Abstract
Background
Most patients expect an improvement of walking ability and an increase in activity levels after TKA. Unfortunately, few studies report qualitative and quantitative activity improvements after TKA.
Questions/purposes
The aims of this study were (1) to evaluate quantity and quality of physical activity before and after TKA with an accelerometer, and to compare activity level with that of an age-matched control group without lower-extremity disorders. (2) Improvement in measured steps per day after TKA and the ability to meet physical activity guidelines were evaluated. (3) The influence of patient-specific and implant parameters were assessed.
Patients and Methods
An accelerometer was used to measure activity in 97 patients who were assessed before TKA and 1 year after TKA. The measurements included the total number of steps, moderate to vigorous activity defined as at least 100 steps per minute, and time spent lying, sitting/standing, or walking. We then calculated the proportion of patients who met the 10,000 steps per day guideline recommendation and determined factors that predicted failure to meet that goal. Thirty-nine age-matched control subjects without lower-extremity disorders were selected and underwent the same assessments using the accelerometer for comparison with patients 1 year after TKA.
Results
Measured steps per day improved from a mean of 5278 (SD, 2999) preoperatively to 6473 (SD, 3654) postoperatively (effect size, 1.23; 95% CI, 1.10–1.35; p < 0.001). Moderate to vigorous steps per day improved from a mean of 1150 (SD, 982) to 1935 (SD, 1728; p < 0.001). Times spent in lying, sitting, or standing position or during walking did not change after TKA. For all measured parameters, activity of the patients after TKA was considerably less than that of the age-matched control subjects, who walked a mean of 13,375 (SD, 4614) steps per day (p < 0.001), performed a mean of 6562 (SD, 3401) vigorous steps per day (p < 0.001), and spent a mean of 2.9 hours (SD, 1.1) per day walking (p < 0.001). Only 16 patients (16.5%) met physical activity guidelines after TKA. BMI (p = 0.017), sex (p = 0.027), and comorbidities (American Society of Anesthesiologists Grade, p = 0.042) were independent factors associated with steps per day after TKA.
Conclusions
One year after TKA, patients had increased walking and moderate to vigorous steps. However, only 16.5% achieved the guideline recommendations for walking activity. BMI, sex, and comorbidities are patient factors that are associated with activity after TKA. Even with improvements in walking, activity level after TKA remains less than that seen for age-matched control subjects. Surgeons should be aware of this when counseling patients undergoing TKA.
Level of Evidence
Level III, therapeutic study. See the Instructions for Authors for a complete description of levels of evidence.
Introduction
Deterioration of physical activity is common in patients with osteoarthritis of the knee. Most patients expect improvement of walking ability and an increase in activity levels after TKA [26, 29, 42]. Fulfillment of these expectations has an effect on patient satisfaction after surgery [42].
Physical activity has a positive effect on prevention of several chronic diseases [11, 55]. National guidelines recommend a certain amount of physical activity to obtain beneficial effects on general health [15, 41, 44, 49, 50]. These are mostly step based, and there is a consistent direction of a total number of 10,000 steps per day with a minimum of 30 minutes per day (or 150–210 minutes per week) of moderate to vigorous physical activity [15, 41, 44, 49, 50]. Moderate to vigorous activity is defined as more than 100 steps per minute [30, 37, 49]. Some studies report on physical activity in patients with osteoarthritis and after TKA [35, 54], but few report on step-based activity measurements before and after TKA [2, 53]. Although self-reporting of activity levels is commonly used (and is a part of many outcomes scoring instruments), self-reported data are subjective, not verifiable, vulnerable to recall bias, and therefore not very reliable [4, 17, 34]. More objective instruments involve the use of physical activity monitors, such as pedometers and accelerometers. A wide variety of these monitors are available commercially; we believe accelerometers are preferred as they measure activity more accurately [10, 23, 24, 38]. Patients with osteoarthritis had lower physical activity compared with control subjects [3, 6, 18, 56] and mainly were not able to meet physical activity guidelines [8]. Furthermore a relationship between age, obesity, inadequate diet, pain, and knee dysfunction with inactivity has been reported [18, 25, 36]. Studies regarding physical activity of patients before and after TKA showed an inconsistent increase of physical activity in the majority of their patients [2, 6, 20, 48, 51, 52]. One recent study did not find any improvement in accelerometer recorded physical activity in a cohort of 25 patients 6 months after TKA [14]. The authors concluded that patients did not necessarily change their physical activity behavior even if pain reduction and better function were accomplished. This suggests that patient-specific parameters might influence the amount of physical activity after TKA.
We therefore aimed to objectively quantify the influence of patient-specific parameters on activity before and after TKA through accelerometer recordings. Specific aims were to evaluate: (1) changes after TKA in terms of total numbers of daily steps, percent of moderate to vigorous steps, average times spent lying, sitting, standing, and walking, and to compare patients who had TKA after a year of recovery with an age-matched control group without lower-extremity disorders; (2) what proportion of patients who had TKA met physical activity guidelines of 10,000 steps per day including a minimum of 30 minutes of moderate to vigorous activity; and (3) factors that were associated with physical activity.
Patients and Methods
Study Design and Setting
For this prospective assessment of activity, patients included in a randomized study comparing two TKA implants were used [28]. Activity was measured with an accelerometer preoperatively and 1 year postoperatively. The results were compared with those of age-matched control subjects who had no lower-extremity pain or injury.
Study Participants
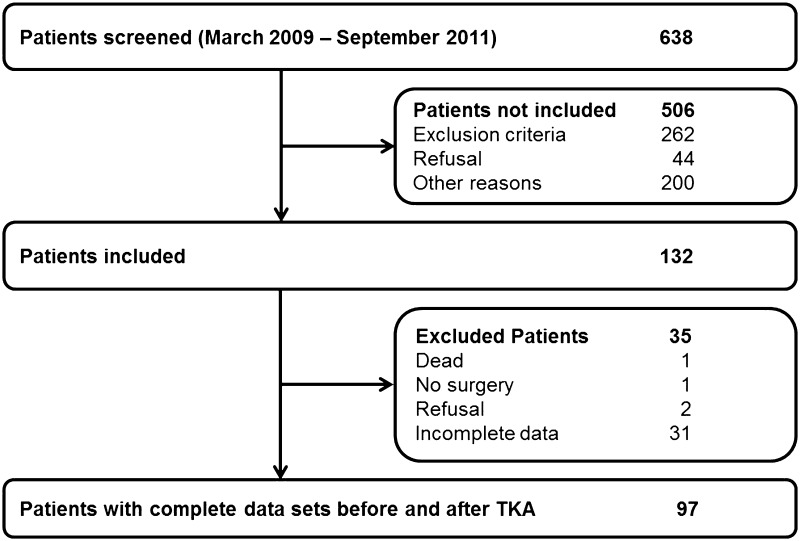
Between March 2009 and September 2011, all patients referred to our department for an unconstrained TKA (n = 638) were screened. Patients with varus or valgus malalignment greater than 15° were excluded (n = 76) as were patients who were involved in another study (n = 135) or were not able to understand and/or to comply with the study protocol (n = 51). All other patients were asked to participate; 44 declined, 200 had an implant or surgeon preference or needed a higher constraint implant, leaving 132 patients who consented to participate and who were included. All patients were interviewed by a trained study nurse 1 week preoperatively and 1 year postoperatively. The Knee Society Score [19] which consists of the Knee Score and the Function Score, each with a maximum of 100 points, was obtained by the same study nurse. Sociodemographic data (Table 1), operative details, and adverse events were documented for all patients. All patients were asked to wear an accelerometer 1 week preoperatively and at the 1-year followup. Patients were excluded from this study if preoperative activity data were incomplete, as there could be no comparison second measurement. At followup, patients with incomplete or lost activity data were asked to wear the monitor a second time (n = 42). Ninety-seven patients had complete preoperative and postoperative activity data that could be evaluated (73%) (Fig. 1).
Table 1.
Demographic data of the patients with TKA and control subjects*
| Variable | Patients with TKA (n = 97) | Control subjects (n = 39) | p value |
|---|---|---|---|
| Sex | |||
| Male | 52 (53.6%) | 16 (41.0%) | 0.703 |
| Female | 45 (46.4%) | 23 (59.0%) | |
| Age (years) | 68.9 (67.2–70.6) | 67.9 (65.3–70.7) | 0.568 |
| BMI (kg/m2) | 31.3 (30.3–32.3) | 24.1 (23.0–25.2) | < 0.001 |
| ASA | |||
| Grade 1 or 2 | 50 (51.5%) | 39 (100%) | < 0.001 |
| Grade 3 or 4 | 47 (48.5%) | 0 | |
| Implant | |||
| Standard | 43 (44.3%) | NA | NA |
| High flexion | 54 (55.7%) | NA | NA |
| Knee Society Knee Score | |||
| Preoperative | 45.9 (42.8–49.0) | NA | NA |
| Postoperative | 87.1 (84.6–89.6) | NA | NA |
| Knee Society Function Score | |||
| Preoperative | 52.5 (49.3–55.6) | NA | NA |
| Postoperative | 72.8 (69.3–76.5) | 97.7 (96.1–99.3) | < 0.001 |
* Mean (95% CI) for continuous variables, and absolute and relative frequencies for categorical variables; ASA = American Society of Anesthesiologists; NA = not applicable.
Fig. 1.
A flowchart of our patient selection is shown.
Physical activity was compared with that of an age-matched control group of 39 subjects who did not report any pain or previous surgeries in the lower extremities. These volunteers were recruited from a community-based exercise class. The Knee Society Function Score was obtained for comparison to that of the patients (Table 1).
Description of Experiment, Treatment, or Surgery
All operations were performed with the use of a tourniquet after one dose of antibiotics. A medial parapatellar approach with a measured resection technique was used in all cases. All components were cemented. Patellar resurfacing was not performed in any of the procedures. Implants were classified as standard and high-flexion (Scorpio and Scorpio NRG, Stryker, Mahwah, NJ, USA), which are FDA approved.
Variables, Outcome Measures, Data Sources, and Bias
Activity Measurement
The activPAL™ activity monitor (PAL Technologies, Glasgow, UK) is a comprehensively validated accelerometer [5, 12, 39, 45], lightweight (20 g), and measuring 53 × 35 × 7 mm. It includes an inclinometer. The accelerometer was attached over the anterolateral tibia, an appropriate position if the main outcome parameter is step number [27]. Preoperatively, the patients were instructed to wear the monitor for 4 consecutive days while awake and while sleeping (however, not during washing, showering, or bathing) under their clothes and secured by adhesive tape. They were briefed by a trained study nurse, given an additional instruction sheet, and returned the monitor on the day of their surgery. One year postoperatively, the monitor was sent to the patient 1 week before the followup.
Before each measurement, the monitor was charged and activated using the proprietary software package (activPAL™ Professional Research Edition). The software uses proprietary algorithms to transform the activity records into graphic or numeric formats, which can be exported to Microsoft Excel allowing detailed analyses [12]. For each measured day the summary of recorded steps and the time spent in lying, sitting and standing, or walking were analyzed. Furthermore the algorithms provide a division of the recorded steps owing to their intensity in decades, eg, number of steps in the intensity of 100 to 110 steps per minute. From this extended analyses the numbers of steps performed in moderate to vigorous activity (more than 100 steps per minute) could be calculated.
During the duration of the study, 16 separate monitors were used. Three monitors had to be replaced owing to technical errors. During all measurements (n = 301[132 measurements preoperative, 127 measurements postoperative, 42 repeated measurements – some of these repeat measurements were attributable to the activity data not being reproducible or the break between activity counts was too long]), 62 data sets were not recorded because of technical failure or lack of patient compliance, representing a 20.6% loss from the data collection. In the control group four of 43 measurements could not be analyzed, representing a 9.3% loss from the data collection.
Statistical Analysis, Study Size
Statistical Analysis
After each sampling the recorded data from each activPAL™ device was exported to Microsoft Excel (Microsoft Corp, Redmond, WA, USA) using proprietary software. For comparison to other studies, valid days have been defined as the continuous measure of activity counts during a minimum of 10 hours with an interruption less than 3 hours [9, 31, 32, 46]. All data were transferred to a database and analyzed using SPSS release 21 for Windows (SPSS Inc, Chicago, IL, USA). Endpoints of this investigation were differences in steps per day, moderate to vigorous intensity steps per day before and after surgery, and meeting the guideline on health-enhancing activity as described before. For the comparison of presurgical with postsurgical values, a one-sample paired t-test was used. Comparisons between groups were based on t-tests for continuous variables and on chi-square tests for categorical variables, respectively. The influence of different patient characteristics was evaluated by linear and logistic regression analysis, including age, sex, BMI, and type of implant. Results of these significance tests were summarized as p values, where a probability less than 0.05 indicates statistically significant differences between groups.
Results
Patients’ activity levels increased after compared with before TKA, but one year postoperative patients still had lower activity levels than age-matched control subjects. Overall, measured steps per day improved from a mean of 5278 (SD, 2999) preoperatively to 6473 (SD, 3654) postoperatively (effect size, 1.23; 95% CI, 1.10–1.35; p < 0.001). This is an improvement of 1195 steps per day (SD, 3224) and results in approximately 2.4 million steps per year (SD, 1.3 million steps). Moderate to vigorous steps per day improved from a mean of 1150 (SD, 982) to 1935 (SD, 1728; p < 0.001). This results in approximately 19 minutes of moderate to vigorous activity per day. Times spent in lying or sitting and standing positions or during walking did not change after TKA. Lying time was a mean 12.2 (SD, 2.4) hours per day preoperatively and 12.2 (SD, 2.7) at followup (p = 0.982). Sitting and standing time was a mean 10.8 (SD, 3.7) hours per day preoperatively and 10.3 (SD, 2.6) at followup (p = 0.258). Walking time was a mean 1.4 (SD, 1.3) hours per day preoperatively and 1.5 (SD, 0.8) hours at followup (p = 0.586). For all measured parameters, activity of the patients after TKA was considerably less than that of the age-matched control subjects (Table 2). The control subjects walked a mean of 13,375 (SD, 4614; p < 0.001) steps per day which represents approximately 4.9 (SD, 1.7) million steps per year. Furthermore they performed a mean of 6562 (SD, 3401) vigorous steps per day (p < 0.001) which results in approximately 66 minutes of moderate to vigorous activity per day. Control subjects spent a mean of 11.2 hours per day (SD, 1.5) in the lying position (p = 0.030), 9.9 hours (SD, 1.5) in sitting or standing position (p = 0.605), and 2.9 hours (SD, 1.1) walking (p < 0.001).
Table 2.
Physical activity of the patients and control subjects
| Variable | Patients with TKA n = 97 Mean (95% CI) |
Control subjects n = 39 Mean (95% CI) |
p value |
|---|---|---|---|
| Steps per day | 6473 (5737–7210) | 13,375 (11,879–14,871) | < 0.001 |
| Proportion of moderate to vigorous activity | 26.7% (23.2–30.1) | 47.6% (43.6–51.7) | < 0.001 |
| Hours lying | 12.2 (11.6–12.7) | 11.2 (10.6–11.7) | 0.030 |
| Hours sitting and standing | 10.3 (9.8–10.8) | 10.1 (9.6–10.6) | 0.605 |
| Hours walking | 1.5 (1.3–1.7) | 2.7 (2.5–3.0) | < 0.001 |
The majority of patients did not meet health-enhancing physical activity guideline recommendations. After TKA, only 16 patients (16.5%) achieved the recommended quantity and quality of activity. An additional four patients achieved at least 80% of the recommended activity (8000 steps per day including 2400 moderate to vigorous steps), which means that 79.4% of all patients did not achieve at least 80% of the recommended activity after TKA.
Patient factors had an influence on activity after TKA (Table 3). In a linear multivariate model BMI (p = 0.017), sex (p = 0.027), and comorbidities (American Society of Anesthesiologists [ASA] Grade, p = 0.042) were independent factors associated with the number of steps per day after TKA, but not age at surgery (p = 0.071) or implant type (p = 0.970). The proportion of moderate to vigorous activity was not different after surgery after stratification for these parameters (Table 4). Taking recommended health-enhancing physical activity as outcome parameter, fewer comorbidities (ASA Grade 1 or 2, p = 0.007) and male gender (p = 0.043) were independent factors associated with achieving this goal.
Table 3.
Number of steps per day
| Patient factors | Amounts per factor Mean (95% CI) | p value | |
|---|---|---|---|
| Male (n = 45) | Female (n = 52) | ||
| Sex | |||
| Preoperative | 6026 (5083–6968) | 4630 (3867–5394) | 0.022 |
| Followup | 7471 (6294–8648) | 5610 (4718–6501) | 0.012 |
| Age | ≤ 70 years (n = 49) | > 70 years (n = 48) | |
| Preoperative | 5688 (4693–6682) | 4859 (4161–5557) | 0.175 |
| Followup | 6716 (5449–7983) | 6225 (5443–7008) | 0.511 |
| BMI | < 30 (n = 42) | ≥ 30 (n = 55) | |
| Preoperative | 5445 (4548–6342) | 5150 (4309–5990) | 0.634 |
| Followup | 7387 (6177–8598) | 5775 (4873–6677) | 0.031 |
| Comorbidities | ASA Grade 1or 2 (n = 50) | ASA Grade 3 or 4 (n = 47) | |
| Preoperative | 5841 (4966–6715) | 4679 (3849–5508) | 0.056 |
| Followup | 7676 (6530–8822) | 5194 (4401–5987) | 0.001 |
| Implant | Standard (n = 43) | High-flexion (n = 54) | |
| Preoperative | 5490 (4516–6465) | 5108 (4323–5894) | 0.536 |
| Followup | 6330 (5289–7371) | 6587 (5527–7648) | 0.732 |
ASA = American Society of Anesthesiologists.
Table 4.
Proportion of moderate to vigorous activity per day (%)
| Patient factors | Amounts per factor Mean (95% CI) | p value | |
|---|---|---|---|
| Male (n = 45) | Female (n = 52) | ||
| Sex | |||
| Preoperative | 21.1 (17.8–24.3) | 18.2 (14.7–21.7) | 0.233 |
| Followup | 27.8 (23.7–31.8) | 25.7 (20.2–31.2) | 0.559 |
| Age | ≤ 70 years (n = 49) | > 70 years (n = 48) | |
| Preoperative | 21.4 (18.0–24.7) | 17.7 (14.2–21.1) | 0.126 |
| Followup | 27.6 (22.7–32.4) | 25.8 (20.7–30.8) | 0.613 |
| BMI | < 30 (n = 42) | ≥ 30 (n = 55) | |
| Preoperative | 19.2 (15.4–22.9) | 19.8 (16.6–23.0) | 0.790 |
| Followup | 29.7 (24.4–35.1) | 24.3 (19.8–28.8) | 0.120 |
| Comorbidities | ASA Grade 1or 2 (n = 50) | ASA Grade 3 or 4 (n = 47) | |
| Preoperative | 21.9 (18.7–25.1) | 16.9 (13.4–20.5) | 0.040 |
| Followup | 29.6 (25.2–34.1) | 23.5 (18.2–28.9) | 0.079 |
| Implant | Standard (n = 43) | High-flexion (n = 54) | |
| Preoperative | 21.7 (17.9–25.6) | 17.8 (14.7–20.8) | 0.100 |
| Followup | 26.0 (21.3–30.8) | 27.2 (22.2–32.2) | 0.736 |
ASA = American Society of Anesthesiologists.
Discussion
Improvement in physical activity is a major expectation of patients undergoing knee surgery [26, 29, 42], and fulfillment has an influence on patient satisfaction [42]. Therefore it is important to know if and how activity improves after major surgery such as a TKA. Although some studies have looked at objectively measured activity levels after knee arthroplasty [22, 40, 43, 48, 58], others have compared measurements before and after TKA [2, 6, 14, 16, 33, 51–53]. These studies were limited by the number of patients, short postoperative followup, and few were step based [2, 51, 53]. We therefore used accelerometer-based activity measurements to evaluate changes in step number and intensity after TKA and to compare these patients after a year of recovery with an age-matched control group without lower-extremity disorders. Furthermore we evaluated what proportion of patients who had TKAs met physical activity guidelines and which patient-specific factors were associated with physical activity.
Limitations of this study include increased inaccuracy of the activity monitor at very slow velocities. However, these measurements have greater accuracy than self-reported activity questionnaires. The activity on the recorded days might not always reflect typical days. However, a 3- to 7-day monitoring period has been suggested to provide sufficient data regarding activity behavior [31, 47]. Patients taking part in a study about activity might change their normal behavior and measurements might not always reflect the real activity. Furthermore, 20.6% of the data could not be analyzed owing to technical errors or inadequate patient compliance. However, the number of patients is greater than in previous studies reporting longitudinal data [2, 6, 14, 51–53] . The 1-year followup might not always reflect maximum functional benefit after TKA, but for most patients this is sufficient time to assess major functional improvement. Finally, there is a risk of selection bias as many eligible patients were not included for different reasons.
Improvement in the number of steps per day was 22.6% in our patients. This is consistent with the results of Brandes et al. [2] who reported an 18.8% improvement in the number of steps of 44 patients from preoperative to 1 year after TKA. Walker et al. [53] measured steps in 19 patients before and 3 and 6 months after TKA and reported a 55% improvement in the total number of steps per day at the latest followup. However, measurements were performed for one day only, which is less than recommended. Other studies measured steps after TKA only [33, 40, 43, 48, 58]. The total numbers of steps per day varied from 3518 [48] to 15,641 [53] at different followup periods. Some of these studies used pedometers which are considered less accurate in detecting step numbers [10, 24, 38]. Furthermore, measurements early after TKA might not always reflect full recovery. A followup of at least 1 year has been suggested to be sufficient [57]. Daily time of activity did not change after surgery in our patients, which is consistent with the results of other studies [7, 14, 51]. In comparison to patients who had TKAs, the age-matched control subjects were considerably more active. The total number of 13,375 steps per day is consistent with other studies that had a control group [3, 56]. This suggests that although patients benefit from TKA in terms of pain relief and functional improvement, this does not result in activity comparable to that of control subjects. Although moderate to vigorous walking ability increased, patients might not be willing to change their activity behavior [14].
The total number of steps taken at followup was considerably fewer than guideline recommendations [15, 41, 44, 49, 50]. Moderate to vigorous activity, as part of the recommendation for health-enhancing activity, showed more pronounced improvement but still was less than the recommended 30 minutes per day at followup. Only 16.5% of our patients reached the recommended activity. A recent study [14] reported that only one of 52 patients met American Physical Activity Guidelines after THA or TKA. The total number of steps per day reported in other studies was considerably below the recommended number [33, 40, 43, 48], as in our patients. The mean number of steps was reported as being greater than the recommended 10,000 steps per day in only two studies [2, 53]. Therefore the majority of patients might not reach recommended health-enhancing activity levels after TKA. Two studies that used questionnaires to assess physical activity postoperatively found nearly ½ of the observed patients who had TKAs met recommended activity guidelines [13, 21]. As self-reported data are more unreliable, these data should be viewed with caution as reported before [53].
In all studies the standard deviations of step-based measured activity are large, suggesting there are considerable differences between patients. In our study obesity, female sex, and comorbidities were related to reduced activity, measured as total step number. While the increase in step number per day was approximately the same for male and female patients, there was a more pronounced increase in nonobese compared with obese patients and patients with fewer comorbidities (ASA Grades 1 and 2) compared with those with more comorbidities (ASA Grades 3 and 4). This is consistent with previous studies that have reported age, sex, and BMI to be associated with activity [33, 40, 58]. Although one recent study showed decreased activity with increasing age [1], this was not an independent factor for step-based activity in our patients. This is consistent with the results of another study of objectively measured activity level after TKA [51] which did not find any difference related to age. Improvement in moderate to vigorous activity was consistent for all patients in our study. This suggests that all patients, regardless of BMI, sex, comorbidities, or age, benefited from TKA, but not all were willing to change their activity behavior in terms of walking more steps per day. This is consistent with the results of Harding et al. [14], who did not find any change in activity after TKA.
Our study showed moderate improvement in the total number of steps and moderate to vigorous walking but no change in daily walking time. After 1 year, the patients who had a TKA walked only approximately ½ as many steps as the age-matched control subjects. Most patients did not meet the recommendation for health-enhancing activity levels. Female sex, obesity, and comorbidities were found to be predictive factors that were associated with daily step number after TKA. This should be kept in mind when counseling patients before TKA. To avoid overextended expectations surgeons should consider a patient’s motivation to participate in a more active lifestyle. Further research is required to better understand the factors influencing physical activity after successful surgery.
Acknowledgments
We thank Brit Brethfeld and Heike Voigt (Department of Orthopaedic Surgery, University Hospital Carl Gustav Carus, Dresden, Germany) for valuable assistance during followup and data management.
Footnotes
The institution of the authors (CL, SK, JL) has received, during the study period, funding from Stryker Orthopaedics (Mahwah, NJ, USA) directly related to this study. Each author certifies that he or she, or a member of his or her immediate family, has no funding or commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research editors and board members are on file with the publication and can be viewed on request.
Each author certifies that his or her institution approved the human protocol for this investigation, that all investigations were conducted in conformity with ethical principles of research, and that informed consent for participation in the study was obtained.
Clinical Orthopaedics and Related Research neither advocates nor endorses the use of any treatment, drug, or device. Readers are encouraged to always seek additional information, including FDA-approval status, of any drug or device prior to clinical use.
References
- 1.Battenberg AK, Hopkins JS, Kupiec AD, Schmalzried TP. The 2012 Frank Stinchfield Award: Decreasing patient activity with aging: implications for crosslinked polyethylene wear. Clin Orthop Relat Res. 2013;471:386–392. doi: 10.1007/s11999-012-2497-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Brandes M, Ringling M, Winter C, Hillmann A, Rosenbaum D. Changes in physical activity and health-related quality of life during the first year after total knee arthroplasty. Arthritis Care Res (Hoboken). 2011;63:328–334. doi: 10.1002/acr.20384. [DOI] [PubMed] [Google Scholar]
- 3.Brandes M, Schomaker R, Mollenhoff G, Rosenbaum D. Quantity versus quality of gait and quality of life in patients with osteoarthritis. Gait Posture. 2008;28:74–79. doi: 10.1016/j.gaitpost.2007.10.004. [DOI] [PubMed] [Google Scholar]
- 4.Coughlin SS. Recall bias in epidemiologic studies. J Clin Epidemiol. 1990;43:87–91. doi: 10.1016/0895-4356(90)90060-3. [DOI] [PubMed] [Google Scholar]
- 5.Dahlgren G, Carlsson D, Moorhead A, Hager-Ross C, McDonough SM. Test-retest reliability of step counts with the ActivPAL™ device in common daily activities. Gait Posture. 2010;32:386–390. doi: 10.1016/j.gaitpost.2010.06.022. [DOI] [PubMed] [Google Scholar]
- 6.de Groot IB, Bussmann HJ, Stam HJ, Verhaar JA. Small increase of actual physical activity 6 months after total hip or knee arthroplasty. Clin Orthop Relat Res. 2008;466:2201–2208. doi: 10.1007/s11999-008-0315-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.de Groot IB, Bussmann JB, Stam HJ, Verhaar JA. Actual everyday physical activity in patients with end-stage hip or knee osteoarthritis compared with healthy controls. Osteoarthritis Cartilage. 2008;16:436–442. doi: 10.1016/j.joca.2007.08.010. [DOI] [PubMed] [Google Scholar]
- 8.Dunlop DD, Song J, Semanik PA, Chang RW, Sharma L, Bathon JM, Eaton CB, Hochberg MC, Jackson RD, Kwoh CK, Mysiw WJ, Nevitt MC, Hootman JM. Objective physical activity measurement in the osteoarthritis initiative: are guidelines being met? Arthritis Rheum. 2011;63:3372–3382. doi: 10.1002/art.30562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Esliger DW, Tremblay MS, Copeland JL, Barnes JD, Huntington GE, Bassett DR., Jr Physical activity profile of Old Order Amish, Mennonite, and contemporary children. Med Sci Sports Exerc. 2010;42:296–303. doi: 10.1249/MSS.0b013e3181b3afd2. [DOI] [PubMed] [Google Scholar]
- 10.Feito Y, Bassett DR, Thompson DL. Evaluation of activity monitors in controlled and free-living environments. Med Sci Sports Exerc. 2012;44:733–741. doi: 10.1249/MSS.0b013e3182351913. [DOI] [PubMed] [Google Scholar]
- 11.Garber CE, Blissmer B, Deschenes MR, Franklin BA, Lamonte MJ, Lee IM, Nieman DC, Swain DP, American College of Sports Medicine Quantity and quality of exercise for developing and maintaining cardiorespiratory, musculoskeletal, and neuromotor fitness in apparently healthy adults: guidance for prescribing exercise. Med Sci Sports Exerc. 2011;43:1334–1359. doi: 10.1249/MSS.0b013e318213fefb. [DOI] [PubMed] [Google Scholar]
- 12.Grant PM, Ryan CG, Tigbe WW, Granat MH. The validation of a novel activity monitor in the measurement of posture and motion during everyday activities. Br J Sports Med. 2006;40:992–997. doi: 10.1136/bjsm.2006.030262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Groen JW, Stevens M, Kersten RF, Reininga IH, van den Akker-Scheek I. After total knee arthroplasty, many people are not active enough to maintain their health and fitness: an observational study. J Physiother. 2012;58:113–116. doi: 10.1016/S1836-9553(12)70091-7. [DOI] [PubMed] [Google Scholar]
- 14.Harding P, Holland AE, Delany C, Hinman RS. Do activity levels increase after total hip and knee arthroplasty? Clin Orthop Relat Res. 2014;472:1502–1511. doi: 10.1007/s11999-013-3427-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Haskell WL, Lee IM, Pate RR, Powell KE, Blair SN, Franklin BA, Macera CA, Heath GW, Thompson PD, Bauman A. Physical activity and public health: updated recommendation for adults from the American College of Sports Medicine and the American Heart Association. Circulation. 2007;116:1081–1093. doi: 10.1161/CIRCULATIONAHA.107.185649. [DOI] [PubMed] [Google Scholar]
- 16.Hayes DA, Watts MC, Anderson LJ, Walsh WR. Knee arthroplasty: a cross-sectional study assessing energy expenditure and activity. ANZ J Surg. 2011;81:371–374. doi: 10.1111/j.1445-2197.2010.05570.x. [DOI] [PubMed] [Google Scholar]
- 17.Hertogh EM, Monninkhof EM, Schouten EG, Peeters PH, Schuit AJ. Validity of the modified Baecke questionnaire: comparison with energy expenditure according to the doubly labeled water method. Int J Behav Nutr Phys Act. 2008;5:30. doi: 10.1186/1479-5868-5-30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Holsgaard-Larsen A, Roos EM. Objectively measured physical activity in patients with end stage knee or hip osteoarthritis. Eur J Phys Rehabil Med. 2012;48:577–585. [PubMed] [Google Scholar]
- 19.Insall JN, Dorr LD, Scott RD, Scott WN. Rationale of the Knee Society clinical rating system. Clin Orthop Relat Res. 1989;248:13–14. [PubMed] [Google Scholar]
- 20.Keeney JA, Nunley RM, Wright RW, Barrack RL, Clohisy JC. Are younger patientsundergoing TKAs appropriately characterized as active? Clin Orthop Relat Res. 2014;472:1210–1216. doi: 10.1007/s11999-013-3376-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kersten RF, Stevens M, van Raay JJ, Bulstra SK, Akker-Scheek I. Habitual physical activity after total knee replacement. Phys Ther. 2012;92:1109–1116. doi: 10.2522/ptj.20110273. [DOI] [PubMed] [Google Scholar]
- 22.Krenk L, Jennum P, Kehlet H. Activity, sleep and cognition after fast-track hip or knee arthroplasty. J Arthroplasty. 2013;28:1265–1269. doi: 10.1016/j.arth.2013.02.013. [DOI] [PubMed] [Google Scholar]
- 23.Le Masurier GC, Lee SM, Tudor-Locke C. Motion sensor accuracy under controlled and free-living conditions. Med Sci Sports Exerc. 2004;36:905–910. doi: 10.1249/01.MSS.0000126777.50188.73. [DOI] [PubMed] [Google Scholar]
- 24.Le Masurier GC, Tudor-Locke C. Comparison of pedometer and accelerometer accuracy under controlled conditions. Med Sci Sports Exerc. 2003;35:867–871. doi: 10.1249/01.MSS.0000064996.63632.10. [DOI] [PubMed] [Google Scholar]
- 25.Lee J, Song J, Hootman JM, Semanik PA, Chang RW, Sharma L, van Horn L, Bathon JM, Eaton CB, Hochberg MC, Jackson R, Kwoh CK, Mysiw WJ, Nevitt M, Dunlop DD. Obesity and other modifiable factors for physical inactivity measured by accelerometer in adults with knee osteoarthritis. Arthritis Care Res (Hoboken). 2013;65:53–61. doi: 10.1002/acr.21754. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Lingard EA, Sledge CB, Learmonth ID, Kinemax Outcomes Group Patient expectations regarding total knee arthroplasty: differences among the United States, United Kingdom, and Australia. J Bone Joint Surg Am. 2006;88:1201–1207. doi: 10.2106/JBJS.E.00147. [DOI] [PubMed] [Google Scholar]
- 27.Lützner C, Voigt H, Roeder I, Kirschner S, Lützner J. Placement makes a difference: accuracy of an accelerometer in measuring step number and stair climbing. Gait Posture. 2014;39:1126–1132. doi: 10.1016/j.gaitpost.2014.01.022. [DOI] [PubMed] [Google Scholar]
- 28.Lützner J, Hartmann A, Lützner C, Kirschner S. Is range of motion after cruciate retaining total knee arthroplasty influenced by prosthesis design? A prospective randomized trial. J Arthroplasty. 2014;29:961–965. doi: 10.1016/j.arth.2013.09.046. [DOI] [PubMed] [Google Scholar]
- 29.Mancuso CA, Sculco TP, Wickiewicz TL, Jones EC, Robbins L, Warren RE, Williams Russo P. Patients’ expectations of knee surgery. J Bone Joint Surg Am. 2001;83:1005–1012. doi: 10.1302/0301-620X.83B7.12105. [DOI] [PubMed] [Google Scholar]
- 30.Marshall SJ, Levy SS, Tudor-Locke CE, Kolkhorst FW, Wooten KM, Ji M, Macera CA, Ainsworth BE. Translating physical activity recommendations into a pedometer-based step goal: 3000 steps in 30 minutes. Am J Prev Med. 2009;36:410–415. doi: 10.1016/j.amepre.2009.01.021. [DOI] [PubMed] [Google Scholar]
- 31.Matthews CE, Hagstromer M, Pober DM, Bowles HR. Best practices for using physical activity Monitors in population-based research. Med Sci Sports Exerc. 2012;44(1 suppl):S68–S76. doi: 10.1249/MSS.0b013e3182399e5b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Mattocks C, Ness A, Leary S, Tilling K, Blair SN, Shield J, Deere K, Saunders J, Kirkby J, Smith GD, Wells J, Wareham N, Reilly J, Riddoch C. Use of accelerometers in a large field-based study of children: protocols, design issues, and effects on precision. J Phys Act Health. 2008;5(suppl 1):S98–S111. doi: 10.1123/jpah.5.s1.s98. [DOI] [PubMed] [Google Scholar]
- 33.McClung CD, Zahiri CA, Higa JK, Amstutz HC, Schmalzried TP. Relationship between body mass index and activity in hip or knee arthroplasty patients. J Orthop Res. 2000;18:35–39. doi: 10.1002/jor.1100180106. [DOI] [PubMed] [Google Scholar]
- 34.Müller C, Winter C, Rosenbaum D. [Current objective techniques for physical activity assessment in comparison with subjective methods][in German] Deutsche Z Sportmed. 2010;61:11–18. [Google Scholar]
- 35.Naal FD, Impellizzeri FM. How active are patients undergoing total joint arthroplasty?: A systematic review. Clin Orthop Relat Res. 2010;468:1891–1904. doi: 10.1007/s11999-009-1135-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Robbins SM, Birmingham TB, Callaghan JP, Jones GR, Chesworth BM, Maly MR. Association of pain with frequency and magnitude of knee loading in knee osteoarthritis. Arthritis Care Res (Hoboken). 2011;63:991–997. doi: 10.1002/acr.20476. [DOI] [PubMed] [Google Scholar]
- 37.Rowe DA, Welk GJ, Heil DP, Mahar MT, Kemble CD, Calabro MA, Camenisch K. Stride rate recommendations for moderate-intensity walking. Med Sci Sports Exerc. 2011;43:312–318. doi: 10.1249/MSS.0b013e3181e9d99a. [DOI] [PubMed] [Google Scholar]
- 38.Rowlands AV, Stone MR, Eston RG. Influence of speed and step frequency during walking and running on motion sensor output. Med Sci Sports Exerc. 2007;39:716–727. doi: 10.1249/mss.0b013e318031126c. [DOI] [PubMed] [Google Scholar]
- 39.Ryan CG, Grant PM, Tigbe WW, Granat MH. The validity and reliability of a novel activity monitor as a measure of walking. Br J Sports Med. 2006;40:779–784. doi: 10.1136/bjsm.2006.027276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Schmalzried TP, Szuszczewicz ES, Northfield MR, Akizuki KH, Frankel RE, Belcher G, Amstutz HC. Quantitative assessment of walking activity after total hip or knee replacement. J Bone Joint Surg Am. 1998;80:54–59. doi: 10.1302/0301-620X.80B1.7739. [DOI] [PubMed] [Google Scholar]
- 41.Schneider PL, Bassett DR, Jr, Thompson DL, Pronk NP, Bielak KM. Effects of a 10,000 steps per day goal in overweight adults. Am J Health Promot. 2006;21:85–89. doi: 10.4278/0890-1171-21.2.85. [DOI] [PubMed] [Google Scholar]
- 42.Scott CE, Bugler KE, Clement ND, MacDonald D, Howie CR, Biant LC. Patient expectations of arthroplasty of the hip and knee. J Bone Joint Surg Br. 2012;94:974–981. doi: 10.1302/0301-620X.94B7.28219. [DOI] [PubMed] [Google Scholar]
- 43.Silva M, McClung CD, Dela Rosa MA, Dorey FJ, Schmalzried TP. Activity sampling in the assessment of patients with total joint arthroplasty. J Arthroplasty. 2005;20:487–491. doi: 10.1016/j.arth.2004.08.013. [DOI] [PubMed] [Google Scholar]
- 44.Sisson SB, Camhi SM, Tudor-Locke C, Johnson WD, Katzmarzyk PT. Characteristics of step-defined physical activity categories in U.S. adults. Am J Health Promot. 2012;26:152–159. doi: 10.4278/ajhp.100326-QUAN-95. [DOI] [PubMed] [Google Scholar]
- 45.Taraldsen K, Askim T, Sletvold O, Einarsen EK, Bjastad KG, Indredavik B, Helbostad JL. Evaluation of a body-worn sensor system to measure physical activity in older people with impaired function. Phys Ther. 2011;91:277–285. doi: 10.2522/ptj.20100159. [DOI] [PubMed] [Google Scholar]
- 46.Troiano RP, Berrigan D, Dodd KW, Masse LC, Tilert T, McDowell M. Physical activity in the United States measured by accelerometer. Med Sci Sports Exerc. 2008;40:181–188. doi: 10.1249/mss.0b013e31815a51b3. [DOI] [PubMed] [Google Scholar]
- 47.Trost SG, McIver KL, Pate RR. Conducting accelerometer-based activity assessments in field-based research. Med Sci Sports Exerc. 2005;37(11 suppl):S531–S543. doi: 10.1249/01.mss.0000185657.86065.98. [DOI] [PubMed] [Google Scholar]
- 48.Tsonga T, Kapetanakis S, Papadopoulos C, Papathanasiou J, Mourgias N, Georgiou N, Fiska A, Kazakos K. Evaluation of improvement in quality of life and physical activity after total knee arthroplasty in Greek elderly women. Open Orthop J. 2011;5:343–347. doi: 10.2174/1874325001105010343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Tudor-Locke C, Craig CL, Brown WJ, Clemes SA, De Cocker K, Giles-Corti B, Hatano Y, Inoue S, Matsudo SM, Mutrie N, Oppert JM, Rowe DA, Schmidt MD, Schofield GM, Spence JC, Teixeira PJ, Tully MA, Blair SN. How many steps/day are enough? For adults. Int J Behav Nutr Phys Act. 2011;8:79. doi: 10.1186/1479-5868-8-79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Tudor-Locke C, Hatano Y, Pangrazi RP, Kang M. Revisiting, “how many steps are enough?”. Med Sci Sports Exerc. 2008;40(7 suppl):S537–S543. doi: 10.1249/MSS.0b013e31817c7133. [DOI] [PubMed] [Google Scholar]
- 51.Vissers MM, Bussmann JB, de Groot IB, Verhaar JA, Reijman M. Physical functioning four years after total hip and knee arthroplasty. Gait Posture. 2013;38:310–315. doi: 10.1016/j.gaitpost.2012.12.007. [DOI] [PubMed] [Google Scholar]
- 52.Vissers MM, de Groot IB, Reijman M, Bussmann JB, Stam HJ, Verhaar JA. Functional capacity and actual daily activity do not contribute to patient satisfaction after total knee arthroplasty. BMC Musculoskelet Disord. 2010;11:121. doi: 10.1186/1471-2474-11-121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Walker DJ, Heslop PS, Chandler C, Pinder IM. Measured ambulation and self-reported health status following total joint replacement for the osteoarthritic knee. Rheumatology (Oxford). 2002;41:755–758. doi: 10.1093/rheumatology/41.7.755. [DOI] [PubMed] [Google Scholar]
- 54.Wallis JA, Webster KE, Levinger P, Taylor NF. What proportion of people with hip and knee osteoarthritis meet physical activity guidelines? A systematic review and meta-analysis. Osteoarthritis Cartilage. 2013;21:1648–1659. doi: 10.1016/j.joca.2013.08.003. [DOI] [PubMed] [Google Scholar]
- 55.Ward DS, Evenson KR, Vaughn A, Rodgers AB, Troiano RP. Accelerometer use in physical activity: best practices and research recommendations. Med Sci Sports Exerc. 2005;37(11 suppl):S582–S588. doi: 10.1249/01.mss.0000185292.71933.91. [DOI] [PubMed] [Google Scholar]
- 56.Winter CC, Brandes M, Müller C, Schuber T, Ringling M, Hillmann A, Rosenbaum D, Schulte TL. Walking ability during daily life in patients with osteoarthritis of the knee or the hip and lumbar spinal stenosis: a cross sectional study. BMC Musculoskelet Disord. 2010;11:233. doi: 10.1186/1471-2474-11-233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Wollmerstedt N, Glatzel M, Kirschner S, Schneider J, Faller H, Konig A. [Comparative analysis of patient-centered outcome of total hip and knee arthroplasty][in German] Z Orthop Ihre Grenzgeb. 2006;144:464–471. doi: 10.1055/s-2006-942241. [DOI] [PubMed] [Google Scholar]
- 58.Zahiri CA, Schmalzried TP, Szuszczewicz ES, Amstutz HC. Assessing activity in joint replacement patients. J Arthroplasty. 1998;13:890–895. doi: 10.1016/S0883-5403(98)90195-4. [DOI] [PubMed] [Google Scholar]