harzenberg JE, Paley D. Tibial lengthening over nails (LON) Techniques in Orthopaedics. 1997;12:250–259. doi: 10.1097/00013611-199712000-00003. [DOI] [Google Scholar]
- 15.Kocaoglu M, Eralp L, Kilicoglu O, Burc H, Cakmak M. Complications encountered during lengthening over an intramedullary nail. J Bone Joint Surg Am. 2004;86:2406–2411. doi: 10.2106/00004623-200411000-00007. [DOI] [PubMed] [Google Scholar]
- 16.Lowenberg DW, Buntic RF, Buncke GM, Parrett BM. Long term results and costs of muscle flap coverage with Ilizarov bone transport in lower limb salvage. J Orthop Trauma. 2013;27:576–581. doi: 10.1097/BOT.0b013e31828afde4. [DOI] [PubMed] [Google Scholar]
- 17.Paley D. Problems, obstacles and complications of limb lengthening by the Ilizarov technique. Clin Orthop Relat Res. 1990;250:81–104. [PubMed] [Google Scholar]
- 18.Paley D. Principles of Deformity Correction. Berlin, Germany: Springer; 2002. [Google Scholar]
- 19.Paley D, Catagni MA, Argnani F, Villa A, Benedetti GB, Cattaneo R. Ilizarov treatment of tibial nonunions with bone loss. Clin Orthop Relat Res. 1989;241:146–165. [PubMed] [Google Scholar]
- 20.Paley D, Herzenberg JE, Paremain G, Bhave A. Femoral lengthening over an intramedullary nail. A matched-case comparison with Ilizarov femoral lengthening. J Bone Joint Surg Am. 1997;79:1464–1480. doi: 10.2106/00004623-199710000-00003. [DOI] [PubMed] [Google Scholar]
- 21.Papineau LJ, Alfageme A, Dolcourt JP, Pilon L. Chronic osteomyelitis: open excision and grafting after saucerization. Int Orthop. 1979;3:165–176. doi: 10.1007/BF00265708. [DOI] [PubMed] [Google Scholar]
- 22.Rozbruch RS, Pugsley JS, Fragomen AT, Ilizarov S. Repair of tibial nonunions and bone defects with the Taylor Spatial Frame. J Orthop Trauma. 2008;22:88–95. doi: 10.1097/BOT.0b013e318162ab49. [DOI] [PubMed] [Google Scholar]
- 23.Rozbruch RS, Weitzman AM. Tracey Watson J, Freudigman P, Katz HV, Ilizarov S. Simultaneous treatment of tibial bone and soft-tissue defects with the Ilizarov method. J Orthop Trauma. 2006;20:197–205. doi: 10.1097/00005131-200603000-00006. [DOI] [PubMed] [Google Scholar]
- 24.Sala F, Thabet AM, Castelli F, Miller AN, Capitani D, Lovisetti G, Talamonti T, Singh S. Bone transport for postinfectious segmental tibial bone defects with a combined Ilizarov/Taylor spatial frame technique. J Orthop Trauma. 2011;25:162–168. doi: 10.1097/BOT.0b013e3181e5e160. [DOI] [PubMed] [Google Scholar]
- 25.Saleh M, Rees A. Bifocal surgery for deformity and bone loss after lowerlimb fractures. comparison of bone-transport and compression-distraction methods. J Bone Joint Surg Br. 1995;77:429–434. [PubMed] [Google Scholar]
- 26.Salis de Gauzag J, Vidal H, Cahuzac JP. Primary shortening followed by callus distraction for the treatment of a posttraumatic bone defects, case report. J Trauma. 1993;34:461–463. doi: 10.1097/00005373-199303000-00031. [DOI] [PubMed] [Google Scholar]
- 27.Sen C, Eralp L, Gunes T, Erdem M, Ozden VE, Kocaoglu M. An alternative method for the treatment of nonunion of the tibia with bone loss. J Bone Joint Surg Br. 2006;88:783–789. doi: 10.1302/0301-620X.88B6.17515. [DOI] [PubMed] [Google Scholar]
- 28.Sen C, Kocaoglu M, Eralp L, Gulsen M, Cinar M. Bifocal compression-distraction in the acute treatment of grade III open tibia fractures with bone and soft-tissue loss: a report of 24 cases. J Orthop Trauma. 2004;18:150–157. doi: 10.1097/00005131-200403000-00005. [DOI] [PubMed] [Google Scholar]
- 29.Tetsworth K, Cierny G., 3rd Osteomyelitis debridement techniques. Clin Orthop Relat Res. 1999;360:87–96. doi: 10.1097/00003086-199903000-00011. [DOI] [PubMed] [Google Scholar]