Abstract
Background
Previous designs of internal bone lengthening devices have been fraught with imprecise distraction, resulting in nerve injuries, joint contractures, nonunions, and other complications. Recently, a magnet-operated PRECICE® nail (Ellipse Technologies, Inc, Irvine, CA, USA) was approved by the FDA; however, its clinical efficacy is unknown.
Questions/purposes
We evaluated this nail in terms of (1) accuracy and precision of distraction, (2) effects on bone alignment, (3) effects on adjacent-joint ROM, and (4) frequency of implant-related and non-implant-related complications.
Methods
We reviewed medical and radiographic records of 24 patients who underwent femoral and/or tibial lengthening procedures using the PRECICE® nail from August 2012 to July 2013 for conditions of varied etiology, the most common being congenital limb length discrepancy, posttraumatic growth arrest, and fracture malunion. This group represented 29% of patients (24 of 82) who underwent a limb lengthening procedure for a similar diagnosis during the review period. At each postoperative visit, the accuracy and precision of distraction, bone alignment, joint ROM, and any complications were recorded by the senior surgeon (SRR). Accuracy reflected how close the measured lengthening was to the prescribed distraction at each postoperative visit, while precision reflected how close the repeated measurements were to each other over the course of total lengthening period. No patients were lost to followup. Minimum followup from surgery was 3 weeks (mean, 14 weeks; range, 3–29 weeks).
Results
Mean total lengthening was 35 mm (range, 14–65 mm), with an accuracy of 96% and precision of 86%. All patients achieved target lengthening with minimal unintentional effects on bone alignment. The knee and ankle ROM were minimally affected. Of the complications requiring return to the operating room for an additional surgical procedure, there was one (4%) implant failure caused by a nonfunctional distraction mechanism and six (24%) non-implant-related complications, including premature consolidation in one patient (4%), delayed bone healing in two (8%), delayed equinus contracture in two (8%), and toe clawing in one (4%).
Conclusions
We conclude that this internal lengthening nail is a valid option to achieve accurate and precise limb lengthening to treat a variety of conditions with limb shortening or length discrepancy. Randomized, larger-sample, long-term studies are required to further confirm clinical efficacy of these devices, monitor for any late failures and complications, and compare with other internal lengthening devices with different mechanisms of operation.
Level of Evidence
Level IV, therapeutic study. See Instructions for Authors for a complete description of levels of evidence.
Introduction
Leg length discrepancy can arise from congenital or acquired etiologies, including growth plate arrest, malunion, nonunion, bone loss from open fractures, osteomyelitis, or tumor [37]. Often, the treatment involves bone lengthening at the rate of 1 mm/day according to Ilizarov’s principles of distraction osteogenesis [21]. Accurate distraction control is critical since too rapid a process can lead to nonunion, nerve damage, and joint contractures, while too slow a process runs a risk of premature consolidation. The circular and monolateral external fixators that traditionally have been utilized for bone lengthening are accurate but cumbersome devices that need to be worn for several months with daily strut/nut adjustments and can be overwhelming for the patient. Furthermore, problems such as pin track infections, hardware breakage or loosening, soft tissue transfixation, scarring, muscle contractures, and joint stiffness often arise [10, 13, 20, 31–33, 39, 41]. Hybrid techniques combining internal and external fixation, such as lengthening over nail [5, 29, 33], lengthening and then nailing [36], and lengthening and plating [19], minimize the time duration in an external fixator frame; however, these techniques are not free from external fixator-related complications.
During the last couple of decades, internal bone lengthening devices, such as the Albizzia®/Guichet® [16] (Medinov-AMP, Roanne, France), Fitbone® [11, 26] (Wittenstein, Igersheim, Germany), and Intramedullary Skeletal Kinetic Distractor (ISKD) [9, 23] (Orthofix, Inc, Lewisville, TX, USA), have been developed to obviate the need for external fixators. These are telescopic nails that are inserted into the intramedullary canal of long bones after osteotomy. With the distal and proximal nail pieces fixed to the respective bone segments, distraction of the nail results in lengthening of the bone. Diverse mechanisms of operation have been employed, including an electronically controlled linear actuator, spring-ratchet, and roller-clutch-threaded-rod mechanisms driven by specific limb rotations. However, previous designs of internal lengthening devices have lacked a reliable mechanism for distraction monitoring and control [1, 4, 9, 17]. Several authors have reported inconsistent distraction of these devices, leading to nonunions, nerve injuries, nail fractures, joint contractures, and other serious complications [6, 16, 22, 23, 29, 35, 38–40, 42].
Recently, a novel magnet-operated telescopic internal lengthening device called the PRECICE® nail (Ellipse Technologies, Inc, Irvine, CA, USA) (Fig. 1) [12] was approved for clinical use by the FDA. The internal architecture of this nail includes a generic rare earth magnet connected to a gear box and screw shaft assembly (Fig. 2). Elongation of the nail occurs on interaction of the internal magnet with the two revolving magnets within the external controller unit, which can be custom programmed to adjust the distraction rate. Nevertheless, a magnet-driven internal lengthening device is a novel technology, and literature regarding its safety, efficacy, reliability, patient satisfaction, and complication rates is sparse [8, 12, 24].
Fig. 1.

The PRECICE® nail of the selected size and diameter is assembled by connecting the two telescopic nail pieces as per manufacturer guidelines.
Fig. 2.
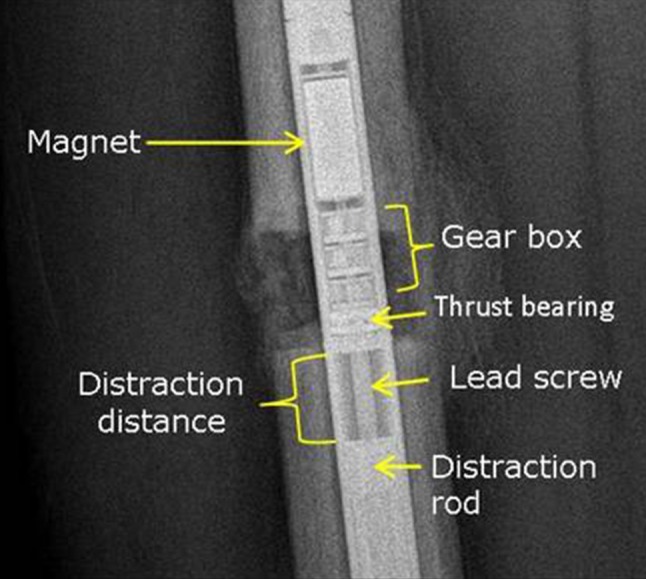
The internal architecture of the PRECICE® nail consists of a permanent rare earth magnet that is connected to a gear box and screw shaft assembly.
We therefore evaluated our initial experience using the PRECICE® nail for femoral and/or tibial lengthening in terms of (1) accuracy and precision of distraction, (2) effects on bone alignment, (3) effects on adjacent-joint ROM, and (4) frequency of implant-related and non-implant-related complications.
Patients and Methods
Study Patients
We retrospectively reviewed the initial 24 patients who underwent lengthening of the femur (17 patients, 17 femurs) or tibia (seven patients, eight tibias) using the PRECICE® nail at the Limb Lengthening and Complex Reconstruction Service of the Hospital for Special Surgery (New York, NY, USA) from August 2012 to July 2013. Details regarding patient age and sex, etiology, bone deficiency, surgery, distraction process, and complications were tabulated. The group of patients comprised 19 males and five females, with a mean age of 31 years (range, 13–67 years) (Table 1). The group of patients in whom we used this nail represented 29% of patients (24 of 82) who underwent a limb lengthening procedure for a similar diagnosis during the review period. Congenital/developmental conditions, posttraumatic growth arrest, and fracture malunion were the most common etiologies (Table 2). General indications for using this nail for the above diagnoses included relatively linear alignment with minimal to moderate angular deformity, target lengthening of no more than 65 mm (maximum lengthening possible with the current version of the nail), and patient’s willingness and capability to use the external magnet controller. Additional requirements included those for standard intramedullary nailing such as closed physes and adequate width of the intramedullary canal. Contraindications included the need for simultaneous lengthening and complex deformity correction, multiple-level deformity, and concern for infection; these patients were treated using an external fixator such as the Taylor Spatial Frame (Smith & Nephew, Inc, Memphis, TN, USA). Furthermore, patients were cautioned about potential magnet interactions and risk of bodily harm if they underwent an MRI study with the nail inside the body. They were also informed about the need for implant removal surgery a few months after consolidation of the newly regenerated bone. The minimum followup was 3 weeks (mean, 14 weeks; range, 3–29 weeks) from surgery. None of the patients were lost to followup.
Table 1.
Patient demographic data
| Variable | Value |
|---|---|
| Number of patients | 24 |
| Number of bones lengthened | 25 |
| Lengthening (number of patients/bones) | |
| Femoral | 17/17 |
| Tibial | 7/8 |
| Sex (number of patients) | |
| Female | 5 |
| Male | 19 |
| Age (years)* | 31 (13–67) |
* Values are expressed as mean, with range in parentheses.
Table 2.
Distribution of etiology of bone deficiency among the study patients
| Etiology | Number of patients |
|---|---|
| Congenital/developmental | 11 |
| Posttraumatic growth arrest | 5 |
| Fracture malunion | 4 |
| Short stature | 2 |
| Postarthrodesis | 1 |
| Posttumor resection | 1 |
Treatment and Surgery
Clinical and radiographic assessments of limb length discrepancy and any associated varus/valgus, procurvatum/recurvatum, or rotational deformities were performed. A single-level osteotomy was planned at the apex of any associated deformity to enable acute correction during surgery [16, 26]; none of the patients underwent multiple-level osteotomies. Optimal nail dimensions were determined based on preoperative measurements of bone length and canal diameter using a calibrated digital radiography system (picture archiving and communications system [PACS]; OnePacs LLC, New York, NY, USA). As per manufacturer recommendations, nail length was selected such that at least 2 to 3 cm of the thicker nail piece would be contained within the distracting bone segment at the end of lengthening [12]. The operation was performed under fluoroscopic guidance similar to standard intramedullary nailing with certain unique features as outlined below. As a reference for rotational alignment, two 3-mm K-wires were inserted parallel to each other and proximal and distal to the intended osteotomy, while ensuring that these wires would not obstruct nail passage. Next, a series of drill holes was made at the osteotomy site through a 1-cm incision. These holes served to mark the osteotomy location and also to vent the canal during reaming to protect against fat embolism. The entry portal for the nail was located using a thick K-wire either at the greater trochanter or the piriformis fossa for an anterograde femoral nail, the intercondylar notch for a retrograde femoral nail, and just anterior to the proximal tibial articular surface for a tibial nail. A retrograde nail was used in two of 17 femoral lengthenings because the apex of the associated deformity was located in the distal femur. A cannulated drill was used over the K-wire to enter the intramedullary canal. The K-wire was exchanged for a ball-tipped guide wire that was passed down the canal, and reaming was done over it up to about 1.5 mm to 2 mm greater than the selected nail diameter. After reaming, the guide wire was removed to allow passage of the nail, which is a noncannulated solid implant. A nail of appropriate length and size was assembled by locking the two telescopic pieces together as per manufacturer guidelines and was introduced into the canal using a jig. The nail was advanced until the distal tip was at the intended osteotomy site (vent holes). Osteotomy was then completed with an osteotome [34], and the nail was driven across. Completion of osteotomy was confirmed by free limb rotations over the nail. Any preexisting varus/valgus, procurvatum/recurvatum, or rotational deformity was corrected, and interlocking screws were inserted using the jig and free-hand techniques. Malalignment was prevented by ensuring appropriate fit of the nail into the canal and adequate nail length beyond the osteotomy. In case of a loose fit, blocking (Poller) screws were inserted into the concavity of the potential deformity [25], especially for larger amounts of lengthening and for osteotomies in the metaphyseal region. Specifically, Poller screws were used to secure the two retrograde femur nails and seven of eight tibia nails. No Poller screws were inserted for the proximal femoral lengthening using an anterograde nail. Knee and ankle ROM were evaluated for the potential for developing contractures during lengthening. In case of restricted ROM, prophylactic iliotibial band release was performed to prevent knee contracture during femoral lengthening, and gastrocnemius-soleus recession was done to prevent ankle equinus contracture during tibial lengthening. Care was taken to release only the tight fibrous strands, while preserving muscle tissue and paratenon. Lastly, the internal nail magnet was located and marked on the skin under fluoroscopic guidance (Fig. 3).
Fig. 3A–B.
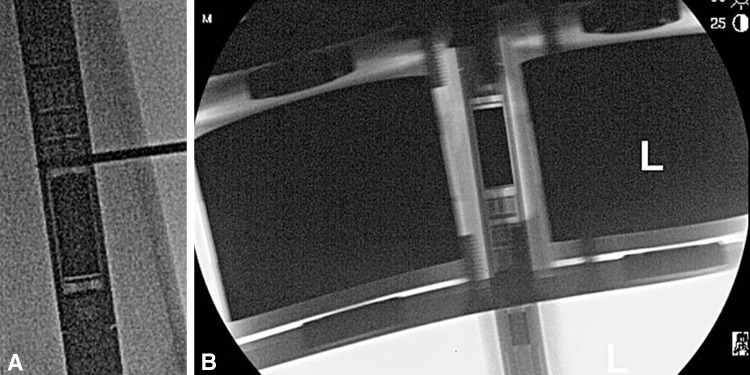
(A) The internal magnet within the nail is localized intraoperatively using a wire under fluoroscopic guidance. (B) The external controller unit is placed directly over the internal nail magnet under fluoroscopy and the location is marked on the skin using a marker pen.
Aftercare
The distraction process was initiated soon after the surgery, typically on the fifth postoperative day for the femur and seventh postoperative day for the tibia (Fig. 4). The conventional distraction rate of 1 mm/day was adopted for most lengthenings. The schedule was comprised of the prescribed daily distraction split either into 0.33 mm three times a day or 0.25 mm four times a day as per patient’s convenience until the desired length was attained. The distraction rate was reduced to 0.75 mm/day for three patients for a short period of time because of inadequate callus formation on serial radiographs indicating possible delayed union. Patients were provided an external magnet controller for home use along with detailed instructions. The protocol for using the controller was straightforward and easy to explain to the patients.
Fig. 4.

Distraction of the nail is initiated during the early postoperative period, typically Day 5 for the femur and Day 7 for the tibia. The external remote controller unit is applied on the skin marking corresponding to the location of the internal nail magnet. Distraction is performed at the rate of 1 mm/day split into 0.33 mm three times a day or 0.25 mm four times a day.
Followup Routine and Outcome Measures
Our followup protocol involved clinical and radiographic examinations at 2-weekly intervals during the active lengthening phase and 1-monthly intervals during the consolidation phase until complete bony healing was achieved. Radiographic measurements were done using the PACS as mentioned earlier. Outcome measures included accuracy and precision of distraction, absolute changes in bone alignment, adjacent-joint ROM, and frequency of complications. At each followup visit, a single observer (the senior surgeon, SRR) performed clinical measurements of adjacent-joint ROM and radiographic measurements of bone alignment and distraction gap (Fig. 5). The lengthening measured on calibrated radiographs at each followup visit was tabulated against the prescribed distraction during the respective time period. Thus data at multiple time points (typically three to five) were available for each patient. Preoperative alignment and any intentional deformity correction were taken into account. Bone healing was graded as complete or incomplete and also based on the number of healed cortices on AP and lateral images. However, no comparisons were done in terms of quality or speed of callus formation because that was not the premise of this study. Changes in bone alignment in the sagittal plane (procurvatum/recurvatum angles) and the coronal plane (lateral distal femoral angle and medial proximal tibial angle) were measured. Patients’ complaints, complications, and any additional procedures performed were noted. Complications that resulted in an unplanned return to the operating room for an additional surgical procedure were segregated into implant-related and non-implant-related complications.
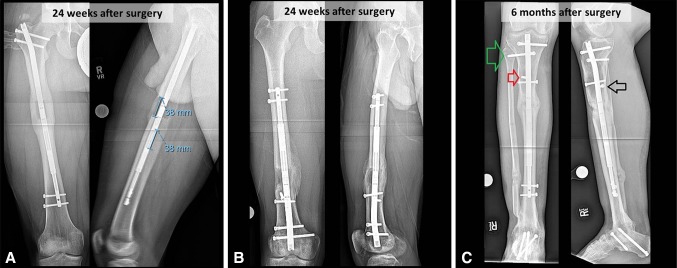
Fig. 5A–C.
AP (left) and lateral (right) radiographs show distraction measurements and consolidating bone regenerate in selected representative case examples. (A) A 14-year-old boy underwent anterograde femoral lengthening for a 3.8-cm congenital leg length discrepancy and 20° external rotation deformity. (B) A 30-year-old man underwent retrograde femoral lengthening for a 3.6-cm leg length discrepancy, 7° genu valgum, and 10° external rotation deformity due to posttraumatic growth arrest. (C) A 41-year-old man underwent tibial lengthening for 4.0-cm shortening from bone loss and tibiotalocalcaneal arthrodesis. Radiographs also show additional screw stabilization across the proximal tibia-fibula joint (green arrow), a lateral blocking screw to prevent valgus malalignment (red arrow), and a posterior blocking screw to prevent procurvatum deformity (black arrow).
Statistical Analysis
Variables were analyzed using descriptive statistics only. A power analysis was not performed because this was an observational case series report that did not involve any groupwise comparisons. Accuracy of distraction (reliability of measurements) was calculated by comparing the amount of distraction performed to the amount of lengthening measured at each postoperative visit using the following standard equations:
Precision (repeatability of measurements) was calculated from the relative standard deviation (SD) of accuracy using the following equations:
The data reflected multiple measurements of prescribed distraction versus measured lengthening at several postoperative followup visits during the lengthening phase. Smaller values of absolute percent error and relative SD indicated greater accuracy and precision, respectively.
Results
Accuracy and Precision of Distraction
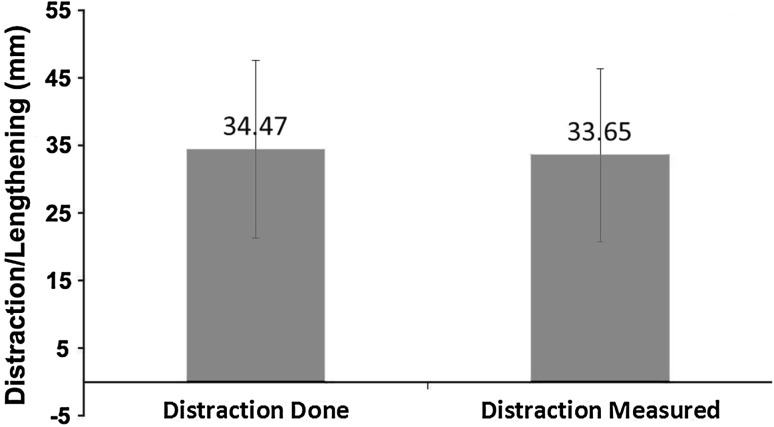
All patients completed target lengthening. The mean total lengthening for all patients combined was 35 mm (range, 14–65 mm) (Fig. 6). The accuracy of distraction was 96% ± 15% and the precision was 86% (Table 3).
Fig. 6.
The accuracy and precision of distraction of the PRECICE® nail were calculated by comparing performed distraction to achieved lengthening. The plot shows the mean and SD of multiple postoperative measurements of distraction versus lengthening for all femoral and tibial lengthenings combined (n = 25).
Table 3.
Followup, lengthening, accuracy, and precision for all patients
| Bone | Followup (weeks)* | Lengthening (mm)* | Accuracy (%) | Precision (%) |
|---|---|---|---|---|
| Femur + tibia | 14 (3–29) | 35 (14–65) | 96 | 86 |
| Femur | 12 (3–24) | 31 (14–48) | 98 | 89 |
| Tibia | 17 (3–30) | 43 (15–65) | 91 | 82 |
* Values are expressed as mean, with range in parentheses.
Effects on Bone Alignment
Acute intentional correction of external rotation deformities ranged from 5° to 20° in three patients with femoral lengthening for one patient with tibial lengthening and posttraumatic limb length discrepancy. Likewise, correction of varus deformities ranged from 6° to 20° in two patients with femur fracture malunion with bone deficiency. Furthermore, excessive anterior femoral bow (procurvatum) was corrected from 11° (range, 5°–24°) to 3° (range, 0°–13°) to facilitate nail insertion in five patients. In patients who did not undergo correction of a varus or valgus deformity, there was an unintentional +2° change in lateral distal femoral angle and a +3° change in medial proximal tibial angle, while the unintentional lateral shift in the mechanical axis deviation was 1 mm and 5 mm during femoral and tibial lengthening, respectively (Table 4). Among patients without any procurvatum/recurvatum deformity correction, the unintentional change in the sagittal plane angle was +3º for the femur and 0º for the tibia. A tendency for varus-procurvatum malalignment after proximal femur osteotomies and valgus-procurvatum malalignment after tibia osteotomies was observed. We attempted to minimize malalignment by selecting appropriate osteotomy level, by ensuring adequate length of the thicker nail piece beyond the osteotomy, and by using blocking screws [25] whenever indicated.
Table 4.
Unintentional changes in femoral and tibial alignment during lengthening
| Angle | Absolute change | |
|---|---|---|
| Femur | Tibia | |
| Mechanical axis deviation (mm) | 1 [lateral] (2 [medial] to 8 [lateral]) | 5 [lateral] (0 [medial] to 8 [lateral]) |
| Procurvatum/recurvatum (°) | +3 (0–12) | 0 (−5 to 4) |
| Lateral distal femoral angle (°) | +2 (0–5) | +3º (0–6) |
Values are expressed as mean, with range in parentheses.
Effects on Adjacent-joint ROM
Moderate temporary loss of knee and ankle ROM was observed during the early postoperative period. A temporary loss of 1° (range, 0°–5°) of knee extension and 8° (range, 5°–30°) of knee flexion was observed during femoral lengthening, and a loss of 2° (range, 0°–15°) of ankle dorsiflexion and 8° (range, 0°–20°) of plantarflexion was observed during tibial lengthening. Two patients with tibial lengthening developed equinus contracture during the late distraction phase, which was successfully treated with gastrocnemius-soleus recession. One of them also developed simultaneous claw toe deformities necessitating flexor tenotomies. The patients treated with a retrograde femur nail had a greater temporary loss of knee flexion in the immediate postoperative period. However, with continued physical therapy, all patients demonstrated continued improvement to achieve their preoperative knee and ankle ROM and a normal gait pattern within a few months after surgery.
Frequency of Implant-related and Non-implant-related Complications
We encountered one implant-related (4%) and six non-implant-related (24%) complications that resulted in an additional unplanned visit to the operating room for those patients. The implant-related complication (4%) was a nonfunctional distraction mechanism in a femoral lengthening, which was treated with nail exchange. There was premature consolidation of the osteotomy in another patient (4%) undergoing femoral lengthening because he was unable to follow a meticulous distraction schedule; this was treated with repeat osteotomy and nail exchange. Bone healing was satisfactory in all 17 patients with femoral lengthening; however, two of seven patients with tibial lengthening (8%) exhibited signs of delayed bone healing and were treated with insertion of demineralized bone matrix allograft and autologous bone marrow concentrate. As mentioned earlier, two other patients with tibial lengthening (8%) developed delayed equinus contracture, which was treated by gastrocnemius-soleus recession, and one patient (4%) developed toe clawing, which was treated by toe flexor tenotomies. All complications were successfully treated, and there were no other major complications.
Discussion
Internal bone lengthening devices were developed to eliminate the need for external fixators and the associated problems during bone lengthening. Successful bone lengthening has been reported with the use of internal lengthening devices in the past [2, 16, 18, 27, 30]; however, these devices have their own unique complications, including infection, substantial pain during distraction, nail fracture, asymmetrical bone healing, premature ossification, pseudoarthrosis, failure of distraction mechanism, and uncontrolled distraction (the so-called runaway nail phenomenon). These complications often require manipulations under anesthesia or additional operative procedures [14, 28, 35, 42]. Previous designs of internal lengthening devices operate on diverse mechanisms, including a linear actuator driven by an external electronic controller (Fitbone®) [2], a spring-and-ratchet system driven by voluntary limb rotations (Blisnikov [4] and Albizzia®/Guichet® nails [15]), and a roller-clutch-threaded-rod assembly also driven by limb rotations (ISKD) [9]. Regardless of the mechanism, the root cause for complications seems to be imprecise control of distraction. Recently, a magnet-operated telescopic PRECICE® internal lengthening device [12] was approved for clinical use by the FDA. Distraction of this nail is claimed by the manufacturer to be accurately controlled via a custom-programmable external remote controller [12]. However, a magnet-driven internal lengthening device is a novel technology, and literature regarding its clinical efficacy is limited [8, 12, 24]. We present our initial results with the PRECICE® nail in terms of accuracy and precision of distraction, effects on bone alignment and adjacent-joint ROM, and frequency of implant failure and other complications in our initial series of patients undergoing femoral and/or tibial lengthening.
This study has several limitations. This is an initial case series report involving a small number of subjects. We acknowledge that patients were not randomized and that only descriptive statistical analyses were performed. No patients were lost to followup; however, limited sample size in this study precluded any comparisons with other limb lengthening devices. Comparative studies involving this nail and other devices should be conducted in the future using groupwise comparisons and other in-depth statistical analyses. We chose the PRECICE® nail for patients who were to undergo more or less linear lengthening with only mild to moderate deformity correction, while external fixators such as the Taylor Spatial Frame were used for bone lengthening along with more complex deformity correction. A concern for infection, multiple-level deformity, open physes, target lengthening of more than 65 mm, and too narrow intramedullary canal were contraindications for the use of this nail. Patient selection was done based on detailed clinical and radiographic evaluations done by the chief surgeon (SRR), who also performed the measurements; we recognize these aspects of the study as noteworthy limitations. This was a short-term study, and it is possible that longer-term studies may reveal other hardware failure complications, such as nail loosening, breakage, or magnet-related biologic consequences. We observed an accuracy of 96% and a precision of 86% for distraction for both femoral and tibial lengthenings combined. We did not find any published accuracy or precision data regarding any of the other internal lengthening devices for comparison. This may be a topic worthy of investigation in the future.
In our study, acute correction of mild to moderate bowing, rotational or angular deformities was possible during surgery, which is consistent with the literature on other internal lengthening devices [16, 26]. Unintentional changes in alignment were analyzed separately from the intentional corrections of angular deformities and reductions of femoral bow that was done to facilitate insertion of a straight intramedullary nail. We did not observe any significant unintentional malalignment, contrary to prior reports regarding iatrogenic malalignment with bone lengthening. In particular, we did not observe iatrogenic genu valgus deformity as a result of lengthening of the femur along its anatomic axis using an intramedullary device [7, 32], which may have been because of limited magnitude of lengthening in our patients. However, we did observe a tendency for varus-procurvatum malalignment at proximal femur osteotomies and valgus-procurvatum malalignment at proximal tibia osteotomies, which is consistent with past studies [7, 32]. A greater tendency for malalignment was observed during tibial lengthening as compared to femoral lengthening, possibly due to anatomic differences. We believe that we were able to minimize malalignment by selecting appropriate nail size and osteotomy level and by inserting blocking screws [25] in case of a loose fit of the nail. These precautionary measures are probably more important for large amounts of lengthening and for metaphyseal osteotomies. Overall, we observed minimal unintentional changes in sagittal and coronal plane alignment.
We observed moderate temporary loss of knee and ankle ROM during the early postoperative phase. All patients regained their preoperative joint ROM and displayed a normal gait pattern within a few months after surgery. These results are similar to earlier reports on postoperative function after lengthening using an internal lengthening device such as the Albizzia®/Guichet® [16], Fitbone® [11, 26], and ISKD [9, 23]. As discussed earlier, the premise of internal lengthening devices was to obviate the need for external fixators and to minimize the associated complications [10, 13, 20, 31–33, 39, 41]. However, several past designs of internal lengthening devices have had substantial incidence of complications as well. In contrast, we believe that we encountered fewer complications in our initial series of 25 bone lengthening procedures using this nail. There was one (4%) implant-related complication (nonfunctional magnet mechanism) in a femoral lengthening and six (24%) non-implant-related complications that resulted in an additional unplanned visit to the operating room. The non-implant related complications included one premature consolidation of the osteotomy (4%) in a patient undergoing femoral lengthening because he was unable to follow a meticulous distraction schedule, delayed bone healing in two tibial lengthenings (8%), delayed equinus contracture in two tibial lengthenings (8%), and toe clawing in one tibial lengthening (4%). All complications were treated successfully with an additional appropriate surgical procedure for the respective complication. The feedback from patients in terms of ease of using the device was generally very positive. Although we did not specifically attempt to quantify pain or discomfort, none of the patients in this study reported perception of clicking, pain, or discomfort during distraction. Furthermore, there was no need for anesthesia to perform nail adjustments during lengthening, which is in contrast to some reports regarding previous designs of internal lengthening devices [9, 14, 16].
Major complications associated with external fixators have ranged from 46% to 72% [32, 33, 41], those related to mechanically driven internal lengthening devices have ranged from 11% to 47% [9, 14, 16], and those related to electromechanical nails have ranged from 12.5% to 13% [3, 26] (Table 5). Complications directly attributable to the previous designs of internal lengthening devices have included substantial pain during distraction, nail fracture, asymmetrical bone healing, premature ossification, pseudoarthrosis, failure of distraction mechanism, and uncontrolled distraction, often requiring manipulations or operative procedures under anesthesia [14, 28, 35, 42]. Although our numbers were insufficient for formal analysis, our sense is that tibial lengthening was generally associated with more difficulties than femoral lengthening, which is in concurrence with prior studies [26, 32, 38].
Table 5.
Comparative data regarding implant-related complications of different designs of internal lengthening devices
| Device | Study | Number of limbs | Implant-related complications (%) |
|---|---|---|---|
| ISKD | Cole et al. [9] (2001) | 20 | 11 |
| Schiedel et al. [38] (2011) | 69 | 47 | |
| Mahboubian et al. [29] (2012) | 12 | 50 | |
| Kenaway et al. [23] (2011) | 57 | 33 | |
| Simpson et al. [40] (2009) | 33 | 30 | |
| Albizzia®/Guichet® | Guichet et al. [16] (2003) | 41 | 29 |
| Garcia-Cimbrelo et al. [14] (2002) | 24 | 20.8 | |
| Fitbone® | Baumgart et al. [3] (2006) | 150 | 13 |
| Krieg et al. [27] (2008) | 32 | 12.5 | |
| Dincyurek et al. [11] (2012) | 15 | 13.3 | |
| PRECICE® | Current study | 25 | 4 |
In summary, based on our initial series of 25 femoral and/or tibial lengthening procedures, the new PRECICE® internal lengthening nail appears to be a valid treatment option for straightforward bone lengthening procedures with mild to moderate deformity correction. The accuracy and precision of nail distraction were 96% and 86%, respectively, frequency of implant failure was 4%, and effects on bone alignment and adjacent-joint ROM were minimal. An additional surgical procedure was performed to treat 4% of implant-related complications (nonfunctional distraction mechanism) and 24% of non-implant-related complications, including one premature consolidation due to patient noncompliance (4%), two cases of delayed equinus contracture (8%), and one case of toe clawing (4%). Patients must be cautioned against undergoing an MRI study while carrying this nail within their body because of the possibility of magnet interaction and risk of bodily injury. Furthermore, removal of the nail should be recommended soon after complete bony union to prevent any unknown magnet-related biologic complications and to allow for future MRI studies if needed. Randomized, larger-sample studies are warranted to compare clinical efficacy of the PRECICE® nail to different internal lengthening devices available in the market.
Acknowledgments
We thank the Ellipse Technologies sales representatives and engineers for technical guidance.
Footnotes
Each author certifies that he or she, or a member of his or her immediate family, has no funding or commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research ® editors and board members are on file with the publication and can be viewed on request.
Clinical Orthopaedics and Related Research ® neither advocates nor endorses the use of any treatment, drug, or device. Readers are encouraged to always seek additional information, including FDA approval status, of any drug or device before clinical use.
Each author certifies that his or her institution approved the human protocol for this investigation, that all investigations were conducted in conformity with ethical principles of research, and that informed consent for participation in the study was obtained.
References
- 1.Baumann F, Harms J. The extension nail: a new method for lengthening of the femur and tibia (author’s transl) [in German] Arch Orthop Unfallchir. 1977;90:139–146. doi: 10.1007/BF00414987. [DOI] [PubMed] [Google Scholar]
- 2.Baumgart R, Betz A, Schweiberer L. A fully implantable motorized intramedullary nail for limb lengthening and bone transport. Clin Orthop Relat Res. 1997;343:135–143. doi: 10.1097/00003086-199710000-00023. [DOI] [PubMed] [Google Scholar]
- 3.Baumgart R, Thaller P, Hinterwimmer S, Krammer M, Hierl T, Mutschler W. A fully implantable, programmable distraction nail (Fitbone)—new perspectives for corrective and reconstructive limb surgery. In: Kempf I, Leung KS, Alt V, Haarman H, Taglang G, Schnettler R, Seidel H, editors. Practice of Intramedullary Locked Nail: New Developments in Techniques and Applications. New York, NY: Springer; 2006. pp. 189–198. [Google Scholar]
- 4.Bliskunov AI. Implantable devices for lengthening the femur without external drive mechanisms [in Russian] Med Tekh. 1984;2:44–49. [PubMed] [Google Scholar]
- 5.Bost FC, Larsen LJ. Experiences with lengthening of the femur over n intramedullary rod. J Bone Joint Surg Am. 1956;38:567–584. [PubMed] [Google Scholar]
- 6.Burghardt RD, Herzenberg JE, Specht SC, Paley D. Mechanical failure of the Intramedullary Skeletal Kinetic Distractor in limb lengthening. J Bone Joint Surg Br. 2011;93:639–643. doi: 10.1302/0301-620X.93B5.25986. [DOI] [PubMed] [Google Scholar]
- 7.Burghardt RD, Paley D, Specht SC, Herzenberg JE. The effect on mechanical axis deviation of femoral lengthening with an intramedullary telescopic nail. J Bone Joint Surg Br. 2012;94:1241–1245. doi: 10.1302/0301-620X.94B9.28672. [DOI] [PubMed] [Google Scholar]
- 8.Cheung KM, Cheung JP, Samartzis D, Mak KC, Wong YW, Cheung WY, Akbarnia BA, Luk KD. Magnetically controlled growing rods for severe spinal curvature in young children: a prospective case series. Lancet. 2012;379:1967–1974. doi: 10.1016/S0140-6736(12)60112-3. [DOI] [PubMed] [Google Scholar]
- 9.Cole JD, Justin D, Kasparis T, DeVlught D, Knobloch C. The Intramedullary Skeletal Kinetic Distractor (ISKD): first clinical results of a new intramedullary nail for lengthening of the femur and tibia. Injury. 2001;32:SD129–SD139. doi: 10.1016/S0020-1383(01)00116-4. [DOI] [PubMed] [Google Scholar]
- 10.Dahl MT, Gulli B, Berg T. Complications of limb lengthening: a learning curve. Clin Orthop Relat Res. 1994;301:10–18. [PubMed] [Google Scholar]
- 11.Dincyurek H, Kocaoglu M, Eralp IL, Bilen FE, Dikmen G, Eren I. Functional results of lower extremity lengthening by motorized intramedullary nails. Acta Orthop Traumatol Turc. 2012;46:42–49. doi: 10.3944/AOTT.2012.2671. [DOI] [PubMed] [Google Scholar]
- 12.Ellipse Technologies Inc. PRECICE Nail System: Ellipse Technologies. Available at: http://www.ellipse-tech.com/?q=ip. Accessed December 15, 2012.
- 13.Faber FW, Keessen W, van Roermund PM. Complications of leg lengthening. 46 procedures in 28 patients. Acta Orthop Scand. 1991;62:327–332. doi: 10.3109/17453679108994463. [DOI] [PubMed] [Google Scholar]
- 14.Garcia-Cimbrelo E, Curto de la Mano A, Garcia-Rey E, Cordero J, Marti-Ciruelos R. The intramedullary elongation nail for femoral lengthening. J Bone Joint Surg Br. 2002;84:971–977. doi: 10.1302/0301-620X.84B7.12984. [DOI] [PubMed] [Google Scholar]
- 15.Guichet JM, Casar RS. Mechanical characterization of a totally intramedullary gradual elongation nail. Clin Orthop Relat Res. 1997;337:281–290. doi: 10.1097/00003086-199704000-00032. [DOI] [PubMed] [Google Scholar]
- 16.Guichet JM, Deromedis B, Donnan LT, Peretti G, Lascombes P, Bado F. Gradual femoral lengthening with the Albizzia intramedullary nail. J Bone Joint Surg Am. 2003;85:838–848. doi: 10.2106/00004623-200305000-00011. [DOI] [PubMed] [Google Scholar]
- 17.Guichet JM, Grammont PM, Trouilloud P. A nail for progressive lengthening: an animal experiment with a 2-year follow-up [in French] Chirurgie. 1992;118:405–410. [PubMed] [Google Scholar]
- 18.Hankemeier S, Gosling T, Pape HC, Wiebking U, Krettek C. Limb lengthening with the Intramedullary Skeletal Kinetic Distractor (ISKD) Oper Orthop Traumatol. 2005;17:79–101. doi: 10.1007/s00064-005-1123-5. [DOI] [PubMed] [Google Scholar]
- 19.Harbacheuski R, Fragomen AT, Rozbruch SR. Does lengthening and then plating (LAP) shorten duration of external fixation? Clin Orthop Relat Res. 2012;470:1771–1781. doi: 10.1007/s11999-011-2178-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Herzenberg JE, Scheufele LL, Paley D, Bechtel R, Tepper S. Knee range of motion in isolated femoral lengthening. Clin Orthop Relat Res. 1994;301:49–54. [PubMed] [Google Scholar]
- 21.Ilizarov GA. The tension-stress effect on the genesis and growth of tissues. Part II. The influence of the rate and frequency of distraction. Clin Orthop Relat Res. 1989;239:263–285. [PubMed] [Google Scholar]
- 22.Kenawey M, Krettek C, Liodakis E, Meller R, Hankemeier S. Insufficient bone regenerate after intramedullary femoral lengthening: risk factors and classification system. Clin Orthop Relat Res. 2011;469:264–273. doi: 10.1007/s11999-010-1332-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kenawey M, Krettek C, Liodakis E, Wiebking U, Hankemeier S. Leg lengthening using Intramedullary Skeletal Kinetic Distractor: results of 57 consecutive applications. Injury. 2011;42:150–155. doi: 10.1016/j.injury.2010.06.016. [DOI] [PubMed] [Google Scholar]
- 24.Konofaos P, Kashyap A, Neel MD, Ver Halen JP. A novel device for long bone osteodistraction: description of device and case series. Plast Reconstr Surg. 2012;130:418e–422e. doi: 10.1097/PRS.0b013e31825dc069. [DOI] [PubMed] [Google Scholar]
- 25.Krettek C, Miclau T, Schandelmaier P, Stephan C, Mohlmann U, Tscherne H. The mechanical effect of blocking screws (“Poller screws”) in stabilizing tibia fractures with short proximal or distal fragments after insertion of small-diameter intramedullary nails. J Orthop Trauma. 1999;13:550–553. doi: 10.1097/00005131-199911000-00006. [DOI] [PubMed] [Google Scholar]
- 26.Krieg AH, Lenze U, Speth BM, Hasler CC. Intramedullary leg lengthening with a motorized nail. Acta Orthop. 2011;82:344–350. doi: 10.3109/17453674.2011.584209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Krieg AH, Speth BM, Foster BK. Leg lengthening with a motorized nail in adolescents: an alternative to external fixators? Clin Orthop Relat Res. 2008;466:189–197. doi: 10.1007/s11999-007-0040-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Leidinger B, Winkelmann W, Roedl R. Limb lengthening with a fully implantable mechanical distraction intramedullary nail [in German] Z Orthop Ihre Grenzgeb. 2006;144:419–426. doi: 10.1055/s-2006-942169. [DOI] [PubMed] [Google Scholar]
- 29.Mahboubian S, Seah M, Fragomen AT, Rozbruch SR. Femoral lengthening with lengthening over a nail has fewer complications than intramedullary skeletal kinetic distraction. Clin Orthop Relat Res. 2012;470:1221–1231. doi: 10.1007/s11999-011-2204-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Mazeau P, Assi C, Louahem D, L’Kaissi M, Delpont M, Cottalorda J. Complications of Albizzia femoral lengthening nail: an analysis of 36 cases. J Pediatr Orthop B. 2012;21:394–399. doi: 10.1097/BPB.0b013e328354b029. [DOI] [PubMed] [Google Scholar]
- 31.Noonan KJ, Leyes M, Forriol F, Canadell J. Distraction osteogenesis of the lower extremity with use of monolateral external fixation: a study of two hundred and sixty-one femora and tibiae. J Bone Joint Surg Am. 1998;80:793–806. doi: 10.2106/00004623-199806000-00003. [DOI] [PubMed] [Google Scholar]
- 32.Paley D. Problems, obstacles, and complications of limb lengthening by the Ilizarov technique. Clin Orthop Relat Res. 1990;250:81–104. [PubMed] [Google Scholar]
- 33.Paley D, Herzenberg JE, Paremain G, Bhave A. Femoral lengthening over an intramedullary nail: a matched-case comparison with Ilizarov femoral lengthening. J Bone Joint Surg Am. 1997;79:1464–1480. doi: 10.2106/00004623-199710000-00003. [DOI] [PubMed] [Google Scholar]
- 34.Paley D, Tetsworth K. Percutaneous osteotomies: osteotome and Gigli saw techniques. Orthop Clin North Am. 1991;22:613–624. [PubMed] [Google Scholar]
- 35.Papanna MC, Monga P, Al-Hadithy N, Wilkes RA. Promises and difficulties with the use of femoral intra-medullary lengthening nails to treat limb length discrepancies. Acta Orthop Belg. 2011;77:788–794. [PubMed] [Google Scholar]
- 36.Rozbruch SR, Kleinman D, Fragomen AT, Ilizarov S. Limb lengthening and then insertion of an intramedullary nail: a case-matched comparison. Clin Orthop Relat Res. 2008;466:2923–2932. doi: 10.1007/s11999-008-0509-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Sabharwal S, Rozbruch SR. What’s new in limb lengthening and deformity correction? J Bone Joint Surg Am. 2011;93:2323–2332. doi: 10.2106/JBJS.K.01215. [DOI] [PubMed] [Google Scholar]
- 38.Schiedel FM, Pip S, Wacker S, Popping J, Tretow H, Leidinger B, Rodl R. Intramedullary limb lengthening with the Intramedullary Skeletal Kinetic Distractor in the lower limb. J Bone Joint Surg Br. 2011;93:788–792. doi: 10.1302/0301-620X.93B6.25581. [DOI] [PubMed] [Google Scholar]
- 39.Simpson AH, Kenwright J. Fracture after distraction osteogenesis. J Bone Joint Surg Br. 2000;82:659–665. doi: 10.1302/0301-620X.82B5.9945. [DOI] [PubMed] [Google Scholar]
- 40.Simpson AH, Shalaby H, Keenan G. Femoral lengthening with the Intramedullary Skeletal Kinetic Distractor. J Bone Joint Surg Br. 2009;91:955–961. doi: 10.1302/0301-620X.91B7.21466. [DOI] [PubMed] [Google Scholar]
- 41.Tjernstrom B, Olerud S, Rehnberg L. Limb lengthening by callus distraction: complications in 53 cases operated 1980–1991. Acta Orthop Scand. 1994;65:447–455. doi: 10.3109/17453679408995491. [DOI] [PubMed] [Google Scholar]
- 42.Wang K, Edwards E. Intramedullary Skeletal Kinetic Distractor in the treatment of leg length discrepancy—a review of 16 cases and analysis of complications. J Orthop Trauma. 2012;26:e138–e144. doi: 10.1097/BOT.0b013e318238b5b1. [DOI] [PubMed] [Google Scholar]