Abstract
IN BRIEF Type 2 diabetes and its associated comorbidities often require polypharmacotherapy, which may result in poor adherence to treatment. This study evaluated, using subjective patient and physician questionnaire surveys, the impact of pill burden and its associated consequences on patients treated with vildagliptin as add-on to metformin, a fixed-dose combination of vildagliptin/metformin, or another dual oral antidiabetic therapy. Patients’ responses were also analyzed by age (<65 or ≥65 years). The surveys revealed that a high pill count in antidiabetic therapy constitutes a large burden for patients with type 2 diabetes. Treating physicians are aware of the problems that result from a high pill burden, and a majority of them prefer prescribing fixed-dose combinations that have better efficacy and tolerability to reduce pill burden.
Type 2 diabetes is a chronic metabolic disease with a steadily increasing prevalence worldwide. Current statistics published by the International Diabetes Federation show that ∼8.3% of the population aged 20–79 years in Germany are suffering from diabetes. This is equivalent to ∼7.56 million diagnosed patients (1). Treatment guidelines recommend an A1C <7.0% as a glycemic goal (2). Because of the progressive nature of type 2 diabetes, a stepwise intensification of pharmacological therapy is often required, along with lifestyle intervention, to sustain this glycemic goal for prevention of long-term complications (2). Diabetes-related microvascular and macrovascular complications, in addition to the risk of associated comorbidities such as hypertension and hyperlipidemia in many patients with type 2 diabetes, result in polypharmacotherapy and a high pill burden (3,4).
Pill burden, that is, the number of pills a patient needs to take each day, may have a substantial impact on adherence to therapy. Studies in patients with hypertension and dyslipidemia have shown that adherence to treatment decreases with increases in the number of prescribed medications (5,6). Similarly, adherence among patients with type 2 diabetes appears to decrease if the dosing frequency or the number of antidiabetic medications administered each day is increased (7–9).
A large, noninterventional study with the DPP-4 inhibitor vildagliptin (PROVIL—Pill buRden and cOmpliance in type-2 diabetic patients treated with VILdagliptin) was conducted to generate in-depth insights into the management of type 2 diabetes in day-to-day patient care in Germany. The efficacy and safety results of this study were published earlier (10). Here, we report on another objective of this study, which was to evaluate the impact of pill burden on patients with type 2 diabetes in clinical practice settings.
Methods
Study Design
PROVIL, a multicenter, noninterventional study, was conducted among 867 general practitioners and internists across 2,500 centers in Germany between October 2009 and January 2011. Before the initiation of this study, the German Federal Institute for Drugs and Medical Devices (Bundesinstitut für Arzneimittel und Medizinprodukte), the Federal Association of German Panel Doctors (Kassenärztliche Bundesvereinigung), and the Central Federal Association of German Health Insurance Funds (Spitzenverband Bund der Krankenkassen) were notified of the research project in accordance with section 67, paragraph 6, of the German Medicinal Products Act (Arzneimittelgesetz). This study was conducted in compliance with applicable regulatory requirements and recommendations. This study was conducted as per the International Conference on Harmonization of Technical Requirements for Registration of Pharmaceuticals for Human Use, using good clinical practice guidelines, and in accordance with the ethical principles of the Declaration of Helsinki.
Because this was a noninterventional study, the participation of the patients in the study had no influence on their treatment, which was solely prescribed on the basis of medical need. The decisions and treatment choices of the physicians were not influenced. The frequency and scope of assessments were on the basis of the standard of care, and study participation did not entail any additional assessments above and beyond the standard of care.
Study Population
A total of 3,881 male and female patients with type 2 diabetes who were previously receiving oral monotherapy and for whom the treating physicians were considering the addition of a second oral antidiabetic medication were enrolled in this study. Patients were prescribed vildagliptin as an add-on therapy to metformin, a fixed-dose combination of vildagliptin and metformin, or other dual oral antidiabetic therapy (free combinations). Exclusion criteria were as per the contraindications listed in the respective summary of product characteristics. Further details of the study design and data collection are reported elsewhere (10).
Assessments
Pill burden was analyzed by noting total medications and antidiabetic medications taken by patients at baseline. Analyses of patient and physician questionnaires completed at baseline were also performed. Efficacy and tolerability ratings of the medications were assessed by physicians at the end of the study.
Questionnaire
The impact of pill burden on patients’ daily lives and physicians’ day-to-day practice was assessed at baseline using a six-item patient questionnaire and a five-item physician questionnaire, respectively (Table 1). In the patient questionnaire, patients were asked to respond to questions related to the impact of pill burden on their daily lives (e.g., subjective feeling of illness and need for assistance) and associated consequences (e.g., tablet appearance as an identification aid, and concern about medication errors). In addition, treating physicians were asked to complete a questionnaire related to the consequences of medication-related pill burden on day-to-day patient care. There were four response options for most questions in both of the questionnaires: 1) strongly agree, 2) agree, 3) disagree, and 4) strongly disagree. Physicians were asked to rate the efficacy and tolerability of drugs on a scale of “very good,” “good,” “satisfactory,” or “insufficient.”
TABLE 1.
Patient and Physician Questionnaires
| PATIENT QUESTIONNAIRE | |||||
| # | Question | Response options | |||
| 1. | The number of tablets I must take has an influence on how sick I feel. | Strongly agree | Agree | Disagree | Strongly disagree |
| 2. | I need help at home in order to prepare the intake of tablets for the day/week. | Strongly agree | Agree | Disagree | Strongly disagree |
| 3. | How much time do you need per day on average to prepare your tablets? | (data captured in minutes) | |||
| 4. | The appearance of the tablets is important for me to correctly assign my drugs. | Strongly agree | Agree | Disagree | Strongly disagree |
| 5. | The correct use of drugs is harder for me when their appearance changes. | Strongly agree | Agree | Disagree | Strongly disagree |
| 6. | I am concerned about accidentally forgetting pills or taking the wrong tablets/dose. | Strongly agree | Agree | Disagree | Strongly disagree |
| PHYSICIAN QUESTIONNAIRE | |||||
| # | Question | Response options | |||
| 1. | The number of tablets which patients with type 2 diabetes mellitus must take is a challenge for me in the daily treatment routine. | Strongly agree | Agree | Disagree | Strongly disagree |
| 2. | In the daily treatment routine, patients with type 2 diabetes mellitus describe a high number of tablets as a burden. | Strongly agree | Agree | Disagree | Strongly disagree |
| 3. | I am informed about the importance of the subject “number of tablets and treatment adherence (compliance/persistence) and the associated impact.” | Strongly agree | Agree | Disagree | Strongly disagree |
| 4. | I would like more information about the subject “number of tablets and treatment adherence (compliance/persistence) and the related impact.” | Strongly agree | Agree | Disagree | Strongly disagree |
| 5. | If possible, I prefer combination products because they help me reduce the number of tablets which my patients must take every day. | Strongly agree | Agree | Disagree | Strongly disagree |
Note: These subjective questionnaires for patients and physicians were developed in German and translated to English for publication.
Patient questionnaires were analyzed for all patients who signed an informed consent form, regardless of whether a completed case report form (CRF) was available. The data captured on the questionnaires were checked for plausibility by Kantar Health (Munich, Germany). In addition, a random sample of study sites (2%, or 28 sites, in line with the standard practice in Germany [11]) was selected for onsite verification of CRF data against source documents.
Data Analysis
In accordance with the statistical analysis plan defined before the start of the study, descriptive statistics were used for these analyses. In addition, a subgroup analysis by age-group was performed (<65 and ≥65 years) for the patient questionnaire. Statistical analyses were performed using SAS version 9.2 for Windows (SAS Institute, Cary, N.C.).
Results
Patient Demographics and Baseline Characteristics
A total of 3,854 patients completed the questionnaire, but signed informed consent forms were not available for 11 patients. Therefore, data analysis of the patient questionnaire was performed with responses from 3,843 patients. The physician questionnaire was completed by 610 physicians. There were no major differences in demographic data between the CRF population and the patient questionnaire population. Overall, 2,128 patients (55.4%) were male and 1,564 (40.7%) were ≥65 years of age (Table 2). The mean duration of diabetes was 6.1 years (SD 5.1 years, median 4.9 years). The duration of the disease was shorter among younger patients (<65 years of age: mean 5.0 ± 4.4 years, median 3.9 years) compared with older patients (≥65 years of age: mean 7.6 ± 5.6 years, median 6.7 years).
TABLE 2.
Demographic and Clinical Characteristics
| Parameters | Total (n = 3,834) |
|
| n* | Mean ± SD or n (%) | |
| On the basis of the number of patients who completed the CRF | ||
| Age (years) | 3,689 | 62.6 ± 10.8 |
| Men | 2,124 (55.4) | |
| Women | 1,684 (43.9) | |
| Weight (kg) | 3,805 | 89.8 ± 17.2 |
| Men | 2,110 | 94.3 ± 16.7 |
| Women | 1,669 | 84.1 ± 16.1 |
| BMI (kg/m2) | 3,802 | 30.8 ± 5.4 |
| Men | 2,109 | 30.5 ± 5.1 |
| Women | 1,667 | 31.3 ± 5.8 |
| Diabetes duration (years) | 3,307 | 6.1 ± 5.1 (median 4.9) |
| On the basis of the number of patients who completed the questionnaire | ||
| Men | 2,128 (55.4) | |
| <65 years | 1,255 (58.8) | |
| ≥65 years | 791 (50.6) | |
| Women | 1,687 (43.9) | |
| <65 years | 863 (40.4) | |
| ≥65 years | 765 (48.9) | |
| Diabetes duration (years) | 3,293 | 6.1 ± 5.1 (median 4.9) |
| <65 years | 1,846 | 5.0 ± 4.4 (median 3.9) |
| ≥65 years | 1,350 | 7.6 ± 5.6 (median 6.7) |
The reported number of patients (n) is based on the number of patients for whom data were available for the respective parameter (e.g., age and weight) in the CRF population or in the questionnaire population.
Baseline Overall and Oral Antidiabetic Medication Pill Burden
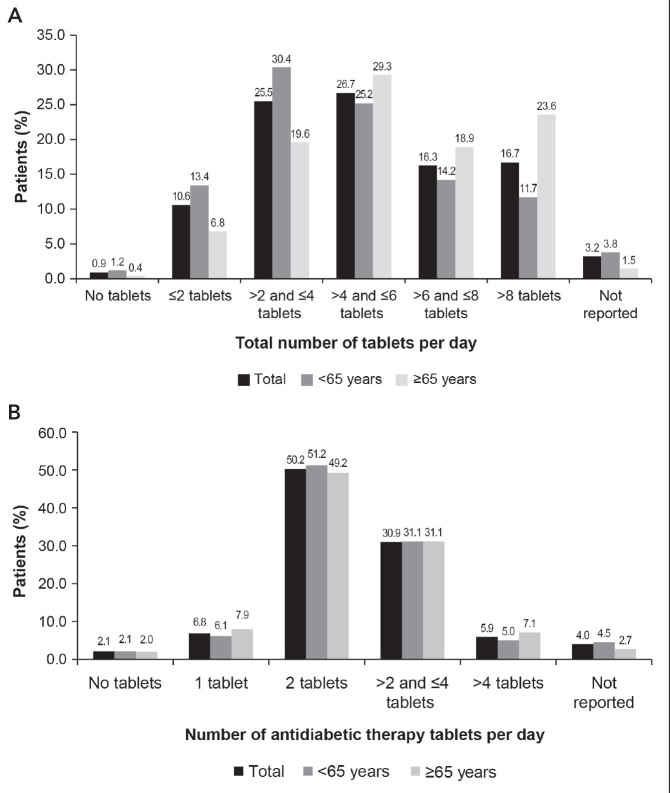
Figure 1 provides an overview of the total number of tablets taken by patients. A majority of the patients were taking three to six tablets per day (total 52.2%, those <65 years of age 55.6%, and those ≥65 years of age 48.9%) (Figure 1A). Younger patients were typically taking fewer tablets per day than older patients. Overall, 42.5% of patients aged ≥65 years were taking more than six tablets daily; of those, 23.6% were taking more than eight tablets daily.
FIGURE 1.
The number of tablets taken per day by total population and age-groups. (A) Total number of tablets. (B) Number of antidiabetic therapy tablets.
Further analysis of the pill burden of antidiabetic medications showed that approximately half of the patients (50.2%) were taking two tablets per day for the treatment of type 2 diabetes (Figure 1B). In addition, 30.9% of patients were taking three to four tablets, and 5.9% of patients were taking more than four tablets for the treatment of type 2 diabetes. There was no difference between older and younger patients in pill burden for antidiabetic medications.
Responses to the Patient Questionnaire
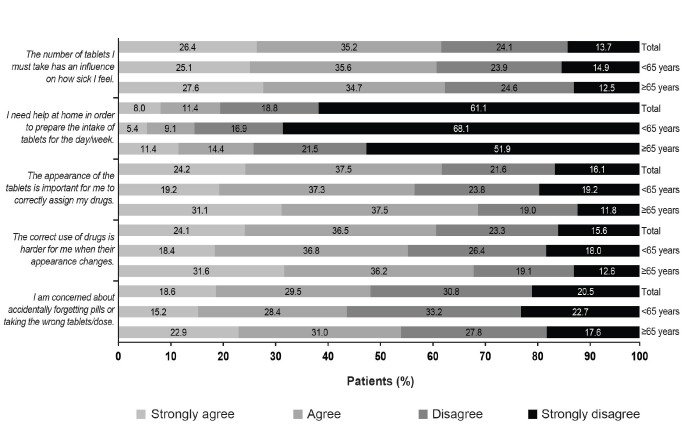
Subjective pill burden responses given by the patients are shown in Figure 2. In total, 61.6% of patients “strongly agreed” or “agreed” that the number of tablets they had to take had an influence on how sick they felt. Approximately one in five patients needed assistance from others for preparing the doses of their tablets. The average time needed per day to prepare the tablets was 6.6 ± 7.4 minutes (median 5.0 minutes) for the overall population (Figure 3). The appearance of the tablet was an important clue for most (61.7%) of the patients to help them identify their medication correctly. Slightly more than 60% of patients “strongly agreed” or “agreed” that the correct use of medications becomes more difficult when the appearance changes, for example, because of a switch of products. Approximately half of the patients (48.1%) were concerned about accidentally forgetting their pills or taking the wrong tablets/dose.
FIGURE 2.
Responses to the patient questionnaire.
FIGURE 3.
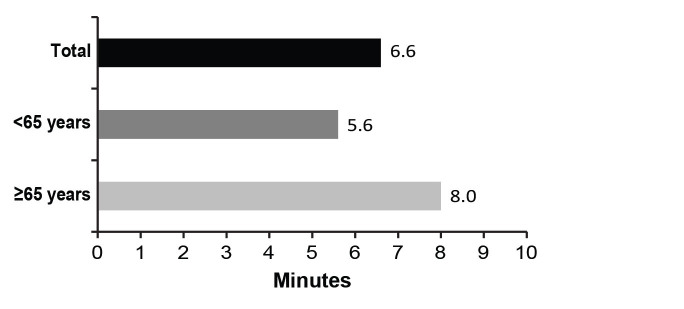
Average time needed for tablet preparation.
Older patients (≥65 years of age) were more often burdened by the high number of tablets and its consequences than younger patients (<65 years of age). A difference in response between older and younger patients of >10% was evident for questions related to the need for assistance with preparing and taking tablets at home for the days of each week, the importance of tablet appearance for medication identification, problems with the correct use of medications when their appearance has changed, and concern about accidentally forgetting their pills or making dosing errors. However, the difference in response between the age-groups was least pronounced in the subjective perception of being ill.
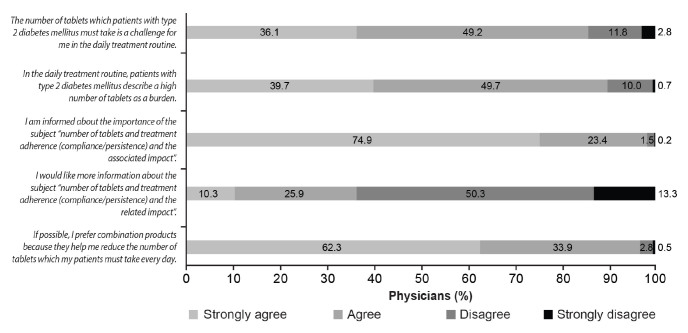
Responses to the Physician Questionnaire
The results of the physician survey are presented in Figure 4. A total of 85.3% of the physicians “strongly agreed” or “agreed” that the number of tablets their patients with type 2 diabetes need to take each day is a therapeutic challenge for them in routine practice. In addition, 89.4% of physicians “strongly agreed” or “agreed” that, in day-to-day patient care, patients with type 2 diabetes said that the need to take a large number of tablets every day was a burden to them. A total of 98.3% of physicians “strongly agreed” or “agreed” that they were aware of the impact of polypharmacotherapy on therapeutic adherence (compliance/persistence) and the associated consequences. This was further evident by the response that a majority (63.6%) of the physicians did not wish to receive more information about the “number of tablets and therapeutic adherence (compliance/persistence) issue and the associated consequences.” Most of the physicians (96.2%) preferred to prescribe fixed-dose combinations to their patients to reduce their pill burden.
FIGURE 4.
Responses to the physician questionnaire.
Efficacy and Tolerability Ratings
At the end of the study, surveyed physicians were asked to rate the efficacy and safety of the antidiabetic therapies used. Regardless of which treatments patients were taking, a high proportion of physicians rated efficacy (83.4%) and tolerability (94.0%) as “very good” or “good.” The percentage of “very good” ratings for both efficacy and tolerability was higher for the vildagliptin add-on therapy (efficacy 47.4%, tolerability 56.4%) and fixed-dose combination of vildagliptin and metformin (50.5 and 62.8%, respectively) than for other dual oral antidiabetic medications (30.8 and 37.4%, respectively). A similar trend was observed when “very good” and “good” ratings for efficacy and tolerability were assessed together.
Discussion
High pill burden may result in poor treatment adherence, which in turn leads to inadequate glycemic control. Long-term complications increase morbidity, pre-mortality, and the burden on health care services. Reasons for nonadherence are multifactorial and difficult to identify; they include age, information, perception, duration of disease, complexity of dosing regimen, polypharmacy, psychological factors, safety, tolerability, and cost (12). Some practical approaches to improve patients’ adherence to medications include reducing treatment complexity by using fixed-dose combination pills, implementing regimens involving less frequent dosing, and using medications that are associated with better efficacy and fewer adverse events (13).
The number of tablets taken each day by patients with type 2 diabetes has an impact on how they subjectively perceive their disease status. In this study, the perception of patients that a high number of pills made them feel sicker is consistent with the previously conducted Brief Illness Perception Questionnaire survey, in which there was a direct relationship between the number of prescribed medications and the severity of illness perceived by patients with type 2 diabetes and cardiovascular disease (14).
Older patients have to cope with a substantially larger pill burden than younger patients (15), as also seen in this study, with one-fourth of patients aged >65 years of age reporting a pill burden of more than eight tablets per day. The high pill burden seen among older patients is presumably because of multiple morbidities and higher age, and it also entails the risk of drug interactions (16). Although this study shows that a large number of tablets taken on a daily basis is perceived as a burden by a majority of patients regardless of age, it is evident that older patients (≥65 years of age) are affected more than younger patients (<65 years of age) by the consequences of pill burden. The difference relates primarily to practical aspects of daily living (e.g., whether patients need assistance with taking their tablets), rather than to subjective feelings of illness. In fact, there were practically no differences between older and younger patients in the latter regard. The greater impact of a high pill burden on older patients is also highlighted by the fact that a majority of older patients agree that appearance is important for medication identification. Patients find it harder to take their medications correctly if the appearance of their medication changes. Patients are also concerned about accidentally forgetting their pills or taking the wrong tablets or doses. Given the specific situation of older patients, often characterized by multiple comorbidities, health care providers should take care in selecting treatments that offer high efficacy and safety.
Treating physicians who were surveyed were aware of the problems that result from a high pill burden, and most of them were willing to use fixed-dose combinations to reduce the pill burden. The “very good” ratings by the physicians for both efficacy and tolerability were higher for vildagliptin and a fixed-dose combination of vildagliptin and metformin than for other dual oral antidiabetic medications. Results from previously conducted retrospective analyses drawn from surveys of the Adelphi Diabetes Disease Specific Programme database of primary care physicians and diabetologists/endocrinologists in Europe suggest that fixed-dose combinations with dipeptidyl peptidase-4 inhibitors are considered to be a positive prescribing choice to improve compliance; they are also associated with improved glycemic control. From the patients’ perspective, the decision to prescribe a fixed-dose combination is associated with improved satisfaction with treatment for type 2 diabetes (17).
Pharmacological therapy should not unnecessarily entail a large number of tablets to be taken because this has an adverse effect on patients’ therapeutic adherence, pill burden, and quality of life (7–9). In light of the aging population in Germany and the expected increasing number of older patients with diabetes in the future, it is particularly important to design strategies for their medical care that address these issues.
The subjective patient and physician questionnaire surveys described here showed that, in day-to-day patient care, a high pill burden in antidiabetic therapy constitutes a large burden for patients with type 2 diabetes. Treating physicians are aware of the problems that result from a high pill burden and prefer to prescribe fixed-dose combinations having better efficacy and tolerability to reduce the pill burden of their patients with type 2 diabetes.
Acknowledgments
The authors thank the patients and staff who participated in this study. All authors participated in the study design, data collection, and data interpretation. The authors take full responsibility for the content of the article and participated in all stages of manuscript development and approval of the final article for publication. The authors thank Anuja Shah, PhD, of Novartis Healthcare Pvt., Ltd., in Hyderabad, India, for medical writing and editorial assistance.
Funding
This study was funded by Novartis Pharma GmbH.
Duality of Interest
M.B. has received honoraria for speaking engagements and has served on advisory boards for Novartis. He has also received honoraria for lecturing or participation on advisory boards from Novo Nordisk, Eli Lilly and Co., AstraZeneca, Sanofi, Boehringer-Ingelheim, Merck Sharpe & Dohme, Bristol-Myers Squibb, and Berlin Chemie.
I.K. is an employee of Kantar Health GmbH, which was contracted by Novartis Pharma GmbH to conduct the PROVIL study.
S.D. and M.D. are employees of the Clinical Research Department of Novartis Pharma GmbH and as such may be eligible for company stock and stock options.
No other potential conflicts of interest relevant to this article were reported.
References
- 1.International Diabetes Federation IDF Diabetes Atlas. 6th ed. Brussels, Belgium, International Diabetes Federation, 2013. Available from http://www.idf.org/diabetesatlas/data-visualisations. Accessed 4 March 2014 [Google Scholar]
- 2.Inzucchi SE, Bergenstal RM, Buse JB, et al. . Management of hyperglycemia in type 2 diabetes: a patient-centered approach: position statement of the American Diabetes Association (ADA) and the European Association for the Study of Diabetes (EASD). Diabetes Care 2012;35:1364–1379 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Morrish NJ, Wang S-L, Steves LK, Fuller JH, Keen H. Mortality and causes of death in the WHO multinational study of vascular disease in diabetes. Diabetologia 2001;44 (Suppl. 2):S14–S21 [DOI] [PubMed] [Google Scholar]
- 4.Stamler J, Vaccaro O, Neaton JD, Wentworth D. Diabetes, other risk factors and 12-year cardiovascular mortality for men screened in the Multiple Risk Factor Intervention Trial. Diabetes Care 1993;16:434–444 [DOI] [PubMed] [Google Scholar]
- 5.Chapman RH, Benner JS, Petrilla AA, et al. . Predictors of adherence with antihypertensive and lipid-lowering therapy. Arch Intern Med 2005;165:1147–1152 [DOI] [PubMed] [Google Scholar]
- 6.Schwartz JS, McLaughlin T, Griffis D, et al. . Adherence to chronic therapy among patients treated for hypertension, dyslipidemia or both. J Am Coll Cardiol 2003;41 (Suppl. A):526A [Google Scholar]
- 7.Cramer JA. A systematic review of adherence with medication for diabetes. Diabetes Care 2004;27:1218–1224 [DOI] [PubMed] [Google Scholar]
- 8.Guillausseau PJ. Impact of compliance with oral anti-hyperglycaemic agents on health outcomes in type 2 diabetes mellitus: a focus on frequency of administration. Treat Endocrinol 2005;4:167–175 [DOI] [PubMed] [Google Scholar]
- 9.Odegard PS, Capoccia K. Medication taking and diabetes. Diabetes Educ 2007;33:1014–1029 [DOI] [PubMed] [Google Scholar]
- 10.Blüher M, Kurz I, Dannenmaier S, Dworak M. Efficacy and safety of vildagliptin in clinical practice-results of the PROVIL study. World J Diabetes 2012;3:161–169 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Theobald K, Capan M, Herbold M, Schinzel S, Hundt F. Quality assurance in non-interventional studies. GMS Ger Med Sci 2009;7:Doc29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.García-Pérez LE, Alvarez M, Dilla T, Gil-Guillén V, Orozco-Beltrán D. Adherence to therapies in patients with type 2 diabetes. Diabetes Ther 2013;4:175–194 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Blonde L, San Juan ZT. Fixed-dose combinations for treatment of type 2 diabetes mellitus. Adv Ther 2012;29:1–13 [DOI] [PubMed] [Google Scholar]
- 14.Stack RJ, Bundy C, Elliott RA, New JP, Gibson JM, Noyce PR. Patient perceptions of treatment and illness when prescribed multiple medicines for co-morbid type 2 diabetes. Diabetes Metab Syndr Obes 2011;4:127–135 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.American Geriatrics Society Expert Panel on the Care of Older Adults with Multimorbidity: Guiding principles for the care of older adults with multimorbidity: an approach for clinicians. J Am Geriatr Soc 2012;60:E1–E25 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kirkman MS, Briscoe VJ, Clark N, et al. . Diabetes in older adults. Diabetes Care 2012;35:2650–2664 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Benford M, Milligan G, Pike J, Anderson P, Piercy J, Fermer S. Fixed-dose combination antidiabetic therapy: real-world factors associated with prescribing choices and relationship with patient satisfaction and compliance. Adv Ther 2012;29:26–40 [DOI] [PubMed] [Google Scholar]