Abstract
Background
Posttraumatic arthritis and prolonged recovery are typical after a severely comminuted tibial pilon fracture, and ankle arthrodesis is a common salvage procedure. However, few reports discuss the option of immediate arthrodesis, which may be a potentially viable approach to accelerate overall recovery in patients with severe fracture patterns.
Questions/purposes
(1) How long does it take the fracture to heal and the arthrodesis to fuse when primary ankle arthrodesis is a component of initial fracture management? (2) How do these patients fare clinically in terms of modified American Orthopaedic Foot and Ankle Society (AOFAS) scores and activity levels after this treatment? (3) Does primary ankle arthrodesis heal in an acceptable position when anterior ankle arthrodesis plates are used?
Methods
During a 2-year period, we performed open fracture reduction and internal fixation in 63 patients. Eleven patients (12 ankles) with severely comminuted high-energy tibial pilon fractures were retrospectively reviewed after surgical treatment with primary ankle arthrodesis and fracture reduction. Average patient age was 58 years, and minimum followup was 6 months (average, 14 months; range, 6–22 months). Anatomically designed anterior ankle arthrodesis plates were used in 10 ankles. Ring external fixation was used in nine ankles with concomitant tibia fracture or in instances requiring additional fixation. Clinical evaluation included chart review, interview, the AOFAS ankle-hindfoot score, and radiographic evaluation.
Results
All of the ankle arthrodeses healed at an average of 4.4 months (range, 3–5 months). One patient had a nonunion at the metaphyseal fracture, which healed with revision surgery. The average AOFAS ankle-hindfoot score was 83 with 88% having an excellent or good result. Radiographic and clinical analysis confirmed a plantigrade foot without malalignment. No patients required revision surgery for malunion.
Conclusions
Primary ankle arthrodesis combined with fracture reduction for the severely comminuted tibial pilon fracture reliably healed and restored acceptable function in this highly selective patient group. Ring external fixation may be a useful adjunct to internal fixation, and this concept should be further studied.
Level of Evidence
Level IV, therapeutic study. See Guidelines for Authors for a complete description of levels of evidence.
Introduction
A small percentage of tibial pilon fractures have damage to the ankle articular surface severe enough to preclude anatomic reduction and effective internal fixation. They are often the result of a high-energy injury such as a fall, jump, or motor vehicle accident. In these fractures, the joint surface either is severely fragmented or the articular cartilage has been sheared, typically involving the anterior half of the joint. Posttraumatic arthritis, prolonged return to work and activities, pain, stiffness, and further surgery are common after injuries of this severity [9, 11].
Most articles about treating pilon fractures focus on the results of open reduction and internal fixation. The use of primary ankle arthrodesis with reconstruction of the fracture has received much less attention; the literature on the subject of which we are aware consists of no more than several dozen patients using a diversity of approaches, including blade plates [2], intramedullary nails [10], and the Ilizarov method or other forms of external fixation [4, 6]. Because these reports were generally so small, and because of the kinds of severe complications they observed—including nonunions and even amputations [4, 6]—alternative approaches merit our attention. We have been using an anterior plating technique, acute bone grafting of tibial bone defects, selective use of adjunctive ring external fixation, along with soft tissue management for severe injuries of this type [12], and we wished to evaluate the performance of this approach. Specifically, we sought to answer the following questions: (1) How long does it take the fracture to heal and the arthrodesis to fuse when primary ankle arthrodesis is a component of initial fracture management? (2) How do these patients fare clinically in terms of modified American Orthopaedic Foot and Ankle Society (AOFAS) scores and activity levels after this treatment? (3) Using an approach that combined the use of an anterior plate with a ring fixator in certain scenarios, with weightbearing permitted in patients who had the fixator, is correct ankle alignment maintained at the time of healing?
Patients and Methods
Study Design and Setting
This study is a retrospective case series. All patients were treated by the two authors at the same Level I trauma center (Emanuel Hospital, Portland, OR, USA) and followed at the Summit Orthopaedics Clinic. The authors planned each surgery in tandem and used the same surgical methods. The collection period was from May 2010 to September 2012. The minimum followup for the definitive surgical reconstruction was 6 months (average, 14 months; range, 6–22 months).
Participants/Study Subjects
All patients included in this study sustained comminuted (Ruedi-Allgower, Feibel modification [4] Grade 3B, AO/OTA Type C3) tibial pilon fractures with greater than 50% articular cartilage loss (Fig. 1). During the period in question, patients with less than 50% articular cartilage loss generally were managed with open reduction and internal fixation and attempted joint salvage. This determination was made based on imaging studies (CT scan and plain radiographs) and intraoperative evaluation. Patients requiring bone transport, greater than 3 cm of shortening, those with low-energy neuropathic injuries, or with delayed presentation (greater than 3 weeks) were excluded.
Fig. 1.
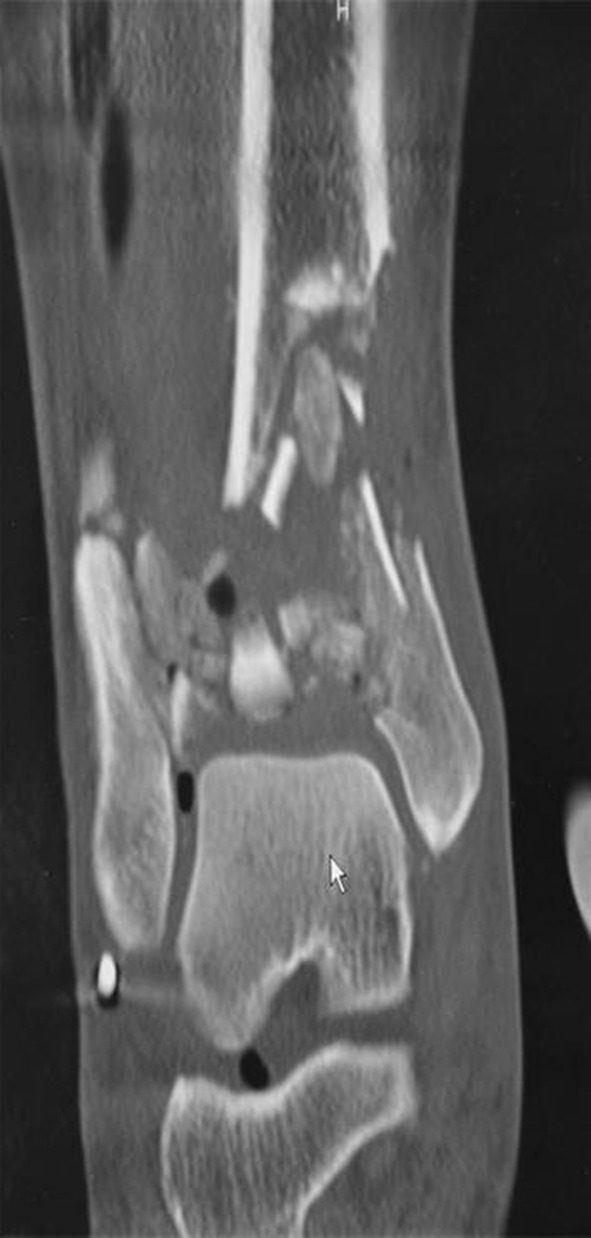
Coronal CT scan cut demonstrates a high degree of tibial plafond comminution associated with severe articular cartilage damage, our primary indication for the inclusion of an ankle fusion with pilon fracture repair.
Description of Experiment, Treatment, or Surgery
Our standard pilon fracture treatment protocol was followed for this group of patients. This protocol includes: irrigation, débridement, and soft tissue management for open injuries; spanning external fixation (Figs. 1–3) to obtain anatomic length; and definitive reconstruction when swelling and soft tissues allow wound closure. Reconstructive surgery of the tibia and ankle was performed through an anterior approach (interval between the tibialis anterior and extensor hallucis longus) in 10 ankles (Figs. 4, 5 show treatment of one patient). Because of soft tissue concerns, one ankle was managed through a lateral approach and one through combined medial and lateral approaches. The fibula was typically fixed with plates and screws. Intramedullary pins and Kirschner wire were used to facilitate the alignment of the fusion or fractures (Figs. 3–5). The pilon fracture components were reduced, and remaining articular cartilage from the ankle was removed. The subchondral bone was drilled with a 2.0-mm drill. Internal fixation of the fracture and arthrodesis was performed using an anatomically designed anterior ankle arthrodesis plate in 10 ankles. The anatomically designed modern anterior ankle arthrodesis plates used in this study included those manufactured by Smith & Nephew (Memphis, TN, USA), Tornier (Bloomington, MN, USA), Integra (Plainsboro, NJ, USA), and Synthes (West Chester, PA, USA). All were of sufficient length for an isolated ankle arthrodesis, but insufficient in length to treat a concomitant tibia fracture, necessitating the use of additional fixation, which was successfully accomplished with ring external fixation (Figs. 6–12).
Fig. 2.

This is the injury AP radiograph of an open pilon fracture sustained resulting from a logging accident.
Fig. 7.

The lateral radiograph more clearly depicts the plafond damage, which is better visualized on the CT scan shown in Figure 8.
Fig. 8.

This CT scan depicts plafond damage.
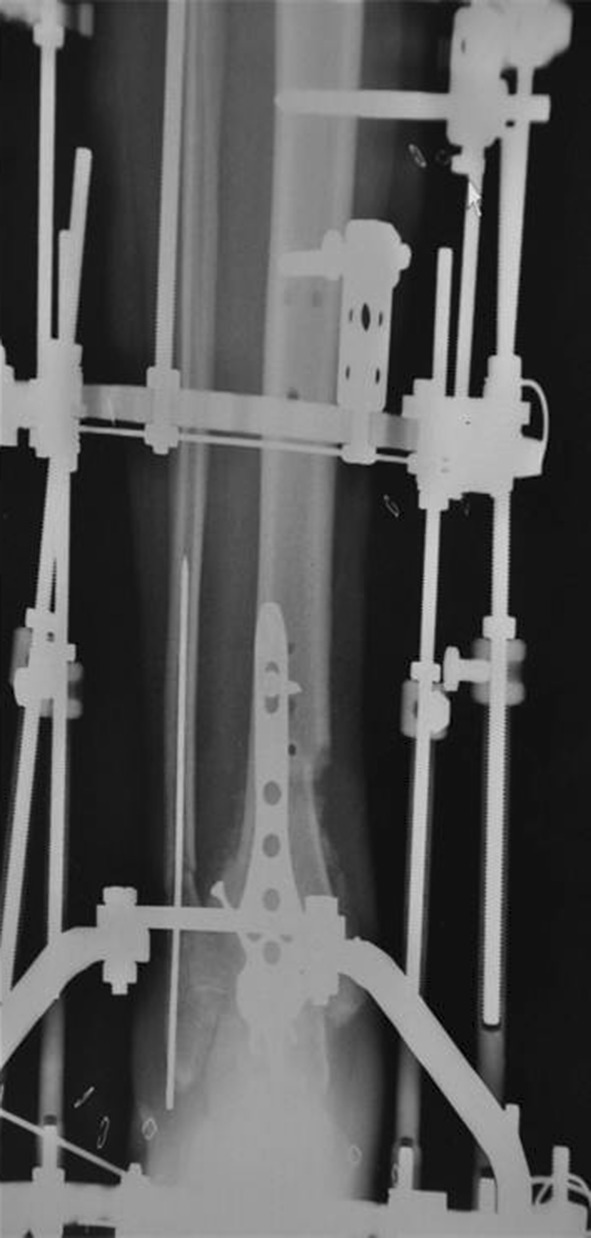
Fig. 9.

The AP radiograph is after surgical treatment, including fracture stabilization and ankle arthrodesis with an anatomically designed anterior fusion plate and ring external fixation.
Fig. 3.

This AP radiograph is after initial spanning external fixation, open fracture management, and intramedullary fibular fixation.
Fig. 4.
This AP radiograph, after definitive fracture management and ankle arthrodesis, shows the use of both internal ankle arthrodesis plate fixation and ring external fixation.
Fig. 5.

This is the lateral radiograph of the same patient in Figure 4.
Fig. 6.

The AP radiograph shows a closed pilon fracture after spanning external fixation performed the day of injury.
Fig. 12.

The hindfoot alignment view of this patient with bilateral injuries shows the comparison with the contralateral limb, which was treated with traditional open reduction and internal fixation.
In two instances, additional plates provided stability for a tibial shaft component of the fracture pattern, and in seven, a multiplanar ring external fixator was placed for this purpose. Our rationale for this decision was based on a combination of the soft tissue envelope, bone integrity around the ankle, stability achieved with plate fixation at the arthrodesis site, and patient compliance with weightbearing restrictions. If adequate stability could be achieved and the soft tissue envelope allowed, plate fixation alone was used in the compliant patient. The ring external fixator consisted of two rings placed proximal to the fracture and one foot ring. All patients had neutral frames. As a general rule, a combination of 1.8-mm wires and 6-mm half-pins were used in the tibia. In the foot ring, two 1.8-mm smooth wires engaged the metatarsal shafts, and two crossed 1.8-mm smooth wires fixed the calcaneal tuberosity. In the tibia, all external fixation points were at least 2.5 cm from any internal fixation. Wires were not used in the talus when internal fixation was present. If no internal fixation was present, an additional smooth wire was placed in the talar neck. In two patients, because of soft tissue injury, only an Ilizarov device was used to stabilize the fracture and arthrodesis.
Bone defects in the distal tibia were filled at the time of fracture repair with allograft bone chips (Figs. 13–18) in 10 ankles and iliac crest autograft in one. In one patient, a defect was initially managed with antibiotic-containing methylmethacrylate beads, which were replaced with allograft bone chips at 9 weeks. The fibula underwent open reduction and internal fixation in four patients through a separate lateral incision. The variability in the definitive fracture management of this group was the result of individual fracture, soft tissue, and patient factors.
Fig. 14.

Lateral view shows a comminuted pilon fracture and calcaneal fracture from Figure 13.
Fig. 15.

AP radiograph shows a pilon fracture fixation and ankle arthrodesis performed through an anterior approach and the calcaneal fracture repair through a lateral approach. Ring external fixation provided additional fracture stability and allowed this patient with bilateral injuries to ambulate during the healing period.
Fig. 16.

Lateral view shows a pilon and calcaneal fracture from Figure 15.
Fig. 17.

AP radiograph after fracture healing shows restoration of limb alignment. This patient regained function and healed within 5 months after bilateral limb-threatening injuries without the need for additional reconstructive procedures.
Fig. 13.

AP radiograph shows both the comminuted pilon fracture and calcaneal fracture sustained after a suicide attempt.
Fig. 18.

Lateral view shows the patient in Figure 17.
The preferred position of ankle fusion was 0° to 3° valgus neutral flexion with rotation symmetric to the contralateral limb.
Aftercare
Routine postoperative intravenous antibiotics were administered for 24 hours in the closed fractures and 48 hours in the open fracture group. The two patients treated with plated fixation alone were nonweightbearing for 12 weeks in a short leg cast and then gradually advanced to weightbearing as tolerated in a removable fracture walker (retained until fracture and fusion healing). The nine treated with ring external fixation were allowed to be weightbearing as tolerated 2 weeks after frame application. Aspirin was used as an antithrombotic agent in all ankles.
Variables, Outcome Measures, Data Sources, and Bias
Outcome evaluation was performed in the outpatient clinic by or with the direct supervision of the authors and included chart review, patient interview, physical examination, and radiographs. Demographic and treatment data were obtained from the medical records. Interview and examination were performed based on the AOFAS ankle-hindfoot scale [8]. As a result of the nature of the cohort’s ankle injury, 8 points accounting for sagittal motion were unable to be assessed. Parameters assessed included pain, activity limitations, walking ability, gait, hindfoot motion, sagittal motion, hindfoot stability, and alignment.
Weightbearing radiographs at followup included hindfoot alignment, AP view of the ankle and tibia, and lateral view including the foot, ankle, and tibia (Figs. 10–12). The intersection of the tibial anatomic axis was measured relative to the midpoint of the talus on the AP view, the center of the talar lateral process on the lateral view, and the most inferior point of the calcaneus on the hindfoot alignment view. The angle of the tibial axis to the sole of the foot was measured. Postoperative radiographs were obtained at monthly intervals to determine healing. These radiographs were collected monthly, and all but two participants completed the full set.
Fig. 10.

The AP radiograph at followup demonstrates the radiographic measurements analyzed in this study.
Demographics and Description of the Study Population
Eleven patients with 12 pilon fractures comprised the study population (Table 1). The study population consisted of seven men and four women with an average age of 58 years (range, 25–76 years). The mechanism of injury was a fall in six (seven fractures), motor vehicle accident in two, a logging accident in one, and a kiteboard injury in one fracture. Seven fractures were closed and five were open. All had severely comminuted tibial pilon fractures with a nonreconstructable joint surface, classified as 3B using the Feibel modification of the Ruedi-Allgower system. Fractures extended into the tibial shaft in nine ankles. Six patients sustained other significant orthopaedic injuries. In close proximity to the pilon fracture, two sustained an ipsilateral talus fracture, the bilateral patient sustained bilateral displaced comminuted calcaneal fractures (Figs. 13–18), and one had peroneal brevis and longus tendon tears.
Table 1.
Subject injury and treatment summary
| Ankle fracture number | Age (years) | Sex | R/L | Means of injury | Fracture extension to tibial shaft | Open/closed | Ring external fixation | Duration of ring external fixation | Internal fixation | Approach | Graft | AOFAS score | Healing time (months) |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 60 | M | L | Fall | Yes | Open | No | – | Yes | Anterior | Autograft TOF | 81 | 3.75 |
| 2 | 76 | M | L | Fall | No | Closed | No | – | Yes | Anterior | Allograft | 91 | 3 |
| 3 | 45 | F | R | Kiteboard | Yes | Closed | No | – | Yes | Anterior | Allograft with infuse and local graft TOF | 87 | 4 |
| 4 | 25 | M | L | Jump | No | Open | Yes | 111 | Yes | Anterior | Allograft with infuse 9 weeks postframe application | – | 4.5 |
| 5 | 55 | F | R | MVA | No | Open | Yes | 116 | Yes | Medial/lateral | Allograft with infuse TOF | – | 3.75 |
| 6 | 51 | M | L | Fall | Yes | Closed | Yes | 120 | Yes | Anterior | Allograft TOF | 82 | 5 |
| 7 | 66 | M | R | Logging | Yes | Open | Yes | 57 | Yes | Anterior | Allograft TOF | 91 | 3 |
| 8 | 56 | M | R | Jump | Yes | Closed | Yes | 150 | Yes | Anterior | Allograft TOF | – | 5 |
| 9 | 56 | M | L | Jump | Yes | Closed | Yes | 150 | Yes | Anterior | Allograft TOF | – | 5 |
| 10 | 42 | M | L | Jump | Yes | Closed | Yes | 119 | Yes | Anterior | Allograft TOF | 82 | 4 |
| 11 | 33 | F | L | Fall | Yes | Closed | Yes | 105 | Yes | Anterior | Allograft TOF | 87 | 3.5 |
| 12 | 66 | F | R | MVA | Yes | Open | Yes | 167 | No | Lateral | Autograft with allograft chips 7 weeks postframe application | 69 | 3.75 |
R = right; L = left; AOFAS = American Orthopaedic Foot and Ankle Society; M = male; F = female; MVA = motor vehicle accident; Y = yes; N = no; TOF = at time of frame application.
The time from injury to definitive reconstruction averaged 15 days in 11 fractures with a range of 8 to 24 days. This excluded one patient who underwent definitive reconstruction at 67 days as a result of a severe soft tissue injury, which was managed with 2.5 cm of bone resection and wound closure without tissue transfer. Initial management in 11 fractures included a spanning external fixator device to maintain length and stability, and one length-stable fracture was managed with a short leg splint.
Accounting for All Patients/Study Subjects
During the period of study, the two authors performed fracture reduction and internal fixation on 63 pilon fractures. During this timeframe, 12 fractures were treated with primary arthrodesis, all of which were included for review in this study. Two patients were unable to return for final followup radiographs, interview, and examination. One was unable to be located. The other died approximately 2 years after the original fracture.
Results
All ankle fusions and 11 of the 12 fractures healed at an average of 4.4 months (range, 3–5 months). One patient developed a nonunion at the tibial metaphyseal/diaphyseal region but subsequently healed after revision internal fixation with iliac crest autograft. Average ring external fixation time (nine patients) was 120 days (range, 57–167 days). The one patient whose frame was removed at 57 days developed a tibial nonunion.
The mean AOFAS ankle-hindfoot score was 83 with a range from 69 to 91. Using this scale, eight patients had a score of 80 or better, and one scored 69. Patients who were not limited by their other orthopaedic injuries or psychiatric conditions were able to return to a level of function consistent with patients who have had ankle fusions performed on an elective basis. Three patients were able to do short hikes. One patient was able to snowboard, kitesurf, and bike. No patient required prescription pain medication at followup. At the end of treatment, we recommended that one patient obtain rocker-sole shoes, but the patient has opted not to consistently use them; no other patients in this series had symptomatic limb length discrepancy.
All patients who returned for followup physical examination had a well-aligned leg, ankle, and hindfoot. All received the maximum score for alignment on the AOFAS scale. Radiographic analysis confirmed these clinical findings. On the AP view (Fig. 10), the tibial anatomic axis was on average of 1.4 mm lateral to the midpoint of the talus with a range from 6 mm medial to 5 mm lateral. On the lateral view (Fig. 11), the tibial anatomic axis averaged 7.3 mm posterior to the midpoint of the talar lateral process with a range from 2 mm to 11 mm posterior. On the lateral view (Fig. 11), the tibial axis to sole of the foot angle averaged 89° with a range from 83° to 95°. On the hindfoot alignment view (Fig. 12), the tibial anatomic axis was an average of 0.1 mm lateral to the most plantar point of the calcaneus with a range from 11 mm medial to 10 mm lateral.
Fig. 11.

Lateral followup radiograph demonstrates radiographic measurements.
Other Relevant Findings
Complications included one tibial nonunion (as previously discussed) that was successfully treated with additional surgery. One patient had a superficial anterior ankle wound dehiscence that was successfully managed with a split-thickness skin graft. One patient developed a pulmonary embolus and was managed with medical treatment. One patient required revision of internal fixation for a rotational deformity. This deformity was corrected with the reinsertion of the proximal screws in the plate 4 weeks after the initial procedure. Two patients had hardware removal for activity-related symptoms. All patients with ring external fixators had at least one superficial pin tract infection, which was successfully treated with oral antibiotics and pin care. No deep infections were observed.
Discussion
Background and Rationale
It had been our protocol to try to salvage all ankles associated with pilon fractures using open reduction internal fixation, and there are many series evaluating this approach. However, after observing the long-term clinical results of certain severe fracture patterns, we theorized that primary ankle arthrodesis may expedite the recovery for a select group of patients whose fracture patterns are especially severe. The findings of this retrospective case series showed high healing rates without malalignment, good overall function, and minimal pain.
Limitations
This study had a number of limitations. First, this was a retrospective review of a small case series. Owing to the small number of included subjects, these outcomes were collected by the care team, which included the authors of this study. Although unavoidable, this leads to a source of observer bias. These limitations alone influence the strength of the conclusions that can be drawn; however, we believe the results have sufficient validity to warrant the continued use of the concepts presented and further study. Second, our followup was limited or lost in several patients. This is, unfortunately, a frequent problem in the trauma population. However, based on our experience with ankle fusions, we believe we obtained sufficient followup to evaluate our study questions. Third, there was no control group, and so it is possible that alternative approaches might prove better than the approaches we used. Fourth, determining time to healing has to be considered a relatively soft endpoint, because not every patient had radiographs at exactly the same time intervals; however, one can consider that, if anything, the times presented here are longer than actual healing times, because patients may have achieved union and arthrodesis before the first radiographs demonstrated those findings. Additionally, the definitive reconstructive surgical technique was not identical for all patients. This could have been avoided by excluding certain patients in this study, but our intention was to evaluate the validity of early primary ankle arthrodesis, and various surgical techniques could be used to accomplish this goal. Also, each patient in this select group of severe pilon fractures has individual injury characteristics that necessitated different techniques. Subject numbers were insufficient to determine if there was a difference between the various plates used in this study or between patients treated with or without the ring fixator. Finally, the AOFAS is not validated for this population.
Healing
It is conceivable that primary ankle arthrodesis at the time of pilon fracture fixation could create additional healing complications, especially given that most of the fractures included bone defects treated with allograft. However, in our patient series, healing rates were excellent and consistent with other similar published reports. All 14 subjects in the study by Bozic et al. [2] had complete healing at both the ankle fusion and fracture sites at an average of 15 weeks. Additionally, both subjects in a study by Niikura et al. [10] experienced complete healing. In these two patients, the distal fibula was used as bone graft. Stiehl and Dollinger [13] reported healing in all three instances, and Kenzora et al. [6] had healing in four of five subjects with both groups using external fixation.
AOFAS Scores
Our study found an average AOFAS score of 83, which is compatible with satisfactory overall function. This group of patients was able to achieve high levels of function after a severe ankle injury without the need for multiple reconstructive procedures and prolonged recovery times. As a result of the variability in patient populations, reporting methods, and patient outcome scoring systems, it is difficult to quantitate our patients’ function compared with similar patient populations treated with fracture reconstruction alone with or without delayed ankle arthrodesis or ankle arthroplasty. However, several recent studies using the AOFAS outcome score provide some comparative historical data. Jansen et al. [5] reported on 35 patients in 2013 and found a mean AOFAS ankle-hindfoot score of 82 in 14 patients with AO Type B fractures and a mean score of 55 in 21 patients with Type C fractures. Davidovitch et al. [3] retrospectively reviewed 46 patients (47 fractures) with OTA Type 43C (comminuted intraarticular) pilon fractures treated with either open reduction or internal fixation or limited internal fixation and spanning articulated external fixation. At a followup of 18 months, the external fixation group had a mean AOFAS ankle-hindfoot score of 77.1, and 81% had evidence of posttraumatic ankle arthritis. The open reduction and internal fixation group had a followup of 20 months, AOFAS score of 72.4, and 73% incidence of radiographic arthritis. Boraiah et al. [1] reported the outcome of open pilon fractures treated with open reduction and internal fixation using patient-specific treatment regimens. They showed a low incidence of soft tissue complications. Using a modified Mazur score, 24% had good or excellent results and 62% had a poor result with an average 34-month followup. The AO/OTA C3 fractures had a higher infection incidence. In 2012, Ketz and Sanders [7] reported a comparative study of comminuted pilon fractures treated with different surgical approaches for open reduction and internal fixation with a 40-month average followup. The staged posterolateral and anterior approach group had a mean AOFAS score of 85.2, whereas the standard anterior approach group had a mean AOFAS score of 76.4.
Radiographic Alignment
Radiographic analysis showed a tendency for slight talar anterior translation with respect to the tibia anatomic axis. Acceptable alignment in the frontal plane and sagittal plane angular alignment were achieved. To our knowledge, alignment measurements have not been specifically reported in the other studies of primary ankle arthrodesis for pilon fractures.
Conclusions
Highly comminuted tibial pilon fracture with severe articular cartilage damage can be managed successfully using modern soft tissue protocols and definitive surgical reconstruction with primary ankle arthrodesis. The anterior approach using anatomically designed ankle arthrodesis plates and ring external fixation methods provided good clinical and functional results with predictable healing. Based on the findings of this initial series, our clinical practice incorporates primary ankle arthrodesis into our treatment options for OTA C3 pilon injury patterns. Future directions include the development of internal fixation devices that provide the necessary stability to treat both distal tibia fractures and ankle arthrodeses. Future clinical research will focus on the outcome of patients treated with primary ankle arthrodesis compared with joint-sparing options.
Acknowledgments
We thank Kari Komloske FNP, and Paula Kupier PA, for their assistance in patient contact and data collection and Paxton Gehling for editorial assistance.
Footnotes
Each author certifies that he or she, or a member of his or her immediate family, has no funding or commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research ® editors and board members are on file with the publication and can be viewed on request.
Clinical Orthopaedics and Related Research ® neither advocates nor endorses the use of any treatment, drug, or device. Readers are encouraged to always seek additional information, including FDA-approval status, of any drug or device prior to clinical use.
Each author certifies that his or her institution approved the human protocol for this investigation, that all investigations were conducted in conformity with ethical principles of research, and that informed consent for participation in the study was obtained.
References
- 1.Boraiah S, Kemp TJ, Erwteman A, Lucas PA, Asprinio DE. Outcome following open reduction and internal fixation of open pilon fractures. J Bone Joint Surg Am. 2010;92:346–352. doi: 10.2106/JBJS.H.01678. [DOI] [PubMed] [Google Scholar]
- 2.Bozic V, Thordarson DB, Hertz J. Ankle fusion for definitive management of non-reconstructable pilon fractures. Foot Ankle Int. 2008;29:914–918. doi: 10.3113/FAI.2008.0914. [DOI] [PubMed] [Google Scholar]
- 3.Davidovitch RI, Elkhechen RJ, Romo S, Walsh M, Egol KA. Open reduction with internal fixation versus limited internal fixation and external fixation for high grade pilon fractures (OTA type 43C) Foot Ankle Int. 2011;32:955–961. doi: 10.3113/FAI.2011.0955. [DOI] [PubMed] [Google Scholar]
- 4.Feibel RJ, Uhthoff HK. [Primary Ilizarov ankle fusion for nonreconstructable tibial plafond fractures] [in German] Oper Orthop Traumatol. 2005;17:457–480. doi: 10.1007/s00064-005-1139-5. [DOI] [PubMed] [Google Scholar]
- 5.Jansen H, Fenwick A, Doht S, Frey S, Meffert R. Clinical outcome and changes in gait pattern after pilon fractures. Int Orthop. 2013;37:51–58. doi: 10.1007/s00264-012-1716-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kenzora JE, Simmons SC, Burgess AR, Edwards CC. External fixation arthrodesis of the ankle joint following trauma. Foot Ankle. 1986;7:49–61. doi: 10.1177/107110078600700108. [DOI] [PubMed] [Google Scholar]
- 7.Ketz J, Sanders R. Staged posterior tibial plating for the treatment of Orthopaedic Trauma Association 43C2 and 43C3 tibial pilon fractures. J Orthop Trauma. 2012;26:341–347. doi: 10.1097/BOT.0b013e318225881a. [DOI] [PubMed] [Google Scholar]
- 8.Kitaoka HB, Alexander IJ, Adelaar RS, Nunley JA, Myerson MS, Sanders M. Clinical rating systems for the ankle-hindfoot, midfoot, hallux, and lesser toes. Foot Ankle Int. 1994;15:349–353. doi: 10.1177/107110079401500701. [DOI] [PubMed] [Google Scholar]
- 9.Lewis JA, Vint H, Pallister I. Pilot study assessing functional outcome of tibial pilon fractures using the VSTORM method. Injury. 2013;44:1112–1116. doi: 10.1016/j.injury.2013.02.019. [DOI] [PubMed] [Google Scholar]
- 10.Niikura T, Miwa M, Sakai Y, Lee SY, Oe K, Iwakura T, Koh A, Koga T, Kurosaka M. Ankle arthrodesis using antegrade intramedullary nail for salvage of nonreconstructable tibial pilon fractures. Orthopedics. 2009;32. pii: orthosupersite.com/view.asp?rID=41937. [DOI] [PubMed]
- 11.Pollak AN, McCarthy ML, Bess RS, Agel J, Swiontkowski MF. Outcomes after treatment of high-energy tibial plafond fractures. J Bone Joint Surg Am. 2003;85:1893–1900. doi: 10.2106/00004623-200310000-00005. [DOI] [PubMed] [Google Scholar]
- 12.Sirkin M, Sanders R, DiPasquale T, Herscovici D., Jr A staged protocol for soft tissue management in the treatment of complex pilon fractures. J Orthop Trauma. 1999;13:78–84. doi: 10.1097/00005131-199902000-00002. [DOI] [PubMed] [Google Scholar]
- 13.Stiehl JB, Dollinger B. Primary ankle arthrodesis in trauma: report of three cases. J Orthop Trauma. 1988;2:277–283. doi: 10.1097/00005131-198802040-00003. [DOI] [PubMed] [Google Scholar]


