Abstract
Background
Wear and corrosion occurring in patients with hip and knee arthroplasty are common causes of failure leading to revision surgery. A variety of surgical approaches to these problems have been described, with varying efficacy. Polyethylene wear, metal-on-metal (MoM) hip bearing wear, and problems associated with modular taper corrosion are the areas of greatest clinical impact; results of revisions for these problems are likely to dictate a large portion of revision resources for the foreseeable future, and so they call for specific study.
Questions/purposes
We identified the most frequently reported procedures to treat hip polyethylene wear, knee polyethylene wear, MoM wear after THA, and modular taper corrosion and determined the timing and reasons these failed.
Methods
We performed systematic reviews of the published literature on the four topics using MEDLINE® and Embase in October 2013; searches were supplemented by hand searches of bibliographies. Prespecified criteria resulted in the identification of 38 relevant articles, of which 33 were either case reports or Level IV evidence. Followup was generally at short term and ranged from 0.2 to 8 years.
Results
The most frequently reported procedures for treating clinically important wear were a partial or complete revision. When treating polyethylene wear, the more frequently reported reasons for hip and knee rerevisions were loosening, continued wear, and instability. Soft tissue reactions were more common and occasionally extensive in patients with MoM or modular taper corrosion. Patients with soft tissue reactions had more complications and higher rerevision rates.
Conclusions
Studies with longer followup and higher levels of evidence are needed to direct the treatment of wear and corrosion. When soft tissue damage secondary to MoM wear or taper corrosion is present, the results of treatment can be poor. There is an urgent need to better understand these two mechanisms of failure.
Introduction
The treatment options available for wear or corrosion with or without osteolysis generally involve surgery and can include either partial or complete revision. The current areas of interest include polyethylene wear in hip and knee implants, metal wear in metal-on-metal (MoM) bearing hips, and corrosion in THA. Each of these areas of interest presents unique problems even though the surgical options sometimes are similar. Wear and osteolysis associated with polyethylene generally are late problems and can cause synovitis, instability, and loosening, although many patients will be asymptomatic and their osteolysis will be detected only on surveillance radiographs obtained at routine followup. Clinical decision making for patients with MoM bearings is more complex than for those with polyethylene bearing implants. The problematic hip resurfacing (HR) or MoM stemmed THA may present with pain and altered function, either with or without elevation of serum markers for metal [28]. In addition, there have been reported cases of patients presenting with systemic symptoms that have been ultimately attributable to the MoM bearing and marked elevation of metal levels [41]. In many cases, cross-sectional imaging depicts destruction of the soft tissue envelope around the joint and, in some cases, periprosthetic bone loss [24]. While corrosion of modular junctions is not a new finding, its contribution to failed arthroplasties seems to be on the rise. Multiple theories have been proposed for the apparent increase, including increased use of larger-diameter heads, modular adaptors with the larger heads, smaller and shorter tapers, poor assembly, and component metallurgy issues [9, 10, 23, 29, 42, 47]. In each instance, the underlying process leading to corrosion appears to be mechanically assisted crevice corrosion generating particulate debris. These failures occur early, can cause severe soft tissue damage, and present different options depending on the type of implant that fails.
Treatment options for these conditions are generally similar in that there are few suitable nonsurgical options other than observation in selected circumstances. For those patients with severe polyethylene wear, synovitis, or late instability, the surgical options are liner exchange and partial or full revision, while patients with loosening secondary to wear and osteolysis usually undergo revision of the loose component. Surgical options for treatment of most MoM THAs will be guided by the cause of failure that is identified but generally will center on acetabular revision; however, there is a subset of MoM THAs that have a modular metal insert that can be treated with an insert exchange. When corrosion at a total hip taper leads to revision, options are a femoral head exchange (even retaining a corroded femoral stem because of the morbidity associated with removal of a well-fixed femoral component) or a complete femoral revision. However, it is unclear the degree to which each of these approaches is used and, more importantly, how effective each one is.
We therefore performed a systematic review of the literature to identify the most frequently reported procedures to treat (1) hip polyethylene wear, (2) knee polyethylene wear, (3) MoM wear after THA, and (4) modular taper corrosion and to determine the timing and reasons these failed.
Search Strategy and Criteria
We performed four different searches on the MEDLINE® and Embase databases in October 2013. Studies were included only if they were peer reviewed and reported clinical outcome and type of treatment. Titles were screened to eliminate articles not associated with the implant system (hip or knee) searched or unrelated to either wear or treatment. A final screen was done of the abstract and when necessary the manuscript to eliminate review articles, articles in which the treatment was not specified, and articles with no outcome data. Search terms for the systematic reviews were agreed on by all authors and the analysis of search results was performed by one of the authors (HH). The bibliographies of the final articles were all searched for articles that might have been missed by the initial query. The search terms and reasons for exclusion of articles are summarized in selection flowcharts (Figs. 1–4).
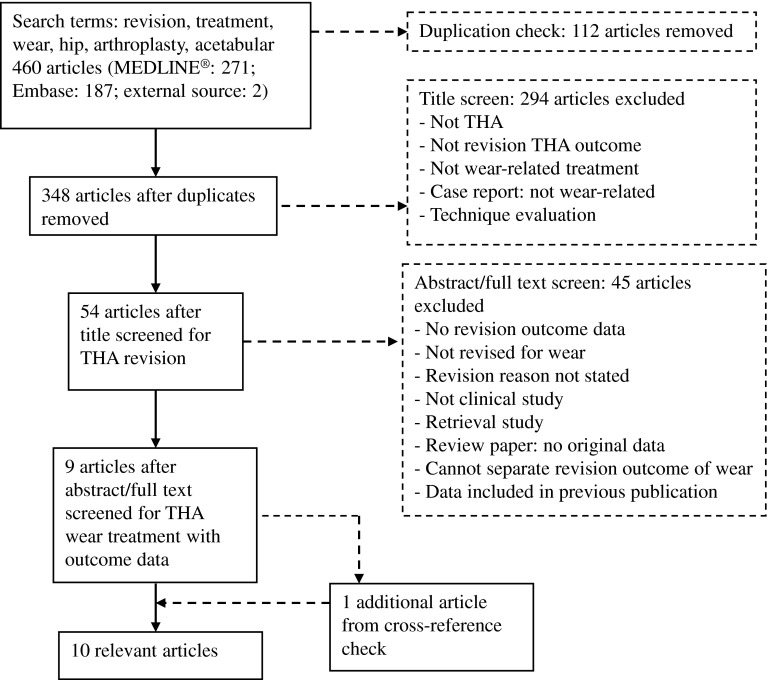
Fig. 1.
A flow diagram shows the method of article selection for review of articles reporting on hip polyethylene wear.
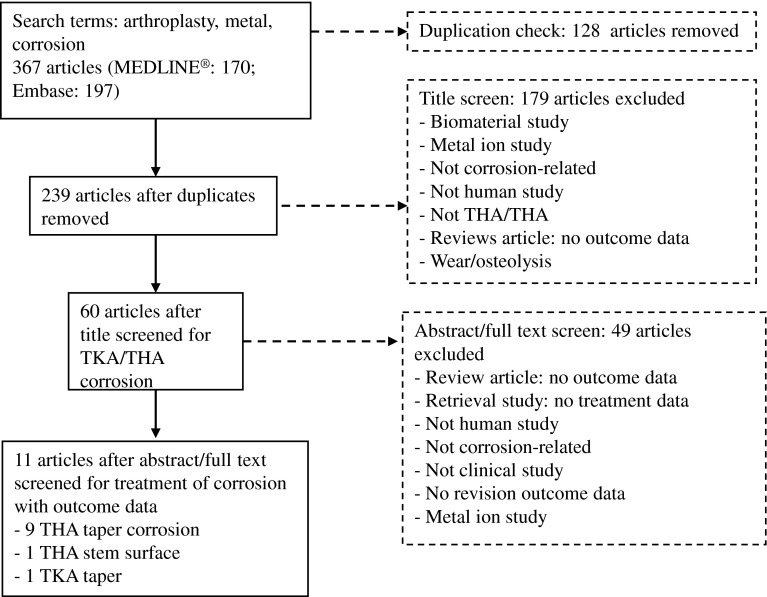
Fig. 4.
A flow diagram shows the method of article selection for review of articles reporting on taper corrosion.
For polyethylene wear in the hip, the search terms were “revision”, “treatment”, “wear”, “hip”, “arthroplasty”, and “acetabular”. We did not search for femoral results because virtually all late hip failures related to wear in the presence of stable implants do not require femoral revision. We focused on stable implants because it is difficult to determine when loosening is caused solely by wear. Nine articles remained after 460 were screened. One additional article was identified during the review of the bibliographies from the nine articles, resulting in a total of 10 articles for this topic [5, 6, 19, 21, 25, 31, 36, 39, 40, 45] (Fig. 1).
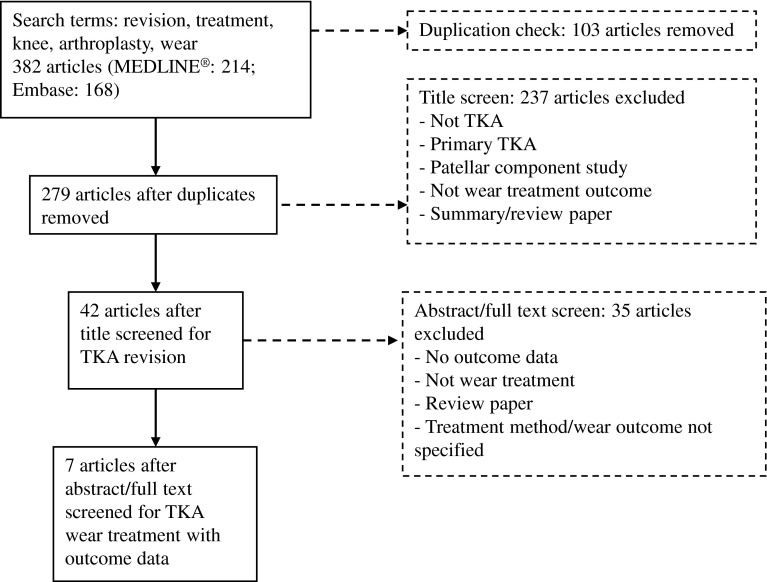
For polyethylene wear in the knee, the search terms included “revision”, “treatment”, “knee”, “arthroplasty”, and “wear”. Seven articles remained after 382 were screened [2, 3, 8, 14, 15, 20, 27] (Fig. 2).
Fig. 2.
A flow diagram shows the method of article selection for review of articles reporting on knee polyethylene wear.
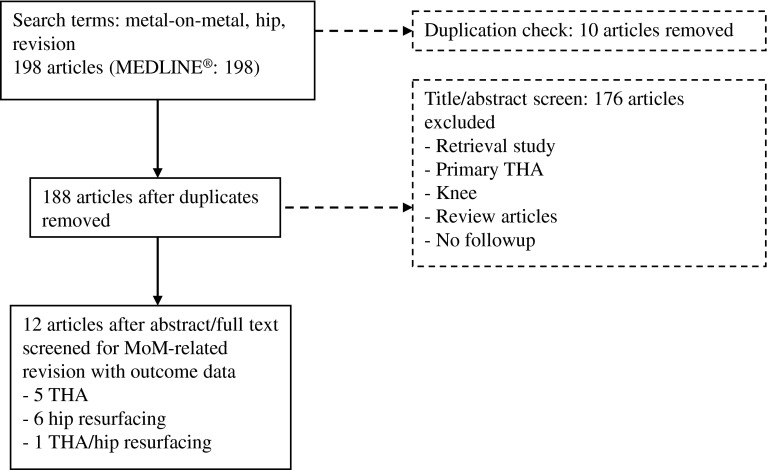
For MoM wear, the search terms were “metal-on-metal”, “hip”, and “revision”. Twelve articles remained after 198 articles were screened [4, 11, 12, 18, 24, 28, 30, 34, 38, 43, 44, 48] (Fig. 3).
Fig. 3.
A flow diagram shows the method of article selection for review of articles reporting on MoM wear.
For corrosion, the search terms included “metal”, “corrosion”, and “arthroplasty”. Eleven articles remained after 367 were screened (Fig. 4). Two of the final articles were removed because they addressed corrosion secondary to stem loosening and a knee modular revision component. This left nine articles focused on corrosion in femoral hip components [9, 10, 23, 29, 32, 37, 42, 46, 47].
The quality of the included articles was measured by the level of evidence as reported by the studies themselves.
Results
Polyethylene Wear in the Hip
The most frequently reported procedures for treating hip polyethylene wear with or without osteolysis were cup revision and isolated polyethylene exchange (Table 1) [5, 6, 19, 21, 25, 31, 36, 39, 40, 45]. The mean followup in these articles ranged from 2.5 to 4.8 years. Of the 10 studies identified addressing the frequent procedures used to treat total hip polyethylene wear, eight were Level IV and one each was a Level II and III.
Table 1.
Summary of articles included in the hip polyethylene wear review
| Study | Level of evidence | Number of patients revised for wear | Revision reason | Number of revised components | Followup (years) | Outcomes | Complications |
|---|---|---|---|---|---|---|---|
| Hamilton et al. [21] | IV | 187 | Polyethylene wear and osteolysis | 187 PE | 4.2 | 25 rerevisions at mean 2.3 years; survival rate: 87% at 5 years | 10 instability, 9 cup loosening, 3 recurrence of excessive wear or osteolysis, 2 infection, 1 dissociation of the replaced liner |
| Griffin et al. [19] | IV | 55 | Accelerated polyethylene wear and osteolysis | 55 PE | 2.5 | 6 rerevisions; time to rerevision not reported | 3 instability, 2 femoral implant fracture and bone loss; 1 cup fail into lesion |
| Wade et al. [45] | IV | 35 | Polyethylene wear and osteolysis/instability | 35 PE | 2.6 | None rerevised | 2 instability |
| O’Brien et al. [36] | IV | 24 | Polyethylene wear and acetabular osteolysis | 24 PE | 3 | 2 rerevisions at mean 3.75 years | 1 loose cup; 1 accelerated polyethylene wear; all scores improved postoperatively; no dislocations |
| Boucher et al. [6] | IV | 24 | Wear and osteolysis | 24 PE | 4.5 | 3 rerevisions at mean 6.5 years | 2 revised for instability; 1 cup loose |
| Schelfaut et al. [40] | IV | 14 | Acetabular bone loss wear | 14 CR | 3.6 | 4 rerevisions at mean 2.7 years; survival rate: 67.1% at 42 months | 3 allograft fragmentation with collapse of total construction; 1 instability; 9 good clinical result |
| Koh et al. [25] | IV | 80 | Polyethylene wear and osteolysis without cup loosening | 45 CR 35 PE |
4.3 | 1 rerevision in CR group and 2 rerevisions in PE group; time to rerevision not reported | 1 loose cup in CR group; 1 accelerated wear; 1 instability in PE group |
| Maloney et al. [31] | III | 68 | Osteolysis in the pelvis and polyethylene wear | 28 CR 40 PE |
3.5 | None rerevised | Successful in arresting the process of osteolysis |
| Restrepo et al. [39] | II | 67 | Polyethylene wear and osteolysis | 31 CR 36 PE |
2.8 | 1 rerevision in CR group at 0.4 years and 3 rerevisions in PE group at mean 2.9 years | Cup loosening is the only reason to revise |
| Blom et al. [5] | IV | 38 | Polyethylene wear | 25 CR 13 PE |
4.8 | 3 rerevisions in CR group; survival rate: 92.1% at under 5 years | 1 instability, 1 loose stem, 1 periprosthetic fracture in CR group |
PE = polyethylene exchange; CR = cup revision.
When a cup revision was done to treat wear, a common mechanism of failure leading to rerevision was aseptic acetabular loosening reported to occur between 0.4 and 2.7 years after the initial revision [25, 39, 40]. Recurrent dislocation was also reported as a failure mode in two articles [5, 40]. Only one of those reported the timing, which was 2.7 years after the initial revision [40]. When a polyethylene exchange was done to treat hip wear, the reasons for failure included recurrent dislocation, acetabular loosening, and polyethylene wear. Six articles reported recurrent dislocation rerevision rates from 0% to 8% [5, 6, 19, 21, 25, 31]. Two of the articles reported a time frame for these rerevisions of 2.3 to 6.5 years [6, 21]. Seven articles reported rerevisions for aseptic cup loosening after the initial polyethylene exchange was done, with rates ranging from 0% to 8% [5, 6, 19, 21, 31, 36, 39]. Four of the articles mentioned the timing of the rerevisions, which ranged from 2.3 to 6.5 years after the initial polyethylene exchange [6, 21, 36, 39].
Polyethylene Wear in the Knee
The most frequently reported methods for treating total knee wear with or without osteolysis were polyethylene exchange, full revision, or partial revision (Table 2) [2, 3, 8, 14, 15, 20, 27]. The mean followup in these articles ranged from 3.7 to 8.1 years. Of the seven studies identified addressing the frequent procedures used to treat total knee polyethylene wear, six were Level IV and one was Level III.
Table 2.
Summary of articles included in the knee polyethylene wear review
| Study | Level of evidence | Number of patients revised for wear | Revision reason | Number of revised components | Followup (years) | Outcomes | Complications |
|---|---|---|---|---|---|---|---|
| Griffin et al. [20] | IV | 68 | Polyethylene wear | 68 PE | 3.7 | 11 rerevisions; time to revision not reported | 10 septic loosening, 1 infection |
| Engh et al. [15] | IV | 48 | Polyethylene wear | 48 PE | 7.4 | 8 rerevisions at mean 4.5 years | 7 accelerated wear, 1 instability |
| Callaghan et al. [8] | IV | 25 | Polyethylene wear and osteolysis | 25 PE | 5.3 | 1 rerevision at mean 5.1 years | 1 aseptic loosening |
| Babis et al. [2] | III | 24 | Polyethylene wear | 24 PE | 4.6 | 5 rerevisions at mean 4 years; survival rate: 76% at 5.5 years | 4 accelerated wear, 1 pain, 1 other |
| Lachiewicz and Soileau [27] | IV | 12 | Polyethylene wear | 12 PE | 4.3 | None revised | |
| Bae et al. [3] | IV | 110 | Polyethylene wear | 119 complete revision | 8.1 | 9 rerevisions at mean 7.2 years | 2 accelerated wear, 2 loose, 4 infection, 1 periprosthetic fracture |
| Engh et al. [14] | IV | 119 | Polyethylene wear | 31 PE | 4.6 | 7 rerevisions at mean 4.7 years | 1 loose tibia, 4 accelerated wear, 1 osteolysis/fracture, 1 wear instability |
| 39 complete revision | 4 rerevisions at mean 2.7 years | 1 infection, 1 loose femur, 1 pain, 1 unknown | |||||
| 49 partial revision | 6 rerevisions at mean 5.3 years | 1 infection, 2 lysis, 1 wear/instability, 1 wear, 1 loose tibia |
PE = polyethylene exchange.
When a polyethylene exchange was done, four articles reported rerevisions for loosening of the retained tibial or femoral component, with rates ranging from 0% to 8% and occurring from 4.5 to 5.5 years [2, 8, 14, 20]. Three articles reported recurrent wear as a cause of failure, with rates ranging from 13% to 17% and occurring 4.5 to 5.5 years after the polyethylene exchange [2, 14, 15]. One of these articles emphasized a reduced rerevision for polyethylene wear when newer non-gamma-in-air-sterilized polyethylene revision inserts were used [14]. One paper reported 49 partial revisions initially done with 6% rerevised for wear or osteolysis and 2% rerevised for loosening [14]. The timing of these rerevisions was a mean of 5.3 years after the initial revision. The one article that reported complete revisions as a treatment had 119 revisions with 2% of failures from continued wear and 2% for loosening [3]. The revisions occurred at a mean 7.2 years after the initial revision.
MoM Wear in THA/HR
Because stemmed MoM THA and MoM HR are very different procedures with different surgical options, they are presented separately. The most frequently reported methods for treating a failed stemmed MoM THA were acetabular revision for modular and nonmodular acetabular components, liner insert exchange for modular acetabular components, and full revision of the femoral and acetabular components (Table 3) [4, 24, 28, 30, 34, 48]. The mean followup for these articles ranged from 3 to 33 months. Of the six studies identified addressing the frequent procedures used to treat failure of stemmed MoM THA, four were Level IV and two were Level II.
Table 3.
Summary of articles included in the MoM THA review
| Study | Level of evidence | Number of patients | Revision reason | Number of revised components | New bearing | Followup (months) | Outcomes | Complications |
|---|---|---|---|---|---|---|---|---|
| Wyles et al. [48] | IV | 37 | 19 loose 8 ALTR 4 periprosthetic fracture 3 impingement 2 dislocation 1 unknown pain |
25 CR 7 liner/head exchange 3 complete revision 2 stem revision |
Mostly COP | 33 | 95% survivorship | 3 infections (10%) |
| Munro et al. [34] | IV | 32 | 19 ALTR 10 loose Cups, 3 infection |
31 CR 1 complete revision |
MOP | 25 | 3 new pseudotumor (1 ceramic, 2 metal) | 38% complications; 28% dislocation; 13% failure of cup to ingrow (all fiber mesh cups) |
| Ball et al. [4] | II | 25 | Elevated metal ions | All complete revision | MOP | 3 | 90% return to baseline; more severe elevation, returned slower | Not reported |
| Maezawa et al. [30] | IV | 10 | Loose cups/ions | All liner exchange only | MOP | 6 | Normalization of ions | None |
| Kemp et al. [24] | IV | 3 | Pseudotumor | All complete revision | COC | 8 | Pseudotumor size decrease | None |
| Liddle et al. [28] | II | 32 (hip resurfacing) 7 (THA) |
8 infection 14 synovitis 6 cystic pseudotumors 4 solid pseudotumors 7 osteolysis (reasons not distinguished between THA and hip resurfacing) |
5 complete revision 2 CR |
MOP/COP | 19 | Worse outcomes in solid pseudotumor group | 2 reoperations both in the solid pseudotumor group |
MoM = metal-on-metal; ALTR = adverse local tissue reaction; CR = cup revision; COP = ceramic-on-polyethylene; MOP = metal-on-polyethylene; COC = ceramic-on-ceramic.
Acetabular revision was the most commonly reported treatment [28, 34, 48]. Regardless of the surgical procedure, the majority of patients demonstrated improvements in their symptoms. For patients undergoing revision for elevated serum cobalt and chromium, there were two reports of normalization of blood levels with up to 90% return by 12 weeks [4, 30]. However, most other studies emphasized complications and rerevisions, especially when a pseudotumor was present [28, 34, 48]. One report demonstrated that revision surgery for solid pseudotumors had a poorer outcome as measured by Oxford Hip Score [28]. In a report by Munro et al. [34], three new pseudotumors developed after revision: two with metal-on-polyethylene implants and one with a ceramic-on-polyethylene implant. In addition, there was a 28% dislocation rate despite using head diameters of 36 mm or greater and a 13% cup loosening rate, which all occurred in new inserted sockets coupled with the so-called less highly porous metals, implying some effect on acetabular ingrowth potential. Lastly, Wyles et al. [48] noted that, while the vast majority of patients improved in their group of revisions, they noted an 8.1% infection rate, which is substantially higher than any other revision cohort reported from their institution.
The most frequently reported surgical treatment for failed MoM HR was a complete revision followed by a femoral revision (Table 4) [11, 12, 18, 28, 38, 43, 44]. Complete revisions resulted in placement of a stemmed THA with the predominant use of a ceramic-on-polyethylene bearing. One series reported on the outcome of single-component revision [38], and in this series, almost ½ of the patients retained MoM bearings. Of the seven studies identified addressing the frequent procedures used to treat failure of MoM HR, five were Level IV, one was Level II, and one was a case study.
Table 4.
Summary of articles included in the MoM hip resurfacing review
| Study | Level of evidence | Number of patients | Revision reason | Number of revised components | New bearing | Followup (months) | Outcomes | Complications |
|---|---|---|---|---|---|---|---|---|
| Verhelst et al. [44] | Case study | 3 | Elevated ions level | New stem, retained cup | MOP | 6 | Normal metal ions; HOOS increase | Not reported |
| De Haan et al. [11] | IV | 42 | Malpositioning/wear | Cup/stem | COC/MoM | 26 | Not reported | 4 (10%) dislocation, 3 due to lysis; 3 reoperations related to cup component |
| Van der Weegen et al. [43] | IV | 5 | Severe pseudotumor | Cup/stem | COP | 2 | Metal ion levels dropped 6 weeks after revision surgery | None reported |
| Pritchett [38] | IV | 90 | ALTR to wear debris | 76 cup 14 femur |
47 MOP 43 MoM |
61 | Single-component revision is alternative to THA | 3 revisions include 1 deep infection |
| Grammatopoulos et al. [18] | IV | 53 | 16 pseudotumor | Pseudotumor group: cup/stem revised |
8 COC 6 COP 2 MOP |
36 | Worse outcomes in pseudotumor group | Pseudotumor group: 3 dislocation; 3 nerve palsy; 6 reoperation |
| De Smet et al. [12] | IV | 113 | 48 soft tissue reaction | 72% complete revision | COP mostly | 43 | Poorer results in single-component revision | 6 (5%) dislocation; extensive débridement of pseudocapsule likely more complications |
| Liddle et al. [28] | II | 32 (hip resurfacing) 7 (THA) |
8 infections 14 synovitis 6 cystic pseudotumors 4 solid pseudotumors 7 osteolysis (reasons not distinguished between THA and hip resurfacing) |
Cup/stem for all but 2 | MOP/COP | 19 | Worse outcomes in solid pseudotumor group | 2 revisions in the solid pseudotumor group |
MoM = metal-on-metal; ALTR = adverse local tissue reaction; MOP = metal-on-polyethylene; COC = ceramic-on-ceramic; COP = ceramic-on-polyethylene; HOOS = Hip Disability and Osteoarthritis Outcome Score.
In the single series performing revision for elevated metal ions, Velherst et al. [44] demonstrated that conversion to a stemmed THA with a dual-mobility bearing led to the normalization of serum ions by 6 months. Most of the series suggest that patient clinical improvement is seen whether revision is of one or both components. However, the 2013 report of the Australian Orthopaedic Association National Joint Replacement Registry [1], which has data through December 2012, suggests that revision of failed HR has a high rerevision rate as seen at 1, 3, and 5 years. Of the types of revision possible, both single-component revision and major revision were associated with substantial rerevision rates at 3 years (acetabular only 16.2%, femoral only 9.2%) compared with major revision (acetabular and femoral 8.0%) and up to 14.4% at 5 years. As seen in the revision stemmed MoM THA, dislocation rates remain high [11, 12, 18]. Also, revisions performed for adverse local tissue reaction and pseudotumors did poorer than revisions for other indications such as fracture or component malposition [18]. In the series by De Smet et al. [12], the authors discussed the issue of extent of débridement of pseudotumor at the time of revision. While specific guidelines were not proposed, the authors stated that, early in their experience, they were more radical in soft tissue débridement whereupon they noted a higher rate of complications. They have since advocated that soft tissue débridement be more limited to obvious necrotic tissue.
Treatment of Corrosion
There were nine studies identified addressing the surgical treatment of implant failures secondary to taper corrosion (Table 5) [9, 10, 23, 29, 32, 37, 42, 46, 47]. Eight articles were case report studies and one was Level IV. The followup reported in the articles was very short, ranging from 1 to 36 months.
Table 5.
Summary of articles included in the corrosion review
| Study | Level of evidence | Number of patients revised for wear | Bearing/diameter (mm) | Index to revision (years) | Corrosion location | Treatment | Followup (months) | Outcomes/complications |
|---|---|---|---|---|---|---|---|---|
| Cooper et al. [10] | IV | 10 | MOP/28–40 | 3.91 | Head-neck junction | All treated with débridement and a femoral head and liner exchange, with use of a ceramic femoral head with a titanium sleeve; 2 with cup revision because of loosening and malposition | 13 | Mean Harris hip score improved at 13 months after the revision surgery; repeat serum cobalt levels, measured in six patients, decreased and chromium levels similar to prerevision levels 8 months after revision; 1 rerevision because patient with moderate hip abductor muscle necrosis developed recurrent instability |
| Lindgren et al. [29] | Case report | 1 | MOP/28 | 2.8 | Head-neck junction | Extended trochanteric osteotomy performed to remove the femoral component; a constrained acetabular insert in the Trident® shell, a stainless steel Exeter® stem with a 22-mm head cemented in place; stainless steel chosen to eliminate exposure to cobalt | 6 | Infection developed postoperatively; 6 months after this operation, patient was not considered free of infection and a new prosthesis has not been implanted |
| Whitehouse et al. [47] | Case report | 1 | Unipolar modular hip hemiarthroplasty | 5 | Head-neck junction | Thorough débridement performed; cup revised and well-fixed stem retained; cobalt-chrome head used; cavitary lesion débrided and packed with bone graft | < 12 | At followup, patient’s pain and stiffness had resolved, although he still had some abductor weakness and is continuing physiotherapy |
| Scully and Teeny [42] | Case report | 1 | MOP/32 | 7 | Head-neck junction | Metallic head replaced with a ceramic component; polyethylene liner exchanged | 1 | Patient had complete resolution of his preoperative symptoms but had persistent problems with dislocations |
| Mao et al. [32] | Case report | 1 | MOP/32 | 7 | Head-neck junction | Articulating surfaces subsequently replaced with a 32-mm ceramic head and corresponding ceramic acetabular liner | 9 | Patient remained systematically well and pain free, with no recurrence of the bursa cyst on clinical examination |
| Pansard et al. [37] | Case report | 1 | MoM/46 | 2 | Junction at head connected to the adaptor sleeve | Revision required femoral stem exchange because of the damage to the Morse taper; cup replaced with new MoM bearings | 36 | Favorable |
| Chana et al. [9] | Case report | 1 | BHR®/50 | 4 | Junction at head connected to the adaptor sleeve | Thickened, indurated cyst measuring 8 cm × 3 cm × 8 cm with a gray-stained wall, posterolateral to the greater trochanter, excised; stem not revised, converted to COC/36 | 6 | At 6 months’ followup, patient was mobilizing unaided and free of pain |
| Hsu et al. [23] | Case report | 1 | COP/44 | 1 | Stem-neck taper junction | Extended trochanteric osteotomy; long-stem revision femoral component; head/liner exchange | 9 | At 9 months from revision surgery, patient had continued improvements in function and Harris hip score; serum levels of cobalt, chromium, and titanium decreased |
| Werner et al. [46] | Case report | 1 | MOP/40 | 0.5 | Stem-neck taper junction | Extensive débridement; cup retained; femoral component revised to a modular tapered titanium revision prosthesis and 36-mm ceramic head | Not reported | After the procedure, patient experienced immediate and sustained relief of her lateral hip and groin pain, improved ambulation and function, and no perioperative complications |
| 1 | MOP/40 | 0.9 | Stem-neck taper junction | Same as above | Not reported | After revision, patient had remarkable and nearly instantaneous relief of his preoperative pain with an uncomplicated recovery |
MOP = metal-on-polyethylene; MoM = metal-on-metal; BHR® = Birmingham Hip® Resurfacing; COP = ceramic-on-polyethylene; COC = ceramic-on-ceramic.
Of the 19 bearings reported, 15 were metal-on-polyethylene (two dual-modular necks), one ceramic-on-polyethylene (one dual-modular neck), and three MoM (two adaptor sleeves of titanium, one modular unipolar). Bearing diameters ranged from 28 to 54 mm, with the majority being 28 and 32 mm. On analyzing head-neck junctions, there were nine cobalt chrome-titanium, seven cobalt chrome-cobalt chrome, and three modular necks. Bearing combinations included 15 metal-on-polyethylene, three MoM, and one ceramic-on-polyethylene bearings. The vast majority of revision procedures were stem retention with head and liner exchange. When the stem was retained, a ceramic head with titanium adaptor sleeve was almost always used. Most of the femoral revisions performed were for dual-modular neck implants with corrosion. Regardless of the procedure, the majority of patients reported pain relief and there were no reports of recurrence of symptoms. When metal levels were tested postoperatively, levels trended toward normal between 8 and 9 months of followup.
Discussion
Because wear debris can lead to failure of hip and knee arthroplasty, there is continued interest in polyethylene wear in hip and knee implants, MoM hip wear, and modular junction corrosion in THA. Each of these areas of interest presents unique problems, although the surgical treatment options are similar. Wear and osteolysis secondary to polyethylene debris are typically late problems and are often asymptomatic even when there is extensive bone loss. In contrast, problems related to MoM wear and modular junction corrosion appear to occur earlier and are often associated with substantial soft tissue damage. Even though the areas of interest are similar in that they occur secondary to wear debris and the surgical treatment options are similar (partial or complete revision), the literature is unclear as to the best surgical treatment in each area of interest and the reasons for failure of that treatment. We therefore performed systematic reviews and analyses of the resulting articles on four topics: polyethylene wear of hip and knee arthroplasty, MoM hip wear, and modular taper corrosion. Our purposes were to identify the most frequently reported procedures to treat hip polyethylene wear, knee polyethylene wear, MoM wear after THA, and taper corrosion and to determine the timing and reasons these failed.
The main limitation of our analysis is the absence of studies with a high level of evidence. Thirty-three of the 38 articles that comprised the analysis of our four reviews had Level IV evidence or were case reports (n = 8, about corrosion treatment). Studies with higher levels of evidence may become available as national registries compile more data on the results of revision. However, registries have not commonly addressed patient function or radiographic outcomes of treatment for osteolysis. Another weakness of this study and the available literature is the short followup of the publications reviewed. The mean followup for polyethylene wear treatment studies ranged from 3 to 8 years. The MoM and corrosion treatment articles had an even shorter mean followup of 0.2 to 5 years. As the number of young patients undergoing arthroplasty increases, surgeons will need longer-term revision followup data to counsel these patients who will likely need revision in their lifetime.
Our analysis of surgical treatment options for patients who have polyethylene wear with or without osteolysis in the hip and knee confirmed that the options are isolated liner exchange or component revision. Because wear is a late complication of hip and knee arthroplasty occurring in patients with functioning implants, there has been a tendency to perform an isolated liner exchange because the procedure is easier and quicker and does not result in additional bone loss. The key unanswered question relating to the treatment of polyethylene wear is the impact crosslinked polyethylene will have on the occurrence of wear as a problem and the outcome of revisions in which crosslinked polyethylene is used. Recent publications have shown an absence of hip osteolysis and wear-related revisions at 7 to 10 years [7, 13, 33]. One of the main causes of hip revisions for wear identified in our review is recurrent dislocation. Crosslinked polyethylene has allowed the use of larger-head diameters in revision hip surgery and there is evidence that the larger heads have a lower dislocation rate [17]. Some of the knee polyethylene wear studies we identified indicated that continued wear occurring after revision was a failure mode. One of the knee studies we identified demonstrated fewer rerevisions when non-gamma-in-air polyethylene was used as the revision insert, thus implicating polyethylene quality as a cause of failure [14]. Since most of the articles we identified predated the use of crosslinked polyethylene in revision hip and knee surgery, readers should continue to monitor reports in which crosslinked polyethylene is used for revision hip and knee surgery.
The results treating MoM bearings and corrosion are less specific than those for polyethylene wear because these problems are newer and not as well understood and importantly these failures seem to have a much higher frequency of major soft tissue damage. The relative novelty of MoM and corrosion-related failures is evidenced by the short length of followup and the high number of simple case reports in our analysis. Our analyses reveal that, for surgical treatment for MoM wear and corrosion, once the diagnosis has been made, surgical intervention can achieve clinical improvement. However, it is also clear that, when a patient has a large amount of tissue damage, there will be more complications and a higher reoperation rate. This observation implies that earlier recognition of the clinical entity and diagnosis prompting earlier intervention may play a role in reducing the complications associated with wear and corrosion. Current research is focusing on routine use of three-dimensional imaging to diagnose corrosion and MoM wear problems before there is extensive soft tissue damage [16, 35]. Many of the studies we identified also mentioned the use of metal level testing. Currently, there are efforts focusing on management of patients with MoM implants that include guidelines for the use and importance of metal levels that will help surgeons counsel patients and use the levels as one of many tools to help determine when to intervene [22, 26]. Lastly, the one case series on corrosion is interesting because it highlights the relative increase in cobalt levels compared to chromium levels in situations where corrosion is the process driving particle generation and failure [10]. This article will be helpful as surgeons evaluate patients with pain and have an implant with a modular junction.
In conclusion, polyethylene wear failures are likely going to decrease because of the advent of crosslinked polyethylene used at the index arthroplasty. In addition, the results of surgical treatment of polyethylene wear will likely improve because of the improved wear resistance of crosslinked polyethylene used at revision and the corresponding acceptance of larger-diameter heads used in hip revision, which has decreased revision hip instability. In contrast, because of the large number of MoM bearings that remain in service, MoM failures will continue to need surgical treatment. Early intervention algorithms and diagnostic tools are needed to minimize the soft tissue damage and therefore improve surgical outcomes. However, this issue is likely to decline over time, as the usage of MoM bearings in THA has decreased substantially. Corrosion is a problem that seems to be reoccurring. While it is not entirely clear why corrosion-related failures are reoccurring, there is some evidence that it may be related to larger-diameter heads placed on smaller tapers, which can create and increase moment on the taper, resulting in mechanically assisted corrosion; however, there have been cases of trunnion-related corrosion observed in traditional head sizes of 28 and 32 mm. While taper specifications may have changed, new metals are being used, and surgeons may not be assembling modular implants using ideal techniques, the exact mechanism by which this phenomenon is occurring is still unknown. Awareness of this problem combined with the use of three-dimensional imaging and metal levels should allow for timely intervention, which is important, since current treatment of these patients has demonstrated a high frequency of major soft tissue disruption among patients with corrosion-related complications from MoM bearings or corrosion at modular junctions.
Footnotes
The institution of one or more of the authors has received, during the study period, funding from Inova Health Care Services (Falls Church, VA, USA) (CAE Jr, HH). One of the authors (CAE Jr) certifies that he or she, or a member of his or her immediate family, has received or may receive payments or benefits, during the study period, an amount of USD (USD 10,000 to USD 100,000), from DePuy Orthopaedics Inc (Warsaw, IN, USA). One of the authors (DEP) certifies that he or she, or a member of his or her immediate family, has received or may receive payments or benefits, during the study period, an amount of USD (USD 100,001 to USD 1,000,000), from Mako Surgical Corp (Fort Lauderdale, FL, USA).
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research ® editors and board members are on file with the publication and can be viewed on request.
Clinical Orthopaedics and Related Research ® neither advocates nor endorses the use of any treatment, drug, or device. Readers are encouraged to always seek additional information, including FDA approval status, of any drug or device before clinical use.
This work was performed at Anderson Orthopaedic Research Institute, Alexandria, VA, USA, and Hospital for Special Surgery, New York, NY, USA.
References
- 1.Australian Orthopaedic Association National Joint Replacement Registry. Revision of hip and knee arthroplasty. Supplementary Reports 2013. Available at: https://aoanjrr.dmac.adelaide.edu.au/en/annual-reports-2013. Accessed December 2013.
- 2.Babis GC, Trousdale RT, Morrey BF. The effectiveness of isolated tibial insert exchange in revision total knee arthroplasty. J Bone Joint Surg Am. 2002;84:64–68. doi: 10.2106/00004623-200201000-00010. [DOI] [PubMed] [Google Scholar]
- 3.Bae DK, Song SJ, Heo DB, Lee SH, Song WJ. Long-term survival rate of implants and modes of failure after revision total knee arthroplasty by a single surgeon. J Arthroplasty. 2013;28:1130–1134. doi: 10.1016/j.arth.2012.08.021. [DOI] [PubMed] [Google Scholar]
- 4.Ball ST, Severns D, Linn M, Meyer RS, Swenson FC. What happens to serum metal ion levels after a metal-on-metal bearing is removed? J Arthroplasty. 2013;28(8 suppl):53–55. doi: 10.1016/j.arth.2013.06.040. [DOI] [PubMed] [Google Scholar]
- 5.Blom AW, Astle L, Loveridge J, Learmonth ID. Revision of an acetabular liner has a high risk of dislocation. J Bone Joint Surg Br. 2005;87:1636–1638. doi: 10.1302/0301-620X.87B12.16349. [DOI] [PubMed] [Google Scholar]
- 6.Boucher HR, Lynch C, Young AM, Engh CA, Jr, Engh C., Sr Dislocation after polyethylene liner exchange in total hip arthroplasty. J Arthroplasty. 2003;18:654–657. doi: 10.1016/S0883-5403(03)00266-3. [DOI] [PubMed] [Google Scholar]
- 7.Bragdon C, Burke D, Ekeledo A, Freiberg A, Greene M, Harris W, Malchau H. Seven to ten year follow-up of highly cross-linked polyethylene liners in total hip arthroplasty. J Bone Joint Surg Br. 2010;92:511. [Google Scholar]
- 8.Callaghan JJ, Reynolds ER, Ting NT, Goetz DD, Clohisy JC, Maloney WJ. Liner exchange and bone grafting: rare option to treat wear and lysis of stable TKAs. Clin Orthop Relat Res. 2011;469:154–159. doi: 10.1007/s11999-010-1521-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Chana R, Esposito C, Campbell PA, Walter WK, Walter WL. Mixing and matching causing taper wear: corrosion associated with pseudotumour formation. J Bone Joint Surg Br. 2012;94:281–286. doi: 10.1302/0301-620X.94B2.27247. [DOI] [PubMed] [Google Scholar]
- 10.Cooper HJ, Della Valle CJ, Berger RA, Tetreault M, Paprosky WG, Sporer SM, Jacobs JJ. Corrosion at the head-neck taper as a cause for adverse local tissue reactions after total hip arthroplasty. J Bone Joint Surg Am. 2012;94:1655–1661. doi: 10.2106/JBJS.K.01352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.De Haan R, Campbell PA, Su EP, De Smet KA. Revision of metal-on-metal resurfacing arthroplasty of the hip: the influence of malpositioning of the components. J Bone Joint Surg Br. 2008;90:1158–1163. doi: 10.1302/0301-620X.90B9.19891. [DOI] [PubMed] [Google Scholar]
- 12.De Smet KA, Van Der Straeten C, Van Orsouw M, Doubi R, Backers K, Grammatopoulos G. Revisions of metal-on-metal hip resurfacing: lessons learned and improved outcome. Orthop Clin North Am. 2011;42:259–269. doi: 10.1016/j.ocl.2011.01.003. [DOI] [PubMed] [Google Scholar]
- 13.Engh CA Jr, Hopper RH Jr, Huynh C, Ho H, Sritulanondha S, Engh CA Sr. A prospective, randomized study of cross-linked and non-cross-linked polyethylene for total hip arthroplasty at 10-year follow-up. J Arthroplasty. 2012;27(8 suppl):2–7.e1. [DOI] [PubMed]
- 14.Engh CA, Jr, Parks NL, Engh GA. Polyethylene quality affects revision knee liner exchange survivorship. Clin Orthop Relat Res. 2012;470:193–198. doi: 10.1007/s11999-011-1997-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Engh GA, Koralewicz LM, Pereles TR. Clinical results of modular polyethylene insert exchange with retention of total knee arthroplasty components. J Bone Joint Surg Am. 2000;82:516–523. doi: 10.2106/00004623-200004000-00007. [DOI] [PubMed] [Google Scholar]
- 16.Garbuz DS, Hargreaves BA, Duncan CP, Masri BA, Wilson DR, Forster BB. The John Charnley Award. Diagnostic accuracy of MRI versus ultrasound for detecting pseudotumors in asymptomatic metal-on-metal THA. Clin Orthop Relat Res. 2014;472:417–423. doi: 10.1007/s11999-013-3181-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Garbuz DS, Masri BA, Duncan CP, Greidanus NV, Bohm ER, Petrak MJ, Della Valle CJ, Gross AE. The Frank Stinchfield Award. Dislocation in revision THA: do large heads (36 and 40 mm) result in reduced dislocation rates in a randomized clinical trial? Clin Orthop Relat Res. 2012;470:351–356. doi: 10.1007/s11999-011-2146-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Grammatopoulos G, Pandit H, Kwon YM, Gundle R, McLardy-Smith P, Beard DJ, Murray DW, Gill HS. Hip resurfacing revised for inflammatory pseudotumour have a poor outcome. J Bone Joint Surg Br. 2009;91:1019–1024. doi: 10.1302/0301-620X.91B8.22562. [DOI] [PubMed] [Google Scholar]
- 19.Griffin WL, Fehring TK, Mason JB, McCoy TH, Odum S, Terefenko CS. Early morbidity of modular exchange for polyethylene wear and osteolysis. J Arthroplasty. 2004;19(7 suppl):61–66. doi: 10.1016/j.arth.2004.06.014. [DOI] [PubMed] [Google Scholar]
- 20.Griffin WL, Scott RD, Dalury DF, Mahoney OM, Chiavetta JB, Odum SM. Modular insert exchange in knee arthroplasty for treatment of wear and osteolysis. Clin Orthop Relat Res. 2007;464:132–137. [PubMed] [Google Scholar]
- 21.Hamilton WG, Hopper RH, Engh CA, Engh CA. Survivorship of polyethylene liner exchanges performed for the treatment of wear and osteolysis among porous-coated cups. J Arthroplasty. 2010;25(suppl 6):75–80. doi: 10.1016/j.arth.2010.04.004. [DOI] [PubMed] [Google Scholar]
- 22.Hart AJ, Sabah SA, Bandi AS, Maggiore P, Tarassoli P, Sampson B, Skinner JA. Sensitivity and specificity of blood cobalt and chromium metal ions for predicting failure of metal-on-metal hip replacement. J Bone Joint Surg Br. 2011;93:1308–1313. doi: 10.1302/0301-620X.93B10.26249. [DOI] [PubMed] [Google Scholar]
- 23.Hsu AR, Gross CE, Levine BR. Pseudotumor from modular neck corrosion after ceramic-on-polyethylene total hip arthroplasty. Am J Orthop (Belle Mead NJ). 2012;41:422–426. [PubMed] [Google Scholar]
- 24.Kemp MA, Mitra A, da Costa TM, Spencer RF. Bearing exchange in the management of pseudotumours. Ann R Coll Surg Engl. 2013;95:266–270. doi: 10.1308/003588413X13511609958497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Koh KH, Moon YW, Lim SJ, Lee HI, Shim JW, Park YS. Complete acetabular cup revision versus isolated liner exchange for polyethylene wear and osteolysis without loosening in cementless total hip arthroplasty. Arch Orthop Trauma Surg. 2011;131:1591–1600. doi: 10.1007/s00402-011-1338-x. [DOI] [PubMed] [Google Scholar]
- 26.Kwon YM, Lombardi AV, Jacobs JJ, Fehring TK, Lewis CG, Cabanela ME. Risk stratification algorithm for management of patients with metal-on-metal hip arthroplasty: consensus statement of the American Association of Hip and Knee Surgeons, the American Academy of Orthopaedic Surgeons, and the Hip Society. J Bone Joint Surg Am. 2014;96:e4. doi: 10.2106/JBJS.M.00160. [DOI] [PubMed] [Google Scholar]
- 27.Lachiewicz PF, Soileau ES. Liner exchange in total knee arthroplasty. J Surg Orthop Adv. 2013;22:152–156. doi: 10.3113/JSOA.2013.0152. [DOI] [PubMed] [Google Scholar]
- 28.Liddle AD, Satchithananda K, Henckel J, Sabah SA, Vipulendran KV, Lewis A, Skinner JA, Mitchell AW, Hart AJ. Revision of metal-on-metal hip arthroplasty in a tertiary center: a prospective study of 39 hips with between 1 and 4 years of follow-up. Acta Orthop. 2013;84:237–245. doi: 10.3109/17453674.2013.797313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Lindgren JU, Brismar BH, Wikstrom AC. Adverse reaction to metal release from a modular metal-on-polyethylene hip prosthesis. J Bone Joint Surg Br. 2011;93:1427–1430. doi: 10.1302/0301-620X.93B10.27645. [DOI] [PubMed] [Google Scholar]
- 30.Maezawa K, Nozawa M, Matsuda K, Sugimoto M, Shitoto K, Kurosawa H. Serum chromium levels before and after revision surgery for loosened metal-on-metal total hip arthroplasty. J Arthroplasty. 2009;24:549–553. doi: 10.1016/j.arth.2008.02.001. [DOI] [PubMed] [Google Scholar]
- 31.Maloney WJ, Paprosky W, Engh CA, Rubash H. Surgical treatment of pelvic osteolysis. Clin Orthop Relat Res. 2001;393:78–84. doi: 10.1097/00003086-200112000-00009. [DOI] [PubMed] [Google Scholar]
- 32.Mao X, Tay GH, Godbolt DB, Crawford RW. Pseudotumor in a well-fixed metal-on-polyethylene uncemented hip arthroplasty. J Arthroplasty. 2012;27:493.e13–e17. [DOI] [PubMed]
- 33.McCalden RW, MacDonald SJ, Rorabeck CH, Bourne RB, Chess DG, Charron KD. Wear rate of highly cross-linked polyethylene in total hip arthroplasty: a randomized controlled trial. J Bone Joint Surg Am. 2009;91:773–782. doi: 10.2106/JBJS.H.00244. [DOI] [PubMed] [Google Scholar]
- 34.Munro JT, Masri BA, Duncan CP, Garbuz DS. High complication rate after revision of large-head metal-on-metal total hip arthroplasty. Clin Orthop Relat Res. 2014;472:523–528. doi: 10.1007/s11999-013-2979-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Nawabi DH, Hayter CL, Su EP, Koff MF, Perino G, Gold SL, Koch KM, Potter HG. Magnetic resonance imaging findings in symptomatic versus asymptomatic subjects following metal-on-metal hip resurfacing arthroplasty. J Bone Joint Surg Am. 2013;95:895–902. doi: 10.2106/JBJS.K.01476. [DOI] [PubMed] [Google Scholar]
- 36.O’Brien JJ, Burnett RS, McCalden RW, MacDonald SJ, Bourne RB, Rorabeck CH. Isolated liner exchange in revision total hip arthroplasty: clinical results using the direct lateral surgical approach. J Arthroplasty. 2004;19:414–423. doi: 10.1016/j.arth.2004.02.001. [DOI] [PubMed] [Google Scholar]
- 37.Pansard E, Fouilleron N, Dereudre G, Migaud H, Girard J. Severe corrosion after malpositioning of a metallic head over the Morse taper of a cementless hip arthroplasty: a case report. Orthop Traumatol Surg Res. 2012;98:247–250. doi: 10.1016/j.otsr.2011.05.018. [DOI] [PubMed] [Google Scholar]
- 38.Pritchett JW. One-component revision of failed hip resurfacing from adverse reaction to metal wear debris. J Arthroplasty. 2014;29:219–224. doi: 10.1016/j.arth.2013.04.011. [DOI] [PubMed] [Google Scholar]
- 39.Restrepo C, Ghanem E, Houssock C, Austin M, Parvizi J, Hozack WJ. Isolated polyethylene exchange versus acetabular revision for polyethylene wear. Clin Orthop Relat Res. 2009;467:194–198. doi: 10.1007/s11999-008-0533-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Schelfaut S, Cool S, Mulier M. The use of structural periacetabular allografts in acetabular revision surgery: 2.5–5 years follow-up. Arch Orthop Trauma Surg. 2009;129:455–461. doi: 10.1007/s00402-008-0622-x. [DOI] [PubMed] [Google Scholar]
- 41.Tower SS. Arthroprosthetic cobaltism: neurological and cardiac manifestations in two patients with metal-on-metal arthroplasty: a case report. J Bone Joint Surg Am. 2010;92:2847–2851. doi: 10.2106/JBJS.J.00125. [DOI] [PubMed] [Google Scholar]
- 42.Scully WF, Teeny SM. Pseudotumor associated with metal-on-polyethylene total hip arthroplasty. Orthopedics. 2013;36:e666–e670. doi: 10.3928/01477447-20130426-33. [DOI] [PubMed] [Google Scholar]
- 43.Van der Weegen W, Sijbesma T, Hoekstra HJ, Brakel K, Pilot P, Nelissen RG. Treatment of pseudotumors after metal-on-metal hip resurfacing based on magnetic resonance imaging, metal ion levels and symptoms. J Arthroplasty. 2014;29:416–421. doi: 10.1016/j.arth.2013.06.021. [DOI] [PubMed] [Google Scholar]
- 44.Verhelst LA, Van der Bracht H, Vanhegan IS, Van Backlé B, De Schepper J. Revising the well-fixed, painful resurfacing using a double-mobility head: a new strategy to address metal-on-metal complications. J Arthroplasty. 2012;27:1857–1862. doi: 10.1016/j.arth.2012.05.012. [DOI] [PubMed] [Google Scholar]
- 45.Wade FA, Rapuri VR, Parvizi J, Hozack WJ. Isolated acetabular polyethylene exchange through the anterolateral approach. J Arthroplasty. 2004;19:498–500. doi: 10.1016/j.arth.2004.02.005. [DOI] [PubMed] [Google Scholar]
- 46.Werner SD, Bono JV, Nandi S, Ward DM, Talmo CT. Adverse tissue reactions in modular exchangeable neck implants: a report of two cases. J Arthroplasty. 2013;28:543.e13–e15. [DOI] [PubMed]
- 47.Whitehouse MR, Endo M, Masri BA. Adverse local tissue reaction associated with a modular hip hemiarthroplasty. Clin Orthop Relat Res. 2013;471:4082–4086. doi: 10.1007/s11999-013-3133-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Wyles CC, Van Demark RE, Sierra RJ, 3rd, Trousdale RT. High rate of infection after aseptic revision of failed metal-on-metal total hip arthroplasty. Clin Orthop Relat Res. 2014;472:509–516. doi: 10.1007/s11999-013-3157-6. [DOI] [PMC free article] [PubMed] [Google Scholar]