Abstract
Background
Recent studies have attributed adverse local tissue reactions (ALTRs) in patients with total hip arthroplasties (THAs) to tribocorrosion debris generated by modular femoral stems. The presentations of ALTR are diverse, as are the causes of it, and the biological responses can be important reasons for failure after THA.
Question/purposes
(1) What clinical problems have been reported in patients with modular stems since 1988? (2) What THA design features are associated with tribocorrosion in taper junctions? (3) What are the microscopic and tribological characteristics of the debris produced at the taper junctions? (4) What are the cellular and immunological traits of the biological response to taper tribocorrosion debris?
Methods
We conducted a systematic review using MEDLINE and EMBASE-cited articles to summarize failure modes associated with modular femoral stems. One hundred sixty-two of 1043 articles reported on the clinical performances or failure modes attributed to modular femoral stems. There were 10 laboratory studies, 26 case reports, 13 Level IV, 94 Level III, 18 Level II, and one Level I of Evidence papers. To address the remaining questions, we did a second review of 524 articles. One hundred twenty-seven articles met the eligibility criteria, including 81 articles on design features related to tribocorrosion, 15 articles on corrosion debris characteristics, and 31 articles on the biological response to tribocorrosion debris.
Results
Sixty-eight of 162 studies reported failure attributed to modular femoral stems for one of these four modularity-related failure modes: tribocorrosion-associated ALTR, dissociation of a taper junction, stem fracture, and mismatch of a femoral head taper attached to a stem with a different trunnion size. The remaining 94 studies found no clinical consequences related to the presence of a taper junction. THA component features associated with tribocorrosion included trunnion geometry and large-diameter femoral heads. Solid tribocorrosion debris is primarily chromium-orthophosphate material of variable size and may be more biologically reactive than wear debris.
Conclusions
There has been an increase in publications describing ALTR around modular hip prostheses in the last 3 years. Implant design changes, including larger femoral heads and smaller trunnions, have been implicated, but there may also be more recognition of the problem by the orthopaedic community. Analyzing retrieved implants to understand the history of taper-related problems, designing clinically relevant in vitro corrosion tests to test modular junctions, and identifying biomarkers to recognize patients at risk of ALTR should be the focus of ongoing research to help surgeons avoid and detect tribocorrosion-related problems in joint replacements.
Electronic supplementary material
The online version of this article (doi:10.1007/s11999-014-3746-z) contains supplementary material, which is available to authorized users.
Introduction
Since the mid-1980s, there has been a dramatic increase in the use of modular THA designs. Most early modular stem designs had a single head-neck taper junction, and this remains the most common type of femoral component in primary THA. More recently, dual modular stems have been introduced that include an additional neck-stem taper junction. Surgeons adopted head-neck modularity for the intraoperative advantages of adjusting leg length and femoral offset and neck-stem modularity for the opportunity to further fine-tune hip biomechanics and femoral anteversion. Both forms of modularity may also provide intraoperative flexibility when partial hip implant revision is required.
Recently, many reports have discussed adverse local tissue reactions (ALTRs) around modular femoral stems. The presentations of ALTR are diverse, as are the causes of it, and the biological responses can be lead to revision surgery. Given that the majority of THAs implanted around the world have at least one modular junction, we sought to answer the following questions: (1) What clinical problems have been reported in patients with modular stems since 1988? (2) What THA design features are associated with tribocorrosion in taper junctions? (3) What are the microscopic and tribological characteristics of the debris produced at the taper junctions? (4) What are the cellular and immunological traits of the biological response to taper tribocorrosion debris?
Search Strategy and Criteria
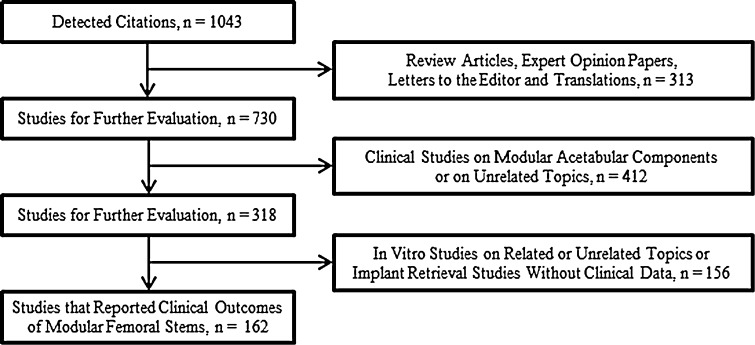
To answer Question 1, we used MEDLINE and EMBASE on May 9, 2014, to perform a systematic search to identify articles with the terms “modular” OR “modularity” AND “hip” in the title or abstract. One thousand forty-three articles were identified, and each article underwent abstract review by one author (CIE). Studies were included only if they were peer-reviewed, published in English, and associated failure of a THA (resulting in revision surgery) to the presence of a modular femoral stem junction or femoral stem fracture (Fig. 1). Retrieval studies of femoral components that did not include the reasons for revision surgery were excluded, because we were interested in the clinical problems associated with taper junctions. We included series and case reports of single modular and dual modular femoral stems, including metaphyseal modular stems (in which the taper junction was located distal to the femoral modular neck osteotomy) and proximal modular stems (in which the taper junction was located proximal to the femoral neck osteotomy).
Fig. 1.
A flow diagram showing the method for selecting articles in which failure of THAs was associated with the presence of a modular femoral stem junction or femoral stem fracture.
Of 1043 articles, 162 articles met our eligibility criteria (Appendix 1 [Supplemental materials are available with the online version of CORR®.]). There were 10 laboratory studies, 26 case reports, 13 Level IV, 94 Level III, 18 Level II, and one Level I of Evidence papers. Sixty-eight of 162 clinical studies associated the reason for revision surgery to taper-related stem problems or stem fracture, whereas 94 studies found no clinical consequences related to the presence of a taper junction.
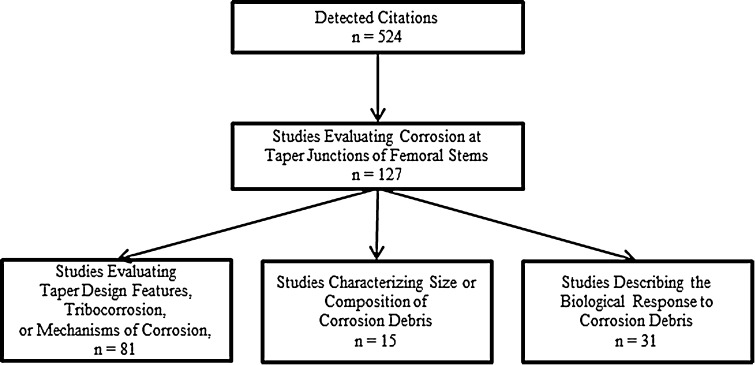
To answer Questions 2, 3, and 4, we performed a second search to review the current knowledge of tribocorrosion in taper junctions of THAs. We queried “corrosion” OR “taper” OR “trunnion” AND “hip” in the title or abstract of MEDLINE and EMBASE-cited articles. Each article underwent abstract review by one author (CIE). Studies were included only if they were peer-reviewed, published in English, and investigated tribocorrosion in taper junctions of THAs (Fig. 2). Retrieval studies of implants or periprosthetic tissues and biomechanical in vitro studies attempting to replicate the clinical findings were included. We excluded studies involving cemented THAs because of confounding factors including tribocorrosion at stem-cement interfaces or biological responses to cement debris. Of 524 articles, 127 articles met our eligibility criteria (Appendix 2). There were 60 retrieval studies, 36 laboratory studies, 20 case reports, 10 Level III, and one Level II of Evidence papers. Eighty-one articles evaluated taper design features, 15 articles characterized corrosion debris, and 31 articles described the biological response to the debris.
Fig. 2.
A flow diagram showing the method for selecting articles that investigated tribocorrosion in taper junctions of THAs.
Results
What Clinical Problems Have Been Reported in Patients With Modular Stems Since 1988?
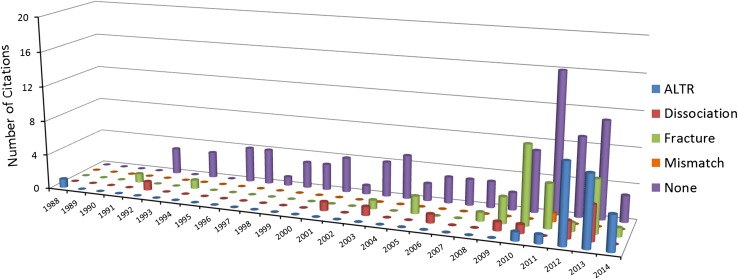
Four modularity-related failure modes were attributed to modular femoral stems: tribocorrosion-associated ALTR, dissociation of a taper junction, stem fracture, and mismatch of a femoral head with one taper size attached to a stem with a different trunnion size (Fig. 3), although the latter was reported in only one study in 2011 [23]. Sixty-eight of 162 clinical studies associated a femoral stem taper junction or stem fracture to the reason for revision surgery, which included 37 studies of single head-neck taper stems and 31 studies of dual modular stems. Ninety-four studies found no clinical consequences related to the presence of a taper junction. Early reports of dissociation and stem fracture were published in 1992 and 1994. The first report of tribocorrosion-associated ALTR leading to revision surgery was in 1988 [39]. A noticeable increase in ALTR as a reason for revision surgery did not start until 2010, over 20 years after the first modular stem was introduced for THA. Metal toxicity or hypersensitivity reactions in periprosthetic tissues containing tribocorrosion debris were reported before 2010 [1, 33, 41], but the reason for revision surgery in these patients was not attributed to ALTR alone.
Fig. 3.
A column chart showing the number of citations from 1988 to 2014 that attributed failure of THAs to the presence of modular femoral junctions.
There were 24 citations that reported tribocorrosion-related ALTRs in patients, of which eight were case reports or case series of patients with dual modular stems. In 16 citations that reported tribocorrosion-related ALTRs with single modular stems, 10 involved large-diameter (> 36 mm) metal femoral heads and six involved smaller (≤ 36 mm) heads made of either metal or ceramic.
Two papers reported “pain” in patients where there was taper tribocorrosion [12, 37], but it is unknown whether these patients had undiagnosed ALTR.
What THA Design Features Are Associated With Tribocorrosion in Taper Junctions?
Large-diameter femoral heads and trunnion geometry were common features identified in the studies that associated elements of implant design with tribocorrosion in taper junctions [7, 18, 19, 32]. Larger head sizes increase torsional forces at the trunnion [9], and this may be a contributing factor in the increased failure rates seen metal-on-metal (MoM) THAs [17, 22], which have a high revision rate of 19% after 12 years [2]. Increasing head offset and increasing varus neck shaft angle have been considered with head size, leading to an increased effective horizontal lever arm [32]. Flexural rigidity of the neck has been shown to be a significant predictor of fretting and corrosion [18], and retrieved implants show a damage pattern on opposite sides of the taper circumference suggesting a toggling effect rather than a rotational moment [5, 35, 36]. Tribocorrosion-related problems are not exclusive to large-diameter (> 36 mm) femoral head sizes alone [13]. In metal-on-polyethylene (MoP) hips, increased corrosion has been shown in 36-mm metal femoral heads compared with 28-mm heads [16]. Another contributing factor to tribocorrosion in MoP and MoM THAs is the dissimilar alloy pairings of a cobalt-chrome femoral head taper and a titanium trunnion [26], and ceramic femoral heads have been shown to decrease taper tribocorrosion compared with cobalt-chrome heads (CoCr) [20, 25, 31].
Trunnion length, trunnion diameter, and taper angle are parameters thought to contribute to tribocorrosion, because these dictate the force distributions at the taper junction [10]. Although there has been a recent trend in increasing femoral head sizes, there has been a trend in decreasing trunnion size [32]. Trunnions have been designed to be shorter in length and thinner in diameter to increase the range of motion before impingement. There is disagreement in the literature as to whether a thinner and shorter taper is more beneficial than a longer, thicker taper. A smaller trunnion that sits inside the head taper may have greater potential for edge loading of the trunnion base [32], but a retrieval study found thicker tapers with longer contact lengths and a higher taper angle had greater fretting scores [35]. Nominally the 12/14 taper has been used over the past 20 years, which suggests the taper angle has not changed, but little is known about the machining tolerances of tapers and trunnions among the different manufacturers. In dual modular stems, material coupling and the taper design are also crucial for the micromotion magnitude at the stem-neck junction with titanium neck adapters having significantly higher interface micromotions than those with CoCr adapters [29]. The additional stem-neck junction in dual modular stems has been associated with increased damage at the head–stem junction [22].
What Are the Microscopic and Tribological Characteristics of the Debris Produced at the Taper Junctions?
Substantial volumetric material loss can take place at the taper junctions of modern large-diameter THAs, and in some cases, the material loss is more than bearing wear [32, 34]. There are both solid and soluble products of corrosion that are variable in size [28]. Regardless of whether the head-neck couple consists of cobalt alloy and cobalt alloy, cobalt alloy and titanium alloy, or alumina ceramic and cobalt alloy, the principal solid tribocorrosion product is chromium-orthophosphate hydrate-rich material [8, 21, 24, 26, 40]. Solid deposits in local periprosthetic tissues have been described as irregularly shaped, green- to yellow-colored, and ranging in size from submicron to 400 µm, showing no birefringence under polarized light [24]. Particles and metal ions can also spread throughout the body. Elevated levels of cobalt ions in the serum and chromium ions in the urine of patients with uncemented THAs have been associated with corrosion of the prostheses [6, 27, 28]. Metal ion levels may be used as a diagnostic tool to identify problems with hip prostheses [14], but the systemic effects of the metal ions remain unknown.
What Are the Cellular and Immunological Traits of the Biological Response to Taper Tribocorrosion Debris?
Tribocorrosion debris may be more biologically reactive than bearing wear debris. There have been reports of extensive tissue necrosis involving nearly the entire hip capsule, short external rotators, and tendinous portion of the gluteus medius muscle [38]. Periprosthetic tissues containing tribocorrosion debris may include some features of a delayed Type IV hypersensitivity immune reaction such as extensive loss of synovial surface and tissue necrosis, but in some cases lack the large perivascular cuffs usually reported with metal allergy [11]. In other reports, corrosion products are present in patients with hypersensitivity-associated reactions including extensive tissue necrosis, lymphocytic tissue infiltrates, and vascular inflammation [24, 33]. It is difficult to determine whether ALTR is the result of taper debris alone, because additional wear debris from the bearing will always be present in the effective joint space around a THA. In this systematic review, for example, 31 articles were concerned with biological reactions to corrosion debris (Fig. 2), and in 18 articles, the authors attributed failure directly to the reaction. A recent case report of a modular hemiarthroplasty (separate stem and head) described a hypersensitivity reaction in the absence of a bearing [30].
Discussion
The majority of primary THAs performed throughout the world have a head-neck taper junction, and yet we have limited knowledge of how these junctions perform in vivo. Twenty years ago, tribocorrosion was recognized primarily as a problem contributing to stem fatigue fracture. Unfortunately, there has been a notable increase in publications describing ALTR in patients with modular femoral components in the last 3 years, and finding solutions to avoid tribocorrosion is complicated by the multifactorial nature of the problem.
There are several main limitations to this work. The first is we only searched the English language and may have missed scientific work published on tribocorrosion in THAs in other parts of the world. The second limitation is that we did not include unpublished material in our search; however, we did thorough searches of two of the largest databases for work of this kind, PubMed and EMBASE, and so the likelihood seems low that we would have missed important clinical reports. Third, the size of our study list precludes an in-depth analysis of study quality, and some of the studies included were laboratory science, for which study quality tools do not exist. The majority of the studies were case reports and small case series, which rarely reported on consecutive series of patients. Therefore, we may be underestimating the scope of tribocorrosion-related problems in patients with THAs. Fourth, we found very few data on the influence of taper angle and geometry [32] and so could draw no firm inferences on what might be a very important topic based on the research available now. Finally, the biological response to wear debris in all likelihood depends on many factors apart from the material properties of the debris itself; no doubt patient-related factors play a substantial role, but the available research did not permit an in-depth analysis of potential patient-level predictor variables.
Tribocorrosion-associated ALTR, dissociation of a taper junction, stem fracture, and mismatch of a femoral head taper to a different size stem trunnion are all potential complications associated with femoral stem modularity. There were few failures of titanium stems implanted with CoCr heads for many years before 2010 (Fig. 3), so it remains unknown whether the diagnosis of taper-related problems was overlooked by the orthopaedic community. Understanding the history of the taper problem is the first step in providing valuable information to clinicians and patients who might have an ALTR and in suggesting strategies to prevent adverse biological reactions in the future. We should continue to promote and analyze joint replacement registries to identify long-term successes and failures.
Trends of larger femoral heads and smaller trunnion geometries may be associated with tribocorrosion at a taper junction. However, tribocorrosion leading to ALTRs has been reported in patients with MoP THAs with 28-mm or 32-mm heads on stems with single head-neck taper junctions [13]. We need to better understand what changes may have been made to taper junctions used in joint arthroplasty across the orthopaedic device industry over time and how changes may have influenced the risk of taper tribocorrosion. Retrieval analysis can be used to study how taper geometry, taper tolerances, taper diameter, taper metallurgy, taper surface finish, and femoral head diameter influence risk of tribocorrosion. Some centers have modeled contact conditions and micromotions on fretting behavior of modular taper connections [3, 15, 17]. Finite element analysis provides clues to these questions, but an in vitro model that reproduces the pattern of taper tribocorrosion seen in vivo will be needed to provide more definitive answers. The influence of how the taper is assembled intraoperatively on the subsequent risk of taper tribocorrosion is not fully understood. This variability is important because taper strength increases linearly with assembly force [36]. Cleaning procedures just before assembly in the hip at surgery and subsequent impaction techniques and loads to assemble the head to the taper are likely quite variable, but how these variations influence subsequent tribocorrosion has not been studied. Improvements in preclinical testing protocols for new devices that incorporate modular connections are needed, including a clinically relevant in vitro tribocorrosion test.
The fragmentation of a tribocorrosion product into solid particles and metal ions is difficult to quantify and chemically define because they can migrate systemically. An important limitation of the literature characterizing debris produced at the taper junctions is bias in the particle size observed, because it is dictated by the methods used to isolate and measure the debris. Better characterization of tribocorrosion products is necessary; then they must be isolated from in vivo tissues or recreated in vitro and used in cell and animal models to understand their influence on ALTR. Recreating the same taper tribocorrosion debris that occurs in vivo poses a challenge for in vitro testing. Tribocorrosion tests that could be a model for iterative preclinical testing that would allow optimization of taper junctions while also providing tribocorrosion debris to researchers for biocompatibility testing would be valuable.
Implant retrieval analysis and histological analysis of periprosthetic tissues from cases of ALTR are essential for understanding the biological response. How host factors influence the biologic response to taper tribocorrosion products is not well understood. It would be useful to understand if some patients are at higher risk for ALTR and, if so, to identify associated biomarkers or genetic markers. In vivo animal models that reproduce a typical tribocorrosion-related ALTR would also be valuable. Supporting fields, including imaging and radiology and cellular biology, should continue to improve imaging modalities and to find metal ion and/or biomarker levels, respectively, to aid surgeons with early detection of ALTR.
Clinicians should use modularity wisely. Protocols for monitoring patients and managing complications that may result from severe soft tissue damage and bone necrosis are evolving to help patients with tribocorrosion-related ALTRs [4]. Rigorous laboratory testing that can replicate the in vivo environment should be further developed, and researchers should understand how to improve tapers and materials to avoid problems in the future.
Electronic supplementary material
Footnotes
Each author certifies that he or she, or a member of his or her immediate family, has no funding or commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research ® editors and board members are on file with the publication and can be viewed on request.
Each author certifies that his or her institution approved the human protocol for this investigation, that all investigations were conducted in conformity with ethical principles of research, and that informed consent for participation in the study was obtained.
This work was performed at the Carl T. Brighton Workshop, Tampa, FL, USA.
References
- 1.Al-Saffar N. Early clinical failure of total joint replacement in association with follicular proliferation of B-lymphocytes: a report of two cases. J Bone Joint Surg Am. 2002;84:2270–2273. doi: 10.2106/00004623-200212000-00022. [DOI] [PubMed] [Google Scholar]
- 2.Anonymous. Australian Orthopaedic Association National Joint Replacement Registry. Annual Report. Adelaide, Australia: AOA; 2013.
- 3.Baxmann M, Jauch SY, Schilling C, Blomer W, Grupp TM, Morlock MM. The influence of contact conditions and micromotions on the fretting behavior of modular titanium alloy taper connections. Med Eng Phys. 2013;35:676–683. doi: 10.1016/j.medengphy.2012.07.013. [DOI] [PubMed] [Google Scholar]
- 4.Berry DJ, Abdel MP, Callaghan JJ. What are the current clinical issues in wear and tribocorrosion? Clin Orthop Relat Res. 2014 Apr 8 [Epub ahead of print]. [DOI] [PMC free article] [PubMed]
- 5.Bolland BJ, Culliford DJ, Langton DJ, Millington JPS, Arden NK, Latham JM. High failure rates with a large-diameter hybrid metal-on-metal total hip replacement. Clinical, radiological and retrieval analysis. J Bone Joint Surg Br. 2011;93:608–615. doi: 10.1302/0301-620X.93B5.26309. [DOI] [PubMed] [Google Scholar]
- 6.Braun E, Schmitt D, Nabet F, Legras B, Coudane H, Mole D. [Urinary concentration of cobalt and chromium in patients with a non-cemented total hip prosthesis] [in French] Int Orthop. 1986;10:277–282. doi: 10.1007/BF00454409. [DOI] [PubMed] [Google Scholar]
- 7.Brown SA, Flemming CA, Kawalec JS, Placko HE, Vassaux C, Merritt K, Payer JH, Kraay MJ. Fretting corrosion accelerates crevice corrosion of modular hip tapers. J Appl Biomater. 1995;6:19–26. doi: 10.1002/jab.770060104. [DOI] [PubMed] [Google Scholar]
- 8.Bryant M, Ward M, Farrar R, Freeman R, Brummitt K, Nolan J, Neville A. Characterisation of the surface topography, tomography and chemistry of fretting corrosion product found on retrieved polished femoral stems. J Mech Behav Biomed Mater. 2014;32:321–334. doi: 10.1016/j.jmbbm.2013.11.016. [DOI] [PubMed] [Google Scholar]
- 9.Burroughs BR, Muratoglu OK, Bragdon CR, Wannomae KK, Christensen S, Lozynsky AJ, Harris WH. In vitro comparison of frictional torque and torsional resistance of aged conventional gamma-in-nitrogen sterilized polyethylene versus aged highly crosslinked polyethylene articulating against head sizes larger than 32 mm. Acta Orthop. 2006;77:710–718. doi: 10.1080/17453670610012881. [DOI] [PubMed] [Google Scholar]
- 10.Cales B, Stefani Y. Risks and advantages in standardization of bores and cones for heads in modular hip prostheses. J Biomed Mater Res. 1998;43:62–68. doi: 10.1002/(SICI)1097-4636(199821)43:1<62::AID-JBM7>3.0.CO;2-K. [DOI] [PubMed] [Google Scholar]
- 11.Chana R, Esposito C, Campbell PA, Walter WK, Walter WL. Mixing and matching causing taper wear: corrosion associated with pseudotumour formation. J Bone Joint Surg. Br. 2012;94:281–286. doi: 10.1302/0301-620X.94B2.27247. [DOI] [PubMed] [Google Scholar]
- 12.Collier JP, Surprenant VA, Jensen RE, Mayor MB, Surprenant HP. Corrosion between the components of modular femoral hip prostheses. J Bone Joint Surg Br. 1992;74:511–517. doi: 10.1302/0301-620X.74B4.1624507. [DOI] [PubMed] [Google Scholar]
- 13.Cooper HJ, Della Valle CJ, Berger RA, Tetreault M, Paprosky WG, Sporer SM, Jacobs JJ. Corrosion at the head-neck taper as a cause for adverse local tissue reactions after total hip arthroplasty. J Bone Joint Surg Am. 2012;94:1655–1661. doi: 10.2106/JBJS.K.01352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.De Smet K, De Haan R, Calistri A, Campbell PA, Ebramzadeh E, Pattyn C, Gill HS. Metal ion measurement as a diagnostic tool to identify problems with metal-on-metal hip resurfacing. J Bone Joint Surg Am. 2008;90(Suppl 4):202–208. doi: 10.2106/JBJS.H.00672. [DOI] [PubMed] [Google Scholar]
- 15.Donaldson FE, Coburn JC, Siegel KL. Total hip arthroplasty head-neck contact mechanics: a stochastic investigation of key parameters. J Biomech. 2014;47:1634–1641. doi: 10.1016/j.jbiomech.2014.02.035. [DOI] [PubMed] [Google Scholar]
- 16.Dyrkacz RMR, Brandt J-M, Ojo OA, Turgeon TR, Wyss UP. The influence of head size on corrosion and fretting behaviour at the head-neck interface of artificial hip joints. J Arthroplasty. 2013;28:1036–1040. doi: 10.1016/j.arth.2012.10.017. [DOI] [PubMed] [Google Scholar]
- 17.Elkins JM, Callaghan JJ, Brown TD. Stability and trunnion wear potential in large-diameter metal-on-metal total hips: a finite element analysis. Clin Orthop Relat Res. 2014;472:529–542. doi: 10.1007/s11999-013-3244-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Goldberg JR, Gilbert JL, Jacobs JJ, Bauer TW, Paprosky W, Leurgans S. A multicenter retrieval study of the taper interfaces of modular hip prostheses. Clin Orthop Relat Res. 2002;401:149–161. doi: 10.1097/00003086-200208000-00018. [DOI] [PubMed] [Google Scholar]
- 19.Grupp TM, Weik T, Bloemer W, Knaebel H-P. Modular titanium alloy neck adapter failures in hip replacement—failure mode analysis and influence of implant material. BMC Musculoskelet Disord. 2010;11:3. doi: 10.1186/1471-2474-11-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hallab NJ, Messina C, Skipor A, Jacobs JJ. Differences in the fretting corrosion of metal-metal and ceramic-metal modular junctions of total hip replacements. J Orthop Res. 2004;22:250–259. doi: 10.1016/S0736-0266(03)00186-4. [DOI] [PubMed] [Google Scholar]
- 21.Hart AJ, Quinn PD, Sampson B, Sandison A, Atkinson KD, Skinner JA, Powell JJ, Mosselmans JFW. The chemical form of metallic debris in tissues surrounding metal-on-metal hips with unexplained failure. Acta Biomater. 2010;6:4439–4446. doi: 10.1016/j.actbio.2010.06.006. [DOI] [PubMed] [Google Scholar]
- 22.Higgs GB, Hanzlik JA, MacDonald DW, Gilbert JL, Rimnac CM, Kurtz SM. Is increased modularity associated with increased fretting and corrosion damage in metal-on-metal total hip arthroplasty devices? A retrieval study. J Arthroplasty. 2013;28(Suppl):2–6. doi: 10.1016/j.arth.2013.05.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hohman DW, Affonso J, Anders M. Ceramic-on-ceramic failure secondary to head-neck taper mismatch. Am J Orthop (Belle Mead, NJ). 2011;40:571–573. [PubMed]
- 24.Huber M, Reinisch G, Trettenhahn G, Zweymuller K, Lintner F. Presence of corrosion products and hypersensitivity-associated reactions in periprosthetic tissue after aseptic loosening of total hip replacements with metal bearing surfaces. Acta Biomater. 2009;5:172–180. doi: 10.1016/j.actbio.2008.07.032. [DOI] [PubMed] [Google Scholar]
- 25.Huot Carlson JC, Van Citters DW, Currier JH, Bryant AM, Mayor MB, Collier JP. Femoral stem fracture and in vivo corrosion of retrieved modular femoral hips. J Arthroplasty. 2012;27:1386–1396.e1. [DOI] [PubMed]
- 26.Jacobs JJ, Gilbert JL, Urban RM. Corrosion of metal orthopaedic implants. J Bone Joint Surg Am. 1998;80:268–282. doi: 10.2106/00004623-199802000-00015. [DOI] [PubMed] [Google Scholar]
- 27.Jacobs JJ, Skipor AK, Patterson LM, Hallab NJ, Paprosky WG, Black J, Galante JO. Metal release in patients who have had a primary total hip arthroplasty. A prospective, controlled, longitudinal study. J Bone Joint Surg Am. 1998;80:1447–1458. doi: 10.2106/00004623-199810000-00006. [DOI] [PubMed] [Google Scholar]
- 28.Jacobs JJ, Urban RM, Gilbert JL, Skipor AK, Black J, Jasty M, Galante JO. Local and distant products from modularity. Clin Orthop Relat Res. 1995;319:94–105. [PubMed] [Google Scholar]
- 29.Jauch SY, Huber G, Haschke H, Sellenschloh K, Morlock MM. Design parameters and the material coupling are decisive for the micromotion magnitude at the stem-neck interface of bi-modular hip implants. Med Eng Phys. 2014;36:300–307. doi: 10.1016/j.medengphy.2013.11.009. [DOI] [PubMed] [Google Scholar]
- 30.Khair MM, Nam D, DiCarlo E, Su E. Aseptic lymphocyte dominated vasculitis-associated lesion resulting from trunnion corrosion in a cobalt-chrome unipolar hemiarthroplasty. J Arthroplasty. 2013;28(196):e11–e14. doi: 10.1016/j.arth.2012.04.010. [DOI] [PubMed] [Google Scholar]
- 31.Kurtz SM, Kocagoz SB, Hanzlik JA, Underwood RJ, Gilbert JL, MacDonald DW, Lee G-C, Mont MA, Kraay MJ, Klein GR, Parvizi J, Rimnac CM. Do ceramic femoral heads reduce taper fretting corrosion in hip arthroplasty? A retrieval study. Clin Orthop Relat Res. 2013;471:3270–3282. doi: 10.1007/s11999-013-3096-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Langton DJ, Sidaginamale R, Lord JK, Nargol AVF, Joyce TJ. Taper junction failure in large-diameter metal-on-metal bearings. Bone Joint Res. 2012;1:56–63. doi: 10.1302/2046-3758.14.2000047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Mathiesen EB, Lindgren JU, Blomgren GG, Reinholt FP. Corrosion of modular hip prostheses. J Bone Joint Surg Br. 1991;73:569–575. doi: 10.1302/0301-620X.73B4.2071637. [DOI] [PubMed] [Google Scholar]
- 34.Matthies AK, Racasan R, Bills P, Blunt L, Cro S, Panagiotidou A, Blunn G, Skinner J, Hart AJ. Material loss at the taper junction of retrieved large head metal-on-metal total hip replacements. J Orthop Res. 2013;31:1677–1685. doi: 10.1002/jor.22431. [DOI] [PubMed] [Google Scholar]
- 35.Nassif NA, Nawabi DH, Stoner K, Elpers M, Wright T, Padgett DE. Taper design affects failure of large-head metal-on-metal total hip replacements. Clin Orthop Relat Res. 2014;472:564–571. doi: 10.1007/s11999-013-3115-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Rehmer A, Bishop NE, Morlock MM. Influence of assembly procedure and material combination on the strength of the taper connection at the head-neck junction of modular hip endoprostheses. Clin Biomech (Bristol, Avon). 2012;27:77–83. [DOI] [PubMed]
- 37.Rodrigues DC, Urban RM, Jacobs JJ, Gilbert JL. In vivo severe corrosion and hydrogen embrittlement of retrieved modular body titanium alloy hip-implants. J Biomed Mater Res B Appl Biomater. 2009;88:206–219. doi: 10.1002/jbm.b.31171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Scully WF, Teeny SM. Pseudotumor associated with metal-on-polyethylene total hip arthroplasty. Orthopedics. 2013;36:e666–e670. doi: 10.3928/01477447-20130426-33. [DOI] [PubMed] [Google Scholar]
- 39.Svensson O, Mathiesen EB, Reinholt FP, Blomgren G. Formation of a fulminant soft-tissue pseudotumor after uncemented hip arthroplasty. A case report. J Bone Joint Surg Am. 1988;70:1238–1242. [PubMed] [Google Scholar]
- 40.Urban RM, Jacobs JJ, Gilbert JL, Galante JO. Migration of corrosion products from modular hip prostheses. Particle microanalysis and histopathological findings. J Bone Joint Surg Am. 1994;76:1345–1359. doi: 10.2106/00004623-199409000-00009. [DOI] [PubMed] [Google Scholar]
- 41.Willert HG, Semlitsch M. Tissue reactions to plastic and metallic wear products of joint endoprostheses. Clin Orthop Relat Res. 1996;333:4–14. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.