Abstract
Background
Metal-on-metal (MoM) total hip arthroplasties (THAs) and the head-neck and neck-body junctions in modular THA are associated with a variety of local and systemic reactions to their related wear and corrosion products. Although laboratory testing is available, the relationship between laboratory values—including serum metal ion levels—and adverse local tissue reactions (ALTRs) remains controversial and incompletely characterized.
Questions/purposes
(1) What is the range of serum metal levels associated with ALTR in patients who have MoM THAs or corrosion at the head-neck and neck-body junctions in metal-on-polyethylene (or ceramic-on-polyethylene) THAs? (2) How much wear occurs in patients with MoM total hips? (3) Is there evidence of a dose-response relationship between wear and ALTR?
Methods
PubMed and Embase databases were reviewed for English-language studies assessing serum metal levels in the presence of ALTR and papers describing the results of wear measurements from revised MoM implants and ALTR histopathology were systematically reviewed. Reported linear wear data were separated into groups with ALTR and without ALTR as listed in individual papers and graphed to determine whether a dose-response relationship was present between wear and ALTR. Overall, 15 studies including 338 hips with ALTR with corresponding serum metal levels were identified and analyzed. Twelve studies reported the wear depth or volume of MoM components from patients with a variety of local reactions. Two studies investigated corrosion at the head-neck and neck-body junctions in metal-on-polyethylene THA. There was a high level of variability and study heterogeneity, and so data pooling (meta-analysis) could not be performed.
Results
Average reported metal concentrations were elevated above established normal values in patients with ALTR (cobalt concentrations ranged from 5 to 40 ppb, and chromium levels ranged from 5 to 54 ppb). Whereas several studies demonstrated that patients with ALTR had higher average linear wear of the bearing surfaces, this finding was not made in all studies that we identified in this systematic review. Because of this high degree of variability, no clear dose-response relationship between wear and ALTR could be established.
Conclusions
Serum metal level analysis and implant retrieval analysis both contribute to the understanding of ALTR. Serum metal levels generally are elevated in the presence of ALTR but should not be used in isolation for clinical decision-making. Many but not all patients with ALTR, including those with pseudotumors, demonstrate high wear, but more data and more systematic descriptions of the histopathology are needed to define the amount of wear that induces adverse reactions.
Introduction
Technological advances in tribology, material composition, implant design, and polyethylene manufacturing have together provided durable fixation, improved stability, and low wear rates in THA. However, over the last decade, the use of metal-on-metal (MoM) THA, MoM hip resurfacing as well as modular head-neck and neck-stem components with a range of bearing materials have resulted in an increase of local and circulating metal products [11, 13, 22]. Metal deposition into periprosthetic soft tissues and the resulting biological responses can present with a broad array of laboratory and imaging findings from no detectable abnormalities to a variety of complications including elevated serum metal levels with adverse local tissue reactions (ALTRs) including necrosis [16], inflammation [26, 38], and tumor-like masses (pseudotumors) [2, 25, 34].
Although ALTR can often be diagnosed by metal artifact reduction sequence (MARS)-MRI, it is clear that not all patients with high ions and high wear develop adverse reactions [6, 7, 12, 16]. The reported frequency of ALTR in MoM hips is variable and the prevalence at long-term followup or with other THA bearing couples is unknown. Whether there is a threshold level of metal tribocorrosion that leads to an ALTR or whether there is a threshold level of blood metal concentration that is diagnostic of an ALTR has not been determined and is the subject of ongoing investigation. Techniques to accurately measure the levels of metals including cobalt, chromium, and titanium in the serum have been well established in the literature with successful clinical application [21, 22, 27, 40]. The risk of ALTR with MoM THA has been reported to correlate with the serum metal levels, but the overall clinical and prognostic value of these levels remains controversial and without clear cutoff values [20]. Similarly, improvements in the methodology of implant wear measurements have led to more data on the wear depths and wear volumes from retrieved implants. Retrieval analyses have examined correlations between implant wear and patient metal levels [10, 18, 19, 26, 29, 30] but how the amount of wear and circulating metal levels correspond with the type and nature of ALTR is poorly understood.
We therefore sought to determine (1) what is the range of serum metal levels associated with ALTR in patients who have MoM THAs or corrosion at the head-neck and neck-body junctions in metal-on-polyethylene or ceramic-on-polyethylene THAs? (2) How much wear occurs in patients with MoM total hips? (3) Is there evidence of a dose-response relationship between wear and ALTR?
Search Strategy and Criteria
Metal Levels
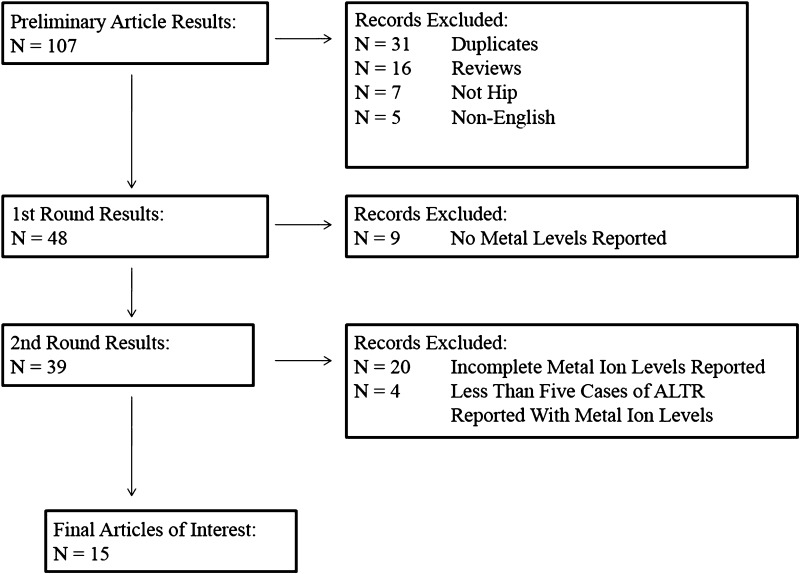
PubMed and Embase-indexed studies up to February 2014 regarding ALTR with reported serum metal levels were identified, summarized, and critically evaluated (Fig. 1). This electronic search was supplemented by a manual search in the reference lists of the included papers. Conference proceedings were not included in our search. The type of implant-bearing surface, patient characteristics, reported metal levels, and study quality characteristics were analyzed. Only studies in English language reporting ALTR and metal levels were included in the review. Search strings included various combinations of the terms arthroplasty, adverse local tissue reaction, pseudotumor/pseudotumour, hip, replacement, prosthesis, modular, resurfacing, metal-on-metal/metal on metal, and metal ions.
Fig. 1.
The flowchart summarizes the search process for inclusion and exclusion of publications, ending with the final set of selected publications reporting ALTRs with serum metal levels.
Serum metal levels in patients with reported ALTR, mostly in the form of pseudotumors, were reported in 13 studies evaluating MoM-bearing implants and two studies investigating corrosion at the head-neck and neck-body junctions in metal-on-polyethylene THA (Table 1). A total of 338 THAs demonstrating ALTR among all 15 studies were evaluated. Of these 15 studies, six were prospective studies related to ALTR with reported serum metal levels and nine were retrospective studies.
Table 1.
Summary of studies reporting serum metal levels with adverse local tissue reactions
| Reference | Hip implant type | ALTR type | Chromium levels in well-functioning implants | Chromium levels in poor-functioning implants/suspected ALTR | Cobalt levels in well-functioning implants | Cobalt levels in poor-functioning implants/suspected ALTR |
|---|---|---|---|---|---|---|
| Almousa et al., 2013 [2] | MoM THA and resurfacing | Pseudotumor | – | 40 (5 patients) | – | 54 (5 patients) |
| Bisschop et al., 2013 [4] | MoM resurfacing | Pseudotumor, ALVAL | 3 (86 patients) | 6 (39 patients) | 3 (86 patients) | 6 (39 patients) |
| Bolland et al., 2011 [5] | MoM THA | ARMD (ALVAL features) | – | 5 (14 patients) | – | 11 (11 patients) |
| Chang et al., 2013 [7] | MoM THA | Pseudotumor | – | – | < 5 ppb (80 patients) | 5 ppb (76 patients) |
| Cooper et al., 2012 [8] | Polyethylene-bearing THA | Pseudotumor | – | 1 (10 patients) | – | 10 (10 patients) |
| Cooper et al., 2013 [9] | Polyethylene-bearing THA, Ceramic-Polyethylene bearing THA | Pseudotumor | – | 0.6 (11 patients) | – | 6 (11 patients) |
| De Smet et al., 2008 [11] | MoM THA and resurfacing | Metallosis | 3* (16 patients) | 34* (10 patients) | 3* (16 patients) | 34* (10 patients) |
| Ebreo et al., 2011 [13] | MoM THA | ARMD (ALVAL features) | – | 6* (23 patients) | – | 10* (23 patients) |
| Kwon et al., 2010 [24] | MoM resurfacing | Pseudotumor | 2 (60 patients) | 15 (10 patients) | 2 (60 patients) | 13 (10 patients) |
| Kwon et al., 2011 [25] | MoM resurfacing | Pseudotumor | 2 (151 patients) | 12 (7 patients) | 2 (151 patients) | 9 (7 patients) |
| Langton et al., 2010 [26] | MoM THA and resurfacing | ARMD (ALVAL features) | 4* (488 patients) | 34* (17 patients) | 3* (488 patients) | 30* (17 patients) |
| Lohmann et al., 2013 [28] | MoM THA | Pseudotumor, ALVAL | – | 22 (27 patients) | – | 14 (27 patients) |
| Matthies et al., 2012 [30] | MoM THA and resurfacing | Pseudotumor | 3* (33 patients) | 7* (72 patients) | 3* (33 patients) | 11* (72 patients) |
| Mokka et al., 2013 [34] | MoM THA | Pseudotumor, ALVAL | – | 12 (11 patients) | – | 13 (11 patients) |
| Munro et al., 2014 [35] | MoM THA and resurfacing | Pseudotumor | 3* (16 patients) | 6* (16 patients) |
All metal ion levels in ppb unless otherwise noted; *median values listed; ALTR = adverse local tissue reaction; MoM = metal on metal; ALVAL = acute lymphocytic vasculitis-associated lesion; ARMD = adverse reactions to metal debris.
Metal-on-metal Wear
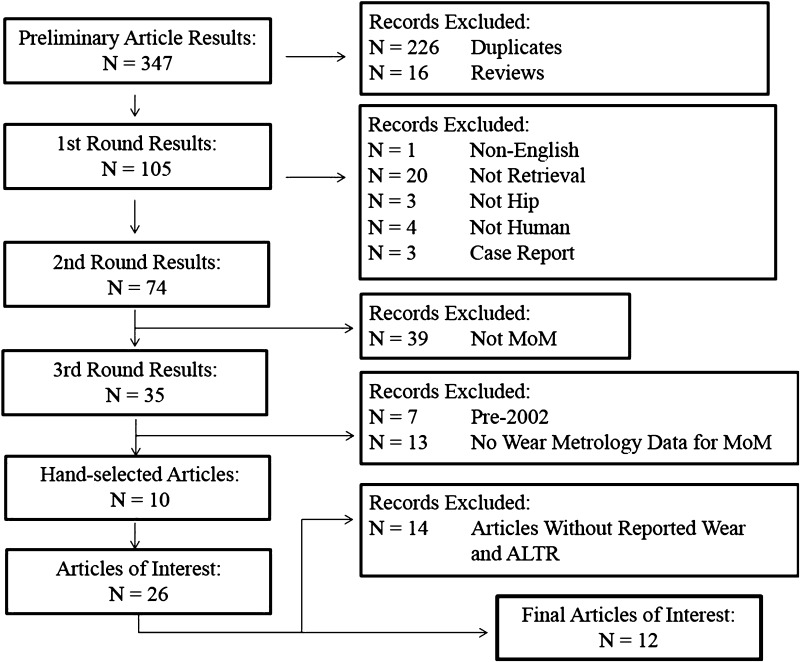
PubMed and Embase databases were used to search for papers that included the text words or keywords hip (with the Boolean search term) AND wear AND retrieval (Fig. 2). From the 347 preliminary search results, 226 duplicates and 16 reviews were excluded leaving 105 original articles. The authors chose to focus this review on MoM implants because of the current concerns of ALTR in some of these failed implants. There were 35 papers that reported retrieval analysis of MoM hips, but to answer the question regarding wear in these bearings, the papers that did not measure wear were excluded. Papers that reported tissue reactions associated with taper wear only were excluded. Bibliographies of the selected papers were checked and additional studies were added for a total of 26. No conference proceedings were included in our search.
Fig. 2.
The flowchart summarizes the search process for inclusion and exclusion of publications, ending with the final set of selected studies reporting implant wear measurements with incidence of ALTRs.
Dose-response Between Wear and ALTR
Lastly, to address the third question about wear dose-response, we excluded articles that did not specifically provide an incidence of ALTR in the MoM wear cohort being described. Twelve studies satisfied the last level review, including 10 in which detailed histological analysis was reported (Table 2). These papers were further reviewed to determine if a possible dose-response relationship between ALTR incidence and wear measurement was examined or reported. Individual papers were reviewed and those that provided linear wear data for the ALTR and non-ALTR patients were further analyzed. Papers reporting wear with pseudotumors and without pseudotumors were compared in a separate analysis. We calculated the weighted average of the linear wear rates based on the number of hips in each group as listed in the individual papers and plotted the resulting distribution. There was a high level of variability and study heterogeneity, and so data pooling (meta-analysis) could not be performed on any of the three research questions.
Table 2.
Summary of studies reporting implant wear measurements with adverse local tissue reactions
| Reference | Number of retrievals measured | Case group | Linear wear rate (um/year) | Wear volume (mm3)/rate (mm3/year) | Type of ALTR | |
|---|---|---|---|---|---|---|
| Campbell et al., 2010 [6] | 24 components | Suspected high wear | Average: 19.9, Range: 3.1–76.2 | – | Pseudotumors and metal sensitivity | |
| Pain and suspected metal sensitivity | Average: 3.7 | |||||
| Range: 1.5–6.7 | ||||||
| Ebramzadeh et al., 2011 [12] | 433 components | No pseudotumor | No suspected hypersensitivity | Median = 6* | – | Pseudotumors and metal sensitivity |
| Suspected hypersensitivity | Median: 3.4* | – | ||||
| Pseudotumor found | No suspected hypersensitivity | Median: 14.9* | – | |||
| Suspected hypersensitivity | Median: 3.42* | – | ||||
| Glyn-Jones et al., 2011 [15] | 36 components | Pseudotumor group | Mean: 8.4* | Mean: 3.3 mm3/year | Pseudotumors | |
| Control | Mean: 2.9* | Mean: 0.8 mm3/year | ||||
| Grammatopoulos et al., 2013 [16] | 56 components | Pseudotumor group | Pseudotumors | |||
| Mean: 26.4 ± 40.3 | Mean: 5.5 ± 10.4 mm3/year | |||||
| Control group | Mean: 2.9 ± 4.3 | Mean: 0.4 ± 0.5 mm3/year | ||||
| Lohmann et al., 2013 [28] | 28 components | Range: 1.9–2.1 for 4–6 years* | Range: 0.3–0.5 mm3/year* | Pseudotumors | ||
| Matthies et al., 2013 [29] | 110 components | Cup | Pseudotumor | Mean: 12.2 mm3
Median: 2.5 mm3 Range: 0.1–194.8 mm3 |
Pseudotumors | |
| No pseudotumor | Mean: 3.2 mm3
Median: 1.1 mm3 Range: 0.1–20.4 mm3 |
|||||
| Head | Pseudotumor | Mean: 14.9 mm3
Median: 4.5 mm3 Range: 0.1–228.3 mm3 |
||||
| No pseudotumor | Mean: 5.5 mm3
Median: 2.2 mm3 Range: 0.1–53.9 mm3 |
|||||
| Milosev et al., 2006 [33] | 6 components | Mean: 6.3 | Mean: 0.4 mm3/year | Lymphocytic infiltrates (metal sensitivity) | ||
| Nawabi et al., 2014 [36] | 94 components | Unexplained pain group | Median: 2.6 | Median: 0.3 mm3/year | Metal sensitivity | |
| Control | Median: 12.8 | Median: 1.5 mm3/year | ||||
| Nich and Hamadouche, 2011 [37] | 2 components | Mean: 1.9 | – | Metal sensitivity | ||
| Pelt et al., 2013 [38] | 15 components | Metallosis group | – | Mean: 16 mm3/year | Metal sensitivity | |
| Nonmetallosis group | – | Mean: 3 mm3/year | ||||
| Takamura et al., 2014 [39] | 39 components | ALTR group | Head | Median: 12.5 | ALTR (osteolysis, pseudotumor) | |
| Cup | Median: 23.0 | |||||
| Non-ALTR group | Head | Median: 1.7 | ||||
| Cup | Median: 1.48 | |||||
| Witzleb et al., 2009 [43] | 10 components | Median: 7.3 Range: 4.7–9.1 for 13 months |
Median: 2.5 mm3/year Range: 1.0–6.4 mm3/year for 13 months |
Mild histiocytic foreign body reaction | ||
All values are total linear wear rates unless otherwise noted; *femoral component wear rate; ALTR = adverse local tissue reaction.
Results
THAs with MoM bearings in the identified studies that demonstrated ALTR had a cobalt concentration of 5 to 40 ppb, which was elevated compared with metal levels in well-functioning implants (range, 2–3 ppb; Table 1). Chromium levels were also elevated in patients with ALTR and MoM bearings (5–54 ppb) compared with patients who had well-functioning implants (2–3 ppb). As a point of comparison, the Mayo Clinic metal testing web site reports reference values of serum cobalt metal levels to be < 1 ppb in the general population and < 10 ppb for well-functioning MoM bearings, whereas chromium reference metal levels are given as < 1 ppb for the general population and for well-functioning MoM implants [31]; however, many of the source studies in our systematic review did not list the reference values they used. The metal levels decreased markedly after revision surgery. In the two reports of ALTR around modular junctions in metal-on-polyethylene or ceramic-on-polyethylene THA, average serum levels of cobalt and chromium were 10 ppb cobalt and 1 ppb chromium for poor-functioning implants and 6 ppb cobalt and 0.6 ppb chromium for well-functioning implants [8, 9]. The reference range values of cobalt and chromium in patients with metal-on-polyethylene THA were cited to be 0.16 and 0.24 ppb, respectively, by those authors.
Among MoM hips revised for ALTR, a large range of linear and volumetric wear was reported in association with ALTR (Table 2). Most retrieval studies were not designed to compare the wear of THAs with and without various forms of ALTR, but two studies reported higher component wear in THAs revised with pseudotumor compared with those without pseudotumor [15, 16]. By contrast, Ebramzadeh et al. [12] demonstrated that neither the femoral head nor the acetabular cup wear rates in 43 patients with pseudotumor were statistically significantly different from 310 patients without pseudotumor. Nawabi et al. [36] reported a lower amount of wear in 35 hips revised for unexplained pain compared with 59 revised for other causes including pseudotumor and acetabular malposition (> 70° of abduction). The unexplained pain group had a higher median acute lymphocytic vasculitis-associated lesion (ALVAL) score than the other revision group, which the authors interpreted as an indication of metal sensitivity in those patients.
We were not able to infer a clear dose-response between the amount of wear and the periprosthetic histology. Ten papers used a semiquantitative rating scale such as the ALVAL score [6, 16] or the grading method of Willert et al. [42] to describe the histology of the periprosthetic tissues. These studies found inconsistent relationships between component wear and histological features. Two studies reported weak negative correlations between ALVAL scores and component wear in patients with suspected metal sensitivity [6, 36]. The patients in these studies had high ALVAL scores (> 5), indicating more inflammation and the presence of lymphocyte-dominated tissue with a low incidence of wear, suggesting the possibility of an idiosyncratic hypersensitivity reaction to metal. Grammatopoulos et al. [16] found higher ALVAL scores in patients with pseudotumors and a moderately positive correlation between wear and the histological rankings for tissue necrosis and lymphocytic response.
Discussion
MoM THAs and the head-neck and neck-body junctions in metal-on-polyethylene or ceramic-on-polyethylene THAs are associated with a variety of local and systemic reactions to their related wear and corrosion products. Although laboratory testing is available, the relationship between laboratory values—including serum metal ion levels—and ALTRs remains controversial and incompletely characterized. We therefore performed a systematic review to determine (1) what serum metal levels are associated with ALTR; (2) how much wear occurs in patients with MoM total hips; and (3) if there is evidence of a dose-response relationship between wear and ALTR.
In both arms of this review, heterogeneity of terminology, methodology, and outcome reporting were major limitations to drawing conclusions from the literature. The term ALTR encompassed a variety of complications including pseudotumor, metal sensitivity (often referred to as ALVAL), and, in a small number of patients, osteolysis or metallosis, but the histological nature of the adverse reaction being reported was often not clearly defined. Furthermore, not all of the studies identified cohorts with and without ALTR so it was often not possible to compare metal levels or retrieval findings between the two. Lastly, factors other than wear or metal sensitivity were rarely included as possible factors influencing local tissue reactions. The overall frequency of ALTR in the total hip or hip resurfacing population is unknown and it may remain difficult to determine the frequency without a consensus regarding the definition of these complications. In a recent meta-analysis of MoM bearings, the incidence of pseudotumor or metal sensitivity/ALVAL was 0.9% of 13,898 MoM hips [41].
The metal levels reported in the studies we found in MoM THAs with ALTR generally were higher than the levels found in well-functioning implants. Most of the 15 selected studies reported serum chromium and/or cobalt levels in patients with ALTR whose ion levels exceeded 7 ppb, which is the United Kingdom Medicines and Healthcare products Regulatory Agency-recommended level for additional patient followup [32]. Other authors have identified lower metal levels associated with the risk of ALTR. Bisschop et al. [4] found that the chance of having a pseudotumor was significantly higher (odds ratio, 4.9) in patients with an elevated serum cobalt level > 85 nM/L (5.5 ug/L or ppb). An increase in cobalt or chromium ions of 1 ppb increased the chance of pseudotumor by 1. Chang et al. [7] reported a threshold of 5 ppb for abnormal metal ion levels associated with pseudotumors. However, no associations between abnormal metal ion levels and patient symptoms, prosthetic femoral head size, or acetabular cup inclination for MoM THA were found. Hart et al. [19] reported that the optimal cutoff for the maximum cobalt or chromium level associated with unexplained failures of MoM hips to be 5 ppb with a sensitivity of 63% and specificity of 86% to predict failure, including, presumably, from ALTR, although this was not specifically studied. A recent informational statement published on the American Academy of Orthopaedic Surgeons’ web site [1] agreed with this suggested cutoff level of 5 ppb.
Two of the papers we identified examined metal ions and ALTR in polyethylene-on-metal or polyethylene-on-ceramic bearing hips [8, 9]. In both studies, patients presented with new-onset and increasing pain typically within 1 year of primary surgery. The prerevision metal levels were elevated compared with reference values and values in well-functioning implants, particularly for cobalt. The intraoperative findings at revision included fluid collections or pseudotumors. The retrieval findings included modular taper corrosion and histological features comparable to changes seen around some MoM total hips such as the loss of synovium and extensive lymphocytic inflammation. The authors concluded that the taper corrosion was the source of metal that led to these adverse reactions. The metal levels in these revised patients declined in the months after revision. Langton et al. [26] noted that not all patients with adverse reactions to metal debris (ARMD), which included soft tissue necrosis or pseudotumor formation, could be explained by component wear and they proposed that some patients with ARMD occurring in modular total hips were associated with the corrosion products of taper damage. They measured a range of taper wear from 0.07 to 3 mm3 per year.
Although there is a large number of implant retrieval reports of failed MoM implants, only a relatively small number examined correlations between wear and the frequency of ALTR or the histological features of the tissues. This is consistent with the observations by Ebramzadeh et al. [12] that the majority of MoM implants are revised for mechanical failures and not for ALTR. A wide range of bearing wear rates was reported in the selected retrieval studies, reflecting a variety of different implant designs, times to revision, and modes of failure. Wear rates were reported to be higher in THAs that failed with pseudotumors, malpositioned cups, and metallosis. Several studies have reported a positive correlation between wear rate and increased serum chromium and cobalt levels [11, 16, 25, 38] and increased metal debris in histology [36]; however, the presence of outliers with high wear or high ions but without a pseudotumor or with low wear or low metal levels and with a pseudotumor was noted in several papers [2, 6, 12, 15]. The inclusion of patients with cup malposition and high wear as well as patients with metal hypersensitivity in which component wear may be low could explain this observation. Many of the selected papers noted that metal hypersensitivity was a likely cause of ALTR in patients with failed MoM implants [12, 15, 33, 37]. In one study, a positive correlation of wear and metal deposition was found [36]. The contribution of metal wear from taper corrosion could also explain the lack of correlation between ALTR and wear. Retrieval studies in which modular taper junctions are being scored for corrosion damage or measured for material lost through wear or corrosion have been recently reported and such studies are likely to provide important new information [3, 14, 23, 26, 29]. The inclusion of nonwear variables such as mechanical tissue damage from impingement or implant loosening may also be informative in understanding the full spectrum of local tissue reactions to arthroplasty devices.
The high degree of variability in both component wear and periprosthetic tissue histology among the studies suggests that a clear threshold level or dose of metal cannot yet be linked to the etiology of ALTR. This is not surprising because there is clear agreement within the literature that differences in individual patient reactivity to implant wear products are likely the key in determining the risk of ALTR [30]. Whether patient reactivity can be related to the innate versus the adaptive immune response as suggested by Grammatopoulos et al. [16, 17] or to the nature of the metal products as suggested by Lohmann et al. [28] will require more detailed histological analyses of periprosthetic tissues in future studies. Rather than focusing only on wear depth or wear volume, future studies may find a more sensitive variable with which to examine correlations with clinical or histological outcomes, which may include factors other than wear.
In summary, the results of these literature reviews support that metal levels and implant retrieval are useful to the understanding of ALTR. Although there is no clear evidence of a dose-response, higher wear is associated with a higher frequency of adverse reactions and efforts to understand the implant, surgical, and patient factors leading to high wear should be continued.
Acknowledgments
We thank Dr Edward Ebramzadeh for his statistical advice related to the analysis of these papers.
Footnotes
One of the authors (JJJ) certifies that he has or may receive payments or benefits, during the study period, an amount of USD 10,000 to USD 100,000 from Medtronics Sofamor Danek (Memphis, TN, USA), an amount of USD 10,000 to USD 100,000 from Nuvasive (San Diego, CA, USA), and an amount of USD 10,000 to USD 100,000 from Zimmer (Warsaw, IN, USA). One of the authors (PAC) certifies that she has or may receive payments or benefits, during the study period, an amount of USD 10,000 to USD 100,000 from DePuy (Warsaw, IN, USA). The institution of one of the authors (PAC) has received, during the study period, funding from DePuy.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research ® editors and board members are on file with the publication and can be viewed on request.
References
- 1.AAOS. Current Concerns with Meta-on-metal Hip Arthroplasty. Information Statement. Available at: www.aaos.org/about/papers/advistmt/1035.asp. Accessed March 18, 2014.
- 2.Almousa SA, Greidanus NV, Masri BA, Duncan CP, Garbuz DS. The natural history of inflammatory pseudotumors in asymptomatic patients after metal-on-metal hip arthroplasty. Clin Orthop Relat Res. 2013;471:3814–3821. doi: 10.1007/s11999-013-2944-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bishop N, Witt F, Pourzal R, Fischer A, Rutschi M, Michel M, Morlock M. Wear patterns of taper connections in retrieved large diameter metal-on-metal bearings. J Orthop Res. 2013;31:1116–1122. doi: 10.1002/jor.22326. [DOI] [PubMed] [Google Scholar]
- 4.Bisschop R, Boomsma MF, Van Raay JJ, Tiebosch AT, Maas M, Gerritsma CL. High prevalence of pseudotumors in patients with a Birmingham Hip Resurfacing prosthesis: a prospective cohort study of one hundred and twenty-nine patients. J Bone Joint Surg Am. 2013;95:1554–1560. doi: 10.2106/JBJS.L.00716. [DOI] [PubMed] [Google Scholar]
- 5.Bolland BJ, Culliford DJ, Langton DJ, Millington JP, Arden NK, Latham JM. High failure rates with a large-diameter hybrid metal-on-metal total hip replacement: clinical, radiological and retrieval analysis. J Bone Joint Surg Br. 2011;93:608–615. doi: 10.1302/0301-620X.93B5.26309. [DOI] [PubMed] [Google Scholar]
- 6.Campbell P, Ebramzadeh E, Nelson S, Takamura K, De Smet K, Amstutz HC. Histological features of pseudotumor-like tissues from metal-on-metal hips. Clin Orthop Relat Res. 2010;468:2321–2327. doi: 10.1007/s11999-010-1372-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Chang EY, McAnally JL, Van Horne JR, Van Horne JG, Wolfson T, Gamst A, Chung CB. Relationship of plasma metal ions and clinical and imaging findings in patients with ASR XL metal-on-metal total hip replacements. J Bone Joint Surg Am. 2013;95:2015–2020. doi: 10.2106/JBJS.L.01481. [DOI] [PubMed] [Google Scholar]
- 8.Cooper HJ, Della Valle CJ, Berger RA, Tetreault M, Paprosky WG, Sporer SM, Jacobs JJ. Corrosion at the head-neck taper as a cause for adverse local tissue reactions after total hip arthroplasty. J Bone Joint Surg Am. 2012;94:1655–1661. doi: 10.2106/JBJS.K.01352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Cooper HJ, Urban RM, Wixson RL, Meneghini RM, Jacobs JJ. Adverse local tissue reaction arising from corrosion at the femoral neck-body junction in a dual-taper stem with a cobalt-chromium modular neck. J Bone Joint Surg Am. 2013;95:865–872. doi: 10.2106/JBJS.L.01042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.De Haan R, Campbell PA, Su EP, De Smet KA. Revision of metal-on-metal resurfacing arthroplasty of the hip: the influence of malpositioning of the components. J Bone Joint Surg Br. 2008;90:1158–1163. doi: 10.1302/0301-620X.90B9.19891. [DOI] [PubMed] [Google Scholar]
- 11.De Smet K, De Haan R, Calistri A, Campbell PA, Ebramzadeh E, Pattyn C, Gill HS. Metal ion measurement as a diagnostic tool to identify problems with metal-on-metal hip resurfacing. J Bone Joint Surg Am. 2008;90(Suppl 4):202–208. doi: 10.2106/JBJS.H.00672. [DOI] [PubMed] [Google Scholar]
- 12.Ebramzadeh E, Campbell PA, Takamura KM, Lu Z, Sangiorgio SN, Kalma JJ, De Smet KA, Amstutz HC. Failure modes of 433 metal-on-metal hip implants: how, why, and wear. Orthop Clin North Am. 2011;42:241–250, ix. [DOI] [PubMed]
- 13.Ebreo D, Khan A, El-Meligy M, Armstrong C, Peter V. Metal ion levels decrease after revision for metallosis arising from large-diameter metal-on-metal hip arthroplasty. Acta Orthop Belg. 2011;77:777–781. [PubMed] [Google Scholar]
- 14.Gill IP, Webb J, Sloan K, Beaver RJ. Corrosion at the neck-stem junction as a cause of metal ion release and pseudotumour formation. J Bone Joint Surg Br. 2012;94:895–900. doi: 10.1302/0301-620X.94B7.29122. [DOI] [PubMed] [Google Scholar]
- 15.Glyn-Jones S, Roques A, Taylor A, Kwon YM, McLardy-Smith P, Gill HS, Walter W, Tuke M, Murray D. The in vivo linear and volumetric wear of hip resurfacing implants revised for pseudotumor. J Bone Joint Surg Am. 2011;93:2180–2188. doi: 10.2106/JBJS.J.01206. [DOI] [PubMed] [Google Scholar]
- 16.Grammatopoulos G, Pandit H, Kamali A, Maggiani F, Glyn-Jones S, Gill HS, Murray DW, Athanasou N. The correlation of wear with histological features after failed hip resurfacing arthroplasty. J Bone Joint Surg Am. 2013;95:e81. doi: 10.2106/JBJS.L.00775. [DOI] [PubMed] [Google Scholar]
- 17.Hallab NJ, Anderson S, Caicedo M, Skipor A, Campbell P, Jacobs JJ. Immune responses correlate with serum-metal in metal-on-metal hip arthroplasty. J Arthroplasty. 2004;19:88–93. doi: 10.1016/j.arth.2004.09.012. [DOI] [PubMed] [Google Scholar]
- 18.Hart AJ, Muirhead-Allwood S, Porter M, Matthies A, Ilo K, Maggiore P, Underwood R, Cann P, Cobb J, Skinner JA. Which factors determine the wear rate of large-diameter metal-on-metal hip replacements? Multivariate analysis of two hundred and seventy-six components. J Bone Joint Surg Am. 2013;95:678–685. doi: 10.2106/JBJS.J.01447. [DOI] [PubMed] [Google Scholar]
- 19.Hart AJ, Sabah SA, Bandi AS, Maggiore P, Tarassoli P, Sampson B, Skinner JA. Sensitivity and specificity of blood cobalt and chromium metal ions for predicting failure of metal-on-metal hip replacement. J Bone Joint Surg Br. 2011;93:1308–1313. doi: 10.1302/0301-620X.93B10.26249. [DOI] [PubMed] [Google Scholar]
- 20.Hartmann A, Hannemann F, Lutzner J, Seidler A, Drexler H, Gunther KP, Schmitt J. Metal ion concentrations in body fluids after implantation of hip replacements with metal-on-metal bearing—systematic review of clinical and epidemiological studies. PLoS One. 2013;8:e70359. doi: 10.1371/journal.pone.0070359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Jacobs JJ, Gilbert JL, Urban RM. Corrosion of metal orthopaedic implants. J Bone Joint Surg Am. 1998;80:268–282. doi: 10.2106/00004623-199802000-00015. [DOI] [PubMed] [Google Scholar]
- 22.Jacobs JJ, Skipor AK, Patterson LM, Hallab NJ, Paprosky WG, Black J, Galante JO. Metal release in patients who have had a primary total hip arthroplasty. A prospective, controlled, longitudinal study. J Bone Joint Surg Am. 1998;80:1447–1458. doi: 10.2106/00004623-199810000-00006. [DOI] [PubMed] [Google Scholar]
- 23.Kop AM, Keogh C, Swarts E. Proximal component modularity in THA—at what cost? An implant retrieval study. Clin Orthop Relat Res. 2012;470:1885–1894. doi: 10.1007/s11999-011-2155-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kwon YM, Glyn-Jones S, Simpson DJ, Kamali A, McLardy-Smith P, Gill HS, Murray DW. Analysis of wear of retrieved metal-on-metal hip resurfacing implants revised due to pseudotumours. J Bone Joint Surg Br. 2010;92:356–361. doi: 10.1302/0301-620X.92B3.23281. [DOI] [PubMed] [Google Scholar]
- 25.Kwon YM, Ostlere SJ, McLardy-Smith P, Athanasou NA, Gill HS, Murray DW. ‘Asymptomatic’ pseudotumors after metal-on-metal hip resurfacing arthroplasty: prevalence and metal ion study. J Arthroplasty. 2011;26:511–518. doi: 10.1016/j.arth.2010.05.030. [DOI] [PubMed] [Google Scholar]
- 26.Langton DJ, Jameson SS, Joyce TJ, Hallab NJ, Natu S, Nargol AV. Early failure of metal-on-metal bearings in hip resurfacing and large-diameter total hip replacement: a consequence of excess wear. J Bone Joint Surg Br. 2010;92:38–46. doi: 10.1302/0301-620X.92B1.22770. [DOI] [PubMed] [Google Scholar]
- 27.Levine BR, Hsu AR, Skipor AK, Hallab NJ, Paprosky WG, Galante JO, Jacobs JJ. Ten-year outcome of serum metal ion levels after primary total hip arthroplasty: a concise follow-up of a previous report*. J Bone Joint Surg Am. 2013;95:512–518. doi: 10.2106/JBJS.L.00471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Lohmann CH, Meyer H, Nuechtern JV, Singh G, Junk-Jantsch S, Schmotzer H, Morlock MM, Pfluger G. Periprosthetic tissue metal content but not serum metal content predicts the type of tissue response in failed small-diameter metal-on-metal total hip arthroplasties. J Bone Joint Surg Am. 2013;95:1561–1568. doi: 10.2106/JBJS.L.01273. [DOI] [PubMed] [Google Scholar]
- 29.Matthies AK, Racasan R, Bills P, Blunt L, Cro S, Panagiotidou A, Blunn G, Skinner J, Hart AJ. Material loss at the taper junction of retrieved large head metal-on-metal total hip replacements. J Orthop Res. 2013;31:1677–1685. doi: 10.1002/jor.22431. [DOI] [PubMed] [Google Scholar]
- 30.Matthies AK, Skinner JA, Osmani H, Henckel J, Hart AJ. Pseudotumors are common in well-positioned low-wearing metal-on-metal hips. Clin Orthop Relat Res. 2012;470:1895–1906. doi: 10.1007/s11999-011-2201-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Mayo Clinic MCL. Metal-on-metal Wear of Orthopedic Implants: Role of Serum Cobalt and Chromium Testing. October 2011. Available at: www.mayomedicallaboratories.com/articles/features/metal-ortho/index.html. Accessed July 8, 2014.
- 32.MHRA. Medical Device Alert. Available at: www.mhra.gov.uk/home/groups/dts-bs/documents/medicaldevicealert/con155767.pdf. Accessed March 18, 2014.
- 33.Milosev I, Trebse R, Kovac S, Cor A, Pisot V. Survivorship and retrieval analysis of Sikomet metal-on-metal total hip replacements at a mean of seven years. J Bone Joint Surg Am. 2006;88:1173–1182. doi: 10.2106/JBJS.E.00604. [DOI] [PubMed] [Google Scholar]
- 34.Mokka J, Junnila M, Seppanen M, Virolainen P, Polonen T, Vahlberg T, Mattila K, Tuominen EK, Rantakokko J, Aarimaa V, Kukkonen J, Makela KT. Adverse reaction to metal debris after ReCap-M2A-Magnum large-diameter-head metal-on-metal total hip arthroplasty. Acta Orthop. 2013;84:549–554. doi: 10.3109/17453674.2013.859419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Munro JT, Masri BA, Duncan CP, Garbuz DS. High complication rate after revision of large-head metal-on-metal total hip arthroplasty. Clin Orthop Relat Res. 2014;472:523–528. doi: 10.1007/s11999-013-2979-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Nawabi DH, Nassif NA, Do HT, Stoner K, Elpers M, Su EP, Wright T, Potter HG, Padgett DE. What causes unexplained pain in patients with metal-on metal hip devices? A retrieval, histologic, and imaging analysis. Clin Orthop Relat Res. 2014;472:543–554. doi: 10.1007/s11999-013-3199-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Nich C, Hamadouche M. Cup loosening after cemented Metasul® total hip replacement: a retrieval analysis. Int Orthop. 2011;35:965–970. doi: 10.1007/s00264-010-1061-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Pelt CE, Erickson J, Clarke I, Donaldson T, Layfield L, Peters CL. Histologic, serologic, and tribologic findings in failed metal-on-metal total hip arthroplasty: AAOS exhibit selection. J Bone Joint Surg Am. 2013;95:e163. doi: 10.2106/JBJS.L.01446. [DOI] [PubMed] [Google Scholar]
- 39.Takamura KM, Amstutz HC, Lu Z, Campbell PA, Ebramzadeh E. Wear analysis of 39 conserve plus metal-on-metal hip resurfacing retrievals. J Arthroplasty. 2014;29:410–415. doi: 10.1016/j.arth.2013.05.032. [DOI] [PubMed] [Google Scholar]
- 40.Van Der Straeten C, Grammatopoulos G, Gill HS, Calistri A, Campbell P, De Smet KA. The 2012 Otto Aufranc Award: The interpretation of metal ion levels in unilateral and bilateral hip resurfacing. Clin Orthop Relat Res. 2013;471:377–385. doi: 10.1007/s11999-012-2526-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Wiley KF, Ding K, Stoner JA, Teague DC, Yousuf KM. Incidence of pseudotumor and acute lymphocytic vasculitis associated lesion (ALVAL) reactions in metal-on-metal hip articulations: a meta-analysis. J Arthroplasty. 2013;28:1238–1245. doi: 10.1016/j.arth.2013.03.027. [DOI] [PubMed] [Google Scholar]
- 42.Willert HG, Buchhorn GH, Gobel D, Koster G, Schaffner S, Schenk R, Semlitsch M. Wear behavior and histopathology of classic cemented metal on metal hip endoprostheses. Clin Orthop Relat Res. 1996;329(Suppl):S160–S186. doi: 10.1097/00003086-199608001-00016. [DOI] [PubMed] [Google Scholar]
- 43.Witzleb WC, Hanisch U, Ziegler J, Guenther KP. In vivo wear rate of the Birmingham Hip Resurfacing arthroplasty. A review of 10 retrieved components. J Arthroplasty. 2009;24:951–956. doi: 10.1016/j.arth.2008.06.022. [DOI] [PubMed] [Google Scholar]