According to the most recent data from the Centers for Disease Control and Prevention, 25.8 million people in the United States (8.3% of the population) have diabetes (1). Type 2 diabetes accounts for 90–95% of diabetes diagnoses, and >85% of people with type 2 diabetes are overweight or obese (1). Increased BMI, which is common in the type 2 diabetes population, has a well-established association with symptoms of gastroesophageal reflux disease (GERD) (2,3). Central adiposity is an important risk factor in the development of reflux and, subsequently, erosive esophagitis, Barrett’s esophagus, esophageal adenocarcinoma, and gastric cardia adenocarcinoma (2,3).
Increased BMI is not the only risk factor for the development of GERD, particularly among people with diabetes. Among those with type 2 diabetes, peripheral neuropathy is an independent risk factor for erosive esophagitis (4). In this population, there is a greater incidence of erosive esophagitis among individuals with neuropathy than among those without neuropathy, although those with and without neuropathy experience similar GERD symptoms (4). Approximately 60–70% of people with diabetes have mild to severe forms of nervous system damage, which may partly explain why low-grade esophageal dysplasia is twice as likely in individuals with than in those without diabetes (1,5). Additionally, both asymptomatic and symptomatic reflux is more prevalent in individuals with diabetes than in those without diabetes (6,7). Likewise, type 2 diabetes has been demonstrated to be a risk factor for symptomatic GERD (8).
Among individuals with diabetes, 40.7% experience symptomatic GERD, and 70% of those use oral antidiabetic medications. Thus, it is likely that millions of individuals are managing blood glucose and GERD concomitantly with oral medications (1,7) Therefore, it is important to assess the drug interactions and clinical sequelae that may occur with this particular polypharmacy scenario. This article addresses the potential for vitamin B12 depletion induced by concomitant use of metformin and acid-suppressing medications to contribute to neuropathy among individuals with diabetes.
Vitamin B12, Diabetes, and Neuropathy
Vitamin B12 is a water-soluble micronutrient that serves as a co-factor for methionine synthase and L-methylmalonyl-CoA mutase (9–11). As a result, B12 is important for the production of S-adenosylmethionine, nucleic acid methylation, and hemoglobin synthesis, as well as protein and fat metabolism (9,11). The signs and symptoms of vitamin B12 deficiency can be easily mistaken for those of diabetic neuropathy. These include paresthesias, diminished vibratory sensation, diminished proprioception, loss of cutaneous sensation, muscle weakness, abnormal reflexes, urinary and fecal incontinence, loss of vision, reduced sensory nerve conduction velocities, and axonal degeneration, as well as evoked potential and magnetic resonance imaging abnormalities consistent with demyelination (12–15).
Most individuals with diabetes have mild to severe forms of nervous system damage (1). B12 supplementation, alone or in combination with other substances, has been demonstrated to improve multiple aspects of diabetic neuropathy, including lower-extremity epidermal nerve fiber density, cutaneous sensitivity, pain, paresthesia, autonomic symptoms, and ulnar motor and median sensory nerve conduction velocities (16–25).
Although numerous forms of vitamin B12 exist, supplement and pharmaceutical formulations typically contain vitamin B12 as cyanocobalamin, a synthetic form that the body readily converts to the active forms methylcobalamin and 5-deoxyadenosylcobalamin (26). Because of the liberation of cyanide during the conversion of cyanocobalamin to its active forms, individuals with Leber’s optic neuropathy (a genetic disorder exacerbated by chronic cyanide intoxication) should not be administered cyanocobalamin (26). Administration of vitamin B12 in forms other than cyanocobalamin (e.g., methylcobalamin), eliminates the risk of cyanide toxicity and subsequent neuropathy.
Successful strategies for managing diabetic neuropathy with B12 are summarized below.
Intrathecal injections (2,500 µg in 10 mL saline, monthly) of methylcobalamin have been shown to improve paresthesia and burning pain in individuals with diabetes (16).
Oral administration of two 250-mg methylcobalamin capsules three times daily for 4 months resulted in improvement of both somatic and autonomic symptoms and regression of diabetic neuropathy signs (17).
Oral methylcobalamin (2 mg), in combination with 3 mg L-methylfolate and 35 mg pyridoxal-5´-phosphate (MC-LMF-PP) twice daily for 4 weeks and then once daily for 48 weeks, was reported to result in significant improvement in peripheral nerve sensitivity (19).
Likewise, oral MC-LMF-PP twice daily for 6 months demonstrated significant improvement in epidermal nerve fiber density, as assessed by biopsy, in 8 of 11 patients (73%) (20).
Patients receiving a 500-µg methycobalamin intravenous injection three times per week for 6 months were reported to have improvement in pain, paresthesia, and nerve conduction velocities (21).
Methylcobalamin injections of 500 µg administered intramuscularly three times per week for 4 weeks, followed by 500 µg administered orally three times a day for an additional 8 weeks, improved spontaneous pain and numbness (22).
Oral supplementation with methylcobalamin (1,500 µg daily for 24 weeks) in individuals with diabetes has been demonstrated to improve tingling, upper limb symptoms, ataxia, signs of impaired position sense, vibration sense, pinprick sensation, and knee reflexes (25).
These reports all noted improvement in diabetic neuropathy without also documenting baseline B12 levels. Therefore, it is reasonable to assume that the neuropathy that responded to B12 supplementation could have been, at least in part, B12 deficiency neuropathy rather than diabetic neuropathy.
Metformin-Induced Vitamin B12 Depletion
In 1969, Berchtold et al. (27) noted that patients managed with metformin therapy for 2–3 months malabsorbed vitamin B12. Since then, B12 deficiency among individuals managed with metformin has been reported to occur at an incidence ranging between 5.6 and 36% (Table 1) (28–34). The broad range of incidence rates reported in Table 1 may be attributed to cumulative drug-induced B12 depletion related to both the dosage and the duration of metformin use (35–38). However, findings of cumulative effects are not entirely consistent throughout the literature (33).
TABLE 1.
Incidence of Vitamin B12 Deficiency Among Individuals Managed With Metformin
| Study | Sample Size (n) | Individuals With B12 Deficiency (n) | Individuals With B12 Deficiency (%) |
| Tomkin et al., 1971 (28) | 71 | 4* | 5.6 |
| Adams et al., 1983 (29) | 33 | —† | — |
| Hermann et al., 2004 (30) | 53 | 19‡ | 36 |
| Pflipsen et al., 2009 (31) | 195 | 44 | 23 |
| Qureshi et al., 2001 (32) | 70 | 23 | 33 |
| Calvo Romero and Ramiro Lozano, 2012 (33) | 81 | 7 | 8.6 |
| Sato et al., 2013 (34) | 62 | 8 | 13 |
Twenty-one individuals (30%) were identified as having B12 malabsorption.
Twelve individuals (36%) were identified as having B12 malabsorption.
Individuals identified as being deficient had ≥1 abnormal B12 marker (e.g., subnormal/reduced cobalamin, reduced holotranscobalamin, elevated homocysteine, and elevated methylmalonic acid)
Individuals treated with metformin have lower B12 levels and worse diabetic neuropathy than individuals managed with medications other than metformin (37,39). It has been suggested that neuropathy may be the result, in part, of the sequelae of B12 depletion, including elevations in homocysteine and methylmalonic acid levels (37). Although metformin is a common first-line pharmacotherapy and the primary biguanide used for the management of type 2 diabetes, less clinically relevant biguanides, including buformin and phenformin, also have been demonstrated to affect B12 levels (29,40,41).
Mechanisms
Various reports have attributed metformin-induced B12 depletion to:
A metformin-induced decrease in bile acid secretion promoting small intestinal bacterial overgrowth, which, in turn, causes increased intrinsic factor–vitamin B12 complex binding to bacteria and decreased intestinal absorption (40)
Decreased intrinsic factor secretion (29)
Decreased intestinal absorption resulting from metformin’s antagonism of the calcium-dependent B12-intrinsic factor cell surface receptors in the ileum (42)
Mitigation
Vitamin B12 levels have been shown to improve as a result of:
Administration of the antibiotic doxycycline (100 mg daily for 8 days) (40)
Oral calcium supplementation (42)
A study examining individuals undergoing metformin therapy for 4 months examined the potential for calcium supplementation to aid in the mitigation of B12 malabsorption. After 3 months of metformin therapy, calcium carbonate, 1.2 g/day, was administered for 1 month. From the third to the fourth month, serum holotranscobalamin II levels increased by 53 ± 15% (42).
Histamine H2 Receptor Antagonist/Proton Pump Inhibitor–Induced Vitamin B12 Depletion
In general, acid suppressors including both histamine H2 receptor antagonists (H2RAs) and proton pump inhibitors (PPIs) have been documented to interfere with B12 absorption (43–47). In 1980, Steinberg et al. (48) found that, while undergoing treatment with H2RAs, patients were able to absorb unbound B12 (i.e., B12 from a vitamin supplement) but not protein-bound B12 (i.e., B12 from food sources). Numerous subsequent articles have also reported H2RA-induced B12 depletion (49–51). When protein-bound B12 absorption was assessed before and after H2RA therapy, a 53% drop in absorption was noted (from 5.3% before treatment to 2.5% after treatment) (49). When protein-bound B12 absorption was assessed before and after ranitidine therapy, an 89% drop in absorption was noted (from 7.66% before treatment to 0.84% after treatment) (52). Other studies analyzing ranitidine have also noted decreases in B12 (53). In addition to H2RAs, studies have noted an inverse correlation between duration of PPI therapy and B12 levels (54–57).
Mechanisms
Various reports have attributed acid suppressor–induced B12 depletion to decreased gastric acid, pepsin, and intrinsic factor output (49,50,53,58,59).
Mitigation
In H2RA-induced B12 depletion, B12 levels have been shown to improve as a result of:
B12 supplementation as crystalline B12 in the form of oral supplementation, as opposed to protein-bound B12 ingestion (from food sources) (43,49,51)
In PPI-induced B12 depletion, strategies to improve B12 levels include:
B12 supplementation, potentially in dosages beyond recommended daily allowance levels, including administration via cyanocobalamin nasal spray, 500 µg in one nostril once weekly for 8 weeks) (44,56,57)
Genotyping; S-mephenytoin hyd-roxylase, a polymorphic cytochrome P450 (CYP) enzyme identified as CYP2C19, catalyzes the metabolism of PPIs (60). The polymorphism of S-mephenytoin hydroxylase has been shown to influence B12 levels in those using PPIs. Therefore, genotyping may be useful in identifying individuals with a greater predisposition to B12 depletion while undergoing long-term PPI therapy (60). Those who poorly metabolize PPIs would have increased acid suppression and therefore more interference with B12 absorption. Conversely, those with elevated metabolism of PPIs would have poor acid suppression and less interference with B12 absorption.
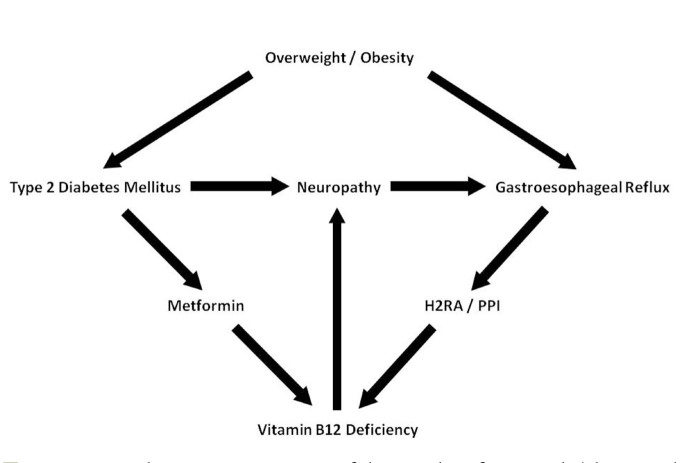
Figure 1 shows a schematic flowchart of the sequelae resulting from type 2 diabetes and GERD managed with metformin and acid-suppressing medications.
FIGURE 1.
Schematic representation of the sequelae of overweight/obesity and type 2 diabetes with regard to neuropathy and GERD. A positive feedback exists among neuropathy, GERD, management with acid-suppressing medications, and vitamin B12 deficiency. The figure illustrates an additive effect of concomitant metformin and acid-suppression therapy leading to neuropathy via compounded vitamin B12 depletion.
Discussion
Prevalence rates of both obesity and type 2 diabetes continue to increase over time (1,61). As previously mentioned, 70% of people with diabetes take oral antidiabetic agents, and 40.7% have symptomatic GERD. Thus, millions of people are most likely managing hyperglycemia and GERD concomitantly with oral medications (1,7). Additionally, PPIs and H2RAs are often overused (62). Regardless of the appropriateness of acid-suppressing medication use, in 2013 the acid-suppressing PPI esomeprazole was second in sales only to the antipsychotic aripiprazole (63). Given the increases in obesity and type 2 diabetes prevalence rates and the high consumption of PPIs, the potential exists for increasing concomitant use of antidiabetic and acid-suppressing medications.
Monotherapy with either metformin, an H2RA, or a PPI can deplete vitamin B12. In a recent study, 22.2% of individuals in a nondiabetic control group were found to be B12 deficient, an incidence that did not differ statistically from that of the experimental groups of metformin users (21.9%) or PPI users (25.6%). However, a significant difference was found between control subjects and the 34.2% of concomitant users of metformin and PPI who were B12 deficient (64). This study supports the notion that concomitant therapy has an additive effect. Because metformin and acid-suppressing medications have been demonstrated to deplete B12 independently and to have a compounded effect when used concomitantly, it is important to recognize the potential for neuropathy to develop as a result of this likely polypharmacy scenario.
Pharmacists, clinicians, and patients need to be aware of the potential for polypharmacy-induced B12 depletion and the potential for subsequent neuropathy. Awareness is particularly important because metformin and acid-suppressing medications are commonly used in the diabetic population, which has a high prevalence of neuropathy (60–70%) (1). Thus, what is generally thought of as “diabetic” neuropathy may be, at least in part, B12 deficiency–induced neuropathy resulting from the concomitant use of these medications. Health care providers and people with diabetes also should be aware of the many strategies and alternatives that have been shown to improve B12 deficiency and resultant neuropathy.
Duality of Interest
No potential conflicts of interest relevant to this article were reported.
References
- 1.Centers for Disease Control and Prevention National diabetes fact sheet: national estimates and general information on diabetes and prediabetes in the United States, 2011. Atlanta, Ga, U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, 2011 [Google Scholar]
- 2.Hampel H, Abraham NS, El-Serag HB. Meta-analysis: obesity and the risk for gastroesophageal reflux disease and its complications. Ann Intern Med 2005;143:199–211 [DOI] [PubMed] [Google Scholar]
- 3.Friedenberg FK, Xanthopoulos M, Foster GD, Richter JE. The association between gastroesophageal reflux disease and obesity. Am J Gastroenterol 2008;103:2111–2122 [DOI] [PubMed] [Google Scholar]
- 4.Lee SD, Keum B, Chun HJ, Bak YT. Gastroesophageal reflux disease in type II diabetes mellitus with or without peripheral neuropathy. J Neurogastroenterol Motil 2011;17:274–278 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Promberger R, Lenglinger J, Riedl O, et al. . Gastro-esophageal reflux disease in type 2 diabetics: symptom load and pathophysiologic aspects: a Retro-Pro study. BMC Gastroenterol 2013;13:132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lluch I, Ascaso JF, Mora F, et al. . Gastroesophageal reflux in diabetes mellitus. Am J Gastroenterol 1999;94:919–924 [DOI] [PubMed] [Google Scholar]
- 7.Wang X, Pitchumoni CS, Chandrarana K, Shah N. Increased prevalence of symptoms of gastroesophageal reflux diseases in type 2 diabetics with neuropathy. World J Gastroenterol 2008;14:709–712 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Nishida T, Tsuji S, Tsujii M, et al. . Gastroesophageal reflux disease related to diabetes: analysis of 241 cases with type 2 diabetes mellitus. J Gastroenterol Hepatol 2004;19:258–265 [DOI] [PubMed] [Google Scholar]
- 9.Allen RH, Stabler SP, Savage DG, Lindenbaum J. Metabolic abnormalities in cobalamin (vitamin B12) and folate deficiency. FASEB J 1993;7:1344–1353 [DOI] [PubMed] [Google Scholar]
- 10.Takahashi-Iñiguez T, García-Hernandez E, Arreguín-Espinosa R, Flores ME. Role of vitamin B12 on methylmalonyl-CoA mutase activity. J Zhejiang Univ Sci B 2012;13:423–437 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.National Institutes of Health Office of Dietary Supplements Vitamin B12 dietary supplement fact sheet. Available from http://ods.od.nih.gov/factsheets/VitaminB₁₂-HealthProfessional. Accessed 23 April 2014.
- 12.Steiner I, Kidron D, Soffer D, Wirguin I, Abramsky O. Sensory peripheral neuropathy of vitamin B12 deficiency: a primary demyelinating disease? J Neurol 1988;235:163–164 [DOI] [PubMed] [Google Scholar]
- 13.Healton EB, Savage DG, Brust JC, Garrett TJ, Lindenbaum J. Neurologic aspects of cobalamin deficiency. Medicine (Baltimore) 1991;70:229–245 [DOI] [PubMed] [Google Scholar]
- 14.Misra UK, Kalita J, Das A. Vitamin B12 deficiency neurological syndromes: a clinical, MRI and electrodiagnostic study. Electromyogr Clin Neurophysiol 2003;43:57–64 [PubMed] [Google Scholar]
- 15.Kalita J, Chandra S, Bhoi SK, et al. . Clinical, nerve conduction and nerve biopsy study in vitamin B12 deficiency neurological syndrome with a short-term follow-up. Nutr Neurosci 2014;17:156–163 [DOI] [PubMed] [Google Scholar]
- 16.Ide H, Fujiya S, Asanuma Y, Tsuji M, Sakai H, Agishi Y. Clinical usefulness of intrathecal injection of methylcobalamin in patients with diabetic neuropathy. Clin Ther 1987;9:183–192 [PubMed] [Google Scholar]
- 17.Yaqub BA, Siddique A, Sulimani R. Effects of methylcobalamin on diabetic neuropathy. Clin Neurol Neurosurg 1992;94:105–111 [DOI] [PubMed] [Google Scholar]
- 18.Sun Y, Lai MS, Lu CJ. Effectiveness of vitamin B12 on diabetic neuropathy: systematic review of clinical controlled trials. Acta Neurol Taiwan 2005;14:48–54 [PubMed] [Google Scholar]
- 19.Walker MJ Jr, Morris LM, Cheng D. Improvement of cutaneous sensitivity in diabetic peripheral neuropathy with combination L-methylfolate, methylcobalamin, and pyridoxal 5’-phosphate. Rev Neurol Dis 2010;7:132–139 [PubMed] [Google Scholar]
- 20.Jacobs AM, Cheng D. Management of diabetic small-fiber neuropathy with combination L-methylfolate, methylcobalamin, and pyridoxal 5’-phosphate. Rev Neurol Dis 2011;8:39–47 [PubMed] [Google Scholar]
- 21.Kuwabara S, Nakazawa R, Azuma N, et al. . Intravenous methylcobalamin treatment for uremic and diabetic neuropathy in chronic hemodialysis patients. Intern Med 1999;38:472–475 [DOI] [PubMed] [Google Scholar]
- 22.Li G. Effect of mecobalamin on diabetic neuropathies: Beijing Methycobal Clinical Trial Collaborative Group. Zhonghua Nei Ke Za Zhi 1999;38:14–17 [PubMed] [Google Scholar]
- 23.Talaei A, Siavash M, Majidi H, Chehrei A. Vitamin B12 may be more effective than nortriptyline in improving painful diabetic neuropathy. Int J Food Sci Nutr 2009;5:71–76 [DOI] [PubMed] [Google Scholar]
- 24.Farvid MS, Homayouni F, Amiri Z, Adelmanesh F. Improving neuropathy scores in type 2 diabetic patients using micronutrients supplementation. Diabetes Res Clin Pract 2011;93:86–94 [DOI] [PubMed] [Google Scholar]
- 25.Dominguez JC, Ng AR, Damian LF. A prospective, open label, 24-week trial of methylcobalamin in the treatment of diabetic polyneuropathy. J Diabetes Mellit 2012;2:408–412 [Google Scholar]
- 26.Institute of Medicine Dietary Reference Intakes for Thiamin, Riboflavin, Niacin, Vitamin B6, Folate, Vitamin B12, Pantothenic Acid, Biotin, and Choline. Washington, D.C, National Academies Press, 1998 [PubMed] [Google Scholar]
- 27.Berchtold P, Bolli P, Arbenz U, Keiser G. Disturbance of intestinal absorption following metformin therapy (observations on the mode of action of biguanides). Diabetologia 1969;5:405–412 [DOI] [PubMed] [Google Scholar]
- 28.Tomkin GH, Hadden DR, Weaver JA, Montgomery DA. Vitamin B12 status of patients on long-term metformin therapy. BMJ 1971;2:685–687 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Adams JF, Clark JS, Ireland JT, Kesson CM, Watson WS. Malabsorption of vitamin B12 and intrinsic factor secretion during biguanide therapy. Diabetologia 1983;24:16–18 [DOI] [PubMed] [Google Scholar]
- 30.Hermann L, Nilsson B, Wettre S. Vitamin B12 status of patients treated with metformin: a cross-sectional cohort study. Br J Diabetes Vasc Dis 2004;4:401–406 [Google Scholar]
- 31.Pflipsen MC, Oh RC, Saguil A, Seehusen DA, Seaquist D, Topolski R. The prevalence of vitamin B(12) deficiency in patients with type 2 diabetes: a cross-sectional study. J Am Board Fam Med 2009;22:528–534 [DOI] [PubMed] [Google Scholar]
- 32.Qureshi SA, Ainsworth A, Winocour PH. Metformin therapy and assessment for vitamin B12 deficiency: is it necessary? Pract Diabetes 2001;28:302–304 [Google Scholar]
- 33.Calvo Romero JM, Ramiro Lozano JM. Vitamin B(12) in type 2 diabetic patients treated with metformin. Endocrinol Nutr 2012;59:487–490 [DOI] [PubMed] [Google Scholar]
- 34.Sato Y, Ouchi K, Funase Y, Yamauchi K, Aizawa T. Relationship between metformin use, vitamin B12 deficiency, hyperhomocysteinemia and vascular complications in patients with type 2 diabetes. Endocr J 2013;60:1275–1280 [DOI] [PubMed] [Google Scholar]
- 35.Pongchaidecha M, Srikusalanukul V, Chattananon A, Tanjariyaporn S: Effect of metformin on plasma homocysteine, vitamin B12 and folic acid: a cross-sectional study in patients with type 2 diabetes mellitus. J Med Assoc Thai 2004;87:780–787 [PubMed] [Google Scholar]
- 36.Ting RZ, Szeto CC, Chan MH, Ma KK, Chow KM. Risk factors of vitamin B(12) deficiency in patients receiving metformin. Arch Intern Med 2006;166:1975–1979 [DOI] [PubMed] [Google Scholar]
- 37.Wile DJ, Toth C. Association of metformin, elevated homocysteine, and methylmalonic acid levels and clinically worsened diabetic peripheral neuropathy. Diabetes Care 2010;33:156–161 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Gatford KL, Houda CM, Lu ZX, et al. . Vitamin B12 and homocysteine status during pregnancy in the metformin in gestational diabetes trial: responses to maternal metformin compared with insulin treatment. Diabetes Obes Metab 2013;15:660–667 [DOI] [PubMed] [Google Scholar]
- 39.Singh AK, Kumar A, Karmakar D, Jha RK. Association of B12 deficiency and clinical neuropathy with metformin use in type 2 diabetes patients. J Postgrad Med 2013;59:253–257 [DOI] [PubMed] [Google Scholar]
- 40.Caspary WF, Zavada I, Reimold W, Deuticke U, Emrich D, Willms B. Alteration of bile acid metabolism and vitamin B12 absorption in diabetics on biguanides. Diabetologia 1977;13:187–193 [DOI] [PubMed] [Google Scholar]
- 41.Müller P, Fischer H, Sorger D. Vitamin B12 level in serum of diabetics receiving long-term buformin therapy. Z Gesamte Inn Med 1981;36:226–228 [PubMed] [Google Scholar]
- 42.Bauman WA, Shaw S, Jayatilleke E, Spungen AM, Herbert V. Increased intake of calcium reverses vitamin B12 malabsorption induced by metformin. Diabetes Care 2000;23:1227–1231 [DOI] [PubMed] [Google Scholar]
- 43.Mitchell SL, Rockwood K. The association between antiulcer medication and initiation of cobalamin replacement in older persons. J Clin Epidemiol 2001;54:531–534 [DOI] [PubMed] [Google Scholar]
- 44.Force RW, Meeker AD, Cady PS, Culbertson VL, Force WS, Kelley CM. Ambulatory care increased vitamin B12 requirement associated with chronic acid suppression therapy. Ann Pharmacother 2003;37:490–493 [DOI] [PubMed] [Google Scholar]
- 45.Valuck RJ, Ruscin JM. A case-control study on adverse effects: H2 blocker or proton pump inhibitor use and risk of vitamin B12 deficiency in older adults. J Clin Epidemiol 2004;57:422–428 [DOI] [PubMed] [Google Scholar]
- 46.DeVault KR, Talley NJ. Insights into the future of gastric acid suppression. Nat Rev Gastroenterol Hepatol 2009;6:524–532 [DOI] [PubMed] [Google Scholar]
- 47.Lam JR, Schneider JL, Zhao W, Corley DA. Proton pump inhibitor and histamine 2 receptor antagonist use and vitamin B12 deficiency. JAMA 2013;310:2435–2442 [DOI] [PubMed] [Google Scholar]
- 48.Steinberg WM, King CE, Toskes PP. Malabsorption of protein-bound cobalamin but not unbound cobalamin during cimetidine administration. Dig Dis Sci 1980;25:188–191 [DOI] [PubMed] [Google Scholar]
- 49.Salom IL, Silvis SE, Doscherholmen A. Effect of cimetidine on the absorption of vitamin B12. Scand J Gastroenterol 1982;17:129–131 [DOI] [PubMed] [Google Scholar]
- 50.Aymard JP, Aymard B, Netter P, Bannwarth B, Trechot P, Streiff F. Haematological adverse effects of histamine H2-receptor antagonists. Med Toxicol Adverse Drug Exp 1988;3:430–448 [DOI] [PubMed] [Google Scholar]
- 51.Ruscin JM, Page RL 2nd, Valuck RJ. Vitamin B(12) deficiency associated with histamine(2)-receptor antagonists and a proton-pump inhibitor. Ann Pharmacother 2002;36:812–816 [DOI] [PubMed] [Google Scholar]
- 52.Kirch W, Hoensch H, Janisch HD. Interactions and non-interactions with ranitidine. Clin Pharmacokinet 1984;9:493–510 [DOI] [PubMed] [Google Scholar]
- 53.Bélaïche J, Zittoun J, Marquet J, Nurit Y, Yvart J. Effect of ranitidine on secretion of gastric intrinsic factor and absorption of vitamin B12. Gastroenterol Clin Biol 1983;7:381–384 [PubMed] [Google Scholar]
- 54.Termanini B, Gibril F, Sutliff VE, Yu F, Venzon DJ, Jensen RT. Effect of long-term gastric acid suppressive therapy on serum vitamin B12 levels in patients with Zollinger-Ellison syndrome. Am J Med 1998;104:422–430 [DOI] [PubMed] [Google Scholar]
- 55.Hirschowitz BI, Worthington J, Mohnen J. Vitamin B12 deficiency in hypersecretors during long-term acid suppression with proton pump inhibitors. Aliment Pharmacol Ther 2008;27:1110–1121 [DOI] [PubMed] [Google Scholar]
- 56.Dharmarajan TS, Kanagala MR, Murakonda P, Lebelt AS, Norkus EP. Do acid-lowering agents affect vitamin B12 status in older adults? J Am Med Dir Assoc 2008;9:162–167 [DOI] [PubMed] [Google Scholar]
- 57.Rozgony NR, Fang C, Kuczmarski MF, Bob H. Vitamin B(12) deficiency is linked with long-term use of proton pump inhibitors in institutionalized older adults: could a cyanocobalamin nasal spray be beneficial? J Nutr Elder 2010;29:87–99 [DOI] [PubMed] [Google Scholar]
- 58.Festen HP. Intrinsic factor secretion and cobalamin absorption: physiology and pathophysiology in the gastrointestinal tract. Scand J Gastroenterol Suppl 1991;188:1–7 [DOI] [PubMed] [Google Scholar]
- 59.Force RW, Nahata MC. Effect of histamine H2-receptor antagonists on vitamin B12 absorption. Ann Pharmacother 1992;26:1283–1286 [DOI] [PubMed] [Google Scholar]
- 60.Sagar M, Janczewska I, Ljungdahl A, Bertilsson L, Seensalu R. Effect of CYP2C19 polymorphism on serum levels of vitamin B12 in patients on long-term omeprazole treatment. Aliment Pharmacol Ther 1999;13:453–458 [DOI] [PubMed] [Google Scholar]
- 61.Flegal KM, Carroll MD, Ogden CL, Curtin LR. Prevalence and trends in obesity among U.S. adults, 1999–2008. JAMA 2010;303:235–241 [DOI] [PubMed] [Google Scholar]
- 62.Heidelbaugh JJ, Kim AH, Chang R, Walker PC. Overutilization of proton-pump inhibitors: what the clinician needs to know. Therap Adv Gastroenterol 2012;5:219–232 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Drugs.com U.S. pharmaceutical sales—2013. Available from http://www.drugs.com/stats/top100/2013/sales. Accessed 23 April 2014.
- 64.Long AN, Atwell CL, Yoo W, Solomon SS. Vitamin B(12) deficiency associated with concomitant metformin and proton pump inhibitor use. Diabetes Care 2012;35:e84. [DOI] [PMC free article] [PubMed] [Google Scholar]