Abstract
Background
Triangular fibrocartilage complex abnormalities seem to be more common with age, but the degree to which this is so, and the degree to which the presence of an abnormality is associated with symptoms, are topics of controversy.
Questions/purposes
We wished to perform a systematic review to determine the prevalence of triangular fibrocartilage complex abnormalities, and to determine if the prevalence of abnormalities are greater with increasing age. In addition, we stratified age groups based on symptoms.
Methods
We searched MEDLINE, EMBASE, and the Cochrane Library through August 15, 2013. Studies that reported triangular fibrocartilage complex abnormalities by age were included. Fifteen studies including 977 wrists met our criteria and reported a total of 368 (38%) triangular fibrocartilage complex abnormalities. Eight studies included symptomatic patients; the remainder studied cadavers (six studies) or asymptomatic volunteers (one study). Patients were divided into four age groups (< 30, 30–49, 50–69, and 70 years and older) for pooled analysis, comparing the proportions of patients with and without abnormalities between groups using chi-square analysis. We also evaluated the proportions after stratifying each age group by symptoms.
Results
Overall, the prevalence of triangular fibrocartilage complex abnormalities increased with age, from 27% (80/301) in patients younger than 30 years to 49% (130/265) in patients 70 years and older (p < 0.001), odds ratio (OR), 2.7, 95% CI, 1.9–3.8 (p < 0.001). In asymptomatic patients, triangular fibrocartilage complex prevalence abnormality increased from 15% (24/159) to 49% (129/263) in the same age groups (p < 0.001), OR, 5.4, 95% CI, 3.3–8.9 (p < 0.001). For symptomatic patients prevalence ranged from 39% (56/142) to 70% (14/20) in patients between 50 and 69 years old (p < 0.034), OR, 3.6, 95% CI, 1.3–9.9 (p < 0.014).
Conclusion
Triangular fibrocartilage complex abnormalities are common in symptomatic and asymptomatic wrists, and they are increasingly common with age. As in all situations where abnormalities are so common that they may be incidental, we need (1) a reliable and accurate method for determining whether these abnormalities are the cause of symptoms; and (2) evidence that treatment of these abnormalities improves symptoms better than placebo.
Level of Evidence
Level III, prognostic study. See the Instructions for Authors for a complete description of levels of evidence.
Electronic supplementary material
The online version of this article (doi:10.1007/s11999-014-3825-1) contains supplementary material, which is available to authorized users.
Introduction
Triangular fibrocartilage complex abnormalities are common in symptomatic [13, 22] and asymptomatic wrists [10, 12] and in affected and unaffected wrists in the same patient [4, 5]. Moreover, triangular fibrocartilage complex abnormalities seem increasingly common with age [10, 11, 16, 25]. Signal abnormalities on MRI and pathophysiology identified on wrist arthroscopy tend to be interpreted as “tears”, but as with lower back pain, wrist pain is common and often difficult to relate to a specific pathophysiology. A substantial percentage of displaced fractures of the distal radius are associated with traumatic injury to the triangular fibrocartilage complex, but these traumatic lesions rarely are repaired and seem to have little or no long-term consequences [19].
These observations have raised questions concerning the relevance of triangular fibrocartilage complex abnormalities in the diagnosis of wrist pain. Using the word “tear” to describe the variations identified with diagnostic studies might reinforce the maladaptive coping strategy of catastrophic thinking. The word tear suggests damage needing repair. If triangular fibrocartilage complex abnormalities are part of normal human aging and are common in symptomatic and asymptomatic patients, then the likelihood that a triangular fibrocartilage complex abnormality is incidental to the cause of symptoms may be high. The realization that triangular fibrocartilage complex abnormalities are part of normal ageing and that surgery potentially is unhelpful or unnecessary may decrease the appeal of operative treatment.
Our aim was to perform a systematic review to determine the prevalence of triangular fibrocartilage complex abnormalities, and to determine if the prevalence of abnormalities is greater with increasing age. In addition, we stratified age groups based on symptoms.
Materials & Methods
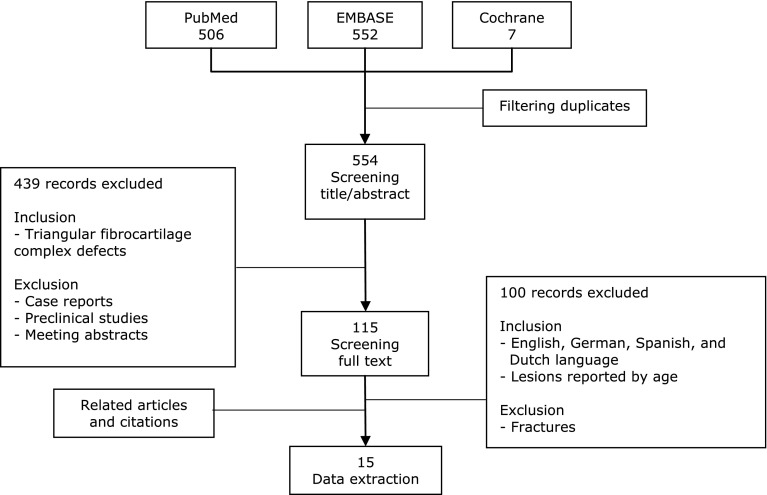
We searched PUBMED, EMBASE, and the Cochrane Library up to August 15, 2013, using the search string for title and abstract: (TFCC OR triangular fibrocartilage) AND (degeneration* OR tear*[Title/Abstract]) OR disruption* OR perforation* OR injur*). This yielded 506 results from PubMed, 552 from EMBASE, and seven from the Cochrane Library. Two of the reviewers (JJC, TT) examined the title and abstract for each result from the databases, and subsequently screened the full texts of eligible articles. They also scanned the reference lists for additional studies that met the inclusion criteria (Fig. 1). We included studies that established triangular fibrocartilage complex abnormalities by individual patient’s age in English, Dutch, German, or Spanish language. Case reports, meeting abstracts, preclinical studies, and fracture studies were excluded. We found no overlapping patient cohorts.
Fig. 1.
A flow chart of our study selection is shown.
Two reviewers independently extracted study data using standardized sheets. Discordant judgments were resolved by consensus discussion between the two reviewers. Our review is registered with PROSPERO, registration number: CRD42013006546 (Appendix 1. Supplemental material is available with the online version of CORR®).
After removal of duplicates, our search identified 554 publications of which 115 were potentially eligible based on their title and abstract. After reading the full text, 15 articles were included in our final analysis (Fig. 1).
Eight studies included patients who presented with pain or clicking symptoms. The other ½ included asymptomatic patients (n = 1) or cadavers (n = 6). Abnormalities were identified by arthrotomy (n = 5), arthroscopy (n = 5), arthrography (n = 1), CT (n = 1), and MRI (n = 3). The definition of triangular fibrocartilage complex abnormalities varied across studies (Table 1).
Table 1.
Study characteristics
| Study | Wrists (number per age group) | Age (years) (median, interquartile range) | Type of study | NOS | Symptomatic | Method of identification | Definition of abnormality | Tears (total) | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| < 30 | 30–49 | 50–69 | > 69 | < 30 | 30–49 | 50–69 | > 69 | |||||||
| Blair et al. [2] | 12 | 3 | 1 | NR | 22.5 (21–27) | 32 (32–29) | 54 | NR | P | NA | Cadaver | CT + contrast | Defects in the radial and ulnar sides | 4 (16) |
| Cerofolini et al. [6] | 6 | 1 | 3 | NR | 20.5 (18–27) | 49 | 57 (50–58) | NR | P | 2 | + | Arthroscopy | Lesions of the articular disc | 10 (10) |
| Cooney [8] | 13 | 6 | 1 | NR | 24 (19–26) | 39 (34–41) | 57 | NR | P | 2 | + | Arthroscopy | Acute traumatic and degenerative tear | 9 (20) |
| Dwek et al. [9] | 13 | NR | NR | NR | 14 (13–14) | NR | NR | NR | R | 3 | + | MRI | Central communicating ligamentous injuries | 4 (13) |
| Iordache et al. [10] | 51 | 41 | 11 | NR | 25* | 35* | 56* | NR | P | 4 | – | MRI | Full/partial-thickness tear or abnormal appearance | 39 (103) |
| Kinninmonth & Chan [11] | 8 | 4 | 18 | 20 | 22 (18–25) | 46 (44–48) | 65 (60–65) | 74 (72–78) | P | NA | Cadaver | Arthrotomy | Linear and degenerative tear | 26 (50) |
| Levinsohn & Palmer [13] | 71 | 38 | NR | NR | 25* | 43* | NR | NR | P | 0 | + | Arthroraphy | TFC perforation | 28 (109) |
| Mahmood et al. [15] | 5 | 18 | 6 | 1 | 21 (20–22) | 41 (38–48) | 54 (50–56) | 70 | P | 4 | + | Arthroscopy | Tear | 21 (30) |
| Metz et al. [16] | NR | NR | 2 | 4 | NR | NR | 60 (57–62) | 76 (72–83) | P | NA | Cadaver | Arthrotomy | Tear | 4 (6) |
| Mikic [17] | 46 | 26 | 21 | 49 | 15* | 45* | 56* | 78* | P | NA | Cadaver | Arthrotomy | Disc perforation | 45 (142) |
| Ogden et al. [20] | 31 | NR | NR | NR | 2 (0.17–9) | NR | NR | NR | P | NA | Cadaver | Arthrotomy | Disc perforation | 0 (31) |
| Tanaka et al. [24] | 6 | 3 | 2 | NR | 21 (18–27) | 32 (31–36) | 52 (50–54) | NR | P | 1 | + | MRI | Discontinuity or high signal intensity in entire TFCC | 3 (11) |
| Viegas & Ballantyne [26] | 11 | 39 | 126 | 190 | 25* | 45* | 65* | 75* | P | NA | Cadaver | Arthrotomy | Identifiable disruption of TFC | 134 (366) |
| Weiss et al. [28] | 17 | 28 | 4 | 1 | 23 (23–27) | 39 (34–43) | 55 (53–57) | 70 | P | 4 | + | Arthroscopy | Tear | 30 (50) |
| Yamamoto et al. [29] | 11 | 5 | 4 | 0 | 18 (17–24) | 36 (35–38) | 60 (56–63) | NR | R | 1 | + | Arthroscopy | Disruption of TFC, loss trampoline effect | 11 (20) |
* Average age imputed from group range; NOS = Newcastle-Ottawa scale; NR = not reported, NA = not applicable, P = prospective, R = retrospective; + = positive; TFC = triangular fibrocartilage; TFCC = triangular fibrocartilage complex.
Two studies collected their data retrospectively, the remainder of the studies were prospective. We assessed methodologic quality of the included studies by the relevant criteria for assessing the quality of nonrandomized cohort studies. This scale provided a maximum of four stars for method of selection (2) and outcome assessment (2) (Table 3 in Appendix 2) [23]. The six anatomic studies could not be graded as no good grading tools exist. Average quality score was 2.3 stars, ranging from 0 to 4 (Table 1).
Table 3.
Methodologic quality of the included studies
| Cerofolini et al. [6] | Cooney [8] | Dwek et al. [9] | Iordache et al. [10] | Levinsohn and Palmer [13] | Mahmood et al. [15] | Tanaka et al. [24] | Weiss et al. [28] | Yamamoto et al. [29] | |
|---|---|---|---|---|---|---|---|---|---|
| Selection | |||||||||
| (1) Representativeness of the exposed cohort | |||||||||
| (a) Truly representative of the average symptomatic patient/general population (describe) in the community (*) | x | x | x | x | |||||
| (b) Somewhat representative of the average symptomatic patient/general population in the community (*) | x | ||||||||
| (c) Selected group of users (eg, nurses, volunteers) | x | ||||||||
| (d) No description of the derivation of the cohort | x | x | x | ||||||
| (2) Ascertainment of exposure | |||||||||
| (a) Secure record (eg, surgical records) (*) | x | x | x | ||||||
| (b) Structured interview (*) | x | ||||||||
| (c) Written self report | |||||||||
| (d) No description | x | x | x | x | x | ||||
| Outcome | |||||||||
| (1) Assessment of triangular fibrocartilage complex tear | |||||||||
| (a) Independent blind assessment (*) | x | ||||||||
| (b) Record linkage (*) | x | x | x | x | |||||
| (c) Self report | x | x | x | ||||||
| (d) No description | x | ||||||||
| (2) Adequacy of followup of cohorts | |||||||||
| (a) Complete followup - all subjects accounted for (*) | x | x | x | x | x | x | x | ||
| (b) Subjects lost to followup unlikely to introduce bias - small number lost - > 80% followup, or description provided of those lost) (*) | |||||||||
| (c) Followup rate < 80% (select an adequate %) and no description of those lost | |||||||||
| (d) No statement | x | x | |||||||
| Total stars | 2 | 2 | 3 | 4 | 0 | 4 | 1 | 4 | 1 |
Based on the Newcastle-Ottawa scale; (*) this provides 1 star.
Pooled analysis included 977 wrists with a total of 368 (38%) triangular fibrocartilage complex abnormalities.
Outcome Measures
The following data were extracted: author, year, institute, patient age, method of triangular fibrocartilage complex observation, population, and abnormality. Four studies [10, 13, 17, 26] reported groups per decade rather than individual patient age. Individual patient’s age was imputed as an average of the range of each decade, eg, age of patients in the second decade (range, 11–20 years) = 15.5 ((11+20)/2).
Patients were divided in four groups based on their maturity: (1) younger than 30 years, (2) between 30 and 49 years, (3) between 50 and 69 years, and (4) 70 years and older. Pooled overall prevalence of triangular fibrocartilage complex abnormalities per age group was calculated, in addition to odds ratios (OR) and 95% CI. Additionally, we calculated the prevalence in symptomatic and asymptomatic wrists per age group, where we regarded cadaveric wrists as asymptomatic. Differences were assessed by Pearson’s chi-square test, a p value less than 0.05 was regarded as significant. Asymptomatic patients and cadavers were drafted from the general population, while most symptomatic patients were surgically treated. We feel the difference in cohort selection introduces too much selection bias for direct comparison of symptomatic and asymptomatic patients.
Results
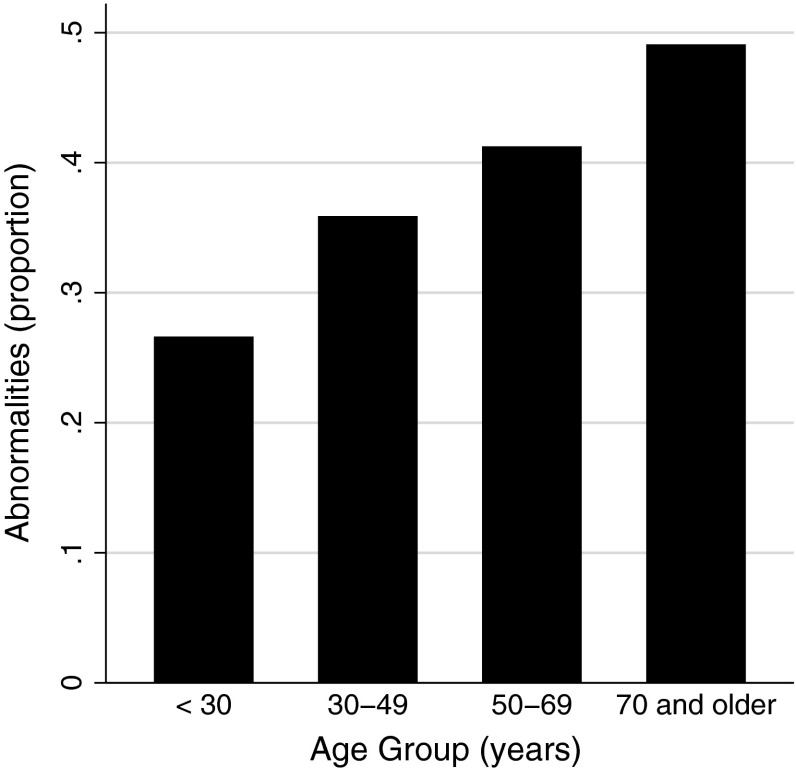
Prevalence of abnormalities ranged from 27% (80/301) in the youngest age group and increased to 49% (130/265) in patients 70 years and older (p < 0.001; Fig. 2), OR, 2.7; 95% CI, 1.9–3.8 (p < 0.001; Table 2).
Fig. 2.
The histogram shows the proportion of triangular fibrocartilage complex abnormalities in the different age groups across all studies.
Table 2.
Group characteristics
| Overall | < 30 years | 30–49 years | 50–69 years | 70 years and older |
|---|---|---|---|---|
| Median age (years) (interquartile range) | 23 (15–25) | 43 (35–45) | 63 (55–65) | 75 (75–85) |
| Number of wrists per age group | 301 | 212 | 199 | 265 |
| Percentage of tears (number) | 27% (80) | 36% (76) | 41% (82) | 49% (130) |
| p value | < 0.001 | |||
| Odds ratio (95% CI) | 1.5 (1.1–2.3) | 1.9 (1.3–2.8) | 2.7 (1.9–3.8) | |
| p value | 0.025 | 0.001 | < 0.001 | |
| Asymptomatic | ||||
| Number of wrists | 159 | 113 | 179 | 263 |
| Percentage of tears (number) | 15% (24) | 27% (31) | 38% (68) | 49% (129) |
| p value | < 0.001 | |||
| Odds ratio (95% CI) | 2.1 (1.2–3.9) | 3.4 (2.0–5.8) | 5.4 (3.3–8.9) | |
| p value | 0.014 | < 0.001 | < 0.001 | |
| Symptomatic* | ||||
| Number of wrists | 142 | 99 | 20 | 2 |
| Percentage of tears (number) | 39% (56) | 45% (45) | 70% (14) | 50% (1) |
| p value | 0.034 | |||
| Odds ratio (95% CI) | 1.3 (0.76–2.2) | 3.6 (1.3–9.9) | ||
| p value | 0.352 | 0.014 |
* Group of patients 70 years and older was excluded from comparison analysis.
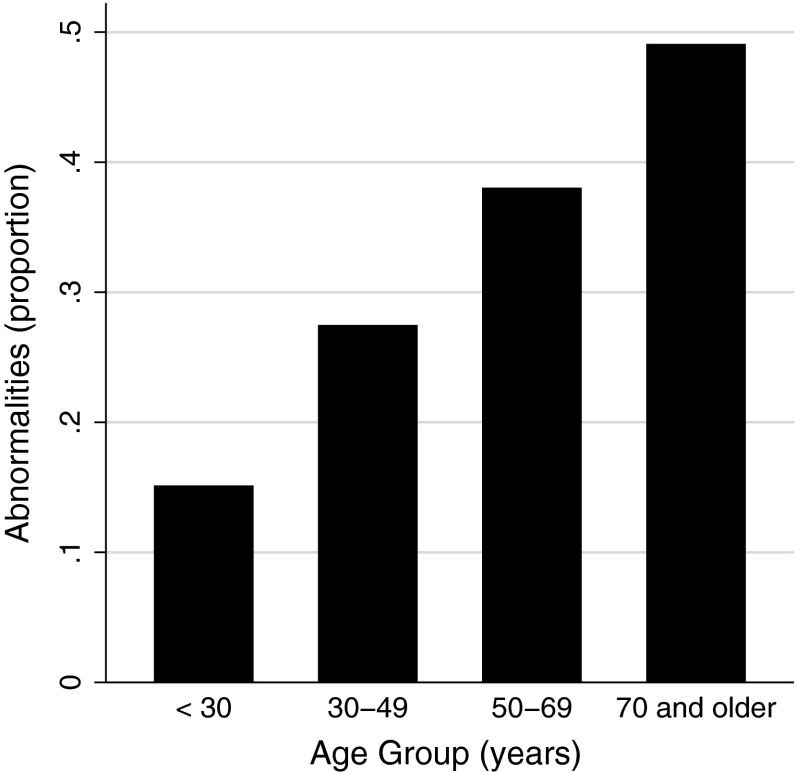
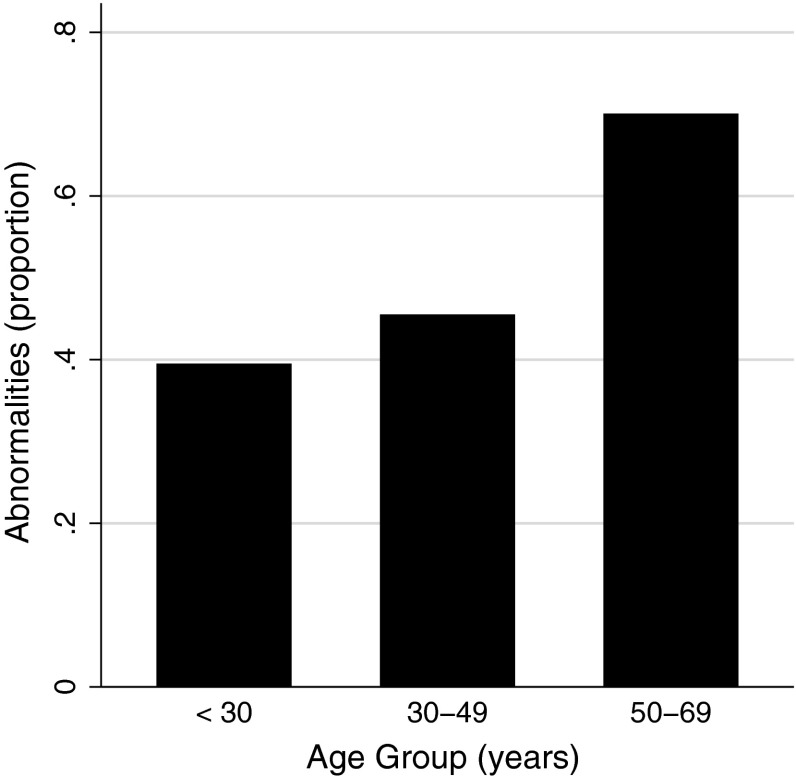
Increasing prevalence persisted regardless of symptoms; abnormalities ranged from 15% (24/159) to 49% (129/263) in asymptomatic patients (p < 0.001), OR, 5.4; 95% CI, 3.3–8.9 (p < 0.001; Fig. 3) and from 39% (56/142) to 70% (14/20) in symptomatic patients (p < 0.034), precluding two observations in the oldest symptomatic group from analysis; OR, 3.6; 95% CI, 1.3–9.9 (p < 0.014; Fig. 4).
Fig. 3.
The histogram shows the proportion of triangular fibrocartilage complex abnormalities by age group in patients with no symptoms.
Fig. 4.
The histogram shows the proportion of triangular fibrocartilage complex abnormalities by age group in patients with symptoms.
Discussion
Triangular fibrocartilage complex abnormalities seem to be more common with age, but the degree to which this is so and the degree to which the presence of an abnormality is associated with symptoms are incompletely understood. This systematic review aimed to determine the prevalence of triangular fibrocartilage complex abnormalities, and to assess if the prevalence of abnormalities is greater with increasing age in general and in patients with and without symptoms.
This study has several potential limitations. Triangular fibrocartilage complex abnormalities were diagnosed by several modalities of which direct observation by arthroscopy or arthrotomy is considered the reference standard [1, 14, 21]. The cadaver studies assume donors were asymptomatic, which may be inaccurate. Because of the inclusion of cadaver studies, not all studies could be assessed for methodologic quality. The included studies identified only two patients older than 69 years old with symptoms (an interesting finding given the findings of this review), limiting the validity and reliability of this age group in the analysis of symptomatic patients. There was wide variety of definitions and criteria for diagnosing a triangular fibrocartilage complex abnormality and this may hinder determination of a definitive rate. Future studies and clinical practice would benefit from a common interpretation.
We found an increasing prevalence of triangular fibrocartilage complex abnormalities diagnosed by various modalities. The triangular fibrocartilage complex was unaffected in only ½ of the patients older than 70 years.
Previous studies found a correlation between age and abnormalities [10, 17] in cadavers [17] and asymptomatic patients [10]. This review also shows that abnormality rate increases in symptomatic patients. These results seem to emphasize that triangular fibrocartilage complex abnormalities are common independent of symptoms, more so with age, and therefore can be difficult to isolate as the primary symptom generator and a good target for operative treatment. It has not been clearly established that interventions to address triangular fibrocartilage complex variations are better than the natural history owing to varying surgical outcomes [3] and the absence of sham surgery controlled trials. We know from studies on knee arthritis [18] and other conditions [7, 22, 27] that the placebo affect associated with surgery is very strong and that surgical interventions with entirely subjective outcomes (eg, pain) require sham surgery controls to be certain of their effectiveness. It is possible that the majority of operative interventions for the triangular fibrocartilage complex are no better than regression to the mean, the natural history of wrist symptoms, or the placebo effect.
Several lines of investigation are necessary before we can have confidence in the diagnosis and treatment of triangular fibrocartilage complex abnormalities. First, we must know the prevalence of normal variations and age-related changes to determine and quantify the likelihood that a given abnormality is traumatic. Second, we must show that we can reliably and accurately distinguish traumatic from nontraumatic anomalies. Third, we must show that a given finding is the cause of symptoms and disability. Fourth, we must show that our interventions are better than the natural history of the disease and better than placebo interventions.
This systematic review begins to address the first two of these aims by reviewing all the studies of age-related prevalence of triangular fibrocartilage complex abnormalities and confirming that abnormalities are common in symptomatic and asymptomatic wrists alike and that they are more common with age. A high prevalence of asymptomatic abnormalities makes interpretation of diagnostic tests more difficult and the likelihood that a given abnormality is new or traumatic much lower. If we had a consensus reference standard for a traumatic or symptomatic abnormality, prospective studies could determine the positive and negative predictive values of various diagnostic tests.
Our results show triangular fibrocartilage complex abnormalities are more common with age independent of symptoms and therefore can be difficult to isolate as the primary symptom generator. Patients and surgeons should understand the current limitations in the management of wrist pain that may or may not be attributable to an abnormality of the triangular fibrocartilage complex.
Electronic supplementary material
Appendix 2
See Table 3.
Footnotes
One of the authors (TT) received research grants from the Prince Bernhard Culture Fund & Kuitse Fung (USD less than 10,000) (Amsterdam, The Netherlands), Fundatie van de Vrijvrouwe van Renswoude te’s-Gravenhage (USD less than 10,000) (The Hague, The Netherlans).
One of the authors (DR) certifies that he, or a member of his immediate family, has or may receive payments or benefits, during the study period from Wright Medical (USD less than 10,000) (Memphis, TN, USA); Skeletal Dynamics (USD less than 10,000) (Miami, FL, USA); Biomet (USD less than 10,000) (Warsaw, IN, USA); AO North America (USD less than 10,000) (Paoli, PA, USA); and AO International (USD less than 10,000) (Dubendorf, Switzerland).
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research editors and board members are on file with the publication and can be viewed on request.
International Prospective Register of Systematic Reviews (PROSPERO) registration number CRD42013006546
References
- 1.Anderson ML, Skinner JA, Felmlee JP, Berger RA, Amrami KK. Diagnostic comparison of 1.5 Tesla and 3.0 Tesla preoperative MRI of the wrist in patients with ulnar-sided wrist pain. J Hand Surg Am. 2008;33:1153–1159. doi: 10.1016/j.jhsa.2008.02.028. [DOI] [PubMed] [Google Scholar]
- 2. Blair WF, Berger RA, el-Khoury GY. Arthrotomography of the wrist: an experimental and preliminary clinical study. J Hand Surg Am. 1985;10:350–359. [DOI] [PubMed]
- 3.Bottke CA, Louis DS, Braunstein EM. Diagnosis and treatment of obscure ulnar-sided wrist pain. Orthopedics. 1989;12:1075–1079. doi: 10.3928/0147-7447-19890801-07. [DOI] [PubMed] [Google Scholar]
- 4.Brown JA, Janzen DL, Adler BD, Stothers K, Favero KJ, Gropper PT, Connell DG. Arthrography of the contralateral, asymptomatic wrist in patients with unilateral wrist pain. Can Assoc Radiol J. 1994;45:292–296. [PubMed] [Google Scholar]
- 5.Cantor RM, Stern PJ, Wyrick JD, Michaels SE. The relevance of ligament tears or perforations in the diagnosis of wrist pain: an arthrographic study. J Hand Surg Am. 1994;19:945–953. doi: 10.1016/0363-5023(94)90094-9. [DOI] [PubMed] [Google Scholar]
- 6.Cerofolini E, Luchetti R, Pederzini L, Soragni O, Colombini R, D’Alimonte P, Romagnoli R. MR evaluation of triangular fibrocartilage complex tears in the wrist: comparison with arthrography and arthroscopy. J Comput Assist Tomogr. 1990;14:963–967. doi: 10.1097/00004728-199011000-00018. [DOI] [PubMed] [Google Scholar]
- 7.Cobb LA, Thomas GI, Dillard DH, Merendino KA, Bruce RA. An evaluation of internal-mammary-artery ligation by a double-blind technic. N Engl. Med. 1959;260:1115–1118. doi: 10.1056/NEJM195905282602204. [DOI] [PubMed] [Google Scholar]
- 8.Cooney WP. Evaluation of chronic wrist pain by arthrography, arthroscopy, and arthrotomy. J Hand Surg Am. 1993;18:815–822. doi: 10.1016/0363-5023(93)90047-7. [DOI] [PubMed] [Google Scholar]
- 9.Dwek JR, Cardoso F, Chung CB. MR imaging of overuse injuries in the skeletally immature gymnast: spectrum of soft-tissue and osseous lesions in the hand and wrist. Pediatr Radiol. 2009;39:1310–1316. doi: 10.1007/s00247-009-1428-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Iordache SD, Rowan R, Garvin GJ, Osman S, Grewal R, Faber KJ. Prevalence of triangular fibrocartilage complex abnormalities on MRI scans of asymptomatic wrists. J Hand Surg Am. 2012;37:98–103. doi: 10.1016/j.jhsa.2011.10.006. [DOI] [PubMed] [Google Scholar]
- 11.Kinninmonth AW, Chan KM. A study of age-related changes of the articular disc of the wrist in Hong Kong Chinese. J Hand Surg Br. 1990;15:358–361. doi: 10.1016/0266-7681(90)90020-5. [DOI] [PubMed] [Google Scholar]
- 12.Kirschenbaum D, Sieler S, Solonick D, Loeb DM, Cody RP. Arthrography of the wrist: assessment of the integrity of the ligaments in young asymptomatic adults. J Bone Joint Surg Am. 1995;77:1207–1209. doi: 10.2106/00004623-199508000-00010. [DOI] [PubMed] [Google Scholar]
- 13.Levinsohn EM, Palmer AK. Arthrography of the traumatized wrist: correlation with radiography and the carpal instability series. Radiology. 1983;146:647–651. doi: 10.1148/radiology.146.3.6828677. [DOI] [PubMed] [Google Scholar]
- 14.Magee T. 3-T MRI of the shoulder: is MR arthrography necessary? AJR Am. Roentgenol. 2009;192:86–92. doi: 10.2214/AJR.08.1097. [DOI] [PubMed] [Google Scholar]
- 15.Mahmood A, Fountain J, Vasireddy N, Waseem M. Wrist MRI arthrogram v wrist arthroscopy: what are we finding? Open Orthop J. 2012;6:194–198. doi: 10.2174/1874325001206010194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Metz VM, Schratter M, Dock WI, Grabenwoger F, Kuzbari R, Lang S, Wanivenhaus AH, Puigg S, Imhof H. Age-associated changes of the triangular fibrocartilage of the wrist: evaluation of the diagnostic performance of MR imaging. Radiology. 1992;184:217–220. doi: 10.1148/radiology.184.1.1609083. [DOI] [PubMed] [Google Scholar]
- 17.Mikic ZD. Age changes in the triangular fibrocartilage of the wrist joint. J Anat. 1978;126:367–384. [PMC free article] [PubMed] [Google Scholar]
- 18.Moseley JB, O’Malley K, Petersen NJ, Menke TJ, Brody BA, Kuykendall DH, Hollingsworth JC, Ashton CM, Wray NP. A controlled trial of arthroscopic surgery for osteoarthritis of the knee. N Engl J Med. 2002;347:81–88. doi: 10.1056/NEJMoa013259. [DOI] [PubMed] [Google Scholar]
- 19.Mrkonjic A, Geijer M, Lindau T, Tagil M. The natural course of traumatic triangular fibrocartilage complex tears in distal radial fractures: a 13–15 year follow-up of arthroscopically diagnosed but untreated injuries. J Hand Surg Am. 2012;37:1555–1560. doi: 10.1016/j.jhsa.2012.05.032. [DOI] [PubMed] [Google Scholar]
- 20.Ogden JA, Beall JK, Conlogue GJ, Light TR. Radiology of postnatal skeletal development: IV. Distal radius and ulna. Skeletal Radiol. 1981;6:255–266. doi: 10.1007/BF00347198. [DOI] [PubMed] [Google Scholar]
- 21.Shionova K, Nakamura R, Imaeda T, Makino N. Arthrography is superior to magnetic resonance imaging for diagnosing injuries of the triangular fibrocartilage. J Hand Surg Br. 1998;23:402–405. doi: 10.1016/S0266-7681(98)80068-5. [DOI] [PubMed] [Google Scholar]
- 22.Sihvonen R, Paavola M, Malmivaara A, Itala A, Joukainen A, Nurmi H, Kalske J. Jarvinen TL; Finnish Degenerative Meniscal lesion Study (FIDELITY) Group. Arthroscopic partial meniscectomy versus sham surgery for a degenerative meniscal tear. N Engl J Med. 2013;369:2515–2524. doi: 10.1056/NEJMoa1305189. [DOI] [PubMed] [Google Scholar]
- 23.Stang A. Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur J Epidemiol. 2010;25:603–605. doi: 10.1007/s10654-010-9491-z. [DOI] [PubMed] [Google Scholar]
- 24.Tanaka T, Yoshioka H, Ueno T, Shindo M, Ochiai N. Comparison between high-resolution MRI with a microscopy coil and arthroscopy in triangular fibrocartilage complex injury. J Hand Surg Am. 2006;31:1308–1314. doi: 10.1016/j.jhsa.2006.05.001. [DOI] [PubMed] [Google Scholar]
- 25.Uchiyama S, Nakatsuchi Y. Anatomical and radiological evaluation of the triangular fibrocartilage complex of the wrist. J Hand Surg Br. 1994;19:319–324. doi: 10.1016/0266-7681(94)90080-9. [DOI] [PubMed] [Google Scholar]
- 26.Viegas SF, Ballantyne G. Attritional lesions of the wrist joint. J Hand Surg Am. 1987;12:1025–1029. doi: 10.1016/S0363-5023(87)80103-X. [DOI] [PubMed] [Google Scholar]
- 27.Wartolowska K, Judge A, Hopewell S, Collins GS, Dean BJ, Rombach I, Brindley D, Savulescu J, Beard DJ, Carr AJ. Use of placebo controls in the evaluation of surgery: systematic review. BMJ. 2014;348:g3253. doi: 10.1136/bmj.g3253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Weiss AP, Akelman E, Lambiase R. Comparison of the findings of triple-injection cinearthrography of the wrist with those of arthroscopy. J Bone Joint Surg Am. 1996;78:348–356. doi: 10.2106/00004623-199603000-00005. [DOI] [PubMed] [Google Scholar]
- 29.Yamamoto M, Koh S, Tatebe M, Shinohara T, Shionoya K, Hirata H, Nakamura R. Importance of distal radioulnar joint arthroscopy for evaluating the triangular fibrocartilage complex. J. Orthop Sci. 2010;15:210–215. doi: 10.1007/s00776-009-1445-5. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.