Abstract
Background
Appendicitis remains a common indication for urgent surgical intervention in the United States, and early appendectomy has long been advocated to mitigate the risk of appendiceal perforation. To better quantify the risk of perforation associated with delayed operative timing, this study examines the impact of length of inpatient stay preceding surgery on rates of perforated appendicitis in both adults and children.
Methods
This study was a cross-sectional analysis using the National Inpatient Sample and Kids’ Inpatient Database from 1988–2008. We selected patients with a discharge diagnosis of acute appendicitis (perforated or nonperforated) and receiving appendectomy within 7 d after admission. Patients electively admitted or receiving drainage procedures before appendectomy were excluded. We analyzed perforation rates as a function of both age and length of inpatient hospitalization before appendectomy.
Results
Of 683,590 patients with a discharge diagnosis of appendicitis, 30.3% were recorded as perforated. Over 80% of patients underwent appendectomy on the day of admission, approximately 18% of operations were performed on hospital days 2–4, and later operations accounted for <1% of cases. During appendectomy on the day of admission, the perforation rate was 28.8%; this increased to 33.3% for surgeries on hospital day 2 and 78.8% by hospital day 8 (P < 0.001). Adjusted for patient, procedure, and hospital characteristics, odds of perforation increased from 1.20 for adults and 1.08 for children on hospital day 2 to 4.76 for adults and 15.42 for children by hospital day 8 (P < 0.001).
Conclusions
Greater inpatient delay before appendectomy is associated with increased perforation rates for children and adults within this population-based study. These findings align with previous studies and with the conventional progressive pathophysiologic appendicitis model. Randomized prospective studies are needed to determine which patients benefit from nonoperative versus surgically aggressive management strategies for acute appendicitis.
Keywords: Surgical outcomes, National Inpatient Sample, Kids’ Inpatient Database, Acute appendicitis, Perforated appendicitis, Appendectomy, Delayed operation
1. Introduction
Acute appendicitis is the most common indication for emergent surgical procedures in the United States. It affects approximately 250,000 patients each year [1], including 77,000 children [2]. Lifetime incidence for appendicitis is 8.6% for males and 6.7% for females, with maximal incidence at age 10–14 y in males and 15–19 in females [3]. After a period in which research focused primarily on options for surgical management, including laparoscopy [4] and selective nonoperative management [5], attention has increasingly turned to operative timing during the index admission. The conventional disease model for acute appendicitis was described in the early 20th century [6,7], which proposes a progressive inflammatory process triggered by luminal obstruction of the appendix and culminating in perforation resulting from infection and ischemic necrosis. The presumptive time-dependent progression from appendiceal inflammation to rupture and abscess formation has served as the primary justification for prompt surgical intervention.
By this paradigm, delay of either antibiotic administration or appendectomy is deleterious, because it permits the pathologic process of appendicitis to proceed unchecked toward perforation. Impediments to immediate treatment may occur at multiple points as the patient proceeds through the health care system: in the pre-hospital setting, patients may not immediately seek treatment for symptoms; in the outpatient clinic or Emergency Department, providers may not diagnose the condition or refer appropriately; and even after diagnosis and hospital admission, facilities may be inadequately equipped or staffed to provide timely surgery. The present study sought to examine the specific interval of delay separating hospital admission and appendectomy using a nationwide discharge database. In comparing patients receiving same-day appendectomy with those whose operation was delayed, we were able to attempt to quantify the increased risk of an operative finding of perforated appendicitis resulting from delay in surgical treatment after hospital presentation.
2. Methods
2.1. Data acquisition
We performed a retrospective analysis using a combination of the Nationwide Inpatient Sample (NIS) (1988–2008) and the Kids’ Inpatient Database (KID) (1997, 2000, 2003, and 2006). Both the NIS and KID have been developed as part of the Healthcare Cost and Utilization Project (HCUP) of the Agency for Healthcare Research and Quality. The NIS is an all-payer database that currently compiles information on up to 8.16 million inpatient discharges across the United States each year. Hospitals are selected to represent a 20% stratified sample of all community hospitals. Data from 759–1056 hospitals located in eight to 42 states were available in the data set under study [8]. The KID contains a sample of pediatric (age ≤20) discharges from all community, non-rehabilitation hospitals from states that participate in HCUP. The KID samples 1.91–3.13 million patient discharges, rather than sampling at the hospital level like the NIS. Patient discharges are then weighted to obtain national estimates. The KID contains information from 2521–3739 hospitals in 22–38 states over the period studied [9]. Because of overlap between the NIS and KID for the years 1997, 2000, 2003, and 2006, we used only KID data when selecting pediatric cases for these years.
The Institutional Review Board of Johns Hopkins Medicine deemed this study exempt. The data use agreement from Agency for Healthcare Research and Quality and HCUP does not allow the reporting of information when the number of observations is ≤10, to help maintain patient confidentiality. Therefore, we have entered “≤10” in cases where there were 10 or fewer observations in any category. We calculated the reported P values and confidence intervals using the exact number of observations obtained in the analysis. All statistical analyses were performed using Stata MP, version 11 (College Station, TX).
We initially selected patients from the NIS and KID databases if they had an International Classification of Diseases, 9th Revision (ICD-9) diagnosis code corresponding to acute appendicitis, with (540 and 540.9) or without evidence of perforation (540.0 and 540.1), and International Classification of Diseases, Clinical Modification (ICD-9-CM) procedure codes for therapeutic open or laparoscopic appendectomy (470, 470.1, and 470.9). We excluded patients with admission types designated as other than “emergent” or “urgent,” as well as patients who underwent simple abdominal drainage before appendectomy (ICD-9 CM procedure codes 472, 472.0, and 54.91). Both NIS and KID report the interval (in calendar days) that separates hospital admission from inpatient surgical procedures; we excluded patients receiving surgery more than 7 d after admission to avoid capturing interval appendectomy.
2.2. Data analysis
We performed a descriptive analysis using variables of gender, race, insurancestatus (uninsured or insured), geographic region (Northeast, Midwest, South, or West), type of hospital (urban teaching, urban non-teaching, or rural) and type of surgical procedure performed (laparoscopic or open appendectomy). We performed comparisons between groups (perforated and nonperforated) using Pearson's chi-square for categorical variables and the Kruskal-Wallis test for non-normally distributed continuous variables.
For analysis of outcome associated with increasing delay of surgery after admission, we performed multiple logistic regression to assess the risk of perforation associated with each interval. This multivariate analysis controlled for the variables of age, gender, race, insurance status, geographic region, type of hospital, type of surgical procedure (laparoscopic or open appendectomy), and comorbid conditions. We assessed the number of comorbid conditions by counting the number of unique ICD-9 codes associated with each admission. We calculated odds ratios using the immediate operation (occurring on the same day as admission) as the reference group.
3. Results
3.1. Patient demographics and hospital characteristics
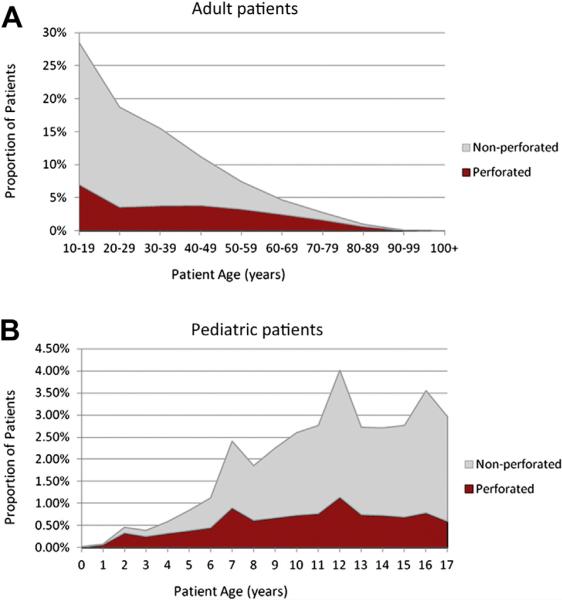
We identified a total of 683,590 discharged patients who met inclusion criteria; of these, 450,858 (66%) were adults (age >18 y) and 232,732 were children. Figure 1 provide age distributions for perforated and nonperforated cases. A total of 400,352 patients (59%) were male, and 388,879 patients (57%) were white (Table 1). Most patients were treated in hospitals in the South (34%) and Northeast (25%); 85% of admissions were to urban hospitals, most of which were non-teaching institutions (47% of all discharges).
Fig. 1.
Age at presentation for acute perforated and nonperforated appendicitis. (A) Adult patients. (B) Pediatric patients. (Color version of figure is available online.)
Table 1.
Patient characteristics.
| Nonperforated | Perforated | P value | |||
|---|---|---|---|---|---|
| Adult | |||||
| Male, n (%) | 176,101 | (56.3) | 81,760 | (59.2) | <0.001 |
| Age, y, mean (SD) | 36.0 | (14.6) | 45.9 | (17.8) | <0.001 |
| Race, n (%) | <0.001 | ||||
| White | 181,415 | (58.0) | 83,339 | (60.3) | |
| Black | 17,300 | (5.5) | 8012 | (5.8) | |
| Hispanic | 36,838 | (11.8) | 13,189 | (9.5) | |
| Other/unspecified | 77,078 | (24.7) | 33,687 | (24.4) | |
| Insured, n (%) | 248,028 | (79.3) | 111,884 | (80.9) | <0.001 |
| Comorbid diagnoses, mean (SD) | 2.19 | (1.89) | 3.73 | (2.88) | <0.001 |
| Total | 312,631 | (69.3) | 138,227 | (30.7) | |
| Pediatric | |||||
| Male, n (%) | 100,018 | (61.1) | 42,473 | (61.4) | 0.174 |
| Age, y, mean (SD) | 12.0 | (3.6) | 10.5 | (4.1) | <0.001 |
| Race, n (%) | <0.001 | ||||
| White | 90,432 | (55.3) | 33,693 | (48.7) | |
| Black | 9099 | (5.6) | 5080 | (7.4) | |
| Hispanic | 25,578 | (15.6) | 13,507 | (19.5) | |
| Other/unspecified | 38,487 | (23.5) | 16,856 | (24.4) | |
| Insured, n (%) | 144,062 | (88.1) | 59,787 | (86.5) | <0.001 |
| Comorbid diagnoses, mean (SD) | 1.46 | (0.93) | 2.31 | (1.72) | <0.001 |
| Total | 163,596 | (70.3) | 69,136 | (29.7) | |
SD = standard deviation.
3.2. Case characteristics
Most patients (70%; n = 476,192) were discharged with a diagnosis of uncomplicated acute appendicitis; 207,346 were discharged with a diagnosis of acute appendicitis complicated by peritonitis or intra-abdominal abscess. A total of 72% of patients (n = 493,191) were treated with open appendectomy and 190,399 patients received laparoscopic appendectomy. A total of 554,368 procedures (81.1%) were performed on the day of admission and 107,989 (15.8%) were performed on the second hospital day. Thereafter, the number of procedures decreased from 11,638 (1.7%) on the third hospital day to 560 (0.1%) by hospital day 8. The proportion of appendectomies performed on the day of admission ranged from 79.0%–82.5% for each of the years studied, with a significant trend toward earlier appendectomy in more recent admission years (P = 0.015).
Pediatric patients were significantly more likely to have perforation at the time of operation, and were more likely to receive open appendectomy than were adult patients (P < 0.001); children also received surgical intervention earlier in their hospital course than did adults (P < 0.001). Examined separately, patients at both extremes of age were significantly more likely to have perforated appendicitis at operation. Male patients were more likely to experience perforation, independent of age (Table 1). With respect to hospitals, most patients were seen in the South region and in urban, non-teaching hospitals. Patients with perforated appendicitis had longer inpatient admissions, with a median length of stay of 5 d (interquartile range [IQR] 3–7 d), versus 2 d (IQR 1–3 d) for patients with uncomplicated appendicitis. Patients with perforated appendicitis also had higher total hospital charges (adjusted for inflation to 2008 US dollars); median charges were $18,034 (IQR 11,869–27,786) versus $11,081 (IQR 7327–16,925) for patients with uncomplicated appendicitis.
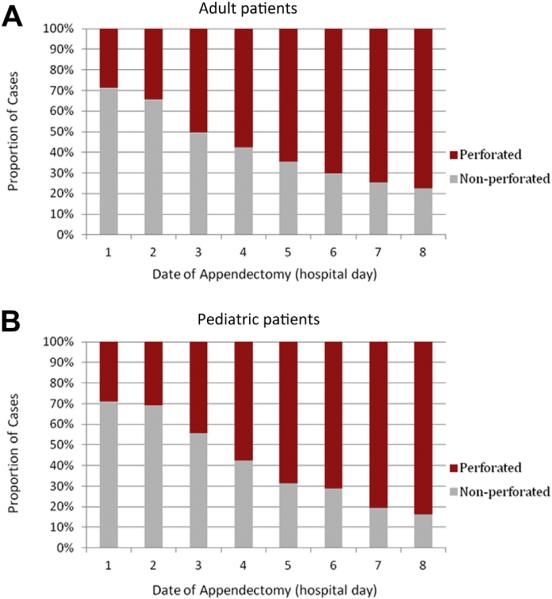
Patients undergoing appendectomy on the day of admission had an overall rate of perforation of 28.8%. The rate of perfo-ration progressively increased with each additional interval day between admission and appendectomy, reaching 78.8% by the eighth hospital day (P < 0.001). This association was independent of patient age, with the proportion of perforated cases rising from 28.7% to 77.4% for adult patients (Fig. 2A) and from 28.9% to 83.8% for children (Fig. 2B). After adjusting for patient, procedural, and hospital factors, as well as for year of admission, the odds ratio for perforation when appendectomy was performed on the second hospital day was 1.10 (95% confidence interval [CI]: 1.08–1.13) for adults and 0.96 (95% CI: 0.92–1.01) for children, relative to appendectomy performed at admission. We observed increasing odds ratios for perforation for each additional intervening day between admission and operation. Relative to immediate appendectomy, a delay of 7 d was associated with an odds ratio of 2.79 (95% CI: 2.12–3.67) for adults and 9.53 (95% CI: 5.03–18.05) for children (Table 2).
Fig. 2.
Proportion of perforated and nonperforated appendicitis displayed by interval between admission and appendectomy. (A) Adult patients. (B) Pediatric patients. (Color version of figure is available online.)
Table 2.
Adjusted risk of perforation.*
| Adult |
Pediatric |
|
|---|---|---|
| odds ratio (95% CI) | odds ratio (95% CI) | |
| Day of admission (1) | Ref | Ref |
| Hospital day 2 | 1.10 (1.08-1.13) | 0.96 (0.92-1.01) |
| Hospital day 3 | 1.63 (1.54-1.73) | 1.33 (1.20-1.48) |
| Hospital day 4 | 1.79 (1.64-1.96) | 2.47 (2.02-3.04) |
| Hospital day 5 | 2.25 (1.98-2.54) | 3.35 (2.58-4.35) |
| Hospital day 6 | 2.74 (2.32-3.23) | 3.67 (2.52-5.34) |
| Hospital day 7 | 2.52 (2.04-3.11) | 8.29 (4.86-14.16) |
| Hospital day 8 | 2.79 (2.12-3.67) | 9.53 (5.03-18.05) |
Logistic regression, adjusting for procedures performed (open versus laparoscopic appendectomy), patient demographics, number of comorbid diagnoses, hospital characteristics, and admission year.
4. Discussion
The present study demonstrates a significant rise in the risk of perforation in cases of acute appendicitis associated with delay in inpatient surgical management. Results are drawn from the largest sample of inpatient records, 683,590 cases, representing clinical progression of appendicitis, which represent a nationwide sample over a 20-y period. The use of all-payer administrative databases avoids management biases that may exist in single-center retrospective studies or patient registries, and therefore reflects the outcomes generated by the US health care system in aggregate. We observed an overall rate of perforation of 30.3% in the present study, which is similar to rates previously reported in studies at the population level [10].
Delay to surgery independently predicted increased odds of perforation, with escalating risk associated with appendectomy undertaken at progressively later times after admission. This is consistent with the findings of previous single-institution investigations in both adult and pediatric patients. Golladay and Sarrett [11] examined delayed diagnosis in 422 pediatric patients over 7.5 y in the 1980s, finding an 81% perforation rate for patients with delayed diagnosis, versus 28% for those who received a timely diagnosis. Bickell et al [12] reviewed the records of 219 cases of appendicitis treated between 1996 and 1998, and found that perforation rates rose in association with increasing delay between symptom onset and treatment. In that study, patients with untreated symptoms for >36 h had a relative risk of perforation 6.6 times greater than did patients with a shorter symptomatic interval. Ditillo and colleagues [13] similarly examined the interval between onset of symptoms and operation in 1081 adult patients with acute appendicitis between 1998 and 2004, and found that greater delay was associated with worsening pathologic grade of the appendix at appendectomy. Busch et al [14] examined in-hospital delay in 1827 cases of adult appendicitis between 2003 and 2006, and observed a significantly increased perforation rate (29.7% versus 22.7%) when appendectomy was delayed >12 h. In-graham and colleagues [15] analyzed 32,782 patient records from the American College of Surgeons National Surgical Quality Improvement Program database and reported significant differences in perforation rates between when appendectomy was delayed for >12 h versus <6 h, although overall perioperative morbidity was unchanged.
Within the context of the historical model describing the time-dependent pathogenesis of appendicitis, the finding of increased perforation risk with greater delay comes as no surprise. This phenomenon, taken together with the increased morbidity and cost associated with perforation [14,16–22], serves for many as the primary justification for prompt surgical intervention in all cases of acute appendicitis. Indeed, differential perforation rates have been proposed by multiple investigators as a proxy for timely referral and operative intervention and, by extension, as a means to estimate disparities in health care access and quality of care [23–32]. Differences in the rate of escalation of odds ratios between adults and children in this temporal analysis suggest that a more individualized approach in future research examining discrete risk factors for perforation may yield important insights necessary to reconcile conflicting perspectives in the literature.
Alternative models have been proposed that call into question the value of early intervention. The existence of spontaneousresolution ofnonperforatedappendicitisisacknowledged, but estimates of its incidence relative to progressive disease vary widely [33,34], as do accounts of recurrent disease [35]. Some authors have hypothesized the existence of two distinct disease variants, one with greater propensity for perforation [36–38]. Considering the low morbidity of appendectomy, the relative magnitude of risk associated with urgent intervention for nonperforated appendicitis versus the risk entailed with failure of nonoperative management with antibiotic therapy alone remains the subject of active inquiry [5,39,40]. Two recent meta-analyses of randomized prospective studies comparing antibiotic and operative therapy conducted between 1995 and 2011 reached different conclusions regarding the practical implications of the overall findings: One reported that the extant data were inconclusive, and the other determined that management with antibiotics alone is safe and effective [41,42]. Ingraham and colleagues [15] reported no difference in 30-d morbidity when treatment was delayed, despite the increased perforation rate. These data are difficult to reconcile with the traditional understanding of appendicitis and data supporting the desirability of early intervention. Given the breadth of literature supporting a progressive pathophysiologic model and lack of prospectively validated clinical criteria to employ in selecting patients who might benefit from nonoperative management, this debate will likely continue.
Reporting patterns from administrative databases is always susceptible to bias; however, we attempted to control for recognizable factors in this analysis. Changing clinical patterns over time are apparent (e.g., ratio of open to laparoscopic appendectomies), but the question of whether delay in recognition or intervention leads to perforation should not be greatly confounded by advances in practice. Conversely, and to the advantage of these data, the national databases are presumably free of unquantified geographic variation and institutional practice patterns, perhaps relatingmore directly to an unbiased natural history of appendicitis.
Other limitations of this study are largely attributable to the data reporting within the NIS and KID databases. The present study used days from the date of admission as the time variable for its association with perforation. However, this is unable to account for the time of day a patient is admitted or receives an operation. For example, a patient admitted at 10:00 PM who underwent appendectomy 3 h later at 1:00 AM would be assigned to the “second hospital day” category, whereas a patient admitted at 1:00 AM and receiving appendectomy at 10:00 PM on the same calendar day would be assigned to the “day of admission” group. This increases the uncertainty of the findings because it may lead to misclassification of operative intervention as “early” versus “late” and introduce bias into the results reported here. In addition, operative timing was not universally reported, and we excluded approximately 17% of all patients receiving appendectomy for missing data. A post hoc comparison of this excluded cohort revealed no difference in perforation rates (P = 0.351) after controlling for demographic and clinical differences.
A second important limitation is a confounding effect from patients who present to the hospital with appendicitis that has already progressed to perforation. The findings of investigators suggest that perforation in the pre-hospital setting is common and may represent the most significant interval of risk [36–38]. These patients may have been managed differently as inpatients, although it is not possible to identify these cases or adjust for such an effect in our analysis. Although many factors, including diagnostic uncertainty, surgeon availability, or clinical judgment, likely contribute to delays in surgery observed in the present study, it is not possible to ascertain their relative contributions from the data used. Details regarding antibiotic administration are likewise unavailable. The proportionately small numbers of patients receiving appendectomy after the fourth hospital day (0.75%; N = 5101) also raises the question as to whether the association observed between perforation and delay reflects intrinsic differences in this narrow subpopulation. The addition of concurrent diagnoses to adjust the multivariate analysis for patient complexity resulted in smaller odds ratios for perforation, but the association of escalating odds of perforation with greater delay persisted in the results reported here.
Other factors that may influence the patient outcomes were not specifically addressed in this analysis, but are relevant to medical decision making in cases of suspected appendicitis. We included only patients who received an appendectomy, but further review of the NIS and KID data reveal that nonoperative management of acute appendicitis was rare in the population selected. Only 4% of patients admitted with acute appendicitis did not have procedure codes for appendectomy, but over half of thesepatients received other invasive procedures, such as abdominal drainage, cecectomy, and hemicolectomy. Up to 15% of appendectomy specimens do not reveal appendicitis, and negative appendectomy is associated with significant health care costs as well as peri-operative morbidity [43]; however, the present study did not consider the rates of negative appendectomy.
Whereas a growing body of evidence has demonstrated some success in the nonoperative management of patients with appendicitis, to the benefit of selected patients who may safely avoid the risks of surgery [5,39,44], this option has its own inherent risk. Patients receiving appendectomy fare better in this analysis when the operation is performed early, even after adjusting for other factors. These datademonstrate a significant association between inpatient delay preceding operation and the outcome of perforation, which may or may not be causal. Prompt diagnosis of acute appendicitis should be emphasized, irrespective of the ultimate management strategy, to make the safest and most informed decisions regarding patient care.
Acknowledgment
Dr. Abdullah has had full access to all data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Footnotes
Presented at the Academic Surgical Congress, Las Vegas, Nevada, February 16, 2012.
REFERENCES
- 1.Prystowsky JB, Pugh CM, Nagle AP. Current problems in surgery. appendicitis. Curr Probl Surg. 2005;42:688. doi: 10.1067/j.cpsurg.2005.07.005. [DOI] [PubMed] [Google Scholar]
- 2.Guthery SL, Hutchings C, Dean JM, Hoff C. National estimates of hospital utilization by children with gastrointestinal disorders: analysis of the 1997 kids’ inpatient database. J Pediatr. 2004;144:589. doi: 10.1016/j.jpeds.2004.02.029. [DOI] [PubMed] [Google Scholar]
- 3.Addiss DG, Shaffer N, Fowler BS, Tauxe RV. The epidemiology of appendicitis and appendectomy in the United States. Am J Epidemiol. 1990;132:910. doi: 10.1093/oxfordjournals.aje.a115734. [DOI] [PubMed] [Google Scholar]
- 4.Liu Z, Zhang P, Ma Y, et al. Laparoscopy or not: a meta-analysis of the surgical effects of laparoscopic versus open appendicectomy. Surg Laparosc Endosc Percutan Tech. 2010;20:362. doi: 10.1097/SLE.0b013e3182006f40. [DOI] [PubMed] [Google Scholar]
- 5.Andersson RE, Petzold MG. Nonsurgical treatment of appendiceal abscess or phlegmon: a systematic review and meta-analysis. Ann Surg. 2007;246:741. doi: 10.1097/SLA.0b013e31811f3f9f. [DOI] [PubMed] [Google Scholar]
- 6.Van Zwalenburg C. The relation of mechanical distention to the etiology of appendicitis. Ann Surg. 1905;41:437. doi: 10.1097/00000658-190503000-00008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wangensteen OH, Dennis C. Experimental proof of the obstructive origin ofappendicitis in man. AnnSurg. 1939;110:629. doi: 10.1097/00000658-193910000-00011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Agency for Healthcare Research and Quality . Introduction to the HCUP nationwide inpatient sample (NIS) Rockville, MD.: [30.12.2011]. http://www.hcup-us.ahrq.gov/db/nation/nis/NIS_Introduction_2009.jsp/; 2009. [Google Scholar]
- 9.Agency for Healthcare Research and Quality . Introduction to the HCUP kids’ inpatient database (KID) Rockville, MD.: [30.12.2011]. http://www.hcup-us.ahrq.gov/db/nation/kid/kid_2009_introduction.jsp/; 2009. [Google Scholar]
- 10.Flum DR, Morris A, Koepsell T, Dellinger EP. Has misdiagnosis of appendicitis decreased over time? A population-based analysis. JAMA. 2001;286:1748. doi: 10.1001/jama.286.14.1748. [DOI] [PubMed] [Google Scholar]
- 11.Golladay ES, Sarrett JR. Delayed diagnosis in pediatric appendicitis. South Med J. 1988;81:38. doi: 10.1097/00007611-198801000-00008. [DOI] [PubMed] [Google Scholar]
- 12.Bickell NA, Aufses AH, Jr, Rojas M, Bodian C. How time affects the risk of rupture in appendicitis. J Am Coll Surg. 2006;202:401. doi: 10.1016/j.jamcollsurg.2005.11.016. [DOI] [PubMed] [Google Scholar]
- 13.Ditillo MF, Dziura JD, Rabinovici R. Is it safe to delay appendectomy in adults with acute appendicitis? Ann Surg. 2006;244:656. doi: 10.1097/01.sla.0000231726.53487.dd. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Busch M, Gutzwiller FS, Aellig S, et al. In-hospital delay increases the risk of perforation in adults with appendicitis. World J Surg. 2011;35:1626. doi: 10.1007/s00268-011-1101-z. [DOI] [PubMed] [Google Scholar]
- 15.Ingraham AM, Cohen ME, Bilimoria KY, et al. Effect of delay to operation on outcomes in adults with acute appendicitis. Arch Surg. 2010;145:886. doi: 10.1001/archsurg.2010.184. [DOI] [PubMed] [Google Scholar]
- 16.Scher KS, Coil JA. The continuing challenge of perforating appendicitis. Surg Gynecol Obstet. 1980;150:535. [PubMed] [Google Scholar]
- 17.Aiello FA, Gross ER, Krajewski A, et al. Post-appendectomy visits to the emergency department within the global period: a target for cost containment. Am J Surg. 2010;200:357. doi: 10.1016/j.amjsurg.2009.10.010. [DOI] [PubMed] [Google Scholar]
- 18.Fike FB, Mortellaro VE, Juang D, et al. The impact of postoperative abscess formation in perforated appendicitis. J Surg Res. 2011;170:24. doi: 10.1016/j.jss.2011.03.038. [DOI] [PubMed] [Google Scholar]
- 19.Pittman-Waller VA, Myers JG, Stewart RM, et al. Appendicitis: why so complicated? Analysis of 5755 consecutive appendectomies. Am Surg. 2000;66:548. [PubMed] [Google Scholar]
- 20.Harrison MW, Lindner DJ, Campbell JR, Campbell TJ. Acute appendicitis in children: factors affecting morbidity. Am J Surg. 1984;147:605. doi: 10.1016/0002-9610(84)90123-5. [DOI] [PubMed] [Google Scholar]
- 21.Eldar S, Nash E, Sabo E, et al. Delay of surgery in acute appendicitis. Am J Surg. 1997;173:194. doi: 10.1016/s0002-9610(96)00011-6. [DOI] [PubMed] [Google Scholar]
- 22.Ponsky TA, Huang ZJ, Kittle K, et al. Hospital- and patient-level characteristics and the risk of appendiceal rupture and negative appendectomy in children. JAMA. 2004;292:1977. doi: 10.1001/jama.292.16.1977. [DOI] [PubMed] [Google Scholar]
- 23.Braveman P, Schaaf VM, Egerter S, et al. Insurance-related differences in the risk of ruptured appendix. N Engl J Med. 1994;331:444. doi: 10.1056/NEJM199408183310706. [DOI] [PubMed] [Google Scholar]
- 24.Gadomski A, Jenkins P. Ruptured appendicitis among children as an indicator of access to care. Health Serv Res. 2001;36(1 Pt 1):129. [PMC free article] [PubMed] [Google Scholar]
- 25.Bratu I, Martens PJ, Leslie WD, et al. Pediatric appendicitis rupture rate: disparities despite universal health care. J Pediatr Surg. 2008;43:1964. doi: 10.1016/j.jpedsurg.2008.05.013. [DOI] [PubMed] [Google Scholar]
- 26.Krajewski SA, Hameed SM, Smink DS, Rogers SO., Jr Access to emergency operative care: a comparative study between the Canadian and American health care systems. Surgery. 2009;146:300. doi: 10.1016/j.surg.2009.04.005. [DOI] [PubMed] [Google Scholar]
- 27.Camp M, Chang DC, Zhang Y, et al. Provider density and health system facility factors and their relationship to rates of pediatric perforated appendicitis in US counties. Arch Surg. 2010;145:1139. doi: 10.1001/archsurg.2010.271. [DOI] [PubMed] [Google Scholar]
- 28.Nwomeh BC, Chisolm DJ, Caniano DA, Kelleher KJ. Racial and socioeconomic disparity in perforated appendicitis among children: where is the problem? Pediatrics. 2006;117:870. doi: 10.1542/peds.2005-1123. [DOI] [PubMed] [Google Scholar]
- 29.Lee SL, Shekherdimian S, Chiu VY. Effect of race and socioeconomic status in the treatment of appendicitis in patients with equal health care access. Arch Surg. 2011;146:156. doi: 10.1001/archsurg.2010.328. [DOI] [PubMed] [Google Scholar]
- 30.Pieracci FM, Eachempati SR, Barie PS, Callahan MA. Insurance status, but not race, predicts perforation in adult patients with acute appendicitis. J Am Coll Surg. 2007;205:445. doi: 10.1016/j.jamcollsurg.2007.04.010. [DOI] [PubMed] [Google Scholar]
- 31.Smink DS, Fishman SJ, Kleinman K, Finkelstein JA. Effects of race, insurance status, and hospital volume on perforated appendicitis in children. Pediatrics. 2005;115:920. doi: 10.1542/peds.2004-1363. [DOI] [PubMed] [Google Scholar]
- 32.Paquette IM, Zuckerman R, Finlayson SR. Perforated appendicitis among rural and urban patients: implications of access to care. Ann Surg. 2011;253:534. doi: 10.1097/SLA.0b013e3182096d68. [DOI] [PubMed] [Google Scholar]
- 33.Cobben LP, de Van Otterloo AM, Puylaert JB. Spontaneously resolving appendicitis: frequency and natural history in 60 patients. Radiology. 2000;215:349. doi: 10.1148/radiology.215.2.r00ma08349. [DOI] [PubMed] [Google Scholar]
- 34.Heller MB, Skolnick ML. Ultrasound documentation of spontaneously resolving appendicitis. Am J Emerg Med. 1993;11:51. doi: 10.1016/0735-6757(93)90060-o. [DOI] [PubMed] [Google Scholar]
- 35.Barber MD, McLaren J, Rainey JB. Recurrent appendicitis. Br J Surg. 1997;84:110. [PubMed] [Google Scholar]
- 36.Luckmann R. Incidence and case fatality rates for acute appendicitis in California: a population-based study of the effects of age. Am J Epidemiol. 1989;129:905. doi: 10.1093/oxfordjournals.aje.a115224. [DOI] [PubMed] [Google Scholar]
- 37.Andersson RE. The natural history and traditional management of appendicitis revisited: spontaneous resolution and predominance of prehospital perforations imply that a correct diagnosis is more important than an early diagnosis. World J Surg. 2007;31:86. doi: 10.1007/s00268-006-0056-y. [DOI] [PubMed] [Google Scholar]
- 38.Livingston EH, Woodward WA, Sarosi GA, Haley RW. Disconnect between incidence of nonperforated and perforated appendicitis: implications for pathophysiology and management. Ann Surg. 2007;245:886. doi: 10.1097/01.sla.0000256391.05233.aa. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Liu K, Fogg L. Use of antibiotics alone for treatment of uncomplicated acute appendicitis: a systematic review and meta-analysis. Surgery. 2011;150:673. doi: 10.1016/j.surg.2011.08.018. [DOI] [PubMed] [Google Scholar]
- 40.Sakorafas GH, Mastoraki A, Lappas C, et al. Conservative treatment of acute appendicitis: heresy or an effective and acceptable alternative to surgery? Eur J Gastroenterol Hepatol. 2011;23:121. doi: 10.1097/MEG.0b013e32834233b6. [DOI] [PubMed] [Google Scholar]
- 41.Wilms IM, de Hoog DE, de Visser DC, Janzing HM. Appendectomy versus antibiotic treatment for acute appendicitis. Cochrane Database Syst Rev. 2011;11:CD008359. doi: 10.1002/14651858.CD008359.pub2. [DOI] [PubMed] [Google Scholar]
- 42.Varadhan KK, Neal KR, Lobo DN. Safety and efficacy of antibiotics compared with appendicectomy for treatment uncomplicated acute appendicitis: meta-analysis of randomised controlled trials. BMJ. 2012;344:e2156. doi: 10.1136/bmj.e2156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Flum DR, Koepsell T. The clinical and economic correlates of misdiagnosed appendicitis: nationwide analysis. Arch Surg. 2002;137:799. doi: 10.1001/archsurg.137.7.799. discussion 804. [DOI] [PubMed] [Google Scholar]
- 44.Kirby CP, Sparnon AL. Active observation of children with possible appendicitis does not increase morbidity. ANZ J Surg. 2001;71:412. doi: 10.1046/j.1440-1622.2001.02148.x. [DOI] [PubMed] [Google Scholar]