Abstract
IN BRIEF Low socioeconomic status (SES) is consistently identified as a major risk factor for poor health outcomes in youths with type 1 diabetes, yet little is known about the social factors that yield such disparities. This study used survey research to examine the role of SES by focusing on differential resourcing in social support systems for youths with type 1 diabetes and their parents/caregivers. We identified significant inequalities in social support systems and found that parents from lower-income households engage in few coping activities and rarely identify a primary care provider as the main point of contact when facing a diabetes-related problem. Our findings underscore the need to better connect low SES families to diabetes-specific professional resourcing and to raise awareness about the importance of extracurricular activities as a form of social support for youths.
The importance of maintaining optimal glycemic control for individuals with type 1 diabetes is well established (1). Lower socioeconomic status (SES) is consistently identified as a risk factor for poor glycemic control and increased morbidity and mortality (2–6). The Pittsburgh Epidemiology of Diabetes Complications (EDC) study (3) found that individuals with type 1 diabetes from lower SES backgrounds were more likely to suffer from renal disease, coronary heart disease, and neuropathy. The EDC study also found that risk factors for mortality in type 1 diabetes increase fourfold for individuals from lower SES backgrounds (2). Although SES has been identified as a key variable in health outcomes for type 1 diabetes, quantitative studies generating these findings often fail to explicate differences in social life that may lead to such disparities. Because SES is a social, rather than biological, feature, it is imperative to examine characteristics of social context that may influence glycemic control to develop the most effective interventions for reducing health disparities. This is crucial for pediatric patients with type 1 diabetes because early efforts to establish optimal glycemic control happen within the broader social environment.
Sociological studies on inequality in childhood and life experience demonstrate that middle- and upper-class children have vastly different levels of social resourcing than children from less affluent households (7–9). Middle- and upper-class children are exposed to a breadth of extracurricular and other engagement activities such as organized sports, artistic performance groups, and clubs, and their parents tend to have high levels of involvement and intervention in the organizations in which they engage (7–10). Involvement in such activities in childhood is associated with many benefits, including higher graduation rates, improved self-efficacy, decreased risk for depression, greater social network density, and overall “thriving” (10–14). Working-class and poor families have fewer resources to provide such experiences for their children, and, consequently, children from these families are often expected to structure their own free time, are less likely to be directly supervised by adults, and function with greater levels of responsibility at earlier ages (9,10). Although participation in extracurricular activities and high levels of parental involvement in childhood are identified as key variables in educational success (8,9,14), depression, and social isolation (10–12), this research could also be relevant to health disparities among pediatric populations with type 1 diabetes.
There is a tremendous focus on social support in diabetes as it relates to glycemic control for pediatric populations (15–17). For example, parental involvement is crucial in attaining optimal glycemic control and consistent blood glucose monitoring (15–17). However, research on glycemic control and social support focuses primarily on family, teacher, and peer interactions surrounding diabetes (and blood glucose monitoring in particular) and tends to examine diabetes-specific support systems (15–17). Also, existing studies consider parent interactions with the child rather than exploring patterns of interactions between parents and diabetes care providers. This particular way of approaching social support fails to include a consideration of larger group memberships, general parental interaction styles, or social identities unrelated to diabetes that may also have a profound impact on glycemic control.
Given the importance of social support in diabetes as it relates to health outcomes (15–17) and existing research on inequality in childhood experiences (8,9), we examined social support resources available to youths with type 1 diabetes according to SES. Many factors contribute to disparities in health outcomes in type 1 diabetes given the complex interplay of SES and life experience that affect dietary choices, levels of physical activity, access to medical care, and exposure to stress. We specifically focus on social support because of its importance for pediatric populations and its propensity to be changed through intervention, as opposed to other factors that may be more difficult to change. Our framework extends previous studies by considering both diabetes-specific social supports, and nondiabetes social supports.
Although there are many established scales for measuring social support in diabetes (16,17), we chose simple list generators (18) because of their demonstrated reliability as an appropriate methodological tool for pediatric populations (19,20). List-generating questions prompt respondents to create a list for a particular measure (e.g., “List how many people you know who also have type 1 diabetes”) rather than using closed-ended multiple-choice categories (e.g., I know 0–4 people, 5–9 people, etc.).
We examined three general dimensions of social support for youths: 1) “diabetes contacts,” including the number of people a youth knows and is in regular contact with who also have diabetes (network size) and how he or she knows them (role relationship), 2) “youth diabetes coping activities,” or the number of activities a youth engages in that he or she identifies as helpful in coping with diabetes, and 3) “extracurricular activities,” consisting of all the social activities a youth engages in regularly. Parental social support was explored on two dimensions: 1) “parental diabetes coping activities,” or the number of diabetes coping activities engaged in by parents, and 2) “parental support for diabetes care,” or who parents/caregivers identify as the most important “go-to” people when there is a diabetes management problem.
Methods
Recruitment and Measures
Data were collected over a 2-year period during the summers of 2011 and 2012 for patients recruited from endocrine clinics at a university hospital (n = 49). Informed consent and assent was obtained from all subjects under a protocol approved by the institutional review board where the research took place. Selection criteria included 1) age 12–19 years and 2) a diagnosis of type 1 diabetes for at least 2 years to ensure that the honeymoon phase of the disease had ended. All eligible youths were approached, and only three families declined recruitment attempts. Separate youth and parent/caregiver surveys taking no more than 30 minutes to complete were conducted. Surveys were either completed in clinic or taken home and returned by mail in postage-paid envelopes. Participants were compensated with a $30 money order. In addition to survey data, A1C levels were obtained on all participants to measure glycemic control.
Demographic Variables
Measures for most sociodemographic variables, including age, sex, race, and SES, came from the General Social Survey codebook, with the inclusion of an open-ended category of “Other, please explain.” Parent/caregiver surveys contained all demographic questions; youths did not complete these questions. There were two measures for SES: 1) total household income and 2) parental education. Knowing total household income allowed us to create income thresholds in keeping with existing typologies on U.S. economic stratification (21).
Social Support
On the youth survey, the question for diabetes contacts was worded as follows: “List the names of people you know who have diabetes that you are in contact with at least once a year. Also, please tell how you know them (for example: Julie from camp, Mark from school).” Youths were also asked about participation in diabetes coping activities with a list-generating question worded: “List any activities that you participate in that help you cope with the challenges of diabetes.” Youths were assigned a numeric score based on how many distinct names or activities they provided. For example, listing seven names resulted in a diabetes contacts score of 7. Although most diabetes social support scales ask about membership in a diabetes support group, we included more general wording to evoke any activities or group memberships the youths themselves identify as coping activities specific to diabetes.
We also included a measure for youths’ engagement in extracurricular activities with a list-generating question worded: “List your hobbies and/or extracurricular activities you participate in (sports you play, clubs you belong to, things you like doing in your spare time, etc.).” Although there was some overlap between diabetes coping activities and extracurricular activities (addressed below in our results), we believe this particular question adds a missing layer to research on social support within diabetes because the networks that connect youths to larger group memberships outside of their diagnosis deserve specific empirical consideration. Overall, numeric scores were created for social supports by quantifying the total number of distinct items listed for each measure.
Parent/caregiver surveys contained a similar measure for social support with an item worded: “List any activities that you participate in on a regular basis that help you cope with the challenges of diabetes.” Parents/caregivers were thus assigned a numeric score for parental diabetes coping activities. Additionally, parents were asked to complete the following open-ended question designed to capture and better understand who the most important “go-to” people are when a problem arises with diabetes: “List the people that you most count on to help manage the challenges of diabetes. Briefly explain why.” We conceptualized this measure as parental support for diabetes care.
Data Analysis
Our list-generating questions were used to quantitatively analyze social support network size according to SES. Also, the social support lists were used to qualitatively examine role relationships for youths’ diabetes contacts and variations in the types of youth and parent coping activities. SPSS version 21 (IBM; Armonk, NY) was used for all quantitative data analysis, which included basic frequency distributions, a comparison of means, t tests, and Pearson’s correlation for A1C, and numeric demographic variables. A content analysis of social support answers was conducted using a method of constant comparison (22,23) through the following coding schema: 1) diabetes contacts role relationships: “family tie,” “school tie,” “neighborhood tie,” “diabetes-specific activity tie,” and “other”; 2) youth and parent diabetes coping activities: “diabetes-specific professional resource” (activities/groups organized by local or national diabetes chapters or interests) and “diabetes nonspecific” (activities/groups not organized by local or national diabetes chapters or interests); and 3) parental support for diabetes care: “professional resource” (medical professionals) or “kinship resources” (family members).
Results
Table 1 presents participants’ characteristics and mean A1C levels. In keeping with etiological trends in type 1 diabetes, our sample contained equal sex ratios and an overrepresentation of whites. The mean age was 15 ± 2.1 years. The mean duration of disease was 6.4 ± 3.4 years. Family income ranges varied; 38% were from the poor/working-class bracket (<$40,000), 33% were from the middle-class bracket ($40,000–$80,000), and 29% were from the upper middle–class/upper-class bracket (>$80,000). Youths from lower SES households had higher mean A1C levels that were found to be statistically significant both through t tests for means and Pearson’s correlation coefficients. This was true when SES was measured by household income (r = –0.39, P <0.01) and by level of parental education (r = –0.32, P <0.05). There were high levels of correlation between the measures for SES (income and parental education; r = 0.75, P <0.000). High levels of collinearity among our variables and our small sample size limited our ability to use a true linear regression model. However, for preliminary purposes, it is important to note that, as each numeric social support measure increased, A1C decreased with a statistically significant correlation for youth extracurricular activities (r = –0.38, P <0.007).
TABLE 1.
Characteristics of the Study Population and Comparison of Mean Glycemic Control and Social Supports
| n (of total 49) | A1C (%) | Diabetes Contacts Score | Youth Coping Score | Extracurricular Activities Score | Parent Coping Score | |
| Age (years) (mean 15 ± 2.1) | ||||||
| Ages 12–15 | 27 | 8.6 ± 1.0 | 3.6 ± 3.1 | 1.5 ± 1.3 | 4.2 ± 2.7 | 1.9 ± 1.5 |
| Ages 16–19 | 22 | 8.7 ± 1.3 | 3.3 ± 2.9 | 1.6 ± 1.6 | 3.2 ± 2.5 | 2.2 ± 2.4 |
| Disease duration (years) (mean 6.4 ± 3.4) | ||||||
| ≤6 | 26 | 8.7 ± 1.4 | 2.5 ± 1.7* | 1.2 ± 1.0 | 3.6 ± 1.9 | 1.8 ± 1.7 |
| ≥7 | 23 | 8.5 ± 0.8 | 4.3 ± 3.6 | 1.7 ± 1.5 | 4.2 ± 2.8 | 2.1 ± 2.2 |
| P <0.05, t test | ||||||
| r = 0.29, P <0.05 | ||||||
| Sex | ||||||
| Female | 24 | 8.6 ± 1.0 | 4.2 ± 3.0* | 1.8 ± 1.7 | 3.8 ± 2.8 | 2.5 ± 2.1 |
| Male | 25 | 8.7 ± 1.4 | 2.7 ± 2.8 | 1.4 ± 0.9 | 3.7 ± 2.8 | 1.6 ± 1.4 |
| P <0.05, t test | ||||||
| Race/ethnicity | ||||||
| Black | 4 | 10.2 ± 0.6† | 1.6 ± 1.9 | 1.5 ± 1.1 | 2.6 ± 1.9 | 1.0 ± 0.4 |
| Hispanic | 3 | 8.8 ± 0.4 | 4.0 ± 0.8 | 2.3 ± 2.3 | 3.3 ± 1.5 | 1.6 ± 1.1 |
| White | 41 | 8.5 ± 1.1 | 3.7 ± 3.1 | 1.6 ± 1.4 | 4.0 ± 2.7 | 2.3 ± 2.1 |
| Other | 1 | — | — | — | — | |
| Household income ($) | ||||||
| <40,000 | 18 | 9.4 ± 1.4* | 1.6 ± 1.6* | 0.7 ± 0.7* | 2.5 ± 2.3* | 1.1 ± 1.0* |
| 40,000–80,000 | 15 | 8.1 ± 0.8 | 4.5 ± 2.8 | 2.0 ± 1.4 | 4.0 ± 2.4 | 2.1 ± 1.8 |
| >80,000 | 14 | 8.3 ± 0.9 | 4.7 ± 3.8 | 2.2 ± 1.6 | 5.0 ± 2.5 | 2.9 ± 2.3 |
| Other: “don’t know” | 2 | — | — | — | — | — |
| P <0.01, t test | P <0.01, t test | P <0.01, t test | P <0.01, t test | P <0.01, t test | ||
| r = –0.39, P <0.01 | r = 0.40, P <0.01 | r = 0.42, P <0.01 | r = 0.38, P <0.01 | r = 0.44, P <0.01 | ||
| Parental Education | ||||||
| Did not complete HS | 3 | 10.9 ± 1.3* | 1.6 ± 1.1* | 1.0 ± 1.2* | 1.2 ± 0.9* | 1.3 ± 1.5* |
| HS diploma | 17 | 8.8 ± 0.9 | 2.8 ± 1.9 | 1.3 ± 0.9 | 3.1 ± 2.5 | 1.6 ± 1.1 |
| AA/skilled degree | 10 | 8.2 ± 0.9 | 3.2 ± 2.8 | 1.5 ± 1.1 | 4.0 ± 2.7 | 3.3 ± 3.1 |
| BA/BS degree | 10 | 8.2 ± 1.1 | 4.8 ± 3.0 | 2.0 ± 1.5 | 5.0 ± 2.0 | 3.4 ± 1.9 |
| Graduate degree | 7 | 8.3 ± 0.8 | 4.5 ± 4.7 | 2.8 ± 2.0 | 4.8 ± 3.3 | 3.2 ± 1.8 |
| Other: missing data | 2 | — | — | — | — | — |
| r = –0.32, p <0.05 | r = 0.25, p <0.05 | r = 0.32, p <0.05 | r = 0.39, p <0.01 | r = 0.29, p <0.05 |
P values (indicated when significant) are for t tests when examining categorical variables and for Pearson’s correlation coefficients when examining numeric variables. SES is examined numerically by using income in dollars and parental education in years. tTests are only used when there is symmetry among cell values and are only presented in terms of the significant P values.
Three of the black participants were at the <$40,000 income threshold (poor/working class), and one was at the >$80,000 income threshold (upper middle/upper class); one Hispanic youth was at the <$40,000 income threshold, and one was at the $40,000–$80,000 threshold, and one was at the >$80,000 threshold. There were not enough non-white participants to perform t tests.
AA, associate of arts; BA, bachelor of arts; BS, bachelor of science; HS, high school.
Youth Social Support and Demographic Variables
Table 1 also presents a mean comparison of social support measures for youths. SES was significant in social support; youths from higher-SES households (whether determined by income or parental education level) had higher mean scores for diabetes contacts, diabetes coping activities, and extracurricular activities than youths from working-class households (P <0.01 for t tests with $40,000 as the defining income cusp level). Sex was found to be significant for diabetes contacts; females had significantly more diabetes contacts than their male counterparts (P <0.05, t test). Diabetes contacts were also significantly higher for youths who had lived with diabetes the longest (P <0.05, t test; r = 0.29, P <0.05 for Pearson’s correlation).
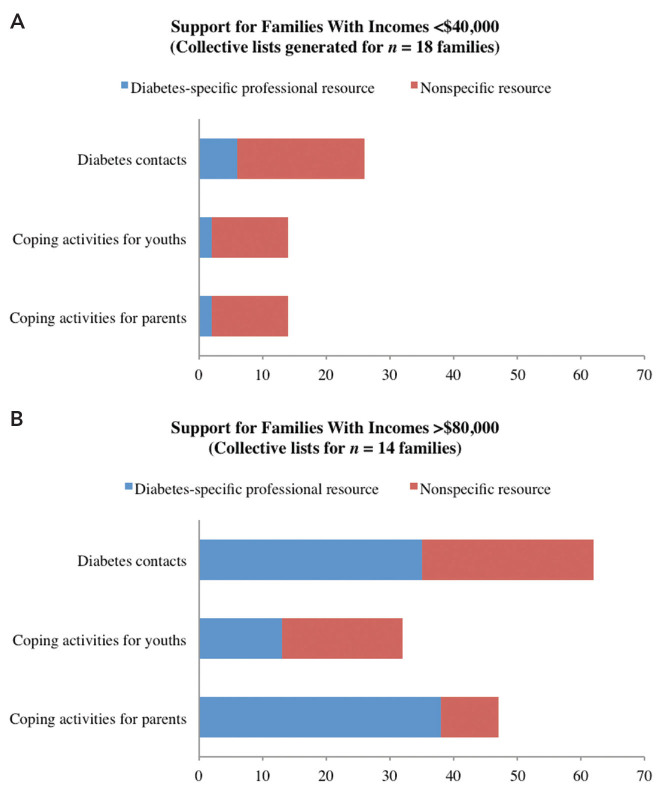
Figure 1 presents a content analysis of diabetes contacts and diabetes coping activities revealing patterned differences in the type of activity by SES; affluent youths listed three times more diabetes-specific professional organizations or activities in which they were regularly involved. This was also seen with diabetes contacts; a content analysis of role relationship revealed that youths from more affluent households were more likely to be connected to other youths with diabetes through diabetes-specificprofessional activities, whereas youths from less affluent households knew other people with diabetes mainly through happenstance (e.g., a school tie rather than a tie from a diabetes-specific group).
FIGURE 1.
Content analysis for type of social support by total household income (A, <$40,000; B, >$80,000). Diabetes-specific professional resources include such things as local Juvenile Diabetes Research Foundation chapters, diabetes camps, Children with Diabetes events, and American Diabetes Association membership. Nonspecific resources for youth contacts include knowing someone with diabetes through a neighborhood tie or a school tie rather than through a diabetes-specific professional tie. Nonspecific resources for youth and parent coping activities include such things as attending church, family vacations, and hobbies such as crafting or hiking.
There were areas of overlap in the lists youths generated for extracurricular activities and diabetes coping activities; 40% of youths listed at least one activity as both an extracurricular and a coping activity, and of those youths, all but two were from middle- or upper-class households. Almost all (90%) of the youths who listed something as both an extracurricular and a coping activity explained (without being prompted to do so) that the extracurricular activity functioned as a coping mechanism because it made them forget about diabetes or allowed them to feel “normal.” Youths elaborated in their lists for diabetes coping activities by saying things such as, “The best activity to help me cope is where I am treated like everyone else” (white male, 19 years of age, household income >$80,000) or “Anything that lets them see I am just like them [people without diabetes]” (white female, 17 years of age, household income $40,000–$80,000).
Parental Social Supports and SES
A comparison of mean parental social supports by each demographic variable also appears in Table 1. Parental coping activities were significantly higher for families with incomes >$40,000 and parental education levels at the Associate of Arts/Skilled Trade degree or higher. Figure 1 shows a content analysis of types of parental support by household income. More than 80% of parents from middle- and upper-class households listed diabetes-specific professional activities (e.g., support groups, Children with Diabetes events, and Juvenile Diabetes Research Foundation [JDRF] walks), whereas there were only two occasions in which parents/caregivers from poor/working-class households listed such activities. In addition, 40% of parents from the middle to upper class noted that they held leadership titles in diabetes-specific organizations, with comments such as:
“I mentor newly diagnosed families. [Husband’s name] serves on the JDRF board.” (parents of a white male, 17 years of age; household income >$80,000; maternal level of education bachelor’s degree)
“I regularly chair diabetes fundraising events and co-chair several committees related to diabetes events and groups.” (mother of a white male, 15 years of age; household income $40,000–$80,000; maternal level of education graduate degree)
“I work in different capacities in diabetes education as a nurse and through local organizations.” (mother of a black male, 17 years of age; household income >$80,000; maternal level of education graduate degree)
There were no examples of parents from working-class or poor families listing such leadership positions.
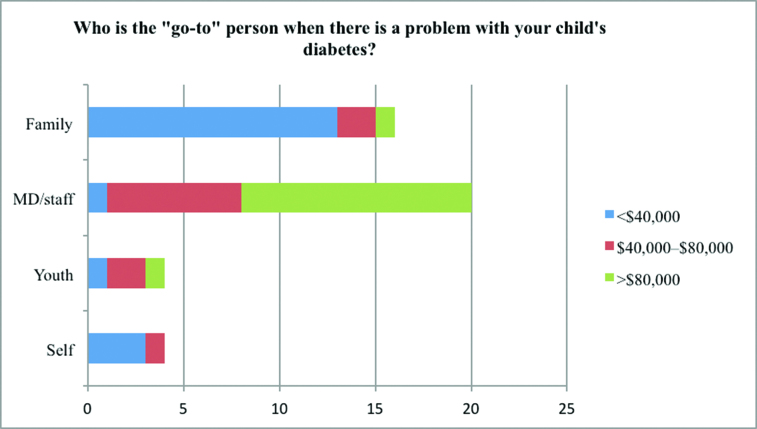
Figure 2 presents parental support for diabetes care by total household income and parental level of education. With regard to who their “go-to” people are when it comes to a problem in diabetes care, 80% of parents from the highest income brackets and educational levels listed their child’s pediatric endocrinologist/medical staff (professional resource) as their most important “go-to” person. In contrast, 80% of parents from the lowest income bracket and educational levels listed a family member (kinship resource). Interestingly, when asked to explain their answers, affluent parents commented readily on the quality and access of their children’s diabetes medical staff, whereas less affluent parents focused on the primacy and value of family. These contrasting viewpoints are captured in the answers of two parents in our sample who share the same physician—one from the highest income and education threshold and the other from the lowest:
“Dr. [name of pediatric endocrinologist] and [name of nurse educator] are the most important people to us—always available for education or trouble-shooting. Our psychologist also helps [youth’s name] cope and to understand his responsibilities.” (mother of a white male, 15 years of age; household income >$80,000; maternal level of education graduate degree)
“My sister and cousin help me when there is a problem with [youth’s name] diabetes. Family is so important. Family’s all you got in this world!” (grandmother of a white male, 14 years of age; household income <$40,000; maternal level of education less than a high school diploma)
FIGURE 2.
Parental support for diabetes care by total household income.
Discussion
Our data indicate that youths with type 1 diabetes from lower SES backgrounds are under-resourced in many areas of social support. They know few people who also have diabetes; neither they nor their parents typically engage in diabetes-specific groups or organizations; they participate in few, if any, extracurricular activities; and their parents turn to other family members rather than to medical professionals for help when there are challenges in diabetes management. We posit that this lack of social support has important implications for disparities in health outcomes.
These discrepancies in social activities indicate that youths from lower SES households participate less often in activities supervised by adults and are less likely to have parents interact with the pediatric endocrine staff. Consequently, they may have fewer prompts for blood glucose monitoring and other behaviors that improve glycemic control (15,24,25). This point helps clarify that providing more diabetes education for low-income parents may not be as valuable as increasing adult supervision during after-school hours or providing more opportunities for contact with diabetes-specific professionals in general because youths who most need the help of diabetes professionals remain isolated from them.
Also, although sex was not the focus of our study, our findings indicate that males may have fewer social supports when it comes to diabetes contacts. Although there were no observed sex differences in glycemic control, the differential resourcing may have a bearing on other health outcomes such as depression and social isolation.
Research on social support in diabetes could be enhanced by considering the extracurricular activities youths engage in, as well as the types of support activities related to diabetes in which their parents engage. Roughly half of the youths in our sample commented that participation in extracurricular activities or groups unrelated to diabetes were their most valuable coping activities because they allowed them an identity beyond their diagnosis. Theoretically, the lower levels of involvement in extracurricular and other structured engagement activities by working-class and poor youth demonstrated here and in research unrelated to diabetes (8–10) may have direct implications for youths with type 1 diabetes because depression, social isolation, and lack of parental involvement can hinder efforts to achieve optimal glycemic control (15,26). Extracurricular involvement can also serve as a bridge for youths in poor and working-class households, providing resources beyond their local communities and often serving as liaisons for college scholarships. Moreover, the infrequency with which parents from lower SES households engage in diabetes professional groups or seek professional help with diabetes care warrants further attention. We need to better understand the barriers that keep some parents from professional resources, whether these stem from a lack of time, money, or cultural ease in such engagement or from other concerns.
The limitations of our study include its small sample size, an underrepresentation of non-white participants, and a lack of focus on social media as a mechanism of social support. Further investigation is needed to increase our understanding of the empirical relationship between social support, SES, and glycemic control. Given the limited sample size and nature of this exploratory study, we cannot statistically test these relationships; rather, we can simply demonstrate differences in social life for youths with type 1 diabetes according to their family SES.
More research is also needed to better understand racial disparities in social support as it may relate to glycemic control (27,28). Given the fact that black and Hispanic youths living in the United States have a three-times-greater risk for living in poverty (29), racial disparities are somewhat entangled with SES disparities. In fact, SES has been found to be more important in overall disparities for type 1 diabetes than race/ethnicity alone (6). Our sample, however, lacked enough non-white participants to adequately demonstrate any comparisons of social supports according to race or ethnicity.
In addition, our research did not allow for a systematic comparison of social networks facilitated through social media versus face-to-face contact (e.g., gaming with friends online vs. participating in a monthly videogame club through a local organization).
Despite these limitations, our data have important implications for youths with type 1 diabetes. Unearthing the basic notion that youths from lower SES households have few opportunities for diabetes-specific or nonspecific social support provides a new lens through which to frame solutions. Efforts to increase family education and involvement should be paired with interventions that also provide resourcing beyond the family level. Increasing social support in the forms of diabetes contacts, social activities for youths, and professional resources for parents may provide effective intervention strategies for reducing health disparities in youths with type 1 diabetes. We couple the findings from this study with existing research on childhood inequalities to offer the recommendations for diabetes health care providers listed in Table 2.
TABLE 2.
Recommendations to Reduce Health Disparities Among Youths With Type 1 Diabetes
| Recommendation | Rationale |
| Make preemptive efforts with at-risk families to maintain regular contact with households between office visits using text messaging or phone contact based on available resources to quickly ascertain issues of concern. | Lower-income families in this study indicated that they rely more readily on kinship networks than on diabetes professionals in diabetes management and tend to be involved in few activities that connect them to health care providers. Lower-income youths are also hospitalized much more frequently for serious diabetes-related complications (5). |
| Do not rely on the Internet as the sole source of communication with at-risk families, and update contact information frequently. | Research on computer use in the United States indicates that only 49% of households making ≤$25,000/year have access to the Internet (29). Phone outreach will be important. Also, the working poor tend to move more and change telephone numbers frequently given the constraints of poverty. |
| Consider cultural differences in parenting styles when assigning insulin regimens. | Youths from lower-SES households are more likely to be unsupervised by adults and to have low levels of direct monitoring (8,9). In addition, for publically insured youths, access to supplies or technology may change as they transition into adulthood. |
| Recognize extracurricular involvement as a meaningful resource for coping with the challenges of diabetes. | There are many documented benefits of engaging in extracurricular activities in childhood and adolescence. For youths with type 1 diabetes, such involvement increases social resourcing and provides an identity beyond their diagnosis, thus offsetting disease stigma (30). |
| Reduce barriers that keep lower-income families from gaining access to diabetes professional resourcing. | Income constraints can create obstacles for having transportation to office visits, affording diabetes camps for children, or having access to online diabetes resources. Direct financial support in the form of transportation vouchers or scholarships, as well as incentives for keeping office visits, are invaluable. |
Supplementary Material
Acknowledgments
The authors thank the families who participated in this research. They also thank Dr. Don Russell of Mars Hill University for statistical analysis support and the staff at the University of Florida’s Diabetes Center of Excellence, including Kathryn Parker, RD, LD/N, Shannon Lyles, RN, CDE, and Shannon Patrick, ARNP, MSN.
Duality of Interest
No potential conflicts of interest relevant to this article were reported.
References
- 1.DCCT Research Group Effect of intensive therapy on the microvascular complications of type 1 diabetes mellitus. JAMA 2002;287:2563–2569 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Secrest AM, Costacou T, Gutelius B, Miller RG, Songer TJ, Orchard TJ. Association of socioeconomic status with mortality in type 1 diabetes: the Pittsburgh Epidemiology of Diabetes Complications study. Ann Epidemiol 2011;21:367–373 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Secrest AM, Costacou T, Gutelius B, Miller RG, Songer TJ, Orchard TJ. Associations between socioeconomic status and major complications in type 1 diabetes: the Pittsburgh Epidemiology of Diabetes Complications (EDC) study. Ann Epidemiol 2011;21:374–381 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Cutfield SW, Derraik JGB, Reed PW, Hofman PL, Jefferies C, Cutfield WS. Early markers of glycaemic control in children with type 1 diabetes mellitus. PLoS One 2011;6:1–6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Keenan HT, Foster HT, Bratton SL. Social factors associated with prolonged hospitalization among diabetic children. Pediatrics 2002;109:40–44 [DOI] [PubMed] [Google Scholar]
- 6.Gallegos-Macias AR, Macias SR, Kaufman E, Skipper B, Kalishman N. Relationship between glycemic control, ethnicity and socioeconomic status in Hispanic and non-Hispanic youths with type 1 diabetes mellitus. Pediatr Diabetes 2003;4:19–23 [DOI] [PubMed] [Google Scholar]
- 7.Bourdieu P. Distinctions: A Social Critique of the Judgment of Taste. Cambridge, Mass, Harvard University Press, 1984 [Google Scholar]
- 8.Lareau A. Invisible inequality: social class and childrearing in black families and white families. Am Sociol Rev 2002;67:747–776 [Google Scholar]
- 9.Lareau A. Unequal Childhoods: Class, Race and Family Life. Berkeley, Calif, University of California Press, 2003 [Google Scholar]
- 10.Horvat E, Weininger EB, Lareau A. From social ties to social capital: class differences in the relations between schools and parent networks. Am Educ Res J 2003;40:319–351 [Google Scholar]
- 11.Lerner RM, Dowling EM, Anderson PM. Positive youth development: thriving as the basis of personhood and civil society. Appl Dev Sci 2003;7:172–180 [DOI] [PubMed] [Google Scholar]
- 12.Li Y, Lerner R. Trajectories of school engagement during adolescence: implications for grades, depression, delinquency and substance use. Dev Psychol 2011;47:233–247 [DOI] [PubMed] [Google Scholar]
- 13.Mason MJ, Schmidt C, Abraham A, Walker L, Tercyak K. Adolescents’ social environment and depression: social networks, extracurricular activity, and family relationship influences. J Clin Psychol Med Settings 2009;16:346–354 [DOI] [PubMed] [Google Scholar]
- 14.Zarrett N, Fay K, Li Y, Carrano J, Phelps E, Lerner R. More than child’s play: variable- and pattern-centered approaches for examining effects of sports participation on youth development. Dev Psychol 2009;45:368–382 [DOI] [PubMed] [Google Scholar]
- 15.Laffel L, Vangsness L, Connell A, Goebel-Fabbri A, Butler D, Anderson BJ. Impact of ambulatory, family-focused teamwork intervention on glycemic control in youth with type 1 diabetes. J Pediatr 2003;142:409–416 [DOI] [PubMed] [Google Scholar]
- 16.La Greca A, Bearman K. The Diabetes Social Support Questionnaire–Family Version: evaluating adolescents’ diabetes-specific support from family members. J Pediatr Psychol 2002;27:665–676 [DOI] [PubMed] [Google Scholar]
- 17.Yanover T, Sacco WP. Reliability of diabetes-specific social support scales. Psychol Health Med 2008;13:627–631 [DOI] [PubMed] [Google Scholar]
- 18.Hlebec V, Kogovsek T. How (not) to measure social support networks: the name generator vs. the role relation approach. Adv Method Stat 2011;8:191–207 [Google Scholar]
- 19.Tisdall K, Davis JM, Gallagher M. Researching with Children and Young People: Research Design, Methods, and Analysis. Thousand Oaks, Calif, Sage, 2009 [Google Scholar]
- 20.Borgers N, Hox J, Sikkel D. Response quality in survey research with children and adolescents: the effect of labeled response options and vague quantifiers. Int J Public Opin Res 2003;15:83–94 [Google Scholar]
- 21.Gilbert D. The American Class Structure in an Age of Growing Inequality. 8th ed. Thousand Oaks, Calif, Sage, 2010 [Google Scholar]
- 22.Glaser BG, Strauss AL. The Discovery of Grounded Theory. Chicago, Aldine, 1967 [Google Scholar]
- 23.Strauss AL, Corbin J. Basics of Qualitative Research: Grounded Theory Procedures and Research. Newbury Park, Calif, Sage, 1990 [Google Scholar]
- 24.Haller MJ, Stavley MS, Silverstein JH. Predictors of control of diabetes monitoring may be the key. J Pediatr 2004;144:660–661 [DOI] [PubMed] [Google Scholar]
- 25.Wysocki T, Nansel TR, Holmbeck GN, et al. Collaborative involvement of primary and secondary caregivers: associations with youths’ diabetes outcomes. Pediatr Psychol 2009;34:869–881 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Stewart S. Adolescents with type 1 diabetes: depression and poor metabolic control. Curr Med Lit Diabetes 2006;23:1–5 [Google Scholar]
- 27.Kamps JL, Hempe JM, Chalew SA. Racial disparity in A1C independent of mean blood glucose in children with type 1 diabetes. Diabetes Care 2010;33:1025–1027 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Danielson KK, Drum ML, Estrada CL, Lipton RB. Racial and ethnic differences in an estimated measure of insulin resistance among individuals with type 1 diabetes. Diabetes Care 2010;33:614–619 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.U.S. Bureau of the Census Computer and Internet Use in the United States. Report P20, No. 569. Washington, D.C, U.S. Bureau of the Census, May 2013 [Google Scholar]
- 30.Goffman E. Stigma: Notes on the Management of Spoiled Identity. New York, Simon & Schuster, 1963 [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.